Abstract
OBJECTIVE:
Although end-of-life care in the ICU accounts for a large proportion of health-care costs, few studies have examined the association between costs and satisfaction with care. The objective of this study was to investigate the association of ICU costs with family- and nurse-assessed quality of dying and family satisfaction.
METHODS:
This was an observational study surveying families and nurses for patients who died in the ICU or within 30 h of transfer from the ICU. A total of 607 patients from two Seattle hospitals were included in the study. Survey data were linked with administrative records to obtain ICU and hospital costs. Regression analyses assessed the association between costs and outcomes assessing satisfaction with care: nurse- and family-assessed Quality of Death and Dying (QODD-1) and Family Satisfaction in the ICU (FS-ICU).
RESULTS:
For family-reported outcomes, patient insurance status was an important modifier of results. For underinsured patients, higher daily ICU costs were significantly associated with higher FS-ICU and QODD-1 (P < .01 and P = .01, respectively); this association was absent for privately insured or Medicare patients (P = .50 and P = .85, QODD-1 and FS-ICU, respectively). However, higher nurse-assessed QODD-1 was significantly associated with lower average daily ICU cost and total hospital cost (P < .01 and P = .05, respectively).
CONCLUSIONS:
Family-rated satisfaction with care and quality of dying varied depending on insurance status, with underinsured families rating satisfaction with care and quality of dying higher when average daily ICU costs were higher. However, patients with higher costs were assessed by nurses as having a poorer quality of dying. These findings highlight important differences between family and clinician perspectives and the important role of insurance status.
In the United States, 20% of patients die during a hospitalization with an ICU stay,1 and 25% of our health-care costs are spent on the 6% of people who die each year.2‐4 Our aging population, coupled with medical advances, has led to an increasing number and proportion of ICU beds and increasing costs of critical care.2,5,6 Whether these trends of increased ICU use are consistent with patient values and preferences or are associated with the quality of end-of-life care is unclear.
There is evidence to suggest that ensuring patient-centered care for those at high risk of death leads to a reduction in intensity of care near the end of life.7‐11 However, there is a notable discrepancy between the setting in which terminally ill patients prefer to die and the setting in which they actually die.12,13 Teno and colleagues14 found that ICU use in the last 30 days of life increased between 2000 and 2009 despite public opinion surveys reporting that most patients would prefer to die at home if diagnosed with a terminal illness.13 In a study of patients with advanced cancer recruited from the outpatient setting, higher medical costs in the final week of life were associated with more physical distress and worse overall quality of death as perceived by the family caregiver.15 For patients who die in the ICU, the association between hospital costs at the end of life and quality of death remains unclear.
The objectives of our study were to investigate the associations between ICU or hospital costs at the end of life and family- or nurse-reported outcomes for patients who died in, or shortly after a stay in, the ICU. For families, these outcomes include ratings of the quality of dying and satisfaction with care in the ICU; for nurses, outcomes include ratings of the quality of dying. We hypothesized that higher costs at the end of life, reflecting longer length of ICU stays and more invasive, aggressive treatment, could have a negative impact on the quality of dying and satisfaction with care for family members of patients who die in the ICU. We also hypothesized that the impact of an expensive ICU stay on quality of dying and satisfaction with care would be most pronounced in the uninsured/underinsured and other patients of lower socioeconomic status.
Materials and Methods
Design Overview
Data were collected as part of two studies (a before-after trial and a cluster-randomized trial) of an interdisciplinary, multifaceted intervention to improve the quality of end-of-life care for critically ill patients and their families.16‐18 Eligible patients were those who had died in an ICU after a minimum stay of 6 h or within 30 h of transfer from the ICU to another hospital location. Questionnaires were sent to patients’ homes 4 to 6 weeks after death, addressed to “the family of” the patient, requesting a response from the person most knowledgeable about the patient’s end-of-life experience. Nurse questionnaires were distributed within 72 h of death to the hospital mailbox of the nurse caring for the patient at the time of death/transfer and the nurse from the prior shift. Data were linked to hospital financial records to obtain detailed cost information on hospital and ICU expenditures. All procedures were approved by the institutional review boards at all institutions (UW HSC#23503).
Setting
The two hospitals in this study are both part of a single network and, therefore, had a common system for calculating ICU and hospital costs. The hospitals included one academic level I trauma center and one community-based hospital.
Outcome Measures
Outcome measures were the nurse- and family-assessed Quality of Death and Dying (QODD-1) rating and the Family Satisfaction in the ICU (FS-ICU) questionnaire’s total score. The QODD-1 provides a succinct measure of the overall quality of dying using a single-item summary question: “Overall, how would you rate the quality of your loved one’s dying?” Ratings range from zero (a “terrible” experience) to 10 (an “almost perfect” experience). The QODD-1 has been associated with the quality of ICU palliative care.19
The FS-ICU is a reliable and valid 34-item tool designed to measure family satisfaction with ICU care.20,21 Recently, the FS-ICU was reduced to 24 items, and a validated scoring method was developed.22 Higher values indicate increased satisfaction. The survey is available online.23
Cost Variables
Total hospital and total ICU costs, rather than charges, were obtained from administrative financial databases. Charges bear little resemblance to costs, and use of charges as a proxy for costs may lead to unwarranted conclusions about economic efficiency.24 Therefore, we chose to use actual costs. The reported costs represent indirect and direct costs and include all facility and professional fees, with the exception of physician fees. Collectively, these costs represent the total costs for all services provided on each hospital day, including overhead costs, labor costs, and supply costs. Direct costs represent costs that are traceable back to a specific cost center providing direct patient care, such as pharmacy, radiology, respiratory, microbiology, and hematology. Indirect costs, which are included in the patient bill, represent services provided by cost centers not directly linked to patient care, such as information technology, environmental services, and hospital administration. In this network of hospitals, physician fees are not generated in a similar way at each institution and were, therefore, not included. To obtain average daily costs, total ICU costs were divided by the ICU length of stay (LOS). All costs were adjusted for inflation and compared at the 2013 US dollar value. Because of the skewness of the cost data, we use the log-transformed value.
