Abstract
BACKGROUND AND OBJECTIVES:
Foster youth have high rates of health problems in childhood. Little work has been done to determine whether they are similarly vulnerable to increased health problems once they transition to adulthood. We sought to prospectively evaluate the risk of cardiovascular risk factors and other chronic conditions among young adults formerly in foster care (FC) and young adults from economically insecure (EI) and economically secure (ES) backgrounds in the general population.
METHODS:
We used data from the Midwest Evaluation of the Adult Functioning of Former Foster Youth (FC group; N = 596) and an age-matched sample from the National Longitudinal Study of Adolescent Health (EI and ES groups; N = 456 and 1461, respectively). After controlling for covariates, we performed multivariate regressions to evaluate health outcomes and care access by group at 2 time points (baseline at late adolescence, follow-up at 25–26 years).
RESULTS:
Data revealed a consistent pattern of graduated increase in odds of most health outcomes, progressing from ES to EI to FC groups. Health care access indicators were more variable; the FC group was most likely to report having Medicaid or no insurance but was least likely to report not getting needed care in the past year.
CONCLUSIONS:
Former foster youth appear to have a higher risk of multiple chronic health conditions, beyond that which is associated with economic insecurity. Findings may be relevant to policymakers and practitioners considering the implementation of extended insurance and foster care programs and interventions to reduce health disparities in young adulthood.
Keywords: foster youth, young adult, cardiovascular disease, health care disparities
What’s Known on This Subject:
Youth in foster care are at higher risk of health problems at entrance and during their stays in care. Little is known about this group’s risk of health problems in young adulthood, in comparison with other populations of young adults.
What This Study Adds:
This is the first prospective study to our knowledge demonstrating that former foster youth are at higher risk of chronic health problems than economically secure and insecure general population young adults.
Foster youth are an understudied population with high rates of chronic and untreated health conditions, both upon entrance into and while in foster care.1–5 Consequently, in 2009 the Institute of Medicine highlighted them as a priority population for federally funded research.6
There are many reasons to expect that former foster youth may be vulnerable to similarly elevated rates of chronic health problems once they transition to adulthood. Foster youth are often exposed to poverty and many other adverse childhood experiences including abuse, neglect, domestic violence, and parental substance use, and many undergo frequent placement and school changes while in foster care.1,7,8 Several theories exist regarding the effects of chronic and early exposures to adversity, all of which suggest that the more stressors to which one is exposed, the higher the likelihood of a chronic physical or mental health condition later in life.9–15 However, to our knowledge only 1 retrospective study has evaluated this question specifically in foster youth; this study suggested that adults with foster care experience had higher odds of a physical health problem than those who had never been in foster care.16
In addition to, and likely because of, these early exposures, a large percentage of youth emancipating from foster care live in poverty or experience unemployment or homelessness in young adulthood, potentially limiting access to needed health care.17–22 Conversely, extended Medicaid and FC programs during young adulthood have been associated with improved reproductive health access and outcomes for this population; the impact of extended FC on other types of physical health problems in this population has not been studied.23,24 Two provisions of the Affordable Care Act (ACA), in effect as of 2014, are relevant to former foster youth: a provision extending Medicaid coverage through age 26 years to young adults who were in foster care on their 18th birthday and a provision that provides coverage to all nonelderly people with incomes ≤133% of the federal poverty level in participating states.24 However, many states have not extended Medicaid to low-income single adults, pursuant to a recent US Supreme Court decision that upheld the constitutionality of the ACA but also held that state participation in Medicaid expansion is optional.25 Thus, former foster youth who have incomes <133% of the federal poverty level who were not in care on their 18th birthday may not have access to Medicaid, depending on the state in which they were emancipated from care. Additionally, many states do not provide Medicaid coverage to former foster youth who were emancipated in another state. Finally, recent federal legislation has also provided financial incentives for states to extend foster care to age 21 (with accompanying extended medical coverage),26 although many still routinely discharge foster youth at age 18.
