Abstract
Background
Neovascular glaucoma (NVG) is a potentially blinding secondary glaucoma. It is caused by the formation of abnormal new blood vessels which prevent normal drainage of aqueous from the anterior segment of the eye. Anti-vascular endothelial growth factor (anti-VEGF) agents are specific inhibitors of the primary mediators of neovascularization. Studies have reported the effectiveness of anti-VEGFs for the control of intraocular pressure (IOP) in NVG.
Objectives
To compare the IOP lowering effects of intraocular anti-VEGF agents to no anti-VEGF treatment, as an adjunct to existing modalities for the treatment of NVG.
Search methods
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (The Cochrane Library 2012, Issue 12), Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE, (January 1950 to January 2013), EMBASE (January 1980 to January 2013), Latin American and Caribbean Literature on Health Sciences (LILACS) (January 1982 to January 2013), the metaRegister of Controlled Trials (mRCT) (www.controlled-trials.com), ClinicalTrials.gov (www.clinicaltrials.gov/) and the WHO International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). We did not use any date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 11 January 2013.
Selection criteria
We included randomized controlled trials (RCTs) and quasi-RCTs of people treated with anti-VEGF agents for NVG.
Data collection and analysis
Two authors independently assessed the search results for trials to be included in the review. Discrepancies were resolved by discussion with a third author. Since no trial met our inclusion criteria, no assessment of risk of bias or meta-analysis was undertaken.
Main results
No RCTs were found that met the inclusion criteria for this review. Two RCTs of anti-VEGF agents for treating NVG were not included in the review due to the heterogeneity and uncontrolled assignment of adjunct treatments received by the study participants.
Authors’ conclusions
Currently available evidence is insufficient to evaluate the effectiveness of anti-VEGF treatments, such as intravitreal ranibizumab or bevacizumab, as an adjunct to conventional treatment in lowering IOP in NVG. Well designed RCTs are needed to address this issue, particularly trials that evaluate long-term (at least six months) benefits and risks since the effects of anti-VEGF agents may be short-term only. An RCT comparing anti-VEGF agents with no anti-VEGF agents taking into account the need for co-interventions, such as panretinal photocoagulation (PRP), glaucoma shunt procedures, cyclodestructive procedures, cataract surgery, and deep vitrectomy, could be of use to investigate the additional beneficial effect of anti-VEGF agents in treating NVG. Since decisions for when and which co-interventions should be used are based on clinical criteria, they would not be appropriate for randomization. However, the design of a study on this topic should aim to balance groups by stratification of co-intervention at time of randomization or by enrolling a sufficient number of participants to conduct subgroup analysis by co-interventions (ideally 15 participants per treatment group for each subgroup). Alternatively, the inclusion criteria for a trial could limit participants to those who receive the same co-intervention.
BACKGROUND
Description of the condition
Neovascular glaucoma (NVG) is a secondary glaucoma in which new vessels, and subsequently fibrous tissue, form in the anterior chamber angle of the eye. This leads to blockage of the angle which inhibits aqueous drainage causing elevated intraocular pressure (IOP). This condition was described as early as 1871 (Pagenstecher 1871; Tsai 2008). Historically, it also has been referred to as rubeotic glaucoma, hemorrhagic glaucoma, thrombotic glaucoma, congestive glaucoma, and diabetic hemorrhagic glaucoma.
Clinical conditions causing retinal ischemia such as proliferative diabetic retinopathy (PDR), central retinal vein occlusion (CRVO), and ocular ischemic syndrome are associated with NVG. The condition can be unilateral or bilateral depending on the underlying cause for the NVG. Diabetic retinopathy is usually bilateral and CRVO unilateral. Retinal ischemia results in the release of angiogenic factors such as vascular endothelial growth factor (VEGF). The angiogenic factors then diffuse into the aqueous and anterior segment and trigger neovascularization of the iris and anterior chamber angle. This process leads to fibrous tissue proliferation and subsequent synechial angle-closure (closure of the angle due to the iris adhering to the cornea). Increased levels of VEGF have been measured in the aqueous of patients with NVG (Aiello 1994; Sone 1996; Tripathi 1998). Elevated IOP is a direct result of this secondary angle-closure glaucoma.
NVG is a potentially devastating glaucoma. Delayed diagnosis or poor management can result in complete loss of vision with intractable pain. Early diagnosis of the disease, followed by immediate and aggressive treatment, is imperative. In managing NVG, it is essential to treat both the elevated IOP and the underlying cause of the disease.
General principles for treating patients with NVG include identifying the underlying etiology, reducing the symptoms, and controlling or eliminating retinal ischemia. Panretinal photocoagulation (PRP) ablates the ischemic retina by shrinking and eliminating the abnormal blood vessels; however, when most of the angle is closed due to synechiae consequent to the angle neovascularization, surgical treatment to control IOP is necessary. Aqueous drainage devices (Minckler 2006; Yalvac 2007), Nd-Yag cyclophotocoagulation (Delgado 2003), vitrectomy with PRP and trabeculectomy (Kiuchi 2006), as well as cyclocryotherapy (Kovacic 2004) are the methods of treatment for NVG. These surgical treatments may be done in conjunction with wound healing agents, such as 5-Fluorouracil (5-FU) or mitomycin C (MMC) (Wilkins 2005; Wormald 2001). Conventional filtering surgery has had poor success in treating NVG.
Description of the intervention
Currently, anti-VEGF agents are being used for various conditions in which hypoxia-induced VEGF release and subsequent neovascularization lead to ocular damage. Initially used in ophthalmology for the treatment of choroidal neovascularization in age-related macular degeneration (ARMD), the application of anti-VEGF agents has expanded rapidly to include treatment for other conditions such as NVG, diabetic macular edema and retinopathy of prematurity. Bevacizumab (Avastin™), ranibizumab (Lucentis™), and pegaptanib sodium (Macugen™) are some of the anti-VEGF agents most frequently used in the eye (Andreoli 2007). Multiple clinical trials have shown that intravitreal injections of anti-VEGF agents not only prevent loss of vision, but also may improve vision in patients with ARMD - ANCHOR (Brown 2006), MARINA (Chang 2007), PrONTO (Lalwani 2009), SAILOR (Boyer 2009), SUSTAIN (Meyer 2008), VISION (VISION 2006). In most of these studies, three initial induction injections at monthly intervals are followed by injections administered on an ’as needed’ basis (i.e., pro re nata (PRN)) during follow-up of the patients. The mean number of injections administered in the first year was similar in various studies: 5.6 injections in PrONTO (Lalwani 2009) and SUSTAIN (Meyer 2008) and 4.9 injections in SAILOR (Boyer 2009). Fewer number of injections were reported in the second year (PrONTO) (Lalwani 2009).
