Abstract
We conducted a study designed to evaluate whether the benefits of intentional weight loss exceed the potential risks in a group of community-dwelling, obese, older adults who were at increased risk for cardiometabolic disease. The CROSSROADS trial used a prospective randomized controlled design to compare the effects of changes in diet composition alone or combined with weight loss with an exercise only control intervention on body composition and adipose tissue deposition (Specific Aim #1: To compare the effects of changes in diet composition alone or combined with weight loss with an exercise only control intervention on body composition, namely visceral adipose tissue (VAT)), cardiometabolic disease risk (Specific Aim #2: To compare the effects of a change in diet composition alone or combined with weight loss with an exercise only control intervention on cardiometabolic disease risk), functional status and quality of life (Specific Aim #3: To compare the effects of a change in diet composition alone or combined with weight loss with an exercise only control intervention on functional status and quality of life). Participants were randomly assigned to one of three groups: Exercise Only (Control) Intervention, Exercise + Diet Quality + Weight Maintenance Intervention, or Exercise + Diet Quality + Weight Loss Intervention. CROSSROADS utilized a lifestyle intervention approach consisting of exercise, dietary, and behavioral components. The development and implementation of the CROSSROADS protocol, including a description of the methodology, detailing specific elements of the lifestyle intervention, assurances of treatment fidelity, and participant retention; outcome measures and adverse event monitoring; as well as unique data management features of the trial results, are presented in this article.
INTRODUCTION
The CROSSROADs study was designed to evaluate whether the benefits of intentional weight loss exceed the potential risks in a group of community-dwelling, obese, older adults who were at increased risk for cardiometabolic disease.
Older adults represent the fastest growing segment of the United States (US) population, as well as the entire global population in both developed and developing countries. Among older adults, both the absolute number of persons who are obese and the percentage of persons who are obese (defined as body mass index ≥ 30 kg/m2) is either increasing or remaining stable at high rates (1, 2, 3). For example, more than one-third of US adults aged 65 and older (representing approximately 13 million people) were obese between the years 2007–2010 (4). The increase in obesity prevalence among older adults is especially concerning because of its adverse effects on functional status and quality of life, which may lead to decreased mobility and increased frailty and pain (5, 6, 7). The increase in obesity prevalence among older adults is additionally concerning because of its association with a higher risk of development or exacerbation of chronic diseases, including hypertension, diabetes, hyperlipidemia, osteoarthritis, and heart disease. Furthermore, the medical costs attributable to obesity are high, and are higher for older adults compared with younger populations (8). Thus, obesity among older adults represents a major public health challenge (9).
A straightforward initial response to this potential threat is to recommend weight loss programs for those obese older adults—anticipating corresponding decreases in disease risk with achieved weight loss. While intentional weight loss among older adults has been associated with significant improvements in cardiometabolic function, physical function, and quality of life, weight loss also may be associated with potential harm in older adults (7, 9). At the time this study began, there were no reports in the literature of randomized trials of voluntary, diet-induced weight loss interventions in older adults over age 65 that carefully assessed whether weight loss can improve cardiometabolic risk factors, physical function, and quality of life without causing harm (7, 10, 11, 12). Studies that evaluated whether the benefits of intentional weight loss using lifestyle interventions and moderate calorie restriction among older adults outweigh any risks associated with weight loss were limited, and those that existed did not study a full range of cardiometabolic risk factors, physical function, and quality of life outcomes likely to be most pertinent to evaluating the clinical appropriateness of recommending weight loss in an older adult population.
A key part of the controversy raised at the time this study began, that still remains today, stems from epidemiologic studies that suggest that weight loss, normal weight, or a pattern of weight instability are associated with increased mortality in older adults (13, 14, 15). Some of the mortality risk associated with weight loss may be a function of the effects that reduced calories has on body composition in older adults. Weight loss induced through caloric restriction alters body composition not only by decreasing fat mass, but also by also decreasing lean mass and bone mineral density (BMD) (7, 9). Reduction in lean mass and BMD occurs normally with age; and these may be negatively altered in unanticipated ways with intentional weight loss (7). Despite several randomized controlled trials having reported data since our study began, the extent to which intentional weight loss contributes to decreases in physical function and strength and/or elevated rates of osteoporosis and hip fractures remain uncertain and the controversies surrounding recommending weight loss for older adults persist (9, 16, 17, 18).
Contributing to the controversy is that studies in which BMI and DXA (dual energy x-ray absorptiometry) are used to measure total adiposity may only provide a partial picture of the true interactions between fat mass and disease risk/function in older adults because the total increase in adiposity among older adults is significantly underestimated due to age-related changes in body composition and fat distribution (7, 19). In older adults, BMI has a lower correlation with total body fat because there is an age-related shift in the amount of lean mass relative to fat mass, resulting in a higher percent of body fat for the same BMI (20). While DXA can measure total body fat, it cannot measure separately visceral and subcutaneous adipose tissue in the abdomen.
Because of age-related changes in body fat distribution, much of the overall disease risk and functional decline in obese older adults may not be a direct result of total adiposity, but rather, visceral adipose tissue (VAT), a component of total adipose tissue. VAT has been shown to increase with age even when there is a decline in overall body weight (10). Increased VAT is linked to insulin resistance and is responsible for a pro-inflammatory state (21) that is believed to not only have harmful effects on skeletal muscle in older adults (22, 23, 24, 25, 26), but also increases markers for cardiometabolic disease risk (26, 27). Despite the observed relationships between VAT and disease risk, we do not fully understand how changes in VAT with intentional dietary change and calorie restriction affect cardiometabolic and functional health risk in older adults.
While our study was ongoing, Dennis Villareal and his colleagues, as well as a few others, reported that weight loss in older adults could be achieved through lifestyle interventions over a one-year period (16, 17, 18, 28). Not unexpectedly, weight loss was associated with a loss of both lean body mass and BMD. However, improvements were observed in muscle quality and physical function. Improvements were also observed for inflammatory cytokines, metabolic markers, quality of life, and cognition (29). While these results are informative and suggest that voluntary weight loss is beneficial for older adults, there were some key aspects of weight loss outcomes that remain largely unexplored including limited information on changes in VAT with a range of lifestyle interventions (30). Furthermore, the independent and additive effects of exercise, change in diet, and weight loss on various mechanistic pathways (e.g., metabolic) have not been fully explicated.
Ideally, older adults using a prescribed dietary intervention combined with exercise would be able to preferentially reduce visceral fat mass, while minimizing loss of lean mass and bone, to obtain maximum improvements in both cardiometabolic and functional health risk. The CROSSROADS study is the first to address all of these questions directly, using a three-arm, randomized controlled trial among obese, community-dwelling adults aged 65 and older at-risk for cardiometabolic disease. The development and implementation of the CROSSROADS protocol, including a description of the methodology, detailing specific elements of the lifestyle intervention, assurances of treatment fidelity, and participant retention; outcome measures and adverse event monitoring; as well as unique data management features of the trial results, are presented in this article.
