Abstract
Fibroblast growth factor (FGF)21 is an endocrine hormone that is expressed in multiple tissues and functions physiologically to maintain energy homeostasis. FGF21 is being pursued as a therapeutic target for diabetes and obesity because of its rapid and potent effects on improving insulin sensitivity. However, whether FGF21 enhances insulin sensitivity under physiologic conditions remains unclear. Here, we show that liver-derived FGF21 enters the circulation during fasting but also remains present and functional during the early stage of refeeding. After a prolonged fast, FGF21 acts as an insulin sensitizer to overcome the peripheral insulin resistance induced by fasting, thereby maximizing glucose uptake. Likewise, FGF21 is produced from the liver during overfeeding and mitigates peripheral insulin resistance. DIO FGF21 liver-specific knockout, but not FGF21 adipose-specific knockout, mice have increased insulin resistance and decreased brown adipose tissue–mediated glucose disposal. These data are compatible with the concept that FGF21 functions physiologically as an insulin sensitizer under conditions of acute refeeding and overfeeding.
Introduction
Fibroblast growth factor (FGF)21 is an endocrine hormone that signals through a cell-surface receptor complex composed of a classic FGF receptor, FGFR1c, and the FGF coreceptor, β-klotho (1). FGF21 is expressed in several tissues including liver, white adipose tissue (WAT), brown adipose tissue (BAT), and pancreas and has multiple proposed physiological functions (2), some of which remain controversial (3). Pharmacologically, FGF21 is a potent insulin sensitizer that improves metabolic dysfunction in a number of obese animal models and humans (4,5). A single pharmacological dose of FGF21 to obese mice can decrease plasma glucose levels by ∼40–50% within 1 h, an effect lasting up to 6 h (6). Additionally, extended administration of FGF21 to obese rodents and primates significantly increases energy expenditure and weight loss (7–9). Although incompletely understood, adipose tissue is particularly important for the pharmacological actions of FGF21 as the hormone’s acute glucose-lowering effect is lost in mice lacking either β–klotho (10) or FGFR1c in adipose tissue (11). Here, we show that circulating FGF21 levels are completely derived from the liver during prolonged fasting and diet-induced obesity (DIO). Interestingly, loss of FGF21 in the liver, but not adipose tissue, impairs insulin-mediated glucose uptake during refeeding and overfeeding. These data show that FGF21 functions as an insulin sensitizer under specific physiologic conditions.
Research Design and Methods
Animals
FGF21 knockout (12), albumin-Cre (13), adiponectin-Cre (14,15), and FLP-transgenic mice (16) have previously been described. FGF21fl/fl mice were generated by crossing the FGF21neo-loxP/+ mice (12) with FLP-transgenic mice to remove the neo cassette. Subsequent FGF21fl/+ mice were backcrossed seven generations to C57Bl/6 mice. FGF21fl/+ mice were then crossed together to generate FGF21fl/fl mice. FGF21fl/fl mice were then crossed to albumin-Cre or adiponectin-Cre transgenic mice (C57Bl/6J background) to generate liver-specific FGF21 knockout (FGF21fl/fl;Albumin-Cre) or adipose-specific FGF21 knockout (FGF21fl/fl;Adiponectin-Cre) mice, respectively. Mice were maintained on a chow (2920X; Teklad Global Diets, Harlan Laboratories) or high-fat diet (HFD; Research Diets [D12492i]). Twenty-four hour fasting experiments were performed from 9 a.m. to 9 a.m., and refeeding was performed via oral gavage as previously described (17). Plasma glucose, insulin, triglycerides, nonesterified fatty acid (NEFA), and β-hydroxybutyrate were determined as previously described (12,17). For measurement of plasma glucagon, plasma was mixed with aprotinin and then snap-frozen in liquid nitrogen and stored at −80°C until assayed by the Vanderbilt Hormone Assay & Analytical Services Core. Plasma FGF21 was measured using an FGF21 ELISA assay (BioVendor). All procedures and use of mice were approved by the Institutional Animal Care and Use Committee of the University of Iowa.
