Abstract
Background and Objectives:
Studies of patients with benign pathologic lesions who underwent laparoscopic radical nephroureterectomy (RNU) with preoperative suspicion of upper urinary tract urothelial carcinoma are lacking. The aim of this retrospective cross-sectional study was to evaluate the incidence of benign pathologic lesions on laparoscopic RNU for upper urinary tract tumors that are presumed to be urothelial carcinoma. The clinicopathologic characteristics of these lesions were also determined.
Methods:
Between January 2004 and December 2010, 244 patients underwent laparoscopic RNU for possible upper urinary tract urothelial carcinoma at our institute. Seven (2.9%) had benign lesions at the final pathologic examination. The preoperative features of these patients were investigated, including imaging findings, urine cytologic results, and ureteroscopic findings.
Results:
The 7 patients comprised 5 men and 2 women. The lesions were located in the ureter in 5 patients and in the renal pelvis in 2. All patients underwent preoperative voided urine cytology and cystoscopy. Two patients underwent preoperative ureteroscopy. In 1 patient, definite pathologic lesions were not identified in the surgical specimen. Urinary tract tuberculosis was diagnosed in 1 patient, inflammatory pseudotumor in 2, and fibroepithelial polyps in 1. In 2 patients, stones were detected (stone with atypical papillary urothelial hyperplasia and polypoid ureteritis with ureter stone, respectively) after laparoscopic RNU.
Conclusion:
Benign pathologic lesions were detected in 7 patients (2.9%) who had undergone laparoscopic RNU for upper urinary tract tumors that were presumed to be urothelial carcinoma. The description of these false-positive cases will help improve the preoperative counseling of these patients.
Keywords: Benign, Nephroureterectomy, Upper urinary tract, Urothelial carcinoma
INTRODUCTION
Upper urinary tract (UUT) urothelial carcinoma (UUTUC) arises from the urothelial lining of the urinary tract between the renal calyces and the ureteral orifice. The incidence of these tumors has been increasing over the past 2 decades; at present, they account for approximately 5% to 10% of all renal tumors and 5% of all urothelial carcinomas (UCs).1,2 It is essential that malignant causes of UUT filling defects be differentiated from benign causes to avoid unnecessary radical treatment. However, the clinical presentation of UC and other diseases of the UUT are nonspecific, which means that most of these lesions must be evaluated using imaging modalities. For the detection of most UUT lesions, computed tomographic (CT) urography is superior to excretory urography, ultrasonography, and magnetic resonance imaging.3–6 For patients with UUTUCs, the detection rate is satisfactory: for polypoid lesions between 5 and 10 mm, sensitivity and specificity are 96% and 99%, respectively. Sensitivity drops to 89% for polypoid lesions <5 mm and to 40% for polypoid lesions <3 mm.7,8 However, radiologic findings alone may not be sufficient to distinguish ureteral malignancies from nonneoplastic and inflammatory disorders, because all of these lesions can manifest as focal upper urinary nodules with features suggestive of malignancy. For example, a few rare lesions, including endometriosis, nephrogenic adenoma, mycetomas, malakoplakia, and inflammatory pseudotumors, should be included in the differential diagnosis of UUTUC in some patients with suspicious UUT filling defects.9–11
Radical nephroureterectomy (RNU), either open or laparoscopic, with the excision of a cuff of bladder mucosa, is the gold standard for the management of UUTUCs.12,13 Although chronic kidney disease is a reported consequence of radical nephrectomy for renal cell carcinoma, its prevalence in the UUTUC patient population, both before and after RNU, has not been determined. To our knowledge, studies of patients with benign pathology who undergo laparoscopic RNU with preoperative suspicion of UUTUC are lacking. In our retrospective cross-sectional study of patients with suspected UUTUC who underwent laparoscopic RNU at our institution between 2004 and 2010, we identified 7 patients with benign pathologic lesions within the UUT rather than UC. These 7 cases are described herein.
MATERIALS AND METHODS
Between January 2004 and December 2010, 244 patients admitted to our institution underwent laparoscopic RNU with the excision of a cuff of bladder mucosa. The demographic information and imaging results of all patients were retrieved directly from the medical charts. Laparoscopic RNU was performed by 1 of 4 experienced urologic surgeons. The catheter generally remained in place for approximately 7 days, after which it was removed following cystography.
