Abstract
Apical membrane antigen 1 (AMA1) is a leading malarial vaccine candidate; however, its polymorphic nature may limit its success in the field. This study aimed to circumvent AMA1 diversity by dampening the antibody response to the highly polymorphic loop Id, previously identified as a major target of strain-specific, invasion-inhibitory antibodies. To achieve this, five polymorphic residues within this loop were mutated to alanine, glycine, or serine in AMA1 of the 3D7 and FVO Plasmodium falciparum strains. Initially, the corresponding antigens were displayed on the surface of bacteriophage, where the alanine and serine but not glycine mutants folded correctly. The alanine and serine AMA1 mutants were expressed in Escherichia coli, refolded in vitro, and used to immunize rabbits. Serological analyses indicated that immunization with a single mutated form of 3D7 AMA1 was sufficient to increase the cross-reactive antibody response. Targeting the corresponding residues in an FVO backbone did not achieve this outcome. The inclusion of at least one engineered form of AMA1 in a biallelic formulation resulted in an antibody response with broader reactivity against different AMA1 alleles than combining the wild-type forms of 3D7 and FVO AMA1 alleles. For one combination, this extended to an enhanced relative growth inhibition of a heterologous parasite line, although this was at the cost of reduced overall inhibitory activity. These results suggest that targeted mutagenesis of AMA1 is a promising strategy for overcoming antigenic diversity in AMA1 and reducing the number of variants required to induce an antibody response that protects against a broad range of Plasmodium falciparum AMA1 genotypes. However, optimization of the immunization regime and mutation strategy will be required for this potential to be realized.
INTRODUCTION
The apicomplexan parasite Plasmodium falciparum, the causative agent of the most severe form of human malaria, is responsible for >0.5 million deaths annually. There are currently no licensed vaccines for malaria; however, the development of clinical immunity in naturally exposed individuals suggests that a vaccine that reduces the morbidity and mortality associated with malaria is likely to be achievable (1). RTS,S/ASO1, a vaccine targeting the preerythrocytic stages of P. falciparum, is showing partial efficacy in a large multicenter phase III trial in Africa (2), but ultimately, an improved vaccine with higher efficacy and longer duration of protection will be required (3). This may be achieved through new vaccine approaches or by incorporating one or more asexual blood-stage antigens into a vaccine containing RTS,S.
Of the asexual blood-stage antigens assessed as potential vaccine components, apical membrane antigen 1 (AMA1) has been considered particularly promising, and a large body of preclinical data supported the decision by several groups to take AMA1 vaccines into clinical development (recently reviewed in reference 4). Additionally, AMA1 is an important target of acquired immunity; antibodies to AMA1 have been associated with protection from malaria in different populations and settings (5, 6), and human antibodies to AMA1 can inhibit blood-stage replication of P. falciparum (7). AMA1 is one of very few candidate malaria vaccines that has shown efficacy in phase II clinical trials (1). One of two AMA1 vaccines to reach phase II testing in the field showed significant efficacy, but this was restricted to protection against parasites with vaccine-like alleles of AMA1, indicating that the protective effect was allele specific (8). As molecular epidemiological studies showed that many of the polymorphic sites in AMA1 were under balancing selection, presumably by protective antibody responses (9–12), it is not surprising that a vaccine containing a single allelic form of AMA1 failed to generate protection against the majority of P. falciparum AMA1 genotypes. This has highlighted the problem that polymorphisms in AMA1 and other asexual blood-stage antigens may limit the effectiveness of these antigens as vaccine components.
Based on disulfide bond connectivity (13) and the three-dimensional crystal structure (14), AMA1 has been divided into three domains. Domain I harbors the majority of the polymorphic sites, and these sites can be grouped into three clusters according to their spatial distribution: C1, C2, and C3 (14–16). The C1 cluster was shown to be largely responsible for allowing the FVO strain of P. falciparum to escape inhibition by rabbit anti-3D7 AMA1 antibodies in vitro (15). Within this cluster, residues located in the highly polymorphic loop Id made the largest contribution to escape. This group of polymorphisms, termed C1-L, forms a large part of the epitope recognized by the strain-specific, inhibitory monoclonal antibody (MAb) 1F9 and is a target of naturally acquired antibodies to AMA1 (17, 18). Human antibodies to this epitope are acquired with increasing exposure to malaria and are associated with both protective immunity and growth-inhibitory activity in vitro (18). Compelling evidence of the importance of this polymorphic cluster has come from an analysis of the breakthrough parasites in the phase II trial of a 3D7 AMA1 vaccine in Mali; there was no significant efficacy against all malarial episodes, but efficacy was 64% for malaria episodes caused by parasites identical to vaccine-strain AMA1 at polymorphic sites within C1-L (residues 196, 197, 199, 200, 201, 204, 206, and 207) (8, 19). If the development of AMA1 as a component of a malaria vaccine is to continue, strategies to circumvent the problem posed by polymorphisms must be a priority.
Although sequence diversity within AMA1 is large, genetic analyses suggest that variants can be grouped into as few as six different populations, and it is possible that development of a vaccine containing representative alleles from each population or broadly covering the diversity in AMA1 may be an effective approach to cover the majority of parasite genotypes (16, 20–24). However, AMA1 haplotype groups are only weakly predictive of the cross-reactivity or cross-inhibitory activity of antibodies (21); this highlights the need for further studies to understand key polymorphic epitopes and strategies to overcome diversity in AMA1. Immunization of animals with combinations of multiple AMA1 alleles has been shown by several groups to induce an antibody response more directed toward conserved epitopes (23, 25–28). If these antibodies are equally protective as allele-specific responses, as some data suggest, a combination of a relatively small number of alleles may be sufficient. However, it should be noted that immunization with a combination of two forms of Plasmodium chabaudi AMA1 did not protect mice from challenge with P. chabaudi expressing a third allelic form of AMA1 (29). Also, no efficacy was observed in a phase II trial using a combination of 3D7 and FVO allelic forms of AMA1 (30). However, the lack of protection in this trial has been attributed to insufficient immunogenicity rather than an inability to control heterologous infections (31).
An alternative, or complementary, strategy to multiallele vaccine approaches involves the generation of mutated forms of AMA1 with the aim of dampening the antibody response to dominant strain-specific epitopes and with the expectation that there will be an enhanced response to cross-reactive epitopes. Others have used this strategy with little success (32), but here we have explored this approach using a smaller subset of polymorphic residues in both FVO and 3D7 AMA1, which differ in the extent to which they induce a strain-specific antibody response. Furthermore, we replaced each target site with alanine, glycine, and serine, all of which are likely to reduce immunogenicity, and used phage display to rapidly assess the integrity of important conformational epitopes. We report that replacement of 5 residues (residues 196, 197, 200, 201, and 204) within 3D7 C1-L with serine can generate a more cross-reactive antibody response and increase relative growth inhibition of a heterologous parasite line.
MATERIALS AND METHODS
Monoclonal antibodies.
This study utilized the reduction-sensitive, growth-inhibitory MAbs 1F9 (17, 33) and 4G2 (34) and the reduction-insensitive, noninhibitory MAb 5G8 (33). Generation of MAbs 1F9 and 5G8 was performed as previously described (33). MAb 4G2 was a kind gift from Clemens Kocken, Biomedical Primate Research Centre, Rijswijk, The Netherlands.
Mutagenesis of AMA1.
Five residues in loop Id (residues 196, 197, 200, 201, and 206) of AMA1 were mutated to alanine, glycine, or serine essentially as described previously (35). Briefly, codon-optimized 3D7 and FVO AMA1 genes were inserted into the phage display vector pHENH6, and single-stranded, uracilated DNA was produced. Oligonucleotides (GeneWorks) incorporating the desired substitutions were annealed to this single-stranded DNA and used to prime the synthesis of covalently closed, double-stranded DNA. Following transformation of Escherichia coli TG1 cells, colonies harboring AMA1 mutants were identified by DNA sequencing (Australian Genome Research Facility).
Phage display.
Phage displaying AMA1 (residues 25 to 546) with a C-terminal Myc tag were prepared essentially as described previously (36). Briefly, TG1 cells harboring the pHENH6 vector with the desired ama1 gene inserted were cultured to turbidity. Following the addition of M13K07 helper phage (GE Healthcare), the starter culture was transferred into 200 ml of medium and incubated at 37°C for approximately 16 h. Phage were then precipitated with a polyethylene glycol-NaCl solution (30% [wt/vol] polyethylene glycol 8000 [Sigma], 2.6 M NaCl) and harvested by centrifugation. The phage pellet was then resuspended in phosphate-buffered saline (PBS).
Phage enzyme-linked immunosorbent assay (ELISA).
