Abstract
The objective of this study was to systematically review the literature and compare the effectiveness of controlled interventions with a focus on physical activity (PA) and/or sedentary behaviours (SBs) for reducing sedentary time in adults. Six electronic databases were searched to identify all studies that examined the effects of interventions that targeted PA and/or SBs and that reported on changes in SBs (sedentary, sitting or television time). A qualitative synthesis was performed for all studies, and meta-analyses conducted among studies with mean differences (min/d) of sedentary time. PROSPERO: CRD42014006535. Sixty-five controlled studies met inclusion criteria; 33 were used in the meta-analyses. Interventions with a focus on PA or that included a PA and SB component produced less consistent findings and generally resulted in modest reductions in sedentary time (PA: standardized mean differences [SMD] = −0.22 [95% confidence interval {CI}: −0.35, −0.10], PA + SB: SMD = −0.37 [95% CI: −0.69, −0.05]). Moderate quality evidence from the randomized controlled trial meta-analysis coupled with the qualitative synthesis provides consistent evidence that large and clinically meaningful reductions in sedentary time can be expected from interventions with a focus on reducing SBs (SMD = −1.28 [95% CI: −1.68, −0.87] ). There is evidence to support the need for interventions to include a component focused on reducing SBs in order to generate clinically meaningful reductions in sedentary time.
Keywords: Intervention, physical activity, sedentary behaviour, systematic review
Introduction
The majority of North American adults' waking time is spent being sedentary 1,2. Sedentary behaviour (SB) refers to an energy expenditure ≤1.5 metabolic equivalents while in a sitting or reclining posture during waking hours and not simply the absence of physical activity (PA) 3. Research consistently identifies SBs as independent risk factors for weight gain, as well as related chronic diseases including heart disease, diabetes and cancer 4,5. Greater amounts of sedentary time are also associated with a 49% increased risk for premature mortality 5. Importantly, a gradient effect exists whereby the risks for morbidity and mortality are higher in those engaging in greater amounts of SB with these risks being independent of regular moderate-to-vigorous PA (MVPA) 3,4,6–11.
While evidence has established the efficacy of various PA interventions for increasing MVPA 12,13, it is unknown if these interventions can also produce clinically meaningful reductions in sedentary time or whether more targeted interventions are warranted. It is also possible that the opposite might occur, whereby individuals who increase their PA levels might become more sedentary throughout the rest of the day feeling satisfied that they have attained the minimal PA levels required to meet PA guidelines. Further, the impact of interventions that specifically target SBs are likely unclear.
In light of the fact that adults spend a large proportion of their days being sedentary 1 and that SBs are associated with increased risk for disease and premature mortality independent of PA 4,5, it is important to design interventions that are efficacious in producing significant and clinically meaningful reductions in SBs. Although several reviews exist having examined the efficacy of PA interventions for increasing PA levels 12–15, it remains unknown as to whether these interventions also have the capacity to reduce time spent being sedentary. Two previous reviews targeting SBs and workplace specific sitting identified a lack of controlled interventions, and were unable to make strong conclusions regarding their impact on total sedentary time 16,17. While interventions targeting SBs have begun to emerge, there have been no attempts to identify whether they are in fact more efficacious at reducing SBs than PA interventions or than PA interventions that include a component targeting SBs. Therefore, the objective of this paper is to systematically review and compare the effectiveness of interventions with a focus on PA and/or SBs (PA only vs. PA + SB vs. SB only) for reducing sedentary time in adults.
Methods
Study inclusion criteria
The review sought to identify all studies that examined the effects of an intervention that targeted PA and/or SB (including broader lifestyle or weight loss interventions), and that reported a SB-related outcome (e.g. sedentary time, sitting time, television [TV] time). Only adult populations were included (mean age ≥18 years). Both self-reported and objectively measured SB outcomes were included. A minimum follow-up time of 1 d was required so as to exclude studies that looked at one-time immediate effects of an exposure (e.g. studies that validated accelerometers). All study designs were eligible (e.g. pre-post, quasi-experimental, randomized controlled trial [RCT], etc.) in the original search strategy as it was uncertain how many relevant studies would be identified. Because of the large number of papers identified in the initial search, only higher-quality study designs with a control group were included in this review. Both published (peer-reviewed) and unpublished literatures were examined.
There were no restrictions placed on the sex or characteristics of the participants beyond their age (≥18 years). Although no language restrictions were imposed in the search, only papers published in English or French were included. Abstracts were used if they provided sufficient details to meet the inclusion criteria. The review methodology was prospectively registered in PROSPERO (Registration number: CRD42014006535).
Search strategy
The following electronic bibliographic databases were searched using a comprehensive search strategy to identify relevant studies reporting on SB outcomes of PA and/or SB interventions in adult populations: Ovid Medline(R) In-Process & Other Non-Indexed Citation and Ovid Medline(R) (1946 to October Week 5 2013); Embase Classic + Embase (1947–2013 October 31); EBM Reviews – Cochrane Central Register of Controlled Trials 〈October 2013〉; PsycINFO (1806 to October Week 5 2013); SPORTDiscus (1830 to November 2013); and Dissertations and Theses (1861 to November 2013). The search strategy was developed with the assistance of a research librarian and was carried out by SAP. The strategy is illustrated using the Medline search as an example (Table 1) and was modified according to the indexing systems of the other databases. The OVID interface was used to search Medline, Embase, EBM Reviews and PsycINFO; Ebscohost was used to search SPORTDiscus; and ProQuest for Dissertations and Theses. Grey literature (non–peer-reviewed works) included dissertations, conference abstracts and unpublished data and manuscripts (provided by original authors). If a paper employed a measure that could capture SBs (e.g. International Physical Activity Questionnaire [IPAQ], accelerometers, etc), but did not report SBs in the paper, the authors were contacted to ascertain whether SB-related outcomes could be provided as ‘unpublished data’. Knowledgeable researchers in the field affiliated with the Sedentary Behaviour Research Network (http://www.sedentarybehaviour.org) were also solicited for studies of interest. The bibliographies of key studies selected for the review and related systematic reviews were examined to identify further studies.
Table 1.
Medline search strategy
| References obtained | ||
|---|---|---|
| 1 | Sedentary lifestyle/ | 2,251 |
| 2 | (sedentary adj [lifestyle* or life-style* or behavior?r* or time]).tw. | 4,238 |
| 3 | ([sitting or lying] adj2 time).tw. | 678 |
| 4 | Screen time.tw. | 527 |
| 5 | Television/ | 11,487 |
| 6 | Computers/ | 48,914 |
| 7 | Video games/ | 2,081 |
| 8 | ([television or TV] adj viewing).tw | 1,385 |
| 9 | ([watch* or view*] adj [television or TV]).tw. | 1,594 |
| 10 | ([computer or internet] adj [time or ‘use’ or usage]).tw. | 2,636 |
| 11 | ([computer or video] adj game*).tw. | 2,168 |
| 12 | ([screen or screen-based] adj [entertainment or behavior?r* or ‘use']).tw. | 48 |
| 13 | Automobile driving/ | 13,761 |
| 14 | Low energy expenditure*.tw. | 109 |
| 15 | Physical* inactive*.tw. | 4,756 |
| 16 | Or/1–15 | 89,494 |
| 17 | Motor activity/ | 78,952 |
| 18 | Exp exercise/ | 114,811 |
| 19 | Exp exercise therapy/ | 30,184 |
| 20 | Exp sports/ | 113,459 |
| 21 | Dancing/ | 1,843 |
| 22 | Physical exertion/ | 54,932 |
| 23 | Physical fitness/ | 22,421 |
| 24 | Exp ‘physical education and training'/ | 13,706 |
| 25 | Walk*.tw. | 72,021 |
| 26 | Aerobics.tw. | 439 |
| 27 | (physical* adj [active* or fit* or train*]).tw. | 69,881 |
| 28 | Or/17–27 | 397,336 |
| 29 | Intervention studies/ | 6,802 |
| 30 | Intervention*.tw. | 558,188 |
| 31 | Exp health promotion/ | 55,103 |
| 32 | Health education/ | 52,853 |
| 33 | (promot* or educat* or program*).tw. | 1,449,471 |
| 34 | Monitoring, ambulatory/ | 5,555 |
| 35 | Pedometer*.tw. | 1,506 |
| 36 | Accelerometer*.tw. | 5,445 |
| 37 | Step count*.tw. | 639 |
| 38 | Steps per day.tw. | 418 |
| 39 | ‘steps/d’.tw. | 396 |
| 40 | Or/29–39 | 1,935,326 |
| 41 | 28 and 40 | 81,616 |
| 42 | ([lifestyle or life-style] adj [intervention* or modification*]).tw. | 6,849 |
| 43 | (exercise adj [promotion or program* or intervention*]).tw. | 9,412 |
| 44 | Or/42–43 | 16,043 |
| 45 | 41 or 44 | 87,913 |
| 46 | 16 and 45 | 5,482 |
| 47 | Child/ not exp adult/ | 814,239 |
| 48 | 46 not 47 | 4,395 |
Papers were imported into EndNote (Thompson Reuters, San Francisco, CA, USA) and duplicates removed using the ‘duplicate’ function. Remaining duplicates were removed manually. Two independent reviewers (SAP and KG) screened the titles and abstracts of all studies to identify potentially relevant papers. The full texts of all studies that met the inclusion criteria were then obtained and reviewed independently by SAP and KG or TJS. When disagreements between reviewers occurred, consensus was achieved through discussion and/or with a third reviewer.