How the intervention might work
In treating NVG, it is critical to address the underlying pathology: angiogenic factors released by the ischemic retina. The issue of retinal ischemia can be addressed by PRP, which ablates the ischemic retina and reduces further production of angiogenic agents. However, in many patients, the view of the fundus is poor due to corneal edema or vitreous hemorrhage and therefore precludes PRP. Hence, interventions aimed at blocking angiogenic factors directly could help reduce the formation of new vessels and possibly reverse the neovascularization. Reduction in levels of VEGF in the aqueous following intraocular injection of bevacizumab has been demonstrated (Grover 2009).
In eyes in which PRP can be done, variable times for regression of new vessels have been reported and the newly formed vessels may not regress until four to six weeks after treatment. In one study, Doft and Blankenship reported regression of new vessels in 20% of patients at three days, 50% at two weeks, 72% at three weeks and 62% at six months (Doft 1984). Rogell reported substantial regression in 38% of patients at one month which improved 88% after retreatment (Rogell 1983). Blankenship in another study reported regression in 97% of patients at one month (Blankenship 1988). Comparision of studies is difficult due to variation in the laser treatments, variation in the response to laser between type 1 and 2 diabetics as well as the variation in the definition of substantial regression in different studies.
Anti-VEGF agents, on the other hand, have been shown to cause regression of new vessels in the anterior chamber angle within a few days, along with a drop in IOP (Avery 2006; Iliev 2006). Intravitreal (Iliev 2006; Yazdani 2007), and less commonly intracameral (Grover 2009) anti-VEGF agents have been used in the management of NVG to control angiogenesis in the angle and iris. The effects of anti-VEGF agents for treating NVG, however, are temporary, generally lasting four to six weeks (Wakabayashi 2008). Thus many studies have combined the use of anti-VEGF agents with traditional treatments such as PRP (Ehlers 2008) with or without other surgery (Wakabayashi 2008).
Why it is important to do this review
Various reports of the excellent response to anti-VEGF agents in NVG have been published (Ehlers 2008; Iliev 2006; Wakabayashi 2008). In most cases, anti-VEGF treatment has been supplemented with PRP and, in some cases, treatments such as aqueous drainage devices, Nd-Yag cyclophotocoagulation, vitrectomy with pars plana implantation of glaucoma drainage devices and cyclocryotherapy. Anti-VEGF agents alone may not be sufficient to treat NVG related to conditions with a progressive natural history, such as PDR. However, the combination of anti-VEGF treatments with conventional treatments have the potential to be more effective than conventional treatments alone.
PRP may not be effective in controlling NVG associated with CRVO (Hayreh 1990). On the basis of studies showing that ischemic CRVO tends eventually to subside to a state of quiescence (Hayreh 2003), it has been suggested that anti-VEGF agents alone can treat NVG secondary to CRVO effectively (Gandhi 2008). In two patients with CRVO who had persisting neovascularization and high IOP in spite of PRP, Yazdani et al reported regression of new vessels and control of IOP following intravitreal bevacizumab (Yazdani 2007). Maintenance of IOP control was reported for as long as six months following a second dose of intravitreal bevacizumab in both these patients, one at eight weeks and the other at six weeks. So the question arises: Are intravitreal anti-VEGF agents alone sufficient in the management of NVG due to CRVO? The Rubeosis Anti-VEGF (RAVE) trial is an ongoing trial investigating the role of intravitreal anti-VEGF agents alone in the management of NVG subsequent to CRVO (NCT00406471).
A systematic review of the available literature is necessary to evaluate the effects of anti-VEGF to inform evidence-based practice.
OBJECTIVES
The objective of this review was to compare the beneficial and adverse effects of intraocular anti-VEGF agents to no anti-VEGF treatment as an adjunct to existing modalities for the treatment of NVG. In the subgroup of participants with NVG due to CRVO, we also aimed to compare the effects of intraocular anti-VEGF alone to no anti-VEGF treatment.
METHODS
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) and quasi-RCTs.
Types of participants
We included studies of people with NVG. We included all age groups and ocular comorbidities.
Types of interventions
Intervention group
People with NVG who received intraocular anti-VEGF agents alone or along with any (one or more than one) type of conventional therapy which includes laser PRP, trabeculectomy, aqueous drainage devices, cyclophotocoagulation, cryotherapy. In the subgroup of participants with NVG due to CRVO, the intervention group could be those people who received intraocular anti-VEGF injection alone without additional conventional therapy.
Control group
People who underwent the same conventional therapy as the intervention group but without intraocular anti-VEGF agents. In the subgroup of participants with NVG due to CRVO, the control group could be those people who received placebo injections or no treatment without additional conventional therapy.
We did not include dosing studies in which one dose of anti-VEGF agent was compared to another dose unless the study also had a control arm.
Types of outcome measures
Primary outcomes
The primary outcome of this review was the proportion of participants with control of IOP at six weeks after treatment. Control of IOP was defined as IOP ≤ 21 mmHg with or without ocular hypotensive medications.
Secondary outcomes
Intraocular pressure
Control of IOP at one year: success was defined as IOP ≤ 21 mmHg with or without ocular hypotensive medications or other treatment.
Visual acuity
Proportion of participants with improvement in visual acuity of 2 ETDRS lines or 0.2 logMAR units at six weeks.
Proportion of participants with improvement in visual acuity of 2 ETDRS lines or 0.2 logMAR units at one year.
Regression of new vessels
Proportion of participants with complete regression of iris new vessels at six weeks.
Proportion of participants with complete regression of iris new vessels at one year.
Relief of symptoms
Proportion of participants with relief of pain and resolution of redness at six weeks.
Proportion of participants with relief of pain and resolution of redness at one year.
Adverse events
Infection: proportion of participants with intraocular infection or inflammation (endophthalmitis) within six weeks of the intervention.
Low IOP (hypotony): proportion of participants with IOP ≤ 6 mmHg at six weeks and one year.
Vitreous hemorrhage: proportion of participants with development of vitreous hemorrhage at six weeks and one year.
Tractional retinal detachment: proportion of participants who experienced tractional retinal detachment at six weeks and one year.
No light perception: proportion of participants with no light perception at six weeks and one year.
Other serious adverse events including systemic thrombosis, stroke and coronary thrombosis.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) 2012, Issue 12, part of The Cochrane Library. www.thecochranelibrary.com (accessed 11 January 2013), Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE, (January 1950 to January 2013), EMBASE (January 1980 to January 2013), Latin American and Caribbean Literature on Health Sciences (LILACS) (January 1982 to January 2013), the metaRegister of Controlled Trials (mRCT) (www.controlled-trials.com), ClinicalTrials.gov (www.clinicaltrials.gov/) and the WHO International Clinical Trials Registry Platform (ICTRP) ( www.who.int/ictrp/search/en). We did not use any date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 11 January 2013.
See: Appendices for details of search strategies for CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), LILACS (Appendix 4), mRCT (Appendix 5) ClinicalTrials.gov (Appendix 6) and the ICTRP (Appendix 7).
Searching other resources
We handsearched the reference lists of potentially relevant studies to identify other possible trials. We obtained information about ongoing studies by contacting the relevant trial investigators.
