Abstract
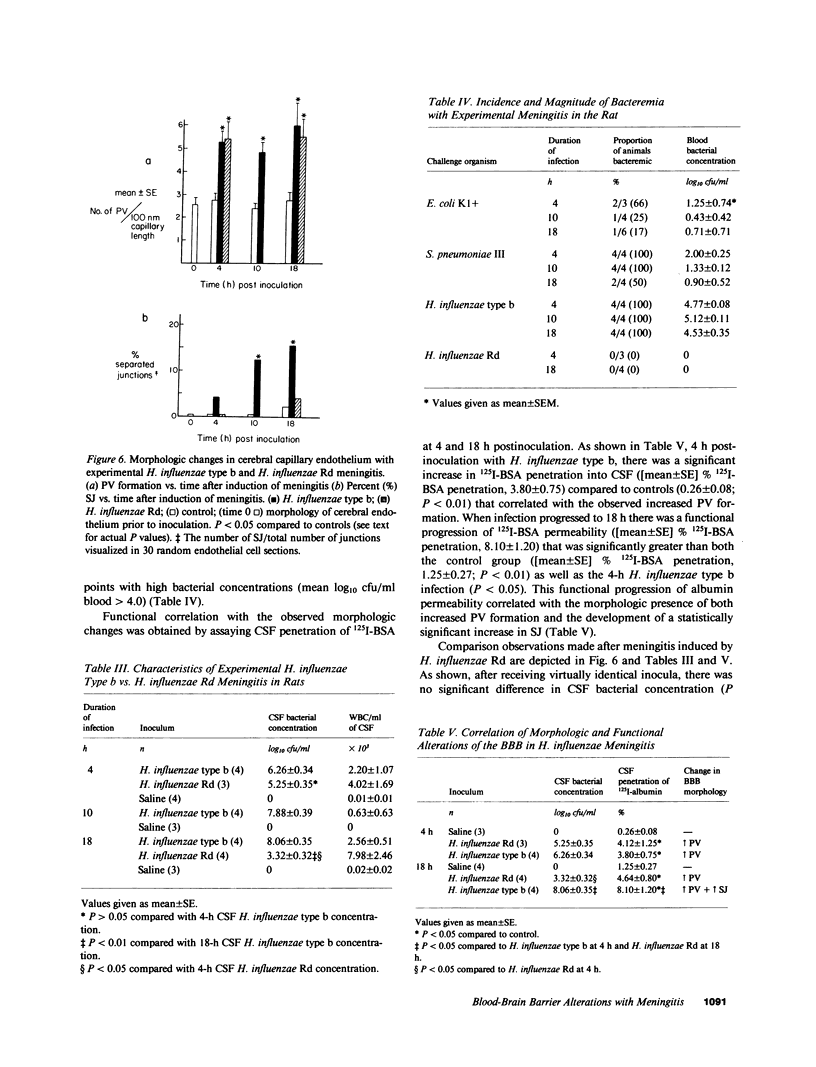
The cerebral capillary endothelium is unique and functions as an effective blood-brain barrier (BBB) owing to its intercellular tight junctions and rare pinocytotic vesicles. To assess how bacterial meningitis alters the BBB, rats were inoculated intracisternally with three encapsulated meningeal pathogens (Escherichia coli K1+, Streptococcus pneumoniae type III, Haemophilus influenzae type b) and an unencapsulated mutant strain (H. influenzae Rd). After defined infection durations, the morphologic alterations of the cerebral capillary endothelium were quantitatively assessed by transmission electron microscopy. Results revealed a significant increase in pinocytotic vesicle formation (P less than 0.001) early after meningitis induction (4 h) that was sustained with longer infection durations (10 h, 18 h) for all encapsulated strains tested. In addition, there was a progressive increase in completely separated intercellular junctions with increasing infection duration, (P less than 0.05). 4 h after induction of meningitis with H. influenzae Rd, cerebrospinal fluid (CSF) bacterial concentrations, cerebral capillary morphologic changes, and functional BBB permeability to circulating 125I-albumin were similar to those observed with H. influenzae type b. However, prolonging the H. influenzae Rd infection to 18 h allowed for CSF clearance of the organism, thereby precluding the significant increase in separated junctions or progression of functional BBB permeability seen with the encapsulated H. influenzae type b. These data suggest a uniform morphologic explanation for altered BBB permeability in meningitis with a reproducible temporal sequence. Encapsulation does not appear essential for BBB injury, but may facilitate its progression by allowing the organism to evade host clearance.
