Abstract
Introduction:
Antimicrobials are widely used in infectious diseases. Only the timely intervention will contribute to the positive outcome of the disease. Unjustified use of antimicrobial prophylaxis may have adverse effects, i.e., result in bacterial resistance to existing antimicrobials, as well as toxic effects on leukocyte lineage and other parameters of the blood.
Goal:
The goal of this study was to confirm that the antimicrobial therapy of urinary, gynecological and respiratory infections has a toxic effect on leukocyte lineage. Followed by lowered immunity and the emergence of risk for health complications especially in oncology and other immunodeficient patients for whom to apply pharmacotherapy it is necessary to have adequate immunity, or white blood cell count that is greater than 4.0x109/L.
Material and methods:
A prospective-retrospective study was conducted on a sample of 30 patients in a Primary Health Care Center in Gracanica during the period from March 01, 2013 until April 01, 2014. Testing of this sample was conducted by survey on health status and treatment, or on taking of antimicrobial therapy and other treatment regimens, with the referral diagnosis and determination of leukocytes count in by hematology counter SYSMEX. Results of leukocytes below and close to the lower reference values were statistically analyzed by Students t-test.
Results:
Mean WBC count in the group treated with antimicrobial therapy was 3.687±0.83 x109/L, in the group which during repeated infection did not use the antimicrobial therapy 5.09±1.04 x109/L, and in the control group of healthy subjects 7.178±1.038 x109/L. Statistical analysis with Student’s t test indicate highly significant differences between group of patients that used antimicrobial therapy with the group of patient that did not used antimicrobial during repeated infection (t=6.091; p=0.0001), as well as significant differences in mean WBC count of both of these groups and the controls (t=4.984; p=0.0001, and t=8.402, p=0.0001).
Conclusion:
Use of antimicrobial drugs leads to serious toxic reactions, or leukopenia. Indications for the use of antimicrobial therapy must be strictly followed, because banal, frequent infections are not indication for antimicrobial therapy. It is necessary to know the types of infection causes. Important is the proper and timely selection of antimicrobial therapy. When selecting the drug we should bear in mind its antimicrobial activity, pharmacokinetic and toxic properties, as well as patient health status. Possible is also the application of preventive medicine as well as other manner of solving infection.
Keywords: antimicrobials, toxic effects, WBC count
1. INTRODUCTION
Antimicrobial therapy involves the application of a remedy against the presumed cause, the microbes. Antimicrobials should have a strong enough chemotherapy activity only toward responsible microbes and limited toxicity to the host (1-6).
Antimicrobials are widely used in infectious diseases. Only the timely intervention will contribute to the positive outcome of the disease (7-11).
Unjustified use of antimicrobial prophylaxis may have adverse effects, i.e., result in bacterial resistance to existing antimicrobials, as well as toxic effects on leukocyte lineage and other parameters of the blood.
This results in a new health problems caused by the decrease of the immunity due to leukopenia and neutropenia, disturbance of flora and electrolytes balance. This further requires a new pharmacotherapy: antimicrobial treatment–antibiotics, as protective, vitamins, immunostimulant drugs and electrolytes.
Also notable are the costs for all that pharmacotherapy, immune therapy and necessary replacement therapy.
2. GOAL
The goal of this study was to confirm that the antimicrobial therapy of urinary, gynecological and respiratory infections has a toxic effect on leukocyte lineage. Followed by lowered immunity and the emergence of risk for health complications especially in oncology and other immunodeficient patients for whom to apply pharmacotherapy it is necessary to have adequate immunity, or white blood cell count that is greater than 4.0x109/L.
3. MATERIAL AND METHODS
A prospective-retrospective study was conducted on a sample of 30 patients in a Primary Health Care Center in Gracanica during the period from March 01, 2013 until April 01, 2014. Testing of this sample was conducted by survey on health status and treatment, or on taking of antimicrobial therapy and other treatment regimens, with the referral diagnosis and determination of leukocytes count in by hematology counter SYSMEX. Results of leukocytes below and close to the lower reference values were statistically analyzed by Students t-test.
4. RESULTS
It is obvious that patients who have a referral diagnosis of urinary tract, gynecological and respiratory infections require the determination of the leukocytes count in the period from March 01, 2013 to April 01, 2014. Tests on a sample of 23 patients who used pharmacotherapy for present urinary, gynecological and respiratory infections are carried out by survey and leukocytes count. Results show that the number of leukocytes in 80 % of cases at or near the lower level of the reference range, or in 24 cases we had mild to moderate leukopenia.