MAbs were diluted to 2 μg/ml in coating buffer (15 mM Na2CO3, 34 mM NaHCO3 [pH 9.6]) and immobilized on a 96-well microtiter plate (Maxisorp; Nunc). Plates were washed with PBS to remove unbound protein and blocked with 10% skim milk powder in PBS. Phage displaying AMA1 (residues 25 to 546) were diluted in PBS–0.05% Tween 20 (PBST; Sigma) and applied to the wells in duplicate. After 1 h of incubation, unbound phage were removed by washing with PBST, and bound phage were detected with peroxidase-conjugated anti-M13 antibodies (1:5,000 dilution; GE Healthcare). Binding was visualized by using 3,3′,5,5′-tetramethylbenzidine (Sigma), and the absorbance was read at 450 nm.
Recombinant protein expression and purification.
AMA1 was expressed and purified essentially as described previously (7). Briefly, the codon-optimized genes encoding wild-type (wt) and mutant forms of 3D7 and FVO AMA1 (residues 25 to 546) were inserted into the expression vector pQE9 (Qiagen) and introduced into E. coli SG13009 cells. AMA1 expression was induced with isopropyl-β-d-thiogalactopyranoside (IPTG), and after 3 h, cells were harvested by centrifugation. Pellets were solubilized in guanidine buffer. An N-terminal 6×His tag facilitated capture of AMA1 by Ni-nitrilotriacetic acid-coupled agarose (Qiagen). Eluted AMA1 was refolded in vitro and further purified by anion-exchange and size exclusion chromatography.
Preparation of rabbit antisera.
New Zealand White rabbits were immunized intramuscularly with 500 μl of AMA1 formulated in Montanide ISA-720 (3 parts antigen in PBS to 7 parts adjuvant [vol/vol]; Seppic) to a final concentration of 100 to 200 μg/ml. Rabbits were immunized on days 0, 28, and 70, and sera were collected on days 42 and 84 (bleeds 1 and 2, respectively) and on either day 98 or 140 (kill-bleed). Three rabbits per group were immunized with individual forms of AMA1, and four to six rabbits per group were immunized with combined forms of AMA1.
IgG was purified from whole sera by using protein G-Sepharose (GE Healthcare). A total of 4 ml of sera diluted 1 in 5 in binding buffer (20 mM phosphate, pH 7) was passed twice over 3 ml of resin. The beads were washed with 5 column volumes of binding buffer, and bound IgG was eluted at low pH (0.1 M glycine, pH 2.7). The pH was immediately neutralized with phosphate buffer. The sample was buffer exchanged into PBS by using either dialysis or Amicon Ultra-15 centrifugal filter units (30 molecular weight cutoff [MWCO]; Millipore) and was concentrated by using Amicon Ultra-15 centrifugal filter units. IgG was then sterile filtered and stored at 4°C until use.
Antibody ELISA.
AMA1 was diluted to 2 μg/ml in PBS and immobilized on a 96-well microtiter plate (Maxisorp; Nunc). Coating was allowed to occur overnight at 4°C. Unbound protein was removed by washing with PBST. Sera or MAbs were diluted to the appropriate concentration in 5% skim milk powder in PBS and applied to the wells in duplicate. Following 1.5 h of incubation, unbound antibodies were removed by washing with PBST. The appropriate peroxidase-conjugated secondary antibody (anti-rabbit [1:1,000; GE Healthcare], anti-mouse [1:1,000; Jackson ImmunoResearch], or anti-rat [1:2,500; Jackson ImmunoResearch]) was diluted in 5% skim milk powder in PBS and added to the wells. Following 1 h of incubation, excess secondary conjugate was removed by washing. Binding was visualized by the addition of 150 μl/well of ABTS [2,2′-azino-bis(3-ethylbenzthiazoline-6-sulfonic acid)] substrate (0.98 mM ABTS, 0.98 mM citric acid, and 0.003% H2O2). After 45 min, the absorbance was read at 414 nm.
Competition ELISA.
Competition ELISAs were carried out to more sensitively assess the fine specificity of the antibody response. Rabbit sera were initially titrated on AMA1, as detailed above, and the serum dilution resulting in an optical density (OD) of 3.5 to 3.8 (i.e., the upper section of the linear part of the curve) was determined. Sera were then prepared at 2-fold the desired dilution and mixed 1:1 with increasing concentrations of the appropriate forms of AMA1 (competitor antigens). The typical final concentration range of the competing antigen was 0.316 to 31.6 μg/ml. This mixture was incubated for 1 h before being applied to wells coated with AMA1 (2 μg/ml). Binding of sera to immobilized AMA1 was then detected as indicated above. Data were displayed as a percentage of maximal binding, with maximal binding being indicated by the no-inhibitor control wells. To enable quantitative comparison of the competition curves, GraphPad Prism software was used to plot a 3-parameter sigmoidal curve through the data, and the predicted minimal value was determined (26). This “residual binding” reflects the proportion of antibodies captured by the immobilized target protein that do not react with a given competitor antigen.
Parasite growth inhibition assays.
P. falciparum growth inhibition assays (GIAs) were performed as previously described (21, 37). Briefly, synchronized early-trophozoite-stage parasites were adjusted to 0.1% parasitemia and 2% hematocrit. Five microliters of stock antibody or peptide was added to 45 μl of infected red blood cells and mixed to generate a final culture volume of 50 μl. Parasites were allowed to develop through two cycles of erythrocyte invasion for 72 h at 37°C. Early-trophozoite-stage parasites formed after the second round of invasion were fixed for 1 h at room temperature by the addition of glutaraldehyde (ProSciTech) to a final concentration of 0.25% (vol/vol). After fixation, parasites were washed in human tonicity PBS (HTPBS) and stained with 10× SYBR green dye (Invitrogen), and 5 × 105 red blood cells were counted per well by using a BD FACSCantoII flow cytometer. Fluorescence-activated cell sorter (FACS) counts were analyzed by using FlowJo (version 6.4.7) software (Treestar). Percent growth inhibition was calculated as [1 − (parasitemia in test well/mean parasitemia in preimmunization rabbit controls wells)] × 100. All GIAs were run in a 96-well-plate format, with each IgG being tested in duplicate wells. Parasite growth inhibition is represented as the combined mean of duplicate wells from a single assay or as percent inhibition relative to another parasite line.
To calculate parasite inhibition of the heterologous parasite line (W2mef) as a percentage of that of the homologous parasite line (3D7 or FVO), we used an IgG concentration that could induce between 40 and 90% inhibition of the homologous parasite lines. This was done to avoid the loss of linearity and greater error associated with levels of inhibition outside this range. We also set a threshold of 20% for meaningful parasite inhibition of the heterologous parasite line. Failure of an IgG preparation to reach the minimum levels of inhibition at any of the concentrations tested led to exclusion from the analysis.
RESULTS
Analysis of phage-displayed AMA1 mutants.
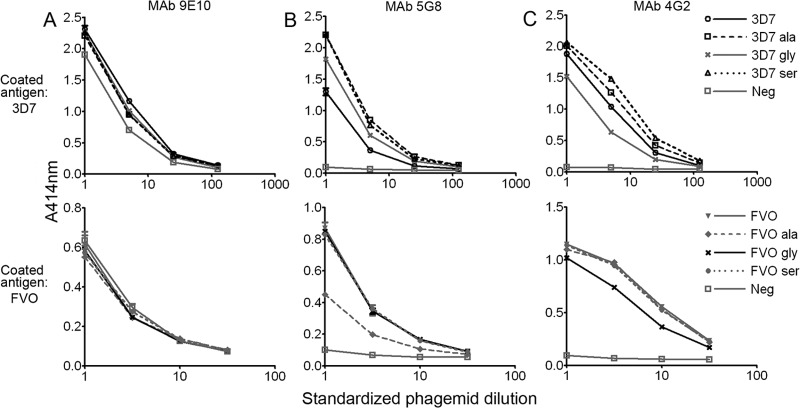
This study aimed to decrease the immunogenicity of loop Id by replacing five surface-exposed polymorphic residues (at positions 196, 197, 200, 201, and 204) with either alanine, glycine, or serine (Fig. 1). To avoid lengthy protein synthesis and purification of mutants with impaired folding ability, wt and mutant forms of 3D7 and FVO AMA1 were first expressed on the surface of phage. Protein expression at the phage surface was standardized by equalizing MAb binding to a C-terminal Myc tag (Fig. 2A). Binding to MAb 5G8, which recognizes a linear epitope in the prodomain of AMA1 (33), indicated that some N-terminal degradation of two AMA1 phage preparations was present: 3D7 wt and FVO containing serine substitutions (FVO Ser) (Fig. 2B). However, this degradation had a minimal impact on the conserved, conformational epitope recognized by the inhibitory MAb 4G2 (Fig. 2C) (34, 38). In contrast, both the 3D7 Gly and FVO Gly mutants showed reduced reactivity with MAb 4G2 compared with the wt, indicating that the introduction of glycine at these 5 positions hindered folding ability. For this reason, the glycine mutants were not produced as purified recombinant proteins.
FIG 1.