Data collection and analysis
Selection of studies
Two review authors independently screened the titles and abstracts of all the reports of studies identified by the electronic searches and handsearching. Each review author classified the studies as follows: (1) definitely include, (2) possibly include, and (3) definitely exclude. Each author obtained and independently assessed the full text of each study report classified by either review author as (1) or (2) and reclassified as: (a) include, (b) awaiting classification, or (c) exclude. For reports from studies classified as (b), we requested additional information from study investigators for clarification. The two review authors compared their individual classifications and discussed differences in interpretation. When consensus was not reached after discussion, a third review author reclassified the studies. We documented all studies classified as (c) exclude. We retrieved and reviewed all pertinent references from each potentially relevant study in order to provide the most complete published information possible about study design, methods and findings.
As no studies were included in this review, we completed no data extraction, risk of bias assessment, or data analysis. If, in the future, studies are included in updates to this review, we will apply the following methods for data collection and analysis.
Data extraction and management
Two authors will independently extract data from studies included in the review using data extraction forms developed by the Cochrane Eyes and Vision Group. We will resolve any discrepancies through discussion and by consulting a third review author when necessary. One author will enter data into Review Manager software (Review Manager 2012) and a second author will verify the entries.
Categories of information to be extracted for each study include methods (for example, study design, number of participants and setting), intervention details, outcomes (definitions and time points) and results for each outcome (sample size, missing data, summary data for each intervention). We will contact study authors whenever additional information or clarification is needed.
Assessment of risk of bias in included studies
We will assess the risk of bias as recommended in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). Two review authors will assess the risk of bias independently. This assessment requires a description and a judgement on domains about selection bias, performance bias, detection bias, attrition bias, and reporting bias. The judgement for each domain will be given as low risk of bias; high risk of bias; or unclear risk of bias, indicating either lack of information or uncertainty over the potential for bias. Specific criteria for assessing risk of bias will focus on adequate sequence generation, allocation concealment, masking (blinding) of study participants, personnel and outcome assessors, adequate handling of incomplete outcome data, absence of selective outcome reporting, and absence of other potential sources of bias.
If the information available in the published trial reports is inadequate to assess risk of bias, we will contact the trial authors for clarification. If they do not respond within two months, we will classify the trial on the basis of the available information.
Measures of treatment effect
Data analysis will follow guidelines set forth in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011). We will present dichotomous data as risk ratios with 95% confidence intervals.
Dichotomous outcome measures
Primary outcome
Proportion of participants with IOP ≤ 21 mmHg with or without ocular hypotensive medications at six weeks.
Secondary outcomes
We will include both short- and long-term time periods for the following secondary outcomes:
Control of IOP at one year or the longest follow up available: proportion of participants with IOP ≤ 21 mmHg (with or without ocular hypotensive medications or other treatment).
Visual acuity: improvement in vision of 2 Early Treatment Diabetic Retinopathy Study (ETDRS) lines (or 0.2 logMAR unit) at six weeks, one year or the longest follow up available. In participants with visual acuity restricted to perception of light or hand movements close to face, improvement of vision to 6/60 will be considered as improvement of vision of 1 ETDRS line (0.1 logMAR unit). We will analyze further improvement in vision according to ETDRS line acuity or corresponding logMAR units.
Regression of new vessels: proportion of participants with complete regression of iris new vessels at six weeks and one year.
Relief of symptoms(pain and redness): yes or no at six weeks and one year.
- Adverse events:
- ○ Endophthalmitis: yes or no at six weeks.
- ○ Ocular hypotony: IOP ≤ 6 mmHg at six weeks, one year or the longest follow up available.
- ○ Vitreous hemorrhage: yes or no at six weeks and one year.
- ○ Tractional retinal detachment: yes or no at six weeks and one year.
- ○ No light perception: yes or no at six weeks and one year.
Unit of analysis issues
The unit of analysis will be the affected eye of an individual participant. We will document studies that included participants with bilateral NVG and use data based on the individual when possible (e.g., average of both eyes or one eye selected per patient). When data are not available based on the individual or appropriate were not used to account for paired data due to the correlation between eyes, we will extract the data as reported and perform sensitivity analysis if the data are included in meta-analysis.
Dealing with missing data
We will consult the guidelines in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b) to inform the analysis of studies with missing data. Where data are missing due to loss of follow up or a mismatch between reported time endpoints and our endpoints of interest, we will conduct a primary analysis based on the data as reported. Where essential data needed for statistical analysis are incomplete or missing, we will contact the principal investigators for details. Whenever possible, outcome data will be derived from the study reports and we will describe any assumptions made when extracting data. When possible, we will conduct sensitivity analyses to investigate the influence of studies with missing data.
Assessment of heterogeneity
We will assess heterogeneity by examining study characteristics and forest plots of the results. We will use the I2 value to assess the impact of statistical heterogeneity, interpreting an I2 value of 50% or more as significant. In addition we will examine the funnel plot for evidence of other sources of heterogeneity if at least 10 studies are found.
Assessment of reporting biases
We will examine funnel plots from each meta-analysis to assess reporting bias when at least 10 studies are included.
Data synthesis
We will analyze data using a random-effects model unless there are fewer than three trials available for analysis, in which case we will use a fixed-effect model. If we find significant heterogeneity, we will report results in tabular form and will not pool data across trials.
Subgroup analysis and investigation of heterogeneity
If sufficient data are available, we will undertake subgroup analyses based on the etiology of NVG, including retinal vein occlusions, PDR, ocular ischemic syndrome or other causes.
Sensitivity analysis
We will perform sensitivity analysis to investigate the influence of studies with quasi-random allocation methods, and those without masking of participants, providers, or outcome assessors on the overall estimates of effect.