An understanding of this population’s risk of chronic medical problems and health care access will be helpful to inform policies and practices at the state and federal levels. Our objective was to compare the risks of chronic health problems and access indicators among young adults transitioning out of the foster system with those of youth in the general population with and without exposure to economic insecurity.
Methods
Study Design, Sample, and Data Collection Procedures
We used data from 2 longitudinal cohorts: the National Longitudinal Study of Adolescent Health (Add Health), a large, nationally representative sample of youth transitioning to adulthood in the United States,27 and the Midwest Evaluation of the Adult Functioning of Former Foster Youth (Midwest Study), a study evaluating youth in Illinois, Iowa, and Wisconsin as they transitioned out of foster care.1–4 Human subjects approval and informed consent were obtained in both studies. The present analyses were determined exempt for human subjects review, because all data were deidentified.
Add Health (Economically Secure and Insecure Groups)
The Add Health Study consists of 4 data waves collected primarily via in-home audio computer-assisted methods (baseline N for in-home interviews = 20 745). Youth were included in the current study if they participated in waves 3 (2001–2002) and 4 (2007–2009), were 25 to 26 years old at wave 4, and had not been in foster care by wave 3 (N = 1917). The sample was then subdivided into 2 groups. The economically insecure (EI) group included youth who reported any of the following in the past 12 months at wave 3: receipt of income from food stamps, Aid to Families With Dependent Children, public assistance, welfare, or a state Temporary Assistance to Needy Families program, inability to pay full amount of rent or utilities, eviction, having utilities shut off, inability to see doctor or dentist because they could not afford it, or current receipt of Medicaid (N = 456). The economically secure (ES) group included youth who reported none of these markers (N = 1461).
Midwest Study (foster care Group)
Youth were eligible for the Midwest Study if they were 17 years old at recruitment and had been in out-of-home care for ≥1 year. Youth who were in a psychiatric or correctional facility, were on runaway status, or had a disability preventing survey completion were excluded. Most interviews were conducted in person, and computer-assisted techniques were used for sensitive subjects. Participants were interviewed every 2 years until age 25 or 26; we used data from waves 1 (2002–2003; age 17–18) and 5 (2010–2011; age 25–26). A total of 732 participated in wave 1. Of those, 81% participated in wave 5 as well and were included in the current study (foster care or FC group; N = 596). Hereafter, wave 3 of Add Health and wave 1 of the Midwest Study will be referred to as time 1, and wave 4 of Add Health and wave 5 of the Midwest Study will be referred to as time 2.
Variables
All variables were collected via self-report.
Outcomes
Individual Health Outcomes
Data were available at time 1 and 2 in both studies for 2 outcomes: general health (dichotomized at fair/poor versus good/very good/excellent) and BMI.
We also evaluated several chronic health conditions assessed at time 2 only. Wording of questions for these variables differed slightly between studies (Table 1). Participants were initially asked whether they had a condition or health problem, whether it limited their activities, and how long it had been present. They were then asked about the following conditions: seizure disorder, attention-deficit/hyperactivity disorder (ADHD), asthma, dyslipidemia, hypertension, and diabetes. For these outcomes, youth were coded as 0 if the youth reported that a condition did not limit their daily activities or had been present for <1 year. We also assessed whether participants reported being a chronic, regular smoker, defined as having ever smoked “regularly” and smoking all of the past 30 days.
TABLE 1.
