Abstract
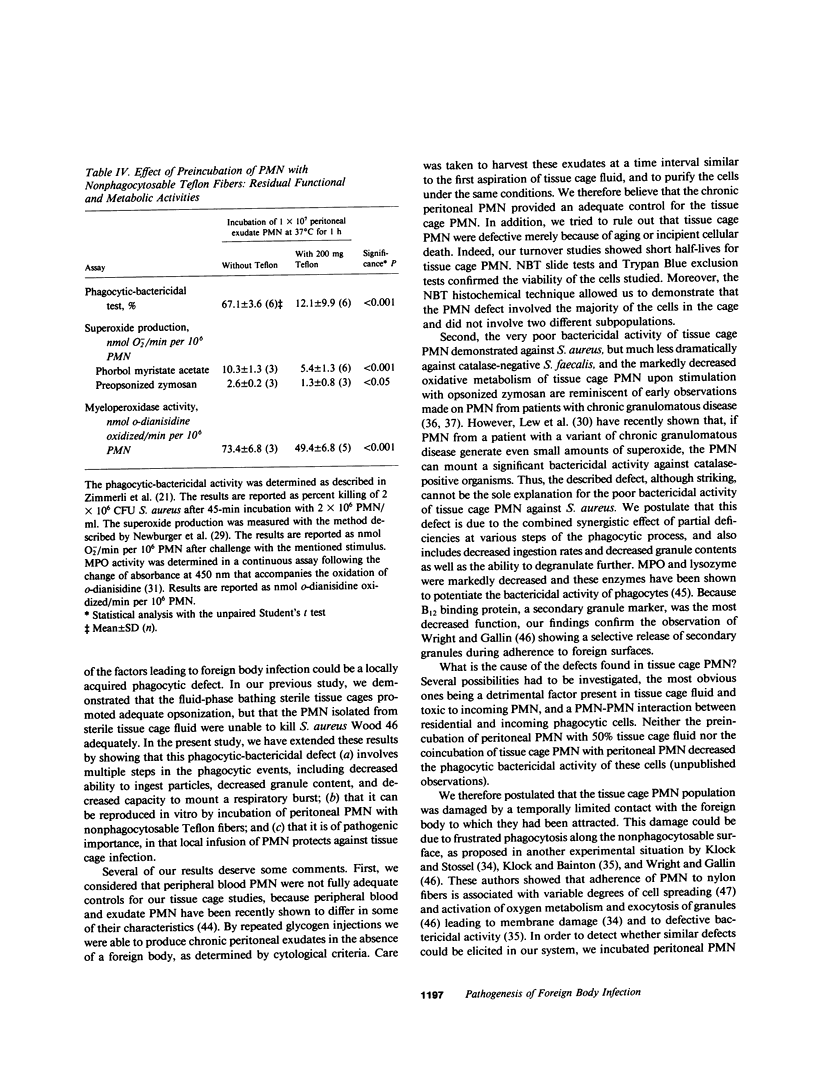
Implanted foreign bodies are highly susceptible to pyogenic infections and represent a major problem in modern medicine. In an effort to understand the pathogenesis of these infections, we studied the phagocytic function in the vicinity of a foreign body by using a recently developed guinea pig model of Teflon tissue cages subcutaneously implanted (Zimmerli, W., F.A. Waldvogel, P. Vaudaux, and U.E. Nydegger, 1982, J. Infect. Dis., 146:487-497). Polymorphonuclear leukocytes (PMN) purified from tissue cage fluid had poor bactericidal activity against a catalase-positive microorganism. When compared with blood or exudate PMN, they exhibited a significant reduction in their ability to generate superoxide in response to a particulate or a soluble stimulus (72 and 57%, respectively, P less than 0.001). Not only their total contents in myeloperoxidase, beta-glucuronidase, lysozyme, and B12 binding protein were significantly reduced (by 62, 21, 47, and 63%, respectively, P less than 0.01), but also their capability for further secretion of residual B12 binding protein upon stimulation. Ingestion rates of endotoxin-coated opsonized oil particles were reduced by 25% (P less than 0.05). In an effort to reproduce these abnormalities in vitro, fresh peritoneal exudate PMN were incubated with Teflon fibers in the presence of plasma. Interaction of PMN with the fibers led to significant increases in hexose monophosphate shunt activity and exocytosis of secondary granules (P less than 0.01). PMN eluted after such interaction showed defective bactericidal activity, oxidative metabolism, and granular enzyme content similar to those observed in tissue cage PMN. The local injection of fresh blood PMN into tissue cages at the time of, or 3 h after, inoculation with 100 microorganisms (Staphylococcus aureus Wood 46) reduced the infection rate from 50 to 56 cages to 1 of 21 (P less than 0.001) and 3 of 8 cages (P less than 0.001), respectively. These results suggest that the in vivo as well as in vitro interaction of PMN with a nonphagocytosable foreign body induces a complex PMN defect, which may be partly responsible for the high susceptibility to infection of foreign bodies.
