Abstract
Integrating research on stress generation and the interpersonal theory of suicide we examined whether eating disorder symptoms are related to stress generation and whether negative life events (stressors) contribute to feelings of burdensomeness and low belongingness. At two time points (approximately one month apart), participants (n = 186; 75% female) completed questionnaires measuring eating disorder symptoms, negative life events, burdensomeness, and belongingness. Regression analyses indicated that while controlling for depression, anxiety, and baseline frequency of negative events, dietary restraint significantly predicted negative events at follow-up. Dietary restraint indirectly influenced higher levels of perceived burdensomeness and low belongingness through its influence on negative events. Thus, dietary restraint may contribute to stress generation, and in turn exacerbate feelings of burdensomeness and low belongingness, two important constructs of the interpersonal theory of suicide. Greater understanding of these factors could lead to more effective and targeted suicide interventions for individuals who restrict food intake.
Keywords: Eating Disorders, Suicide, Stress Generation, Dietary Restraint, Suicidality, Interpersonal Theory of Suicide
1. Introduction
Eating disorders are serious mental illnesses (Klump, Bulik, Kaye, Treasure, & Tyson, 2009) that occur in a small percentage of the population and are associated with an increased risk of mortality (Franko et al., 2013; Smink, van Hoeken, & Hoek, 2012). This increased mortality risk can be partially attributed to an elevated risk for death by suicide among individuals with eating disorders (Arcelus, Mitchell, Wales, & Nielsen, 2011; Bodell, Joiner, & Keel, 2013; Crow et al., 2009; Preti, Rocchi, Sisti, Camboni, & Miotto, 2011). Risk for death by suicide is particularly elevated among individuals with anorexia nervosa (AN). Large meta-analyses have revealed that one out of five deaths among those with AN are from suicide (Arcelus et al., 2011), and that individuals with AN are 40 times more likely to die by suicide compared to individuals in the general population (Preti et al., 2011). Given the high rates of suicide among individuals with eating disorders, and particularly AN, it is important to understand why and how eating disorder symptoms lead to this outcome.
The interpersonal theory of suicide (IPTS) suggests that people die by suicide when three factors are present: low belonging, high perceived burdensomeness, and acquired capability for suicide (Joiner, 2005;K. A. Van Orden et al., 2010). Understanding how eating disorder behaviors affect the three constructs of the IPTS may offer insight into the elevated rates of suicide among individuals with eating disorders. Previous work has found a positive relationship between eating disorders and acquired capability for suicide (ACS) (Selby et al., 2010; Smith et al., 2013). Importantly, this positive relationship may not be generally applicable to all eating disorders, but rather, specific eating disorder behaviors may differentially increase ACS. For example, there is evidence to suggest that repetitive, painful, and provocative behaviors such as self-induced vomiting and laxative use are associated with suicidal behavior among individuals with the binge-purge subtype of AN, while the painful experience of continuous starvation is associated with suicidal behavior among individuals with the restricting subtype of AN (Selby et al., 2010). Further, over-exercise is associated with ACS and suicide attempts among individuals with bulimia nervosa (Smith et al., 2013). However, no research to date has directly examined the relationship between eating disorder behaviors and the other IPTS constructs: perceived burdensomeness and low belonging. Thus, one aim of the present study is to examine the relationship between various eating disorder symptoms and perceived burdensomeness and low belonging.
Informed by research on the stress generation hypothesis (Hammen, 1991, 2006), the present study also aims to examine a third variable that may indirectly affect (Preacher & Hayes, 2004) the relationship between eating disorder symptoms and the IPTS constructs of perceived burdensomeness and low belonging: negative life events. The stress generation hypothesis theorizes that individuals with depression actively generate additional stress in their lives, particularly interpersonal stress, which subsequently worsens depressive symptoms (Hammen, 1991, 2006). The depression literature provides substantial support for the stress generation hypothesis (Liu & Alloy, 2010). Meanwhile, research has consistently found that eating disorder behaviors are associated with significant psychosocial impairment (Klump et al., 2009; Mond, Hay, Rodgers, & Owen, 2009), that stressful life events contribute to eating disorder development and relapse (Grilo et al., 2012), and that low social support and negative life events can predict increases in eating disorder symptoms (Bodell, Smith, Holm-Denoma, Gordon, & Joiner, 2011). Given the links between stress and eating disorder maintenance and relapse, it would be important to know if behaviors and experiences specific to eating disorders are not only associated with stress, but also contribute to stress generation, as is the case with depression.