RESULTS
Description of studies
Results of the search
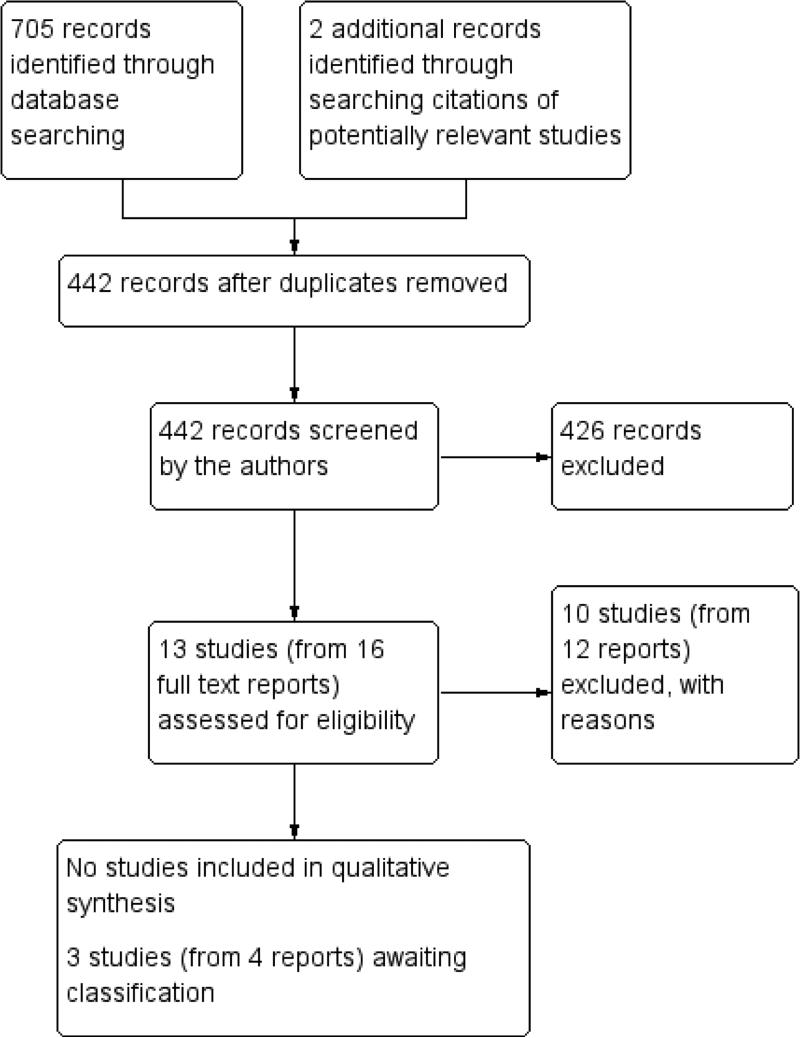
The electronic search as of 11 January 2013 identified 442 unique records (Figure 1). Of these, we excluded 426 records and reviewed the full text of 16 records (representing 13 studies). Ten studies did not meet the inclusion criteria for this review and three studies did not provide sufficient information to include or exclude. No studies were eligible for this review.
Figure 1.
Results from searching for studies for inclusion in the review
We assessed the three studies with insufficient information to include or exclude as awaiting classification until we can receive further information about the study characteristics from the primary investigators (Arcieri 2010; Chakrabarti 2008; NCT01128699). In these studies, it was unclear whether the study methods and populations met the criteria for this review and none of the studies have been published in full. Details of studies awaiting classification appear in the ’Characteristics of studies awaiting classification’ table.
Excluded studies
The 10 studies excluded after full text review were documented in the ’Characteristics of excluded studies’ table. One study, a retrospective case series, evaluated ranibizumab (Caujolle 2012), while eight studies evaluated bevacizumab. The tenth study, an ongoing RCT, is evaluating a single injection of aflibercept followed by observation with injections of aflibercept at eight week intervals (NCT01711879). Of the eight studies using bevacizumab, three were non-comparative case series (Costagliola 2008; Jonas 2010; Miki 2011), one was a historical cohort (Eid 2009), one was an RCT of people with primary or secondary open angle glaucoma (excluded people with NVG) (Sedghipour 2011), and three were RCTs excluded for other reasons (Gupta 2009; Wittstrom 2012; Yazdani 2009).
Gupta 2009 randomized participants with NVG to receive either a 1.25 mg or 2.5 mg single injection of intracameral bevacizumab prior to undergoing trabeculectomy with mitomycin C (MMC). This study was excluded because there was no control group that did not receive an injection and because participants had been treated previously in varying ways (such as PRP, anterior retinal cryopexy, or no treatment). In Wittstrom 2012, 19 participants undergoing PRP were randomized to receive an injection of intravitreal bevacizumab (IVB) or no injection prior to PRP. The study participants were described as having NVG, defined as “iris or anterior chamber angle neovascularization (NVI or NVA) and IOP greater than 22 mmHg,” although 11/19 (58%) had preexisting glaucoma. Thus it was unclear whether all study participants had NVG as defined by this review. The study investigators also stated that all study participants received supplemental NVG therapy, such as medical therapy with IOP-lowering agents or steroids, additional PRP, cyclodestructive procedures, and/or glaucoma surgery, as needed. Yazdani 2009 also was an RCT of IVB for treating NVG, but ultimately was excluded from the review due to the heterogeneity of adjunct treatments received by the study participants. Details of Yazdani 2009 (Table 1) and the additional interventions used during the study (Table 2) were documented.
Table 1.
Characteristics of Yazdani 2009 study
| Methods | Randomized controlled trial Number of participants randomized: 26 Six months follow-up |
| Participants | Country: Iran Baseline characteristics, including age, sex, intraocular pressure (IOP), iris neovascularization, and causes of neovascular glaucoma (NVG) were comparable between groups Follow up: 3 participants were lost to follow-up at six months (1 participant in the treatment group and 2 participants in the control group) |
| Intervention Co-interventions | Treatment group (n = 14): 3 intravitreal injections of 2.5 milligrams (mg) (0.1 milliliters (ml)) bevacizumab at monthly intervals for six months Control group (n = 12) : 3 subconjunctival injections of 0.1 ml normal saline at monthly intervals for six months All participants received conventional treatment for NVG including medications, retinal ablation, glaucoma shunt, and/or cyclodestructive procedures to achieve target IOP of high teens to low 20s The allotment of participants to specific co-interventions was not uniform or randomized. Some participants received multiple co-interventions |
| Outcomes | Primary outcomes: change in IOP and change in the extent of iris neovascularization Secondary outcomes: change in visual acuity and change in glaucoma medication requirement |
Table 2.
Additional conventional procedures* in the Yazdani 2009 study
| Intervention | IVB group | Sham group |
|---|---|---|
| Panretinal photocoagulation | 8 | 9 |
| Glaucoma shunt procedures | 4 | 2 |
| Cyclodestructive procedures | 2 | 1 |
| Cataract surgery | 3 | 4 |
| Deep vitrectomy | 1 | 1 |
35 additional procedures were performed in 23 eyes which included 18 procedures in 12 eyes in the IVB group and 17 procedures in 11 eyes in the sham group
IVB: intraocular bevacizumab
Risk of bias in included studies
There were no studies included in this review.
Effects of interventions
There were no studies included in this review.
DISCUSSION
Summary of main results
Many of the published reports which showed excellent response to intravitreal anti-VEGF agents in NVG were retrospective studies or case series (Costagliola 2008; Ehlers 2008; Gheith 2007; Grisanti 2006; Iliev 2006; Kotecha 2011; Martínez-Carpio 2008; Oshima 2006; Wakabayashi 2008). We excluded three RCTs that investigated anti-VEGF agents in people with NVG. In one RCT, two doses of intracameral bevacizumab prior to undergoing MMC trabeculectomy were compared in participants with NVG, but there was no control group that did not receive intracameral bevacizumab (Gupta 2009). The other two RCTs studied the use of intravitreal bevacizumab (IVB) in NVG; however, adjunctive treatments were assigned at the discretion of investigators, not by random assignment (Wittstrom 2012; Yazdani 2009).