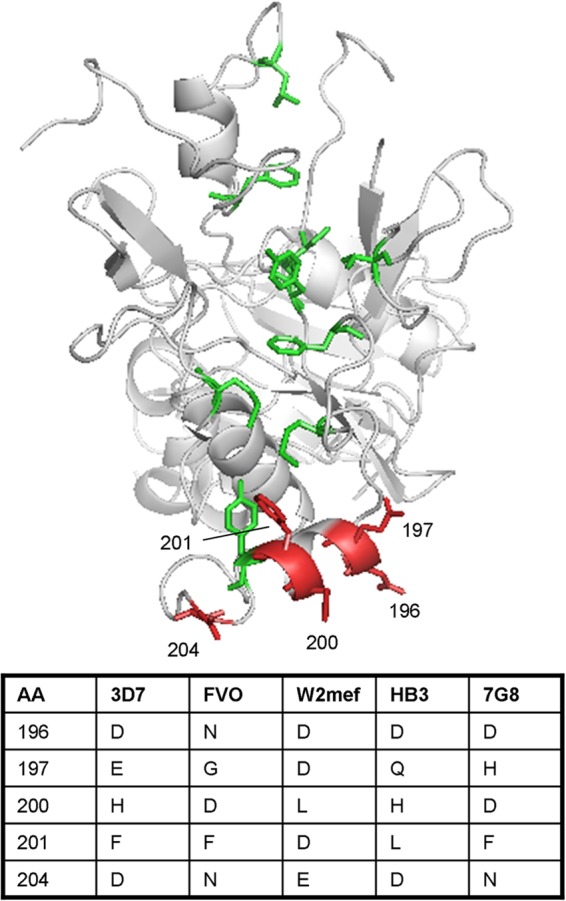
Mutagenesis of loop Id. Shown is the structure of AMA1 (14) (PyMOL software [http://www.pymol.org/]) showing the hydrophobic pocket (green) and the five residues in loop Id targeted for mutagenesis (red). The identities of these residues in the allelic forms of AMA1 used in this study are also indicated.
FIG 2.
MAb reactivity of AMA1 displayed on the surface of phage. Phage-displayed wt or mutant forms of 3D7 and FVO AMA1 were allowed to interact with MAbs 9E10 (A), 5G8 (B), and 4G2 (C) immobilized on a microtiter plate. The average data from duplicate wells are shown, and error bars indicate ranges. MAb 9E10 binds the Myc tag C terminal to phage-displayed AMA1, MAb 5G8 binds a linear epitope in the AMA1 prodomain, and MAb 4G2 binds a conserved, conformational epitope in AMA1.
Synthesis and characterization of recombinant AMA1.
Six recombinant forms of AMA1 (residues 25 to 546; N-terminal 6×His tag) were produced by using our established procedure for synthesis, refolding, and purification of AMA1: 3D7, 3D7 Ala, 3D7 Ser, FVO, FVO Ala, and FVO Ser. The final products were highly pure, as indicated by silver staining after SDS-PAGE (Fig. 3A). Western blotting showed that MAb 5G8, which reacts with a linear determinant in AMA1, showed strong reactivity with both the reduced and nonreduced antigens (Fig. 3B). All six proteins reacted with MAb 4G2 only under nonreducing conditions, consistent with the conformational nature of the 4G2 epitope (34) (Fig. 3C).
FIG 3.
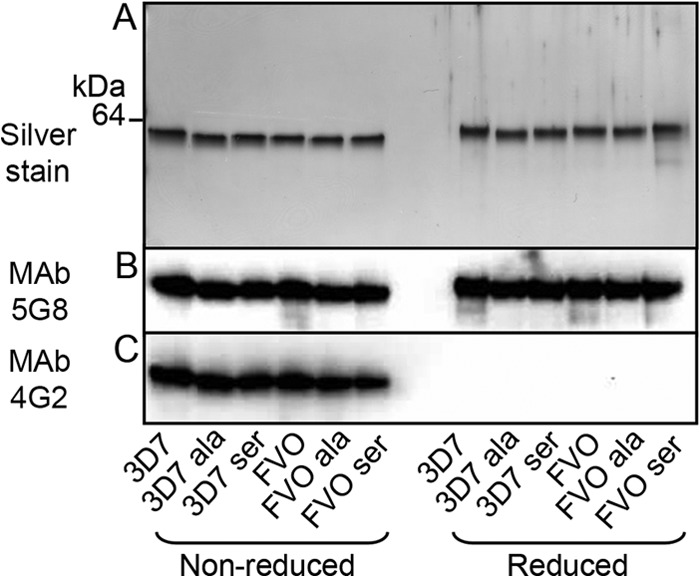
wt and mutant forms of 3D7 and FVO AMA1 expressed recombinantly are highly pure and react with MAbs 4G2 and 5G8 by Western blotting. (A) Twenty nanograms of each protein was subjected to SDS-PAGE followed by silver staining. (B and C) Two hundred nanograms of each protein was transferred onto a polyvinylidene difluoride membrane and probed with MAb 5G8 (B) or MAb 4G2 (C).
The five polymorphic residues selected for mutagenesis make a large contribution to the epitope recognized by the strain-specific, inhibitory MAb 1F9, and this epitope is a target of naturally acquired human antibodies (17, 18). Consistent with this, 1F9 bound well to wt 3D7 AMA1 but did not bind to the 3D7 mutants or any of the FVO variants produced (see Fig. S1A in the supplemental material). In contrast, the reactivity of all proteins with MAb 4G2 was almost identical, indicating that the conserved, conformation-dependent epitope recognized by this MAb was not significantly affected by mutagenesis of loop Id (see Fig. S1B in the supplemental material).
To assess folding on a more global level, each protein was also tested for binding to conformation-sensitive polyclonal sera raised against 3D7 AMA1 (see Fig. S1C in the supplemental material) or FVO AMA1 (see Fig. S1D in the supplemental material). Reactivity of the 3D7 mutants with the homologous polyclonal sera was slightly decreased compared with that of the wt antigen; however, this can most likely be attributed to disruption of epitopes incorporating the mutated residues rather than aberrant folding. As expected, each conformation-specific serum showed reduced reactivity with both wt and mutant forms of the heterologous antigen.
Generation of anti-AMA1 sera.
Since antibody reactivity data indicated that the AMA1 mutants were correctly folded, all six forms of recombinant AMA1 were used to immunize rabbits. Blood was collected 2 weeks after the first boost (bleed 1), 2 weeks after the second boost (bleed 2), and 10 weeks after the second boost (kill-bleed; day 140). The relative titer of each bleed on the corresponding wt antigen was determined by ELISA (see Fig. S2 in the supplemental material). In most cases, the titers of anti-AMA1 antibodies were similar in bleeds 1 and 2, whereas, surprisingly, lower antibody titers were seen in the kill-bleeds. All further analyses were carried out using bleed 2. There was no clear overall reduction in the response generated against the wt antigen when rabbits were immunized with 3D7 Ala, FVO Ala, or FVO Ser compared with the antibody response induced by the wt antigen itself. However, in 2/3 rabbits immunized with 3D7 Ser, a reduced response to 3D7 wt was observed. Immunization of more rabbits would be required to determine if this difference is statistically significant.
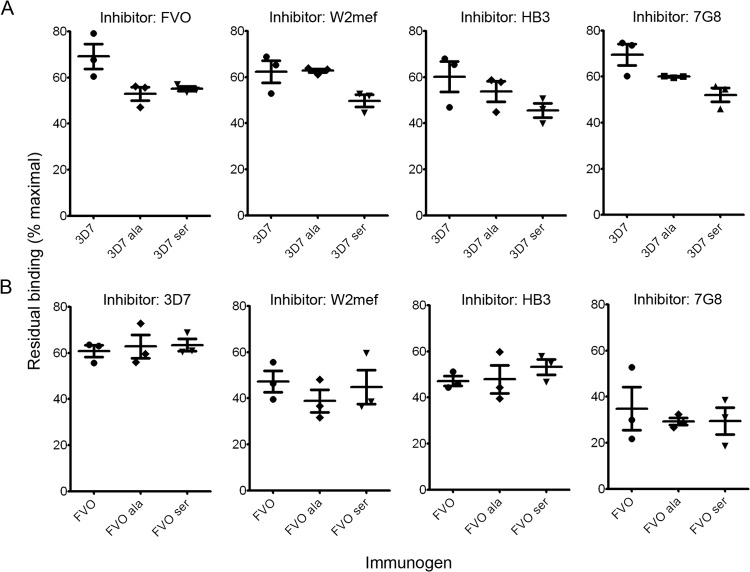
Analysis of the antibody response to loop Id.