In Vivo Glucose Uptake Assays
Six-week-old male wild-type (WT) and FGF21 liver-specific knockout mice (FGF21 LivKO) were placed on an HFD for 6 weeks. After an overnight fast, tail blood was collected from all mice (time = 0). All mice were then injected with 8–10 µCi [3H]2-deoxyglucose i.p. in a 20% glucose solution and tail blood was collected over the course of 60 min (15 min, 30 min, and 60 min). At the end of the time course, all mice were killed by decapitation and tissues immediately dissected, flash frozen in liquid nitrogen, and placed at −80°C until analysis. Plasma radioactivity (18) and determination of tissue-specific uptake of [3H]2-deoxyglucose was performed as previously described (19,20).
Isolation of Primary Brown and White Adipocytes
Primary brown and white preadipocytes were isolated from the intrascapular brown fat and white fat depots, respectively, of 4-day-old C57Bl6 pups as previously described (21).
In Vitro Glucose Uptake
Primary adipocytes were treated with one of the following conditions prepared in glucose-free media: vehicle, insulin (100 nmol/L), FGF21 (1 µg/mL), or insulin combined with FGF21. Recombinant FGF21 generation and purification have previously been described (12). Adipocytes were treated for 60 min, followed by in vitro glucose uptake assays performed as previously described (7).
Data Analysis
Gene expression analyses were performed as previously described (12). Statistical comparison of two groups was determined using Student t test.
Results and Discussion
Plasma FGF21 Levels Are Derived From the Liver and Regulate Fasting and Refeeding Responses
To examine the physiological conditions regulating FGF21 levels, we profiled plasma FGF21 protein levels during fed, fasted, or refed conditions and compared them with circulating insulin levels. Plasma FGF21 levels were increased with 24 h fasting and remained elevated 15 min after refeeding (Supplementary Fig. 1A), when insulin levels were also elevated (Supplementary Fig. 1B). The increased circulating FGF21 concentrations observed after refeeding are likely residual levels produced during fasting, as circulating FGF21 levels return to those of the fed state by 1 h (Supplementary Fig. 1A), consistent with the half-life of FGF21 in mice being <30 min (9). Notably, the time period immediately after refeeding is a unique physiological condition in which both FGF21 and insulin are circulating.
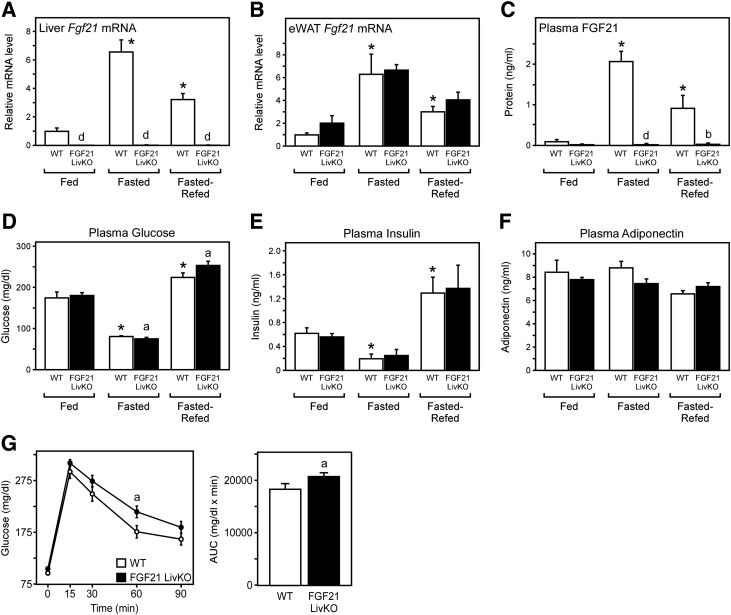
To determine which tissues contribute to circulating FGF21, we generated FGF21 LivKO mice by crossing FGF21fl/fl mice with albumin-Cre transgenic mice. Fed, fasted, or refed WT and FGF21 LivKO mice were analyzed. While Fgf21 mRNA was induced in the livers of fasted and refed WT mice, Fgf21 mRNA expression was completely abolished in the livers (Fig. 1A), but not epididymal WAT (eWAT) (Fig. 1B), of FGF21 LivKO mice. Plasma FGF21 was induced during fasting and refeeding in WT mice but was abolished in FGF21 LivKO mice (Fig. 1C). There was no difference in the level of fed plasma glucose between groups. However, fasted FGF21 LivKO mice exhibited a slight, but significant, decrease in plasma glucose (Fig. 1D). Importantly, refed FGF21 LivKO mice had significantly elevated plasma glucose compared with WT littermates (Fig. 1D) despite having similar plasma insulin (Fig. 1E) and adiponectin (Fig. 1F) levels. FGF21 LivKO mice displayed an elevation in their glucose excursion curves compared with WT littermates when subjected to a glucose tolerance test (GTT) (Fig. 1G), despite having insulin levels similar to control (data not shown). Together, these data show that the function of FGF21 extends beyond fasting into the early refeeding response to enhance insulin-stimulated glucose uptake.