METHODOLOGY
A standardized protocol was employed to implement the CROSSROADs Study that was aligned with the Consolidated Standards of Reporting Trials (CONSORT) (31). The following sections describe key elements relevant for a comprehensive understanding of delivery of this intervention (Figure 1).
Figure 1.
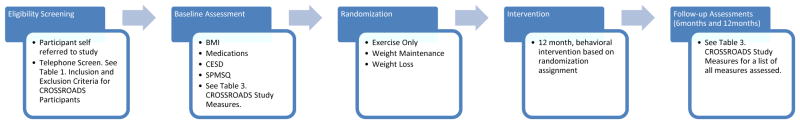
Flow of CROSSROADs study relevant to delivery and assessment of the intervention.
Eligibility Screening
CROSSROADS recruited participants from the greater Birmingham, Alabama, metropolitan area using various forms of advertisement and word-of-mouth recruitment techniques. The study recruited potential volunteers who were at least 65 years old at the time of the initial telephone screening. In addition to the requirement to be obese (body mass index of 30–40 kg/m2), participants had to be taking at least one medication for control of lipids, blood pressure, or blood glucose (Table 1). By setting these eligibility criteria, volunteers for CROSSROADS were considered to have co-morbid conditions that would likely be negatively affected by their weight status, and thus at higher risk medically with greater potential health benefit to be gained by weight reduction. An upper limit of body mass index (BMI) of 40 kg/m2 was chosen because a BMI greater than 40 kg/m2 represents severe obesity, which is considered a different class of disease (32). Key exclusion criteria included major factors that might confound lifestyle-related changes in body weight either intentionally (e.g., use of pharmacotherapy for weight loss) or unintentionally (e.g., ongoing treatment for cancer, uncontrolled depression). The investigative team also excluded participants with limitations in their ability to engage in the prescribed interventions at baseline during a run-in phase (i.e., through keeping logs of food intake and exercise activity that would be necessary to keep throughout the study). This was important because the assessment of safety and engagement depended on all participants having a similar capacity to be actively involved in treatment at baseline and to monitor changes in status over time. Because of the completeness of our eligibility criteria, determination of inclusion/exclusion took place over several exchanges with participants (described below).
Table 1.
Inclusion and Exclusion Criteria for CROSSROADS Participants
| Inclusion Criteria |
| At least 65 years old at the time of the initial screening visit |
| BMI 30–40 kg/m2 |
| At increased cardiometabolic health risk (taking at least one medication for hypertension, hyperlipidemia, or type 2 diabetes) |
| Exclusion Criteria |
| Cognitive impairment (SPMSQ)1 |
| Depression (CES-D)2 |
| Ischemic changes on exercise treadmill test (for those who required additional screening) |
| Poorly controlled blood pressure |
| History of prior surgical procedure for weight control or liposuction |
| Unable to make changes to their diet |
| Unable to exercise (walk for at least 6 minutes and perform simple strength and stretch exercise tests) |
| Unwilling to complete MRI |
| Unable to have an MRI due to a pacemaker, neuro stimulator, defibrillator, aneurysm clips, hearing aids, stent, or other device deemed unsafe by the MRI Safety guidelines |
| Use of weight loss medications in previous 3 months |
| Recent Weight change (+/− 10lbs in the last 12 months) |
| Current use of insulin or sulfonylurea agents |
| Current use of oral corticosteroids more than 5 days/month on average |
| Current use of estrogen or testosterone replacement therapy |
| Current use of medications for psychosis or manic-depressive illness |
| History of osteopenia or osteoporosis (self-reported) |
| Cardiovascular disease event within the past 6 months |
| HIV, severe pulmonary disease, or renal failure |
| History of non-skin cancer in the past 5 years |
| Major liver dysfunction within the last 2 years |
| Current smoker or recently quit less than 6 months prior |
| Inability to attend visits and adhere to study protocols |
Participants who scored > 2 (indicative of not being fully intellectually intact) were excluded from participation.
Participants who scored between 16–21 were flagged by research staff for further screen by Dr. Ard; based upon clinical impression, persons whose depression was controlled or situational were eligible to participate, while persons whose depression was uncontrolled and more than situational were excluded from participation. Additionally, persons who scored > 21 were excluded.
Randomization
Once enrolled, participants were randomly assigned to one of three groups: Exercise Only (Control) Intervention, Exercise + Diet Quality + Weight Maintenance Intervention, or Exercise + Diet Quality + Weight Loss Intervention. Random assignment was stratified by age category (65–74, 75+), sex, and race. A blocked randomization program with a varying block size was used, and the condition assignments were place in sealed, sequentially-numbered envelopes that were not opened until a specific participant was assigned. Because this was a behavioral intervention study, it was not possible for participants or all study personnel to be blinded to group assignment. However, in order to minimize bias and ensure allocation concealment, the randomization schedule included sequentially-numbered, opaque sealed envelopes. Additionally, study personnel involved in data collection were blinded to group assignments to minimize potential bias.
Following randomization, participants consented to participate in a 12-month behavioral intervention consisting of individual and group sessions. All participants also agreed to return for an Intermediate Assessment 6-months following randomization and for Post-Intervention Assessment at 12-months.
Components of the Intervention
Components of the intervention for each group are shown in Table 2. Because the recommendations for exercise were consistent across all groups, the Exercise Only group served as the control group for the study, accounting for the effects of exercise training on body composition and physical function. This group received recommendations for cardiovascular exercise and strength training, along with behavioral recommendations for adopting these lifestyle changes. The Exercise + Diet Quality + Weight Maintenance group received the same exercise recommendations as the Exercise Only group. They also received recommendations for improving dietary composition as described below. The Weight Maintenance group had a primary goal of maintaining baseline weight throughout the duration of the study by maintaining baseline caloric intake, but improving the quality of dietary intake and increasing activity levels. The Exercise + Diet Quality + Weight Loss group received the same exercise recommendations as the other two groups, and the same dietary composition recommendations as the Weight Maintenance group. They also received recommendations to reduce caloric intake as described in detail below. The goal of participants in this group was a 10% weight loss by the end of the 12 month intervention.
Table 2.
Components of CROSSROADS Intervention Groups
| Intervention Arm | Behavioral Recommendations | Exercise Recommendations | Dietary Pattern Recommendations | Calorie Restriction Recommendations |
|---|---|---|---|---|
| Exercise Only (Control Group) | X | X | ||
| Exercise + Diet Quality + Weight Maintenance | X | X | X | |
| Exercise + Diet Quality + Weight Loss | X | X | X | X |
All groups met weekly for the first 24 weeks of the intervention, then every two weeks for the remainder of the 12 month intervention. Each session lasted 60 minutes and included 30 minutes of group discussion related to a dietary, exercise, or behavioral topic, followed by 30 minutes of supervised exercise using the prescribed resistance bands exercises detailed below. Weight Loss and Weight Maintenance groups were facilitated by a registered dietician and exercise trainer. Exercise Only groups were led by an exercise trainer.