Previous research examining the potential connection between eating disorders and stress generation (Bodell et al., 2012) found that in a sample of 290 female undergraduates, bulimic symptoms and drive for thinness at baseline did not predict, above and beyond depressive symptoms, negative life events approximately eight weeks later. However, it is important to note that Bodell and colleagues (2012) examined only three aspects of eating disorders (bulimic symptoms, body dissatisfaction, and drive for thinness) in relation to stress generation. Notably missing from their examination was actual dietary restraint, or attempts to reduce caloric intake, which is a prominent feature of both anorexia and bulimia (American Psychiatric Association, 2013). As previously discussed, there appear to be different routes to increased ACS across eating disorder behaviors and diagnoses (Selby et al., 2010; Smith et al., 2013). This research suggests that distinct eating disorder behaviors contribute differently to IPTS constructs, and that eating disorder behaviors associated with AN may be particularly harmful. Although bulimic symptoms, body dissatisfaction, and drive for thinness did not generate stress above and beyond depressive symptoms in the Bodell et al. (2012) study, other eating disorder symptoms (i.e., restraint) may. Thus, an additional aim of the present study was to replicate and extend the Bodell et al. (2012) study by examining whether restraint might contribute to increased stress generation. In keeping with previous studies (Bodell et al., 2012; Hammen, 1991; Joiner, Wingate, Gencoz, & Gencoz, 2005) we operationalized stress generation in the current study as an increased occurrence of negative life events over a particular time span.
To summarize, the present study aims to integrate research on stress generation, disordered eating, and the IPTS. The main aim of this study is to examine whether dietary restraint may be related to stress generation, defined as an increased occurrence of negative life events. Additionally, given the often interpersonal nature of stress generation, as well as the existing literature on stress generation in depression and eating disorders, the present study examines whether the experience of negative life events is related to burdensomeness and low belongingness. Specifically, we examine the relationship between various disordered eating behaviors at Time 1 (T1), and burdensomeness and belongingness at Time 2 (T2; approximately one month later) in an undergraduate population, and further, we examine whether that relationship is indirectly affected by negative life events at T2.
2. Methods
All procedures described below were approved by the university's Institutional Review Board.
2.1. Participants
One hundred ninety-four undergraduates from a large southeastern university participated in exchange for course credit. To be eligible for participation, participants had to be at least 18 years old. There were no other inclusion or exclusion criteria. Participants that did not complete the Time 2 study visit (n = 8) were not included in the present analyses, which resulted in a final sample size of 186. A one-way ANOVA revealed there were no significant differences between T2 completers and non-completers on any T1 scale or subscale scores included in the analyses, or on demographic variables (all p's > .09). Participants were majority female (78.0%; n = 145). Participants primarily self-reported their race as White (76.3%; n = 142), followed by Black or African-American (8.6%, n = 16), Asian (3.8%, n = 7), Hawaiian/Other Pacific Islander (0.5%, n = 1), and other or unanswered (10.8%, n = 20). The participants ranged in age from 18 years old to 25 years old (mean age = 18.7 years, SD = 1.2 years).
2.2. Procedure
Participants chose to enroll in the present study after reading an online list of studies (including brief descriptions of each study) for which they could receive research participation course credit in exchange for participating. All study activities were completed online via a secure website. Participants read an informed consent form and then provided informed consent via an electronic signature. Study participation involved filling out self-report questionnaires on two occasions. The study was designed to have a minimum of 28 days between Time 1 and Time 2, however, seven participants prematurely completed Time 2 and thus had a slightly shorter interval between time points. The mean length of time between T1 and T2 was 31 days (SD = 4.38 days, Range: 19–58 days).
2.3. Measures
The Beck Depression Inventory II (BDI-II) is a 21-item scale designed to measure the severity of self-reported depression (Beck, Steer, & Brown, 1996). Respondents are asked to indicate, on a scale from 0 to 3, how much each item describes the way the respondent has been feeling in the past two weeks. Items ask about many common depressive symptoms (e.g., feeling indecisive, irritable, or worthless; experiencing changes in sleeping patterns or appetite). The BDI-II yields a total score from 0 to 63, with higher scores indicating more severe depression. Specifically, scores below 13 indicate no depression, scores from 13 to 19 indicate mild depression, and scores from 20 to 63 indicate depression (Dozois, Dobson, & Ahnberg, 1998). The BDI-II has been shown to have good psychometric properties (Beck, Steer, Ball, & Ranieri, 1996) and has been used with undergraduate samples (Dozois et al., 1998). For the purposes of the present study, one item from the BDI-II (item #9, which asks about suicidal thoughts and wishes) was removed from the instrument. The nature of the study (e.g. participation occurring exclusively online) was such that investigators could not guarantee clinically sufficient and prompt assessment and intervention if suicidality was endorsed. Furthermore, the information assessed for by the BDI-II suicidality item was not necessary for the present analyses. Therefore, in the interest of participant safety the investigators opted to omit the BDI-II suicidality item. The BDI-II was used as the measure of depression in the present study; it was administered at Time 1. Cronbach's alpha for the present sample was 0.81 at T1.
The Beck Anxiety Inventory (BAI) is a self-report, 21-item survey designed to assess severity of anxiety in the past two weeks (Beck, Epstein, Brown, & Steer, 1988). The BAI asks about many common symptoms of anxiety (e.g. fear of losing control, inability to relax, feelings of nervousness, psychosomatic symptoms such as feeling dizzy or experiencing a racing heart). Using a 4 point Likert scale (from not at all‖ to severely‖) respondents indicate how much they have been affected by particular symptoms in the past two weeks. The BAI yields a score from 0 to 63, with higher scores indicating more severe anxiety. Specifically, scores below 8 indicate minimal anxiety, scores ranging from 8 to 15 indicate mild anxiety, scores ranging from 16 to 25 indicate moderate anxiety, and scores 26 and higher indicate severe anxiety; the suggested cutoff for clinically significant anxiety on the BAI is 16 (Beck & Steer, 1993). The BAI has good internal consistency, test-retest reliability, and concurrent and discriminant validity (Beck et al., 1988) and is validated for use with undergraduate samples (Creamer, Foran, & Bell, 1995). The BAI was used as the measure of anxiety in the present study; it was administered at T1. Cronbach's alpha for the present sample at T1 was 0.84.