Figure 1.
Generation and characterization of FGF21 LivKO mice. A–F: 12- to 14-week-old male WT (FGF21fl/fl) and FGF21 LivKO mice were either ad libitum–fed chow, fasted 24 h, or fasted 24 h and then refed for 15 min via oral gavage (n = 5–8/group). Levels of hepatic Fgf21 mRNA (A), eWAT Fgf21 mRNA (B), plasma FGF21 protein (C), plasma glucose (D), plasma insulin (E), and plasma adiponectin (F) in the indicated mice are shown. G: Levels of plasma glucose and area under the curve (AUC) from WT and FGF21 LivKO mice during a GTT (n = 5–6/group). Data are presented as mean ± SEM. Different lowercase letters represent statistical significance between genotypes (a, P < 0.05; b, P < 0.01; d, P < 0.001). *Significance between control mice in different conditions (P < 0.05).
Liver, but Not Adipose, Produces Circulating FGF21 to Improve Insulin Sensitivity in Mice With DIO
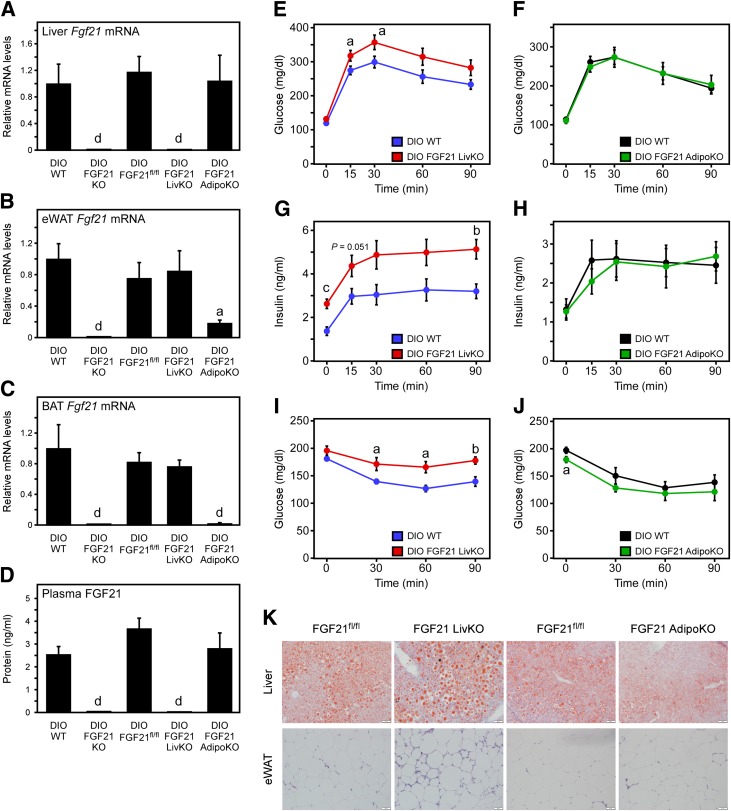
Circulating FGF21 levels are elevated in obese and diabetic rodents and humans (rev. in 2). To determine the relative tissue-specific contribution and function of FGF21 during obesity, we generated both liver-specific and adipose-specific DIO FGF21 knockout mice. Adipose-specific FGF21 knockout mice (FGF21 AdipoKO) were generated by crossing FGF21fl/fl mice with adiponectin-Cre transgenic mice. We then examined HFD diet DIO WT, FGF21 total knockout, FGF21fl/fl, FGF21 LivKO, and FGF21 AdipoKO mice. Fgf21 mRNA expression was completely abolished in the livers of DIO FGF21 LivKO mice (Fig. 2A), while eWAT (Fig. 2B) and BAT (Fig. 2C) Fgf21 mRNA levels remained unchanged. In contrast, the levels of Fgf21 mRNA were significantly reduced in eWAT (Fig. 2B) and BAT (Fig. 2C) of DIO FGF21 AdipoKO mice, while levels of hepatic Fgf21 mRNA expression remained unchanged (Fig. 2A). Notably, plasma FGF21 levels were completely abolished in DIO FGF21 LivKO mice, while DIO FGF21 AdipoKO mice had normal levels of plasma FGF21 (Fig. 2D). These results demonstrate that elevated circulating FGF21 in obesity is derived from the liver.
