Abstract
BACKGROUND AND OBJECTIVE:
Breastfeeding has been associated with early infant food preferences, but less is known about how breastfeeding is associated with later child diet. The objective of this study was to assess whether any and exclusive breastfeeding duration are associated with child diet at 6 years.
METHODS:
We linked data from the Infant Feeding Practices Study II and Year 6 Follow-Up. We used approximately monthly questionnaires throughout infancy to calculate any and exclusive breastfeeding duration (n = 1355). We calculated median daily frequency of intake of water, milk, 100% juice, fruits, vegetables, sugar-sweetened beverages, sweets, and savory snacks at 6 years from a dietary screener and examined frequency of consumption of each food or beverage group by any and exclusive breastfeeding duration. We used separate multivariable logistic regression models to calculate odds of consuming more than the median daily frequency of intake of food or beverage items, adjusting for confounders.
RESULTS:
Intake of milk, sweets, and savory snacks at 6 years was not associated with any or exclusive breastfeeding duration in unadjusted analyses. Frequency of consumption of water, fruits, and vegetables was positively associated, and intake of sugar-sweetened beverages was inversely associated with any and exclusive breastfeeding duration in adjusted models; 100% juice consumption was inversely associated with exclusive breastfeeding duration only.
CONCLUSIONS:
Among many other health benefits, breastfeeding is associated with a number of healthier dietary behaviors at age 6. The association between breastfeeding and child diet may be an important factor to consider when examining associations between breastfeeding and child obesity and chronic diseases.
Keywords: breastfeeding duration, exclusive breastfeeding, diet, fruits, vegetables, sugar-sweetened beverages
A high-quality diet in childhood is important for optimal growth and development and can help children maintain a healthy body weight. The Dietary Guidelines for Americans (DGA) describes a healthy diet as one that increases intake of nutrient-dense foods such as fruits, vegetables, whole grains, and low-fat and fat-free dairy products and limits consumption of solid fats, added sugars, and refined grains.1 Most children in the United States consume too many low-nutrient, energy-dense foods and do not meet recommendations for intake of fruits and vegetables.2 These suboptimal dietary patterns put children at risk for obesity, chronic diseases, and poor health.1 Dietary patterns have been shown to track from early childhood to later childhood3 and adulthood,4 making it important to establish healthy eating patterns at an early age.
Children’s eating behaviors and food preferences develop early and are influenced by a variety of factors. Infants have an innate preference for sweet and salty flavors and an innate dislike for bitter flavors.5 These preferences can be modified by repeated exposures to different flavors.5 Exposure to flavor begins in utero, when flavors from the mother’s diet are transmitted to amniotic fluid, and continues with early infant milk feeding. A mother’s diet is reflected in her breast milk, exposing breastfed infants to a variety of tastes, whereas formula-fed infants are typically fed 1 brand of formula, providing little variation in flavor.5 Experimental studies have shown that compared with formula-fed infants, breastfed infants are more accepting of new foods during infancy.6–8 This may contribute to breastfed infants being less picky9 and more willing to try and like new foods8,10 than formula fed infants.
Although these experimental studies suggest breastfed infants may be more willing to eat foods such as fruits and vegetables in the short term, it is less clear how early infant feeding is associated with longer-term dietary patterns. Using principal components factor analysis, a nationally representative study from Australia found breastfeeding duration associated with a “healthy, meat, and vegetable” pattern but not with a “noncore food group” or “combination” pattern at 2 to 8 years of age.11 Noncore foods included whole-fat dairy products and sweetened cereals and biscuits, and the combination pattern included candy, pasta and rice, nuts and seeds, and cakes and chocolate. A recent analysis of 4 European cohorts from the United Kingdom, France, Greece, and Portugal found that longer breastfeeding duration was consistently associated with higher fruit and vegetable intake in children 2 to 4 years old.12 Another study from Quebec, Canada found that children exclusively breastfeeding for ≥3 months were more likely to consume ≥2 servings of vegetables per day at 4 years of age, compared with infants who were formula fed or never exclusively breastfed.13 Our objective was to describe how any and exclusive breastfeeding duration were associated with frequency of consumption of foods and beverages at 6 years of age.