All patients with suspected UUTUC underwent preoperative CT urography, voided urine cytology, and cystoscopy to exclude concomitant bladder tumors. Typically, CT urography consisted of a multiphasic helical CT protocol. Ureteroscopy was indicated in principle when patients had radiographic findings that were suspicious for UUTUC and/or had gross hematuria originating from the UUT and malignancy could not be ruled out by conventional diagnostic modalities or other etiologies. Ureteroscopy was performed under general anesthesia and was preceded by retrograde pyeloureterography (RGP) and washed urine cytology. All surgically benign specimens were reexamined by dedicated genitourinary pathologists and processed according to standardized procedures. Of the 244 patients in the study period, 7 had benign pathologic lesions. The study protocol was approved by the institutional review board of Asan Medical Center (No. 2013–0283).
RESULTS
Of the 244 patients who underwent RNU for suspected UUTUC, 7 had benign lesions. Thus, the incidence of benign lesions in these patients was 2.9%. The baseline characteristics of the 7 patients, the preoperative study results, and the imaging findings are listed in Tables 1 and 2. The median age of the patients was 55 years (range, 49–64 years). Four patients had flank pain (57.1%), which was the most commonly reported preoperative symptom in this group. In the remaining 3 patients, who lacked specific symptoms associated with UUTUC, the pathology was detected incidentally in 1 (14.3%) during routine workup for gallbladder stones: CT imaging performed for a cholecystectomy detected a 1.6-cm filling defect that was suspected to be UC in the left renal pelvis. In the remaining 2 patients (28.6%), the pathology was detected incidentally during routine workup for lower urinary tract symptoms. Both patients had visited an outpatient clinic for the treatment of benign prostatic hyperplasia. Indeed, 1 patient was treated for 3 years, but the symptoms did not improve. On further evaluation of this patient, small stones were detected in the renal pelvis and ureterovesical junction on ultrasonography; subsequent CT urography identified multifocal wall thickening accompanying a right hydroureteronephrosis and periureteral infiltration. In the other patient, who had symptoms of nocturia and frequent urinary tract infections (as confirmed by urine culture), CT urography detected a 4-cm nodular lesion in the left renal pelvis.
Table 1.
Clinicopathologic Characteristics of the Patients: Chief Symptoms, Laterality, Lesion Location, and Voided Urine Cytologic and Computed Tomographic Results
| Patient | Age (y) | Sex | Chief Symptom | Laterality | Location | Voided Urine Cytology | CT |
|---|---|---|---|---|---|---|---|
| 1 | 62 | M | FP | Left | Proximal ureter | Negative | Mild periureteric fat infiltration and wall thickening in the left proximal ureter |
| 2 | 58 | M | Incidentally discovered during workup for LUTS | Left | Pelvis | Negative | A 4-cm UC involving the left renal pelvis |
| 3 | 52 | M | FP | Right | Midureter | Negative | Ureteral wall enhancement and small soft tissue mass in the right midureter lumen |
| 4 | 55 | F | Incidentally discovered during workup for gallbladder stones | Left | Pelvis | Negative | A 1.6-cm enhancing mass in the left renal pelvis |
| 5 | 49 | M | FP | Left | Midureter | Negative | A 1.5-cm well-enhancing mass in the left midureter with nearly total obstruction |
| 6 | 52 | F | FP | Right | Distal ureter | Negative | Enhancing lesion in the right distal ureter, causing hydroureteronephrosis and decreased renal function |
| 7 | 64 | M | Incidentally discovered during workup for LUTS | Right | Proximal and distal ureter | Negative | Multifocal wall thickening accompanying a right hydroureteronephrosis and periureteral infiltration |
CT, computed tomography; FP, flank pain; LUTS, low urinary tract symptoms; UC, urothelial carcinoma.
Table 2.