Overall completeness and applicability of evidence
In Yazdani 2009, the main outcome measures were changes in IOP and extent of iris neovascularization over six months of treatment. Fourteen eyes received IVB and 12 eyes received sham injections (subconjunctival normal saline). Each eye (one eye per participant) received three injections at four week intervals; however, the sham group had two participants fewer than the calculated sample size of 14 for each group. All participants received additional conventional procedures as indicated. Overall, 35 additional procedures were performed in 23 eyes which included 18 procedures in 12 eyes in the IVB group and 17 procedures in 11 eyes in the sham group (Table 2). The allocation of the additional procedures was pragmatic and not randomized. Some eyes received more than one additional procedure. One participant in the IVB group and two participants in the sham group did not complete the six month study.
In the control (sham injection) group, IOP increased or remained relatively stable compared with baseline at one, three, and six month follow-up intervals (Table 3). Although IVB-treated eyes showed significant reduction in IOP from baseline at one, three and six months follow-up (Table 3), the difference between IVB-treated eyes and sham-injected eyes for the mean change in IOP was not statistically significantly different at six months (mean difference was -9.80 mmHg (95% CI -21.29 to 1.69)). The extent of neovascularization of the iris (NVI, measured as the mean circumference in degrees evaluated by slitlamp photography) was reduced in IVB-treated eyes at all follow up intervals compared with baseline (Table 3). Sham-injected eyes demonstrated more extensive but statistically insignificant worsening of NVI as compared with baseline (Table 3). At six months, the mean difference of -193.00 degrees (95% CI -300.32 to -85.68) was significantly different between IVB-treated eyes compared with the control group. There was no difference between or within study groups in terms of best-corrected visual acuity during the course of the study.
Table 3.
IOP and NVI at baseline and follow up for Yazdani 2009 study
| IVB group Mean ± SD | P | Sham group Mean ± SD | P | |
|---|---|---|---|---|
| IOP baseline | 33.4 ± 14.5 | 32.3 ± 14.3 | ||
| IOP at 1 month | 21.8 ± 13.7 | 0.007 | 34.9 ± 15.2 | 0.046 |
| IOP at 3 months | 25.1 ± 20.0 | 0.058 | 35.2 ± 10.7 | 0.29 |
| IOP at 6 months | 23.9 ± 18.7 | 0.047 | 32.2 ± 7.3 | 0.92 |
| NVI at baseline | 347 ± 48 | 270 ± 138 | ||
| NVI at 1 month | 206 ± 185 | 0.01 | 277 ± 130 | 0.34 |
| NVI at 3 months | 180 ± 187 | 0.004 | 300 ± 117 | 0.22 |
| NVI at 6 months | 180 ± 180 | 0.004 | 324 ± 114 | 0.34 |
IOP: intraocular pressure (mmHg)
IVB: intravitreal bevacizumab
NVI: neovascularization of iris (degrees)
P: P-value compared with baseline
SD: standard deviation
The six-month IOP findings in Yazdani 2009 raised the question of long-term efficacy of IVB treatment in preventing a painful blind eye, which could lead to enucleation. The study authors also clearly mentioned the presence of a few non-responders being responsible for the large standard deviation in IOP. The authors postulated that the subgroup of eyes unresponsive to IVB could be those with severe ischemia and questioned whether some other mechanism for resistance to treatment exists. Due to the small sample size of the study, subgroup analyses would not be meaningful.
Wittstrom 2012 was an RCT comparing a 1.25 mg intravitreal injection of bevacizumab prior to PRP (10 participants) verses PRP alone (nine participants) in patients with NVG secondary to ischemic CRVO. The primary outcome of the trial was to evaluate change in the total retinal function by full-field electroretinography (ERG) in the two groups six months after the treatment. Visual acuity, IOP control, and regression of new vessels were secondary outcomes. The study investigators found no difference in mean IOP between the two groups at one week, two months, or six months follow-up. Six participants received additional treatments (such as retinal cyclocryotherapy, cyclophotocoagulation, and trabeculectomy) during the study; four in the bevacizumab plus PRP group and two in the PRP alone group. The allocation of the additional interventions was not randomized making it difficult to compare the effects of bevacizumab on IOP. Also the study investigators reported that 11 of the 19 participants had pre-existing glaucoma, which may confound the study results if not all study participants had NVG prior to CRVO. Further, three participants were lost to follow up in the bevacizumab plus PRP group reducing the sample size to seven participants in this group (no participants were lost to follow up in the PRP alone group). In another excluded RCT (Gupta 2009), participants with NVG were randomized to different doses of a single injection of intracameral bevacizumab prior to undergoing trabeculectomy with MMC. Nine participants received a 1.25 mg injection and 10 received a 2.5 mg injection. There was no control group in which no anti-VEGF treatment was given. The participants in the two groups previously had received either some form of conventional treatment (such as PRP or anterior retinal cryopexy) or no conventional treatment.
Although there were statistically significant reductions in IOP in both groups compared to baseline IOP, there was no statistically significant difference in the reduction of IOP between the two groups at six months. There were recurrences of NVI at three months in three eyes, two in the lower dose group and one in the higher dose group.
Gupta 2009 also compared the six month results of MMC augmented trabeculectomy without bevacizumab in 16 control eyes (these controls were historical and not randomized) versus the eyes receiving bevacizumab (19 eyes from the RCT). No statistically significant difference in the reduction of IOP (P = 0.5) was observed. However, failure of trabeculectomy (defined as persistently elevated IOP > 21 mmHg following surgery despite maximal topical antiglaucoma therapy) was lower in the eyes receiving bevacizumab (5%) compared to the historical controls (31%) (P = 0.04).
Quality of the evidence
Although the design and conduct of the Yazdani 2009 study suggested remarkable efforts by the investigators to reinforce quality, the small sample size and the use of one or more additional co-interventions made it difficult to analyze objectively the superiority of IVB over sham procedure. The allotment of these co-interventions to participants was pragmatic and not based on study-specific protocols. This rendered the study groups non-comparable. Also, five participants with normal baseline IOPs were included in the study: three participants in the treatment group (baseline IOPs of 8, 10 and 17 mmHg) and two participants in the control group (baseline IOPs of 8 and 14 mmHg). Though these participants were eligible candidates to study iris NV, these participants were not considered to have NVG since their IOPs were not greater than 21 mmHg. Inclusion of these participants reduced the sample size of eligible participants to study the effect of IVB on NVG, though the two groups were comparable with respect to their baseline IOPs.
Interestingly, the above study showed absolute failure of conventional treatment methods, in contrast with the existing literature that has shown success with conventional treatment such as PRP (Ohnishi 1994), cyclodestructive procedures (Bloom 1997; Feibel 1972), as well as glaucoma shunt procedures (Assaad 1999) during similar or even prolonged follow-up periods.
Potential biases in the review process
We attempted to minimize selection bias in this review by developing a comprehensive search of studies from multiple sources, including journal articles, conference abstracts, and registered clinical trials; however, it is impossible to guarantee that we did not miss any relevant trials. As the purpose of the search was to identify relevant clinical trials related to anti-VEGF therapy for NVG, the original search was not designed to capture all possible types of studies, such as cohort studies, case-control studies or case series. Based on peer review comments, we amended the search to remove the study type filter and reran the search to include all types of studies, which may provide important information on harms. The review team was comprised of content experts and methodologists, of which two review authors completed tasks, such as screening references for inclusion and assessing studies, in duplicate in order to minimize errors and bias.