Data extraction and analysis
Standardized data abstraction forms in Microsoft Excel were completed by SAP and verified by TJS. Information was extracted on the participant characteristics (age, sex distribution, population), sample size analysed, study design (pre-post, controlled trial, RCT), intervention focus (i.e. PA only vs. PA + SB vs. SB only), intervention description, methods of SB measurement (self-report and direct measures employed, units of measurement, follow-up length) and SB results (pre-post, mean differences). Reviewers were not blinded to the authors or journals when extracting data. The primary outcome measure was the mean difference or changes in SBs (e.g. sedentary time, sitting time, TV time) in min/d following exposure to an intervention. All data from studies with available mean differences were extrapolated to represent mean min/d where possible (e.g. 5 h/d = 300 min/d).
Unpublished SB data were acquired through email contact with authors of papers that mentioned a measure that could capture SBs (e.g. IPAQ, accelerometers, etc), but did not report on the SBs in the article. When willing, authors provided unpublished SB outcomes in the form of mean differences (pre-post) and a measure of variance for each intervention group, as well as any missing study design information. All available unpublished data were used in the meta-analysis and a sensitivity analysis was completed to ascertain whether differences existed between unpublished and published estimates.
Originally all study designs were included as it was uncertain as to how many studies would have included SBs as an outcome, especially among interventions where this was not the main outcome. However, following data extraction, it became clear that there was adequate evidence to only include higher-quality studies with a control arm (quasi-experimental or RCTs). A sufficient number of studies per intervention type (PA only vs. PA + SB vs. SB only) provided mean differences in sedentary time with comparable units (min/d or could be converted to min/d) to permit a meta-analysis or pooling of the data across studies within the intervention groups. Because not all studies could be included in the meta-analyses (data not obtained, units not comparable), we also performed a qualitative synthesis of the evidence for all studies with a control arm.
Forest plots and the meta-analyses were created using Review Manager (RevMan) 5.2 (The Cochrane Collaboration, 2012, The Nordic Cochrane Centre, Copenhagen, Denmark) to compare the mean differences and 95% confidence intervals (CIs) in sedentary time (min/d) between intervention and control groups. Studies that reported units that could not be converted to min/d or that did not provide the results were not included in the meta-analyses. A few studies 18–21 included multiple arms with multiple intervention types (e.g. PA arm, SB arm and control arm or two PA or SB interventions vs. control), in this case, the applicable ‘arms’ were included in the appropriate meta-analysis and the control group was split to include half in each meta-analysis as per the Cochrane handbook 22. A random-effects meta-analysis was used to provide an overall summary measure of effect (mean difference) and 95% CIs for each intervention type (PA only vs. PA + SB vs. SB only). Standardized mean differences (SMDs) were employed due to the variability in the measurement methods for assessing sedentary time across studies (e.g. different objective and self-report measures). This allowed the results of the studies to be standardized on a uniform scale and represents the general effect size of the intervention 22,23. SMDs were calculated as: SMD = differences in mean outcome between groups/standard deviation of outcome among all participants. A priori determined subgroup analyses were carried out to test differences for RCTs vs. quasi-experimental studies, lengths of follow-up, self-reported vs. directly measured sedentary time, SB domains (e.g. all-domain sedentary time vs. sitting time vs. TV time) and intention-to-treat (ITT) vs. completer analyses.
Risk of bias and quality of the evidence
The quality of individual studies was assessed using the Downs and Black checklist 24 and risk of bias assessed using the Cochrane Collaboration's tool for assessing risk of bias in randomized trials 25. The Downs and Black instrument was employed in this review to assess study quality including reporting, external validity and internal validity (bias). The checklist consists of 27 items and was modified to include 1 point for power if the study was powered to detect a difference in sedentary time with a maximum possible count of 27 points (higher scores indicate superior quality). High vs. low quality was assessed using a median split of the scores. The quality of individual studies was rated by SAP and verified by TJS. The risk of bias assessment was carried out by two independent assessors (SAP and TJS), if disagreements between assessors occurred, consensus was achieved through discussion.
The quality of the evidence within each intervention focus (PA only vs. PA + SB vs. SB only) was assessed as high, moderate, low or very low using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach 26. Within this approach, RCTs begin as high-quality evidence and non-randomized studies begin as low-quality evidence. In addition to study design, the quality of evidence is rated based on possible risk of bias, imprecision, heterogeneity, indirectness or suspicion of publication biased. The final rating of the quality of the evidence is primarily derived from the GRADE of the RCT studies. Risk of bias was assessed using RevMan 5.2 and GRADE was assessed using GRADEpro Version 3.6 (GRADE Working Group).
Results
Description of studies
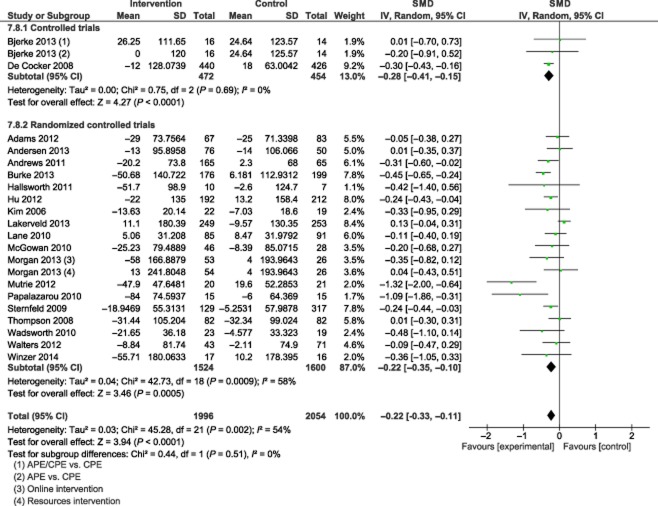
The preliminary search of the electronic databases identified 13,843 potentially relevant papers (see Fig. 1). Of these, 4,456 were identified in MEDLINE, 7,085 in EMBASE, 1,518 in PsycINFO, 373 in Cochrane Central, 312 in SPORTDiscus, and 99 in Dissertations and Theses. Contact with authors of protocols, key informants and bibliographies identified a further 29 papers. After de-duplication, 9,107 relevant papers remained. A preliminary title and abstract review resulted in the retrieval of 1,126 full text papers for a detailed assessment. Of these, 63 unique studies met the criteria for study inclusion, including the added inclusion criteria of a control arm, and were used in the qualitative analysis. Thirty-three of these studies included data on mean differences of sedentary time and were included in the meta-analyses including 20 PA studies, 7 PA + SB studies and 6 SB-only studies. Individual study characteristics can be seen in Supporting Information Tables S1–S3. Common reasons for excluding studies included: animal study (n = 1), populations with mean ages <18 years (n = 25), no measure of SBs (n = 703), the absence of a PA and/or SB intervention (n = 44), results unavailable upon request (n = 46), cross-sectional study design (n = 2), paper not available in English or French (n = 16), conference abstracts with no mention of SB outcomes (n = 121), study protocol (n = 13), unable to locate dissertation (n = 2), and unable to contact author (n = 40).
