Abstract
Objectives
Comparison groups are essential for accurate testing and interpretation of yoga intervention trials. However, selecting proper comparison groups is difficult because yoga comprises a very heterogeneous set of practices and its mechanisms of effect have not been conclusively established.
Methods
We conducted a systematic review of the control and comparison groups used in published randomized controlled trials (RCTs) of yoga.
Results
We located 128 RCTs that met our inclusion criteria; of these, 65 included only a passive control and 63 included at least one active comparison group. Primary comparison groups were physical exercise (43%), relaxation/meditation (20%), and education (16%). Studies rarely provided a strong rationale for choice of comparison. Considering year of publication, the use of active controls in yoga research appears to be slowly increasing over time.
Conclusions
Given that yoga has been established as a potentially powerful intervention, future research should use active control groups. Further, care is needed to select comparison conditions that help to isolate the specific mechanisms of yoga’s effects.
Keywords: Yoga, Randomized Controlled Trials, Systematic Review, Control Group, Comparison Group
Research on yoga interventions is rapidly proliferating; 1 researchers are studying the effects of yoga on a wide range of mental and physical health conditions. Researchers have demonstrated preliminary efficacy for many conditions, including arthritis2 stress3 metabolic syndrome4 asthma5, pain6 and depression.7 However, the literature is replete with many contradictory findings and generally characterized as inconclusive due to the weak design of many studies.4,5
A common methodological limitation of many yoga intervention studies is the lack of an adequate control condition. Although trials of the effects of yoga have often been conducted without a control condition, using pre-post designs, more recent research typically employs a control condition as well as randomization and other elements of experimentation.1 Selection of an appropriate control group is very important in intervention studies because comparison of the intervention and control groups allows researchers to isolate and test the purported active ingredient of the intervention and hold all other factors constant.8
Unlike in studies of drug effects, where a placebo is relatively straightforward, selection of a control condition is much more complex for behavioral interventions. 8 Yet because of its centrality to the interpretation of the study results, the comparison group is essential and must be selected with care and deliberation. The appropriateness of a comparison group depends on the specific research question being asked, so that researchers can be confident that differences found between groups is due to the hypothesized active ingredient of the yoga intervention.9,10 Thus, the theoretical mechanism through which the yoga is presumed to operate and the comparison condition would ideally include all of the elements of the yoga condition minus that active ingredient. Of course, in behavioral interventions, the “active ingredient” is complex and difficult to identify. Still, when interpreting the results of a study, it is critically important to have an adequate condition to which to compare the yoga intervention group so that the effective ingredient(s) of the yoga can be isolated and tested. Yet, perhaps because of the heterogeneous nature of yoga,11,12 the rationale for selecting the comparison is rarely explicated in published reports.10
One common solution is a passive control, such as a wait-list or usual treatment.9 Wait-list typically means that participants in the comparison group get usual care for the intervention period but then are able to receive the intervention after the study ends, while participants in a usual care condition simply receive no additional treatment. Participants in wait-list or usual care groups are sometimes asked to avoid changing their usual treatment unless medically necessary. While inclusion of these groups in the research design controls for the passage of time and natural course of a given problem or condition, they are limited as controls in mind-body interventions such as yoga, given the many nonspecific factors that may confound results or even constitute important elements of the intervention.10 However, passive control groups are reasonable in early stages of research, given the practical demands of active comparison groups, whose inclusion require investigators to recruit many more participants and to deliver the comparison condition.
However, as research advances, the need for more active comparisons becomes obvious. Yoga involves ongoing interaction with an instructor, which can have substantial effects on some outcomes. In addition, a passive control does not account for other potential nonspecific factors, including expectancy effects, attention and time spent in the intervention.11,10 Further, passive control conditions do not typically entail the same amount of participant burden or investment. In addition, some researchers have argued that using a waitlist control may spuriously amplify the difference in treatment effect between the intervention and the control because people assigned to the waitlist may expect to not get better without active treatment.8,13
Study designs that include information-only or self-study control groups in which participants are given informational materials to read on their own are somewhat closer to designs that include an active comparison. Although a few especially motivated participants may read everything they are given and take action that will change their health, these control groups are usually expected to have minimal effects across the whole group of participants randomized to that condition.14 However, this option may have some appeal to potential participants during recruitment and alleviate the potential disappointment some participants experience when getting randomized to the “usual care” condition.10
Investigators may also employ active control conditions such as relaxation or exercise in their studies.10 These control conditions may constitute a stronger comparison group for discerning the effects of yoga, but because few authors reporting on yoga interventions explicitly state the mechanism through which they believe the yoga will affect the outcome, the rationale for the choice of control is often not provided. Active control conditions may or may not control for multiple aspects of the intervention (time, attention from a provider, group setting). Active control groups provide an important practical advantage in research as well, making participation in studies more appealing and improving retention rates.8
To better understand the current state of yoga intervention research, we undertook a systematic review of the control groups employed by investigators in randomized controlled trials (RCTs) of yoga, which are more methodologically rigorous and may be more heavily weighted in determining evidence regarding yoga’s effects. For those studies in which an active control was included, we attempted to examine the rationales provided for that choice. With this information, we endeavor to provide some direction for future studies of yoga interventions.
Method
The results of this paper focus on a subset of data produced for a review of all intervention trials of yoga conducted by the authors. The larger project followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for conducting and reporting items for systematic reviews.8 Two authors searched four electronic databases (PsycInfo, OVID, AgeLine, Pub Med) using the text term “yoga”, from the inception of the database until the end review date of April 27, 2012. In addition, we hand-searched the electronic table of contents of five key journals, selected because of their prominence in our electronic database search (Arch Intern Med, BMC Complement Altern Med, Evid Based Complement Alternat Med, Int J Yoga and J Altern Complement Med). Studies were selected for review if they met the following four criteria: 1) the study consisted of a yoga intervention, defined as providing at least one yoga session to a cohort of people and measuring any outcomes with at least a pre- and post-test; 2) participants in the intervention were at least 18 years of age; 3) the published paper was written in English, and 4) the full text of the article was available for review. If an article was not available in electronic format, we purchased it through one of two university library centers. If a university library was unable to obtain the article, one of the authors wrote to the first author requesting a reprint of the article. The complete search strategy, including our PRISMA Flowchart, is detailed in Elwy et al. 15
This review of all yoga interventions identified 3,062 articles reporting on yoga interventions, with 465 studies meeting the above inclusion criteria. For this paper, we focused on the subset of these, 154 studies, coded as RCTs, meaning that, at minimum, participants were randomly assigned to a group that received yoga or to a comparison group. Of these, authors of 13 articles were reporting additional results beyond those initially reported for that study, 2 were studies in which only two yoga conditions were compared (e.g., yoga versus yoga plus Tui Na16), 4 were reports of combination treatments where yoga was only a small part of the intervention (e.g., 17) and 7 were reports of single sessions that were designed to examine very specific effects of yoga (e.g., optical illusions18). These 26 studies were removed from the present review, which was designed to examine the control conditions used in studies of yoga as an intervention to meaningfully improve health or well-being. Thus, 128 randomized controlled studies were included.