Agreements and disagreements with other studies or reviews
In a retrospective case-control study of 23 participants, Ehlers 2008 observed rapid decreases in IOP and regression of neovascularization in the IVB/PRP group compared with the PRP alone group at the time of initial treatment. However, there was no statistically significant difference in the IOP reduction between groups at final follow-up (range 12 to 372 days). Further, there were no statistically significant differences in the use of additional IOP lowering medications or the need for additional surgical procedures between the two groups at final follow-up.
Wakabayashi 2008 studied 41 eyes which had undergone IVB as an adjunct to PRP in participants with anterior segment neovascularization with or without raised IOP. Though repeat injections of IVB reduced the need for surgical intervention (7/17 eyes) in participants with open angles, in a subgroup of 15 participants with NVG and closed angles, 14 required glaucoma filtering procedures.
In a prospective case series of 50 participants with NVG in which PRP was ineffective or not advisable, IVB was administered alongside traditional anti-glaucoma treatments (topical medication, drainage device, or cyclodiode laser as determined by clinical need) (Kotecha 2011). IVB injections were given at baseline for all participants and as needed during the six-month study. As early as one week after IVB injections, participants in the study reported reduction in pain scores and showed regression of vessels. The study investigators reported that “no serious adverse events attributable to IVB” occurred. The study investigators concluded that IVB was beneficial for treating NVG, but did not find evidence to support the use of IVB for lowering IOP in participants with angle-closure. In a retrospective chart review of participants of NVG with minimum six months follow-up, Vasudev 2009 compared those who had undergone PRP versus those who had received a single injection of IVB followed by PRP. They found no statistically significant difference in the IOP between the two groups at one, four or 12 weeks. However, they found significantly lower mean IOP in the IVB group which trended towards significance at one year follow-up. They also documented long-term preservation of open angle in the IVB group. The decision to use IVB was decided by the physician and patient's preference.
Currently, an aqueous drainage device is the preferred surgical modality of treatment for NVG due to increased chances of failure of conventional trabeculectomy (Katz 1995; Tsai 1995). Anti-VEGF agents may have a role to play as adjuvant therapy to more definitive treatment strategies for NVG. The use of IVB and other anti-VEGF agents could decrease IOP and inflammation preoperatively, leading to better success rates and fewer complications with glaucoma surgical procedures and could possibly improve the success of primary trabeculectomy (Kitnarong 2008). The use of these medications also could decrease considerably the use of cyclodestructive procedures in the management of this disease. However, we have found little or no evidence from RCTs to support this hypothesis. The NCT00406471, a two-year RCT investigating intravitreal ranibizumab for the prevention of NVG in participants with CRVO, was completed recently and the results of which are awaited.
AUTHORS’ CONCLUSIONS
Implications for practice
We did not find any evidence from which to draw reliable conclusions comparing the effects of intraocular anti-VEGF agents with no anti-VEGF injection alone or as an adjunct to existing modalities for the treatment of NVG. Retrospective studies and case series have reported short-term reductions in neovascularization, inflammation, and IOP among people with NVG. Since information regarding the effectiveness of anti-VEGF agents are not available from high-quality RCTs and long-term studies, clinical practice decisions will need to based on the physician's experience and judgment and the patient's wishes.
Implications for research
There was no evidence from controlled clinical trials comparing the effects of intraocular anti-VEGF agents with no anti-VEGF injection alone or as an adjunct to existing modalities for the treatment of NVG. Although the ideal method to evaluate the effectiveness of anti-VEGFs would be to compare directly anti-VEGF treatment with no anti-VEGF treatment in an RCT in which no other co-interventions were given, the established benefit of some surgical procedures (such as PRP) in the management of NVG and the harmful effects of raised IOP that may result from surgeries not being done would make it unethical to withhold conventional procedures. Thus a well thought out RCT comparing anti-VEGF agents with no anti-VEGF agents taking into account the need for co-interventions, such as PRP, glaucoma shunt procedures, cyclodestructive procedures, cataract surgery, and deep vitrectomy, could be of use to investigate the additional beneficial effect of anti-VEGF agents in treating NVG. Since decisions for when and which co-interventions should be used are based on clinical criteria, they would not be appropriate for randomization. However, the design of a study on this topic should aim to balance groups by stratification of co-intervention at time of randomization or by enrolling a sufficient number of participants to conduct subgroup analysis by co-interventions. Sample size calculations reported by Yazdani 2009 suggest enrolling 14 participants per study group to detect an 8 mm Hg change with 90% power. Alternatively, the inclusion criteria for a trial could limit participants to those who receive the same co-intervention.
CHARACTERISTICS OF STUDIES
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Caujolle 2012 | Retrospective, non-randomized study of ranibizumab injections with or without cryotherapy; 14 participants (14 eyes) previously treated with proton therapy for uveal melanomas with minimum of 4 months follow-up; no control group |
| Costagliola 2008 | Prospective pilot study of bevacizumab injections; 23 participants (26 eyes) received injections and were followed for 12 months; no control group |
| Eid 2009 | Historical cohort study of bevacizumab injections and aqueous shunting surgery; 20 participants with NVG received injections followed by surgery and were compared to a historical group of 10 participants treated with PRP and surgery without bevacizumab |
| Gupta 2009 | RCT of intracameral bevacizumab prior to undergoing MMC trabeculectomy; participants received either 1.25 mg injections (n = 9) or 2.5 mg injections (n = 10) and were followed for six months; there was no control group in which no intracameral bevacizumab was given; participants may have been treated previously with some form of conventional treatment (PRP, anterior retinal cryopexy) or no conventional treatment Historical cohort of non-randomized participants who did not receive intracameral bevacizumab injections; outcomes from 16 participants/eyes who had MMC trabeculectomy in years prior to the trial were compared with the outcomes from the trial participants |
| Jonas 2010 | Retrospective chart review of IVB; 14 participants with iris neovascularization and secondary angle-closure glaucoma treated with between one and three intravitreal injections of bevacizumab and followed for at least 4 months; no control group |
| Miki 2011 | Prospective pilot study of bevacizumab injections as an adjunct to trabeculectomy; 15 participants (15 eyes) with previous vitrectomy were treated with trabeculectomy with MMC plus IVB and were followed for 12 months; no control group |
| NCT01711879 | Ongoing RCT of aflibercept in participants with NVG; treatment group 1 consisted of one intravitreal injection of 2 mg (0.05 ml) aflibercept at baseline followed by laser treatment with observation and treatment group 2 consisted of intravitreal injections of 2 mg (0.05 ml) aflibercept at baseline, 4 weeks, and 8 weeks, then every 8 weeks (all study participants received treatment with anti-VEGF therapy) |
| Sedghipour 2011 | RCT of IVB augmentation after trabeculectomy versus control group receiving a placebo injection after trabeculectomy; 37 participants with primary or secondary open angle glaucoma (excluded participants with neovascular glaucoma) |