The Acute Life Events Questionnaire (Haeffel et al., 2007) is a brief, modified version of the Life Events Questionnaire (LEQ) (Needles & Abramson, 1990) and was used to assess acute, naturally occurring stressful life events that are important to college students. The ALEQ assesses a broad range of events (e.g. school achievement, interpersonal, and romantic). In the present study, the measure consisted of 28 yes/no items, and respondents were asked to indicate whether the event or situation described in each item had happened to them in the past 6 months (e.g., Put down or made fun of my boyfriend/girlfriend/spouse [e.g., called names; ridiculed; etc.]”; Sginificant fight or argument with boyfriend/girlfriend/spouse that led to a serious consequence [e.g., you or significant other crying; leaving common residence for one night, etc.]”). This yielded a score from 0 to 28. In the present study, the ALEQ was used as a measure of negative life events and was administered at both T1 and T2. Alphas in the current sample were 0.82 (T1) and 0.82 (T2).
The Eating Disorder Examination Questionnaire – Version 4 (EDEQ-4) is a self-report questionnaire (Fairburn & Beglin, 1994) based on the Eating Disorder Examination (EDE), a structured interview (Cooper & Fairburn, 1987). The EDEQ-4 consists of 36 items that assess for eating disorder thoughts and behaviors in the previous 28 days; the EDEQ-4 has good reliability and validity (Berg, Peterson, Frazier, & Crow, 2012; Luce & Crowther, 1999; Mond, Hay, Rodgers, Owen, & Beumont, 2004). The EDEQ-4 yields a score for each of four subscales: restraint, eating concern, shape concern, and weight concern. The restraint subscale consists of 5 items that assess for thoughts and behaviors related to caloric restriction (e.g. Have you been deliberately trying to limit the amount of food you eat to influence your shape or weight?”; Have you wanted your stomach to be empty?”). The eating concern subscale consists of 5 items that ask about preoccupation with food and its calorie content, fear of losing control over eating, eating in secret, guilt after eating because of the effect on shape and weight, and concern over being seen eating by other people. The shape concern subscale contains 8 items that assess for concerns, preoccupations, and over-evaluation regarding body shape. Lastly, the weight concern subscale consists of 5 items that assess for concerns, preoccupations, and over-evaluation regarding body weight. In the present study the EDEQ-4 subscales for restraint, weight concern, shape concern, and eating concern were used as measures of their corresponding eating disorder symptomatology at T1. Cronbach's alphas for all subscales at T1 were good: 0.87 (weight concerns), 0.93 (shape concerns), 0.84 (eating concerns), and 0.81 (restraint).
The Eating Disorder Inventory (EDI) is a 64-item self-report questionnaire that assesses behavioral and psychological traits common in anorexia nervosa and bulimia nervosa (Garner, Olmstead, & Polivy, 1983). The EDI has strong psychometric properties (Garner et al., 1983). The EDI contains eight subscales: drive for thinness, bulimia, body dissatisfaction, ineffectiveness, perfectionism, interpersonal distrust, interoceptive awareness, and maturity fears. The EDI drive for thinness subscale consists of seven items assessing for excessive preoccupation with thinness, weight, and dieting (e.g., I am terrified of gaining weight”). The EDI bulimia subscale consists of seven items that assess for a tendency towards binging and purging (e.g., I eat or drink in secrecy”; I have the thought of trying to vomit to lose weight”). The EDI body dissatisfaction subscale consists of nine items that assess for the belief that specific parts of the body (particularly those parts associated with pubertal shape change and increased fatness) are too large (e.g., I think that my hips are too big”; I think that my buttocks are too large”). Participants respond to each item by using a scale from 1 (never) to 6 (always), and higher scores on each subscale indicate more severe pathology. As in the Bodell et al. (2012) study, the EDI subscale scores for drive for thinness, bulimia, and body dissatisfaction were used in the present study as measures of their corresponding eating disorder thoughts and behaviors at Time 1. Normative data (Garner & Olmstead, 1984) are used to aid interpretation of scores: in a sample (N = 770) of nonpatient college females, 10% of participants scored 13 or higher on the drive for thinness subscale, 5 or higher on the bulimia subscale, and 21 or higher on the body dissatisfaction subscale; among eating disordered patients 12% of participants scored 20 or higher on the drive for thinness subscale (N = 889), 12% of participants scored 17 or higher on the bulimia subscale (N = 760; sample excluded individuals with anorexia nervosa – restricting subtype), and 16% of participants scored 26 or higher on the body dissatisfaction subscale (N = 889). All three subscales demonstrated good reliability at T1; alphas were 0.87 (bulimia subscale), 0.93 (body dissatisfaction subscale), and 0.91 (drive for thinness subscale).