Figure 2.
Loss of liver-derived FGF21, but not adipose-derived FGF21, impairs glucose homeostasis and insulin sensitivity in DIO mice. A–D: DIO WT, FGF21 total knockout (KO), FGF21fl/fl, FGF21 LivKO, and FGF21 AdipoKO mice were fed an HFD for 16 weeks. Levels of hepatic Fgf21 mRNA (A), eWAT Fgf21 mRNA (B), BAT Fgf21 mRNA (C), and plasma FGF21 protein (D) in the indicated mice are shown. E–K: Age-matched male FGF21fl/fl, FGF21 LivKO, and FGF21 AdipoKO mice were individually caged and maintained on chow diet until 10 weeks of age. At 10 weeks of age, all mice were placed on HFD for 10 weeks (n = 8–9/group). FGF21fl/fl control mice were compared only with their knockout littermates. Levels of plasma glucose (E and F) and plasma insulin (G and H) during a GTT (n = 6/group). GTTs were performed by administering 2 g glucose/kg lean body wt i.p. to mice that had been fasted for 16 h. I and J: Plasma glucose levels during an ITT (n = 5–6/group). ITTs were performed by administering 0.75 units insulin/kg body wt i.p. to mice fasted for 4–6 h. K: Oil Red O staining of livers and hematoxylin-eosin staining of eWAT. Data are presented as mean ± SEM. Different lowercase letters represent statistical significance (a, P < 0.05; b, P < 0.01; c, P < 0.005; d, P < 0.001).
For assessment of the function of hepatic and adipose FGF21, FGF21 LivKO and FGF21 AdipoKO mice were phenotypically characterized on normal chow and an HFD. Body weight (Supplementary Fig. 2A and B), percent fat (Supplementary Fig. 2C and D), and percent lean mass (Supplementary Fig. 2E and F) were not statistically different between FGF21 LivKO and FGF21 AdipoKO mice and their age- and sex-matched control littermates (FGF21fl/fl) either at baseline or on HFD. However, during HFD feeding FGF21 AdipoKO mice exhibited a trend toward reduced percent fat at the 8-week (P = 0.055) and 10-week (P = 0.086) time points (Supplementary Fig. 2D). No statistically significant differences in food intake, plasma triglycerides, nonesterified free fatty acids (NEFAs), glucagon, or ketones were observed between DIO WT and FGF21 LivKO or DIO WT and FGF21 AdipoKO mice (Table 1).
Table 1.
Plasma parameters of DIO FGF21 tissue-specific knockout mice
| DIO FGF21fl/fl | DIO FGF21 LivKO | DIO FGF21fl/fl | DIO FGF21 AdipoKO | |
|---|---|---|---|---|
| n | 8 | 9 | 8 | 8 |
| Food intake (g/day) | 2.61 ± 0.08 | 2.60 ± 0.07 | 2.65 ± 0.06 | 2.68 ± 0.10 |
| Triglycerides (mg/dL) | 65.70 ± 3.75 | 62.73 ± 2.70 | 74.80 ± 4.64 | 82.58 ± 5.89 |
| NEFAs (mmol/L) | 0.49 ± 0.03 | 0.50 ± 0.03 | 0.58 ± 0.04 | 0.53 ± 0.03 |
| β-Hydroxybutyrate (µmol/L) | 54.86 ± 9.87 | 60.78 ± 6.67 | 56.67 ± 7.11 | 43.84 ± 5.09 |
| Glucagon (pg/mL) | 85.99 ± 20.26 | 77.95 ± 26.84 | 50.78 ± 4.10 | 65.24 ± 8.56 |
| Adiponectin (ng/mL) | 15.07 ± 0.44 | 14.57 ± 0.17 | 15.03 ± 0.51 | 15.27 ± 0.50 |
Data are mean ± SEM unless otherwise indicated. Plasma parameters were measured in DIO FGF21 LivKO, FGF21 AdipoKO, and FGF21fl/fl littermate controls.