| Wittstrom 2012 | RCT of IVB; participants received either IVB prior to PRP (n = 10) or no IVB prior to PRP (n = 9) and were followed for six months; 11 of the 19 participants had pre-existing glaucoma (it was not clear whether these 11 participants had glaucoma before central retinal vein occlusion, in which case this RCTdoes not address the issue of pure NVG and pre-existing glaucoma can be a major confounder, or only 11 of the 19 participants had NVG with elevated IOPs at baseline); participants additionally received co-interventions (such as IOP-lowering medications, additional PRP, retinal cyclocryotherapy, transscleral diode laser cyclophotocoagulation, and trabeculectomy) determined by individual clinical assessments; the allocation of co-interventions was pragmatic and randomization was not stratified by co-interventions; subgroup analysis according to co-interventions would not be useful since the number of participants in each co-intervention group was small and some participants received multiple co-interventions |
| Yazdani 2009 | RCT of IVB; participants received either IVB (n = 14) or saline injections (n = 12) and were followed for six months; participants additionally received co-interventions (such as PRP, filtering procedures, cyclodestructive procedures) determined by individual clinical assessments; the allocation of co-interventions was pragmatic and randomization was not stratified by co-interventions; subgroup analysis according to co-interventions would not be useful since the number of participants in each co-intervention group was small |
anti-VEGF: anti-vascular endothelial growth factor
IOP: intraocular pressure
IVB: intravitreal bevacizumab
mg: milligram
ml: milliliter
MMC: mitomycin C
NVG: neovascular glaucoma
PRP: panretinal photocoagulation
RCT: randomized controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Arcieri 2010 | |
|---|---|
| Methods | RCT Number randomized: 29 participants 18 months follow-up planned; mean of 8 months |
| Participants | Country: Brazil Inclusion criteria: age between 18 and 90 years; NVG with history of PRP; and requiring glaucoma drainage device Exclusion criteria: learning difficulties, mental illness, or dementia; and unconscious or severely ill |
| Interventions | Treatment group: implantation of Ahmed valve with intravitreal injections of 1.25 mg (0.05 ml) bevacizumab at end of surgery, and 4 and 8 weeks postoperatively Control group: implantation of Ahmed valve with pars plana injection of 0.05 ml saline at end of surgery |
| Outcomes | Primary outcome specified as: IOP control at 6 months Secondary outcome specified as: safety of intravitreal bevacizumab at 6 months Outcomes reported in conference abstract: mean change in IOP, visual acuity, mean number of anti-glaucoma medications, extension of goniosynechiae, reduction of new vessels in the anterior chamber angle, regression of rubeosis iridis |
| Notes | This study was presented at the 2010 Association for Research in Vision and Ophthalmology (ARVO) conference. Details of study methods and participants were not provided in the conference abstract. The clinical trial registration for this study did not yield additional information to assist with determining eligibility |
DATA AND ANALYSES
This review has no analyses.
DIFFERENCES BETWEEN PROTOCOL AND REVIEW.
Based on peer review comments to the manuscript, we added the following adverse events to consider if studies are added to this review in the future:
Vitreous hemorrhage: proportion of participants with development of vitreous hemorrhage at six weeks and one year
Tractional retinal detachment: proportion of participants who experienced tractional retinal detachment at six weeks and one year
No light perception: proportion of participants with no light perception at six weeks and one year
A further peer review comment suggested that if data from a case-control study were being discussed in the review then the searches should be re-run minus the RCT filter to identify other reports of anti-VEGF agents being used for the treatment of NVG.
PLAIN LANGUAGE SUMMARY.
Anti-vascular endothelial growth factor for neovascular glaucoma
Neovascular glaucoma (NVG) is a painful and potentially blinding secondary glaucoma. It is associated with a reduction of the blood supply to the retina due to blood vessel blockage. To compensate for the lack of blood flow, the retina releases vascular endothelial growth factors (VEGFs) to stimulate the formation of new abnormal blood vessels. Thus, treatment of the underlying cause of NVG is as important as reducing intraocular pressure (IOP) and inflammation associated with NVG.
The conventional treatment for NVG is panretinal photocoagulation (PRP), wherein a laser is used to destroy areas of the retina in order to minimize the blood supply needed by the retina, and thus reduce growth of new abnormal blood vessels. However, poor view of the retina in the back of the eye may prevent its use. Anti-VEGF agents, which are injected into the eye, may prevent the growth of abnormal blood vessels. Another potential advantage of anti-VEGF agents over PRP is the reduced time needed to recover from the procedure because of ocular inflammation and/or blurred vision associated with PRP. The effects of anti-VEGF agents for treating NVG, however, may be temporary, generally lasting four to six weeks.
Although we identified many published reports on anti-VEGF agents in NVG, none were eligible for inclusion. More research is needed to investigate the effect of these agents compared with or in addition to conventional surgical or medical treatment in lowering IOP in NVG.
ACKNOWLEDGEMENTS
This review was produced by the work done with the assistance of protocol development and review completion workshops conducted by the South Asian Cochrane Network, based at the Prof. B.V. Moses and ICMR Advanced Center for Research Training in Evidence Informed Healthcare, Christian Medical College, Vellore, India. We would like to acknowledge Dr. Prathap Tharyan, the director of the Center for his never ending encouragement and help. The South Asian Cochrane Network is funded by the ICMR.
We thank Dr. Soumik Kalita for guidance through the process of training and working with The Cochrane Collaboration's software (Review Manager 2012). We thank Iris Gordon, Trials Search Coordinator for the Cochrane Eyes and Vision Group (CEVG), for designing and undertaking the electronic search strategies. We thank Dr. Barbara Hawkins and other peer reviewers for comments to the protocol and full review.
Richard Wormald (Co-ordinating Editor for CEVG) acknowledges financial support for his CEVG research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology. The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS or the Department of Health.
SOURCES OF SUPPORT
Internal sources
• Christian Medical College, Vellore, India.
Salaries of the authors AS, AB, LA, PS
External sources
• Grant 1 U01 EY020522-01, National Eye Institute, National Institutes of Health, USA.
KL is supported by the Cochrane Eyes and Vision Group US Project, which is funded by the National Eye Institute
APPENDICES
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Glaucoma, Neovascular] explode all trees
#2 (glaucoma* or angle* or iris or anterior) near/4 (neovascular*)
#3 (haemorrhagic or hemorrhagic or thrombotic or congestive or rubeotic or secondary) near/4 (glaucoma*)
#4 NVG or NVI
#5 #1 or #2 or #3 or #4
#6 MeSH descriptor: [Angiogenesis Inhibitors] explode all trees
#7 MeSH descriptor: [Angiogenesis Inducing Agents] explode all trees
#8 MeSH descriptor: [Endothelial Growth Factors] explode all trees
#9 MeSH descriptor: [Vascular Endothelial Growth Factors] explode all trees
#10 macugen* or pegaptanib* or lucentis* or rhufab* or ranibizumab* or bevacizumab* or avastin* or aflibercept*
#11 anti near/2 VEGF*
#12 endothelial near/2 growth near/2 factor*
#13 #6 or #7 or #8 or #9 or #10 or #11 or #12
#14 #5 and #13
Appendix 2. MEDLINE (OvidSP) search strategy
1. neovascular glaucoma/
2. ((glaucoma$ or angle$ or iris or anterior) adj4 neovascular$).tw.