Exercise Recommendations
All participants engaged in a standard exercise program that included both aerobic and resistance training. The exercise program consisted of a combination of home-based and gym-based activities.
Aerobic Exercise
Participants were given weekly exercise goals based on their baseline activity patterns. Participants were instructed to increase weekly minutes of moderate/vigorous exercise gradually until they consistently participated in 90–150 minutes of moderate-vigorous cardiovascular exercise each week. They were provided with heart rate monitors to assist them in monitoring their home-based exercise intensity, and also received instruction on estimating intensity using rate of perceived exertion (RPE). This was necessary given the high number of participants taking medications that impacted heart rate response to exercise. Participants were not restricted to the type of cardiovascular exercise they could perform. They were given a list of common exercises (e.g., walking, swimming) and received counseling during group sessions on trying new exercises, working exercise into the day, and identifying community resources for exercise.
Resistance Training
Participants were given resistance bands and two full sets of exercise prescriptions, with a goal of completing two resistance training sessions each week. One of the two sessions was completed during the 30 minutes of each group session devoted to exercise. This allowed intervention staff to monitor the participants for safety while performing the exercises, as well as to encourage participants to incrementally increase intensity while working with the resistance bands. The second of the two sessions was performed at home. Participants were also allowed to join a gym or fitness facility during the course of the study and expand their workout to include exercises with free weights or weight machines rather than using the resistance bands. When this occurred, intervention staff reviewed the list of exercises being performed at the gym to ensure that they were comparable to those prescribed, and participants noted those exercises performed in the weekly exercise logs.
Dietary Pattern Quality Recommendations
Participants in both the Weight Loss and Weight Maintenance groups received counseling on improving the quality of their dietary intake. The core of the dietary recommendation was the adoption of a low- energy- density diet composition. Recommendations were based on the concept of “time-calorie displacement,” which emphasizes the ingestion of large quantities of high-bulk, low-energy-density foods (primarily vegetables, fruits, and high-fiber grains) and moderation in the consumption of high-energy-density foods (meats, cheeses, sugars, and fats) (33). Participants were given daily goals for each of six food groups: Whole Grains, Vegetables, Fruit, Meats, Dairy, and Fats. Recommendations reflected a target macronutrient intake pattern of 25% of calories from protein, 47% of calories from carbohydrate, and 28% of calories from fat. Dietary composition recommendations were the same for both the Weight Loss and Weight Maintenance groups.
Calorie Prescription
Study participants randomized to the Weight Loss and Weight Maintenance groups were given daily calorie goals based on estimates of total energy expenditure (TEE) obtained from the measured resting metabolic rate (RMR) at baseline using a ReeVue indirect calorimeter (KORR Medical Technologies, Inc., Salt Lake City. TEE was estimated by calculating RMR * 1.7 to cover energy expenditure related to prescribed exercise activity and the thermic effect of food. We chose an activity factor of 1.7 to match the activity energy expenditure targets for the exercise intervention. Participants in the Weight Maintenance group were prescribed sufficient calories to maintain their baseline body weight based on baseline TEE. Those participants randomized to the Weight Loss group received a reduction of 500 calories/day from baseline TEE. This reduction is consistent with recommendations outlined in the Position Statement of the American Society for Nutrition and the Obesity Society who recommend a modest reduction in energy intake for older adults (7). Calories were not decreased below 1000 kcal per day, regardless of the estimated TEE.
Behavioral Recommendations
The behavioral component of CROSSROADS was based on key theoretical constructs developed to guide health behavior change efforts and on practical applications from previous trials of lifestyle change and cardiometabolic risk reduction. Chiefly, behavioral principles of the intervention were derived from social cognitive theory (34), self-applied behavior modification techniques (35), and the relapse prevention model (36); and were informed by the trans-theoretical model (37, 38). Motivational interviewing also provided a useful framework for helping participants make crucial decisions in light of these behavioral theories (39).
Goal setting and self-monitoring were two key components of the CROSSROADS behavioral recommendations. Intervention modules stressed lifestyle goals specific to the assigned treatment group. This included increased daily activity for all groups, increased fruit and vegetable consumption and portion control for the Weight Maintenance and Weight Loss groups, and caloric restriction for the Weight Loss group. The intervention also included frequent contact with and feedback from intervention staff. Participants were instructed to record all food consumed and exercise performed in weekly logs throughout the duration of the intervention. Logs were reviewed by intervention staff each week and written and verbal feedback was given to participants.
A group intervention was chosen as a mechanism for fostering social support for behavior change among participants. The intervention curriculum also included discussions of building social support outside of the group setting, identifying and overcoming barriers to behavior change, and problem-solving strategies to increase adherence to dietary and exercise recommendations.
Fidelity in Design
Intervention fidelity was monitored in accordance with the best practices and guidelines for maximizing treatment fidelity in health behavior change interventions set forth by the Treatment Fidelity Workgroup of the NIH Behavior Change Consortium (40). These guidelines were integrated into the study by emphasizing fidelity in the following areas: 1) design (consistency with underlying theory), 2) training of interventionists (utilizing assessments such as mock sessions to determine the acquisition and maintenance of interventionists’ skills), 3) delivery of the intervention (accuracy of treatment presentation determined through regular supervision), 4) receipt of the intervention (participant understanding of session content assessed through post-session questioning), and 5) enactment (participant out-of-session implementation assessed via report of intervention strategies used via exercise and dietary logs).
To ensure consistency of study assessment and intervention content and delivery, we used standardized treatment procedures and protocols for assessments, treatment delivery, and monitoring of treatment delivery. Study personnel were thoroughly trained in the interventions and given corrective feedback in practice sessions. Even among highly trained interventionists, there is a potential for slight deviations from treatment protocol to occur over time, commonly referred to as “intervention drift.” In order to protect against this drift, regular “booster” training sessions were conducted. A Manual of Operations and Procedures (MOP) was created and available online through a Sharepoint drive© for all study staff to refer to as needed.
All study personnel having contact with participants and both Drs. Ard and Locher participated in a workshop led by Dr. Delia Smith, one of the world’s leading behavioral experts in lifestyle interventions, prior to the start of the study. The three-day intensive workshop was practice focused and interactive and introduced specific micro-skills that are typically encountered in behavioral weight control interventions. Study personnel practiced the skills in a group setting and were critiqued by Dr. Smith. Midway through the study, a two-day refresher workshop was held where study personnel and the PIs attended. The workshop was also led by Dr. Smith and focused on a review of micro-skills with an emphasis on motivational interviewing and strategies to enhance retention of participants. This workshop was structured the same as the first with an interactive format and practicing of skills, particularly role-playing.
Weekly face-to-face team meetings were held with at least one PI and all research staff to deal with data collection and management issues; and regular (sometimes weekly, depending upon participant flow and phase in the study) face-to-face or phone conferences were held with all intervention staff and one PI to assess the progress of participants as well as discuss fidelity issues that arose during the course of the intervention. These calls allowed for identification of protocol changes that were necessary to ensure fidelity in circumstances including participants experiencing extended absences from intervention groups, holiday schedules, and addressing participants who were not meeting dietary and/or exercise recommendations. These discussions related to both intervention delivery protocol changes, as well as refreshing intervention staff training in motivational interviewing to best address challenging situations.