To analyze the overall antibody response to loop Id in rabbits immunized with wt AMA1, competition ELISAs were used. In these assays, we tested the ability of wt and mutant recombinant AMA1 proteins to inhibit the binding of antibodies to immobilized wt AMA1. Since the mutant proteins contain five substitutions within loop Id, subsequent loss of competitor efficacy indicates decreased binding of antibodies that target this region and is reflective of the loop Id antibody response. The competition ELISAs revealed that the corresponding AMA1 mutants were less potent when inhibiting serum raised against 3D7 wt compared with FVO wt, suggesting that loop Id is more dominant when 3D7 wt is the immunogen (Fig. 4A). To enable quantitative comparison of the antibody responses to this region, the predicted minimal values (residual binding displayed as a percentage of the maximal signal) for each competitor antigen were plotted for all rabbits immunized with AMA wt (Fig. 4B). Higher residual binding (i.e., less competition) for a given competitor suggests that it is reactive with a smaller subset of anti-AMA1 antibodies. The response to loop Id was consistently higher in all three rabbits immunized with 3D7 AMA1, as evidenced by high residual binding of 3D7 Ala and Ser (Fig. 4B, immunogen: 3D7) compared with results from the same experiment in the FVO backbone (Fig. 4B, immunogen: FVO).
FIG 4.
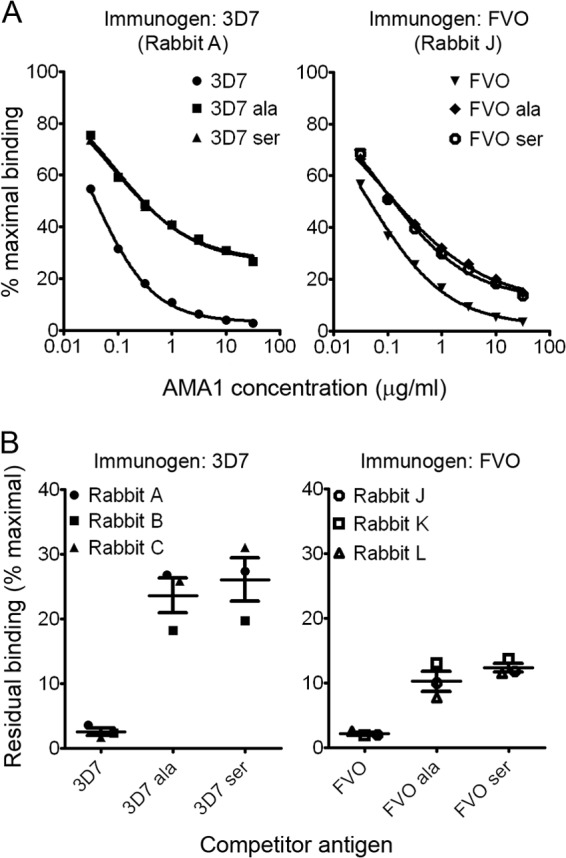
Loop Id is a more dominant target of the antibody response when 3D7 is the immunogen than when FVO is the immunogen. (A) A constant concentration of serum raised against 3D7 or FVO AMA1 was allowed to interact with the immobilized homologous antigen in the presence of increasing concentrations of soluble protein. Rabbit A represents the group immunized with 3D7 AMA1, and rabbit J represents the group immunized with FVO AMA1. The average data from duplicate wells are shown, and error bars indicate ranges. (B) A sigmoidal curve was fitted to the competition data by using a 3-parameter model. The average predicted minimal values (residual binding displayed as percent maximal binding) from two independent experiments are reported for each rabbit. The means ± standard errors of the means of data for each immunization group are also shown.
Generation of a mutant-specific antibody response.
To determine if immunization of rabbits with mutated AMA1 generated mutant-specific antibodies, we evaluated the ability of wt and mutant forms of AMA1 to block each serum from binding to its immunogen and plotted the residual binding (see Fig. S3 in the supplemental material). Higher residual binding of AMA1 wt reflects the presence of a greater proportion of antibodies specific for the mutant form. Although a mutant-specific antibody response was usually present, in most rabbits, this was lower than the response induced by the wt antigens to wt loop Id. Interestingly, the mutant-specific antibody response appeared to be largely independent of the amino acid substitution, suggesting that there may be a structural feature common to the mutants that is absent in the wt antigen.
Analysis of the antibody response to cross-reactive epitopes.
To establish whether limiting the induction of antibodies to loop Id would increase the proportion of antibodies to more cross-reactive epitopes, competition assays using five different allelic forms of recombinant AMA1 (3D7, FVO, W2mef, HB3, and 7G8) as the competitor antigen were used. Residual binding was then plotted for all rabbits (Fig. 5). In rabbits immunized with 3D7 wt, heterologous forms of AMA1 were poor inhibitors of antibody binding to the immobilized antigen, as evidenced by high residual binding (Fig. 5A). This indicates that anti-3D7 wt sera are highly strain specific. Following immunization with 3D7 Ala and 3D7 Ser mutants, a trend toward decreased residual binding values for heterologous antigens was observed, indicating some broadening of antibody reactivity. Although the difference was not dramatic, this illustrates that the replacement of just five residues in 3D7 AMA1 can alter the specificity of the antibody response, leading to more cross-reactive antibodies. Compared with 3D7 wt, anti-FVO wt sera were more cross-reactive with the allelic forms tested, as shown by the lower residual binding of heterologous antigens when competing with these sera (Fig. 5B). Immunization with mutant forms of FVO AMA1 did not further improve cross-strain recognition.
FIG 5.
Immunization with mutant forms of 3D7 AMA1 increases the antibody response to conserved epitopes. Constant concentrations of sera raised against wt or mutant forms of AMA1 were allowed to interact with 3D7 (A) or FVO (B) AMA1 in the presence of increasing concentrations of different allelic forms of AMA1. The average residual binding determined from two independent experiments is reported for each rabbit. The means ± standard errors of the means of data for each immunization group are also shown.
Inhibition of parasite growth: individual antigen immunizations.
To determine if increased cross-reactivity corresponded to more effective inhibition of a heterologous parasite line, we tested the ability of purified IgG from each rabbit to inhibit growth of 3D7 and FVO parasites (Fig. 6; see also Table S1 in the supplemental material). Although the overall inhibition levels were higher for the anti-wt antibodies than for the antimutant antibodies, we observed a trend toward improved relative inhibition of the heterologous parasite line when a mutant form of 3D7 (but not FVO) AMA1 was the immunogen. However, group sizes were insufficient for statistical analysis, and low overall inhibition (<40% inhibition of the homologous parasite line and <20% inhibition of the heterologous parasite line) necessitated the exclusion of one rabbit from the 3D7 Ala group and two rabbits from the 3D7 Ser group. To address this, and to determine the best possible combination of wt and mutant antigens for generating a cross-reactive antibody response, an expanded study incorporating larger group sizes, a modified immunization regime, and concurrent immunization with two antigens was carried out.
FIG 6.
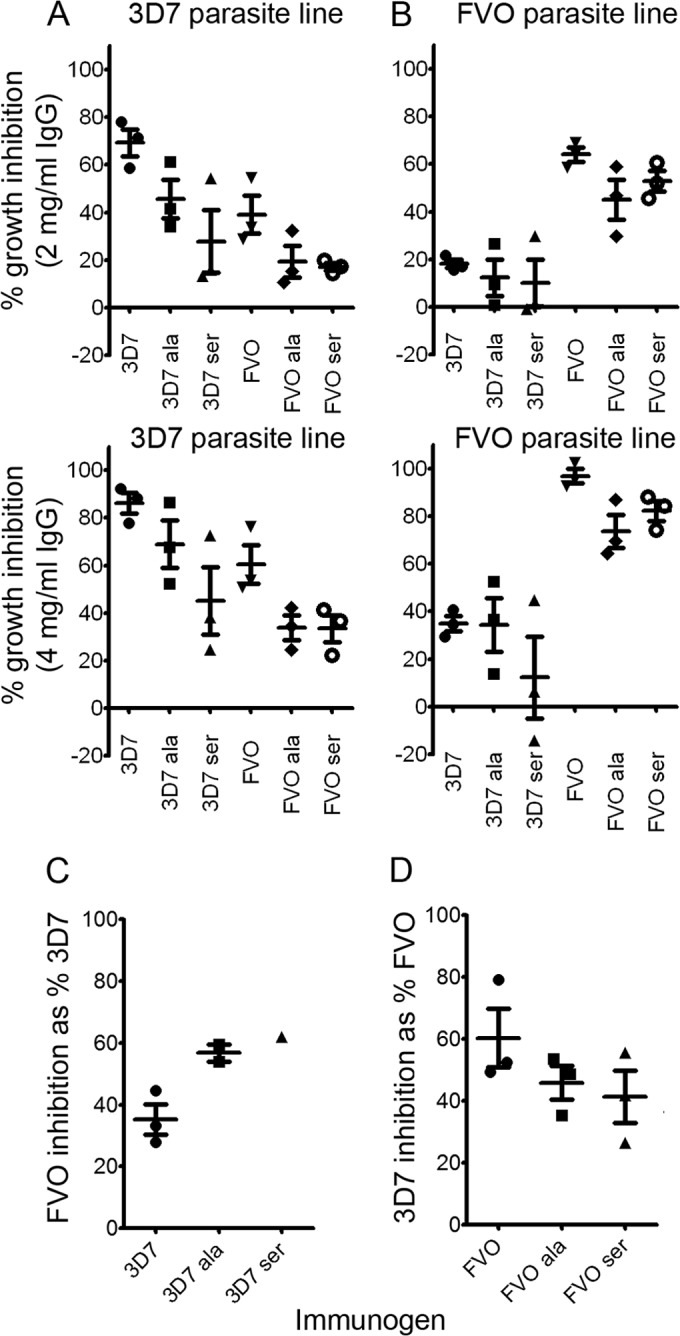
Effect of purified IgG from rabbits immunized with individual antigens on growth of the 3D7 and FVO parasite lines. (A and B) Inhibition of growth of the 3D7 (A) and FVO (B) parasite lines mediated by different concentrations of IgG raised against wt and mutant forms of AMA1. (C) Inhibition of the FVO parasite line expressed as a percentage of inhibition of the 3D7 parasite line. (D) Inhibition of the 3D7 parasite line expressed as a percentage of inhibition of the FVO parasite line. For calculation of relative inhibition levels (C and D), an IgG concentration resulting in 40 to 90% inhibition of the homologous parasite line and >20% inhibition of the heterologous parasite line was used. Two rabbits in the 3D7 Ser group and one rabbit in the 3D7 Ala group were excluded from this analysis due to low overall inhibition levels (<40%). In all cases, the averages of data from duplicate wells from a single representative experiment are reported for each rabbit. The means ± standard errors of the means of data for each immunization group are shown where appropriate.