Results
The 128 RCTs of yoga, representing 28% of the studies eligible for inclusion in the larger review, were nearly evenly split between those in which researchers included only a waitlist or no treatment control and those in which at least one active control was included (see Figure 1). Of the 80 studies in which investigators employed an inactive control condition, 33 included a waitlist control, 32 included usual care, two included patients who were asked avoid usual care, and 13 included a no treatment condition; this latter condition was often the case for non-patient population interventions such as stress management for employees or caregivers (see Table 1).
Figure 1.
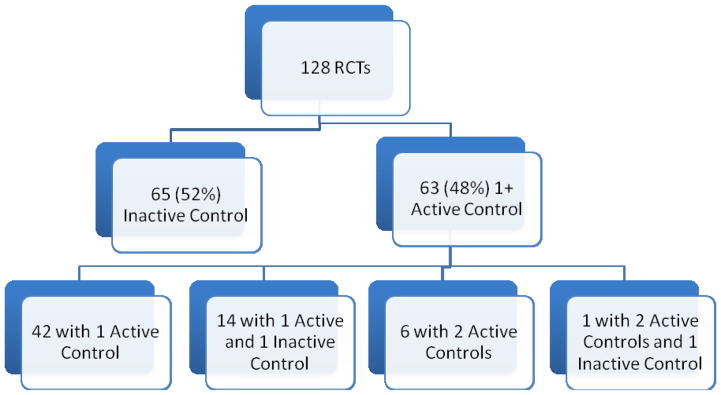
Number of yoga intervention studies using passive and active comparison conditions
Table 1.
Passive control conditions in yoga intervention studies that used at least one passive control condition
| Condition | N | Studies |
|---|---|---|
| Wait list control | 33 | 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 26, 51, 52, 53, 54, 32, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 20 |
| Usual care | 32 | 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96 |
| No treatment/Less than usual care | 2 | 97, 98 |
| No intervention | 13 | 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110 111 |
Among studies that included at least one active comparison group, physical exercise interventions were the most common comparison condition (see Table 2). Most of these conditions comprised group exercise sessions that consisted of aerobics and calisthenics. In four studies, investigators used a stretching group (sometimes referred to as sham yoga), as the comparison, in four, investigators used a walking group as the comparison, and in one study each, investigators used bicycling and sports climbing as the comparison. In these studies, investigators tended to control for amount of time and teacher attention as well as other nonspecific effects such as expectancies and experience within the group.
Table 2.
Active control conditions in yoga intervention studies that used at least one active control condition
| Number | Reasonable Effort to Control for Nonspecific Effects | Studies | |
|---|---|---|---|
| Physical Exercise | 30 (43%) | ||
| Physical Exercise Program/Physical Therapy | 20 | Yes | 2, 3, 14, 38, 47, 52, 56, 57, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, |
| Sham yoga/stretching | 4 | Yes | 19, 35, 105, 124 |
| Walking | 4 | Mixed | 31, 46, 87, 108 |
| Bicycling | 1 | Yes | 125 |
| Sports Climbing | 1 | Yes | 126 |
| Relaxation and Meditation | 14 (20%) | ||
| Relaxation | 6 | Yes | 7, 45, 53, 32, 127, 128 |
| Meditation/Breath Awareness | 4 | Yes | 21, 28, 129, 130 |
| Progressive Muscle Relaxation | 3 | Yes | 131, 132, 133 |
| Brain Wave Vibration | 1 | Yes | 129 |
| Education | 11 (16%) | ||
| Education Materials | 3 | No | 14, 123, 134 |
| Education Group/Lecture | 3 | Mixed | 135, 136, 137 |
| Nutritional Counseling | 2 | Mixed | 65, 138 |
| Film Discussion | 2 | Yes | 22, 49 |
| Workshop Luncheons | 1 | No | 139 |
| Psychotherapy/Counseling | 8 (11%) | ||
| Psychotherapy Group (e.g., ACT, CBT) | 5 | Yes | 23, 24, 76, 136, 140 |
| Supportive Counseling | 3 | Mixed | 25, 37, 141 |
| Medical Intervention | 7 (10%) | ||
| Ayurveda | 2 | No | 26, 54 |
| Additional medical treatment (e.g., medication) | 3 | No | 27 (ECT), 27 (imipramine), 142 |
| Dietary change (salt reduction) | 2 | No | 87, 143 |
The two other large groups of comparison conditions were relaxation/meditation and psychotherapy/counseling. These conditions were primarily administered in group format and usually attempted to control for nonspecific effects. Within each category, there was a great deal of variation. For example, meditation comparisons included techniques focusing on mindfulness20 and breathing.21 Similarly, studies in which investigators used comparison groups comprised of psychotherapy/counseling included cognitive behavioral therapy,21 Acceptance and Commitment Therapy,23 dynamic psychotherapy24 and supportive counseling.25 Most of the relaxation/meditation and psychotherapy/counseling comparisons controlled reasonably well for the nonspecific intervention elements such as time and attention.
Some of the education comparisons were well-designed and attempted to control for nonspecific effects. Exemplary in this regard is the comparison intervention designed by Innes and her colleagues that involves watching a series of health films and having group discussions. This condition carefully matched staff attention, class time and setting, and social interaction.4 Most education comparison conditions, however, did not attempt to control for nonspecific effects (e.g., giving participants booklets related to back pain1). Some studies included a comparison group whose participants received a medical approach, either a holistic treatment through Ayurveda (e.g.,26) or a specific treatment such as medication or electroconvulsive therapy for depression (e.g., 27).
To examine trends in the use of active control conditions in yoga intervention research over time, we examined the absolute and relative number of yoga trials with and without an active condition over time (see Figure 2). Results indicate that while yoga intervention research has become increasingly popular over the past decade, a substantial amount of this research has continued to include only a passive control group.
Figure 2.
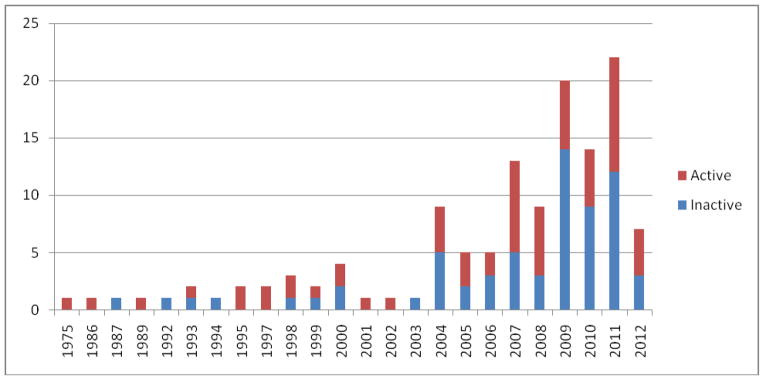
Number of Studies with Passive Only Control Conditions versus Studies with Active Comparison Conditions by Year (ending mid-2012)
Discussion
Although researchers have been studying yoga for many years and the pace of yoga research has accelerated considerably in recent years, the number of RCTs remains small. Only 28% of the published studies examining yoga on health or well-being outcomes were RCTs. Of that 28%, about half included only inactive wait-list or usual care control groups, while in the other half, participants were randomized to a more active treatment condition with elements that comprised attempts to control for a variety of specific or nonspecific effects. Only one study design involved more than one experimental condition, allowing those researchers to compare a yoga intervention to both an inactive group and another active control condition.28
The 63 studies in which researchers included an active comparison condition provide important insights into the theories driving these studies and the mechanisms of effect that the researchers are testing. Among these mechanisms are physiological (e.g., immunological, cardiovascular, musculoskeletal) and psychological (e.g., affect, stress)3, 7. It should be noted that few authors explicitly laid out their hypotheses regarding the purported mechanism of effect or tied it explicitly to their selection of a control condition. However, it may be that although these investigators had a sound rationale for their choice of control group, its omission in the published manuscript was due to journal space constraints.