For determination of whether DIO FGF21 LivKO or FGF21 AdipoKO mice had impaired glucose homeostasis, mice were subjected to GTTs and insulin tolerance tests (ITTs). Unlike lean mice, fasted DIO WT mice (3.0 ± 0.50 ng ⋅ mL−1) show circulating FGF21 levels similar to those in fed DIO WT mice (2.8 ± 0.20 ng ⋅ mL−1). DIO FGF21 LivKO mice, but not DIO FGF21 AdipoKO mice, exhibited a markedly increased glucose excursion curve in response to the GTT compared with WT littermates (Fig. 2E and F). DIO FGF21 LivKO mice also possessed significantly elevated plasma insulin levels throughout the GTT, suggesting increased insulin resistance (Fig. 2G). ITTs revealed that DIO FGF21 LivKO mice had an impaired response to insulin compared with DIO WT littermates (Fig. 2I), while DIO FGF21 AdipoKO mice had normal insulin tolerance (Fig. 2J). Consistent with increased insulin resistance, DIO FGF21 LivKO mice displayed increased hepatic lipid accumulation (Fig. 2K and Supplementary Fig. 2G) and WAT fibrosis compared with WT littermates (Fig. 2K), an effect not observed between DIO FGF21 AdipoKO and WT littermates (Fig. 2K). Recently, it was reported that FGF21 functions pharmacologically by inducing adiponectin levels (22,23). Plasma adiponectin levels were not significantly different in FGF21 LivKO or FGF21 AdipoKO mice compared with WT controls (Table 1). Therefore, loss of hepatic, but not adipose, FGF21 levels impairs insulin sensitivity in HFD-fed mice independent of changes in adiponectin levels.
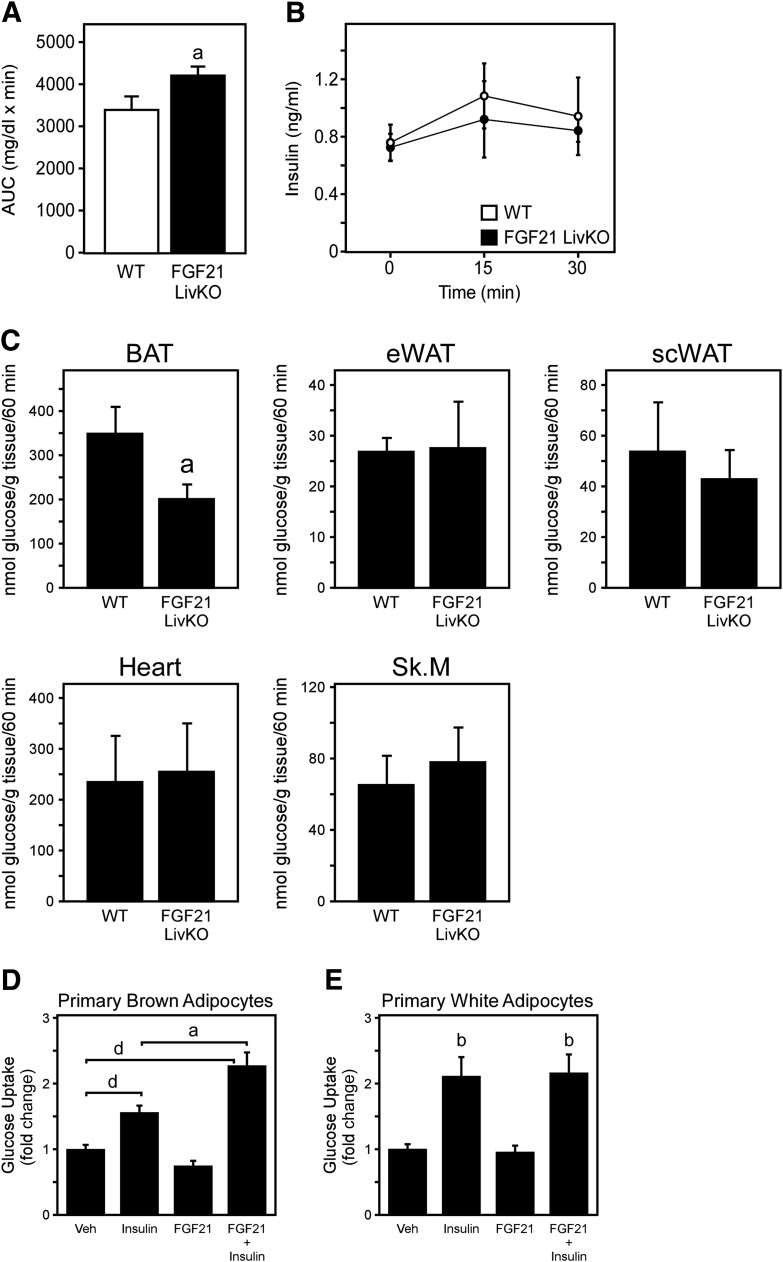
FGF21 Is Induced in Liver by HFD Feeding to Drive Glucose Disposal Into BAT In Vivo
To determine which tissue(s) have reduced glucose disposal and may be responsible for the DIO FGF21 LivKO phenotype, we analyzed tissue-specific glucose uptake in WT and FGF21 LivKO mice fed an HFD for 6 weeks. This was accomplished by injecting mice with labeled [3H]2-deoxyglucose in a 