Participant Retention
A primary goal of the CROSSROADS intervention was to maintain active participation and attendance at the group sessions. To achieve this goal, intervention staff facilitated group interaction that promoted social cohesion and fostered a sense of responsibility to other group members. This was accomplished during group sessions by encouraging participants to share their experiences and offer suggestions to other members on strategies to overcome barriers and incorporate dietary and/or exercise recommendations into their lifestyle. The intervention location was also open at least 30 minutes prior to the scheduled intervention sessions to allow participants to interact with one another outside the formal group meeting. This promoted increased accountability for each individual participant, supporting continued involvement in the intervention.
Because attendance at intervention sessions is essential to the success of the intervention program and is strongly correlated with successful behavior change, we monitored attendance closely and implemented strategies to improve attendance if necessary (41, 42). Specifically, intervention staff contacted participants immediately if he or she failed to attend two consecutive scheduled sessions. Financial incentives were provided at the end of each assessment period (baseline, six months, and twelve months) to compensate participants for their time and effort.
During intervention fidelity conference calls, intervention staff reviewed the progress of each participant with the PI. In each meeting, participants who were not meeting study goals and participants who were not regularly attending group sessions were identified. Staff worked together to discuss potential strategies for reengaging these participants and plans were implemented by intervention staff.
Outcome Measures
CROSSROADS employed an array of outcome measures that were consistent with our specific aims and that sought to better understand response to the interventions anthropometrically (body composition and adipose tissue distribution), metabolically (cardiometabolic disease risk), and functionally (functional status and quality of life). In addition to these measures, a number of co-variates and contextual variables were assessed during the study, as well as ancillary study outcomes. The primary outcome measure was change in VAT from baseline 12-months. Assessments were completed according to the schedule depicted in Table 3. Adipose tissue distribution measures obtained by MRI were only completed at baseline and 12-months to limit expense. The intermediate assessments at 6-months will provide an evaluation of short-term effects of the intervention (including both positive and negative outcomes). Twelve months was chosen deliberately as the primary endpoint because this time frame is accepted as a minimum indicator of sustained weight-loss.
Table 3.
CROSSROADS Study Measures
| Measure | Baseline | 6-month follow up | 12-month follow up |
|---|---|---|---|
| Obtained to Derive Individual Calorie Prescription | |||
| Resting Metabolic Rate | x | ||
| Specific Aim 1 | |||
| Visceral adipose tissue and skeletal muscle (MRI) | x | x | |
| Body composition (DXA) | x | x | x |
| Specific Aim 2 | |||
| Glucose, insulin, lipids, highly sensitive C-reactive protein, leptin, adiponectin, TNF-a, and IL-6 | x | x | x |
| Blood pressure | x | x | x |
| Specific Aim 3 | |||
| SF-36 | x | x | x |
| IWQOL | x | x | x |
| Life-space Assessment | x | x | x |
| Six minute walk | x | x | x |
| Short Performance Physical Battery | x | x | x |
| Leg and hand grip strength | x | x | x |
| Sit and reach | x | x | x |
| Covariates | |||
| 24-hour diet recall | x | x | x |
| Accelerometry | x | x | x |
| Medications | x | x | x |
| Weight | x | x | x |
| Height | x | x | x |
| Waist circumference | x | x | x |
| Nutrition Self-efficacy Scale | x | x | x |
| Behavior Change Scale | x | x | x |
| Social Support Surveys for Diet and Exercise | x | x | x |
| Ancillary Measurements * | x | x | x |
Ancillary measurements included the Everyday Discrimination Scale, Perceived General Stress Scale, MacArthur Scale of Subjective Social Status Questionnaire, Duke Social Support Index, International Prostate Symptom Score Questionnaire, Fecal Incontinence Severity Index, International Consultation on Incontinence Modular Questionnaire, Pittsburg Sleep Quality Index, STOP-Bang Questionnaire, and the Exercise Fear-Avoidance Scale.
In the next section, we present our specific aims, hypotheses, and outcomes used to evaluate those aims and hypotheses.
Specific Aim #1: To compare the effects of changes in diet composition alone or combined with weight loss with an exercise only control intervention on body composition, namely visceral adipose tissue (VAT).
Hypothesis 1: There will be a 10% difference in change in VAT in older adults at one year of follow up,
H1a: for those on a weight reducing diet (10%) compared to control;
H1b: for those on a weight maintenance diet compared to control;
H1c: for those on a weight reducing diet (10%) compared to a weight maintenance diet.
The primary study outcome was change in VAT measured by magnetic resonance imaging (MRI). Trans-axial abdominal images were collected using 3D volumetric T1-weighted Multiple 2D Turbo Field Echo (M2D TFE) imaging sequence using a 3-Tesla Philips Achieva system. Four packets with 12 slices each were collected to cover the abdominal cavity from the zyphoid process to the top of the pelvis under a 17-second breath-hold condition. Of the 48 slices collected, those imaging the abdominal cavity between the L1 and L5 vertebrae were analyzed for subcutaneous-abdominal and VAT volumes. The following acquisition parameters were used with our M2D TFE sequence: contiguous 5 mm volumetric slices, 340 mm × 240 mm in-plane FOV, 340×240 acquisition matrix, Echo Train Length=400, Percent Phase FOV 100%, and a 30 degree Flip Angle. The echo time (TE=2.7 msec), repetition time (TR=5.6 ms), and pulse flip angles (30-degrees) were selected to optimize the signal-intensity contrast between the adipose and non-adipose tissue in the abdomen. We optimized our sequence parameters so that each image slice took approximately 1–2 seconds to acquire.
Other anthropometric body composition outcomes of interest included skeletal muscle, thigh-subcutaneous adipose tissue, thigh-perimuscular adipose tissue, and thigh-intermuscular adipose tissue volumes. Trans-axial images of the thigh were collected using Magnetization Prepared Rapid Gradient Echo (MPRAGE) imaging sequence. The following acquisition parameters were used with the MPRAGE sequence: contiguous 5 mm volumetric slices, 512 mm × 240 mm in-plane FOV, 512×240 acquisition matrix, Percent Phase FOV 100%, and a 8 degree Flip Angle. The echo time (TE=3.2 msec), repetition time (TR=6.5 ms), and pulse flip angles (8-degrees) were selected to optimize the signal-intensity contrast between the adipose and non-adipose tissue in the leg.
Total and regional body composition and bone density were measured with a Lunar DPX-L densitometer using the body composition Adult Software Version 1.33 (Lunar Corp). Participants completed a total body scan, requiring about 10 minutes, while lying on their backs on a padded table in a hospital gown with metal objects removed. The scan provides estimates of soft-tissue attenuation ratios, fat and lean tissue mass, and bone mineral content and density. These parameters can be recorded for the whole body or in defined anatomical regions of interest. We used DXA for estimates of total, trunk, appendicular fat and lean mass, and bone mineral density at the lumbar spine.