The original version of the Interpersonal Needs Questionnaire (INQ) is a 25-item selfreport instrument derived from the IPTS (Van Orden, Cukrowicz, Witte, & Joiner, 2012). The INQ is designed to assess low belongingness (conceptualized as the extent to which the respondent feels a lack of connection to others) and perceived burdensomeness (conceptualized as the extent to which the respondent believes that others would be better off without him or her). The INQ yields subscale scores for each of these two constructs; the belongingness subscale consists of 10 items (e.g., These days I feel unwelcome in most social situations”); the burdensomeness subscale consists of 15 items (e.g., These days I think my death would be a relief to the people in my life”). Participants are instructed to use a Likert scale from 1 (not at all true for me) to 7 (very true for me) to respond to each item based on how they have been feeling recently. Higher subscale scores indicate higher levels of perceived burdensomeness or low (i.e., thwarted) belongingness. The INQ was administered at T1 and T2. Both subscales demonstrated good reliability; alphas for the belongingness subscale were 0.92 (T1) and 0.92 (T2); alphas for the burdensomeness subscale were 0.92 (T1) and 0.94 (T2).
3. Statistical Analyses
SPSS version 21.0 (IBM Corp, 2012) was used to conduct the regression analyses. Given noted limitations with Baron and Kenny's (1986) traditional methods for testing for mediation (Hayes, 2009; MacKinnon et al., 2002; Preacher & Hayes, 2004; Zhao, Lynch, & Chen, 2010), and recent suggestions to test for indirect effects when conducting mediation analyses (Hayes, 2009; MacKinnon et al., 2002; Preacher & Hayes, 2004; Zhao, Lynch, & Chen, 2010), we examined indirect effects using the PRODCLIN program (MacKinnon et al., 2007). Whereas the traditional method of testing mediation (Baron & Kenny, 1986) requires that a significant relationship exists between the independent and dependent variable, tests for indirect effects consider the value of all paths of the model and take into account relationships that may exist (e.g. between the independent variable and mediator, and between the mediator and dependent variable) even in the absence of a significant relationship between the independent and dependent variable. In other words, the independent variable may have an indirect effect on the dependent variable through its effects on a mediating variable – this relationship can be examined using tests of indirect effects. In the present study, the PRODCLIN program (MacKinnon et al., 2007) was used to test the indirect effect of restraint on burdensomeness and low belongingness through negative life events. PRODCLIN uses the distribution of the product method to test for mediation; it examines the product of the unstandardized path coefficients divided by the pooled standard error of the path coefficients (αβ/sαβ) and a confidence interval is generated, whereby statistical significance is indicated by the absence of zero from the confidence interval.
4. Results
Descriptive statistics, including correlations, means, and standard deviations are presented in Table 1.
Table 1. Means and Standard Deviations for, and Intercorrelations between, Measures.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ALEQ T1 | -- | ||||||||||||
| 2. ALEQ T2 | .51** | -- | |||||||||||
| 3. BDI T1 | .39** | .40** | -- | ||||||||||
| 4. BAI T1 | .42** | .41** | .49** | -- | |||||||||
| 5. EDI-Bul T1 | .14* | .19** | .40** | .30** | -- | ||||||||
| 6. EDI-BD T1 | .14 | .15 | .39** | .28** | .41** | -- | |||||||
| 7. EDI-DT T1 | .12 | .16* | .33** | .32** | .58** | .74** | -- | ||||||
| 8. EDEQ-4 Restr T1 | .14* | .28** | .22** | .27** | .44** | .49** | .75** | -- | |||||
| 9. EDEQ-4 EC T1 | .19* | .28** | .39** | .39** | .63** | .55** | .73** | .59** | -- | ||||
| 10. EDEQ-4 SC T1 | .18* | .22** | .37** | .35** | .51** | .79** | .80** | .63** | .73** | -- | |||
| 11. EDEQ-4 WC T1 | .18* | .20** | .32** | .36** | .49** | .75** | .78** | .62** | .75** | .93** | -- | ||
| 12. INQ Burd T2 | .28** | .26** | .51** | .32** | .34** | .31** | .22** | .04 | .36** | .33** | .31** | -- | |
| 13. INQ LowBel T2 | .21** | .21* | .51** | .34** | .31** | .36** | .24** | .03 | .33** | .37** | .31** | .77** | -- |
| M | 3.86 | 3.03 | 8.14 | 8.31 | 13.05 | 29.15 | 19.70 | 1.03 | 0.74 | 1.82 | 1.65 | 32.10 | 24.59 |
| SD | 3.89 | 3.50 | 6.38 | 6.71 | 5.67 | 11.62 | 9.04 | 1.21 | 1.08 | 1.64 | 1.56 | 13.23 | 11.70 |
| Range | 0-18 | 0-20 | 0-41 | 0-34 | 6-35 | 9-54 | 6-42 | 0-5.2 | 0-6 | 0-6 | 0-6 | 15-77 | 10-66 |
Note: ALEQ = Acute Life Events Questionnaire; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; EDI = Eating Disorder Inventory; Bul = Bulimia; BD= Body Dissatisfaction; DT = Drive for Thinness; EDEQ-4 = Eating Disorder Examination Questionnaire-4; Restr = Restraint; EC = Eating Concern; SC = Shape Concern; WC = Weight Concern; INQ = Interpersonal Needs Questionnaire; Burd = Burdensomeness; LowBel = Low Belongingness;
= p<.05,
= p<.001.