Figure 1.
Flow diagram for literature search. PA, physical activity; SB, sedentary behaviour.
Data abstraction identified three papers and one dissertation that analysed and reported duplicate data in multiple papers 27–30. Authors of these suspected duplications were contacted, and in cases where several publications were reported the same analyses from the same data source, only one study per data source/analysis was retained in order to avoid double counting. Studies were retained based on most recent data. Studies included were published over a 10-year period from 2004 to 2014. The included studies were conducted in 18 countries with the majority coming from the United States, Australia and the United Kingdom. A total of nine studies were conducted using non-RCT designs, while the remaining and majority used a RCT design. All studies were written in English.
In total, data from 25,446 participants were included. The sample sizes of the studies ranged from a low of 17 31 to a high of 12,287 32 participants. Participants in the studies ranged from 18 to 94 years of age. The population characteristics varied widely especially among the PA and PA + SB studies. The SB-only studies had more homogeneity in terms of study population, and focused mostly on office employees. It is important to note that several studies reported on both a self-report (e.g. questionnaire) and objective measure (e.g. accelerometer) of sedentary time as an outcome, in such cases, the objective results were used when assessing overall trends in change of sedentary time.
Individual study quality and risk of bias assessment
Quality for all included studies (n = 63), including those used only in the qualitative synthesis, can be found in Supporting Information Tables S1–S3. The range of items met on the modified Downs and Black tool was 4 33 to 22/27 34 with a mean of 17.4 ± 3.1. Results of the quality assessment indicated that 44% (28/63) of the studies were of lower quality (based on a median split score of <18/27). All studies were given maximum points for describing the hypotheses/objectives and main outcomes. Most studies obtained a higher score on items in the reporting section (maximum score of 10) with a mean of 7.8 ± 1.3. The majority of studies did not report on blinding of participants or those measuring outcomes with an average internal validity score of 8.3 ± 1.8 (maximum of 13).
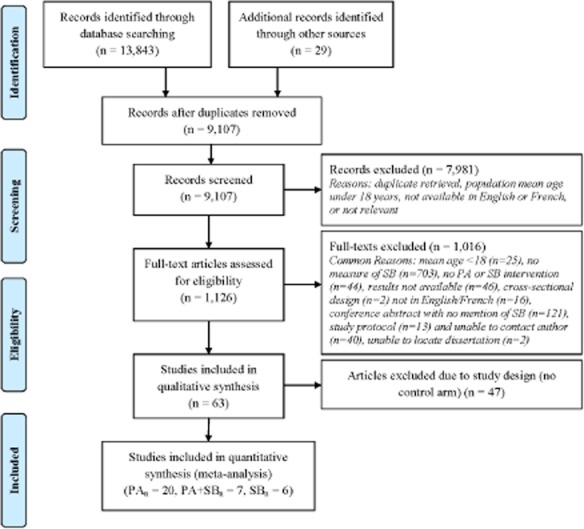
A summary of the risk of bias assessment can be seen in Fig. 2. The largest risk of biases came from selection bias (mainly issues with allocation concealment), performance bias (lack of blinding of participants and personnel delivering intervention) and detection bias (minimal blinding of those assessing outcomes).
Figure 2.
Risk of bias for studies included in meta-analyses (n = 33).
Data synthesis
PA intervention studies
Three non-randomized controlled studies 18,35,36 and 40 RCTs 19,20,29–32,34,37–69 examined changes in SBs following a PA intervention. Twenty-seven studies were solely focused on PA interventions (B.M. Winzer et al., unpublished) 18,20,29–32,35,39–41,44,47,48,50,53–55,57–60,62–65,69, 11 were combined diet and PA interventions 19,34,36,37,43,45,46,51,52,61,66, three were lifestyle interventions that included a PA component 38,56,67, one was a combined diet, PA and breast health intervention 49, and one was a PA intervention with a focus on work style for the prevention of neck and upper limb symptoms 42. Fourteen studies reported that the intervention group had a significantly greater reduction in time spent being sedentary than the control group 34,35,41,42,44,45,47,48,52,55,59,61,64,65, while 29 studies reported no significant difference between the intervention and control groups 18–20,30–32,36–40,43,46,49–51,53,54,56–58,60,62,63,66,67,69 (B.M. Winzer et al., unpublished) (Supporting Information Table S4).
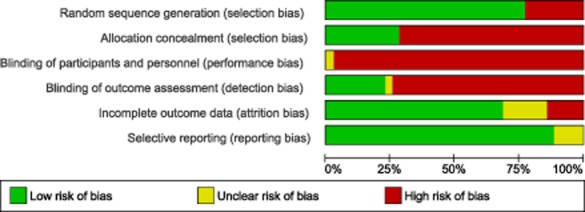
A total of 20 papers reporting on 22 interventions provided mean differences in min/d and were included in the PA intervention meta-analysis. Results of the meta-analysis (Fig. 3) identified that overall, the PA interventions resulted in a significant, but small reduction in sedentary time (SMD = −0.22 [95% CI: −0.35, −0.10] ) equating to a mean difference of approximately 19 min/d less of sedentary time in the intervention groups. Significant heterogeneity was found among the RCT study results. Three studies 45,59,61 with positive and significant reductions in sedentary time represented the greatest deviations from the SMD and explained a large proportion of the heterogeneity of the results.
Figure 3.
Forest plot of standardized mean differences of sedentary time (min/d) from physical activity interventions. APE, activities-based education courses; CI, confidence interval; CPE, conceptually based courses; df, degrees of freedom; SD, standard deviation; SMD, standardized mean differences.
Results of sensitivity analyses identified no significant subgroup differences between studies for: high- vs. low-quality studies; PA focus vs. PA component; length of intervention (≤4 vs. 5–24 vs. 25 weeks); lengths of study follow-up; mode of intervention delivery; intensity of intervention, self-reported vs. objectively measured SBs, domains of SBs (e.g. all-domain sedentary time vs. sitting time vs. TV time), published vs. unpublished results, or ITT analysis vs. completer analysis. Looking within the specific SB domains, there was an overall significant effect of the interventions on sitting time and all-domain sedentary time, but not TV time (n = 3).
Table 2 provides a summary of the evidence for the data used in the meta-analysis including the GRADE of the evidence. The available evidence suggests that interventions that either focus on or include a PA component (and no SB component) may result in minimal reductions of daily sedentary time. The quality of the evidence from the RCT studies is considered moderate. The RCTs began with high-quality evidence and were rated down because of issues with selection bias, allocation bias and significant heterogeneity of study results, and were rated up given the narrow confident limits around the estimate and the large amount of data. It is therefore suggested that the evidence supporting small reductions in sedentary time from PA interventions is of moderate quality and indicates that further research may have an impact on the estimate or the confidence in the estimate.
Table 2.