The most commonly-used active control condition employed by researchers was exercise. Studies in which yoga is compared to an exercise condition can help investigators to determine whether yoga’s effects are “merely” exercise or whether yoga provides something above and beyond physical activity. For example, in a recent study of chronic low back pain, researchers compared yoga to stretching exercises in a condition matched for time, attention, and expectations for improvement, finding that participants in both conditions improved to a similar degree relative to those who received only an educational booklet.14 These results suggest that the effects of yoga on lower back pain may be due to stretching that occurs during asana, although both stretching and yoga may exert unique salutary effects as well.29
Importantly, exercise also produces documented psychological effects as well as physical effects; these psychological effects may also be a pathway through which yoga influences well-being.30 Thus yoga may provide the same psychological and physical benefits that other types of exercise do, as well as providing additional benefits, such as relaxation.29 For example, a study of yoga in healthy participants in which investigators compared yoga to walking found that those in the yoga condition showed greater increases in positive mood and reductions in anxiety.31 Investigators designed this study to test whether yoga adds to the known effects of physical exercise in improving mood and reducing anxiety, and carefully controlled for staff attention and interaction as well as energy expenditure. Based on their findings, the authors speculated that the effect of the yoga intervention (reduction in GABA levels) may be due to the ability of yoga practices to increase parasympathetic nervous system activity.
The second-largest group of comparison conditions was relaxation and meditation. Researchers do not typically provide their rationale for examining yoga vis-à-vis meditation or relaxation in published articles, but some have described the effort to control for relaxation to see whether yoga contributes above and beyond nonspecific effects. For example, Manocha and colleagues32 employed a meditation/relaxation condition “ to control for nonspecific effects associated with reduction in physiological arousal (i.e., “rest”) as well as other nonspecific factors such as therapeutic contact, credibility, and expectancy associated with any behavioral intervention” (p. 3).
The other large group of comparison conditions involved psychotherapy or counseling. Few of the articles reporting on these studies provided a rationale for selecting psychotherapy or counseling as a comparison. Granath and colleagues33 used a cognitive-behavioral therapy (CBT) comparison group, hypothesizing that yoga and CBT may both improve stress levels but have somewhat different impacts on specific outcomes (but did not make more specific hypotheses). Rao and colleagues25 used a supportive counseling intervention to control for nonspecific effects of the intervention, hypothesizing that the yoga intervention would have additional effects on anxiety (which supportive counseling was apparently presumed not to have).
Factors that affect the choice of a control group for behavioral researchers include the level of existing evidence for intervention efficacy, availability of funding for more rigorous studies, the nature of usual care, the complexity of the intervention being studied and the availability and effectiveness of alternative treatments for the targeted disease or condition. Without inclusion of an active control, conclusions regarding the extent to which yoga had effects above and beyond non-specific effects are limited. Comparing yoga (or essentially any psychosocial intervention) to nothing or to usual care is well-established to demonstrate superior effects for the (yoga) intervention group.9,34
Yet studies that used only a wait-list or usual care control have been important in paving the way towards more sophisticated research by demonstrating acceptability and preliminary efficacy. Thus, if yoga has never been used to treat a certain disease or health issue, we may expect to see pilot or proof-of-concept studies without control groups followed by some RCTs with wait-list or usual care groups. We note that the issue of usual care is more complex than it may seem, as some conditions have fairly well-established treatment, yet also some latitude in the care provided. For example, investigators in one study compared three treatments for depressed patients: yoga, electroconvulsive therapy, and antidepressant medication.27 When compared with usual care alone, a wait-list condition has the advantage of limiting the amount of disappointment that may be felt by the group that does not receive the yoga intervention.
However, considerable evidence has already been presented for the efficacy of yoga for treating many diseases, including arthritis,2 stress,3 metabolic syndrome,4 asthma,5 chronic pain6 and depression.7 Thus, investigators for many health conditions should will best advance science by employing more active comparison groups in order to control for nonspecific effects of group participation, attention, and activity. Inclusion of these active controls will enable the isolation and elucidation of the important elements of yoga that impact various health conditions. Such studies are essential for identifying the mechanisms of effect through which yoga affects health outcomes; these mechanisms may vary by outcome, and only through careful selection of comparison groups can this line of research progress.
Investigators’ use of active comparison groups will almost certainly become the standard in yoga research as this area of science matures. Funding for yoga interventions is increasingly available, removing an important barrier to more sophisticated research. For illnesses and other conditions for which other types of interventions have established a level of efficacy, a comparative effectiveness trial may be the next step. Comparative effectiveness designs, implementation considerations and cost-effectiveness analyses are important next steps for expanding the impact of yoga on health.
Highlights.
Our systematic review of control and comparison groups of yoga yielded 128 RCTs.
65 included only a passive control and 63 included an active comparison group.
Physical exercise, relaxation, and education were the most common active groups.
Use of active controls in yoga research appears to be slowly increasing over time.
Future yoga research should carefully consider appropriate control conditions.
Acknowledgments
This work was supported by grant 1R01AT006466-01 from the National Center for Complementary and Alternative Medicine/National Institutes of Health, Principal Investigator Crystal L. Park, Ph.D.