Wording of Specific Outcomes Assessed at Time 2 in Midwest and Add Health Studies
| Variable | Question Wording | |
|---|---|---|
| Midwest Study | Add Health Study | |
| Definition of chronic health condition | Participants initially asked, “Do you have any physical or mental health conditions or disabilities that limit the activities that you can do on a typical day?” | Participants initially asked, “The following questions are about activities you might do on a typical day. How much does your health now limit you in moderate activities such as moving a table, pushing a vacuum cleaner, bowling, playing golf?” |
| If yes, participants were then asked how long the condition had been present. | If yes, participants were then asked how much it limited their activities and how long the condition had been present. | |
| Definitions of specific health conditions | ||
| Seizure disorder | “Seizures or epilepsy.” | “Epilepsy or another seizure disorder.” |
| ADHD | “ADHD or hyperactivity or ADD.” | “Attention problems or ADD or ADHD.” |
| Asthma | “Asthma, chronic bronchitis, emphysema.” | “Asthma or reactive airways disease.” |
| Dyslipidemia | “Increased blood cholesterol or triglycerides or lipids.” | “High cholesterol or high lipids.” |
| Hypertension | “High blood pressure or hypertension.” | Same except if female, added, “when you were not pregnant.” |
| Diabetes | “Diabetes or high blood sugar.” | Same except if female, added “when you were not pregnant.” |
ADD, attention-deficit disorder.
Combined Health Outcome Variables (Time 2 Only)
We generated 2 summary variables: any cardiovascular risk factor (dyslipidemia, hypertension, diabetes, smoker, or BMI ≥30) and other chronic illness (seizure disorder, ADHD, or asthma).
Health Care Access Indicators (Time 2 Only)
We assessed the following dichotomous variables: no insurance, having Medicaid, not getting needed medical care in the past year, and time since last physical examination (≤1 year versus >1 year).
Covariates
We included gender, race (white versus African American versus other race), ethnicity (Hispanic versus non-Hispanic), education level at time 2 (high school diploma versus no diploma) and economic insecurity at time 2 (defined as currently homeless or any of the following in the past 12 months: inability to pay full amount of rent or utilities, eviction, utilities shut off, or being worried whether food would run out before there was money to buy more), and current age as covariates in the main analyses. For female-only analyses, we also included a variable reflecting history of past or current pregnancy, given a known impact on some outcomes (eg, diabetes, hypertension).
Analyses
We performed descriptive statistics comparing univariate associations between the covariates and group status, then we used multivariate regression analyses (linear for continuous outcomes, logistic for dichotomous outcomes) to compare the health outcomes across groups after controlling for covariates. For outcomes measured at times 1 and 2 (BMI, general health), we used multiple regression analyses for repeated measures. As exploratory analyses, we ran these models with and without time by EI and time by FC interaction terms to determine whether the effect of group differed at the 2 time points. We also assessed the following outcomes for moderation by gender due to a priori hypotheses of a potential gender by group interaction: BMI, cardiovascular risk summary variable, no insurance, receipt of Medicaid, not getting needed care, and time since last examination. Statistically, we did this by adding gender by EI and gender by FC interaction terms into analyses, then examining the significance of the interaction and performing stratified analyses where indicated. Finally, we performed sensitivity analyses dropping females who had ever been pregnant from the hypertension and diabetes analyses, given the difference in wording between studies for these questions. For all analyses, we treated ES as the reference group.
Results
Results of univariate analyses indicated that all covariates were associated with group status. They also revealed a consistent pattern of graded increase in risk across cohorts for most outcomes, progressing from ES to EI to FC groups (Table 2). This pattern held after adjustment for covariates. For example, the EI group had a significantly higher odds of reporting poor or fair general health than the ES group (odds ratio [OR] 1.53; 95% confidence interval [CI], 1.19 to 1.97); however, the FC group reported even higher odds of this outcome (OR 2.30; 95% CI, 1.84 to 2.89). The average BMIs in the EI and FC groups were also higher than in the ES group, with the FC group having the highest BMI (β = 0.51; 95% CI, –0.09 to 1.10 for EI and β = 0.90; 95% CI, 0.32 to 1.49 for FC; relationship significant for FC only).
TABLE 2.