Summary of findings table for studies used in the meta-analyses
| Physical activity only vs. physical activity + sedentary behaviour vs. sedentary behaviour focused interventions for sedentary time (including sitting time and TV time) | ||||
|---|---|---|---|---|
| Patient or population: adults (≥18 years) Intervention: Physical activity only vs. physical activity + sedentary behaviour components vs. sedentary behaviour focused interventions Comparator: control group or usual care Outcome: sedentary time as defined as total sedentary time, sitting time, or time spent watching TV in min/d | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | SMD |
| Corresponding risk | ||||
| Physical activity only vs. physical activity + sedentary behaviour components vs. sedentary behaviour focused interventions | ||||
| SB-only studies – sedentary time (min/d) – controlled trials follow-up: 4–24 weeks | The mean SB-only studies – sedentary time (min/d) – controlled trials in the intervention groups was: 1.27 standard deviations lower (1.8–0.73 lower) | 140 (4 studies) |
⊕⊝⊝⊝ very low†‡ |
SMD −1.27 (−1.8 to −0.73) |
| SB-only studies – sedentary time (min/d) – randomized controlled trials follow-up: 3–12 weeks | The mean SB-only studies – sedentary time (min/d) – randomized controlled trials in the intervention groups was: 1.31 standard deviations lower (2.16–0.45 lower) | 76 (2 studies) |
⊕⊕⊕⊝ moderate§ |
SMD −1.31 (−2.16 to −0.45) |
| SB + PA studies – sedentary time (min/d) – controlled trials follow-up: 4–8 weeks | The mean SB + PA studies -sedentary time (min/d) – controlled trials in the intervention groups was: 0.81 standard deviations lower (1.31 to 0.31 lower) | 76 (2 studies) |
⊕⊝⊝⊝ very low†§¶ |
SMD −0.81 (−1.31 to −0.31) |
| SB + PA studies – sedentary time (min/d) – randomized controlled trials follow-up: 4–72 weeks | The mean SB + PA studies – sedentary time (min/d) – randomized controlled trials in the intervention groups was: 0.25 standard deviations lower (0.59 lower to 0.08 higher) | 620 (5 studies) |
⊕⊕⊕⊝ moderate†† |
SMD −0.25 (−0.59 to 0.08) |
| PA-only studies – sedentary time (min/d) – controlled trials follow-up: 8–52 weeks | The mean PA-only studies – sedentary time (min/d) – controlled trials in the intervention groups was: 0.28 standard deviations lower (0.41–0.15 lower) | 926 (2 studies) |
⊕⊝⊝⊝ very low† |
SMD −0.28 (−0.41 to −0.15) |
| PA-only studies – sedentary time (min/d) – randomized controlled trials follow-up: 6–108 weeks | The mean PA-only studies – sedentary time (min/d) – randomized controlled trials in the intervention groups was: 0.22 standard deviations lower (0.35–0.10 lower) | 3,124 (20 studies) |
⊕⊕⊕⊝ moderate‡‡§§¶¶††† |
SMD −0.22 (−0.35 to −0.10) |
The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
Because of the nature of the quasi-experimental designs risk of bias is unavoidable.
Losses to follow-up were minimal.
Small sample size.
Populations and interventions different.
Significant heterogeneity between study results.
Most did not blind participants or personnel.
Most studies did not mention allocation concealment strategies.
Significant moderate level of heterogeneity within results.
Studies were skewed towards those with positive results.
CI, confidence interval; GRADE, Grading of Recommendations Assessment, Development and Evaluation; PA, physical activity; SB, sedentary behaviour; SMD, standardized mean difference.
GRADE Working Group grades of evidence.
High quality, further research is very unlikely to change our confidence in the estimate of effect; moderate quality, further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low quality, further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; very low quality, we are very uncertain about the estimate.
Intervention studies targeting both PA and SB
Two non-randomized controlled studies 70,71 and 12 RCTs 33,38,55,72–80 examined changes in SBs following a combined PA + SB intervention. Six studies included a focus on SB + PA 28,70,71,73,74,77, six were combined diet and SB + PA interventions 72,75,78–80, and one was a lifestyle intervention that included both a PA and SB component 33. Seven studies reported that the intervention group had a significantly greater reduction in time spent being sedentary than the control group 33,55,70,73,74,76,77, while seven studies reported no significant difference between the intervention and control groups 28,71,72,75,78–80 (Supporting Information Table S5).
Results of the meta-analysis (Fig. 4) identified that on average, the SB + PA interventions resulted in a significant, but small reduction in sedentary time (SMD = −0.37 [95% CI: −0.69, −0.05] ) equating to a mean difference of approximately 35 min/d less of sedentary time in the intervention groups compared with the controls. Subgroup tests identified that the interventions tested using quasi-experimental study designs had greater reductions in sedentary time than the RCT studies (I2 = 59.9%, P = 0.11). Examination of the forest plot revealed one RCT 79 with a SMD on the right side of the plot, although not significant, it indicated a trend of lower sedentary time within the control group. Removal of this study from the meta-analysis would result in both the heterogeneity among the RCT studies and the differences with the control studies to no longer be significant (I2 = 0%, P = 0.35).
Figure 4.
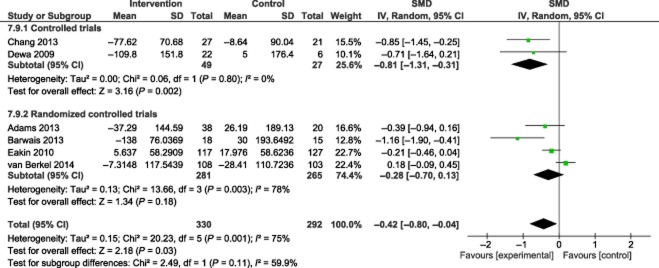
Forest plot of standardized mean differences of sedentary time (min/d) from combined physical activity and sedentary behaviour interventions. CI, confidence interval; df, degrees of freedom; SD, standard deviation; SMD, standardized mean differences.
Results of the subgroup analysis identified differences between published 70,73 and unpublished data (M.M. Adams, unpublished data; C. Dewa, unpublished data; E.G. Eakin, unpublished data; J. van Berkel, unpublished data). SMDs were significantly greater in the published data than among the unpublished data (I2 = 87.3%, P = 0.005) and examination of a funnel plot identified a non-symmetrical distribution of results based on publication status. Subgroup differences (I2 = 87.3%, P = 0.005) were also observed for completer vs. ITT analyses with all of the completer results coming from unpublished data. No significant subgroup differences were identified between studies for high vs. low quality, length of intervention (≤4 vs. 5–24 vs. 25 weeks), lengths of study follow-up, self-reported vs. objectively measured SBs, domains of SBs (e.g. all-domain sedentary time vs. sitting time), or ITT analysis vs. completer analysis. Looking within the specific SB domains, there was an overall significant effect of the interventions on sitting time, but not all domain sedentary time. Qualitatively, all of the studies that reported on TV time showed significant positive effects of the intervention.
The available evidence (Table 2) suggests that interventions that either jointly focus on or include PA and SB components (PA + SB) may result in modest reductions of daily sedentary time. The quality of the evidence from the RCT studies is moderate, largely because of issues with heterogeneity of study results (I2 = 69.6%, P = 0.07) and small number of RCTS (n = 5). These findings suggest that further research is likely to have an impact on the estimate and/or the confidence in the estimate.
SB intervention studies
Three non-randomized controlled studies 81–83 and five RCTs 21,55,84–86 examined changes in SBs following a SB-focused intervention. Six studies 21,55,81–84,86 reported that the intervention group had a significantly greater reduction in time spent being sedentary than the control group, while only one study 85 reported no significant difference between the intervention and control groups (Supporting Information Table S6).
Results of the meta-analysis (Fig. 5) identified that overall, the SB interventions attributed to a significant and large reduction in sedentary time (SMD = −1.28 [95% CI: −1.68, −0.87] ) equating to a mean difference of approximately 91 min/d of sedentary time fewer in the intervention groups compared with the controls.
Figure 5.
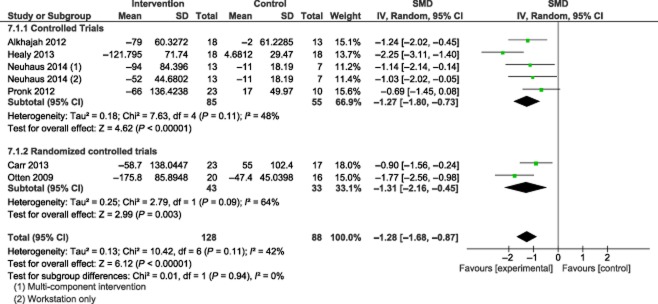
Forest plot of standardized mean differences of sedentary time (min/d) from sedentary behaviour focused interventions. CI, confidence interval; df, degrees of freedom; SD, standard deviation; SMD, standardized mean differences.
Results of the sensitivity analysis identified subgroup differences between the unpublished (G.N. Healy, unpublished data) and published data 21,81,83,84,86. SMDs were significantly greater in the published data than the unpublished data (I2 = 83.3%, P = 0.01); however, only one study provided unpublished data and further studies would be needed to support a possible publication bias. As a result, the unpublished data were retained in the meta-analysis. No significant subgroup differences were observed among studies for high- vs. low-quality, length of intervention (≤4 vs. 5–24 vs. 25 weeks), self-reported vs. objectively measured SBs, across domains of SBs (e.g. all-domain sedentary time vs. sitting time), or ITT vs. completer analyses. Almost all of the studies reported on sitting time at work as an outcome and showed consistent significant effects of the intervention. One study reported results for sedentary time and one for TV time with having shown significant intervention effects.