4.1. Total Effect of Eating Disorder Behaviors on Burdensomeness and Low Belongingness
In order to determine whether eating behaviors lead to increases in burdensomeness and belongingness we conducted two hierarchical regressions. In the prediction of T2 burdensomeness we entered T1 burdensomeness in the first step (thereby creating residual change scores from baseline to follow-up) (Cohen & Cohen, 1983), and then we entered our eating disorder variables (EDI-Bulimia, EDI-Body Dissatisfaction, EDI-Drive for Thinness, EDEQ-4 Eating Concern, EDEQ-4 Shape Concern, EDEQ-4 Weight Concern, EDEQ-4 Restraint) in the second step. This same entry method was used in the prediction of T2 low belongingness, however, T1 belongingness was entered in the first step. Contrary to predictions, none of the eating disorder variables led to increases in perceived burdensomeness (all ps > .24) or low belongingness (all ps > .33).
4.2. Examining whether Restraint Increases Negative Life Events
Following Bodell et al. (2012) we tested whether symptoms of eating disorders, depression, and/or anxiety at T1 predicted T2 negative life events. In the prediction of T2 negative life events we conducted a hierarchical regression in which T1 negative life events was entered in the first step, T1 depression and anxiety were added in the second step, and our eating disorder variables (EDI-Bulimia, EDI-Body Dissatisfaction, EDI-Drive for Thinness, EDEQ-4 Eating Concern, EDEQ-4 Shape Concern, EDEQ-4 Weight Concern, EDEQ-4 Restraint) were added in the third step, see Table 2. When controlling for depression, anxiety, and T1 negative life events, EDE restraint was the only eating disorder variable that predicted increases in T2 negative life events, t = 3.01 , p = .003, rpartial = 0.23. Similar to Bodell et al. (2012), depression also remained a significant predictor of negative life events (t = 1.94 , p = .05, rpartial = 0.15); anxiety remained a significant predictor as well (t = 2.04 , p = .04, rpartial = 0.16). Interestingly, EDI Drive for Thinness demonstrated a significant negative relationship with negative life events (t = -2.02 , p = .05, rpartial = -0.15), indicating that drive for thinness was associated with fewer negative life events at T2.
Table 2. Time 1 Restraint Predicts Time 2 Negative Life Events (ALEQ).
| Step | B | St. Error | t | Partial r | p | R2Δ | |
|---|---|---|---|---|---|---|---|
| 1 | (Constant) | 1.22 | .322 | 3.80 | .26 | ||
| ALEQ T1 | .47 | .06 | 7.94 | .51 | <.001 | ||
| 2 | ALEQ T1 | .35 | .06 | 5.56 | .39 | <.001 | .07 |
| BDI T1 | .09 | .04 | 2.17 | .16 | .03 | ||
| BAI T1 | .10 | .04 | 2.46 | .18 | .02 | ||
| 3 | ALEQ T1 | .34 | .06 | 5.42 | .39 | <.001 | .05 |
| BDI T1 | .09 | .04 | 1.94 | .15 | .05 | ||
| BAI T1 | .08 | .04 | 2.04 | .16 | .04 | ||
| EDI-Bul | -.02 | .05 | -.34 | -.03 | .73 | ||
| EDI-BD | -.02 | .03 | -.66 | -.05 | .51 | ||
| EDI-DT | -.10 | .05 | -2.02 | -.15 | .05 | ||
| EDEQ-4 EC | .55 | .36 | 1.52 | .12 | .13 | ||
| EDEQ-4 SC | .24 | .40 | .62 | .05 | .54 | ||
| EDEQ-4 WC | -.18 | .40 | -.45 | -.03 | .66 | ||
| EDEQ-4 Restrai nt . | .80 | .27 | 3.01 | .23 | .003 | ||
Note: ALEQ = Acute Life Events Questionnaire; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; EDI = Eating Disorder Inventory; Bul = Bulimia; BD= Body Dissatisfaction; DT = Drive for Thinness; EDEQ-4 = Eating Disorder Examination Questionnaire-4; Restr = Restraint; EC = Eating Concern; SC = Shape Concern; WC = Weight Concern
4.3. Indirect Effect of Negative Life Events
The unstandardized path coefficients and standard errors of the path coefficients for the indirect effects of the =a‘ path (i.e., T1 restraint predicting T2 negative life events; path a = .82, SEa = .21) and the =b‘ path (i.e., T2 negative life events predicting T2 low belongingness; path b = 1.28, SEb= .25; T2 negative life events predicting T2 burdensomeness; path b = 1.54, SEb = .30) were entered into PRODCLIN to yield the following 95% confidence intervals: low belongingness [.45, 1.79], burdensomeness [.55, 2.15]. The absence of zero from the confidence intervals indicated that restraint indirectly influenced burdensomeness and low belongingness through its effect on negative life events (figure 1).