Descriptives and Univariate Relationships Between Covariates/Outcomes and Cohort
| Variable | Add Health ES (Total N = 1461) | Add Health EI (Total N = 456) | Midwest FC (Total N = 596) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Proportion/Mean | SD | N | Proportion/Mean | SD | N | Proportion/Mean | SD | |
| Covariates | |||||||||
| Female, % | 1461 | 55 | 456 | 68*** | 596 | 56 | |||
| Race, % | 1459 | 456 | 593 | ||||||
| White | 67 | 59** | 32*** | ||||||
| Black | 18 | 27*** | 57*** | ||||||
| Other race | 10 | 9 | 2*** | ||||||
| Mixed | 5 | 6 | 9*** | ||||||
| Hispanic, % | 1451 | 10 | 453 | 14* | 593 | 8† | |||
| Average age | |||||||||
| Age at T1 (mean and SD) | 1461 | 19.8 | 0.5 | 456 | 19.9** | 0.5 | 596 | 17.8*** | 0.4 |
| Age at T2 (mean and SD) | 1461 | 26.3 | 0.4 | 456 | 26.3† | 0.4 | 596 | 26.1*** | 0.3 |
| High school diploma by T2, % | 1461 | 95 | 456 | 87*** | 593 | 82*** | |||
| Any economic insecurity at T2, % | 1461 | 16 | 456 | 35*** | 596 | 42*** | |||
| Ever pregnant by T2, %a | 810 | 29 | 309 | 51*** | 327 | 79*** | |||
| Outcomes | |||||||||
| General health | |||||||||
| Fair or poor general health at T1 (%) | 1461 | 4 | 456 | 8*** | 595 | 14*** | |||
| Fair/poor general health at T2, % | 1461 | 7 | 456 | 12*** | 596 | 18*** | |||
| Average BMI | |||||||||
| BMI at T1 (mean and SD) | 1433 | 24.6 | 5.1 | 445 | 25.3* | 5.7 | 588 | 25.5** | 5.6 |
| BMI at T2 (mean and SD) | 1438 | 27.3 | 6.3 | 445 | 28.4** | 6.6 | 595 | 29.0*** | 7.0 |
| Dyslipidemia at T2, % | 1461 | 0.5 | 456 | 1.1 | 596 | 0.7 | |||
| Hypertension at T2, % | 1461 | 1.0 | 456 | 2.0† | 596 | 4.2*** | |||
| Diabetes at T2, % | 1461 | 0.2 | 456 | 0.9† | 595 | 0.8† | |||
| Smoker at T2, % | 1461 | 18 | 456 | 30*** | 595 | 40*** | |||
| Seizures at T2, % | 1461 | 0.0 | 456 | 1.1b | 596 | 1.5b | |||
| ADHD at T2, % | 1461 | 0.3 | 456 | 0.2 | 596 | 6.2*** | |||
| Asthma at T2, % | 1461 | 1.2 | 456 | 3.1** | 596 | 5.5*** | |||
| Any cardiovascular risk factor at T2, % | 1438 | 21 | 445 | 35*** | 594 | 47*** | |||
| Any other chronic health condition at T2, % | 1438 | 1.2 | 445 | 3.5** | 594 | 8.7*** | |||
| Nonprivate insurance at T2, % | 1458 | 456 | 591 | ||||||
| No insurance | 19 | 30*** | 41*** | ||||||
| Medicaid | 5 | 20*** | 41*** | ||||||
| Didn’t get needed care in past year at T2, % | 1461 | 24 | 456 | 32*** | 596 | 13*** | |||
| Last examination >1 y ago at T2, % | 1454 | 61 | 454 | 63 | 595 | 65 | |||
T1, time 1; T2, time 2.
Analysis includes females only.
No significance levels because there were 0 with outcome in Add Health ES (reference) group.
P < .10. * P < .05. ** P < .01. *** P < .001.