During the study to patients was suggested (in consultation with their doctors) that in case of repeated urinary, gynecological and respiratory infections not to use specific antimicrobial therapy but urinary antiseptic, as well as other antiseptics and immune stimulating pharmacotherapy.
By examining the leukocytes count at the end of the study period in all cases we have 20% to 30% (or 25%) higher leukocytes count.
In the study we included a control group of 20 healthy respondents aged 19-25 years who had a WBC count in the range from 5.1 to 8.9x109/L.
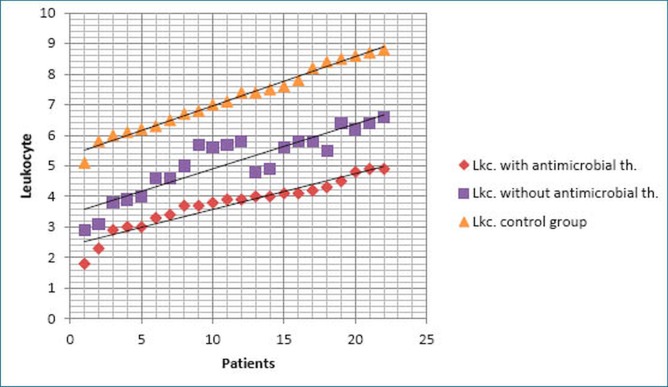
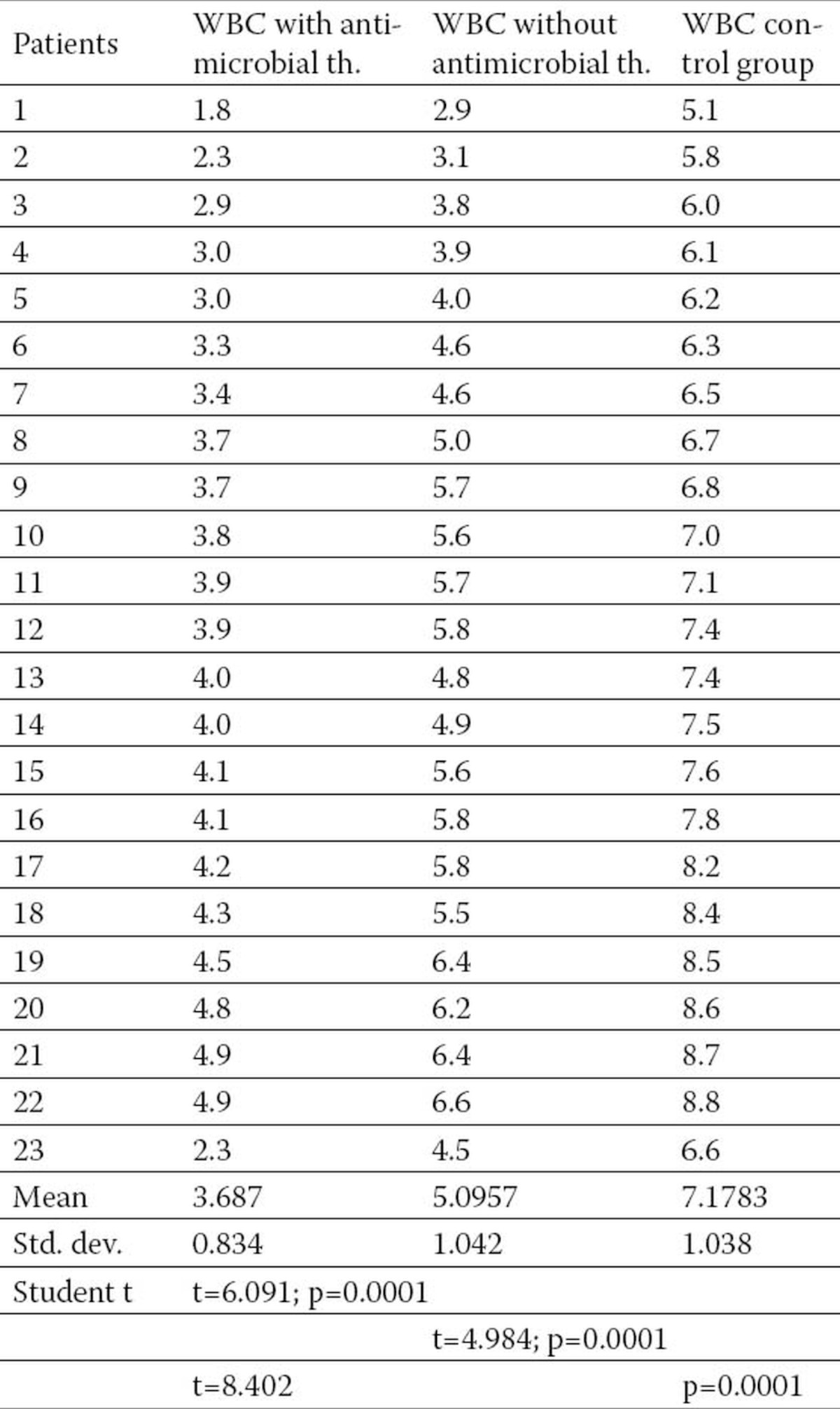
As we can see from the Figure and Table 1 the mean WBC count in the group treated with antimicrobial therapy was 3.687±0.83 x109/L, in the group which during repeated infection did not use the antimicrobial therapy 5.09±1.04 x109/L, and in the control group of healthy subjects 7.178±1.038 x109/L. Statistical analysis with Student’s t test indicate highly significant differences between group of patients that used antimicrobial therapy with the group of patient that did not used antimicrobial during repeated infection (t=6.091; p=0.0001), as well as significant differences in mean WBC count of both of these groups and the controls (t=4.984; p=0.0001, and t=8.402, p=0.0001).