Methods
The Infant Feeding Practices Study II (IFPS II) is a longitudinal survey of mothers interviewed during the third trimester of pregnancy and approximately monthly throughout their infant’s first year. Eligibility criteria included that the mother be ≥18 years old and the infant be a singleton born at ≥35 weeks’ gestation, weighing ≥5 lb, and without medical conditions that would affect feeding. In 2012, when children from IFPS II were approximately 6 years of age, mothers were contacted to participate in a cross-sectional Year 6 Follow-Up (Y6FU) study. Among 3033 newborns who participated in IFPS II, 2958 were eligible for Y6FU; 1334 could not be contacted. Of the 1624 contacted, 1542 completed the questionnaire, for a cooperation rate of 95% and an overall response rate of 52%. Detailed methods of the Y6FU, a comparison of respondents and nonrespondents, and a comparison of respondents with a nationally representative sample are presented in the article by Fein et al in this supplement.14 Generally, participants of Y6FU were more likely to be white, higher educated, and married compared with a national sample.14 Similarly, participants of Y6FU were more likely to be older, white, higher educated, and married compared with participants of IFPS II who did not participate in Y6FU.14 IFPS II and Y6FU were approved by the Research Involving Human Subjects Committee of the Food and Drug Administration.
Infant Feeding
Each of the IFPS II postnatal surveys, administered at approximately monthly intervals, included a food frequency chart that asked about an infant’s intake within the past 7 days. Infants were considered to be exclusively breastfeeding at each survey time point that they received only breast milk but no other solid or liquid. On the first survey where the mother indicated she was no longer breastfeeding, she was asked how old her baby was when she completely stopped breastfeeding or pumping milk; we used these data to categorize breastfeeding duration. For infants missing data on breastfeeding duration (n = 160), recall data from Y6FU were used to categorize duration. We categorized breastfeeding duration as never breastfed, >0 to <6 months, 6 to <12 months, and ≥12 months. Exclusive breastfeeding duration was not asked directly but estimated as the midpoint between the infant’s age the last time the mother indicated exclusively breastfeeding and the first time she indicated she was not exclusively breastfeeding. We categorized exclusive breastfeeding duration as never breastfed, breastfed but never exclusively, ever exclusive to <3 months, and ≥3 months. No recall data from Y6FU were available to categorize exclusive breastfeeding duration for those missing data.
Child Diet
The Y6FU included a 28-item dietary history screener that asked about frequency of consumption (times per day, times per week, times per month, or did not eat) in the past month among these 6-year-old children. This diet screener was adapted from the 26-item Dietary Screener Questionnaire developed by the National Cancer Institute, National Institutes of Health, and used in the 2009–10 National Health and Nutrition Examination Survey.15 We were interested in assessing consumption of foods and beverages generally consistent with the categories that the DGA encourages Americans to eat more of or to limit; however, we were limited by the broad food groupings used in the diet screener, and these categorizations are often not completely comparable. For example, our screener did not distinguish between lower- and higher-fat dairy products. The food and beverage categories examined were “water” (tap, bottled, or unflavored sparkling water), “milk” (all types, to drink or on cereal), “100% juice” (100% pure fruit juice or 100% pure vegetable juice), “vegetables” (green leafy or lettuce salad with or without other vegetables; nonfried potatoes such as baked, boiled, or mashed potatoes, potato salad, or sweet potatoes; other vegetables, fresh, frozen, or canned; tomato sauces including salsa, spaghetti with tomato sauce, or mixed into foods such as lasagna), “fruits” (fresh, frozen, or canned but not including juice), “sugar-sweetened beverages” (regular soda or pop that includes sugar, not including diet soda; sweetened drinks such as Kool-Aid, lemonade, sweet tea, Hi-C, cranberry cocktail, or Gatorade), “sweets” (ice cream or other frozen dairy desserts such as frozen yogurt or sherbet, not including sugar-free kinds; sweet foods including candy, cookies, cake, doughnuts, muffins, and toaster pastries), and “savory snacks” (popcorn; snacks such as potato chips, corn chips, pretzels, or crackers). We did not include fried potatoes in the vegetable category because we were interested in assessing intake of vegetables as a healthier dietary component.