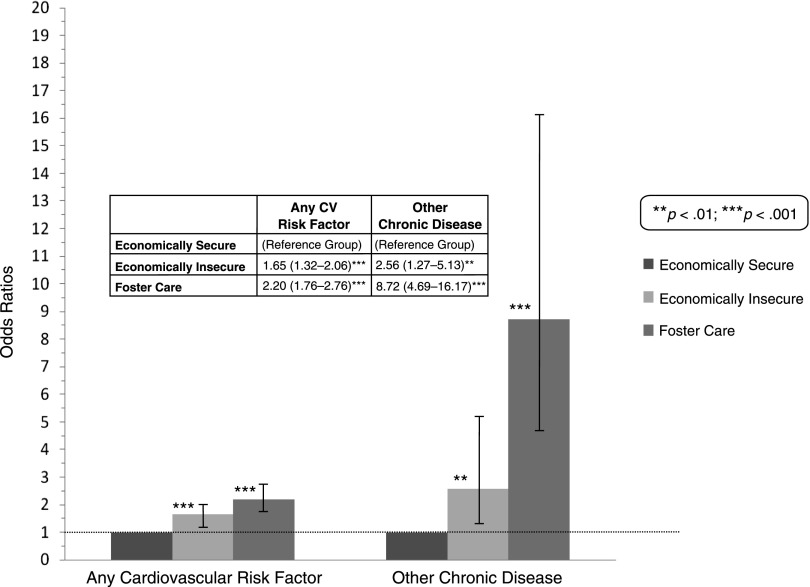
Figure 1 contains results of the multivariate analyses of all time 2–only individual health conditions, excluding seizures because there were no youth with seizures in the ES group. Figure 2 contains results of our 2 summary variables. There were 2 notable exceptions to the pattern of graded increased risk from ES to EI to FC; the EI group was less likely to report ADHD than the ES group, but the FC group was by far the most likely to report this outcome, and no differences were found by group for dyslipidemia. When we compared the FC and ES groups most ORs were significant; for diabetes the relationship was nonsignificant but followed a similar trend (P = .06). In contrast, the EI group had only 2 outcomes for which odds were significant when compared with the ES group (asthma and smoker; OR 2.32; 95% CI, 1.11 to 4.83 and OR 1.81; 95% CI, 1.40 to 2.34, respectively).
FIGURE 1.
Logistic regressions of individual dichotomous outcomes at time 2, by cohort.
FIGURE 2.
Logistic regressions of summary outcomes at time 2, by cohort.
With respect to insurance status, the EI and FC groups were once again more likely to report having no insurance (OR 1.76; 95% CI, 1.36 to 2.27 and OR 2.21; 95% CI, 1.73 to 2.82, respectively) or having Medicaid (OR 3.56; 95% CI, 2.53 to 5.01 and OR 13.16; 95% CI, 9.42 to 18.40, respectively). Although the EI group was also significantly more likely to report not getting needed care in the past year at time 2 (OR 1.32; 95% CI, 1.03 to 1.67), the FC group was less likely to report this outcome (OR 0.36; 95% CI, 0.27 to 0.49) than the ES group. Neither group was significantly different in terms of the time since their last health examination compared with the ES reference group.
The relationship between group status and outcomes did not vary by time for our 2 multiple-time-point outcomes (BMI and general health). With respect to gender moderation, interaction terms for the gender by FC analyses were significant for all outcomes evaluated except time since last examination. Specifically, females in the FC group had a higher BMI than those in the ES group, but FC males had a lower BMI than their ES counterparts (β = 1.73; 95% CI, 0.86 to 2.61 for females and β = –0.26; 95% CI, –1.07 to 0.55 for males; P value of interaction term <.001). In contrast, both males and females in the FC group had a higher odds of having ≥1 cardiovascular risk factor and lower odds of not receiving needed care compared with their ES counterparts, but these gaps were significantly wider for females than males (P = .004 and .041 for cardiovascular risk factor and not receiving needed care interaction terms, respectively). Both genders were more likely to report having no insurance or receiving Medicaid if they were in the FC group; however, males in the FC group had higher ORs than females for the no-insurance outcomes (P < .001), and the reverse was true for odds of receiving Medicaid (P = .001). Only 1 gender by EI interaction was significant; for the Medicaid outcome, the effect of being in the EI group was larger for females than for males (P = .049). Sensitivity analyses revealed trends similar to the main analyses in all instances.