Specific Aim #2. To compare the effects of a change in diet composition alone or combined with weight loss with an exercise only control intervention on cardiometabolic disease risk.
Hypothesis 2: There will be greater improvements in markers of cardiometabolic disease risk, including blood pressure, fasting glucose, insulin, lipids, highly sensitive C-reactive protein, adiponectin, leptin, TNF-α, and IL-6 in older adults at one year of follow up,
H2a: for those on a weight reducing diet (10%) compared to control;
H2b: for those on a weight maintenance diet compared to control;
H2c: for those on a weight reducing diet (10%) compared to a weight maintenance diet.
Fasting blood draws for biomarkers of cardiometabolic disease risk factors were obtained, including glucose, insulin, lipids, highly sensitive C-reactive protein, leptin, adiponectin, TNF-αa, and IL-6. In addition to these laboratory measures, blood pressure was measured by trained research staff using automated blood pressure devices (Omron HEM 907-XL) in duplicates measured 30 seconds apart. All prescription medications were recorded and categorized based on indication for diabetes, hypertension, or hyperlipidemia.
Specific Aim #3: To compare the effects of a change in diet composition alone or combined with weight loss with an exercise only control intervention on functional status and quality of life.
Hypothesis 3: There will be greater improvements in functional status and quality of life in older adults at one year of follow up,
H3a: for those on a weight reducing diet (10%) compared to control;
H3b: for those on a weight maintenance diet compared to control;
H3c: for those on a weight reducing diet (10%) compared to a weight maintenance diet.
We obtained a general assessment of quality of life (QOL) using the SF-36v2™ (43). In addition to this general measure, we obtained a more specific assessment of QOL related to body weight with the Impact of Weight on Quality of Life-Lite (IWQOL-Lite) (44, 45). The UAB LifeSpace Assessment (46), 6-Minute Walk, Short Physical Performance Battery (47), measurements of leg and hand grip strength, and chair sit and reach ability were obtained to assess functional ability.
Diet and Physical Activity Covariates
As part of the baseline and follow up assessments, diet and physical activity were assessed using 24 hour dietary recalls and accelerometry methods, respectively. Three dietary recalls were collected at baseline, 6-months, and 12-months. These were collected over the telephone by research staff trained and certified by the University of Minnesota’s Nutrition Coordinating Center’s Nutrition Data System using the Nutrition Data System for Research (NDSR) (http://www.ncc.umn.edu/ndsrsupport/training.html). The interviewers used a multiple-pass approach. The recalls were collected over a two-week period and included two week days and one weekend day. The three recalls collected at each time point were aggregated to obtain an average daily caloric intake. Participants were provided with an Actigraph Actitrainer accelerometer (http://www.actigraphcorp.com/support/devices/) and were instructed to wear it continuously, except when bathing or swimming, for one week.
Self-Efficacy, Goal-Setting, Relapse Prevention, and Social Support Covariates
We were additionally interested in evaluating whether self-efficacy, goal setting, relapse prevention, and social support and changes in these would mediate the effect of the intervention on primary and secondary outcomes. In order to assess self-efficacy, we used a 5-Item Nutrition Self-Efficacy Scale developed by Schwarzer and Renner (48). This self-efficacy item is specific to nutritional change and well-suited for the study because it allows for assessment of self-efficacy related to weight gain or maintenance. In order to assess goal-setting and relapse prevention behavior we used the Behavior Change Scale developed by Nies and colleagues (49). To evaluate presence of social support, we used the Social Support Surveys for Diet and Exercise Behaviors developed by Sallis (50).
Ancillary Measurements
Because of the rich dataset afforded by the CROSSROADS study, several investigators requested permission to add ancillary studies to piggyback their research questions onto the study. These ancillary projects included research questions related to: 1) social status (PI: Akilah Keita), 2) continence status (PI: Alayne Markland), 3) dietary antioxidants and inflammation (PI: Kristi Crowe), 4) sleep (PI: Megan Reuter), and 5) pain and avoidance of exercise (PI: Brooks Wingo). These ancillary research questions and measurements expand upon the proposed primary aims of the CROSSROADS study and provide opportunities for further insight into obesity management in older adults.
Adverse Event Monitoring
Given that this study involved diet and exercise interventions in older adults, the interventions had the potential for adverse effects such as reduced lean body mass and bone mineral density or musculoskeletal injuries. Thus, participants were actively screened and adverse events were monitored regularly for potential unanticipated problems reportable to the institutional review board (IRB) and sponsor. Participants were interviewed at baseline for signs and symptoms and then screened every three months during their participation in the study either in person or over the telephone for any adverse medical events, signs, or symptoms. All adverse events were compiled in a yearly report to the Data and Safety Monitor and funding institute for further monitoring.
Data Tracking System
Because there were multiple faculty, staff, and trainees who were involved in CROSSROADs and because the study took place at multiple sites (e.g., the assessments took place in three separate buildings, the intervention in another, and data management in another; and midway through the study, Dr. Ard moved to another university), it became clear that a data tracking system would be necessary to allow real-time, interactive monitoring of participants’ flow through various stages of study completion. Therefore, a web-based enrollment, tracking, and data collection system was designed and used in the study. The system used a Microsoft IIS with SSL certificate and secure logon authentication. The web site programming was done using ASP.Net and JAVA script; and the database was stored on an SQL server.
The tracking system was automated to perform the following functions: 1) alert staff of participants who were not eligible for the study during eligibility screening, 2) directly submit participant information, including medication and treadmill screenings results, to Dr. Ard for eligibility review, 3) alert staff when participants had completed one component of the study and were ready for the next, and 4) alert staff of incomplete or out of range outcome measurements and prompt the staff user to cite a reason if it was not completed or verify out of range values, 5) alert intervention staff of participants who had missed two consecutive intervention classes so that a follow-up call could be made to the participant to promote adherence and retention.
Data Management and Analysis
The integrity of the data is of utmost concern in this study. All data, with the exception of the 24-hour recalls were collected on standardized, computerized scannable forms and entered directly into a scannable device (Fujitsu, Scan Partner, 600C). Prior to entering the forms into the scannable device, all forms were carefully reviewed by the Project Coordinator to identify inconsistencies in the data or missing data. If there were inconsistencies or missing data on the data collection forms, errors were corrected. If there was missing data, the study participant was re-contacted. The use of scannable forms reduced the need for dual data entry and verification because the form was entered directly into the computerized scannable device, thus enhancing the accuracy of the data. Questionable entries (e.g., missing data, two responses selected for one item) were flagged and verified to further enhance quality control. The software (Teleform, Version 6) was used with the scannable device readily converting data entry and management forms to compatible statistical software formats. Thus, the raw data entered into the scannable device from standardized computerized data entry forms was converted into a statistical data management file.