Footnotes
Conflict of Interest Statement: None declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sherman KJ. Guidelines for developing yoga interventions for randomized trials. Evid Based Comp Alt Med. 2012:1–15. doi: 10.1155/2012/143271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haaz S, Bartlet SJ. Yoga for arthritis: A scoping review. Rheumatic Dis Clinics of North America. 2011;37:33–46. doi: 10.1016/j.rdc.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chong CS, Tsunaka M, Tsang H, Chan EP, Cheung WM. Effects of yoga on stress management in healthy adults: A systematic review. Alt Ther in Health and Med. 2011;17:32–38. [PubMed] [Google Scholar]
- 4.Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with Type 2 diabetes mellitus: A systematic review. Evid-Based Complem and Altern Med. 2007;4:469–486. doi: 10.1093/ecam/nel103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Posadzki P, Ernst E. Yoga for asthma? A systematic review of randomized clinical trials. J of Asthma. 2011b;48:632–639. doi: 10.3109/02770903.2011.584358. [DOI] [PubMed] [Google Scholar]
- 6.Posadzki P, Ernst E, Terry R, Lee MS. Is yoga effective for pain? A systematic review of randomized clinical trials. Complem Ther in Med. 2011;19:281–287. doi: 10.1016/j.ctim.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW. Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. J Psychiatric Pract. 2010;16:22–33. doi: 10.1097/01.pra.0000367775.88388.96. [DOI] [PubMed] [Google Scholar]
- 8.Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, Kaplan R. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosoms. 2009;78:275–284. doi: 10.1159/000228248. [DOI] [PubMed] [Google Scholar]
- 9.Kinser PA, Robins JL. Control Group Design: Enhancing rigor in research of mind-body. Therapies for Depression. Evid-Based Complem and Altern Med. 2013 doi: 10.1155/2013/140467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stoney CM, Wallerstedt D, Stagl JM, Mansky P. The use of complementary and alternative medicine for pain. In: Moore RJ, editor. Biobehavioral Approaches to Pain. New York: 2009. pp. 381–408. [Google Scholar]
- 11.Khanna S, Greeson JM. A narrative review of yoga and mindfulness as complementary therapies for addiction. Complement Ther Med. 2013;21:244–252. doi: 10.1016/j.ctim.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park CL. Mind-body CAM interventions: Current status and considerations for integration into behavioral medicine. J Clin Psych. 2013;69:45–63. doi: 10.1002/jclp.21910. [DOI] [PubMed] [Google Scholar]
- 13.Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, Klassen TP. Meditation practices for health: State of the research. Evid Reports/Technology Asses. 2007;155:19–24. [PMC free article] [PubMed] [Google Scholar]
- 14.Sherman KJ, Cherkin DC, Wellman RD, Cook AJ, Hawkes RJ, Delaney K, Deyo RA. A Randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch Intern Med. 2011;171:2019–2026. doi: 10.1001/archinternmed.2011.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elwy AR, Groessl EJ, Eisen SV, Riley KE, Maiya M, Lee JP, Sarkin A, Park CL. A Systematic Scoping Literature Review of Yoga Intervention Components and Intervention Quality. Unpublished manuscript. 2013 doi: 10.1016/j.amepre.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Da Silva GD, Lorenzi-Filho G, Lage LV. Effects of yoga and the addition of Tui Na in patients with fibromyalgia. The Journal of Altern and Complem Med. 2007;13:1107–1114. doi: 10.1089/acm.2007.0615. [DOI] [PubMed] [Google Scholar]
- 17.Strijk JE, Proper KI, van der Beek AJ, van Mechelen WA. Process evaluation of a worksite vitality intervention among ageing hospital workers. Int J Behav Nutr Phys Act. 2011;8:58. doi: 10.1186/1479-5868-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Telles S, Maharana K, Balrana B, Balkrishna A. Effects of high-frequency yoga breathing called kapalabhati compared with breath awareness of the degree of optical illusion perceived. Percep Motor Skills. 2011;112:981–990. doi: 10.2466/02.20.22.PMS.112.3.981-990. [DOI] [PubMed] [Google Scholar]
- 19.Sabina A. Yoga intervention for adults with mild-to moderate asthma: A pilot study. Ann Allergy Asthma Immunol. 2005;94:543–8. doi: 10.1016/s1081-1206(10)61131-3. [DOI] [PubMed] [Google Scholar]
- 20.Woolery A. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60–3. [PubMed] [Google Scholar]
- 21.Saxena T, Saxena M. The effect of various breathing exercises (pranayama) in patients with bronchial asthma of mild to moderate severity. Int J Yoga. 2009;2:22–25. doi: 10.4103/0973-6131.53838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bock BC, Morrow KM, Becker BM, Williams DM, Tremont G, Gaskins RB, Marcus BH. Yoga as a complementary treatment for smoking cessation: rationale, study design and participant characteristics of the Quitting-in-Balance study. BMC Complem and Altern Med. 2010;10:14. doi: 10.1186/1472-6882-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lundgren T, Dahl J, Yardi N, Melin L. Acceptance and Commitment Therapy and yoga for drug-refractory epilepsy: randomized controlled trial. Epilepsy Behav. 2008;13:102–108. doi: 10.1016/j.yebeh.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Shaffer HJ, LaSalvia TA, Stein JP. Comparing Hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: a randomized clinical trial. Altern Ther Health Med. 1997;3:57–66. [PubMed] [Google Scholar]
- 25.Rao RM, Nagendra HR, Raghuram N, Vinay C, Chandrashekara S, Gopinath KS, Srinath BS. Influence of yoga on mood states, distress, quality of life and immune outcomes in early stage breast cancer patients undergoing surgery. Int J Yoga. 2008;1:11–20. doi: 10.4103/0973-6131.36789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishnamurthy MN, Telles S. Assessing depression following two ancient Indian interventions: effects of yoga and Ayurveda on older adults in a residential home. J Gerontol Nurs. 2007;33:17–23. doi: 10.3928/00989134-20070201-05. [DOI] [PubMed] [Google Scholar]
- 27.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 28.Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA, Baime M. Effective and viable mind-body stress reduction in the workplace: A randomized controlled trial. J Occupat Health Psych. 2012;17:246–258. doi: 10.1037/a0027278. [DOI] [PubMed] [Google Scholar]
- 29.Sherman KJ, Wellman RD, Cook AJ, Cherkin DC, Ceballos RM. Mediators of Yoga and Stretching for Chronic Low Back Pain. Evid-Based Comp Alt Med. 2013:Article 130818. doi: 10.1155/2013/130818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ross A, Thomas S. The health benefits of yoga and exercise: A review of comparison studies. J Alt Comp Med. 2010;16:3–12. doi: 10.1089/acm.2009.0044. [DOI] [PubMed] [Google Scholar]