Clinicopathologic Characteristics of the Patients: Other Imaging, Washed Urine Cytologic, and Final Pathologic Results
| Patient | Cystoscopy | RGP | Ureteroscopy | Endoscopic Biopsy | Washed Urine Cytology | Final Pathology |
|---|---|---|---|---|---|---|
| 1 | Normal | Filling defect | UC grade II | Polypoid ureteritis and ureteral stone | ||
| 2 | Normal | Filling defect | Negative | Inflammatory pseudotumor | ||
| 3 | Normal | Stricture of the midureter | Atypical cells, possibly reactive | Atypical urothelial hyperplasia and ureteral stone | ||
| 4 | Pseudopolyp in the bladder neck | Filling defect | Negative | Fibroepithelial polyp | ||
| 5 | Normal | Filling defect | Negative | Inflammatory pseudotumor | ||
| 6 | Normal | Complete obstruction in the distal ureter | Failed to advance ureteroscope because of total obstruction | A few atypical cells with mainly fibrous tissue | Negative | Mucosal and submucosal hemorrhage with transmural congestion in the ureter |
| 7 | Bullous change of the right ureteral orifice | Failed because of bullous change of the ureteral orifice | Failed to advance ureteroscope because of total obstruction | Failed to obtain the biopsy specimen | Tuberculosis |
RGP, retrograde ureteropyelography; UC, urothelial carcinoma.
Voided Urine Cytology
All patients underwent preoperative voided urine cytology, with each of the 3 consecutive measurements separated by 1 day. There was no evidence of malignancy in all 7 patients.
Imaging Studies
All patients were evaluated using CT urography, which was performed at our institution. In 4 patients (57.1%), the CT findings met the diagnostic criteria of UUTUC. The remaining 3 patients (42.9%) underwent further studies to rule out other benign diseases despite suspicion of UC. All patients also underwent RGP. This revealed suspected filling defects in 4 patients (57.1%) and a luminal stricture or obstructive findings other than a filling defect or goblet sign suggesting malignancy in 1 patient (14.3%). In 2 patients (28.6%), severe bullous or edematous changes in the ureteral orifice that inhibited the passage of a 5-Fr open-ended ureteral catheter were identified.
Cystoscopy and Ureteroscopy
Cystoscopy was performed in all patients before laparoscopic RNU. Normal findings were observed in all but 2 patients (28.6%), 1 with a bullous change of the right ureteral orifice and the other with a tiny pseudopolyp on the bladder neck. Preoperative ureteroscopy could not be performed in 5 patients (71.4%). Furthermore, the procedure failed in 2 patients because the suspected lesions could not be approached because of the complete obstruction of the distal ureter or ureteral orifice.
Washed Urine Cytology
Six patients (85.7%) underwent washed urine cytology before RGP. The findings were negative for malignancy or atypical cells in 5 patients (83.3%). In the remaining patient (16.7%), UC grade II was diagnosed.
Pathologic Results
Tuberculosis of the UUT was diagnosed in 1 patient (14.3%), inflammatory pseudotumors in 2 (28.6%), and a fibroepithelial polyp in 1 (14.3%). Stones were detected in the remaining 2 patients (28.6%) who underwent RNU; the pathology reports described stones with polypoid ureteritis with ureter stones and atypical papillary urothelial hyperplasia, respectively.