20% glucose bolus to assess glucose uptake during a physiological insulin response. FGF21 LivKO mice on HFD for 6 weeks also exhibited an increased glucose excursion curve compared with WT controls (Fig. 3A). Notably, this increased glucose excursion in the FGF21 LivKO mice fed HFD for 6 weeks occurred despite having normal plasma insulin levels (Fig. 3B), unlike FGF21 LivKO mice fed HFD for 10 weeks (Fig. 2G). Interestingly, FGF21 LivKO mice had a lower rate of glucose uptake in BAT, but not in eWAT, subcutaneous WAT, skeletal muscle, or heart (Fig. 3C). We conclude that FGF21 regulates glycemia at least in part by effecting glucose disposal into BAT in DIO mice. FGF21 has also been shown to reduce hepatic glucose production during obesity (rev. in 2), so multiple mechanisms may be responsible for FGF21-mediated effects on glucose homeostasis. FGF21 enhances glucose disposal under specific physiologic conditions, and a limitation of this study is that only glucose metabolism was examined. Thus, we cannot rule out that other metabolic pathways are regulated by FGF21 under these or other physiological conditions.
Figure 3.
Loss of hepatic FGF21 impairs glucose uptake into BAT in vivo. Plasma glucose area under the curve (AUC) (A), plasma insulin levels (B), and rates of glucose uptake (C) in unanesthetized male WT and FGF21 LivKO fed HFD for 6 weeks. All mice were administered [3H]2-deoxyglucose after an overnight fast; glucose uptake was measured in BAT, eWAT, subcutaneous WAT, heart, and skeletal muscle (tibialis anterior) (n = 5–7/group). Glucose uptake assays in primary brown adipocytes (D) and primary white adipocytes (E) treated with vehicle (Veh), insulin (100 nmol/L), FGF21 (1 µg/mL), or FGF21 plus insulin. Experiments were performed in triplicate twice. Data are presented as mean ± SEM. Different lowercase letters represent statistical significance (a, P < 0.05; b, P < 0.01; d, P < 0.001).