- 31.Streeter CC, Whitfield TH, Owen L, Rein T, Karri SK, Yakhkind A, Perlmutter R, Prescot A, Renshaw PF, Ciraulo DA, Jensen JE. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: A randomized controlled MRS study. J Altern Complement Med. 2010;16:1145–52. doi: 10.1089/acm.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manocha R, Black D, Sarris J, Stough CA. randomized, controlled trial of meditation for work stress, anxiety and depressed mood in full-time workers. Evid-Based Comp Altern Med. 2011 doi: 10.1155/2011/960583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Granath J, Ingvarsson S, von Thiele U, Lundberg U. Stress management: A randomized study of cognitive behavioural therapy and yoga. Cogn Behav Ther. 2006;35:3–10. doi: 10.1080/16506070500401292. [DOI] [PubMed] [Google Scholar]
- 34.Goldberg RJ, McManus DD, Allison J. Greater knowledge and appreciation of commonly-used research study designs. The Amer J of Med. 2013;126:169–e1. doi: 10.1016/j.amjmed.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Afonso RF, Hachul H, Kozasa EH, de Souza Oliveira D, Goto V, Rodrigues D, Tufik S, Leite JR. Yoga decreases insomnia in postmenopausal women: A randomized clinical trial. Menopause. 2011:19. doi: 10.1097/gme.0b013e318228225f. [DOI] [PubMed] [Google Scholar]
- 36.Banasik J. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J the American Acad of Nurse Pract. 2010;23:135–142. doi: 10.1111/j.1745-7599.2010.00573.x. [DOI] [PubMed] [Google Scholar]
- 37.Banerjee B. Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integr Cancer Ther. 2007;6:242–50. doi: 10.1177/1534735407306214. [DOI] [PubMed] [Google Scholar]
- 38.Behere RV, Arasappa R, Jagannathan A, Varambally S, Venkatasubramanian G, Thirthalli J, Subbakrishna DK, Nagendra HR, Gangadhar BN. Effect of yoga therapy on facial emotion recognition deficits, symptoms and functioning in patients with schizophrenia. Acta Psychiatr Scand. 2011;123:147–153. doi: 10.1111/j.1600-0447.2010.01605.x. [DOI] [PubMed] [Google Scholar]
- 39.Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010;151:530–539. doi: 10.1016/j.pain.2010.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carson JW, Carson KM, Porter LS, Keefe FJ, Seewaldt VL. Yoga of Awareness program for menopausal symptoms in breast cancer survivors: results from a randomized trial. Support Care Cancer. 2009;17:1301–1309. doi: 10.1007/s00520-009-0587-5. [DOI] [PubMed] [Google Scholar]
- 41.Chandwani KD, Thornton B, Perkins GH, Arun B, Raghuram NV, Nagendra HR, Wei Q, Cohen L. Yoga improves quality of life and benefit finding in women undergoing radiotherapy for breast cancer. J Soc Integr Oncol. 2010;8:43–55. [PubMed] [Google Scholar]
- 42.Cohen BE, Chang AA, Grady D, Kanaya AM. Restorative yoga in adults with metabolic syndrome: A randomized, controlled pilot trial. Metabolic syndrome and related disorders. 2008;6:223–229. doi: 10.1089/met.2008.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Culos-Reed SN, Carlson LE, Daroux LM, Hately-Aldous S. A pilot study of yoga for breast cancer survivors: Physical and psychological benefits. Psychooncology. 2006;15:891–897. doi: 10.1002/pon.1021. [DOI] [PubMed] [Google Scholar]
- 44.Danhauer SC, Mihalko SL, Russell GB, Campbell CR, Felder L, Daley K, Levine EA. Restorative yoga for women with breast cancer: Findings from a randomized pilot study. Psychooncology. 2009;18:360–368. doi: 10.1002/pon.1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Deuskar M, Poonawala N, Bhatewara SA. Effect of yoga nidra and applied relaxation technique on steadiness and performance of archers. Psych Studies. 2006;51:64–68. [Google Scholar]
- 46.Elavsky S, McAuley E. Exercise and self-esteem in menopausal women: a randomized controlled trial involving walking and yoga. Amer J of Health Prom. 2007;22:83–92. doi: 10.4278/0890-1171-22.2.83. [DOI] [PubMed] [Google Scholar]
- 47.Flegal KE, Kishiyama S, Zajdel D, Haas M, Oken BS. Adherence to yoga and exercise interventions in a 6-month clinical trial. BMC Complement Altern Med. 2007;7:37. doi: 10.1186/1472-6882-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garfinkel MS, Schumacher HR, Jr, Husain A, Levy M, Reshetar RA. Evaluation of a yoga based regimen for treatment of osteoarthritis of the hands. J Rheumatol. 1994;21:2341–2343. [PubMed] [Google Scholar]
- 49.Hartfield N, Havenhand J, Khalsa SB, Clarke G, Krayer A. The effectiveness of yoga for the improvement of well-being and resilience to stress in the workplace. Scand J Work Environ Health. 2011;37:70–76. doi: 10.5271/sjweh.2916. [DOI] [PubMed] [Google Scholar]
- 50.Javnbakht M, Hejazi Kenari R, Ghasemi M. Effects of yoga on depression and anxiety of women. Complement Ther Clin Pract. 2009;15:102–104. doi: 10.1016/j.ctcp.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 51.Littman AJ, Bertram LC, Ceballos R, Ulrich CM, Ramaprasad J, McGregor B, McTiernan A. Randomized controlled pilot trial of yoga in overweight and obese breast cancer survivors: Effects on quality of life and anthropometric measures. Supp Care in Can. 2012;20:267–277. doi: 10.1007/s00520-010-1066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Madden D. Improving Aerobic Capacity in Healthy Older Adults Does Not Necessarily Lead to Improved Cognitive Performance. Psychol Aging. 1989;4:307–320. doi: 10.1037//0882-7974.4.3.307. [DOI] [PubMed] [Google Scholar]
- 53.Malathi A, Damodaran A, Shah N, Krishnamurthy G, Namjoshi P, Ghodke S. Psychophysiological changes at the time of examination in medical students before and after the practice of yoga and relaxation. Indian J Psychiatry. 1998;40:35–40. [PMC free article] [PubMed] [Google Scholar]
- 54.Manjunath NK, Telles S. Influence of Yoga and Ayurveda on self-rated sleep in a geriatric population. Indian J Med Res. 2005;121:683–690. [PubMed] [Google Scholar]
- 55.McIver S, O’Halloran P, McGartland M. Yoga as a treatment for binge eating disorder: A preliminary study. Complement Ther in Med. 2009;17:196–202. doi: 10.1016/j.ctim.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 56.Oken BS, Kishiyama S, Zajdel D, Bourdette D, Carlsen J, Haas M, Hugos C, Kraemer DF, Lawrence J, Mass M. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62:2058–2064. doi: 10.1212/01.wnl.0000129534.88602.5c. [DOI] [PubMed] [Google Scholar]
- 57.Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, Haas M, Kraemer DF, Lawrence J, Leyva J. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med. 2006;12:40–47. [PMC free article] [PubMed] [Google Scholar]
- 58.Shelov D, Suchday S, Friedberg JP. A pilot study measuring the impact of yoga on the trait of mindfulness. Behav Cogn Psychother. 2009;37:595–598. doi: 10.1017/S1352465809990361. [DOI] [PubMed] [Google Scholar]