Covariates
All covariates are from the baseline IFPS II study. Maternal characteristics included age (18–24, 25–29, 30–34, ≥35 years), race or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), poverty income ratio (<185%, 185%–349%, ≥350%), education (high school or less, 1–3 years of college, college or beyond), prepregnancy BMI (<18.5, 18.5–24.9, 25.0–29.9, ≥30.0), marital status (married, not married), and participation in the Special Supplemental Nutrition Program for Women, Infants, and Children any time in the first year of the infant’s life (yes, no). Infant characteristics included gender, birth weight (<2500, 2500–3999, ≥4000 g), gestational age (<37, ≥37 wk), and whether the child had older siblings (yes, no).
Analytic Sample and Statistical Analysis
Data from IFPS II and Y6FU were available for 1542 participants. Of these, 14 were missing data on diet at 6 years, 1 was missing data on breastfeeding duration, 14 were missing data on exclusive breastfeeding duration, and 163 were missing data on covariates. Data were missing for >1 variable for some children, giving a final analytic sample of 1355. Participants included in the analysis were more likely to breastfeed longer and be white, older, and more educated, with normal prepregnancy BMI compared with those excluded from the sample.
For each food or beverage group, frequency of consumption at 6 years was converted to times per day. We calculated mean, median, and 25th and 75th percentiles for each food and beverage group overall and median frequency of intake by any and exclusive breastfeeding duration. Because data were skewed for nearly all food and beverage groups, we used a Kruskal–Wallis analysis of variance test to examine whether daily frequency of consumption differed by any or exclusive breastfeeding duration; this is a nonparametric test that assesses differences in sample distributions. We additionally conducted analyses using the geometric mean instead of the median, and results were consistent, so only data on medians are presented. For those food and beverage groups where frequency of consumption differed significantly (P < .05) by any or exclusive breastfeeding duration, we conducted separate multivariable logistic regression analyses. The outcome variable for each model was dichotomized as above versus at or below the median daily frequency of consumption. Models were adjusted for all covariates described earlier.
Results
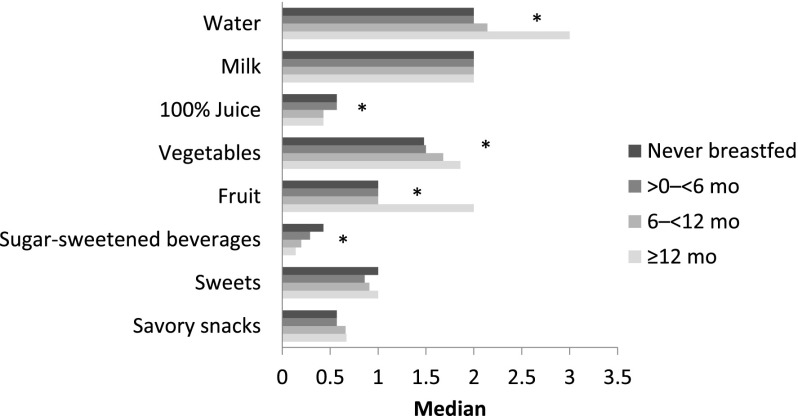
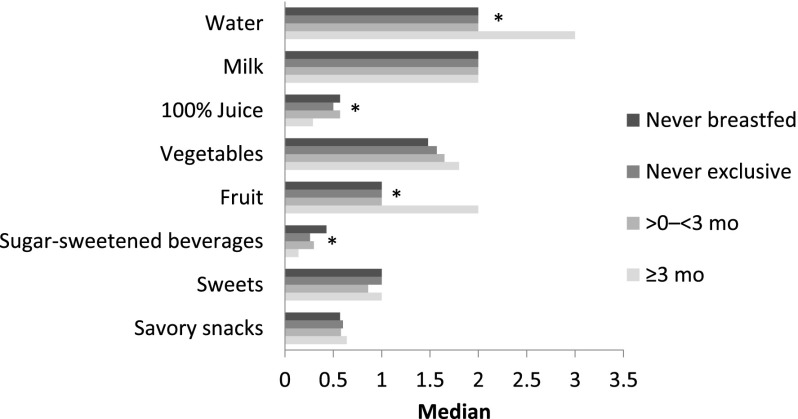
The mean, median, and 25th and 75th percentiles of daily frequency of consumption for each of the food and beverage categories are presented in Table 1. Median daily frequency of consumption ranged from 0.27 for sugar-sweetened beverages to 3.00 for water. Median frequency of consumption of water, fruits, and vegetables was higher among children with longer breastfeeding durations, and frequency of consumption of 100% juice and sugar-sweetened beverages was lower among children with longer breastfeeding durations; there was no association between breastfeeding duration and frequency of consumption of milk, sweets, or savory snacks (Fig 1). These relationships were consistent for exclusive breastfeeding duration, except that the association with frequency of vegetable consumption was no longer significant (P = .08; Fig 2).