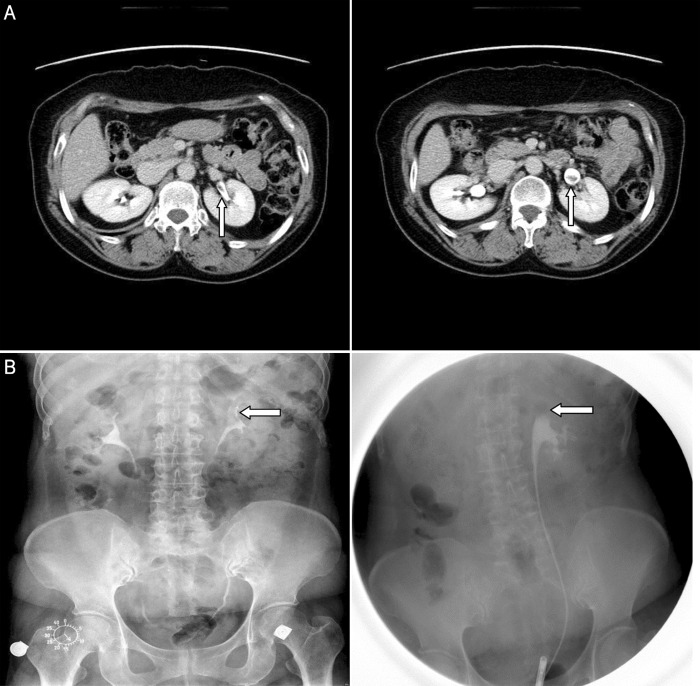
Interestingly, the specimen removed from patient 6, a 52-year-old woman, showed no definite abnormal findings. This patient had visited our outpatient clinic complaining of pain in the right flank. On CT urography, an enhancing lesion that was causing hydroureteronephrosis was detected in the right distal ureter. There was also a moderate decrease in enhancement in the renal parenchyma (Figure 1). Her cystoscopic findings were normal, and voided urine cytology also provided no evidence of malignancy. During RGP, a 5-Fr open-ended ureteral catheter could not be advanced because of the near-complete obstruction of the right distal ureter. When endoscopic biopsy specimens around the obstructive lesion were obtained randomly, they were subsequently determined to mainly constitute a few atypical cells and fibrous tissue. The final pathology of the removed ureter, after the patient underwent laparoscopic RNU, reported a benign lesion that was caused by mucosal and submucosal hemorrhage with transmural congestion.
Figure 1.

A benign lesion caused by mucosal and submucosal hemorrhage with transmural congestion in a 52-year-old woman with right flank pain. A delay pelvis image scan shows an enhancing soft tissue lesion in the right distal ureter (left, circle) causing hydroureteronephrosis of the right kidney and resulting in decreased perfusion of the right renal parenchyma (right).
Another patient (patient 4) was a 55-year-old woman who visited our clinic for further evaluation of a 1.6-cm left renal pelvis mass that was detected incidentally during an attempted workup for gallbladder stones (Figure 2a). Her cystoscopic findings were normal apart from a small pseudopolyp on the bladder neck. Voided urine and washed urine cytology examinations also showed no evidence of malignancy. Intravenous pyelography and RGP revealed focal filling defects in the left renal pelvis and upper calyx (Figure 2b). Laparoscopic RNU was performed without a ureteroscopic biopsy. The final pathology was a fibroepithelial polyp in the left renal pelvis.
Figure 2.
(a) A fibroepithelial polyp in the left renal pelvis in a 55-year-old woman who visited our clinic for further evaluation of a 1.6-cm left renal pelvis mass that was detected incidentally during an attempted workup for gallbladder stones at a local clinic. An excretory-phase scan shows a 1.6-cm ill-defined mass (arrow) as a filling defect in the left renal pelvis. (b) Both the intravenous pyelogram (left) and the retrograde pyelogram (right) show the focal filling defect (arrow) in the upper calyx portion of the left renal pelvis.
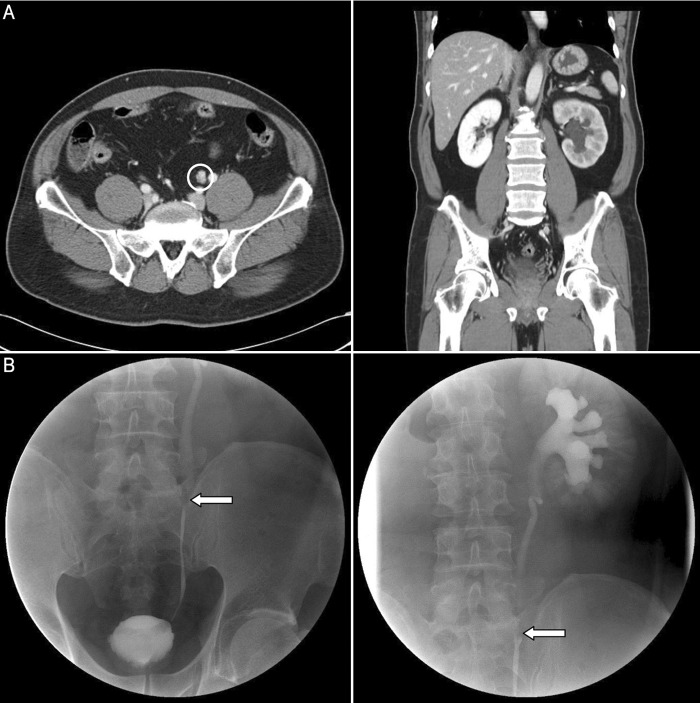
A 49-year-old male patient (patient 5) had reported feeling vague left flank pain several years previously. He did not seek treatment or workup to determine the origin of the pain at that time. However, after symptom aggravation, CT urography was performed at our institution. It showed a 1.5-cm well-enhancing mass with near total obstruction at the left midureter level (Figure 3a). The cystoscopic findings were normal, and there was no evidence of malignancy on voided urine and washed urine cytology examinations. RGP indicated definite filling defects in the left midureter (Figure 3b). Laparoscopic RNU was performed without a ureteroscopic biopsy. The final pathologic finding was an inflammatory pseudotumor (1.5 × 0.7 × 0.7 cm) involving the left midureter.