Covariates
We determined patient age, sex, and insurance type from the medical record. Insurance type was assessed in four categories (private insurance, Medicare, Medicaid, no insurance). For the purposes of these analyses, we assess insurance as insured (private insurance, Medicare) and underinsured (Medicaid, no insurance) based on a prior validation of this approach.25 For associations found to be significant, we conducted sensitivity analyses in which we examined results of regression models across the four uncollapsed insurance categories. Patient race, education, and underlying cause of death were determined from the death certificate. In addition, we used median household income by zip code using the patient’s zip code listed on the death certificate and census tract data.25 We determined family member’s age, sex, level of education, spouse vs other relationship, and presence at the time of death from family surveys and nurses’ age and sex from nurse surveys.
Data Analysis
We used multivariable linear regression with robust SEs26 to explore the linear association between the family-assessed outcomes (QODD-1, FS-ICU) and our three predictors of interest: average daily ICU costs, total ICU costs, and total hospital costs. We adopt a nonparametric interpretation of linear regression that assumes neither linearity nor heteroscedasticity.27 To understand the magnitude of the associations, under the assumption of linearity, the regression coefficients represent the difference in quality of death outcomes per doubling of the cost variable. Generalized linear estimating equations were used to examine the relationship between nurse-assessed QODD-1 and costs, which allowed us to account for correlation between observations attributable to nurses completing surveys for multiple patients.28 If both the nurse at time of death and the nurse for the prior shift responded, we selected the questionnaire that was more complete; if both were equally complete, we randomly selected one per patient.16,17 Baseline, minimally adjusted regression models included dummy-indicator variable for hospital and pre/post intervention adjustment. In addition, we adjusted models for any confounders that changed the minimally adjusted cost parameter estimate by an absolute value ≥ 10%, selecting from the following a priori-identified variables: patient age, race, sex, education, median household income by zip code, insurance type, and underlying cause of death. For models with family-assessed outcomes, we also examined family member’s age, sex, level of education, spouse vs other relationship, and presence at the time of death. For nurse-assessed outcomes, we examined nurses’ age and sex. In addition, a priori we identified patient race, age and underlying cause of death attributable to trauma as potential effect modifiers. For the family-reported outcomes (QODD-1 and FS-ICU), we identified patient insurance status, median household income by zip code, and family member level of education as potential effect modifiers. In sensitivity analyses, we compared available patient information between survey responders and nonresponders to assess the potential extent of selection bias using t tests with unequal variances or χ2 tests, as appropriate. A two-sided α level of ≤ 0.05 was considered statistically significant. Data were analyzed using STATA, version 12.0 (StataCorp LP) statistical software.
Results
Sample Characteristics
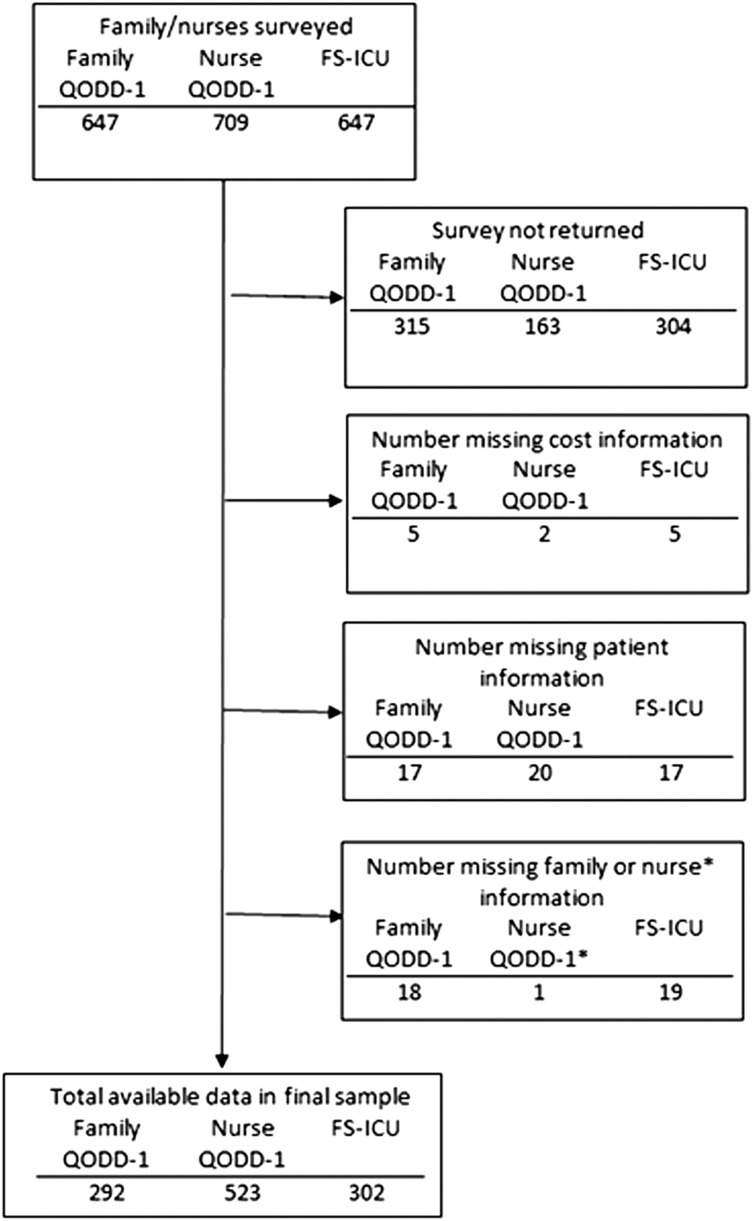
A total of 607 unique patients were included in this study; details of cohort development are displayed in Figure 1. Among these 607 patients, 523 had a nurse-assessed QODD-1 score, 292 had a family-assessed QODD-1 score, and 302 had a total FS-ICU score.