TABLE 1.
Daily Frequency (per Day) of Consumption of Various Food and Beverage Categories Among Children 6 y Old (n = 1355)
| Mean | Median | 25th Percentile | 75th Percentile | |
|---|---|---|---|---|
| Water | 2.80 | 3.00 | 1.00 | 4.00 |
| Milk | 1.77 | 2.00 | 1.00 | 2.00 |
| 100% juice | 0.73 | 0.43 | 0.14 | 1.00 |
| Vegetablesa | 1.85 | 1.58 | 1.01 | 2.43 |
| Fruits | 1.37 | 1.00 | 0.57 | 2.00 |
| Sugar-sweetened beveragesb | 0.50 | 0.27 | 0.07 | 0.64 |
| Sweetsc | 0.97 | 1.00 | 0.46 | 1.17 |
| Savory snacksd | 0.76 | 0.58 | 0.36 | 1.07 |
Includes green leafy vegetables; potatoes (not fried); tomato sauce; and fresh, frozen, or canned vegetables other than green leafy or lettuce, potatoes, or beans.
Includes regular soda or pop that contains sugar, and sweetened drinks such as Kool-Aid, lemonade, sweet tea, Hi-C, cranberry cocktail, or Gatorade.
Includes ice cream and other frozen dairy desserts, and sweet foods such as candy, cookies, cake, doughnuts, and toaster pastries.
Includes popcorn and snacks such as potato chips, corn chips, pretzels, and crackers.
FIGURE 1.
Median daily frequency of intake of various foods and beverages at 6 y, by breastfeeding duration. *Medians vary significantly by breastfeeding duration, P < .05.
FIGURE 2.
Median daily frequency of intake of various foods and beverages at 6 y, by exclusive breastfeeding duration. *Medians vary significantly by exclusive breastfeeding duration, P < .05.
In adjusted analyses, compared with children who were never breastfed, children breastfed for ≥6 months had higher odds of consuming more than the median daily frequency of fruits at 6 years of age, and children breastfed ≥12 months had higher odds of higher frequency of consumption of water and vegetables (Table 2). Breastfeeding for ≥6 months was associated with lower odds of consuming more than the median daily frequency of sugar-sweetened beverages at 6 years. There was no significant association between breastfeeding duration and 100% juice consumption in adjusted analyses.
TABLE 2.