Full text
PDF








Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bernhard V. M. Management of infected vascular prostheses. Surg Clin North Am. 1975 Dec;55(6):1411–1417. doi: 10.1016/s0039-6109(16)40801-7. [DOI] [PubMed] [Google Scholar]
- Bhat D. J., Tellis V. A., Kohlberg W. I., Driscoll B., Veith F. J. Management of sepsis involving expanded polytetrafluoroethylene grafts for hemodialysis access. Surgery. 1980 Apr;87(4):445–450. [PubMed] [Google Scholar]
- Buchholz H. W., Elson R. A., Engelbrecht E., Lodenkämper H., Röttger J., Siegel A. Management of deep infection of total hip replacement. J Bone Joint Surg Br. 1981;63-B(3):342–353. doi: 10.1302/0301-620X.63B3.7021561. [DOI] [PubMed] [Google Scholar]
- Burri C. Die infizierte Osteosynthese. Helv Chir Acta. 1978 Dec;45(4-5):545–552. [PubMed] [Google Scholar]
- Charnley J. Postoperative infection after total hip replacement with special reference to air contamination in the operating room. Clin Orthop Relat Res. 1972 Sep;87:167–187. doi: 10.1097/00003086-197209000-00020. [DOI] [PubMed] [Google Scholar]
- Chenoweth D. E., Lane T. A., Rowe J. G., Hugli T. E. Quantitative comparisons of neutrophil chemotaxis in four animal species. Clin Immunol Immunopathol. 1980 Mar;15(3):525–535. doi: 10.1016/0090-1229(80)90064-1. [DOI] [PubMed] [Google Scholar]
- Christensen G. D., Bisno A. L., Parisi J. T., McLaughlin B., Hester M. G., Luther R. W. Nosocomial septicemia due to multiply antibiotic-resistant Staphylococcus epidermidis. Ann Intern Med. 1982 Jan;96(1):1–10. doi: 10.7326/0003-4819-96-1-1. [DOI] [PubMed] [Google Scholar]
- Cohen A. B., Rossi M., Geczy D., Knight L. Neutrophil turnover in normal rabbit lungs. J Clin Invest. 1982 Apr;69(4):794–798. doi: 10.1172/JCI110518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costerton J. W., Geesey G. G., Cheng K. J. How bacteria stick. Sci Am. 1978 Jan;238(1):86–95. doi: 10.1038/scientificamerican0178-86. [DOI] [PubMed] [Google Scholar]
- Courtiss E. H., Goldwyn R. M., Anastasi G. W. The fate of breast implants with infections around them. Plast Reconstr Surg. 1979 Jun;63(6):812–816. [PubMed] [Google Scholar]
- Dale D. C., Reynolds H. Y., Pennington J. E., Elin R. J., Pitts T. W., Graw R. G., Jr Granulocyte transfusion therapy of experimental Pseudomonas pneumonia. J Clin Invest. 1974 Sep;54(3):664–671. doi: 10.1172/JCI107804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies W. A., Stossel T. P. External membrane proteins of rabbit lung macrophages. Arch Biochem Biophys. 1981 Jan;206(1):190–197. doi: 10.1016/0003-9861(81)90080-1. [DOI] [PubMed] [Google Scholar]
- Dougherty S. H., Simmons R. L. Infections in bionic man: the pathobiology of infections in prosthetic devices-Part II. Curr Probl Surg. 1982 Jun;19(6):265–319. doi: 10.1016/0011-3840(82)90035-1. [DOI] [PubMed] [Google Scholar]
- ELEK S. D., CONEN P. E. The virulence of Staphylococcus pyogenes for man; a study of the problems of wound infection. Br J Exp Pathol. 1957 Dec;38(6):573–586. [PMC free article] [PubMed] [Google Scholar]
- Ericson C., Lidgren L., Lindberg L. Cloxacillin in the prophylaxis of postoperative infections of the hip. J Bone Joint Surg Am. 1973 Jun;55(4):808-13, 843. [PubMed] [Google Scholar]
- Fitzgerald R. H., Jr, Nolan D. R., Ilstrup D. M., Van Scoy R. E., Washington J. A., 2nd, Coventry M. B. Deep wound sepsis following total hip arthroplasty. J Bone Joint Surg Am. 1977 Oct;59(7):847–855. [PubMed] [Google Scholar]
- Fitzgerald R. H., Jr, Peterson L. F., Washington J. A., 2nd, Van Scoy R. E., Coventry M. B. Bacterial colonization of wounds and sepsis in total hip arthroplasty. J Bone Joint Surg Am. 1973 Sep;55(6):1242–1250. [PubMed] [Google Scholar]
- Forsgren A., Schmeling D., Zettervall O. Quantitative phagocytosis by human polymorphonuclear leucocytes. Use of radiolabelled emulsions to measure thae rate of phagocytosis. Immunology. 1977 Apr;32(4):491–497. [PMC free article] [PubMed] [Google Scholar]