Immunization with combinations of 3D7 and FVO AMA1.
Groups of six rabbits were immunized with one of five different antigen combinations. Since the individual antigen immunizations showed that, in contrast to 3D7, mutagenesis of FVO did not achieve the desired outcome, mutated forms of 3D7 AMA1 were combined with wt FVO (3D7 Ala/FVO and 3D7 Ser/FVO immunization groups). However, it was also possible that a synergistic effect could be achieved by combining two engineered forms of AMA1. Therefore, we also assessed formulations that included mutant versions of both 3D7 and FVO AMA1 (3D7 Ala/FVO Ala and 3D7 Ser/FVO Ser immunization groups). The final group included both wt antigens for comparison (3D7/FVO immunization group). One rabbit from each of the 3D7 Ala/FVO and 3D7 Ala/FVO Ala groups was excluded due to illness or injury. Rabbits were immunized with a total of 100 μg of combined antigen per dose. Sera were collected at the same intervals outlined as described above for the rabbit study, except that the kill-bleed sample was taken on day 98. There was a trend toward a decreased overall response to AMA1 when a mutant was included in the formulation (data not shown).
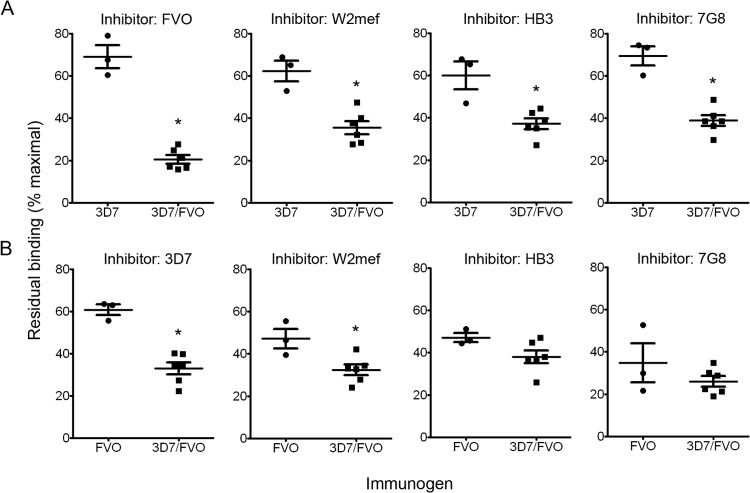
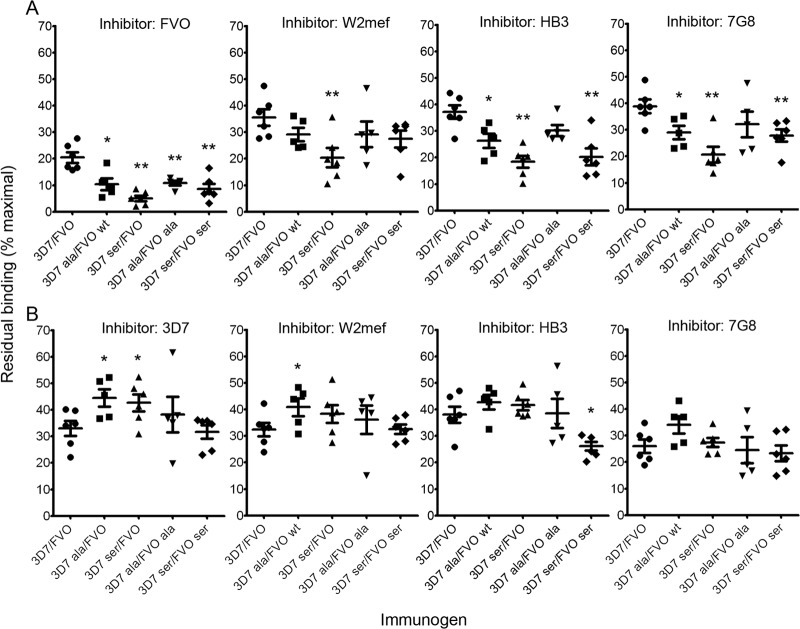
The residual levels of antibody binding measured in competition ELISAs were used to compare responses to cross-reactive epitopes when rabbits were immunized with different combinations of antigens. Relative to a single allelic form, immunization with combinations of wt AMA1 resulted in dramatically improved cross-strain recognition (Fig. 7). However, it was of particular interest to determine if cross-reactivity could be increased further by immunization with combinations that included one or more AMA1 mutants. When assessing the antibody response to 3D7, decreased residual binding values when heterologous competitor antigens were tested indicated an increased response to cross-reactive epitopes when the immunogen included one or more loop Id mutant (Fig. 8A). This was most striking for the 3D7 Ser/FVO group, which exhibited significantly greater cross-reactivity (compared with the wt combination group) with all allelic forms tested (FVO, W2mef, HB3, and 7G8) (P < 0.01). The additional inclusion of an FVO mutant did not further improve cross-reactivity (P > 0.05). When examining the anti-FVO antibody response (Fig. 8B), a significant improvement in cross-reactivity was observed on only one occasion (3D7 Ser/FVO Ser immunization group with HB3 competitor antigen). However, the inclusion of a 3D7 mutant in some cases significantly decreased the cross-reactivity of the FVO response (3D7 Ala/FVO immunization group with 3D7 and W2mef competitor antigens and 3D7 Ser/FVO immunization group with 3D7 competitor antigen). These data suggest that the inclusion of a mutant form of 3D7 AMA1, in particular 3D7 Ser, in a combined formulation is sufficient to elicit a more cross-reactive response to 3D7 AMA1. However, the additional inclusion of FVO AMA1 mutated at loop Id did not consistently shift the antibody response to more cross-reactive epitopes.
FIG 7.
Comparison of immune responses to conserved epitopes in rabbits immunized with individual or combined antigens. Constant concentrations of sera raised against a single wt antigen or combined wt antigens were allowed to interact with immobilized AMA1 in the presence of increasing concentrations of soluble protein. The average residual binding calculated from at least two independent experiments when 3D7 (A) or FVO (B) AMA1 was the target antigen is shown for each rabbit. The means ± standard errors of the means of data for each immunization group are shown. *, P < 0.05, determined by a Mann-Whitney test (one tailed) comparing each single-antigen immunization group with the combined-wt-antigen immunization group.
FIG 8.
Antibody response to conserved epitopes in rabbits immunized with antigen combinations. Constant concentrations of sera raised against combinations of wt and mutant AMA1 were allowed to interact with immobilized AMA1 in the presence of increasing concentrations of soluble protein. The average residual binding calculated from at least four independent experiments when 3D7 (A) or FVO (B) AMA1 was the target antigen is shown for each rabbit. The means ± standard errors of the means of data for each immunization group are also shown. *, P < 0.05; **, P < 0.01 (determined by a Mann-Whitney test [one tailed] comparing each mutant group with the corresponding wt group).
Inhibition of parasite growth: combined antigen immunizations.