Full text
PDF










Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alon U., Naveh Y., Gardos M., Friedman A. Neurological sequelae of septic meningitis. A follow-up study of 65 children. Isr J Med Sci. 1979 Jun;15(6):512–517. [PubMed] [Google Scholar]
- Betz A. L., Csejtey J., Goldstein G. W. Hexose transport and phosphorylation by capillaries isolated from rat brain. Am J Physiol. 1979 Jan;236(1):C96–102. doi: 10.1152/ajpcell.1979.236.1.C96. [DOI] [PubMed] [Google Scholar]
- Betz A. L., Firth J. A., Goldstein G. W. Polarity of the blood-brain barrier: distribution of enzymes between the luminal and antiluminal membranes of brain capillary endothelial cells. Brain Res. 1980 Jun 16;192(1):17–28. doi: 10.1016/0006-8993(80)91004-5. [DOI] [PubMed] [Google Scholar]
- Betz A. L., Goldstein G. W. Polarity of the blood-brain barrier: neutral amino acid transport into isolated brain capillaries. Science. 1978 Oct 13;202(4364):225–227. doi: 10.1126/science.211586. [DOI] [PubMed] [Google Scholar]
- Bradbury M. W. The structure and function of the blood-brain barrier. Fed Proc. 1984 Feb;43(2):186–190. [PubMed] [Google Scholar]
- Brightman M. W., Reese T. S. Junctions between intimately apposed cell membranes in the vertebrate brain. J Cell Biol. 1969 Mar;40(3):648–677. doi: 10.1083/jcb.40.3.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claude P., Goodenough D. A. Fracture faces of zonulae occludentes from "tight" and "leaky" epithelia. J Cell Biol. 1973 Aug;58(2):390–400. doi: 10.1083/jcb.58.2.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper A. J., Beaty H. N., Oppenheimer S. I., Goodner C. J., Petersdorf R. G. Studies on the pathogenesis of meningitis. VII. Glucose transport and spinal fluid production in experimental pneumococcal meningitis. J Lab Clin Med. 1968 Mar;71(3):473–483. [PubMed] [Google Scholar]
- Crone C., Olesen S. P. Electrical resistance of brain microvascular endothelium. Brain Res. 1982 Jun 3;241(1):49–55. doi: 10.1016/0006-8993(82)91227-6. [DOI] [PubMed] [Google Scholar]
- Dodge P. R., Davis H., Feigin R. D., Holmes S. J., Kaplan S. L., Jubelirer D. P., Stechenberg B. W., Hirsh S. K. Prospective evaluation of hearing impairment as a sequela of acute bacterial meningitis. N Engl J Med. 1984 Oct 4;311(14):869–874. doi: 10.1056/NEJM198410043111401. [DOI] [PubMed] [Google Scholar]
- Estrada C., Hamel E., Krause D. N. Biochemical evidence for cholinergic innervation of intracerebral blood vessels. Brain Res. 1983 May 5;266(2):261–270. doi: 10.1016/0006-8993(83)90657-1. [DOI] [PubMed] [Google Scholar]
- Goldstein G. W., Betz A. L. Recent advances in understanding brain capillary function. Ann Neurol. 1983 Oct;14(4):389–395. doi: 10.1002/ana.410140402. [DOI] [PubMed] [Google Scholar]
- Graham R. C., Jr, Karnovsky M. J. The early stages of absorption of injected horseradish peroxidase in the proximal tubules of mouse kidney: ultrastructural cytochemistry by a new technique. J Histochem Cytochem. 1966 Apr;14(4):291–302. doi: 10.1177/14.4.291. [DOI] [PubMed] [Google Scholar]
- Herbst T. J., Raichle M. E., Ferrendelli J. A. beta-Adrenergic regulation of adenosine 3',5'-monophosphate concentration in brain microvessels. Science. 1979 Apr 20;204(4390):330–332. doi: 10.1126/science.34879. [DOI] [PubMed] [Google Scholar]
- Long J. B., Holaday J. W. Blood-brain barrier: endogenous modulation by adrenal-cortical function. Science. 1985 Mar 29;227(4694):1580–1583. doi: 10.1126/science.3975627. [DOI] [PubMed] [Google Scholar]