The available evidence (Table 2) suggests that interventions that focus on SBs may result in large and clinically meaningful reductions in daily sedentary time. The quality of the evidence from the RCT studies is moderate, largely because of issues with imprecision of study results (n = 2 studies). This suggests that further research has the capacity to impact on the estimate and/or the confidence in the estimate.
Discussion
This systematic review examined and compared the efficacy of PA, combined PA + SB and SB-focused interventions to reduce time spent being sedentary among adult populations using all known and available published and unpublished data. Moderate quality evidence from the RCT meta-analysis coupled with the qualitative synthesis of data provides consistent evidence that large and clinically meaningful reductions in sedentary time can be expected from interventions with a focus on reducing SBs. Interventions with either a focus on PA or those including both a PA and SB component were lower in quality, produced less consistent findings, and generally resulted in smaller and more modest reductions in sedentary time.
With American adults spending the majority of their waking hours in sedentary pursuits 1 and the detrimental health risks associated with these behaviours, the design and application of interventions to reduce sedentary time has become increasingly important. The findings of this systematic review therefore have significant implications for the design of these interventions. Evidence from this review supports the need for interventions to place a significant focus on changing SB habits in order to elicit a clinically meaningful reduction in sedentary time.
Interestingly, the SMDs in sedentary time observed in the PA and SB + PA interventions (SMDs: −0.22 [95% CI: −0.35, −0.10] and −0.37 [95% CI: −0.69, −0.05], respectively) were similar to those reported in a systematic review looking at differences in PA following a PA intervention (SMD of 0.28 [95% CI 0.15–0.41] ) 12. This suggests that individuals essentially reallocate time from SBs to MVPA. This assumption was supported by work from Raynor and colleagues who performed a randomized trial to compare an intervention designed to increase PA with an intervention designed to increase PA and decrease time spent watching TV 87. Results of their trial showed that while PA was increased and TV watching decreased, some of the TV watching time was actually reallocated to PA 87. Kozey-Keadle and colleagues also recently reported on a four-armed RCT comparing cardio-metabolic changes between interventions focused on exercise (EX) vs. combined EX and reduced sedentary time (EX + rST) vs. reduced sedentary time (rST) 55. The combined EX + rST group experienced increases in PA similar to their reductions in sedentary time. Only the rST group saw reductions in sedentary time that exceeded gains in PA 55.
Using data from the 2005–2006 National Health and Nutrition Examination Survey (NHANES) and isotemporal substitution modelling, Buman et al. showed that for every 30 min of SBs that were reallocated to MVPA there was a 2–25% improvement in biomarkers of risk (e.g. waist circumference, high-density lipoprotein cholesterol, triglycerides, insulin) 88. Their study also identified that for every 30 min of SBs that were reallocated to light, PA there was a 2–4% improvement in biomarkers (e.g. triglycerides, insulin, β-cell function) 88. This is important as it identifies that the reductions seen in the SB + PA interventions (∼30 min) are clinically meaningful regardless of whether the SBs are reallocated to light PA or MVPA.
The majority of the SMDs among the PA interventions showed no significant differences between the intervention and control groups. While there was variability among the populations and the actual PA interventions, it is worth noting that the only two PA interventions involving older adults (≥60 years) reported significant SMDs in sedentary time 45,59. Burke et al. reported a significant intervention effect with a mean difference of 57 min/d of self-reported sitting time 45, and Mutrie and colleagues reported that sedentary time in the intervention group was 67.5 min/d lower than the control group (P = 0.0001) 59. Older adults are at great risk for sedentary lifestyles and are subsequently the most sedentary segment of the American population, spending more than 60% of their time being sedentary 1. Given that PA interventions have shown to be quite efficacious for increasing PA levels of older adults 89, and that older adults exhibit the highest levels of SBs, it is feasible that PA interventions in this group may result in greater reductions in sedentary time. Unfortunately, only two studies were captured in this group, but the findings do support the need for future studies to understand if targeting PA in this group is sufficient to see meaningful reductions in sedentary time.
While reallocating to MVPA yields far greater ‘per-minute’ reductions in risk factors (30 min reallocated to MVPA = 2%–25% improvement in biomarkers of risk), meaningful reductions in risk can also be achieved by reallocating larger quantities of sedentary time to light PA (90 min reallocated to light PA = 6–12% improvement in biomarkers of risk) 88. Results of the SB intervention meta-analysis identified a significant and large reduction in sedentary time equating to an average difference of approximately 91 fewer min/d of sedentary time in the intervention groups compared with the controls. Supported by Buman's work, this difference is clinically meaningful for the reduction of health risks associated with this behaviour 88. Furthermore, Thorp et al. demonstrated that every 1-h increase in daily TV viewing is associated with increased waist circumference, body mass index, systolic blood pressure, and triglycerides in women and greater 2-h post-load glucose in men 90. Furthermore, using objective accelerometer data from the 2003–2006 NHANES, Healy and colleagues suggest that reductions of 1–2 h of sedentary time could equate to substantial reductions in cardiovascular disease risk 91.
The SB interventions were fairly homogenous, all lasting between 3 and 12 weeks, and mostly targeting sedentary time or sitting time in office settings. All but one study reported primarily on immediate post-intervention changes in SBs. Interestingly, results from Pronk et al. identified that although immediate post-intervention results favoured a reduction in sitting time at work in the intervention arm, 2 weeks post-intervention (removal of sit–stand desks) both groups had actually significantly increased their sitting time 83. This is an important finding as PA interventions have also shown to be efficacious for increasing PA in the short term, but long-term behaviour changes are more challenging to maintain 13,92. While daily minutes of sedentary time provides a tangible measure that is easily understood, it has been suggested that expressing sedentary time as a percentage of the day may provide a more meaningful representation of change in daily behaviour patterns and corrects for variability in wear times 93. Further, where possible, it would be beneficial for studies to report on changes across entire 24-h periods to provide a better representation of changes in individuals' behavioural patterns including sleep time. While Carr and colleagues showed a significant reduction in daily minutes of sedentary time among the intervention group, when results were expressed as a percentage of the day spent being sedentary, the differences were no longer significant 84. Given that changes in daily percentage may be a more meaningful measure, and that Carr et al. identified that intervention effects differ based on whether they are presented as mean differences or percentage, future intervention research would benefit from reporting on both these outcomes.
The strengths of this review included a comprehensive search strategy developed with a research librarian, an a priori-established protocol with inclusion and exclusion criteria and analytic plans, the use of study quality and risk of bias in assessing confidence in the evidence, and an attempt to capture all possible unpublished data. This review included any intervention with a component or focus on PA and/or SBs, and both self-reported and objective measures of SBs in adults. While the inclusion criteria for the interventions was kept fairly broad in anticipation that not many PA or PA + SB interventions would have captured or reported on sedentary time (not likely the main outcome), this did lead to significant heterogeneity in the populations, intervention designs, and in the case of the PA interventions heterogeneity in the outcomes. The use of the random-effects model and the SMDs allowed us to adjust for several of these issues. A priori-established subgroup analyses also allowed us to identify whether any of these design differences may have influenced the results. No significant differences were observed between self-report vs. objectively measured sedentary time, by intervention focus (e.g. PA vs. PA + diet vs. lifestyle), by length of intervention, or by length of study follow-up.
Although no significant differences were observed between the self-reported and objectively measured sedentary time results, there are fundamental issues with the validity of the measurement methods themselves. Self-reported sedentary time has shown to have low to moderate correlation with accelerometer-derived sedentary time, with improved validity when specific domains of sedentary time are recalled (e.g. time spent watching TV, computer use, sitting at work) 93,94. The majority of objective measures involved accelerometers, which rely on the use of cut-points to determine sedentary movement, largely using vertical axis data. While accelerometers remove the issue of recall bias, they are unable to capture domain-specific sitting time and show only moderate ability to detect sitting time 95,96. Future research would benefit from the use of inclinometers, which capture differences in body position (e.g. sitting vs. lying vs. standing), as well as using a combination of information sources such as accelerometers, heart rate monitors, global positioning system technology and activity logs 93.