- 59.Skoro-Kondza L, Tai SS, Gadelrab R, Drincevic D, Greenhalgh T. Community based yoga classes for Type 2 diabetes: An exploratory randomised controlled trial. BMC Health Serv Res. 2009;9:33. doi: 10.1186/1472-6963-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Telles S. Post-traumatic stress symptoms and heart rate variability in Bihar flood survivors following yoga: A randomized controlled study. BMC Psychiatry. 2010;2:10–18. doi: 10.1186/1471-244X-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Telles S. Effect of yoga on musculoskeletal discomfort and motor functions in professional computer users. Work. 2009;33(3):297–306. doi: 10.3233/WOR-2009-0877. [DOI] [PubMed] [Google Scholar]
- 62.Telles S. Effect of yoga on self-rated visual discomfort in computer users. Head Face Med. 2006;3:2–46. doi: 10.1186/1746-160X-2-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vempati R, Bijlani RL, Deepak KK. The efficacy of a comprehensive lifestyle modification programme based on yoga in the management of bronchial asthma: A randomized controlled trial. BMC Pulm Med. 2009;9:37. doi: 10.1186/1471-2466-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: A randomized, controlled pilot study. J Altern Complement Med. 2011;17:601–607. doi: 10.1089/acm.2010.0075. [DOI] [PubMed] [Google Scholar]
- 65.Cade WT, Reeds DN, Mondy KE, Overton ET, Grassino J, Tucker S, Bopp C, Laciny E, Hubert S, Lassa-Claxton S, Yarasheski KE. Yoga lifestyle intervention reduces blood pressure in HIV-infected adults with cardiovascular disease risk factors. HIV Med. 2010;11:379–388. doi: 10.1111/j.1468-1293.2009.00801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chuang LH, Soares MO, Tilbrook H, Cox H, Hewitt CE, Aplin J, Semlyen A, Trewhela A, Watt I, Torgerson DJ. A pragmatic multi-centered randomised controlled trial of yoga for chronic low back pain: Economic evaluation. Spine. 2012;37:1593–1601. doi: 10.1097/BRS.0b013e3182545937. [DOI] [PubMed] [Google Scholar]
- 67.Chuntharapat S, Petpichetchian W, Hatthakit U. Yoga during pregnancy: Effects on maternal comfort, labor pain and birth outcomes. Complement Ther Clin Pract. 2008;14:105–115. doi: 10.1016/j.ctcp.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 68.Cohen L, Warneke C, Fouladi RT, Rodriguez MA, Chaoul-Reich A. Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100:2253–2260. doi: 10.1002/cncr.20236. [DOI] [PubMed] [Google Scholar]
- 69.Cox H, Tilbrook H, Aplin J, Semlyen A, Torgerson D, Trewhela A, Watt I. A randomised controlled trial of yoga for the treatment of chronic low back pain: Results of a pilot study. Complement Ther Clin Pract. 2010;16:187–193. doi: 10.1016/j.ctcp.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 70.Donesky-Cuenco D, Nguyen HQ, Paul S, Carrieri-Kohlman V. Yoga therapy decreases dyspnea-related distress and improves functional performance in people with chronic obstructive pulmonary disease: A pilot study. J Altern Complement Med. 2009;15:225–234. doi: 10.1089/acm.2008.0389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Galantino ML, Bzdewka TM, Eissler-Russo JL, Holbrook ML, Mogck EP, Geigle P, Farrar JT. The impact of modified Hatha yoga on chronic low back pain: A pilot study. Altern Ther Health Med. 2004;10:56–59. [PubMed] [Google Scholar]
- 72.Jatuporn S, Sangwatanaroj S, Saengsiri AO, Rattanapruks S, Srimahachota S, Uthayachalerm W, Kuanoon W, Panpakdee O, Tangkijvanich P, Tosukhowong P. Short-term effects of an intensive lifestyle modification program on lipid peroxidation and antioxidant systems in patients with coronary artery disease. Clin Hemorheol Microcirc. 2003;29:429–436. [PubMed] [Google Scholar]
- 73.Khumar SS, Kaur P, Kaur S. Effectiveness of shavasana on depression among university students. Indian J Clin Psychol. 1993;20:82–87. [Google Scholar]
- 74.Latha DR, Kaliappan KV. Efficacy of yoga therapy in the management of headaches. J of Indian Psych. 1992;10:41–47. [Google Scholar]
- 75.Manchanda SC, Narang R, Reddy KS, Sachdeva U, Prabhakaran D, Dharmanand S, Rajani M, Bijlani R. Retardation of coronary atherosclerosis with yoga lifestyle intervention. J Assoc Physicians India. 2000;48:687–694. [PubMed] [Google Scholar]
- 76.Mitchell KS, Mazzeo SE, Rausch SM, Cooke KL. Innovative interventions for disordered eating: Evaluating dissonance-based and yoga interventions. Int J Eat Disord. 2007;40:120–128. doi: 10.1002/eat.20282. [DOI] [PubMed] [Google Scholar]
- 77.Moadel AB, Shah C, Wylie-Rosett J, Harris MS, Patel SR, Hall CB, Sparano JA. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. J Clin Oncol. 2007;25:4387–4395. doi: 10.1200/JCO.2006.06.6027. [DOI] [PubMed] [Google Scholar]
- 78.Murugesan R. Effect of selected yogic practices on the management of hypertension. Indian J Physiol Pharmacol. 2000;44:207–210. [PubMed] [Google Scholar]
- 79.Oswal P, Nagarathna R, Ebnezar J, Nagendra HR. The Effect of Add-On Yogic Prana Energization Technique (YPET) on Healing of Fresh Fractures: A Randomized Control Study. J Altern Complement Med. 2011;17:253–258. doi: 10.1089/acm.2010.0001. [DOI] [PubMed] [Google Scholar]
- 80.Pal A, Srivastava N, Tiwari S, Verma NS, Narain VS, Agrawal GG, Natu SM, Kumar K. Effect of yogic practices on lipid profile and body fat composition in patients of coronary artery disease. Complement Ther Med. 2011;19:122–127. doi: 10.1016/j.ctim.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 81.Pullen P. Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. J Card Fail. 2008;14:407–413. doi: 10.1016/j.cardfail.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 82.Pullen P. Benefits of yoga for African American heart failure patients. Med Sci Sports Exerc. 2010;42:651–657. doi: 10.1249/MSS.0b013e3181bf24c4. [DOI] [PubMed] [Google Scholar]
- 83.Pushpika AAM, Somarathna KI, Vyas GH, Dash SC. Clinical evaluation of selected Yogic procedures in individuals with low back pain. Ayu. 2010;31:245–250. doi: 10.4103/0974-8520.72409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Raghavendra RM. Effects of an integrated yoga programme on chemotherapy-induced nausea and emesis in breast cancer patients. Eur J Cancer Care. 2007;16:462–474. doi: 10.1111/j.1365-2354.2006.00739.x. [DOI] [PubMed] [Google Scholar]
- 85.Rani K, Tiwari S, Singh U, Agrawal G, Ghildiyal A, Srivastava N. Impact of yoga nidra on psychological general wellbeing in patients with menstrual irregularities: A randomized controlled trial. Int J Yoga. 2011;4:20–25. doi: 10.4103/0973-6131.78176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Saper R, Sherman KJ, Cullum-Dugan D, Davis RB, Phillips RS, Culpepper L. Yoga for chronic low back pain in a predominantly minority population: A pilot randomized controlled trial. Altern Ther Health Med. 2009;15:18–27. [PMC free article] [PubMed] [Google Scholar]