To determine whether inclusion of a mutant form of AMA1 in a dual-antigen formulation would increase the induction of cross-reactive inhibitory antibodies, purified IgGs from individual rabbits were tested for their ability to inhibit growth of the 3D7, FVO, and W2mef parasite lines. We were unable to generate reliable data from further parasite lines due to insufficient amounts of IgG. When growth inhibition of W2mef parasites was assessed relative to inhibition of the 3D7 parasite line, a significant increase (P < 0.01) in cross-strain inhibition in the 3D7 Ser/FVO group relative to the wt group was consistently observed (Fig. 9A; see also Table S2 in the supplemental material). This indicates that the increased proportion of cross-reactive antibodies observed by ELISA corresponds, at least partly, to cross-reactive inhibitory antibodies. In contrast, immunization with loop Id mutants did not result in enhanced inhibition of the W2mef parasite line relative to FVO (Fig. 9B), consistent with the ELISA data. Since this study was primarily concerned with assessing the vaccine potential of each antigen combination, we did not test whether combining antibodies elicited by individual antigens would enable the same level of cross-inhibition to be reached as that achieved when the vaccine formulation incorporated two antigens.
FIG 9.
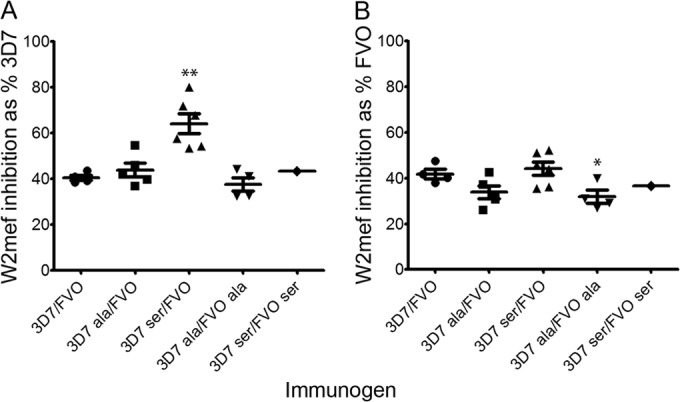
Relative growth inhibition of heterologous versus homologous parasite lines. Shown is IgG-mediated growth inhibition of the W2mef parasite line relative to 3D7 (A) and FVO (B) parasites. The average growth inhibition calculated from duplicate wells from a representative experiment is reported for each rabbit. The means ± standard errors of the means of data for each immunization group are shown where appropriate. IgG concentrations resulting in 40 to 90% inhibition of the 3D7 and FVO parasite lines and >20% inhibition of W2mef parasites were used for this analysis. Failure to meet these parameters resulted in exclusion of two rabbits from the 3D7/FVO group, one rabbit from the 3D7 Ala/FVO Ala group, and five rabbits from the 3D7 Ser/FVO Ser group. *, P < 0.05; **, P < 0.01 (determined by a Mann-Whitney test [one tailed] comparing each combination of mutants with the wt immunization group).
It was evident that the overall inhibition of 3D7 parasites was impaired when 3D7 Ala or Ser was included in the immunogen (see Fig. S4A in the supplemental material). Similarly, inclusion of FVO Ala or Ser resulted in decreased overall inhibition of FVO parasite growth (see Fig. S4B in the supplemental material). This suggests that the overall inhibitory response is reduced when a mutant is included in the formulation, and this is consistent with the observed reduction in anti-AMA1 titers.
DISCUSSION
This study aimed to increase the proportion of broadly neutralizing anti-AMA1 antibodies by dampening the response to the highly variable loop Id. It was found that immunization with mutated forms of 3D7 AMA1, either individually or combined with FVO, induced a more cross-reactive repertoire of 3D7 AMA1-specific antibodies than did the corresponding wt antigen. We also showed that antibodies raised against the 3D7 Ser/FVO wt combination of AMA1 were significantly more effective at inhibiting the relative growth of a heterologous parasite line (P < 0.01). However, the wt antigens were more immunogenic and inhibitory against the homologous parasite line. Consequently, induction of a more broadly cross-reactive antibody response with mutated 3D7 AMA1 may come at the cost of a lower level of response against parasites bearing the 3D7 AMA1 loop Id haplotype; however, it should be noted that AMA1 alleles of this type have represented a minority of parasites in many populations studied (8, 39).
Mutation of highly polymorphic residues to decrease their immunogenicity (immunodampening) is one strategy for overcoming the extreme polymorphism of some vaccine candidates. In a previous report using FVO, seven polymorphic residues identified as being important for escape of strain-specific inhibitory antibodies (residues 187, 190, 196, 197, 200, 204, and 206) were mutated to alanine, with limited success in circumventing diversity. We took a more conservative approach to mutagenesis, targeting five surface-exposed, polymorphic residues within loop Id (residues 196, 197, 200, 201, and 204) of both FVO and 3D7 AMA1. Loop Id forms a two-turn α-helix in the Plasmodium falciparum AMA1 structures solved to date (14, 17, 40). However, this helix may not be present in all isolates, since some allelic forms of AMA1 (including FVO) contain the residue combination Gly197/Asp200, which is predicted to be helix destabilizing (41). Differences in secondary structure may enhance the ability of this region to escape strain-specific inhibitory antibodies. We therefore replaced each target residue with alanine, serine, or glycine. Each of these mutations is likely to exhibit low immunogenicity, but replacement with glycine or serine may preclude helix formation in loop Id.
Mutated forms of AMA1 were first displayed on the surface of phage to enable rapid exclusion of variants with unfavorable folding characteristics. Alanine and serine substitutions were well tolerated, but replacement with glycine resulted in impaired folding, perhaps reflecting its greater propensity to be buried in folded proteins, and no further work was done with this variant. Antibody reactivity of recombinant proteins confirmed that alanine or serine substitution minimized disruption to the native fold, and these antigens were used in immunization studies.
Since a combined 3D7/FVO formulation has progressed to phase II clinical trials (30), we sought to determine whether including mutant forms of 3D7 or FVO AMA1 in a combined vaccine would confer an advantage over combining wt antigens. Of the combinations tested, 3D7 Ser/FVO wt AMA1 induced the most cross-reactive antibody response (P < 0.01) (Fig. 8A) and showed significantly higher relative growth inhibition of the W2mef parasite line (P < 0.01) (Fig. 9A). This is consistent with data from the single-antigen immunizations, where 3D7 Ser offered the most promise for inducing a cross-reactive antibody response (discussed below). A recent clinical trial using a 3D7 single-allele formulation confirmed the importance of C1-L and indicated that residue 197 (mutated in this study) is the most important determinant of allele-specific protection (8, 19). We have shown here that mutagenesis of polymorphic residues within 3D7 C1-L can induce a broader inhibitory antibody response when included in a combination vaccine. Given the demonstrated importance of this region in clinical protection, inclusion of a mutant form of 3D7 may reduce the number of alleles required to achieve broad efficacy in a multiallele vaccine.
There was a trend toward a decreased AMA1 titer (data not shown) and reduced overall parasite inhibition (see Fig. S4 in the supplemental material) following inclusion of a mutant antigen in a biallelic formulation. While optimization of the immunization regime may overcome this to some extent, it does raise the possibility that relative improvements in cross-reactive epitope recognition may simply reflect a reduced response to loop Id, without any change in the repertoire of cross-reactive antibodies. However, when the response to different target antigens was measured following immunization with AMA1 mutants, different effects were observed. For example, the same antigen combination induced an anti-3D7 antibody response that was more cross-reactive with FVO and an anti-FVO response that was less cross-reactive with 3D7 than the antibody response generated against the combined wt antigens (Fig. 8). This suggests that the fine specificity of the cross-reactive antibody component is altered; however, further analyses will be required to address this issue in more detail.
Consistent with the combined antigens, single-allele immunizations with mutated 3D7 AMA1 broadened the overall antibody response, and there was some evidence of improved inhibitory activity against the FVO parasite line (Fig. 5A and 6C). However, when wt FVO was the immunogen, the response was more cross-reactive than the 3D7 response, and immunization with mutant forms of FVO did not further enhance this response (Fig. 5B and 6D). Since we found that a smaller proportion of antibodies target FVO loop Id than 3D7 loop Id (Fig. 4), this result is not unexpected. Furthermore, this is consistent with a previous report where substitution of seven C1 residues in FVO was found to increase cross-reactivity only when analysis was carried out at the domain level, and broader parasite-inhibitory activity was not observed (32). Although the strategy employed here with the FVO allele did not offer any advantages over wt FVO, it is possible that different subsets of polymorphic residues are more important in dictating the strain specificity for this allelic form. Indeed, analysis of escape determinants in invasion inhibition assays indicated that the relative importance of polymorphic clusters varies depending on the immunogen/parasite combination (21, 27). Previous studies found that polymorphisms within the loop Id region correlated with the cross-inhibitory activity of anti-3D7 antibodies against parasites with different AMA1 alleles (21), and naturally acquired human antibodies to this region of 3D7 correlated with growth-inhibitory activity (18), again suggesting the importance of this region of 3D7 as an antibody target and highlighting the importance of polymorphisms in this region for antibody escape.