The systematic review performed both a qualitative and quantitative synthesis of all available literature allowing for trends across all studies regardless of outcome measurement to be assessed. The meta-analyses were limited to studies that reported on mean changes in min/d, but where possible, we converted the units to increase the number of studies included. Furthermore, authors of studies were contacted to request these mean differences. One of the greatest strengths of this systematic review is the acquisition of a large amount of unpublished data. All but two of the SB + PA studies were analysed using unpublished data. Without this, the examination of a combined SB and PA intervention could not have been performed.
A further limitation of this review is the small sample size available for the combined SB + PA and SB-only intervention studies. Very few intervention studies have been conducted to date to evaluate the efficacy of these types of interventions. Furthermore, almost all of the SB interventions have focused on reductions of office workplace sitting in middle-aged employees. This homogeneity limits their external validity to other populations and settings and limits the direct comparison with PA and PA + SB interventions in other settings. Future research is needed to establish whether the clinically meaningful reductions in sedentary time observed would be found in interventions focusing on other settings, domains and segments of the adult population (e.g. TV viewing in the home among seniors). While the direct comparisons are somewhat limited, the consistent trend in reductions of sedentary time underscores the need for considerable focus on specific targeted behaviours and interventions that take into account the limiting factors in the environment.
Conclusion
In conclusion, this review provides a comprehensive and objective summary of the efficacy of PA- and/or SB-focused interventions to reduce time spent being sedentary among adults. The results have important implications for the design of future interventions where the reduction of SBs is a consideration. Current evidence supports that clinically meaningful reductions in sedentary time can be produced in interventions with some degree of focus on reducing SBs, but that interventions that focus solely on SBs result in much greater reductions. Future studies are needed to test whether SB interventions among other settings and populations would garner similar results. From a public health perspective, this has significant importance given the historical reliance on PA- and diet-targeted interventions for reducing health risks, which may not elicit clinically meaningful changes in SBs. Given that it is likely easier for the majority of individuals to reallocate sedentary time to light intensity PA, and that beneficial gains in metabolic health can be obtained from this reallocation, reducing SBs in addition to increasing MVPA is an important public health message. Interventions that place increased focus on SBs are likely to have a larger impact on reducing these behaviours. Future interventions would benefit from concurrently testing the degree of focus on SBs that is needed to elicit these important reductions.
Acknowledgments
The authors would like to thank Erica Wright for her technical assistance with the search strategy and Dr George Wells for his analytical advice for the meta-analyses. SAP is funded by a Gordon E. Allen Post-Doctoral Fellowship in Health Behaviours at the University of Ottawa Heart Institute and a Canadian Institutes of Health Research Fellowship. TJS is funded by a Heart and Stroke Foundation Post-Doctoral Fellowship.
Authors' contributions
SAP conceived the study, carried out the design, bibliographic search, paper screening, data abstraction and synthesis, interpreted the results, and drafted and edited the paper. TJS participated in its design and coordination, verified data abstraction and study quality; independently conducted risk of bias assessments for all studies included in the meta-analyses, assisted in the interpretation of the data, and helped edit the paper. KG participated in paper screening, data abstraction and editing of the paper. RR participated in the design of the study, provided methodological input, and assisted in the editing of the paper. All authors read and approved the final paper.
Conflicts of interest statement
The authors declare that they have no competing interests.
Supporting Information
Additional Supporting Information may be found in the online version of this article, http://dx.doi.org/10.1111/obr.12215
Table S1. Physical activity intervention study characteristics.
Table S2. Physical activity and sedentary behaviour study characteristics.
Table S3. Sedentary behaviour study characteristics.
Table S4. Physical activity intervention study results.
Table S5. Physical activity and sedentary behaviour intervention study results.
Table S6. Sedentary behaviour intervention study results.
References
- Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011;22:7–14. [PubMed] [Google Scholar]
- Sedentary Behaviour Research Network. Letter to the editor: standardized use of the terms ‘sedentary’ and ‘sedentary behaviours’. Appl Physiol Nutr Metab. 2012;37:540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55:2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31:369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- Henson J, Yates T, Biddle SJ, et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56:1012–1020. doi: 10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- Chomistek AK, Lu B, Sands M, et al. Relationship of sedentary behavior and physical inactivity to incident coronary heart disease: results from the women's health initiative. Circulation. 2013;61:2346–2354. doi: 10.1016/j.jacc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koster A, Caserotti P, Patel KV, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS ONE. 2012;7:e37696. doi: 10.1371/journal.pone.0037696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41:1338–1353. doi: 10.1093/ije/dys078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41:998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- Hillsdon M, Foster C, Thorogood M. Interventions for promoting physical activity. Cochrane Database Syst Rev. 2005;(1) doi: 10.1002/14651858.CD003180.pub2. CD003180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Williams DM, Dubbert PM, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2006;114:2739–2752. doi: 10.1161/CIRCULATIONAHA.106.179683. [DOI] [PubMed] [Google Scholar]
- Greaves CJ, Sheppard KE, Abraham C, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119. doi: 10.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller-Riemenschneider F, Reinhold T, Nocon M, Willich SN. Long-term effectiveness of interventions promoting physical activity: a systematic review. Prev Med. 2008;47:354–368. doi: 10.1016/j.ypmed.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Chau JY, der Ploeg HP, van Uffelen JGZ, et al. Are workplace interventions to reduce sitting effective? A systematic review. Prev Med. 2010;51:352–356. doi: 10.1016/j.ypmed.2010.08.012. [DOI] [PubMed] [Google Scholar]
- Healy GN, Lawler S, Thorp AA, et al. Reducing Prolonged Sitting in the Workplace (An Evidence Review: Full Report) Melbourne, Australia: Victorian Health Promotion Foundation; 2012. [Google Scholar]
- Bjerke W. The effects of an activities and conceptually based physical education course on college student health and behavior outcomes. 2013. [PhD]. Walden University (USA): Minneapolis.
- Morgan PJ, Callister R, Collins CE, et al. The SHED-IT community trial: a randomized controlled trial of internet- and paper-based weight loss programs tailored for overweight and obese men. Ann Behav Med. 2013;45:139–152. doi: 10.1007/s12160-012-9424-z. [DOI] [PubMed] [Google Scholar]
- McGowan EL. Increasing Physical Activity Behaviour in First-and Second-Degree Relatives of Colon Cancer Patients: A Matter of Self-Regulation [Ph.D.] Ann Arbor: The University of Western Ontario (Canada); 2010. [Google Scholar]
- Neuhaus M, Healy GN, Dunstan DW, Owen N, Eakin EG. Workplace sitting and height-adjustable workstations: a randomized controlled trial. Am J Prev Med. 2014;46:30–40. doi: 10.1016/j.amepre.2013.09.009. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0. The Cochrane Collaboration; URL www.cochrane-handbook.org (accessed 16 July 2014) [Google Scholar]
- Chau JY, der Ploeg HP, van Uffelen JG, et al. Are workplace interventions to reduce sitting effective? A systematic review. Prev Med. 2010;51:352–356. doi: 10.1016/j.ypmed.2010.08.012. [DOI] [PubMed] [Google Scholar]
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams MM. On our feet: feasibility trial of an intervention to reduce sedentary behavior and increase physical activity. 2012. [PhD]. University of North Carolina (USA); Greensboro.