This is an intention-to treat study. All analyses, unless otherwise specified, will include all randomized cases. Most of the statistical analyses will be conducted using SPSS or SAS. We are also familiar with other statistical packages (e.g., Mplus) that may be used for particular psychometric analyses and/or secondary analyses such as multiple outcomes models. Prior to testing the specific aims, descriptive statistics will be used to characterize the sample. Next, the groups will be compared using the chi-square statistic and analysis of variance to determine whether differences existed prior to randomization between the groups on key variables that may have an effect on outcomes. The stratified randomization should ensure balance between the intervention groups on gender and ethnicity, but additional analyses will be used to examine the comparability between groups on baseline BMI, caloric intake, energy density, and physical activity. The primary endpoints occur at the Post-Intervention Assessment (i.e., 12-months). Because this is an intention-to-treat study, where appropriate we will impute missing data and rely upon measures obtained at the Intermediate Assessment to impute data at the post-intervention assessment if such data are missing. The proposed study meets criteria for an NIH-defined Phase III Clinical Trial; and a valid analysis of intervention effects in gender and ethnic subgroups will be conducted for each aim. We are not, however, hypothesizing specific gender or ethnic interaction effects and our study is only powered to detect main effects that extend across gender and ethnic subgroups.
DISCUSSION
More information is needed regarding the potential benefits and harms of recommending intentional weight loss in older, obese adults who are at risk for cardiovascular disease and functional decline. Older adults (those ≥ 65 years) are expected to make up 20% of the population by 2030 (1). Concomitant with this growth in the older population, there is an increasing percentage of older adults who are or will be obese. Obesity is associated with an increased risk of a number of chronic diseases, including hypertension, diabetes, and increased cardiovascular disease risk. With the prevalence of obesity increasing in a rapidly growing segment of the population, the impact on disease prevalence could be tremendous, presenting a significant challenge for our health care system. Consistent with the mission of the National Institute on Aging and its emphases on interventions and behavior change, the approach used in the CROSSROADS study has the potential to improve health outcomes across a broad spectrum of illnesses and to reduce associated health care costs (51).
As recognized in the 2005 Obesity Society position statement, encouraging weight loss in older adults is not without controversy (7). This controversy arises because there are few randomized trials of voluntary, diet-induced weight loss in older adults (over age 65) that carefully assess whether weight loss can improve cardiometabolic risk factors, physical function, and quality of life without causing harm (7, 10, 11, 12, 12). In a recent overview of the controversy surrounding weight loss in obese older adults 65 years and older, Waters, Ward, and Villareal specifically recommend that “future lifestyle interventions for obese older adults should address the loss of bone and lean body mass (and) inflammatory mechanisms.” (9) This is the precise focus of our research.
The CROSSROADS study will allow us to determine if deleterious adipose tissue depots can be reduced preferentially in older adults while minimizing the loss of lean muscle mass and BMD. This ideal scenario would potentially maximize the health benefits and minimize risk for decline in function with intentional weight loss. Such information can strengthen the evidence that can be used to develop guidelines related to obesity management in older adults.
Furthermore, this study will make several key contributions to the field of nutrition and aging. This study prospectively assessed changes in adipose tissue distribution, body composition, cardiometabolic risk factors, physical function, and quality of life simultaneously. Because of the randomized, controlled experimental design, we will be able to draw inferences regarding the causal relationships between changes in body composition and disease risk or functional status given one of three experimental conditions. The inclusion of a weight- maintenance group with the same dietary composition as the weight loss group provides the opportunity to better isolate the effects of calorie restriction on the outcomes of interest. The inclusion of the weight maintenance group also provides the opportunity to study the impact of changing diet composition alone in older adults. All participants were at least 65 years of age. To the best of the authors’ knowledge, this will be the largest study, of which we are aware, of intentional weight loss and dietary change in a group of older adults all with a mean age over 65 years of age.
If we are to recommend weight reduction to older patients we should be better able to answer the following questions: 1) What are the effects of weight reduction on body compartments that have implications for disease risk? 2) Does weight loss increase the risk of functional decline because of changes in lean muscle mass and bone mass?? Or is the risk offset by larger declines in fat mass? 3) Does change in diet composition with maintenance of body weight have beneficial effects on disease risk? The CROSSROADs study is designed and poised to answer these questions.
TAKE AWAY POINTS.
The CROSSROADs trial is the first evidence-based randomized controlled intervention study in the area of lifestyle intervention education for older adults at risk for cardiometabolic disease.
The design of the intervention and selection of outcome measures was based on an extensive review of the literature and our own preliminary findings and clinical practice—with particular attention paid to both benefits and risks of intervention.
The results of the CROSSROADS trial will determine whether the benefits of weight loss and/or change in diet quality delivered through a standard lifestyle intervention outweigh the potential risks in a group of community dwelling, obese, older adults who were at increased risk for cardiometabolic disease.
Future findings will contribute to evidence-based behavioral health practices that can guide decision makers in formulating polices related to obesity management in older adults.
Acknowledgments
This work was supported by the National Institute on Aging (R01AG033094; K07AG043588), the National Institute of Diabetes and Digestive and Kidney Diseases (P30DK056336, P60DK079626, T32DK062710, R00DK83333) the National Heart, Lung, and Blood Institute (T32HL105349), the National Center for Advancing Translational Sciences (UL1RR025777), and the Agency for Healthcare Research and Quality (T32HS013852).
Footnotes
Author Contributions: Jamy Ard, MD and Julie L. Locher, PhD are Co-Principal Investigators of the study. They contributed equally to the design and management of the study and are to be considered co-anchor authors on this paper. Dr. Ard is a physician who has over fifteen years of clinical and research experience related to weight management in adults. Dr. Locher is a medical sociologist who has over two decades of experience in studying eating behaviors and nutrition-related health outcomes specifically in older adults. She is an expert in delivering behavioral nutrition interventions in older adults. Marilyn Haas, BA served as Project Manager for the study and took the lead in composing the first draft of this manuscript and in soliciting initial input from co-authors. The remaining co-authors are listed alphabetically; they have contributed in various ways and at different levels of involvement throughout the study. Eric Bodner, BS designed and assisted throughout the study in data tracking and management of participant flow through the study. Cynthia Brown, MD MSPH and Christine Ritchie, MD MSPH served as geriatric medical monitors. Additionally, Dr. Ritchie created our adverse events and symptoms events monitoring protocol. David Bryan, MA implemented and supervised assessment of functional status outcomes. David R. Buys, PhD; Akilah Duhlin Keita, PhD; Amy Miskimon Goss, PhD; and Brooks C. Wingo, PhD were Postdoctoral Fellows who contributed substantially to the study particularly with respect to study coordination at the beginning of the study (DRB); inclusion of social outcome measures (ADK); Magnetic Resonance Imaging interpretation (AMG); and implementation, oversight and monitoring of the interventions (BCW). Dr. Wingo subsequently obtained a faculty position and transitioned to a Co-Investigator on the grant assuming on-site clinical oversight of the project when Dr. Ard relocated to Wake Forest. Lee Anne Flagg, MA is a predoctoral fellow on the project who was primarily responsibility for monitoring adverse events. Martha Hovater, MS served as the day-to-day data manager and statistical analyst; while David Roth, PhD served as the Co-Investigator responsible for statistics. Gary Hunter, PhD and Barbara Gower, PhD served as Co-Investigators with Dr. Hunter contributing expertise in exercise intervention development and Dr. Gower contributing expertise in assessment of body composition and cardiometabolic outcomes.