- 87.Saptharishi L, Soudarssanane M, Thiruselvakumar D, Navasakthi D, Mathanraj S, Karthigeyan M, Sahai A. Community-based randomized controlled trial of non-pharmacological interventions in prevention and control of hypertension among young adults. Indian J Community Med. 2009;34:329–334. doi: 10.4103/0970-0218.58393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sareen S. Yoga: A tool for improving the quality of life in chronic pancreatitis. World J Gastroenterol. 2007;13:391–397. doi: 10.3748/wjg.v13.i3.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Satyapriya M, Nagendra HR, Nagarathna R, Padmalatha V. Effect of integrated yoga on stress and heart rate variability in pregnant women. Int J Gynaecol Obstet. 2009;104:218–222. doi: 10.1016/j.ijgo.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 90.Sharma VK. Effect of Sahaj yoga on depressive disorders. Indian J Physiol Pharmacol. 2005;49:462–8. [PubMed] [Google Scholar]
- 91.Tilbrook HE, Cox H, Hewitt CE, Kang’ombe AR, Chuang LH, Jayakody S, Aplin JD, Semlyen A, Trewhela A, Watt I, Torgerson DJ. Yoga for chronic low back pain: A randomized trial. Ann Intern Med. 2011;155:569–578. doi: 10.7326/0003-4819-155-9-201111010-00003. [DOI] [PubMed] [Google Scholar]
- 92.Vedamurthachar A. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006;94:249–253. doi: 10.1016/j.jad.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 93.Williams KA. Effect of Iyengar yoga therapy for chronic low back pain. Pain. 2005;115:107–117. doi: 10.1016/j.pain.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 94.Williams K. Evaluation of the Effectiveness and Efficacy of Iyengar yoga therapy on chronic low back pain. Spine. 2009;34:2066–2076. doi: 10.1097/BRS.0b013e3181b315cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yogendra J, Yogendra HJ, Ambardekar S, Lele RD, Shetty S, Dave M, Husein N. Beneficial effects of yoga lifestyle on reversibility of ischaemic heart disease: caring heart project of International Board of Yoga. J Assoc Physicians India. 2004;52:283–289. [PubMed] [Google Scholar]
- 96.Yurtkuran M. A modified yoga-based exercise program in hemodialysis patients: A randomized controlled study. Complement Ther Med. 2007;15:164–171. doi: 10.1016/j.ctim.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 97.Joshi S, Khandwe R, Bapat D, Deshmukh U. Effect of yoga on menopausal symptoms. Menopause Int. 2011;17:78–81. doi: 10.1258/mi.2011.011020. [DOI] [PubMed] [Google Scholar]
- 98.Taneja I. Yogic versus conventional treatment in diarrhea-predominant irritable bowel syndrome: A randomized control study. Appl Psychophysiol Biofeedback. 2004;29:19–33. doi: 10.1023/b:apbi.0000017861.60439.95. [DOI] [PubMed] [Google Scholar]
- 99.Chen K. Sleep quality, depression state, and health status of older adults after silver yoga exercises: Cluster randomized trial. Int J Nurs Stud. 2009;46:154–163. doi: 10.1016/j.ijnurstu.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 100.Gopal A, Mondal S, Gandhi A, Arora S, Bhattacharjee J. Effect of integrated yoga practices on immune responses in examination stress - A preliminary study. Int J Yoga. 2011;4:26–32. doi: 10.4103/0973-6131.78178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lee JA, Kim JW, Kim DY. Effects of yoga exercise on serum adiponectin and metabolic syndrome factors in obese postmenopausal women. Menopause. 2012;19:296–301. doi: 10.1097/gme.0b013e31822d59a2. [DOI] [PubMed] [Google Scholar]
- 102.Malathi A, Damodaran A. Stress due to exams in medical students--role of yoga. Indian J Physiol Pharmacol. 1999;43:218–224. [PubMed] [Google Scholar]
- 103.Mekonnen D, Mossie A. Clinical effects of yoga on asthmatic patients: a preliminary clinical trial. Ethiop J Health Sci. 2010;20(2):107–112. [PMC free article] [PubMed] [Google Scholar]
- 104.Mourya M, Mahajan AS, Singh NP, Jain AK. Effect of slow- and fast-breathing exercises on autonomic functions in patients with essential hypertension. J Altern Complement Med. 2009;15:711–717. doi: 10.1089/acm.2008.0609. [DOI] [PubMed] [Google Scholar]
- 105.Panjwani U, Gupta HL, Singh SH, Selvamurthy W, Rai UC. Effect of Sahaja yoga practice on stress management in patients of epilepsy. Indian J Physiol Pharmacol. 1995;39:111–116. [PubMed] [Google Scholar]
- 106.Rakhshaee Z. Effect of three yoga poses (cobra, cat and fish poses) in women with primary dysmenorrhea: A randomized clinical trial. J Pediatr Adolesc Gynecol. 2011;24:192–196. doi: 10.1016/j.jpag.2011.01.059. [DOI] [PubMed] [Google Scholar]
- 107.Stoller CC, Greuel JH, Cimini LS, Fowler MS, Koomar JA. Effects of sensory-enhanced yoga on symptoms of combat stress in deployed military personnel. Am J Occup Ther. 2012;66:59–68. doi: 10.5014/ajot.2012.001230. [DOI] [PubMed] [Google Scholar]
- 108.Subramanian S, Elango T, Malligarjunan H, Kochupillai V, Dayalan H. Role of sudarshan kriya and pranayam on lipid profile and blood cell parameters during exam stress: A randomized controlled trial. Int J Yoga. 2012;5:21–27. doi: 10.4103/0973-6131.91702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Vedanthan PK. Clinical study of yoga techniques in university students with asthma: A controlled study. Allergy Asthma Proc. 1998;19:3–9. doi: 10.2500/108854198778557971. [DOI] [PubMed] [Google Scholar]
- 110.Latha MRS, Kaliappan KV. The efficacy of yoga therapy in the treatment of migraine and tension headaches. J Indian Acad Appl Psychol. 1987;13(2):95–100. [Google Scholar]
- 111.Vogler J, O’Hara L, Gregg J, Burnell F. The impact of a short-term Iyengar yoga program on the health and well-being of physically inactive older adults. Int J Yoga Therap. 2011;21:61–72. [PubMed] [Google Scholar]
- 112.Chattha R, Nagarathna R, Padmalatha V, Nagendra HR. Effect of yoga on cognitive functions in climacteric syndrome: A randomised control study. BJOG: An Intern J of Obstet & Gynaecology. 2008;115:991–1000. doi: 10.1111/j.1471-0528.2008.01749.x. [DOI] [PubMed] [Google Scholar]
- 113.Deshpande S, Nagendra HR, Raghuram N. A randomized control trial of the effect of yoga on verbal aggressiveness in normal healthy volunteers. Intern J of Yoga. 2008;1:76–82. doi: 10.4103/0973-6131.41034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia--A randomized controlled trial. Acta Psychiatr Scand. 2007;116:226–232. doi: 10.1111/j.1600-0447.2007.01032.x. [DOI] [PubMed] [Google Scholar]
- 115.Ebnezar J, Nagarathna R, Bali Y, Nagendra HR. Effect of an integrated approach of yoga therapy on quality of life in osteoarthritis of the knee joint: A randomized control study. Int J Yoga. 2011;4:55–63. doi: 10.4103/0973-6131.85486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gordon L, Morrison EY, McGrowder DA, Young R, Fraser YT, Zamora EM, Alexander-Lindo RL, Irving RR. Effect of exercise therapy on lipid profile and oxidative stress indicators in patients with type 2 diabetes. BMC Complement Altern Med. 2008;8:21. doi: 10.1186/1472-6882-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Haber D. Health promotion to reduce blood pressure level among older blacks. Gerontologist. 1986;26:119–121. doi: 10.1093/geront/26.2.119. [DOI] [PubMed] [Google Scholar]