- Adams MM, Davis PG, Gill DL. A hybrid online intervention for reducing sedentary behavior in obese women. Front Public Health. 2013;1:45. doi: 10.3389/fpubh.2013.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen E, Burton NW, Anderssen SA. Physical activity levels six months after a randomised controlled physical activity intervention for Pakistani immigrant men living in Norway. Int J Behav Nutr Phys Act. 2012;9:47. doi: 10.1186/1479-5868-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen E, Hostmark AT, Holme I, Anderssen SA. Intervention effects on physical activity and insulin levels in men of Pakistani origin living in Oslo: a randomised controlled trial. J Immigr Minor Health. 2013;15:101–110. doi: 10.1007/s10903-012-9686-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallsworth K, Fattakhova G, Hollingsworth KG, et al. Resistance exercise reduces liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Gut. 2011;60:1278–1283. doi: 10.1136/gut.2011.242073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen AW, Gronbaek M, Helge JW, Severin M, Curtis T, Tolstrup JS. Effect of a web-based intervention to promote physical activity and improve health among physically inactive adults: a population-based randomized controlled trial. J Med Internet Res. 2012;14:e145. doi: 10.2196/jmir.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriska A, Rockette-Wagner B, Bray GA, et al. Impact of lifestyle intervention on sedentary time in subjects at high-risk for diabetes. Diabetes. 2012;61:A48–A49. [Google Scholar]
- Andrews RC, Cooper AR, Montgomery AA, et al. Diet or diet plus physical activity vs. usual care in patients with newly diagnosed type 2 diabetes: the Early ACTID randomised controlled trial. Lancet. 2011;378:129–139. doi: 10.1016/S0140-6736(11)60442-X. [DOI] [PubMed] [Google Scholar]
- De Cocker KA, De Bourdeaudhuij IM, Brown WJ, Cardon GM. The effect of a pedometer-based physical activity intervention on sitting time. Prev Med. 2008;47:179–181. doi: 10.1016/j.ypmed.2008.05.012. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Blackburn K, Gillman MW, et al. First steps for mommy and me: a pilot intervention to improve nutrition and physical activity behaviors of postpartum mothers and their infants. Matern Child Health J. 2011;15:1217–1227. doi: 10.1007/s10995-010-0696-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abascal LB. The effect of depression and adherence in a dietary and physical activity intervention for overweight and obese adults. 2008. [PhD]. University of California: San Diego.
- Adams AK, LaRowe TL, Cronin KA, et al. The Healthy Children, Strong Families intervention: design and community participation. J Prim Prev. 2012;33:175–185. doi: 10.1007/s10935-012-0275-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aittasalo M, Miilunpalo S, Suni J. The effectiveness of physical activity counseling in a work-site setting. A randomized, controlled trial. Patient Educ Couns. 2004;55:193–202. doi: 10.1016/j.pec.2003.09.003. [DOI] [PubMed] [Google Scholar]
- Aittasalo M, Rinne M, Pasanen M, Kukkonen-Harjula K, Vasankari T. Promoting walking among office employees – evaluation of a randomized controlled intervention with pedometers and e-mail messages. BMC Public Health. 2012;12:403. doi: 10.1186/1471-2458-12-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker G, Gray SR, Wright A, et al. The effect of a pedometer-based community walking intervention ‘Walking for Wellbeing in the West’ on physical activity levels and health outcomes: a 12-week randomized controlled trial. Int J Behav Nutr Phys Act. 2010;7:51. doi: 10.1186/1479-5868-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernaards CM, Ariens GA, Simons M, Knol DL, Hildebrandt VH. Improving work style behavior in computer workers with neck and upper limb symptoms. J Occup Rehabil. 2008;18:87–101. doi: 10.1007/s10926-007-9117-9. [DOI] [PubMed] [Google Scholar]
- Bonnefoy M, Boutitie F, Mercier C, et al. Efficacy of a home-based intervention programme on the physical activity level and functional ability of older people using domestic services: a randomised study. J Nutr Health Aging. 2012;16:370–377. doi: 10.1007/s12603-011-0352-6. [DOI] [PubMed] [Google Scholar]
- Breyer MK, Breyer-Kohansal R, Funk GC, et al. Nordic walking improves daily physical activities in COPD: a randomised controlled trial. Respir Res. 2010;11:112. doi: 10.1186/1465-9921-11-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L, Lee AH, Jancey J, et al. Physical activity and nutrition behavioural outcomes of a home-based intervention program for seniors: a randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:14. doi: 10.1186/1479-5868-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson JA, Sallis JF, Ramirez ER, Patrick K, Norman GJ. Physical activity and dietary behavior change in Internet-based weight loss interventions: comparing two multiple-behavior change indices. Prev Med. 2012;54:50–54. doi: 10.1016/j.ypmed.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin APMJ, van Poppel MN, van Mechelen W. Effects of resistance and functional-skills training on habitual activity and constipation among older adults living in long-term care facilities: a randomized controlled trial. BMC Geriatr. 2006;6:9. doi: 10.1186/1471-2318-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Greef K, Deforche B, Tudor-Locke C, De Bourdeaudhuij I. A cognitive-behavioural pedometer-based group intervention on physical activity and sedentary behaviour in individuals with type 2 diabetes. Health Educ Res. 2010;25:724–736. doi: 10.1093/her/cyq017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Sanchez-Johnsen LA, Wells AM, Dyer A. A combined breast health/weight loss intervention for black women. Prev Med. 2005;40:373–383. doi: 10.1016/j.ypmed.2004.06.018. [DOI] [PubMed] [Google Scholar]
- Gilson ND, Puig-Ribera A, McKenna J, Brown WJ, Burton NW, Cooke CB. Do walking strategies to increase physical activity reduce reported sitting in workplaces: a randomized control trial. Int J Behav Nutr Phys Act. 2009;6:43. doi: 10.1186/1479-5868-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hijazi RR. Exploring the Use of Smart Phones to Influence Healthy Behaviors. Minneapolis: Walden University; 2011. [Google Scholar]
- Hu G, Tian H, Zhang F, et al. Tianjin Gestational Diabetes Mellitus Prevention Program: study design, methods, and 1-year interim report on the feasibility of lifestyle intervention program. Diabetes Res Clin Pract. 2012;98:508–517. doi: 10.1016/j.diabres.2012.09.015. [DOI] [PubMed] [Google Scholar]
- Kallings LV, Johnson JS, Fisher RM, et al. Beneficial effects of individualized physical activity on prescription on body composition and cardiometabolic risk factors: results from a randomized controlled trial. Eur J Cardiovasc Prev Rehabil. 2009;16:80–84. doi: 10.1097/HJR.0b013e32831e953a. [DOI] [PubMed] [Google Scholar]
- Kim CJ, Kang DH, Smith BA, Landers KA. Cardiopulmonary responses and adherence to exercise in women newly diagnosed with breast cancer undergoing adjuvant therapy. Cancer Nurs. 2006;29:156–165. doi: 10.1097/00002820-200603000-00013. [DOI] [PubMed] [Google Scholar]
- Kozey Keadle S, Lyden K, Staudenmayer J, et al. The independent and combined effects of exercise training and reducing sedentary behavior on cardiometabolic risk factors. Appl Physiol Nutr Metab. 2014;39:770–780. doi: 10.1139/apnm-2013-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakerveld J, Bot SD, van der Ploeg HP, Nijpels G. The effects of a lifestyle intervention on leisure-time sedentary behaviors in adults at risk: the Hoorn Prevention Study, a randomized controlled trial. Prev Med. 2013;57:351–356. doi: 10.1016/j.ypmed.2013.06.011. [DOI] [PubMed] [Google Scholar]
- Lane A, Murphy N, Bauman A, Chey T. Randomized controlled trial to increase physical activity among insufficiently active women following their participation in a mass event. Health Educ J. 2010;69:287–296. [Google Scholar]
- Morrison R, Reilly JJ, Penpraze V, et al. Children, Parents and Pets Exercising Together (CPET): exploratory randomised controlled trial. BMC Public Health. 2013;13:1096. doi: 10.1186/1471-2458-13-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutrie N, Doolin O, Fitzsimons CF, et al. Increasing older adults' walking through primary care: results of a pilot randomized controlled trial. Fam Pract. 2012;29:633–642. doi: 10.1093/fampra/cms038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opdenacker J, Boen F. Effectiveness of face-to-face vs. telephone support in increasing physical activity and mental health among university employees. J Phys Act Health. 2008;5:830–843. doi: 10.1123/jpah.5.6.830. [DOI] [PubMed] [Google Scholar]