Contributor Information
Marilyn C. Haas, Division of Gerontology, Geriatrics, and Palliative Care, UAB, Birmingham, Alabama, USA.
Eric V. Bodner, Division of Gerontology, Geriatrics, and Palliative Care, UAB, Birmingham, Alabama, USA.
Cynthia J. Brown, Division of Gerontology, Geriatrics, and Palliative Care, UAB, Birmingham, Alabama, USA; Comprehensive Center for Healthy Aging, UAB, Birmingham, Alabama, USA; Birmingham/Atlanta VA Geriatrics Research, Education, and Clinical Center (GRECC), Birmingham, Alabama.
David Bryan, Department of Human Studies and Nutrition Sciences, UAB, Birmingham, Alabama, USA.
David R. Buys, Department of Food Science, Nutrition, and Health Promotion, Mississippi State University, USA.
Akilah Dulin Keita, Institute for Community Health Promotion, Brown University, Providence, Rhode Island, USA.
Lee Anne Flagg, Department of Sociology, UAB, Birmingham, Alabama, USA; Nutrition Obesity Research Center, UAB, Birmingham, Alabama, USA.
Amy Goss, Department of Nutrition Sciences, UAB, Birmingham, Alabama, USA; Nutrition Obesity Research Center, UAB, Birmingham, Alabama, USA.
Barbara Gower, Department of Nutrition Sciences, UAB, Birmingham, Alabama, USA; Comprehensive Center for Healthy Aging, UAB, Birmingham, Alabama, USA; Nutrition Obesity Research Center, UAB, Birmingham, Alabama, USA.; Diabetes Research Center, UAB, Birmingham, Alabama, USA.
Martha Hovater, Department of Biostatistics, UAB, Birmingham, AL, USA.
Gary Hunter, Departments of Human Studies and Nutrition Sciences, University of Alabama at Birmingham, Alabama, USA; Comprehensive Center for Healthy Aging, UAB, Birmingham, Alabama, USA; Center for Exercise Medicine, University of Alabama at Birmingham, Alabama, USA; Nutrition and Obesity Research Center, University of Alabama at Birmingham, Alabama, USA.
Christine S. Ritchie, Division of Geriatrics, University of California San Francisco, San Francisco, California, USA.
David L. Roth, Division of Geriatric Medicine and Gerontology, Johns Hopkins University, Baltimore, Maryland; Center on Aging and Health, Johns Hopkins University, Baltimore, Maryland; Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA; Department of Biostatistics, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
Brooks C. Wingo, Department of Occupational Therapy, UAB, Birmingham, Alabama, USA.
Jamy Ard, Department of Internal Medicine, Wake Forest University, Winston-Salem, North Carolina, USA.
Julie L. Locher, Division of Gerontology, Geriatrics, and Palliative Care, UAB, Birmingham, Alabama, USA; Comprehensive Center for Healthy Aging, UAB, Birmingham, Alabama, USA; Nutrition Obesity Research Center, UAB, Birmingham, Alabama, USA; Department of Health Care Organization and Policy, UAB, Birmingham, Alabama, USA.
References
- 1.Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key Indicators of Well-Being. Federal Interagency Forum on Aging-Related Statistics; Washington, DC: U.S. Government Printing Office; Jun, 2012. [Accessed 06.04.14]. Available at: http://www.agingstats.gov/Main_Site/Data/2012_Documents/docs/EntireChartbook.pdf. [Google Scholar]
- 2.Marie Ng, Gakidou Emmanuela, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014 doi: 10.1016/S0140-6736(14)60460-8. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Carrol MD, Kit BK, Flegal KM. Preve alance of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fakhouri TH, Ogden CL, Carroll MD, et al. Prevalence of obesity among older adults in the United States, 2007–2010. Hyattsville, MD: National Center for Health Statistics; 2012. NCHS data brief, no 106. [Google Scholar]
- 5.Reynolds SL, McIlvane JM. The Impact of Obesity and Arthritis on Active Life Expactancy in Older Americans. Obesity. 2009;17(2):363–9. doi: 10.1038/oby.2008.534. [DOI] [PubMed] [Google Scholar]
- 6.Ritchie C, Locher J, Roth D, McVie T, Sawyer P, Allman R. Unintentional Weight Loss Predicts Decline in ADL Function and Life Space Mobility over Four Years among Community Dwelling Older Adults. Journal of Gerontology: Medical Sciences. doi: 10.1093/gerona/63.1.67. In press. [DOI] [PubMed] [Google Scholar]
- 7.Villareal DT, Apovian CM, Kushner RF, Klen S. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res. 2005;13(11):1849–63. doi: 10.1038/oby.2005.228. [DOI] [PubMed] [Google Scholar]
- 8.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Affairs. 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 9.Waters DL, Ward AL, Villareal DT. Weight loss in obese adults 65 years and older: A review of the controversy. Experimental Gerontology. 2013;48:1054–61. doi: 10.1016/j.exger.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zamboni M, Mazzali G, Zoico E, et al. Health consequences of obesity in the elderly: a review of four unresolved questions. International Journal of Obesity. 2005;29:1011–1029. doi: 10.1038/sj.ijo.0803005. [DOI] [PubMed] [Google Scholar]
- 11.McTigue KM, Hess R, Ziouras J. Obesity in Older Adults: A Systematic Review of the Evidence for Diagnosis and Treatment. Obesity Research. 2006;14(9):1485. doi: 10.1038/oby.2006.171. [DOI] [PubMed] [Google Scholar]
- 12.Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obesity Reviews. 2001;2(3):173–182. doi: 10.1046/j.1467-789x.2001.00032.x. [DOI] [PubMed] [Google Scholar]
- 13.Lissner L, Odell PM, D’Agostino RB, et al. Variability of body weight and health outcomes in the Framingham population. New England Journal of Medicine. 1991;324(26):1839–1844. doi: 10.1056/NEJM199106273242602. [DOI] [PubMed] [Google Scholar]
- 14.Andres R, Muller DC, Sorkin JD. Long-Term Effects of Change in Body Weight on All-Cause Mortality: A Review. Ann Intern Med. 1993;119(7_Part_2):737–743. doi: 10.7326/0003-4819-119-7_part_2-199310011-00022. [DOI] [PubMed] [Google Scholar]
- 15.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anton SD, Manini TM, Milsom VA, et al. Effects of a weight loss plus exercise program on physical function in overweight, older women: A randomized controlled trial. Clin Interv Aging. 2011;6:141–149. doi: 10.2147/CIA.S17001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frimel TN, Sinacore DR, Villareal DT. Exercise attenuates the weight-loss induced reduction in muscle mass in frail obese older adults. Med Sci Sports Exerc. 2008;40:1213–1219. doi: 10.1249/MSS.0b013e31816a85ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mojtahedi MC, Thorpe MP, Karampinos DC, Johnson CL, Layman DK, Georgiadis JG, Evans EM. The effects of a higher protein intake during energy restriction on changes in body composition and physical function in older women. J Gerontol A Biol Sci Med Sci. 2011;66(11):1218–25. doi: 10.1093/gerona/glr120. [DOI] [PubMed] [Google Scholar]