A mutant-specific antibody response that was largely independent of substitution was generated by immunization with 3D7 Ala, 3D7 Ser, and FVO Ala (see Fig. S3 in the supplemental material). Although antibody reactivity suggested that mutant proteins were correctly folded, mutagenesis appeared to generate a surface feature common to the mutants that was not present in the wt antigen. Subtle localized changes in structure can be difficult to identify but have a significant effect on the fine specificity of antibodies induced by the antigen. The recently reported structure of AMA1 in complex with a peptide corresponding to its native ligand, RON2, revealed that AMA1 undergoes a conformational change upon ligand binding (42), suggesting that this region of AMA1 is amenable to structural rearrangement. The possibility that structural differences are making some contribution to the perceived dominance of loop Id cannot be ruled out. In rabbits immunized with FVO Ser, there was a minimal mutant-specific antibody response, perhaps reflecting a molecular surface that more closely resembles that of the native antigen. Along with structural analysis of the antigens, investigating changes in the proportion of reduction-sensitive antibodies raised against the mutant forms of AMA1 may shed light on this area.
The number of AMA1 alleles found among parasites circulating in areas where malaria is endemic is enormous, but the diversity of epitopes targeted by inhibitory antibodies is less than expected from the sequence diversity (21). Recent studies suggest that a combination of four or five different alleles may be sufficient to overcome this diversity in AMA1 (21, 23, 27) and that allelic variation may not be an insurmountable hurdle to the development of an AMA1-based vaccine. Here, we have shown that mutagenesis of five residues within 3D7 AMA1 is sufficient to induce a more cross-reactive antibody response. Furthermore, inclusion of an engineered form of AMA1 in a biallelic formulation facilitates broader reactivity and inhibitory activity, implying that this approach may reduce the number of antigens required to achieve broad protection in the field and providing an important proof of concept. Affordability constraints dictate that it will be advantageous to minimize the number of allelic forms included in a vaccine, and whether one or more of these forms should be mutagenized to dampen the antibody response to dominant strain-specific epitopes should therefore be examined further.
Supplementary Material
ACKNOWLEDGMENTS
We thank Jana Yip for performing preliminary binding studies. We also thank Clemens Kocken, Biomedical Primate Research Centre, Rijswijk, The Netherlands, for MAb 4G2.
Funding was provided by the National Institutes of Health (NIH) (grant R01AI59229 to M.F.), the National Health and Medical Research Council of Australia (senior research fellowship, project grant, and Infrastructure for Research Institutes Support Scheme grant to J.G.B.), the Australian Research Council (future fellowship to J.G.B.), a Victorian State Government operational infrastructure support grant, the PATH Malaria Vaccine Initiative, and the U.S. Agency for International Development.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Published ahead of print 25 August 2014
Supplemental material for this article may be found at http://dx.doi.org/10.1128/IAI.02061-14.
REFERENCES
- 1.Richards JS, Beeson JG. 2009. The future for blood-stage vaccines against malaria. Immunol. Cell Biol. 87:377–390. 10.1038/icb.2009.27. [DOI] [PubMed] [Google Scholar]
- 2.Bejon P, Lusingu J, Olotu A, Leach A, Lievens M, Vekemans J, Mshamu S, Lang T, Gould J, Dubois MC, Demoitie MA, Stallaert JF, Vansadia P, Carter T, Njuguna P, Awuondo KO, Malabeja A, Abdul O, Gesase S, Mturi N, Drakeley CJ, Savarese B, Villafana T, Ballou WR, Cohen J, Riley EM, Lemnge MM, Marsh K, von Seidlein L. 2008. Efficacy of RTS,S/AS01E vaccine against malaria in children 5 to 17 months of age. N. Engl. J. Med. 359:2521–2532. 10.1056/NEJMoa0807381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fowkes FJ, Simpson JA, Beeson JG. 2013. Implications of the licensure of a partially efficacious malaria vaccine on evaluating second-generation vaccines. BMC Med. 11:232. 10.1186/1741-7015-11-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Remarque EJ, Faber BW, Kocken CHM, Thomas AW. 2008. Apical membrane antigen 1: a malaria vaccine candidate in review. Trends Parasitol. 24:74–84. 10.1016/j.pt.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Polley SD, Mwangi T, Kocken CH, Thomas AW, Dutta S, Lanar DE, Remarque E, Ross A, Williams TN, Mwambingu G, Lowe B, Conway DJ, Marsh K. 2004. Human antibodies to recombinant protein constructs of Plasmodium falciparum apical membrane antigen 1 (AMA1) and their associations with protection from malaria. Vaccine 23:718–728. 10.1016/j.vaccine.2004.05.031. [DOI] [PubMed] [Google Scholar]
- 6.Stanisic DI, Richards JS, McCallum FJ, Michon P, King CL, Schoepflin S, Gilson PR, Murphy VJ, Anders RF, Mueller I, Beeson JG. 2009. Immunoglobulin G subclass-specific responses against Plasmodium falciparum merozoite antigens are associated with control of parasitemia and protection from symptomatic illness. Infect. Immun. 77:1165–1174. 10.1128/IAI.01129-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hodder AN, Crewther PE, Anders RF. 2001. Specificity of the protective antibody response to apical membrane antigen 1. Infect. Immun. 69:3286–3294. 10.1128/IAI.69.5.3286-3294.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thera MA, Doumbo OK, Coulibaly D, Laurens MB, Ouattara A, Kone AK, Guindo AB, Traore K, Traore I, Kouriba B, Diallo DA, Diarra I, Daou M, Dolo A, Tolo Y, Sissoko MS, Niangaly A, Sissoko M, Takala-Harrison S, Lyke KE, Wu Y, Blackwelder WC, Godeaux O, Vekemans J, Dubois MC, Ballou WR, Cohen J, Thompson D, Dube T, Soisson L, Diggs CL, House B, Lanar DE, Dutta S, Heppner DG, Jr, Plowe CV. 2011. A field trial to assess a blood-stage malaria vaccine. N. Engl. J. Med. 365:1004–1013. 10.1056/NEJMoa1008115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garg S, Alam MT, Das MK, Dev V, Kumar A, Dash AP, Sharma YD. 2007. Sequence diversity and natural selection at domain I of the apical membrane antigen I among Indian Plasmodium falciparum populations. Malar. J. 6:154. 10.1186/1475-2875-6-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osier FHA, Weedall GD, Verra F, Murungi L, Tetteh KKA, Bull P, Faber BW, Remarque E, Thomas A, Marsh K, Conway DJ. 2010. Allelic diversity and naturally acquired allele-specific antibody responses to Plasmodium falciparum apical membrane antigen 1 in Kenya. Infect. Immun. 78:4625–4633. 10.1128/IAI.00576-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polley SD, Chokejindachai W, Conway DJ. 2003. Allele frequency-based analyses robustly map sequence sites under balancing selection in a malaria vaccine candidate antigen. Genetics 165:555–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Polley SD, Conway DJ. 2001. Strong diversifying selection on domains of the Plasmodium falciparum apical membrane antigen 1 gene. Genetics 158:1505–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hodder AN, Crewther PE, Matthew ML, Reid GE, Moritz RL, Simpson RJ, Anders RF. 1996. The disulfide bond structure of Plasmodium apical membrane antigen-1. J. Biol. Chem. 271:29446–29452. 10.1074/jbc.271.46.29446. [DOI] [PubMed] [Google Scholar]