- 118.Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, Rai L, Sawhney RC. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10:261–268. doi: 10.1089/107555304323062257. [DOI] [PubMed] [Google Scholar]
- 119.Kovačič T, Kovačič M. Impact of relaxation training according to Yoga in Daily Life® system on perceived stress after breast cancer surgery. Integ Cancer Ther. 2011;10:16–26. doi: 10.1177/1534735410387418. [DOI] [PubMed] [Google Scholar]
- 120.Panjwani U, Selvamurthy W, Singh SH, Gupta HL, Mukhopadhyay S, Thakur L. Effect of Sahaja yoga meditation on auditory evoked potentials (AEP) and visual contrast sensitivity (VCS) in epileptics. Appl Psychophysiol Biofeedback. 2000;25:1–12. doi: 10.1023/a:1009523904786. [DOI] [PubMed] [Google Scholar]
- 121.Rakhshani A. Effects of integrated yoga on quality of life and interpersonal relationship of pregnant women. Qual Life Res. 2010;19(10):1447–55. doi: 10.1007/s11136-010-9709-2. [DOI] [PubMed] [Google Scholar]
- 122.Ray US, Sinha B, Tomer OS, Pathak A, Dasgupta T, Selvamurthy W. Aerobic capacity & perceived exertion after practice of Hatha yogic exercises. The Indian J Med Res. 2001;114:215–221. [PubMed] [Google Scholar]
- 123.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: A randomized, controlled trial. Ann Intern Med. 2005;143:849–56. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 124.Santaella DF, Devesa CR, Rojo MR, Amato MB, Drager LF, Casali KR, Montano N, Lorenzi-Filho G. Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: a randomised controlled trial. Brit Med J Open. 2011;1(1):e000085. doi: 10.1136/bmjopen-2011-000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bowman AJ. Effects of aerobic exercise training and yoga on the baroreflex in healthy elderly persons. Eur J Clin Invest. 1997;27:443–449. doi: 10.1046/j.1365-2362.1997.1340681.x. [DOI] [PubMed] [Google Scholar]
- 126.Velikonja O. Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clin Neurol Neurosurg. 2010;112:597–601. doi: 10.1016/j.clineuro.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 127.Patel C, North WRS. Randomised controlled trial of yoga and bio-feedback in management of hypertension. The Lancet. 1975;306:93–95. doi: 10.1016/s0140-6736(75)90002-1. [DOI] [PubMed] [Google Scholar]
- 128.Shannahoff-Khalsa DS, Ray LE, Levine S, Gallen CC, Schwartz BJ, Sidorowich JJ. Randomized controlled trial of yogic meditation techniques for patients with obsessive-compulsive disorder. CNS Spectr. 1999;4:34–47. doi: 10.1017/s1092852900006805. [DOI] [PubMed] [Google Scholar]
- 129.Bowden D, Gaudry C, An SC, Gruzelier J. A comparative randomised controlled trial of the effects of brain wave vibration training, Iyengar yoga, and mindfulness on mood, well-being, and salivary cortisol. Evid-Based Comp and Altern Med. 2011 doi: 10.1155/2012/234713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Visweswaraiah NK. Randomized trial of yoga as a complementary therapy for pulmonary tuberculosis. Respirology. 2004;9:96–101. doi: 10.1111/j.1440-1843.2003.00528.x. [DOI] [PubMed] [Google Scholar]
- 131.Cusumano JA, Robinson SE. Discontinuing postmenopausal hormone therapy: an observational study of tapering versus quitting cold turkey: Is there a difference in recurrence of menopausal symptoms? Applied Psych: An Intern Review. 1993;42:77–90. doi: 10.1097/gme.0b013e31818fbff5. [DOI] [PubMed] [Google Scholar]
- 132.Ghoncheh S, Smith JC. Progressive muscle relaxation, yoga stretching, and ABC relaxation theory. J Clin Psychol. 2004;60:131–136. doi: 10.1002/jclp.10194. [DOI] [PubMed] [Google Scholar]
- 133.Smith C. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med. 2007;15:77–83. doi: 10.1016/j.ctim.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 134.Yang K, Bernardo LM, Sereika SM, Conroy MB, Balk J, Burke LE. Utilization of 3-month yoga program for adults at high risk for Type 2 diabetes: A pilot study. Evid Based Complement Alternat Med. 2009 doi: 10.1093/ecam/nep117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.John PJ, Sharma N, Sharma CM, Kankane A. Effectiveness of yoga therapy in the treatment of migraine without aura: A randomized controlled trial. Headache. 2007;47:654–661. doi: 10.1111/j.1526-4610.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 136.Kröner-Herwig B, Hebing G, van Rijn-Kalkmann U, Frenzel A, Schilkowsky G, Esser G. The management of chronic tinnitus--comparison of a cognitive-behavioural group training with yoga. J Psychosom Res. 1995;39:153–165. doi: 10.1016/0022-3999(94)00098-p. [DOI] [PubMed] [Google Scholar]
- 137.Shankarapillai R, Nair MA, George R. The effect of yoga in stress reduction for dental students performing their first periodontal surgery: A randomized controlled study. Int J Yoga. 2012;5:48–51. doi: 10.4103/0973-6131.91714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Cohen DL, Wintering N, Tolles V, Townsend RR, Farrar JT, Galantino ML, Newberg AB. Cerebral blood flow effects of yoga training: Preliminary evaluation of 4 cases. The J Altern Complement Med. 2009;15:9–14. doi: 10.1089/acm.2008.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Greendale GA, Huang MH, Karlamangla AS, Seeger L, Crawford S. Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: Results of a randomized controlled trial. J Am Geriatr Soc. 2009;57:1569–1579. doi: 10.1111/j.1532-5415.2009.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Manocha R, Marks GB, Kenchington P, Peters D, Salome CM. Sahaja yoga in the management of moderate to severe asthma: A randomised controlled trial. Thorax. 2002;57:110–115. doi: 10.1136/thorax.57.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rao M. Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: A randomized controlled trial. Complement Ther Med. 2009;17:1–8. doi: 10.1016/j.ctim.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 142.Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR., Jr Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601–1603. doi: 10.1001/jama.280.18.1601. [DOI] [PubMed] [Google Scholar]
- 143.Subramanian H, Soudarssanane MB, Jayalakshmy R, Thiruselvakumar D, Navasakthi D, Sahai A, Saptharishi L. Non-pharmacological interventions in hypertension: A community-based cross-over randomized controlled trial. Indian J Comm Med. 2011;36:191–196. doi: 10.4103/0970-0218.86519. [DOI] [PMC free article] [PubMed] [Google Scholar]