- 19.Woo J, Leund J, Kwok T. BMI, body composition, and physical functioning in older adults. Obesity (Silver Spring) 2007;15(7):1886–94. doi: 10.1038/oby.2007.223. [DOI] [PubMed] [Google Scholar]
- 20.Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996;143(3):228–39. doi: 10.1093/oxfordjournals.aje.a008733. [DOI] [PubMed] [Google Scholar]
- 21.Kohrt WM, Kirwan JP, Staten MA, Bourey RE, King DS, Holloszy JO. Insulin resistance in aging is related to abdominal obesity. Diabetes. 1993;42(2):273–81. [PubMed] [Google Scholar]
- 22.Guillet C, Zangarelli A, Gachon P, et al. Whole Body Protein Breakdown Is Less Inhibted by Insulin, But Still Responsive to Amino Acid, in Nondiabetic Elderly Subjects. Journal of Clinical Endocrinology & Metabolism. 2004;89:6017–6024. doi: 10.1210/jc.2003-031323. Endocrine Soc. [DOI] [PubMed] [Google Scholar]
- 23.Guillet C, Boirie Y. Insulin resistance: a contributing factor to age-related muscle mass loss? Diabetes Metab. 2005;31(Spec No 2):5S20–5S26. doi: 10.1016/s1262-3636(05)73648-x. [DOI] [PubMed] [Google Scholar]
- 24.Corcoran MP, Lamon-Fava S, Fielding RA. Skeletal muscle lipid deposition and insulin resistance: effect of dietary fatty acids and exercise. American Journal of Clinical Nutrition. 2007;85(3):662. doi: 10.1093/ajcn/85.3.662. [DOI] [PubMed] [Google Scholar]
- 25.Defronzo RA. Glucose intolerance and aging: evidence for tissue insensitivity to insulin. Diabetes. 1979;28(12):1095–101. doi: 10.2337/diab.28.12.1095. [DOI] [PubMed] [Google Scholar]
- 26.Villareal DT, Miller BV, 3rd, Banks M, Fontana L, Sinacore DR, Klein S. Effect of lifestyle intervention on metabolic coronary heart disease risk factors in obese older adults. Am J Clin Nutr. 2006;84(6):1317–23. doi: 10.1093/ajcn/84.6.1317. [DOI] [PubMed] [Google Scholar]
- 27.Nicklas BJ, Dennis KE, Berman DM, Sorkin J, Ryan AS, Goldberg AP. Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors obese, postmenopausal, African-American and Caucasian women. J Gerontol A Biol Sci Med Sci. 200;58(2):181–9. doi: 10.1093/gerona/58.2.m181. [DOI] [PubMed] [Google Scholar]
- 28.Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, Napoli N, Qualls C, Shah K. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–1229. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Napoli N, Shah K, Waters DL, Sinacore DR, Qualls C, Villareal DT. Effects of weight loss, exercise, or both on cognition and quality of life in obese older adults. Am J Clin Nutr. 2014;100:189–98. doi: 10.3945/ajcn.113.082883. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bouchonville, et al. Weight loss, exercise or both and cardiometabolic risk factors in obese older adults: results of a randomized controlled trial. Int J Obes. 2014;38:423–431. doi: 10.1038/ijo.2013.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schulz KF, Altman DG, Moher D for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Int Med. 2010:152. [PMC free article] [PubMed] [Google Scholar]
- 32.Jensen MD, et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014 Jul 1;63(25 Pt B):2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 33.Weinsier RL, Bacon JA, Birch R. Time-calorie displacement diet for weight control: a prospective evaluation of its adequacy for maintaining normal nutritional status. Int J Obes. 1983;7(6):539–48. [PubMed] [Google Scholar]
- 34.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, N.J: Prentice-Hall; 1986. (Prentice-Hall series in social learning theory) [Google Scholar]
- 35.Watson DL, Tharp RG. Self-directed behavior: self-modification for personal adjustment. 8. Belmonst, CA: Wadsworth/Thomson Learning; 2002. [Google Scholar]
- 36.Martlatt GA, Gordon JR. Relapse prevention: maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. The Guilford clinical psychology and psychotherapy series) [Google Scholar]
- 37.Prochaska JO, DiClemente CC. The transtheoretical approach: crossing traditional boundries of therapy. Malabar, Fla: Krieger Rub; 1994. [Google Scholar]
- 38.Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, Abrams DB. Using the stages of change model to increase the adoption of physical activity among community participants. Am J Health Promot. 1992;6(6):424–9. doi: 10.4278/0890-1171-6.6.424. [DOI] [PubMed] [Google Scholar]
- 39.Miller WR, Rollnick S. Motivational interviewing: preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- 40.Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, Ogedegbe G, Orwig D, Ernst D St Czajkowski Treatment Fidelity Workgroup of the NIH Behavior Change Consortium. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–51. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 41.Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist PA, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Prev Med. 1984;13(2):155–68. doi: 10.1016/0091-7435(84)90048-3. [DOI] [PubMed] [Google Scholar]
- 42.Wadden TA, Foster GD, Wang J, et al. Clinical correlates of short- and long-term weight loss. Am J Clin Nutr. 1992;56(1 Suppl):271S–274S. doi: 10.1093/ajcn/56.1.271S. [DOI] [PubMed] [Google Scholar]
- 43.SF36.org. [Accessed 08.18.14]; http://www.sf-36.org/
- 44.Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-Lite) in a community sample. Quality of Life Research. 2002;11(2):157–171. doi: 10.1023/a:1015081805439. [DOI] [PubMed] [Google Scholar]
- 45.Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a Brief Measure to Assess Quality of Life in Obesity. Obesity Research. 2001;9(2):102–111. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 46.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51(11):1610–4. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 47.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol Med Sci. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 48.Schwarzer R, Renner B. [13 September 2005];Health-specific self-efficacy scales. Accessed at http://userpage.fuberlin.de/~health/healself.pdf.
- 49.Nies MA, Hepworth JT, Wallston KA, Kershaw TC. Evaluation of an instrument for assessing behavioral change in sedentary women. J Nurs Scholar. 2001;33(4):349–54. doi: 10.1111/j.1547-5069.2001.00349.x. [DOI] [PubMed] [Google Scholar]
- 50.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 51. [on 10 October 2007];National Institute on Aging Web site. Accessed at http://www.nia.nih.gov/