We next examined whether FGF21 can act directly on brown adipocytes to stimulate glucose uptake. Primary brown and white preadipocytes were isolated, differentiated, and then treated with vehicle, insulin, FGF21, or both insulin and FGF21 for 1 h. While extended treatment (24 h) of white adipocytes with FGF21 stimulates glucose uptake independent of insulin (7), 1-h treatment with FGF21 alone did not stimulate glucose uptake in either brown (Fig. 3D) or white (Fig. 3E) adipocytes. Insulin alone, however, was able to significantly increase glucose uptake in brown (Fig. 3D) and white (Fig. 3E) adipocytes. Interestingly, cotreatment of insulin with FGF21 synergistically increased glucose uptake in primary brown adipocytes (Fig. 3D) but not white adipocytes (Fig. 3E). These data demonstrate that FGF21 can signal directly to brown adipocytes to enhance insulin-stimulated glucose uptake and that loss of circulating FGF21 impairs glucose uptake in BAT of DIO mice. These results, however, do not exclude the possibility that FGF21 may also regulate BAT activity through indirect mechanisms (e.g., sympathetic nerve activity) in vivo. Therefore, just as FGF21 functions early during refeeding to mitigate physiological peripheral insulin resistance, FGF21 may also function during overfeeding to overcome diet-induced insulin resistance.
In summary, our data are compatible with FGF21 functioning beyond the fasting/starvation response to enhance insulin action during refeeding and overfeeding. Thus, FGF21 acts as an insulin sensitizer under physiologic conditions, which may explain its acute pharmacological actions. FGF21 may promote glucose uptake into adipose during refeeding to maximize energy replenishment and during overfeeding to protect against lipotoxicity. Interestingly, the ability of FGF21 to enhance insulin action may explain why pharmacological administration of FGF21 increases insulin sensitivity in obese mice, where circulating insulin levels are already elevated, but not in lean mice. Understanding the mechanisms regulating FGF21-mediated enhancement of insulin sensitivity may provide important insight into new treatments for metabolic disease.
Supplementary Material
Article Information
Acknowledgments. The authors thank Dr. Andrew Norris (University of Iowa) for expert advice on in vivo glucose uptake assays and Dr. Dale Abel (University of Iowa) for helpful discussions.
Funding. This work was supported by an American Diabetes Association Junior Faculty award (7-13-JF-49 to M.J.P.), an Edward Mallinckrodt, Jr. Foundation grant (to M.J.P.), and a University of Iowa Carver Trust Medical Research Initiative grant (to M.J.P.). This work also received generous research support from the Fraternal Order of Eagles Diabetes Research Center (to M.J.P.), National Institutes of Health (NIH) grants R01-DK-067158 (to D.J.M. and S.A.K.) and R01-DE-013686 (to M.M.), the Robert A. Welch Foundation (grant I-1275 to D.J.M. and grant I-1558 to S.A.K.), and the Howard Hughes Medical Institute (to D.J.M.). The Vanderbilt Hormone Assay & Analytical Services Core (assayed plasma glucagon levels) is supported by NIH grant DK-20593.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. K.R.M. designed the experiments, performed in vitro and in vivo radioactive glucose uptake assays, and wrote the manuscript. M.C.N. performed in vitro and in vivo radioactive glucose uptake assays, performed gene expression analyses, and reviewed the manuscript. M.K.A. and M.D.A. performed gene expression analyses and reviewed the manuscript. D.J.M., S.A.K., and M.M. generated critical reagents and reviewed the manuscript. M.J.P. designed the experiments and wrote the manuscript. M.J.P. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db14-0595/-/DC1.