Odds of Consuming More Than the Median Daily Frequency of Foods and Beverages at 6 y by Any and Exclusive Breastfeeding Duration (n = 1355)a
| Water | 100% Juice | Fruits | Vegetablesb | Sugar-Sweetened Beverages | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Breastfeeding duration | ||||||||||
| Never breastfed | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| >0 to <6 mo | 1.18 | 0.83–1.69 | 0.87 | 0.60–1.25 | 1.08 | 0.75–1.56 | 1.06 | 0.74–1.51 | 0.87 | 0.61–1.26 |
| 6 to <12 mo | 1.42 | 0.97–2.07 | 0.80 | 0.54–1.18 | 1.61 | 1.09–2.34 | 1.37 | 0.94–1.99 | 0.65 | 0.45–0.96 |
| ≥12 mo | 2.73 | 1.86–4.00 | 0.77 | 0.52–1.12 | 2.09 | 1.40–3.11 | 1.65 | 1.14–2.40 | 0.52 | 0.36–0.78 |
| Exclusive breastfeeding duration | ||||||||||
| Never breastfed | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| Breastfed, never exclusive | 1.31 | 0.93–1.86 | 0.86 | 0.60–1.22 | 1.28 | 0.89–1.82 | 1.10 | 0.78–1.56 | 0.70 | 0.49–0.99 |
| Ever exclusive to <3 mo | 1.13 | 0.74–1.72 | 0.94 | 0.63–1.39 | 1.21 | 0.81–1.81 | 1.32 | 0.90–1.95 | 0.99 | 0.67–1.46 |
| ≥3 mo | 2.70 | 1.79–4.09 | 0.64 | 0.43–0.94 | 2.03 | 1.34–3.06 | 1.45 | 1.00–2.13 | 0.50 | 0.34–0.73 |
CI, confidence interval; OR, odds ratio; —, referent group.
Separate logistic regression models for breastfeeding duration and exclusive breastfeeding duration were each adjusted for baseline maternal characteristics (age, education, race or ethnicity, poverty income ratio, marital status, Special Supplemental Nutrition Program for Women, Infants, and Children participation, and prepregnancy BMI) and child characteristics (gender, birth wt, gestational age, and older siblings).
Includes green leafy vegetables; potatoes (not fried); tomato sauce; and fresh, frozen, or canned vegetables other than green leafy or lettuce, potatoes, or beans.
Compared with children who were never breastfed, children exclusively breastfed for ≥3 months had higher odds of consuming more than the median daily frequency of water, fruits, and vegetables, and lower odds of consumption of 100% juice and sugar-sweetened beverages at 6 years. We conducted an additional analysis limiting our sample to only children who were ever breastfed (n = 1172). Generally the results were consistent, showing that longer durations of any and exclusive breastfeeding were associated with higher odds of consuming more than the mean daily frequency of water, fruits, and vegetables and lower odds of consuming sugar-sweetened beverages and 100% juice (data not shown).
Discussion
We found that both any and exclusive breastfeeding duration were positively associated with frequency of consumption of foods and beverages generally consistent with categories the DGA recommends consuming more of, such as fruits and vegetables. Any and exclusive breastfeeding was inversely associated with consumption of sugar-sweetened beverages, a major contributor to added sugars, and 100% juice, which the DGA recommends limiting. This suggests that in this cohort, among the food and beverage groups we examined, longer durations and exclusivity of breastfeeding generally reflected a healthier dietary pattern at 6 years of age. The associations with fruits and vegetables may result in part from children exposed to breast milk being more willing to accept new foods,8 because reluctance to try new foods has been associated with lower fruit and vegetable intakes.16 Data on the association between breastfeeding and sugar-sweetened beverage intake are limited. One national study from Norway found that among 12-month-old infants, breastfed infants had a significantly lower mean daily intake of sugar-sweetened beverages than nonbreastfed infants.17 The authors did not speculate on the reasons behind this association.
Another explanation for our findings is that women who choose and continue to breastfeed may be more likely to encourage consumption of healthful foods and limit consumption of less healthful foods by their children than women who do not breastfeed. Women who breastfeed longer have been shown to have greater intake of fruits and vegetables themselves,18,19 and maternal dietary preferences are important independent predictors of children’s dietary preferences.20 However, in the UK and Portuguese cohort studies where data on maternal diet were available, longer breastfeeding durations remained significantly associated with higher fruit and vegetable intakes in childhood after adjustment for maternal fruit or vegetable intake.12 Sociodemographic characteristics associated with longer durations of breastfeeding, such as higher income and education levels,21 have also been associated with higher intakes of fruits and vegetables22 and lower intakes of full-fat dairy,23 added sugars,24 and a junk food pattern characterized by high-fat, high-sugar, processed, and convenience foods.25 Although we have adjusted for many of these socioeconomic factors, there may be other differences, such as culture or environmental characteristics that we were not able to control adequately.