Figure 1 –
Development of cohort. FS-ICU = Family Satisfaction in the ICU; QODD-1 = Single-item quality of dying rating from the Quality of Dying and Death Questionnaire.
The mean age of the patient study population was 63 years (± 18). Twenty-eight percent of patients died as a result of trauma; 6% died of cancer. Eighty-seven percent of patients were intubated during the last week of life. The majority of patients were Medicare beneficiaries (53%); 19% had private insurance, and 17% had some other form of government-issued insurance (Table 1). The average age at time of death for privately insured patients was 54 years (± 14), vs 75 years (± 10) for Medicare beneficiaries.
TABLE 1 ] .
Characteristics of Study Cohort
| Patient Characteristic | All Subjects (N = 607) | Patients With a Family Questionnaire Response (n = 307) |
| Age at time of death, y | 63.4 (SD, 17.7) | 65.1 (SD, 17.1) |
| Female | 229 (37.7) | 129 (42.0) |
| Race/ethnicity | ||
| White | 502 (82.7) | 268 (87.3) |
| Black | 33 (5.4) | 13 (4.2) |
| Asian | 43 (7.1) | 15 (4.9) |
| Hispanic | 16 (2.6) | 5 (1.6) |
| Other | 13 (2.1) | 6 (2.0) |
| Level of education (n = 578) | ||
| < Eighth grade | 47 (8.1) | 22 (7.3) |
| Some high school | 64 (11.1) | 24 (8.0) |
| High school/GED | 228 (39.4) | 115 (38.2) |
| Some college | 135 (23.4) | 77 (25.6) |
| 4 y college | 73 (12.6) | 47 (15.6) |
| Graduate level | 31 (5.4) | 16 (5.3) |
| Median income of zip code, 1,000 US$ | 46.1 (SD, 12.2) | 47.2 (SD, 11.7) |
| Per capita income of zip code, 1,000 US$ | 24.4 (SD, 7.2) | 24.3 (SD, 7.2) |
| Hospital | ||
| Hospital 1 | 506 (83.4) | 243 (79.2) |
| Hospital 2 | 101 (16.6) | 64 (20.8) |
| ICU length of stay, median (IQR), d | 3 (1, 8) | 4 (1, 9) |
| Hospital length of stay, median (IQR), d | 4 (2, 10) | 5 (2, 11) |
| Diagnosisa | ||
| Heart disease | 43 (7.1) | 26 (8.5) |
| HIV/infection | 68 (11.2) | 30 (9.8) |
| Respiratory | 51 (8.4) | 25 (8.1) |
| GI/liver | 31 (5.1) | 23 (7.5) |
| Stroke/neurologic | 135 (22.2) | 76 (24.8) |
| Trauma | 59 (9.7) | 33 (10.7) |
| Cancer | 8 (1.3) | 3 (1.0) |
| Unknown/other | 212 (34.9) | 91 (29.6) |
| Cause of deathb | ||
| Trauma | 172 (28.3) | 84 (27.4) |
| Cancer | 37 (6.1) | 19 (6.2) |
| Other | 398 (65.6) | 204 (66.4) |
| Intubated in last wk of life | 528 (87.1) | 256 (83.4) |
| In ICU at time of death | 506 (83.4) | 243 (79.2) |
| Died in setting of full support | 128 (21.1) | 58 (18.9) |
| Documentation of a living will prior to admitc | 154 (42.0) | 97 (47.6) |
| Type of insurance | ||
| Private | 113 (18.6) | 65 (21.2) |
| Medicare | 324 (53.4) | 175 (57.0) |
| Other government | 103 (17.0) | 41 (13.4) |
| Other/none/unknown | 67 (11.0) | 26 (8.5) |
| Post intervention | 333 (54.9) | 165 (53.7) |
| Total hospital cost, 1,000 2013 US$d | 45.2 (SD, 50.3) | 50.7 (SD, 58.7) |
| Median (IQR) | 26.6 (12.2, 61.4) | 28.8 (12.8, 66.6) |
| Total ICU cost, 1,000 2013 US$d | 34.8 (SD, 41.7) | 38.6 (SD, 48.3) |
| Median (IQR) | 20.4 (8.6, 44.0) | 21.1 (7.7, 50.0) |
| Cost per ICU day, 1,000 2013 US$d | 6.8 (SD, 5.8) | 6.8 (SD, 6.9) |
| Median (IQR) | 5.5 (4.2, 7.7) | 5.5 (4.1, 7.4) |
Data presented as mean (SD) or No. (%), unless otherwise indicated. GED = General Education Development; IQR = interquartile range.