- Georgiade N. G., King E. H., Harris W. A., Tenery J. H., Schlech B. A. Effect of three proteinaceous foreign materials on infected and subinfected wound models. Surgery. 1975 Apr;77(4):569–576. [PubMed] [Google Scholar]
- Goldstein I. M., Weissmann G. Nonphagocytic stimulation of human polymorphonuclear leukocytes: role of the plasma membrane. Semin Hematol. 1979 Jul;16(3):175–187. [PubMed] [Google Scholar]
- Hisatsune K., Kobayashi K., Nozaki S., Muramatsu I. Phagocytosis-stimulating activity of tuftsin analogs. Microbiol Immunol. 1978;22(9):581–584. doi: 10.1111/j.1348-0421.1978.tb00407.x. [DOI] [PubMed] [Google Scholar]
- Hjorth R., Jonsson A. K., Vretblad P. A rapid method for purification of human granulocytes using percoll. A comparison with dextran sedimentation. J Immunol Methods. 1981;43(1):95–101. doi: 10.1016/0022-1759(81)90040-5. [DOI] [PubMed] [Google Scholar]
- Hunter G., Dandy D. The natural history of the patient with an infected total hip replacement. J Bone Joint Surg Br. 1977 Aug;59(3):293–297. doi: 10.1302/0301-620X.59B3.893507. [DOI] [PubMed] [Google Scholar]
- KAPLOW L. S. SIMPLIFIED MYELOPEROXIDASE STAIN USING BENZIDINE DIHYDROCHLORIDE. Blood. 1965 Aug;26:215–219. [PubMed] [Google Scholar]
- Kaplan E. L., Laxdal T., Quie P. G. Studies of polymorphonuclear leukocytes from patients with chronic granulomatous disease of childhood: bactericidal capacity for streptococci. Pediatrics. 1968 Mar;41(3):591–599. [PubMed] [Google Scholar]
- Klock J. C., Bainton D. F. Degranulation and abnormal bactericidal function of granulocytes procured by reversible adhesion to nylon wool. Blood. 1976 Jul;48(1):149–161. [PubMed] [Google Scholar]
- Klock J. C., Stossel T. P. Detection, pathogenesis, and prevention of damage to human granulocytes caused by interaction with nylon wool fiber. Implications for filtration leukapheresis. J Clin Invest. 1977 Nov;60(5):1183–1190. doi: 10.1172/JCI108871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladefoged K., Efsen F., Krogh Christoffersen J., Jarnum S. Long-term parenteral nutrition. II. Catheter-related complications. Scand J Gastroenterol. 1981;16(7):913–919. doi: 10.3109/00365528109181822. [DOI] [PubMed] [Google Scholar]
- Lew P. D., Southwick F. S., Stossel T. P., Whitin J. C., Simons E., Cohen H. J. A variant of chronic granulomatous disease: deficient oxidative metabolism due to a low-affinity NADPH oxidase. N Engl J Med. 1981 Nov 26;305(22):1329–1333. doi: 10.1056/NEJM198111263052207. [DOI] [PubMed] [Google Scholar]
- Lidwell O. M., Lowbury E. J., Whyte W., Blowers R., Stanley S. J., Lowe D. Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. Br Med J (Clin Res Ed) 1982 Jul 3;285(6334):10–14. doi: 10.1136/bmj.285.6334.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell G. L., Hook E. W. Leukocyte bactericidal activity in chronic granulomatous disease: correlation of bacterial hydrogen peroxide production and susceptibility to intracellular killing. J Bacteriol. 1969 Oct;100(1):531–532. doi: 10.1128/jb.100.1.531-532.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton L. J., 3rd, Stauffer R. N., Chao E. Y., Ilstrup D. M. Rates of total hip arthroplasty; a population-based study. N Engl J Med. 1982 Nov 11;307(20):1242–1245. doi: 10.1056/NEJM198211113072004. [DOI] [PubMed] [Google Scholar]
- Morgenstern L. Postoperative jaundice. An approach to a diagnostic dilemma. Am J Surg. 1974 Aug;128(2):255–261. [PubMed] [Google Scholar]
- Newburger P. E., Chovaniec M. E., Cohen H. J. Activity and activation of the granulocyte superoxide-generating system. Blood. 1980 Jan;55(1):85–92. [PubMed] [Google Scholar]