Several studies have examined the association between breastfeeding and chronic health outcomes, including child obesity and metabolic illness. Many of these studies have not considered, or considered only limited aspects of, dietary intake in analyses, and residual confounding is often given as a reason for discrepancies in results.26,27 Our results indicate that child diet may be influenced by breastfeeding duration and thus may serve as an important confounder or mediator in the relationship between breastfeeding and chronic health outcomes in childhood that should be considered in future studies.
Our analysis has several strengths and limitations. The study design of IFPS II and Y6FU allowed detailed information to be collected through infancy and at 6 years with a short recall period, reducing the potential for recall bias and allowing us to control for multiple confounders. However, the sample is not nationally representative, with women in the analysis typically more educated and of higher income than women in the general population. Dietary intake at 6 years was based only on frequency of consumption and did not collect portion size information to evaluate total intake. The dietary screener used to assess this information has not been formally validated in children of this age. Finally, we were able to examine only select food groups and could not look at an overall dietary pattern.
Conclusions
The association of breastfeeding with more frequent water, fruit, and vegetable consumption and less frequent sugar-sweetened beverage consumption later in childhood may be an important factor to consider when examining associations between breastfeeding and the development of obesity and other chronic diseases. There is substantial evidence documenting the many benefits of breastfeeding; improved child diet may be 1 additional benefit. Additional research could probe the reasons that breastfeeding is associated with child diet. In the meantime, all mothers should be supported to meet breastfeeding recommendations.
Glossary
- CI
confidence interval
- DGA
Dietary Guidelines for Americans
- IFPS II
Infant Feeding Practices Study II
- OR
odds ratio
- Y6FU
Year 6 Follow-Up
Footnotes
Dr Perrine contributed to the analytic study design, conducted the analysis, and drafted the manuscript; Dr Galuska contributed to the analytic study design; Dr Thompson contributed to development of the dietary screener; Dr Scanlon contributed to development of the dietary screener and contributed to the analytic study design; and all authors reviewed and approved the final manuscript as submitted.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official positions of the Centers for Disease Control and Prevention or the National Institutes of Health.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This study was funded by the US Food and Drug Administration, Centers for Disease Control and Prevention, Office on Women's Health, National Institutes of Health, and Maternal and Child Health Bureau in the US Department of Health and Human Services.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.US Department of Agriculture, US Department of Health and Human Services Dietary Guidelines for Americans, 2010. Washington, DC: US Government Printing Office; 2010 [Google Scholar]
- 2.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. J Acad Nutr Diet. 2012;112(5):624–635, e626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Northstone K, Emmett PM. Are dietary patterns stable throughout early and mid-childhood? A birth cohort study. Br J Nutr. 2008;100(5):1069–1076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mikkilä V, Räsänen L, Raitakari OT, Pietinen P, Viikari J. Consistent dietary patterns identified from childhood to adulthood: the cardiovascular risk in Young Finns Study. Br J Nutr. 2005;93(6):923–931 [DOI] [PubMed] [Google Scholar]
- 5.Beauchamp GK, Mennella JA. Early flavor learning and its impact on later feeding behavior. J Pediatr Gastroenterol Nutr. 2009;48(suppl 1):S25–S30 [DOI] [PubMed] [Google Scholar]
- 6.Hausner H, Nicklaus S, Issanchou S, Mølgaard C, Møller P. Breastfeeding facilitates acceptance of a novel dietary flavour compound. Clin Nutr. 2010;29(1):141–148 [DOI] [PubMed] [Google Scholar]
- 7.Maier AS, Chabanet C, Schaal B, Leathwood PD, Issanchou SN. Breastfeeding and experience with variety early in weaning increase infants’ acceptance of new foods for up to two months. Clin Nutr. 2008;27(6):849–857 [DOI] [PubMed] [Google Scholar]
- 8.Forestell CA, Mennella JA. Early determinants of fruit and vegetable acceptance. Pediatrics. 2007;120(6):1247–1254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galloway AT, Lee Y, Birch LL. Predictors and consequences of food neophobia and pickiness in young girls. J Am Diet Assoc. 2003;103(6):692–698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan SA, Birch LL. Infant dietary experience and acceptance of solid foods. Pediatrics. 1994;93(2):271–277 [PubMed] [Google Scholar]
- 11.Grieger JA, Scott J, Cobiac L. Dietary patterns and breast-feeding in Australian children. Public Health Nutr. 2011;14(11):1939–1947 [DOI] [PubMed] [Google Scholar]
- 12.de Lauzon-Guillain B, Jones L, Oliveira A, et al. The influence of early feeding practices on fruit and vegetable intake among preschool children in 4 European birth cohorts. Am J Clin Nutr. 2013;98(3):804–812 [DOI] [PubMed] [Google Scholar]
- 13.Burnier D, Dubois L, Girard M. Exclusive breastfeeding duration and later intake of vegetables in preschool children. Eur J Clin Nutr. 2011;65(2):196–202 [DOI] [PubMed] [Google Scholar]
- 14.Fein SB, Li R, Chen J, Scanlon KS, Grummer-Strawn LM. Methods for the year 6 follow-up study of children in the Infant Feeding Practices Study II. Pediatrics. 2014;134(suppl 1):S4–S12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Cancer Institute. Dietary Screener Questionnaires (DSQ) & SAS programs. Available at: http://riskfactor.cancer.gov/studies/nhanes/dietscreen/questionnaires.html. Accessed July 2, 2013
- 16.Wardle J, Cooke LJ, Gibson EL, Sapochnik M, Sheiham A, Lawson M. Increasing children’s acceptance of vegetables; a randomized trial of parent-led exposure. Appetite. 2003;40(2):155–162 [DOI] [PubMed] [Google Scholar]
- 17.Lande B, Andersen LF, Veierød MB, et al. Breast-feeding at 12 months of age and dietary habits among breast-fed and non-breast-fed infants. Public Health Nutr. 2004;7(4):495–503 [DOI] [PubMed] [Google Scholar]
- 18.Pesa JA, Shelton MM. Health-enhancing behaviors correlated with breastfeeding among a national sample of mothers. Public Health Nurs. 1999;16(2):120–124 [DOI] [PubMed] [Google Scholar]
- 19.Amir LH, Donath SM. Maternal diet and breastfeeding: a case for rethinking physiological explanations for breastfeeding determinants. Early Hum Dev. 2012;88(7):467–471 [DOI] [PubMed] [Google Scholar]
- 20.Howard AJ, Mallan KM, Byrne R, Magarey A, Daniels LA. Toddlers’ food preferences. The impact of novel food exposure, maternal preferences and food neophobia. Appetite. 2012;59(3):818–825 [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Breastfeeding among US children born 2000–2009, CDC National Immunization Survey. 2012. Available at: www.cdc.gov/breastfeeding/data/nis_data/. Accessed July 10, 2013
- 22.Xie B, Gilliland FD, Li YF, Rockett HR. Effects of ethnicity, family income, and education on dietary intake among adolescents. Prev Med. 2003;36(1):30–40 [DOI] [PubMed] [Google Scholar]
- 23.Dennison BA, Erb TA, Jenkins PL. Predictors of dietary milk fat intake by preschool children. Prev Med. 2001;33(6):536–542 [DOI] [PubMed] [Google Scholar]
- 24.Kranz S, Siega-Riz AM. Sociodemographic determinants of added sugar intake in preschoolers 2 to 5 years old. J Pediatr. 2002;140(6):667–672 [DOI] [PubMed] [Google Scholar]
- 25.Northstone K, Emmett P. Multivariate analysis of diet in children at four and seven years of age and associations with socio-demographic characteristics. Eur J Clin Nutr. 2005;59(6):751–760 [DOI] [PubMed] [Google Scholar]
- 26.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 2005;115(5):1367–1377 [DOI] [PubMed] [Google Scholar]
- 27.Owen CG, Whincup PH, Cook DG. Breast-feeding and cardiovascular risk factors and outcomes in later life: evidence from epidemiological studies. Proc Nutr Soc. 2011;70(4):478–484 [DOI] [PubMed] [Google Scholar]