Determined by first International Classification of Diseases, Ninth Revision code listed; this reflects most reimbursable, not necessarily primary diagnosis.
As reported on death certificate.
Proportion among patients with medical record documentation of presence/absence of living will.
Adjusted for inflation and reported in 2013 US dollars.
Forty percent of family members who answered the QODD-1 or the FS-ICU were the patient’s spouse; 81% of family members were present at the time of death. Additional demographic information is reported in Table 2. Among the 254 individual nurses who answered the QODD-1, 82% were women, with a mean age of 40 years (± 9) (Table 2).
TABLE 2 ] .
Characteristics of Family and Nurse Responders
| Characteristic | Response |
| Family member characteristica | n = 307 |
| Age at time survey was filled out, y | 57.0 (SD, 17.0) |
| Female | 199 (64.8) |
| Level of education | |
| < Eighth grade | 3 (1.0) |
| Some high school | 12 (3.9) |
| High school/GED | 54 (17.6) |
| Some college | 138 (45.0) |
| 4 y college | 54 (17.6) |
| Graduate level | 46 (15.0) |
| Patient’s spouse | 124 (40.4) |
| Present at time of death | 250 (81.4) |
| FS-ICU score (n = 302) | 81.3 (SD, 16.4) |
| Family-assessed QODD-1 (n = 292) | 6.4 (SD, 2.5) |
| Nurse characteristicb | n = 254 |
| Age at time survey was filled out | 39.5 (SD, 8.8) |
| Female | 196 (81.7) |
| Nurse-assessed QODD-1 | 7.0 (SD, 2.7) |
Data presented as mean (SD) or No. (%), unless otherwise indicated. FS-ICU = Family Satisfaction in the ICU; QODD-1 = Single-item quality of dying rating from the Quality of Dying and Death Questionnaire.
Family members who responded to FS-ICU and/or QODD-1.
Two hundred fifty-four individual nurses returned a total of 523 surveys; each nurse filled out an average of 2.0 (SD, 1.5) surveys for eligible patients.
We compared characteristics of patients for whom a family member answered either the QODD-1 and/or the FS-ICU to patients who did not have a responder. There were 647 patients to whom a survey was mailed and not returned to us from the post office as “undelivered.” Of these 647 family members, 349 (54%) completed and returned either the QODD-1 and/or FS-ICU. Patients for whom family members responded had longer hospital (mean 8.8 days vs 7.2 days) and ICU LOS (6.6 days vs 5.5 days) and were less likely to die in the setting of full support (19% vs 24%). They were also more likely to be white (87% vs 77%) and have private or Medicare insurance (79% vs 69%, P < .01 for all). The average daily ICU cost was roughly the same between the two groups ($6,500 vs $6,400, P = .51).
Seventy-seven percent of eligible patients had a nurse questionnaire returned. Patients for whom nurses responded were slightly younger (63 years vs 69 years), more likely to be in the ICU at time of death (89% vs 43%), and more likely to have been intubated in the last week of life (89% vs 73%). Although the LOS was comparable between groups, mean costs were higher in patients for whom nurses responded (total ICU cost, $36,900 vs $21,300; P < .01 for all).
Adjusted Cost Analyses
All a priori-identified potential confounders were systematically tested against the nine different minimally adjusted models (three outcomes: family-assessed QODD-1, nurse-assessed QODD-1, FS-ICU score, and three cost variables: average daily ICU costs, total ICU costs, total hospital costs). Patient age and insurance type were the only two covariates that met criteria for confounding in several of the models and were included in all models. There was no evidence of effect modification by patient race, age, underlying cause of death, family member level of education, or median household income by zip code; however, we found significant effect modification of average daily ICU costs by patient insurance status for both family-reported outcomes (P = .01, P = .05 for FS-ICU and QODD-1, respectively). We subsequently ran fully interacted models with insurance status for the family-assessed QODD-1 and FS-ICU outcomes (Table 3). We additionally examined differences in patient characteristics and family responders stratified by insurance status (Table 4). Compared with insured patients, underinsured patients were younger (49 years vs 70 years, P < .01) and had a slightly larger proportion of minorities. Average daily ICU cost was higher in the underinsured group ($7,800 vs $6,500, underinsured vs insured, respectively; P < .01). However, there was no significant difference in level of education (P = .22) or median household income by zip code (P = .11) between insured and underinsured patients.
TABLE 3 ] .