- Newburger P. E., Pagano J. S., Greenberger J. S., Karpas A., Cohen H. J. Dissociation of opsonized particle phagocytosis and respiratory burst activity in an Epstein-Barr virus-infected myeloid cell line. J Cell Biol. 1980 Jun;85(3):549–557. doi: 10.1083/jcb.85.3.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble W. C. The production of subcutaneous staphylococcal skin lesions in mice. Br J Exp Pathol. 1965 Jun;46(3):254–262. [PMC free article] [PubMed] [Google Scholar]
- Peters G., Locci R., Pulverer G. Adherence and growth of coagulase-negative staphylococci on surfaces of intravenous catheters. J Infect Dis. 1982 Oct;146(4):479–482. doi: 10.1093/infdis/146.4.479. [DOI] [PubMed] [Google Scholar]
- Peters G., Locci R., Pulverer G. Microbial colonization of prosthetic devices. II. Scanning electron microscopy of naturally infected intravenous catheters. Zentralbl Bakteriol Mikrobiol Hyg B. 1981;173(5):293–299. [PubMed] [Google Scholar]
- Root R. K., Cohen M. S. The microbicidal mechanisms of human neutrophils and eosinophils. Rev Infect Dis. 1981 May-Jun;3(3):565–598. doi: 10.1093/clinids/3.3.565. [DOI] [PubMed] [Google Scholar]
- Rubin J., Rogers W. A., Taylor H. M., Everett E. D., Prowant B. F., Fruto L. V., Nolph K. D. Peritonitis during continuous ambulatory peritoneal dialysis. Ann Intern Med. 1980 Jan;92(1):7–13. doi: 10.7326/0003-4819-92-1-7. [DOI] [PubMed] [Google Scholar]
- SCHIMKE R. T., BLACK P. H., MARK V. H., SWARTZ M. N. Indolent Staphylococcus albus or aureus bacteremia after ventriculoatriostomy. Role of foreign body in its initiation and perpetuation. N Engl J Med. 1961 Feb 9;264:264–270. doi: 10.1056/NEJM196102092640602. [DOI] [PubMed] [Google Scholar]
- Sheppeard H., Cleak D. K., Ward D. J., O'Connor B. T. A review of early mortality and morbidity in elderly patients following Charnley total hip replacement. Arch Orthop Trauma Surg. 1980;97(4):243–248. doi: 10.1007/BF00380704. [DOI] [PubMed] [Google Scholar]
- Stossel T. P., Field R. J., Gitlin J. D., Alper C. A., Rosen F. S. The opsonic fragment of the third component of human complement (C3). J Exp Med. 1975 Jun 1;141(6):1329–1347. doi: 10.1084/jem.141.6.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilagyi D. E., Smith R. F., Elliott J. P., Vrandecic M. P. Infection in arterial reconstruction with synthetic grafts. Ann Surg. 1972 Sep;176(3):321–333. doi: 10.1097/00000658-197209000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedesco F., Trani S., Soranzo M. R., Patriarca P. Stimulation of glucose oxidation in human polymorphonuclear leucocytes by C3-Sepharose and soluble C567. FEBS Lett. 1975 Mar 1;51(1):232–236. doi: 10.1016/0014-5793(75)80894-5. [DOI] [PubMed] [Google Scholar]
- Tshefu K., Zimmerli W., Waldvogel F. A. Short-term administration of rifampin in the prevention or eradication of infection due to foreign bodies. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S474–S480. doi: 10.1093/clinids/5.supplement_3.s474. [DOI] [PubMed] [Google Scholar]
- Van Epps D. E., Garcia M. L. Enhancement of neutrophils function as a result of prior exposure to chemotactic factor. J Clin Invest. 1980 Aug;66(2):167–175. doi: 10.1172/JCI109841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright D. G., Gallin J. I. Secretory responses of human neutrophils: exocytosis of specific (secondary) granules by human neutrophils during adherence in vitro and during exudation in vivo. J Immunol. 1979 Jul;123(1):285–294. [PubMed] [Google Scholar]
- Wright D. G., Klock J. C. Functional changes in neutrophils collected by filtration leukapheresis and their relationship to cellular events that occur during adherence of neutrophils to nylon fibers. Exp Hematol. 1979;7(4 Suppl):11–23. [PubMed] [Google Scholar]
- Zimmerli W., Waldvogel F. A., Vaudaux P., Nydegger U. E. Pathogenesis of foreign body infection: description and characteristics of an animal model. J Infect Dis. 1982 Oct;146(4):487–497. doi: 10.1093/infdis/146.4.487. [DOI] [PubMed] [Google Scholar]