Figure 1. Indirect Effects of Negative Life Events.
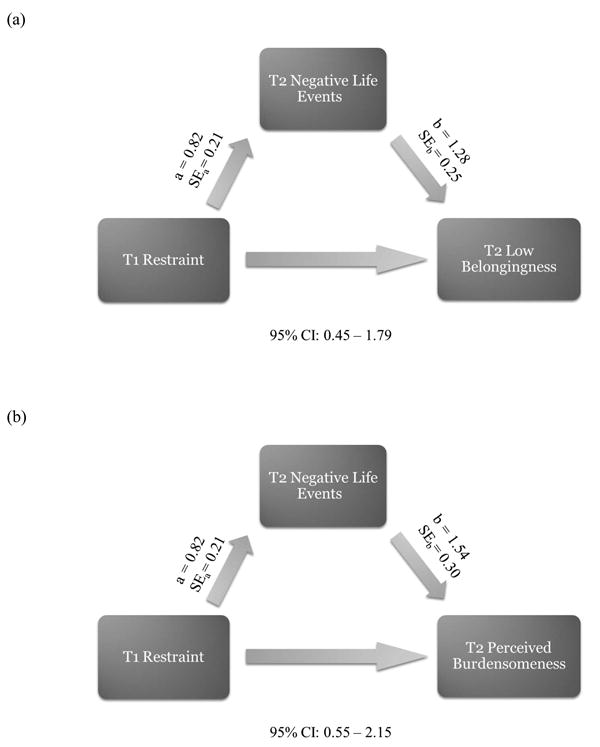
Models depicting the relationships between (a) Time 1 restraint, Time 2 negative life events, and Time 2 low belongingness and (b) Time 1 restraint, Time 2 negative life events, and Time 2 perceived burdensomeness. The absence of zero from the 95% confidence intervals (CIs) indicates that restraint indirectly influences burdensomeness and low belongingness through its effect on negative life events.
5. Discussion
The primary aim of the present study was to replicate and extend previous research on eating disorder symptoms and stress generation (Bodell et al., 2012). We found that when controlling for T1 depression, anxiety, and negative life events, only restraint (and not body dissatisfaction, bulimic symptoms, eating concern, shape concern, or weight concern) predicted more T2 negative life events. Interestingly, the present study did find a relationship between drive for thinness and later negative life events, however, the relationship was in the opposite direction as hypothesized: drive for thinness at T1 predicted fewer negative life events at T2. An additional aim of the present study was to examine the relationship between eating disorder symptoms and two constructs of the IPTS – burdensomeness and belongingness. Counter to our prediction, when controlling for perceived burdensomeness at T1, eating disorder symptoms did not predict perceived burdensomeness at T2, and when controlling for low belongingness at T1, eating disorder symptoms did not predict low belongingness at T2. However, there was an indirect effect of restraint on burdensomeness and belongingness, such that restraint indirectly increased both burdensomeness and belongingness through its effects on negative life events. In other words, it appears the relationships between restraint and burdensomeness, and restraint and belongingness, both flow through negative life events.
These results suggest that dietary restraint may lead to negative life events, which in turn may lead to high perceived burdensomeness and low belongingness. Although the design of the present study prohibits us from determining a specific causal mechanism by which dietary restraint leads to this outcome, there are several possible explanations. In many cases, dietary restraint may be predicated upon secrecy and may therefore necessitate some degree of social withdrawal, or avoidance of social situations involving food (Klein & Walsh, 2003). Alternatively, restraint (or associated secrecy and withdrawal) may lead to other interpersonal conflicts, such as arguments with family or friends (Schmidt & Treasure, 2006; Sim et al., 2009). In either scenario, restraint would increase the likelihood of a negative interpersonal event and thereby decrease feelings of belongingness. Similarly, if restraint were to increase the occurrence of negative life events, it would follow that feelings of increased burdensomeness may result from knowing that one's eating disorder behaviors are causing relationship troubles, but feeling unable to change those behaviors. Additional research is needed to further explain why restraint specifically (and not body dissatisfaction, bulimic symptoms, eating concern, shape concern, and weight concern) may lead to the occurrence of negative life events.
Unexpectedly, the present study found one measure of eating disorder symptoms – drive for thinness – significantly predicted fewer negative life events at Time 2. It is possible that participants who scored high on the drive for thinness subscale of the EDI may more strongly internalize societal standards of a thin ideal” (Low et al., 2003) and desire to adhere to social norms and please others. Therefore, while the actions and behaviors involved in restriction may lead to negative life events, the ideals and intentions associated with having a high drive for thinness may help protect against the occurrence of negative life events. However, given that Bodell et al. (2012) found no association between drive for thinness and later negative life events, further research will be needed to clarify these seemingly conflicting results.