Family-Assessed Outcomes Stratified by Insurance Typea
| Costs per Insurance Group | FS-ICU (n = 302) | QODD-1 (n = 292) | ||||
| No. | β (95% CI) | P Value | No. | β (95% CI) | P Value | |
| Average ICU cost per dayb | ||||||
| Private/Medicare | 236 | −1.0 (−4.0, 2.0) | .50 | 228 | −0.0 (−0.6, 0.5) | .85 |
| Underinsured | 66 | 9.1 (3.9, 14.2) | < .01 | 64 | 1.4 (0.4, 2.3) | .01 |
| Total ICU costb | ||||||
| Private/Medicare | 236 | −0.1 (−1.2, 1.0) | .90 | 228 | −0.0 (−0.3, 0.2) | .70 |
| Underinsured | 66 | −1.1 (−4.7, 2.6) | .56 | 64 | −0.2 (−0.9, 0.4) | .50 |
| Total hospital costb | ||||||
| Private/Medicare | 236 | −0.2 (−1.4, 1.0) | .79 | 228 | −0.0 (−0.3, 0.2) | .72 |
| Underinsured | 66 | −1.2 (−4.6, 2.3) | .50 | 64 | −0.3 (−0.9, 0.3) | .31 |
See Table 2 legend for expansion of abbreviations.
All are fully interacted models that included level and interaction terms for intervention (pre/post), hospital, patient age, and patient insurance status (underinsured vs private/Medicare).
Cost variable of interest has been log transformed and adjusted for inflation and so that all costs were compared at the 2013 US dollar value.
TABLE 4 ] .
Characteristics of Patients and Family Responders by Insurance Type (n = 307)a
| Characteristic | Insured (n = 240) | Underinsured (n = 67) | P Valueb |
| Patient characteristic | |||
| Age at time of death, y | 69.7 (SD, 14.7) | 49.0 (SD, 15.4) | < .01 |
| Female | 108 (45.0) | 21 (31.3) | .05 |
| Race/ethnicity | < .01 | ||
| White | 216 (90.0) | 52 (77.6) | |
| Black | 6 (2.5) | 7 (10.4) | |
| Asian | 10 (4.2) | 5 (7.5) | |
| Hispanic | 3 (1.3) | 2 (3.0) | |
| Other | 5 (2.1) | 1 (1.5) | |
| Level of educationc | .55 | ||
| < Eighth grade | 19 (8.0) | 3 (4.7) | |
| Some high school | 17 (7.2) | 7 (10.9) | |
| High school/GED | 90 (38.0) | 25 (39.1) | |
| Some college | 60 (25.3) | 17 (26.6) | |
| 4 y college | 36 (15.2) | 11 (17.2) | |
| Graduate level | 15 (6.3) | 1 (1.6) | |
| Median income zip code, 1,000 US$ | 47.7 (SD, 11.8) | 45.3 (SD, 11.1) | .11 |
| Per capita income zip code, 1,000 US$ | 24.3 (SD, 7.2) | 23.9 (SD, 7.2) | .66 |
| Hospital | < .01 | ||
| #1 | 179 (74.6) | 64 (95.5) | |
| #2 | 61 (25.4) | 3 (4.5) | |
| ICU length of stay, median (IQR) | 3.0 (1.0, 9.5) | 4.0 (1.0, 7.0) | .47 |
| Hospital length of stay, median (IQR) | 5.0 (2.0, 11.0) | 5.0 (2.0, 13.0) | .42 |
| Diagnosisd | .06 | ||
| Heart disease | 24 (10.0) | 2 (3.0) | |
| HIV/infection | 24 (10.0) | 6 (9.0) | |
| Respiratory | 19 (7.9) | 6 (9.0) | |
| GI/liver | 17 (7.1) | 6 (9.0) | |
| Stroke/neurologic | 63 (26.3) | 13 (19.4) | |
| Trauma | 29 (12.1) | 4 (6.0) | |
| Cancer | 3 (1.3) | 0 (0.0) | |
| Unknown/other | 61 (25.4) | 30 (44.8) | |
| Cause of deathe | .01 | ||
| Trauma | 56 (23.3) | 28 (41.8) | |
| Cancer | 16 (6.7) | 3 (4.5) | |
| Other | 168 (70.0) | 36 (53.7) | |
| Intubated in last week of life | 196 (81.7) | 60 (89.6) | .13 |
| In ICU at time of death | 179 (74.6) | 64 (95.5) | .01 |
| Died in setting of full support | 39 (16.3) | 19 (28.4) | .03 |
| Documentation of a living will prior to admitf | 87 (53.4) | 10 (24.4) | < .01 |
| After hospital intervention | 122 (50.8) | 43 (64.2) | .05 |
| Total hospital cost, 1,000 2013 US$g | 48.2 (SD, 54.9) | 59.4 (SD, 70.5) | .18 |
| Median (IQR) | 26.5 (11.9, 65.6) | 36.7 (13.9, 75.9) | |
| Total ICU cost, 1,000 2013 US$g | 36.3 (SD, 44.8) | 46.9 (SD, 58.9) | < .01 |
| Median (IQR) | 20.2 (6.8, 49.7) | 28.8 (12.9, 52.4) | |
| Cost per ICU day, 1,000 2013 US$g | 6.5 (SD, 7.4) | 7.8 (SD, 4.1) | < .01 |
| Median (IQR) | 5.3 (3.1, 6.9) | 6.8 (5.1, 9.9) | |
| Family member characteristic | |||
| Age at time of survey, y | 57.8 (SD, 13.9) | 53.9 (SD, 13.8) | .04 |
| Female | 155 (64.6) | 44 (65.7) | .87 |
| Level of education | .22 | ||
| < Eighth grade | 2 (0.8) | 1 (1.5) | |
| Some high school | 7 (2.9) | 5 (7.5) | |
| High school/GED | 44 (18.3) | 10 (14.9) | |
| Some college | 107 (44.6) | 31 (46.3) | |
| 4 y college | 47 (19.6) | 7 (10.4) | |
| Graduate level | 33 (13.8) | 13 (19.4) | |
| Patient’s spouse | 108 (45.0) | 16 (23.9) | < .01 |
| Present at time of death | 199 (82.9) | 51 (76.1) | .21 |
| FS-ICU (n = 305) | 81.6 (SD, 15.4) | 80.1 (SD, 19.8) | .13 |
| QODD-1 (n = 296) | 7.4 (SD, 2.8) | 6.7 (SD, 3.3) | .58 |
Data presented as mean (SD) or No. (%), unless otherwise indicated. See Table 1 and 2 legends for expansion of abbreviations.