- Papalazarou A, Yannakoulia M, Kavouras SA, et al. Lifestyle intervention favorably affects weight loss and maintenance following obesity surgery. Obesity (Silver Spring, MD) 2010;18:1348–1353. doi: 10.1038/oby.2009.346. [DOI] [PubMed] [Google Scholar]
- Shaw KL, Page C. A Pilot community-based walking-for-exercise program for senior women. Top Geriatr Rehabil. 2008;24:315–324. [Google Scholar]
- Slootmaker SM, Chinapaw MJ, Schuit AJ, Seidell JC, Van Mechelen W. Feasibility and effectiveness of online physical activity advice based on a personal activity monitor: randomized controlled trial. J Med Internet Res. 2009;11:e27. doi: 10.2196/jmir.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spittaels H, De Bourdeaudhuij I, Vandelanotte C. Evaluation of a website-delivered computer-tailored intervention for increasing physical activity in the general population. Prev Med. 2007;44:209–217. doi: 10.1016/j.ypmed.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Sternfeld B, Block C, Quesenberry CP, et al. Improving diet and physical activity with ALIVE: a worksite randomized trial. Am J Prev Med. 2009;36:475–483. doi: 10.1016/j.amepre.2009.01.036. [DOI] [PubMed] [Google Scholar]
- Thompson JL, Allen P, Helitzer DL, et al. Reducing diabetes risk in American Indian women. Am J Prev Med. 2008;34:192–201. doi: 10.1016/j.amepre.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters JAE, Wills K, Robinson A, et al. Effect of health-mentoring to increase daily physical activity in chronic obstructive pulmonary disease (COPD) Respirology. 2012;17:61. [Google Scholar]
- Walters J, Cameron-Tucker H, Wills K, et al. Effects of telephone health mentoring in community-recruited chronic obstructive pulmonary disease on self-management capacity, quality of life and psychological morbidity: a randomised controlled trial. BMJ Open. 2013;3:e003097. doi: 10.1136/bmjopen-2013-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth DD, Hallam JS. Effect of a web site intervention on physical activity of college females. Am J Health Behav. 2010;34:60–69. doi: 10.5993/ajhb.34.1.8. [DOI] [PubMed] [Google Scholar]
- Chang AK, Fritschi C, Kim MJ. Sedentary behavior, physical activity, and psychological health of Korean older adults with hypertension: effect of an empowerment intervention. Res Gerontol Nurs. 2013;6:81–88. doi: 10.3928/19404921-20121219-01. [DOI] [PubMed] [Google Scholar]
- Dewa CS, de Ruiter W, Chau N, Karioja K. Walking for wellness: using pedometers to decrease sedentary behaviour and promote mental health. Int J Ment Health Promot. 2009;11:24–28. [Google Scholar]
- Anand SS, Davis AD, Ahmed R, et al. A family-based intervention to promote healthy lifestyles in an aboriginal community in Canada. Can J Public Health. 2007;98:447–452. doi: 10.1007/BF03405436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barwais FA, Cuddihy TF, Tomson LM. Physical activity, sedentary behavior and total wellness changes among sedentary adults: a 4-week randomized controlled trial. Health Qual Life Outcomes. 2013;11:183. doi: 10.1186/1477-7525-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Greef KP, Deforche BI, Ruige JB, et al. The effects of a pedometer-based behavioral modification program with telephone support on physical activity and sedentary behavior in type 2 diabetes patients. Patient Educ Couns. 2011;84:275–279. doi: 10.1016/j.pec.2010.07.010. [DOI] [PubMed] [Google Scholar]
- Eakin EG, Reeves MM, Marshall AL, et al. Living Well with Diabetes: a randomized controlled trial of a telephone-delivered intervention for maintenance of weight loss, physical activity and glycaemic control in adults with type 2 diabetes. BMC Public Health. 2010;10:452. doi: 10.1186/1471-2458-10-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: take Action – a group-randomized trial. Obesity (Silver Spring, Md. 2011;19:2082–2088. doi: 10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jago R, Sebire SJ, Turner KM, et al. Feasibility trial evaluation of a physical activity and screen-viewing course for parents of 6 to 8 year-old children: teamplay. Int J Behav Nutr Phys Act. 2013;10:31. doi: 10.1186/1479-5868-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lioret S, Campbell KJ, Crawford D, Spence AC, Hesketh K, McNaughton SA. A parent focused child obesity prevention intervention improves some mother obesity risk behaviors: the Melbourne inFANT program. Int J Behav Nutr Phys Act. 2012;9:100. doi: 10.1186/1479-5868-9-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Berkel J, Boot CR, Proper KI, Bongers PM, van der Beek AJ. Effectiveness of a worksite mindfulness-based multi-component intervention on lifestyle behaviors. Int J Behav Nutr Phys Act. 2014;11:9. doi: 10.1186/1479-5868-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verweij LM, Proper KI, Weel ANH, Hulshof CTJ, Van Mechelen W. The application of an occupational health guideline reduces sedentary behaviour and increases fruit intake at work: results from an RCT. Occup Environ Med. 2012;69:500–507. doi: 10.1136/oemed-2011-100377. [DOI] [PubMed] [Google Scholar]
- Alkhajah TA, Reeves MM, Eakin EG, Winkler EAH, Owen N, Healy GN. Sit–stand workstations: a pilot intervention to reduce office sitting time. Am J Prev Med. 2012;43:298–303. doi: 10.1016/j.amepre.2012.05.027. [DOI] [PubMed] [Google Scholar]
- Healy GN, Eakin EG, Lamontagne AD, et al. Reducing sitting time in office workers: short-term efficacy of a multicomponent intervention. Prev Med. 2013;57:43–48. doi: 10.1016/j.ypmed.2013.04.004. [DOI] [PubMed] [Google Scholar]
- Pronk NP, Katz AS, Lowry M, Payfer JR. Reducing occupational sitting time and improving worker health: the Take-a-Stand Project, 2011. Prev Chronic Dis. 2012;9:E154. doi: 10.5888/pcd9.110323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr LJ, Karvinen K, Peavler M, Smith R, Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ Open. 2013;3:e003261. doi: 10.1136/bmjopen-2013-003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon A. A Theory-Based Pilot Study to Decrease Sitting Time in the Workplace [M.S.] Ann Arbor: Arizona State University; 2013. [Google Scholar]
- Otten JJ, Jones KE, Littenberg B, Harvey-Berino J. Effects of television viewing reduction on energy intake and expenditure in overweight and obese adults: a randomized controlled trial. Arch Intern Med. 2009;169:2109–2115. doi: 10.1001/archinternmed.2009.430. [DOI] [PubMed] [Google Scholar]
- Raynor HA, Steeves EA, Bassett DR, Jr, Thompson DL, Gorin AA, Bond DS. Reducing TV watching during adult obesity treatment: two pilot randomized controlled trials. Behav Ther. 2013;44:674–685. doi: 10.1016/j.beth.2013.04.012. [DOI] [PubMed] [Google Scholar]
- Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014;179:323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med. 2002;22:120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- Thorp AA, Healy GN, Owen N, et al. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian Diabetes, Obesity and Lifestyle (AusDiab) study 2004–2005. Diabetes Care. 2010;33:327–334. doi: 10.2337/dc09-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller-Riemenschneider F, Reinhold T, Nocon M, Willich SN. Long-term effectiveness of interventions promoting physical activity: a systematic review. Prev Med. 2008;47:354–368. doi: 10.1016/j.ypmed.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults' sedentary time in population-based studies. Am J Prev Med. 2011;41:216–227. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders TJ, Prince SA, Tremblay MS. Clustering of children's activity behaviour: the use of self-report vs. direct measures. Int J Behav Nutr Phys Act. 2011;8:48. doi: 10.1186/1479-5868-8-48. author reply 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart TL, Ainsworth BE, Tudor-Locke C. Objective and subjective measures of sedentary behavior and physical activity. Med Sci Sports Exerc. 2011;43:449–456. doi: 10.1249/MSS.0b013e3181ef5a93. [DOI] [PubMed] [Google Scholar]
- Kozey-Keadle S, Libertine A, Staudenmayer J, Freedson P. The feasibility of reducing and measuring sedentary time among overweight, non-exercising office workers. J Obes. 2012;2012:282303. doi: 10.1155/2012/282303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Physical activity intervention study characteristics.
Table S2. Physical activity and sedentary behaviour study characteristics.
Table S3. Sedentary behaviour study characteristics.
Table S4. Physical activity intervention study results.
Table S5. Physical activity and sedentary behaviour intervention study results.
Table S6. Sedentary behaviour intervention study results.