- 14.Bai T, Becker M, Gupta A, Strike P, Murphy VJ, Anders RF, Batchelor AH. 2005. Structure of AMA1 from Plasmodium falciparum reveals a clustering of polymorphisms that surround a conserved hydrophobic pocket. Proc. Natl. Acad. Sci. U. S. A. 102:12736–12741. 10.1073/pnas.0501808102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dutta S, Lee SY, Batchelor AH, Lanar DE. 2007. Structural basis of antigenic escape of a malaria vaccine candidate. Proc. Natl. Acad. Sci. U. S. A. 104:12488–12493. 10.1073/pnas.0701464104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takala SL Coulibaly D, Thera MA, Batchelor AH, Cummings MP, Escalante AA, Ouattara A, Traoré K, Niangaly A, Djimdé AA, Doumbo OK, Plowe CV. 2009. Extreme polymorphism in a vaccine antigen and risk of clinical malaria: implications for vaccine development. Sci. Transl. Med. 1:2ra5. 10.1126/scitranslmed.3000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coley AM, Gupta A, Murphy VJ, Bai T, Kim H, Anders RF, Batchelor AH. 2007. Structure of the malaria antigen AMA1 in complex with a growth-inhibitory antibody. PLoS Pathog. 3:1308–1319. 10.1371/journal.ppat.0030138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mugyenyi CK, Elliott SR, McCallum FJ, Anders RF, Marsh K, Beeson JG. 2013. Antibodies to polymorphic invasion-inhibitory and non-inhibitory epitopes of Plasmodium falciparum apical membrane antigen 1 in human malaria. PLoS One 8:e68304. 10.1371/journal.pone.0068304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ouattara A, Takala-Harrison S, Thera MA, Coulibaly D, Niangaly A, Saye R, Tolo Y, Dutta S, Heppner DG, Soisson L, Diggs CL, Vekemans J, Cohen J, Blackwelder WC, Dube T, Laurens MB, Doumbo OK, Plowe CV. 2013. Molecular basis of allele-specific efficacy of a blood-stage malaria vaccine: vaccine development implications. J. Infect. Dis. 207:511–519. 10.1093/infdis/jis709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barry AE, Schultz L, Buckee CO, Reeder JC. 2009. Contrasting population structures of the genes encoding ten leading vaccine-candidate antigens of the human malaria parasite, Plasmodium falciparum. PLoS One 4:e8497. 10.1371/journal.pone.0008497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drew DR, Hodder AN, Wilson DW, Foley M, Mueller I, Siba PM, Dent AE, Cowman AF, Beeson JG. 2012. Defining the antigenic diversity of Plasmodium falciparum apical membrane antigen 1 and the requirements for a multi-allele vaccine against malaria. PLoS One 7:e51023. 10.1371/journal.pone.0051023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duan JH, Mu JB, Thera MA, Joy D, Pond SLK, Diemert D, Long C, Zhou H, Miura K, Ouattara A, Dolo A, Doumbo O, Su XZ, Miller L. 2008. Population structure of the genes encoding the polymorphic Plasmodium falciparum apical membrane antigen 1: implications for vaccine design. Proc. Natl. Acad. Sci. U. S. A. 105:7857–7862. 10.1073/pnas.0802328105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dutta S, Dlugosz LS, Drew DR, Ge X, Ababacar D, Rovira YI, Moch JK, Shi M, Long CA, Foley M, Beeson JG, Anders RF, Miura K, Haynes JD, Batchelor AH. 2013. Overcoming antigenic diversity by enhancing the immunogenicity of conserved epitopes on the malaria vaccine candidate apical membrane antigen-1. PLoS Pathog. 9:e1003840. 10.1371/journal.ppat.1003840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Remarque EJ, Faber BW, Kocken CHM, Thomas AW. 2008. A diversity-covering approach to immunization with Plasmodium falciparum apical membrane antigen 1 induces broader allelic recognition and growth inhibition responses in rabbits. Infect. Immun. 76:2660–2670. 10.1128/IAI.00170-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kennedy MC, Wang J, Zhang YL, Miles AP, Chitsaz F, Saul A, Long CA, Miller LH, Stowers AW. 2002. In vitro studies with recombinant Plasmodium falciparum apical membrane antigen 1 (AMA1): production and activity of an AMA1 vaccine and generation of a multiallelic response. Infect. Immun. 70:6948–6960. 10.1128/IAI.70.12.6948-6960.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kusi KA, Faber BW, Thomas AW, Remarque EJ. 2009. Humoral immune response to mixed PfAMA1 alleles; multivalent PfAMA1 vaccines induce broad specificity. PLoS Pathog. 4:e8110. 10.1371/journal.pone.0008110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miura K, Herrera R, Diouf A, Zhou H, Mu J, Hu Z, MacDonald NJ, Reiter K, Nguyen V, Shimp RL, Jr, Singh K, Narum DL, Long CA, Miller LH. 2013. Overcoming allelic specificity by immunization with five allelic forms of Plasmodium falciparum apical membrane antigen 1. Infect. Immun. 81:1491–1501. 10.1128/IAI.01414-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miura K, Zhou H, Muratova OV, Orcutt AC, Giersing B, Miller LH, Long CA. 2007. In immunization with Plasmodium falciparum apical membrane antigen 1, the specificity of antibodies depends on the species immunized. Infect. Immun. 75:5827–5836. 10.1128/IAI.00593-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barclay VC, Chan BHK, Anders RF, Read AF. 2008. Mixed allele malaria vaccines: host protection and within-host selection. Vaccine 26:6099–6107. 10.1016/j.vaccine.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sagara I, Ellis RD, Dicko A, Niambele MB, Kamate B, Guindo O, Sissoko MS, Fay MP, Guindo MA, Kante O, Saye R, Miura K, Long C, Mullen GE, Pierce M, Martin LB, Rausch K, Dolo A, Diallo DA, Miller LH, Doumbo OK. 2009. A randomized and controlled phase 1 study of the safety and immunogenicity of the AMA1-C1/Alhydrogel + CPG 7909 vaccine for Plasmodium falciparum malaria in semi-immune Malian adults. Vaccine 27:7292–7298. 10.1016/j.vaccine.2009.10.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ouattara A, Mu JB, Takala-Harrison S, Saye R, Sagara I, Dicko A, Niangaly A, Duan J, Ellis RD, Miller LH, Su XZ, Plowe CV, Doumbo OK. 2010. Lack of allele-specific efficacy of a bivalent AMA1 malaria vaccine. Malar. J. 9:175. 10.1186/1475-2875-9-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dutta S, Dlugosz LS, Clayton JW, Pool CD, Haynes JD, Gasser RA, Batchelor AH. 2010. Alanine mutagenesis of the primary antigenic escape residue cluster, C1, of apical membrane antigen 1. Infect. Immun. 78:661–671. 10.1128/IAI.00866-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coley AM, Campanale NV, Casey JL, Hodder AN, Crewther PE, Anders RF, Tilley LM, Foley M. 2001. Rapid and precise epitope mapping of monoclonal antibodies against Plasmodium falciparum AMA1 by combined phage display of fragments and random peptides. Protein Eng. 14:691–698. 10.1093/protein/14.9.691. [DOI] [PubMed] [Google Scholar]
- 34.Kocken CH, van der Wel AM, Dubbeld MA, Narum DL, van de Rijke FM, van Gemert GJ, van der Linde X, Bannister LH, Janse C, Waters AP, Thomas AW. 1998. Precise timing of expression of a Plasmodium falciparum-derived transgene in Plasmodium berghei is a critical determinant of subsequent subcellular localization. J. Biol. Chem. 273:15119–15124. 10.1074/jbc.273.24.15119. [DOI] [PubMed] [Google Scholar]
- 35.Sidhu SS, Lowman HB, Cunningham BC, Wells JA. 2000. Phage display for selection of novel binding peptides. Methods Enzymol. 328:333–363. 10.1016/S0076-6879(00)28406-1. [DOI] [PubMed] [Google Scholar]
- 36.Coley AM, Parisi K, Masciantonio R, Hoeck J, Casey JL, Murphy VJ, Harris KS, Batchelor AH, Anders RF, Foley M. 2006. The most polymorphic residue on Plasmodium falciparum apical membrane antigen 1 determines binding of an invasion-inhibitory antibody. Infect. Immun. 74:2628–2636. 10.1128/IAI.74.5.2628-2636.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Persson KE, McCallum FJ, Reiling L, Lister NA, Stubbs J, Cowman AF, Marsh K, Beeson JG. 2008. Variation in use of erythrocyte invasion pathways by Plasmodium falciparum mediates evasion of human inhibitory antibodies. J. Clin. Invest. 118:342–351. 10.1172/JCI32138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collins CR, Withers-Martinez C, Bentley GA, Batchelor AH, Thomas AW, Blackman MJ. 2007. Fine mapping of an epitope recognized by an invasion-inhibitory monoclonal antibody on the malaria vaccine candidate apical membrane antigen 1. J. Biol. Chem. 282:7431–7441. 10.1074/jbc.M610562200. [DOI] [PubMed] [Google Scholar]
- 39.Cortes A, Mellombo M, Mueller I, Benet A, Reeder JC, Anders RF. 2003. Geographical structure of diversity and differences between symptomatic and asymptomatic infections for Plasmodium falciparum vaccine candidate AMA1. Infect. Immun. 71:1416–1426. 10.1128/IAI.71.3.1416-1426.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Henderson KA, Streltsov VA, Coley AM, Dolezal O, Hudson PJ, Batchelor AH, Gupta A, Bai T, Murphy VJ, Anders RF, Foley M, Nuttall SD. 2007. Structure of an IgNAR-AMA1 complex: targeting a conserved hydrophobic cleft broadens malarial strain recognition. Structure 15:1452–1466. 10.1016/j.str.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 41.Anders RF, Adda CG, Foley M, Norton RS. 2010. Recombinant protein vaccines against the asexual blood stages of Plasmodium falciparum. Hum. Vaccin. 6:39–53. 10.4161/hv.6.1.10712. [DOI] [PubMed] [Google Scholar]
- 42.Vulliez-Le Normand B, Tonkin ML, Lamarque MH, Langer S, Hoos S, Roques M, Saul FA, Faber BW, Bentley GA, Boulanger MJ, Lebrun M. 2012. Structural and functional insights into the malaria parasite moving junction complex. PLoS Pathog. 8:e1002755. 10.1371/journal.ppat.1002755. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.