Data representative of the 307 patients who had a family member fill out a survey.
t Test with unequal variances or χ2 test.
For private/Medicare, n = 237; for underinsured, n = 64.
Determined by first International Classification of Diseases, Ninth Revision code listed; this reflects most reimbursable, not necessarily primary diagnosis.
As reported on death certificate.
Proportion among patients with medical record documentation of presence/absence of living will.
Adjusted for inflation and reported in 2013 US dollars.
Family-Assessed Outcomes for Underinsured Patients
For underinsured patients, we found strong evidence of a positive association between the family-assessed QODD-1 and average daily ICU costs (P = .01), indicating that higher daily costs in the ICU were associated with higher quality-of-dying ratings. We observed this same relationship with the FS-ICU score (P < .01). In sensitivity analyses, results were similar for Medicaid and uninsured patients when assessed separately (e-Table 1 (124.2KB, pdf) ). Results were also consistent after excluding patients who died on day of admission, as this is known to be the most expensive day of an ICU stay (e-Table 2 (124.2KB, pdf) ).29 For total ICU costs and total hospital costs, however, we found no significant association with either the QODD-1 or FS-ICU (Table 3).
Family-Assessed Outcomes for Insured Patients
For patients with private insurance or Medicare, we found no significant association between the family-assessed QODD-1 and average daily ICU cost (P = .50), total ICU cost (P = .90), or total hospital cost (P = .79) in adjusted analyses. Results were similar for the FS-ICU (Table 3). Sensitivity analyses evaluating Medicare and privately insured patients separately demonstrated consistent results (e-Table 1 (124.2KB, pdf) ).
Nurse-Assessed QODD-1
The nurse-assessed QODD-1 item was significantly associated with average daily ICU costs (P < .01) and total hospital costs (P = .05) after adjusting for hospital, intervention (pre/post), patient insurance type, and patient age. All three cost variables were negatively correlated with nurse-assessed QODD-1, contrary to the findings for family-rated QODD-1, indicating that for nurse assessments, higher costs were associated with lower ratings of quality of dying (Table 5). In sensitivity analyses, we restricted the cohort to patients who also had a family questionnaire returned and found consistent results.
TABLE 5 ] .
Adjusted Regression Models for Nurse-Assessed Quality of Dying (n = 523)
| Cost, 2013 US $a | β (95% CI)b | P Value |
| Average daily cost in the ICU | −0.4 (−0.8, −0.1) | < .01 |
| Total ICU costs | −0.1 (−0.3, 0.0) | .07 |
| Total hospital costs | −0.2 (−0.3, 0.0) | .05 |
Cost variable of interest has been adjusted for inflation and log transformed so that all costs were compared at the 2013 US dollar value.
All models adjusted for intervention (pre/post), hospital, patient insurance type (underinsured vs private/Medicare), patient age, and clustered on nurse ID to account for correlation in nurse surveys.
Discussion
Our findings demonstrated that (1) among underinsured patients, higher average daily ICU costs were associated with better family-assessed quality of dying and satisfaction with care; (2) among patients with Medicare or private insurance, there was no association between end-of-life expenditure and family assessment of either quality of dying or satisfaction with care; and (3) higher costs (total hospital and daily ICU) at the end of life were associated with worse quality of dying from the nurses’ perspective. These findings suggest that, although health-care providers may view invasive, costly therapies at the end of life as negatively affecting the quality of dying, families’ assessments of the quality of dying and satisfaction with care depend on other factors and, for underinsured patients, actually increase with increased intensity of care at the end of life.
There are several possible explanations for our finding that higher average daily ICU costs were associated with higher satisfaction with care and quality of dying ratings as assessed by family members of underinsured patients. Using baseline data from this same trial and including a larger number of hospitals, Gerstel and colleagues30 reported that a longer duration of life-support withdrawal was associated with an increase in family satisfaction with care. They suggested that the longer duration of withdrawal of life support might be perceived by some families as providing time to prepare rather than as an additional burden on the patient. This experience of needing more time to reconcile the realities of serious illness and death may similarly be at play in the current data. Other research suggests that underinsured patients, often representing patients of lower socioeconomic status, are more likely to delay seeking medical care until they are in critical condition.31 For these reasons, death may be more likely to be an unexpected outcome, taking additional time with which to cope.
Additionally, our findings may be in line with those reporting differential preferences for end-of-life care by minorities or those of lower socioeconomic status32; many studies have found that these individuals are more likely to want life-extending care at the end of life and may feel reassured that “everything was done” to save the patient. These differential preferences may explain, in part, why we failed to find similar associations between ICU costs and ratings for families of patients with private or Medicare insurance. Alternatively, the group of private or Medicare insured may also have been sufficiently heterogeneous, making it difficult to observe a clear trend.