The present study had several weaknesses to acknowledge. The data were collected via self-report measures from a non-clinical, fairly homogenous sample. Furthermore, some eating disorder behaviors (e.g. purging, over-exercise, laxative use) were not examined. Because data were collected from a non-clinical sample, base rates of these eating disorder behaviors would have been too low to result in meaningful analyses. The present study also did not examine whether negative life events were independent or dependent (i.e. whether the event was fateful, or occurred because of the behaviors and characteristics of the subjects), which is an important distinction in stress generation research (Hammen, 1991).
Despite these limitations, the current study has several strengths. To our knowledge, this was the first study to examine eating disorder behaviors in relation to burdensomeness and belongingness, two constructs of the IPTS that are key to understanding the association between eating disorders and suicide. Additionally, the present study replicated findings from Bodell et al.'s (2012) study on the relationship between eating disorder symptoms and stress generation, and also extended this line of research by including more measures of eating disorder symptoms than had previously been examined (e.g., the EDEQ-4 eating concern, shape concern, weight concern, and restraint subscales). Furthermore, the present study improved upon the methodology of Bodell et al. (2012) by including a measure of Negative Life Events at both Time 1 and Time 2.
Future studies would benefit from examining these associations in clinical samples with longer duration of follow-up. It would also be important to examine associations among specific types of negative events (i.e., whether or not the event occurred because of the behaviors or characteristics of the individual), which may elucidate the nature of the relationship between restriction (or other eating disorder symptoms) and stress generation. Similarly, examination of specific mediators of the relationship between eating disorder symptoms (i.e., restraint) and negative events may increase understanding of this relationship and potentially highlight targets for treatment. Finally, because this was the first study to examine associations among eating disorder symptoms and burdensomeness and belongingness, replication of these findings is necessary before establishing any strong conclusions.
6. Conclusion
Overall, findings highlight that specific eating disordered behavior (i.e., restraint) may increase stress and problems with interpersonal relationships, which may in turn increase feelings of burdensomeness and low belongingness – two important constructs of the interpersonal theory of suicide. Thus clinicians should target dietary restraint to reduce the frequency of negative events and related increases in burdensomeness and low belongingness. Given the high rates of suicide among individuals with eating disorders (and particularly anorexia nervosa) (Klump et al., 2009), greater understanding of factors that increase risk for death by suicide among individuals who restrict food intake could lead to important improvements in the effectiveness of suicide interventions for this population.
Highlights.
Assessed eating disorder symptoms, stress generation, burdensomeness, belongingness
Dietary restraint predicted negative events (i.e. stress generation) at follow-up
Dietary restraint indirectly increased burdensomeness and low belongingness
Burdensomeness and low belongingness are theorized to contribute to suicide risk
Results help increase understanding of suicide among those with eating disorders
Acknowledgments
Author note: This study was supported, in part, by National Institute of Mental Health grant T32 MH93311. The content of this paper is the sole responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Role of funding: source There were no funding agencies at any level that provided funding for this study.
Footnotes
Contributors: All authors contributed to the design of the study and writing of the manuscript. D. Dodd wrote drafts of the Introduction and Discussion. L. Bodell contributed to the Discussion. A. Smith collected the data and conducted the data analyses. All authors provided substantial feedback and edits on the manuscript.
Conflict of interest: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dorian Dodd, Email: dodddr@miamioh.edu.
April Smith, Email: smith@miamioh.edu.
Lindsay Bodell, Email: bodell@psy.fsu.edu.
References
- American Psychiatric Association. 5th Edition: DSM-5. Arlington, VA: Amer Psychiatric Publising Incorporated; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68(7):724. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56(6):893. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory Manual. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories-IA and-II in psychiatric outpatients. Journal of personality assessment. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: A systematic review of the literature. International Journal of Eating Disorders. 2012;45(3):428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodell LP, Hames JL, Holm-Denoma JM, Smith AR, Gordon KH, Joiner TE. Does the stress generation hypothesis apply to eating disorders?: An examination of stress generation in eating, depressive, and anxiety symptoms. Journal of affective disorders. 2012;142(1):139–142. doi: 10.1016/j.jad.2012.04.016. [DOI] [PubMed] [Google Scholar]
- Bodell LP, Joiner TE, Keel PK. Comorbidity-independent risk for suicidality increases with bulimia nervosa but not with anorexia nervosa. Journal of psychiatric research. 2013;47(5):617–621. doi: 10.1016/j.jpsychires.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodell LP, Smith AR, Holm-Denoma JM, Gordon KH, Joiner TE. The impact of perceived social support and negative life events on bulimic symptoms. Eating behaviors. 2011;12(1):44–48. doi: 10.1016/j.eatbeh.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied Multiple Regression/correlation Analysis for the Behavioral Sciences. L. Erlbaum Associates; 1983. [Google Scholar]