Figure 3.
(a) An inflammatory pseudotumor in a 49-year-old man with vague left flank pain. A parenchymal phase scan shows a 1.5-cm well-enhancing mass in the left midureter with nearly total obstruction causing hydroureteronephrosis (left, circle). In the coronal image, the left kidney has moderately decreased perfusion of the renal parenchyma, which suggests that its renal function is slightly reduced compared with that of the right kidney (right). (b) A retrograde pyelogram shows dilation of the ureter and renal pelvis distal to the obstructing tumor (arrow), namely, the “goblet sign.”
DISCUSSION
To date, there have been few studies on benign findings diagnosed after RNU. Deligne et al14 reported that 11% of patients with filling defects of the UUT had benign disease, including Mostofi papillomas, inverted papilloma, and fibroepithelial tumors. Chitale et al15 found that of 39 patients without preoperative histologic diagnoses, final histology did not show any malignancy in 4 (10.3%), despite radiologic diagnoses of suspected UUTUC on the basis of filling defects. Thus, although the radiologic features of benign lesions have been described, the preoperative diagnosis of nonmalignant tumors in an outpatient setting remains difficult. Our study also shows this.
On the basis of the final pathologic results, one of our patients (patient 6) did not show any definite pathological lesions, including disease entities. Thus, conservative management might have been a more suitable option for this patient than radical treatment. However, a preoperative mercaptoacetyltriglycine renal scan did show moderate to severe decreased renal function in the affected kidney. The attending surgeon considered both the possibility of a true UC and the fact that the kidney of the affected ureter was nearly nonfunctional. Therefore, the decision was made to perform laparoscopic RNU rather than to proceed with conservative management, such as distal ureterectomy with reimplantation or endoscopic surgery. It should be emphasized that the patient and her family agreed to laparoscopic RNU after sufficient surgical consultation, as in all other cases described in this study.
UUT stones, with or without recurrent urinary tract infection, are a known risk factor for UUT cancers, including squamous cell carcinoma, UC, and adenocarcinoma.16 The mechanism is thought to involve chronic inflammation that leads to urothelial proliferation and eventual malignant transformation. In the present study, stone-associated pathologies were diagnosed postoperatively in 2 patients. One of these pathologies was papillary urothelial hyperplasia, which is a precursor to papillary urothelial neoplasm. This is predominantly a lower grade lesion that warrants follow-up.17 The second patient had polypoid ureteritis with a ureter stone. Lane and Epstein18 reported that polypoid cystitis develops as a reaction to injured bladder mucosa. This benign lesion mimics various papillary urothelial neoplasms. Analogous lesions occur throughout the urothelial tract and are referred to as polypoid urethritis, polypoid ureteritis, or polypoid pyelititis when they are present in the urethra, ureter, or renal pelvis, respectively. On the basis of these observations, it can be speculated that the patient with polypoid ureteritis and a ureteral stone was preoperatively misdiagnosed with a papillary urothelial neoplasm.