There are several possible explanations for our findings of no association between total ICU or hospital costs (vs average daily ICU costs) and the family-reported outcomes. First, average daily ICU costs more closely reflect intensity of life-sustaining treatments in the ICU and may be more influential in how quality of dying and satisfaction with care are perceived by family members. Second, variation in the influence of total ICU costs based on LOS may explain why there was no association. In additional exploratory analyses, we found patients with a short LOS had similar results for average daily ICU cost and total ICU cost, whereas for patients with longer LOS, no association was seen between total ICU cost and our outcomes of interest (e-Table 3 (124.2KB, pdf) ). This suggests that patients with high total ICU costs as a result of high intensity of care may rate quality of dying and satisfaction with care differently than patients who have high total costs resulting from a prolonged LOS. Last, since most of these patients died in the ICU, the questionnaires were intended to assess quality of dying and satisfaction with care in the ICU, perhaps attenuating the association between total hospital cost and family-assessed outcomes.
Finally, it is noteworthy that the association between nurse-assessed quality of dying and ICU costs was in the opposite direction of that seen for the family of underinsured patients. Prior studies have shown that ICU clinicians (nurses and physicians) have markedly different views regarding the value of intensive care at the end of life when compared with family members of critically ill patients.33 It seems likely that these differing views also extend to differences in how intensity and costs of care influence the perceived quality of dying.
Our study has several strengths. First, to our knowledge, this is the first study investigating the association between end-of-life expenditure and quality of dying in the ICU. Second, to our knowledge, this is also the first study examining the relationship between family satisfaction with care and ICU or hospital costs. Third, subjects were enrolled over a 5-year period in two diverse centers, reducing the risk of confounding by temporal trends or care specific to a single site.34
This study has several important limitations. First, the low response rate for families may have introduced selection bias for which we were unable to fully account. We previously found evidence that patients who had a family member respond to the surveys had more indicators of palliative care than patients who did not.35 Additionally, nurses appeared to be more likely to respond if care at the end of life was particularly aggressive; this may have introduced a potential for response bias. Second, this study took place in two hospitals in one region of the United States and may not generalize to other regions. In addition, the high proportion of deaths related to trauma and low proportion of deaths related to cancer in this cohort suggest heterogeneity in ICU populations and may also limit the generalizability of our findings. Last, we recognize that residual confounding—especially by socioeconomic status—may have biased our results. Although we assessed patient and family member level of education and median household income based on zip code for potential confounding and effect modification, we recognize that education level and estimated household income by zip code are not exact measures of socioeconomic status. Actual patient and family income data were not available. Nevertheless, describing the association between perceived quality of dying and satisfaction with care and expenditures at the end of life provides valuable information that can be used to generate hypotheses for future studies.
Conclusions
Our study suggests that nurses view invasive, costly therapies at the end of life as negatively impacting the quality of dying. However, families’ evaluations of the quality of dying and satisfaction with care in the ICU setting appear to be influenced by different factors and are modified by patient insurance status, such that families of patients who are underinsured rate the quality of dying higher in the setting of increased average ICU daily costs, whereas no such relationship was identified for families of patients who are insured.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: N. K. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. N. K. served as primary author, designed the study protocol, analyzed the data, and wrote the manuscript and its revisions, and approved the final version of the manuscript. She attests that no undisclosed authors contributed to the manuscript. R. A. E. and J. R. C. designed the study protocol, supervised data collection, reviewed the manuscript, and approved the final version of the manuscript; and D. C. B. and N. B. C. analyzed the data, reviewed the manuscript, and approved the final version of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsors had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: This work was performed at the University of Washington.
Additional information: The e-Tables can be found in the Supplemental Materials section of the online article.
ABBREVIATIONS
- FS-ICU
Family Satisfaction in the ICU
- LOS
length of stay
- QODD-1
Single-item quality of dying rating from the Quality of Dying and Death Questionnaire
Footnotes
FUNDING/SUPPORT: This work was supported by the National Institute of Nursing Research [Grant R01NR005226] and the National Institute of General Medical Sciences [Grant 5T32GM086270].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, et al. ; Robert Wood Johnson Foundation ICU End-Of-Life Peer Group. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32(3):638-643. [DOI] [PubMed] [Google Scholar]
- 2.Curtis JR, Engelberg RA, Bensink ME, Ramsey SD. End-of-life care in the intensive care unit: can we simultaneously increase quality and reduce costs? Am J Respir Crit Care Med. 2012;186(7):587-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010;45(2):565-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seshamani M, Gray AM. A longitudinal study of the effects of age and time to death on hospital costs. J Health Econ. 2004;23(2):217-235. [DOI] [PubMed] [Google Scholar]
- 5.Pastores SM, Dakwar J, Halpern NA. Costs of critical care medicine. Crit Care Clin. 2012;28(1):1-10. [DOI] [PubMed] [Google Scholar]
- 6.Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38(1):65-71. [DOI] [PubMed] [Google Scholar]
- 7.Scheunemann LP, McDevitt M, Carson SS, Hanson LC. Randomized, controlled trials of interventions to improve communication in intensive care: a systematic review. Chest. 2011;139(3):543-554. [DOI] [PubMed] [Google Scholar]
- 8.Molloy DW, Guyatt GH, Russo R, et al. Systematic implementation of an advance directive program in nursing homes: a randomized controlled trial. JAMA. 2000;283(11):1437-1444. [DOI] [PubMed] [Google Scholar]
- 9.Schneiderman LJ, Gilmer T, Teetzel HD. Impact of ethics consultations in the intensive care setting: a randomized, controlled trial. Crit Care Med. 2000;28(12):3920-3924. [DOI] [PubMed] [Google Scholar]
- 10.Schneiderman LJ, Gilmer T, Teetzel HD, et al. Effect of ethics consultations on nonbeneficial life-sustaining treatments in the intensive care setting: a randomized controlled trial. JAMA. 2003;290(9):1166-1172. [DOI] [PubMed] [Google Scholar]
- 11.Dy SM, Aslakson R, Wilson RF, Fawole OA, Lau BD, Martinez KA, Vollenweider D, Apostol C, Bass EB. Closing the Quality Gap: Revisiting the State of the Science. Vol 8: Improving Health Care and Palliative Care for Advanced and Serious Illness. Evidence Report No. 208. (Prepared by Johns Hopkins University Evidence-based Practice Center under Contract No. 290-2007-10061-I.) Rockville, MD: Agency for Healthcare Research and Quality. 2012; AHRQ Publication 12(13)-E014-EF. [PMC free article] [PubMed]
- 12.Wenger NS, Rosenfeld K. Quality indicators for end-of-life care in vulnerable elders. Ann Intern Med. 2001;135(8 pt 2):677-685. [DOI] [PubMed] [Google Scholar]
- 13.Nathan Cummings Foundation, Fetzer Institute, George H. Gallup International Institute. Spiritual Beliefs and the Dying Process: A Report on a National Survey. Princeton, NJ: George H. Gallup International Institute; 1997.