References
- 1.Kurosu H, Choi M, Ogawa Y, et al. Tissue-specific expression of betaKlotho and fibroblast growth factor (FGF) receptor isoforms determines metabolic activity of FGF19 and FGF21. J Biol Chem 2007;282:26687–26695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Potthoff MJ, Kliewer SA, Mangelsdorf DJ. Endocrine fibroblast growth factors 15/19 and 21: from feast to famine. Genes Dev 2012;26:312–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angelin B, Larsson TE, Rudling M. Circulating fibroblast growth factors as metabolic regulators—a critical appraisal. Cell Metab 2012;16:693–705 [DOI] [PubMed] [Google Scholar]
- 4.Zhao Y, Dunbar JD, Kharitonenkov A. FGF21 as a therapeutic reagent. Adv Exp Med Biol 2012;728:214–228 [DOI] [PubMed] [Google Scholar]
- 5.Gaich G, Chien JY, Fu H, et al. The effects of LY2405319, an FGF21 analog, in obese human subjects with type 2 diabetes. Cell Metab 2013;18:333–340 [DOI] [PubMed] [Google Scholar]
- 6.Xu J, Stanislaus S, Chinookoswong N, et al. Acute glucose-lowering and insulin-sensitizing action of FGF21 in insulin-resistant mouse models—association with liver and adipose tissue effects. Am J Physiol Endocrinol Metab 2009;297:E1105–E1114 [DOI] [PubMed] [Google Scholar]
- 7.Kharitonenkov A, Shiyanova TL, Koester A, et al. FGF-21 as a novel metabolic regulator. J Clin Invest 2005;115:1627–1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Véniant MM, Komorowski R, Chen P, et al. Long-acting FGF21 has enhanced efficacy in diet-induced obese mice and in obese rhesus monkeys. Endocrinology 2012;153:4192–4203 [DOI] [PubMed] [Google Scholar]
- 9.Kharitonenkov A, Wroblewski VJ, Koester A, et al. The metabolic state of diabetic monkeys is regulated by fibroblast growth factor-21. Endocrinology 2007;148:774–781 [DOI] [PubMed] [Google Scholar]
- 10.Ding X, Boney-Montoya J, Owen BM, et al. βKlotho is required for fibroblast growth factor 21 effects on growth and metabolism. Cell Metab 2012;16:387–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams AC, Yang C, Coskun T, et al. The breadth of FGF21’s metabolic actions are governed by FGFR1 in adipose tissue. Mol Metab 2012;2:31–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Potthoff MJ, Inagaki T, Satapati S, et al. FGF21 induces PGC-1alpha and regulates carbohydrate and fatty acid metabolism during the adaptive starvation response. Proc Natl Acad Sci U S A 2009;106:10853–10858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Postic C, Shiota M, Niswender KD, et al. Dual roles for glucokinase in glucose homeostasis as determined by liver and pancreatic beta cell-specific gene knock-outs using Cre recombinase. J Biol Chem 1999;274:305–315 [DOI] [PubMed] [Google Scholar]
- 14.Eguchi J, Wang X, Yu S, et al. Transcriptional control of adipose lipid handling by IRF4. Cell Metab 2011;13:249–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee KY, Russell SJ, Ussar S, et al. Lessons on conditional gene targeting in mouse adipose tissue. Diabetes 2013;62:864–874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodríguez CI, Buchholz F, Galloway J, et al. High-efficiency deleter mice show that FLPe is an alternative to Cre-loxP. Nat Genet 2000;25:139–140 [DOI] [PubMed] [Google Scholar]
- 17.Potthoff MJ, Boney-Montoya J, Choi M, et al. FGF15/19 regulates hepatic glucose metabolism by inhibiting the CREB-PGC-1α pathway. Cell Metab 2011;13:729–738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mauvais-Jarvis F, Virkamaki A, Michael MD, et al. A model to explore the interaction between muscle insulin resistance and beta-cell dysfunction in the development of type 2 diabetes. Diabetes 2000;49:2126–2134 [DOI] [PubMed] [Google Scholar]
- 19.Ferré P, Leturque A, Burnol AF, Penicaud L, Girard J. A method to quantify glucose utilization in vivo in skeletal muscle and white adipose tissue of the anaesthetized rat. Biochem J 1985;228:103–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fujii N, Hirshman MF, Kane EM, et al. AMP-activated protein kinase alpha2 activity is not essential for contraction- and hyperosmolarity-induced glucose transport in skeletal muscle. J Biol Chem 2005;280:39033–39041 [DOI] [PubMed] [Google Scholar]
- 21.Dutchak PA, Katafuchi T, Bookout AL, et al. Fibroblast growth factor-21 regulates PPARγ activity and the antidiabetic actions of thiazolidinediones. Cell 2012;148:556–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holland WL, Adams AC, Brozinick JT, et al. An FGF21-adiponectin-ceramide axis controls energy expenditure and insulin action in mice. Cell Metab 2013;17:790–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin Z, Tian H, Lam KS, et al. Adiponectin mediates the metabolic effects of FGF21 on glucose homeostasis and insulin sensitivity in mice. Cell Metab 2013;17:779–789 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.