- Cooper Z, Fairburn C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders. 1987;6(1):1–8. [Google Scholar]
- Creamer M, Foran J, Bell R. The Beck Anxiety Inventory in a non-clinical sample. Behaviour Research and Therapy. 1995;33(4):477–485. doi: 10.1016/0005-7967(94)00082-u. [DOI] [PubMed] [Google Scholar]
- Crow S, Peterson C, Swanson S, Raymond N, Specker S, Eckert E, Mitchell J. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166(12):1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Dozois DJ, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory–II. Psychological Assessment. 1998;10(2):83. [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16(4):363–370. [PubMed] [Google Scholar]
- Franko DL, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, Herzog DB. A Longitudinal Investigation of Mortality in Anorexia Nervosa and Bulimia Nervosa. American Journal of Psychiatry. 2013;170(8):917–925. doi: 10.1176/appi.ajp.2013.12070868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2(2):15–34. [Google Scholar]
- Garner DM, Olmsted MP. Manual for eating disorder inventory (EDI) Odessa, FL: Psychological Assessment Resources, Incorporated; 1984. [Google Scholar]
- Grilo CM, Pagano ME, Stout RL, Markowitz JC, Ansell EB, Pinto A, Skodol AE. Stressful life events predict eating disorder relapse following remission: Six-year prospective outcomes. International Journal of Eating Disorders. 2012;45(2):185–192. doi: 10.1002/eat.20909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeffel GJ, Abramson LY, Brazy PC, Shah JY, Teachman BA, Nosek BA. Explicit and implicit cognition: A preliminary test of a dual-process theory of cognitive vulnerability to depression. Behaviour Research and Therapy. 2007;45(6):1155–1167. doi: 10.1016/j.brat.2006.09.003. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100(4):555. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression: Reflections on origins, research, and future directions. Journal of clinical psychology. 2006;62(9):1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp; 2012. Version 21.0. [Google Scholar]
- Joiner TE. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Joiner TE, Wingate LR, Gencoz T, Gencoz F. Stress generation in depression: Three studies on its resilience, possible mechanism, and symptom specificity. Journal of Social and Clinical Psychology. 2005;24(2):236–253. [Google Scholar]
- Klein DA, Walsh BT. Eating disorders. Int Rev Psychiatry. 2003;15(3):205–216. doi: 10.1080/0954026031000136839. [DOI] [PubMed] [Google Scholar]
- Klump KL, Bulik CM, Kaye WH, Treasure J, Tyson E. Academy for eating disorders position paper: eating disorders are serious mental illnesses. International Journal of Eating Disorders. 2009;42(2):97–103. doi: 10.1002/eat.20589. [DOI] [PubMed] [Google Scholar]
- Liu RT, Alloy LB. Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review. 2010;30(5):582–593. doi: 10.1016/j.cpr.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low KG, Charanasomboon S, Brown C, Hiltunen G, Long K, Reinhalter K, Jones H. Internalization of the thin ideal, weight and body image concerns. Social Behavior & Personality: An International Journal. 2003;31(1):81. [Google Scholar]
- Luce KH, Crowther JH. The reliability of the eating disorder examination— Self-report questionnaire version (EDE-Q) International Journal of Eating Disorders. 1999;25(3):349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Current Directions in Psychological Science. 2009;18(1):16–20. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods. 2007;39(3):384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond JM, Hay P, Rodgers B, Owen C, Beumont P. Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy. 2004;42(5):551–567. doi: 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C. Comparing the health burden of eating-disordered behavior and overweight in women. Journal of Women's Health. 2009;18(7):1081–1089. doi: 10.1089/jwh.2008.1174. [DOI] [PubMed] [Google Scholar]
- Needles DJ, Abramson LY. Positive life events, attributional style, and hopefulness: Testing a model of recovery from depression. Journal of Abnormal Psychology. 1990;99(2):156. doi: 10.1037//0021-843x.99.2.156. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preti A, Rocchi M, Sisti D, Camboni M, Miotto P. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatrica Scandinavica. 2011;124(1):6–17. doi: 10.1111/j.1600-0447.2010.01641.x. [DOI] [PubMed] [Google Scholar]
- Schmidt U, Treasure J. Anorexia nervosa: Valued and visible. A cognitive-interpersonal maintenance model and its implications for research and practice. British Journal of Clinical Psychology. 2006;45(3):343–366. doi: 10.1348/014466505x53902. [DOI] [PubMed] [Google Scholar]
- Selby EA, Smith AR, Bulik CM, Olmsted MP, Thornton L, McFarlane TL, Fichter MM. Habitual starvation and provocative behaviors: two potential routes to extreme suicidal behavior in anorexia nervosa. Behaviour Research and Therapy. 2010;48(7):634–645. doi: 10.1016/j.brat.2010.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological methods. 2002;7(4):422. [PubMed] [Google Scholar]
- Sim LA, Homme JH, Lteif AN, Vande Voort JL, Schak KM, Ellingson J. Family functioning and maternal distress in adolescent girls with anorexia nervosa. International Journal of Eating Disorders. 2009;42(6):531–539. doi: 10.1002/eat.20654. [DOI] [PubMed] [Google Scholar]
- Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Current psychiatry reports. 2012;14(4):406–414. doi: 10.1007/s11920-012-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AR, Fink EL, Anestis MD, Ribeiro JD, Gordon KH, Davis H, Klein MH. Exercise caution: Over-exercise is associated with suicidality among individuals with disordered eating. Psychiatry research. 2013;206(2):246–255. doi: 10.1016/j.psychres.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE., Jr Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychological Assessment. 2012;24(1):197. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]