- 14.Teno JM, Gozalo PL, Bynum JP, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curtis JR, Nielsen EL, Treece PD, et al. Effect of a quality-improvement intervention on end-of-life care in the intensive care unit: a randomized trial. Am J Respir Crit Care Med. 2011;183(3):348-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Curtis JR, Treece PD, Nielsen EL, et al. Integrating palliative and critical care: evaluation of a quality-improvement intervention. Am J Respir Crit Care Med. 2008;178(3):269-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Treece PD, Engelberg RA, Shannon SE, et al. Integrating palliative and critical care: description of an intervention. Crit Care Med. 2006;34(suppl 11):S380-S387. [DOI] [PubMed] [Google Scholar]
- 19.Glavan BJ, Engelberg RA, Downey L, Curtis JR. Using the medical record to evaluate the quality of end-of-life care in the intensive care unit. Crit Care Med. 2008;36(4):1138-1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heyland DK, Cook DJ, Dodek PM. Prevention of ventilator-associated pneumonia: current practice in Canadian intensive care units. J Crit Care. 2002;17(3):161-167. [DOI] [PubMed] [Google Scholar]
- 21.Heyland DK, Rocker GM, Dodek PM, et al. Family satisfaction with care in the intensive care unit: results of a multiple center study. Crit Care Med. 2002;30(7):1413-1418. [DOI] [PubMed] [Google Scholar]
- 22.Wall RJ, Engelberg RA, Gries CJ, Glavan B, Curtis JR. Spiritual care of families in the intensive care unit. Crit Care Med. 2007;35(4):1084-1090. [DOI] [PubMed] [Google Scholar]
- 23.Heyland D. Family satisfaction with care in the intensive care unit survey. Canadian Researchers at the End of Life Network website. http://www.thecarenet.ca/docs/fss/FS_ICU_34.pdf. Accessed June 22, 2014.
- 24.Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96(1):102-109. [DOI] [PubMed] [Google Scholar]
- 25.Muni S, Engelberg RA, Treece PD, Dotolo D, Curtis JR. The influence of race/ethnicity and socioeconomic status on end-of-life care in the ICU. Chest. 2011;139(5):1025-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48(4):817-838. [Google Scholar]
- 27.Szpiro AA, Rice KM, Lumley T. Model-robust regression and a Bayesian “sandwich” estimator. Ann Appl Stat. 2010;4(4):2099-2113. [Google Scholar]
- 28.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13-22. [Google Scholar]
- 29.Kahn JM, Rubenfeld GD, Rohrbach J, Fuchs BD. Cost savings attributable to reductions in intensive care unit length of stay for mechanically ventilated patients. Med Care. 2008;46(12):1226-1233. [DOI] [PubMed] [Google Scholar]
- 30.Gerstel E, Engelberg RA, Koepsell T, Curtis JR. Duration of withdrawal of life support in the intensive care unit and association with family satisfaction. Am J Respir Crit Care Med. 2008;178(8):798-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med. 1991;114(4):325-331. [DOI] [PubMed] [Google Scholar]
- 32.Johnson KS. Racial and ethnic disparities in palliative care. J Palliat Med. 2013;16(11):1329-1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sprung CL, Carmel S, Sjokvist P, et al. ; ETHICATT Study Group. Attitudes of European physicians, nurses, patients, and families regarding end-of-life decisions: the ETHICATT study. Intensive Care Med. 2007;33(1):104-110. [DOI] [PubMed] [Google Scholar]
- 34.DeCato TW, Engelberg RA, Downey L, et al. Hospital variation and temporal trends in palliative and end-of-life care in the ICU. Crit Care Med. 2013;41(6):1405-1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kross EK, Engelberg RA, Shannon SE, Curtis JR. Potential for response bias in family surveys about end-of-life care in the ICU. Chest. 2009;136(6):1496-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement