Abstract
The intestine is the largest mucosal organ of the body and also the first line immune homeostasis. Inflammatory bowel disease or IBD is divided into ulcerative colitis and Crohn's disease. One of the problems that can occur with UC is dietary allergy to some foods. This study aimed to evaluated the dairy allergy among patients with ulcerative colitis. This study is a Case - control study, that studied 72 patients with Ulcerative Colitis, after recording history of the disease, colonoscopy and confirmed by biopsy and 72 person without history of colitis. In this study, in order to investigate of food allergy, used of the EUROMMUM kit with an international code number DP3420-1601-11E. We used chi-square and Monte Carlo method for analysis of data. Among UC patients, 30.6% mild, 52.8% moderate and 16.6% of cases were in sever stage. 9.7% of them reported a history of abdominal surgery due to disease. According to the chi-square and Monte Carlo methods, dairy allergy (including: cow milk, cow milk UHT and casein) in UC group was significant (P=0.00). This study indicated that there is significant relationship between UC and cow milk, cow milk UHT and casein. UC patients who are allergic to dairy products and the use of dairy products can increase the severity of UC.
Keywords: Dairy allergy, ulcerative colitis, cow milk
Background
The intestine is the largest mucosal organ of the body and also the first line immune homeostasis [1, 2], inflammatory bowel disease or IBD is divided into ulcerative colitis and Crohn's disease. Ulcerative colitis (UC) are recognized by recurrent and episodic attacks that limited to the mucosal layer of the colon [3]. In critically ill patients with severe conflicts the inflammation may even pass through the mucous layer and reach the muscle layer. In this condition intestinal motility has been impaired, bowel movements decreased and the patient may go into the toxic mega colon [4, 5]. The disease was introduced first by Wills in London as a separate disease from clinical diarrhea [6]. The genetic relationship between UC and IBD has been demonstrated and if a person is infected, the risk of incidence of IBD in first-degree relatives is 10 % [7]. The incidence of UC varies within different geographic regions. It`s prevalence is lower in Asian races than in European and North American races. The first peak age of UC is between 15 and 30 years. Second peak occurs between the ages of 60 and 80 and male to female ratio for UC is 1:1. Studies have shown that risk of UC and its episodes in smoker persons is 40% in comparison to nonsmokers. In terms of pathology, UC usually involves the rectal mucus and extends proximally to involve all or part of the colon. Most of the patients who have disease limited to the rectum and recto sigmoid and involvement of more than sigmoid is in the next level. On the other hand, genetics and environmental factors play a major role in the pathogenesis of UC and having a family member increase the risk of the other family members [7, 8]. Among environmental factors the micro flora of colon and the components of food (antigens) may play important role in the pathogenesis of IBD and UC [8]. One of the problems that can occur with UC is dietary allergy to some foods. Food allergy involves an abnormal immune response that is usually causes hypersensitivity to the protein [9, 10]. There are three mechanisms for this sensitivity, they are: Dependent to IgE, Independent to IgE and Mix mechanism [11, 12] Dependent to IgE reaction is usually fast and due to specific IgE like food allergens and allergy. Studies have shown that the food allergy in patients with ulcerative colitis is mainly due to an IgE-dependent reaction and IgE in rectal mucosa of patients indicated. It is because that, today is strongly recommended for patients with ulcerative colitis to use of special diets and main diet is milk and dairy-free diet for them [8]. The objective of this study is to assess dairy allergy among patients with ulcerative colitis.
Methodology
Study Population:
Case - control study, in this study, 72 patients with Ulcerative Colitis, after recording history of the disease, colonoscopy and confirmed by biopsy entered into the study. In the control group, we selected 72 persons without a history of intestinal problems, of course with normal colonoscopy view. Control group as possible in terms of status, age and gender is conformed to case groups.
Clinical Investigations:
The diagnosis of ulcerative colitis was performed by the typical history of patient endoscopic, seeing the mucosal view and biopsy of intestinal and final confirmation of pathologist. Biopsy confirmed the diagnosis of ulcerative colitis, in Pathologic appearance can be seen many cases such as chronic mucosal changes, atrophy of the glands and deficiency of niacin in goblet cell. For patients whose disease was in its early stages use of Flexible sigmoidoscopy for diagnosis of disease [13–15] (Figure 1).
Figure 1.
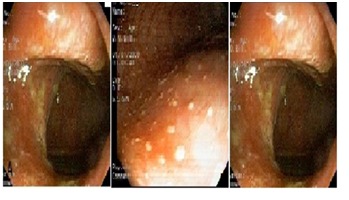
Three view of colon disorder in Ulcerative colitis
Laboratory Investigations:
In this study, in order to investigate of food allergy, we used the EUROMMUM kit with an international code number DP3420-1601-11E. Buy this kit; we checked Cow milk, Cow milk UHT and Casein allergy among case and control groups. Complete Blood Count (CBC) checked for anemia. (World Health Organization criteria for anemia in men and women are hemoglobin ) <13 and <12 g/DL).
Study Measurements:
The food allergy kit is a work based on the measurement of IgE levels and the bands calculated in Enzyme Allergo Sorbent Test (EAST). In this study also were used Mayo Scoring System to investigate and judge about the severity of the disease and control of being treated patients. Received points of patients were between zero and 12 higher numbers indicate greater severity of illness [15].
Feeding in Patients:
Initially, the nutritional status of patients were evaluated that including body mass index, dietary received, daily intake of energy and protein in the serum [16– 18].
Statistical analysis:
The Statistical Package for the Social Science program (SPSS, version 19.0) was used. We used chi-square and Monte Carlo method for analysis of data.
Results
One hundred forty two cases, including 72 patients (50%) with UC and 72 healthy subjects (50%) were studied. Among case group, most patient were between 26-30 and 31-35 years (each category 41.7% ) but in control group, 20-25 and 26-30 years category (each category 38.9%) were the dominant groups (Table 1). Of educational, most patients were bachelor (BA) (41.7%) and in control group, diploma and advanced diploma (38.9%) with BA (38.9%) had the highest frequency. In Complete Blood Count or CBC, 47.2% of patients and 19.4% from control group had anemia. 33.3% of UC patients were active smoker and fourteen cases from control group (38.9%) were active smoker. Among case group, only ten patients (13.9%) reported a history of screening for gastrointestinal cancer and also, twenty patients (27.8%) expressed the familial history about cancer of gastrointestinal. Among UC patients, 30.6% mild, 52.8% moderate and 16.6% of cases were in sever stage. 9.7% of them reported a history of abdominal surgery due to disease. According to the chi-square and Monte Carlo methods, dairy allergy (including: cow milk, cow milk UHT and casein) in UC group was significant (P=0.00). Complete information׳s about severity of allergic reaction in both case and control groups in table was written Table 1 (see supplementary material).
Discussion
Ulcerative colitis is an inflammatory bowel disease, its etiology is not properly identified [19– 22], the pattern of disease is chronic in most patients that determined with acute attacks that periodically takes weeks [23]. Food allergy is one of the problems that can arise with ulcerative colitis. Food allergy is an abnormal immune reaction that usually occurs against proteins [9, 10]. So in Ulcerative colitis patients, it is recommended that have the diet with a minimum consumption of dairy products. Use of some medications, especially non-steroidal anti-inflammatory drugs can because of similar symptoms. Bleeding by induced -Penicillin is rare, but should be considered [24– 26]. The fact of the matter is that, although most of the patients mention specific foods as aggravate their symptoms, but so far do not a complete and comprehensive study in this regard. And this is a very clear need that, in recent study evaluated Dairy allergy among ulcerative colitis patients. In this case-control study, 72 UC patients were compared with 72 healthy persons to determine the dairy allergy. In this study, for better and more precisely study, according to the Mayo criteria, patients with ulcerative colitis were classified to mild, moderate and sever group. In Mekkel G study which has done on IBD patients, results showed that anti casein-antibody in UC group have higher levels in comparison to control group. D'Arienzo et al showed that serum level of antibody against food protein and clinical symptoms in ulcerative colitis patients significantly was higher than normal persons. In this study level of allergic symptoms in 56% and allergic reaction in 52% of UC patients was found. But in control persons these amount was 18% and 26%. In other hand, our results were shown that levels of anti-body against dairy protein significantly were higher than control group [27]. In our study like Mishkin S, using dairy and lactolose due to allergic reaction in UC patients, but D B Jones and Brignola C study expressed different results [28]. In D B Jones and Brignola C study, dairy allergy in both groups (UC patients and control group) haven׳t a clearly difference. Most previous studies has correlate with this study and all of them indicated the dairy allergy between patients with ulcerative colitis and this is very important for treatment of these patients. At the end of, however, in the old studies likes D B Jones and Brignola C, results denied the existence of the food allergy, especially dairy allergy among UC patients, but in new study like this study, there is a significant relationship between dairy allergy and ulcerative colitis [29].
Conclusion
This study indicated that there is significant relationship between UC and cow milk, cow milk UHT and casein. UC patients who are allergic to dairy products and the use of dairy products can increase the severity of UC. It is recommended to UC patients that less use from dairy products.
Supplementary material
Footnotes
Citation:Judaki et al, Bioinformation 10(11): 693-696 (2014)
References
- 1.GARSIDE P, et al. Annals of the New York Academy of Sciences. 2004:1029. doi: 10.1196/annals.1309.002. [DOI] [PubMed] [Google Scholar]
- 2.Nagler-Anderson C. Nat Rev Immunol. 2001;1:59. doi: 10.1038/35095573. [DOI] [PubMed] [Google Scholar]
- 3.Corrao G, et al. Int J Epidemiol. 1998;27:397. doi: 10.1093/ije/27.3.397. [DOI] [PubMed] [Google Scholar]
- 4.Jalan K, et al. Gastroenterology. 1969;57:68. [PubMed] [Google Scholar]
- 5.Greenstein A, et al. J Clin Gastroenterol. 1985;7:137. doi: 10.1097/00004836-198504000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Kedia S, et al. World J Gastrointest Pathophysiol. 2014;5:579. doi: 10.4291/wjgp.v5.i4.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryoo SB, et al. World J Gastroenterol. 2014;20:7488. doi: 10.3748/wjg.v20.i23.7488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mekkel G, et al. Orv Hetil. 2005;146:797. [PubMed] [Google Scholar]
- 9.Burks AW, et al. J Allergy Clin Immunol. 2008;121:1344. doi: 10.1016/j.jaci.2008.02.037. [DOI] [PubMed] [Google Scholar]
- 10.Chehade M, Mayer L. J Allergy Clin Immunol. 2005;115:3. doi: 10.1016/j.jaci.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Blanchard C, et al. J Allergy Clin Immunol. 2006;118:1054. doi: 10.1016/j.jaci.2006.07.038. [DOI] [PubMed] [Google Scholar]
- 12.Hogan SP, et al. Clin & Exp Allergy. 2008;38:229. doi: 10.1111/j.1365-2222.2007.02915.x. [DOI] [PubMed] [Google Scholar]
- 13.Yang H, et al. Gut. 1993;34:517. doi: 10.1136/gut.34.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orholm M, et al. N Engl J Med. 1991;324:84. doi: 10.1056/NEJM199101103240203. [DOI] [PubMed] [Google Scholar]
- 15.Orholm M, et al. Am J Gastroenterol. 1999;94:3236. doi: 10.1111/j.1572-0241.1999.01526.x. [DOI] [PubMed] [Google Scholar]
- 16.Husain A, korzenik JR. Semin Gastrointest Dis. 1998;9:21. [PubMed] [Google Scholar]
- 17.Delgado-Rodriguez M, et al. Arch Surg. 2002;137:805. doi: 10.1001/archsurg.137.7.805. [DOI] [PubMed] [Google Scholar]
- 18.Vagianos K, et al. JPEN J Parenter Enteral Nutr. 2007;31:311. doi: 10.1177/0148607107031004311. [DOI] [PubMed] [Google Scholar]
- 19.Saxena A, et al. J Tradit Complement Med. 2014;4:203. doi: 10.4103/2225-4110.139111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karlinger K, et al. Eur J Radiol. 2000;35:154. doi: 10.1016/s0720-048x(00)00238-2. [DOI] [PubMed] [Google Scholar]
- 21.Garcia Rodriguez LA, et al. Aliment pharmacol Ther. 2005;22:309. doi: 10.1111/j.1365-2036.2005.02564.x. [DOI] [PubMed] [Google Scholar]
- 22.Kurina LM, et al. J Epidemiol Community Health. 2001;55:716. doi: 10.1136/jech.55.10.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dehghani M, et al. Int J Organ Transplant Med. 2012;3:120. [PMC free article] [PubMed] [Google Scholar]
- 24.Davies NM. Dis Colon Rectum. 1995;38:1311. doi: 10.1007/BF02049158. [DOI] [PubMed] [Google Scholar]
- 25.Moulis H, Vender RJ. J Clin Gastroenterol. 1994;18:227. doi: 10.1097/00004836-199404000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Dietrich CF, et al. Dtsch Med Wochenschr. 2000;125:755. doi: 10.1055/s-2007-1024491. [DOI] [PubMed] [Google Scholar]
- 27.D'Arienzo A. Scand J Gastroenterol. 2000;35:624. doi: 10.1080/003655200750023598. [DOI] [PubMed] [Google Scholar]
- 28.Mishkin S. Am J Clin Nutr. 1997;65:564. doi: 10.1093/ajcn/65.2.564. [DOI] [PubMed] [Google Scholar]
- 29.Jones DB, et al. J R Soc Med. 1981;74:292. doi: 10.1177/014107688107400411. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