- Oldendorf W. H., Brown W. J. Greater number of capillary endothelial cell mitochondria in brain than in muscle. Proc Soc Exp Biol Med. 1975 Jul;149(3):736–738. doi: 10.3181/00379727-149-38889. [DOI] [PubMed] [Google Scholar]
- Pardridge W. M. Neuropeptides and the blood-brain barrier. Annu Rev Physiol. 1983;45:73–82. doi: 10.1146/annurev.ph.45.030183.000445. [DOI] [PubMed] [Google Scholar]
- Petito C. K. Early and late mechanisms of increased vascular permeability following experimental cerebral infarction. J Neuropathol Exp Neurol. 1979 May;38(3):222–234. doi: 10.1097/00005072-197905000-00003. [DOI] [PubMed] [Google Scholar]
- Petito C. K., Schaefer J. A., Plum F. Ultrastructural characteristics of the brain and blood-brain barrier in experimental seizures. Brain Res. 1977 May 27;127(2):251–267. doi: 10.1016/0006-8993(77)90539-x. [DOI] [PubMed] [Google Scholar]
- Prockop L. D., Fishman R. A. Experimental pneumococcal meningitis. Permeability changes influencing the concentration of sugars and macromolecules in cerebrospinal fluid. Arch Neurol. 1968 Nov;19(5):449–463. doi: 10.1001/archneur.1968.00480050019001. [DOI] [PubMed] [Google Scholar]
- Reese T. S., Karnovsky M. J. Fine structural localization of a blood-brain barrier to exogenous peroxidase. J Cell Biol. 1967 Jul;34(1):207–217. doi: 10.1083/jcb.34.1.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheld W. M., Dacey R. G., Winn H. R., Welsh J. E., Jane J. A., Sande M. A. Cerebrospinal fluid outflow resistance in rabbits with experimental meningitis. Alterations with penicillin and methylprednisolone. J Clin Invest. 1980 Aug;66(2):243–253. doi: 10.1172/JCI109850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheld W. M., Sande M. A. Bactericidal versus bacteriostatic antibiotic therapy of experimental pneumococcal meningitis in rabbits. J Clin Invest. 1983 Mar;71(3):411–419. doi: 10.1172/JCI110785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simionescu N., Simionescu M., Palade G. E. Structural basis of permeability in sequential segments of the microvasculature of the diaphragm. II. Pathways followed by microperoxidase across the endothelium. Microvasc Res. 1978 Jan;15(1):17–36. doi: 10.1016/0026-2862(78)90002-x. [DOI] [PubMed] [Google Scholar]
- Spector R., Lorenzo A. V. Inhibition of penicillin transport from the cerebrospinal fluid after intracisternal inoculation of bacteria. J Clin Invest. 1974 Aug;54(2):316–325. doi: 10.1172/JCI107767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz M. N. Bacterial meningitis: more involved than just the meninges. N Engl J Med. 1984 Oct 4;311(14):912–914. doi: 10.1056/NEJM198410043111409. [DOI] [PubMed] [Google Scholar]
- Westergaard E. The blood-brain barrier to horseradish peroxidase under normal and experimental conditions. Acta Neuropathol. 1977 Aug 31;39(3):181–187. doi: 10.1007/BF00691695. [DOI] [PubMed] [Google Scholar]
- Williams S. K., Wagner R. C. Regulation of micropinocytosis in capillary endothelium by multivalent cations. Microvasc Res. 1981 Mar;21(2):175–182. doi: 10.1016/0026-2862(81)90030-3. [DOI] [PubMed] [Google Scholar]
- Zwahlen A., Winkelstein J. A., Moxon E. R. Participation of complement in host defense against capsule-deficient Haemophilus influenzae. Infect Immun. 1983 Nov;42(2):708–715. doi: 10.1128/iai.42.2.708-715.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwahlen A., Winkelstein J. A., Moxon E. R. Surface determinants of Haemophilus influenzae pathogenicity: comparative virulence of capsular transformants in normal and complement-depleted rats. J Infect Dis. 1983 Sep;148(3):385–394. doi: 10.1093/infdis/148.3.385. [DOI] [PubMed] [Google Scholar]