Discussion
Results are consistent with the chronic stress literature and previous retrospective work evaluating the adult health outcomes of former foster youth, which suggests that exposure to economic insecurity and the other chronic stressors associated with having been in foster care have the potential to influence young adult health outcomes in a cumulative fashion.9–12,16 Many health conditions have their origins in the childhood and teenage years; thus findings are relevant not only for public and private agencies serving former foster youth but also for those serving youth currently in foster care.
Our access indicators suggest that former foster youth do not perceive a lack of needed medical care during young adulthood; previous analyses reveal that foster youth also perceive similar or higher rates of access to medical care compared with general population youth while they are still in care.1 However, it is important to note that access to “needed care” does not equate to access to high-quality, evidence-based care. Medical care for foster youth is often discontinuous, making it difficult for trusting patient–provider relationships to form and evidence-based treatments to be delivered.28,29 Although little research has evaluated continuity and quality of care among emancipated foster youth, there is little reason to believe these problems improve as foster youth become young adults facing homelessness, unemployment, and other issues known to affect quality of health care.17–22,30,31
Future exploration is merited to determine care-related contributors to this group’s disproportionate disease burden. Quantitative and qualitative research should be conducted to better delineate the specific types of care these youth receive (and lack), the continuity and quality of provider relationships they experience, and the degree to which they receive evidence-based care for chronic medical conditions during adolescence and the transition to adulthood. Current and former foster youth may benefit from a level of preventive health care beyond that which is recommended for general population youth,32,33 including strategies to promote access to state-of-the-art interventions targeting modifiable cardiovascular risk factors such as diet, exercise, and smoking cessation. Training and resources for caseworkers, foster parents, and group home staff emphasizing the importance of continuity and quality of health care provider relationships in addition to timely access may also be beneficial. Previous research on chronic disease management in adult populations with the types of maladaptive relationship styles resultant from early adversity suggests that policies and programs may need to be tailored to the unique life experiences of foster youth to have maximal effect, for example, including individualized strategies to promote the formation of trusting relationships with health care and allied providers.34 Support to maintain these relationships across placement changes may also be beneficial. Given the moderating effect of gender in our analyses of BMI and other cardiovascular risk factors, young women formerly in foster care should be a particular focus in policy and intervention work, although male youth are also likely to benefit.
Finally, the needs of former foster youth should be considered when states are contemplating participation in Medicaid expansion and other policies to extend insurance or foster care for this vulnerable population. Our previous work suggests that the majority of young women emancipating from foster care are likely to be eligible for Medicaid under either the low-income provision or the foster youth–specific provision of the ACA in participating states.20 Given the similar poverty rates and lower insurance rates for male former foster youth, these policies have the potential to affect young men formerly in foster care in a similar if not more profound manner.17,20
This study has several limitations. First, outcomes were assessed by using slightly different questions in the 2 studies, which could have led to differences in classification across cohorts. In particular, the language excluding pregnancy-related hypertension and diabetes in the Add Health cohorts could have artificially inflated ORs because these conditions were not specifically excluded in the Midwest Study. However, sensitivity analyses removing young women ever pregnant from all 3 cohorts and thus removing this potential bias demonstrated similar results. Second, although we adjusted for potential demographic and socioeconomic confounding factors, survey questions cannot completely assess social determinants of health. Thus, some degree of residual confounding is likely. Third, some outcomes were rare, and we had suboptimal power to detect significant differences in these variables (eg, seizures). We were also limited to a subset of health outcomes measured in both studies; future research should explore a wider variety of health problems including mental health and substance-related disorders, which are among the most common problems experienced by young adults.35 Finally, variables were self-report. This limitation may have resulted in some misclassification of outcomes, biasing point estimates toward the null.
Conclusions
Young adult former foster youth appear to have a higher risk of multiple chronic health conditions, above and beyond that which is attributable to economic insecurity. Our data support the Institute of Medicine assertion that foster youth should be prioritized when interventions to reduce health disparities in young adulthood are evaluated and implemented,6 and when state and federal governing bodies are considering policies to extend Medicaid or foster care.
Acknowledgments
The Midwest Evaluation of the Adult Functioning of Former Foster Youth is a collaborative research effort with cooperation and funding from the Illinois Department of Children and Family Services, the Wisconsin Department of Health and Family Services, and the Iowa Department of Human Services. We thank these departments for their support. We also thank all members of the research team at Chapin Hall Center for Children, the University of Wisconsin Survey Center in Madison, Wisconsin, and the people who participated in both parent studies.
Glossary
- ACA
Affordable Care Act
- Add Health
National Longitudinal Study of Adolescent Health
- ADHD
attention-deficit/hyperactivity disorder
- CI
confidence interval
- EI
economically insecure
- ES
economically secure
- FC
foster care
- Midwest Study
Midwest Evaluation of the Adult Functioning of Former Foster Youth
- OR
odds ratio
Footnotes
Dr Ahrens conceptualized and designed the current study, performed analyses, and drafted the initial manuscript; Dr Garrison assisted with conceptualization and design of the current study, provided feedback on analyses and statistical methods and coding, and critically reviewed the manuscript; Dr Courtney conceptualized, designed, and was principal investigator of one of the parent studies, assisted with conceptualization and design of the current study, provided feedback on analyses, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by NIH grant 1K23MH09098. One of the parent studies (the Midwest Study) was also supported by the WT Grant Foundation. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Courtney ME, Terao S, Bost N. Midwest Evaluation of the Adult Functioning of Former Foster Youth: conditions of youth preparing to leave state care. 2004. Available at: www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth. Accessed April 15, 2014
- 2.Flaherty EG, Weiss H. Medical evaluation of abused and neglected children. Am J Dis Child. 1990;144(3):330–334 [DOI] [PubMed] [Google Scholar]
- 3.Farruggia SP, Sorkin DH. Health risks for older US adolescents in foster care: the significance of important others’ health behaviours on youths’ health and health behaviours. Child Care Health Dev. 2009;35(3):340–348 [DOI] [PubMed] [Google Scholar]
- 4.Hansen RL, Mawjee FL, Barton K, Metcalf MB, Joye NR. Comparing the health status of low-income children in and out of foster care. Child Welfare. 2004;83(4):367–380 [PubMed] [Google Scholar]
- 5.Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics. 2000;106(suppl 4):909–918 [PubMed] [Google Scholar]
- 6.O’Connell ME, Boat T, Warner KE, edsNational Research Council and Institute of Medicine Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: The National Academies Press; 2009 [PubMed] [Google Scholar]
- 7.Barth RP, Wildfire J, Green RL. Placement into foster care and the interplay of urbanicity, child behavior problems, and poverty. Am J Orthopsychiatry. 2006;76(3):358–366 [DOI] [PubMed] [Google Scholar]
- 8.McGuinness TM, Schneider K. Poverty, child maltreatment, and foster care. J Am Psychiatr Nurses Assoc. 2007;13(5):296–303 [Google Scholar]
- 9.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):174–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003;37(3):268–277 [DOI] [PubMed] [Google Scholar]
- 11.Lengua LJ, Honorado E, Bush NR. Contextual risk and parenting as predictors of effortful control and social competence in preschool children. J Appl Dev Psychol. 2007;28(1):40–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turner RJ, Lloyd DA. Lifetime traumas and mental health: the significance of cumulative adversity. J Health Soc Behav. 1995;36(4):360–376 [PubMed] [Google Scholar]
- 13.Kim P, Evans GW, Angstadt M, et al. Effects of childhood poverty and chronic stress on emotion regulatory brain function in adulthood. Proc Natl Acad Sci USA. 2013;110(46):18442–18447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuo AA, Etzel RA, Chilton LA, Watson C, Gorski PA. Primary care pediatrics and public health: meeting the needs of today’s children. Am J Public Health. 2012;102(12):e17–e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spencer N, Thanh TM, Louise S. Low income/socio-economic status in early childhood and physical health in later childhood/adolescence: a systematic review. Matern Child Health J. 2013;17(3):424–431 [DOI] [PubMed] [Google Scholar]