Of the different procedures used to diagnose UUTUCs, the best results are achieved with ureteroscopy.19–21 The flexible ureteroscope allows exploration of the ureter macroscopically and reaches the renal cavities in 95% of patients. Ureteroscopy can assess the aspect of the tumor, can obtain a tumor biopsy, can determine tumor grade in 90% of cases, and has a low false-negative rate.22 A combination of endoscopic biopsy grade, ipsilateral hydronephrosis, and urinary cytology may guide the choice of RNU versus endoscopic treatment.19 However, in the present study, ureteroscopy was attempted in only 2 patients (28.6%), both of whom had previously undergone endoscopic biopsy. Although several studies have confirmed that there is a good correlation between tumor grade at endoscopic biopsy and the grade at final pathologic analysis, concerns remain over inadequate tissue sampling in endoscopic biopsy, as this could limit the determination of tumor stage and grade and their usefulness as references for further treatment.23 Indeed, Smith et al24 reported that the accuracy of endoscopic biopsy for upper tract tumors is limited. The difficulty in these cases is that ureteroscopy allows only small amounts of tissue to be sampled, which makes a correct pathologic diagnosis difficult; thus, both the extent and the aggressiveness of the disease may be underestimated.
Thus, our study has 1 important limitation, namely, that diagnostic ureteroscopy was not successfully undertaken in all patients with benign pathologic results after laparoscopic RNU. In some cases, the ureteroscopic examinations were not conducted because of decisions by the attending surgeons or because of the unavailability of flexible ureteroscopy. Flexible ureteroscopy undoubtedly provides better optics and easy access, especially in cases of lesions that have not passed through the lower urinary tract directly into the ureter and calyceal system. This would result in more precise decision making before radical treatment.
Nevertheless, our present study is significant because it is the first time that the incidence of benign pathologic lesions after laparoscopic RNU with preoperative suspicion of UUTUC has been determined in a relatively large study cohort. This incidence (2.9%) is lower than the 10% incidence reported by other studies. Thus, despite thorough expert radiologic review, a small fraction of UUT tumors presumed to be UCs were ultimately shown to be benign on the basis of pathologic findings.
CONCLUSION
This study identified several patients who underwent laparoscopic RNU for UUT tumors that were presumed to be UC but were found after surgery to be benign. These data indicate the need for realistic counseling of patients undergoing radical treatment. Our results will be useful for the establishment of quality control measures for surgeons performing laparoscopic RNU.
Contributor Information
Sungwoo Hong, Department of Urology, Dankook University College of Medicine, Cheonan, Korea.
Taekmin Kwon, Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea..
Dalsan You, Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea..
In Gab Jeong, Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea..
Bumsik Hong, Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea..
Jun Hyuk Hong, Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea..
Hanjong Ahn, Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea..
Choung-Soo Kim, Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea..
References:
- 1. Munoz JJ, Ellison LM. Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. J Urol. 2000;164:1523–1525. [PubMed] [Google Scholar]
- 2. Tawfiek ER, Bagley DH. Upper-tract transitional cell carcinoma. Urology. 1997;50:321–329. [DOI] [PubMed] [Google Scholar]
- 3. Smith RC, Rosenfield AT, Choe KA, et al. Acute flank pain: comparison of non-contrast-enhanced CT and intravenous urography. Radiology. 1995;194:789–794. [DOI] [PubMed] [Google Scholar]
- 4. Kawashima A, Sandler CM, Goldman SM, Raval BK, Fishman EK. CT of renal inflammatory disease. Radiographics. 1997;17:851–866. [DOI] [PubMed] [Google Scholar]
- 5. Kawashima A, Sandler CM, Corl FM, et al. Imaging of renal trauma: a comprehensive review. Radiographics. 2001;21:557–574. [DOI] [PubMed] [Google Scholar]
- 6. Van Der Molen AJ, Cowan NC, Mueller-Lisse UG, et al. CT urography: definition, indications and techniques. A guideline for clinical practice. Eur Radiol. 2008;18:4–17. [DOI] [PubMed] [Google Scholar]
- 7. Roupret M, Yates DR, Comperat E, Cussenot O. Upper urinary tract urothelial cell carcinomas and other urological malignancies involved in the hereditary nonpolyposis colorectal cancer (lynch syndrome) tumor spectrum. Eur Urol. 2008;54:1226–1236. [DOI] [PubMed] [Google Scholar]
- 8. Colin P, Koenig P, Ouzzane A, et al. Environmental factors involved in carcinogenesis of urothelial cell carcinomas of the upper urinary tract. BJU Int. 2009;104:1436–1440. [DOI] [PubMed] [Google Scholar]
- 9. Wong-You-Cheong JJ, Wagner BJ, Davis CJ., Jr Transitional cell carcinoma of the urinary tract: radiologic-pathologic correlation. Radiographics. 1998;18:123–142. [DOI] [PubMed] [Google Scholar]
- 10. Lee TY, Ko SF, Wan YL, et al. Unusual imaging presentations in renal transitional cell carcinoma. Acta Radiol. 1997;38:1015–1019. [DOI] [PubMed] [Google Scholar]
- 11. Chapron C, Chopin N, Borghese B, et al. Deeply infiltrating endometriosis: pathogenetic implications of the anatomical distribution. Hum Reprod. 2006;21:1839–1845. [DOI] [PubMed] [Google Scholar]
- 12. Reservitz GB. A historic review of nephroureterectomy. Surg Gynecol Obstet. 1967;125:853–858. [PubMed] [Google Scholar]
- 13. Gill IS, Sung GT, Hobart MG, et al. Laparoscopic radical nephroureterectomy for upper tract transitional cell carcinoma: the Cleveland Clinic experience. J Urol. 2000;164:1513–1522. [PubMed] [Google Scholar]
- 14. Deligne E, Colombel M, Badet L, et al. Conservative management of upper urinary tract tumors. Eur Urol. 2002;42:43–48. [DOI] [PubMed] [Google Scholar]
- 15. Chitale S, Mbakada R, Irving S, Burgess N. Nephroureterectomy for transitional cell carcinoma—the value of pre-operative histology. Ann R Coll Surg Engl. 2008;90:45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zuckerman JM, Passman C, Assimos DG. Transitional cell carcinoma within a calyceal diverticulum associated with stone disease. Rev Urol. 2010;12:52–55. [PMC free article] [PubMed] [Google Scholar]
- 17. Readal N, Epstein JI. Papillary urothelial hyperplasia: relationship to urothelial neoplasms. Pathology. 2010;42:360–363. [DOI] [PubMed] [Google Scholar]
- 18. Lane Z, Epstein JI. Polypoid/papillary cystitis: a series of 41 cases misdiagnosed as papillary urothelial neoplasia. Am J Surg Pathol. 2008;32:758–764. [DOI] [PubMed] [Google Scholar]
- 19. Brien JC, Shariat SF, Herman MP, et al. Preoperative hydronephrosis, ureteroscopic biopsy grade and urinary cytology can improve prediction of advanced upper tract urothelial carcinoma. J Urol. 2010;184:69–73. [DOI] [PubMed] [Google Scholar]
- 20. Lee KS, Zeikus E, DeWolf WC, Rofsky NM, Pedrosa I. MR urography versus retrograde pyelography/ureteroscopy for the exclusion of upper urinary tract malignancy. Clin Radiol. 2010;65:185–192. [DOI] [PubMed] [Google Scholar]
- 21. Ishikawa S, Abe T, Shinohara N, et al. Impact of diagnostic ureteroscopy on intravesical recurrence and survival in patients with urothelial carcinoma of the upper urinary tract. J Urol. 2010;184:883–887. [DOI] [PubMed] [Google Scholar]
- 22. Tavora F, Fajardo DA, Lee TK, et al. Small endoscopic biopsies of the ureter and renal pelvis: pathologic pitfalls. Am J Surg Pathol. 2009;33:1540–1546. [DOI] [PubMed] [Google Scholar]
- 23. Keeley FX, Jr, Bibbo M, Bagley DH. Ureteroscopic treatment and surveillance of upper urinary tract transitional cell carcinoma. J Urol. 1997;157:1560–1565. [PubMed] [Google Scholar]
- 24. Smith AK, Stephenson AJ, Lane BR, et al. Inadequacy of biopsy for diagnosis of upper tract urothelial carcinoma: implications for conservative management. Urology. 2011;78:82–86. [DOI] [PubMed] [Google Scholar]