Figure 1.
Leukocytes counts of patients with and without antimicrobial therapy and the control group.
Table 1.
Number of leukocytes in patients with and without antimicrobial therapy and the control group
5. DISCUSSION
Uncritical use of antimicrobial drugs carries many risks, the occurrence of severe toxic reactions as in our case leukopenia and the development of resistant strains of bacteria, disruption of the normal bacterial flora (and the possibility of superinfection), the occurrence of hypersensitivity to the drug.
Empirical antibiotic-antimicrobial therapy may be more harmful than helpful because of its often unjustified use for prophylactic purposes and not in therapeutic application as which has the consequence of new health problems.
Patients are often infected with opportunistic organisms that are far more resistant to antimicrobials. As a consequence we have economic problems because of the steady increase in the total cost of the medication, both for the patient and the health insurance fund (the cost of antibiotics amount to 1/3 of the total heal care costs).
6. CONCLUSION
Use of antimicrobial drugs leads to serious toxic reactions, or leukopenia. In our sample 80% of patients with antimicrobial therapy had by 20-30% reduction in the number of leukocytes in relation to the tests conducted on the same patients without antimicrobial therapy in case of reinfection. Indications for the use of antimicrobial therapy must be strictly followed, because banal, frequent infections are not indication for antimicrobial therapy. It is necessary to know the types of infection causes. Important is the proper and timely selection of antimicrobial therapy. When selecting the drug we should bear in mind its antimicrobial activity, pharmacokinetic and toxic properties, as well as patient health status. Possible is also the application of preventive medicine as well as other manner of solving infection.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Rang HP, Dale MM, Ritter JM, Moore PK. translation of the book: Pharmacology. Data status. 5th edition. Beograd: 2005. Farmakologija. [Google Scholar]
- 2.Šibalić S. Printcom, Tuzla: 2008. Antimikrobna sredstva i ljekar praktičar. [Google Scholar]
- 3.Varagić VM, Milošević MP. Beograd: 1999. Farmakologija, XV prerađeno i dopunjeno izdanje. [Google Scholar]
- 4.Vučetić JI. Velarta, Beograd: 1998. Mikrobiološke sinteze antibiotika. [Google Scholar]
- 5.Hukić M. Jež, Sarajevo: 2005. i sar.:Bakteriologija. [Google Scholar]
- 6.Jež, Sarajevo: 2009. Registar lijekova sa osnovama farmakoterapije. Federalno ministarstvo zdravstva, Udruženje farmakologa Federacije BiH. [Google Scholar]
- 7.Riley MA, Chavan MA. New York: Springer; 2007. Bacteriocins Ecology and Evolution. [Google Scholar]
- 8.Harrison G. Split: Placebo; 1997. Principi interne medicine, prevod trinaestog izdanja knjige Principles of Internal medicine. [Google Scholar]
- 9.Varma A, Podila GK. Microbiology series. New Delhi: 2005. Biotechnological Applications of microbes. [Google Scholar]
- 10.Cascales E, Buchanan SK, et al. Colicin biology. Microbiology and Molecular biology Reviews. 2007 Mar;71:158–229. doi: 10.1128/MMBR.00036-06. http://mmbr.asm.org/cgi/content/full/71/1/158 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jenssen H, Hamill P, Hancock R. Clinical Microbiology. London: Oxford Press; 2011. Peptide Antimicrobal Agents. [DOI] [PMC free article] [PubMed] [Google Scholar]