- 16.Zlotnick C, Tam TW, Soman LA. Life course outcomes on mental and physical health: the impact of foster care on adulthood. Am J Public Health. 2012;102(3):534–540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Courtney ME, Dworsky A. Early outcomes for young adults transitioning from out-of-home care in the USA. Child Fam Soc Work. 2006;11(3):209–219 [Google Scholar]
- 18.Courtney ME, Dworsky A, Lee JS, Raap M. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 23 and 24. Chicago, IL: Chapin Hall at the University of Chicago; 2009. Available at: www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth. Accessed April 15, 2014 [Google Scholar]
- 19.Courtney ME, Dworsky A, Ruth GR, Havlicek J, Perez A, Keller TE. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 21. 2007. Available at: www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth. Accessed April 15, 2014
- 20.Dworsky A, Courtney ME. Homelessness and the transition from foster care to adulthood. Child Welfare. 2009;88(4):23–56 [PubMed] [Google Scholar]
- 21.Pecora P, Williams J, Kessler R, et al. Assessing the effects of foster care: early results from the Casey National Alumni Study. 2003. Available at: www.casey.org/Resources/Publications/AssessingEffectsOfFosterCare.htm. Accessed April 15, 2014
- 22.Dworsky A, Napolitano L, Courtney M. Homelessness during the transition from foster care to adulthood. Am J Public Health. 2013;103(suppl 2):S318–S323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahrens KR, McCarty C, Simoni J, Dworsky A, Courtney ME. Psychosocial pathways to sexually transmitted infection risk among youth transitioning out of foster care: evidence from a longitudinal cohort study. J Adolesc Health. 2013;53(4):478–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dworsky A, Ahrens K, Courtney M. Health insurance coverage and use of family planning services among current and former foster youth: implications of the health care reform law. J Health Polit Policy Law. 2013;38(2):421–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howell B. Supreme Court upholds PPACA. ABA Health eSource. 2012. Available at: www.americanbar.org/newsletter/publications/aba_health_esource_home/aba_health_law_esource_0712_howell.html. Accessed April 15, 2014
- 26.GovTrack.us. H.R. 6893–110th Congress (2008): Fostering Connections to Success and Increasing Adoptions Act of 2008. Available at: www.govtrack.us/congress/bills/110/hr6893. Accessed April 15, 2014
- 27.Harris K. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002; Wave IV, 2007–2009 [machine-readable data file and documentation] Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill; 2009 [Google Scholar]
- 28.DiGiuseppe DL, Christakis DA. Continuity of care for children in foster care. Pediatrics. 2003;111(3). Available at: www.pediatrics.org/cgi/content/full/111/3/e208 [DOI] [PubMed] [Google Scholar]
- 29.Rubin DM, Alessandrini EA, Feudtner C, Localio AR, Hadley T. Placement changes and emergency department visits in the first year of foster care. Pediatrics 2004;114(3). Available at: www.pediatrics.org/cgi/content/full/114/3/e354 [DOI] [PubMed]
- 30.Nickasch B, Marnocha SK. Healthcare experiences of the homeless. J Am Acad Nurse Pract. 2009;21(1):39–46 [DOI] [PubMed] [Google Scholar]
- 31.Lebrun-Harris LA, Baggett TP, Jenkins DM, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res. 2013;48(3):992–1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ozer EM, Urquhart JT, Brindis CD, Park MJ, Irwin CE., Jr Young adult preventive health care guidelines: there but can’t be found. Arch Pediatr Adolesc Med. 2012;166(3):240–247 [DOI] [PubMed] [Google Scholar]
- 33.Hagan J, Shaw JS, Duncan PM, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed Elk Grove Village, IL: American Academy of Pediatrics; 2008 [Google Scholar]
- 34.Ciechanowski PS, Russo JE, Katon WJ, et al. The association of patient relationship style and outcomes in collaborative care treatment for depression in patients with diabetes. Med Care. 2006;44(3):283–291 [DOI] [PubMed] [Google Scholar]
- 35.Healthy People 2020: adolescent health. Available at: www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=2. Accessed June 3, 2014