3. ((haemorrhagic or hemorrhagic or thrombotic or congestive or rubeotic or secondary) adj4 glaucoma$).tw.
4. (NVG or NVI).tw.
5. or/1-4
6. exp angiogenesis inhibitors/
7. exp angiogenesis inducing agents/
8. exp endothelial growth factors/
9. exp vascular endothelial growth factors/
10. (macugen$ or pegaptanib$ or lucentis$ or rhufab$ or ranibizumab$ or bevacizumab$ or avastin$ or aflibercept$).tw.
11. (anti adj2 VEGF$).tw.
12. (endothelial adj2 growth adj2 factor$).tw.
13. or/6-12
14. 5 and 13
Appendix 3. EMBASE (OvidSP) search strategy
1. neovascular glaucoma/
2. ((glaucoma$ or angle$ or iris or anterior) adj4 neovascular$).tw.
3. ((haemorrhagic or hemorrhagic or thrombotic or congestive or rubeotic or secondary) adj4 glaucoma$).tw.
4. (NVG or NVI).tw.
5. or/1-4
6. exp angiogenesis/
7. exp angiogenesis inhibitors/
8. exp angiogenic factor/
9. exp endothelial cell growth factor/
10. exp vasculotropin/
11. (macugen$ or pegaptanib$ or lucentis$ or rhufab$ or ranibizumab$ or bevacizumab$ or avastin$ or aflibercept$).tw.
12. (anti adj2 VEGF$).tw.
13. (endothelial adj2 growth adj2 factor$).tw.
14. or/6-13
15. 5 and 14
Appendix 4. LILACS search strategy
glaucoma$ and angiogenesis or endothelial growth factor or macugen$ or pegaptanib$ or lucentis$ or rhufab$ or ranibizumab$ or bevacizumab$ or avastin
Appendix 5. metaRegister of Controlled Trials search strategy
neovascular glaucoma
Appendix 6. ClinicalTrials.gov search strategy
(Neovascular Glaucoma) AND (Macugen OR Pegaptanib OR Lucentis OR Rhufab OR Ranibizumab OR Bevacizumab OR Avastin OR Aflibercept)
Appendix 7. ICTRP search strategy
(Neovascular Glaucoma) = Condition AND (Macugen OR Pegaptanib OR Lucentis OR Rhufab OR Ranibizumab OR Bevacizumab OR Avastin OR Aflibercept) = Intervention
Footnotes
Citation: Simha A, Braganza A, Abraham L, Samuel P, Lindsley K. Anti-vascular endothelial growth factor for neovascular glaucoma. Cochrane Database of Systematic Reviews 2013, Issue 10. Art. No.: CD007920. DOI: 10.1002/14651858.CD007920.pub2.
CONTRIBUTIONS OF AUTHORS
Conceiving the review: AS, AB
Designing the review: AS, AB, LA
Co-ordinating the review: AS
Data collection for the review
- Designing electronic search strategies: Cochrane Eyes and Vision Group editorial base
- Undertaking manual searches: AS, LA
- Screening search results: AS, LA
- Organizing retrieval of papers: AS, LA, KL
- Screening retrieved papers against inclusion criteria: AS, LA
- Appraising quality of papers: AS, LA, AB, KL
- Extracting data from papers: AS, LA
- Writing to authors of papers for additional information: AS, LA
- Providing additional data about papers: AS, AB, LA
- Obtaining and screening data on unpublished studies: AS, AB, LA
Data management for the review
- Entering data into RevMan: AS, LA
- Analysis of data: AS, LA, AB, PS
Interpretation of data
- Providing a methodological perspective: AB, LA, PS, KL
- Providing a clinical perspective: AS, LA, AB
- Providing a policy perspective: AB
Writing the review: AS, LA, KL
Providing general advice on the review: AB
DECLARATIONS OF INTEREST
None known.
REFERENCES
- Caujolle JP, Maschi C, Freton A, Pages G, Gastaud P. Treatment of neovascular glaucoma after proton therapy for uveal melanomas with ranibizumab injection: preliminary results. Ophthalmic Research. 2012;47(2):57–60. doi: 10.1159/000328633. [DOI] [PubMed] [Google Scholar]
- Costagliola C, Cipollone U, Rinaldi M, della Corte M, Semeraro F, Romano MR. Intravitreal bevacizumab (Avastin) injection for neovascular glaucoma: a survey on 23 cases throughout 12-month follow-up. British Journal of Clinical Pharmacology. 2008;66(5):667–73. doi: 10.1111/j.1365-2125.2008.03278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eid T, Radwan A, el-Manawy W, el-Hawary I. Intravitreal bevacizumab and aqueous shunting surgery for neovascular glaucoma: safety and efficacy. Canadian Journal of Ophthalmology. 2009;44(4):451–6. doi: 10.3129/i09-108. [DOI] [PubMed] [Google Scholar]
- Eid T, Radwan A, el-Menawy W, el-Hawary I. Outcome of intravitreal bevacizumab (Avastin) followed by aqueous shunting surgery for management of intractable neovascular glaucoma. American Academy of Ophthalmology. 2008:219. [Google Scholar]
- Georgalas I, Koutsandrea C, Papaconstantinou D, Petrou P, Ladas I. The effect of different doses of intracameral bevacizumab on surgical outcomes of trabeculectomy for neovascular glaucoma. European Journal of Ophthalmology. 2010;20(1):251. doi: 10.1177/112067211002000144. [DOI] [PubMed] [Google Scholar]
- Gupta V, Jha R, Rao A, Kong G, Sihota R. The effect of different doses of intracameral bevacizumab on surgical outcomes of trabeculectomy for neovascular glaucoma. European Journal of Ophthalmology. 2009;19(3):435–41. doi: 10.1177/112067210901900318. [DOI] [PubMed] [Google Scholar]
- Jonas JB, Golubkina L, Libondi T, Rensch F. Intravitreal bevacizumab for neovascular glaucoma. Acta Opthalmologica. 2010;88(2):e22–3. doi: 10.1111/j.1755-3768.2008.01453.x. [DOI] [PubMed] [Google Scholar]
- Miki A, Oshima Y, Otori Y, Matsushita K, Nishida K. One-year results of intravitreal bevacizumab as an adjunct to trabeculectomy for neovascular glaucoma in eyes with previous vitrectomy. Eye. 2011;25(5):658–9. doi: 10.1038/eye.2011.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01711879 [21 August 2013];Use of intravitreal aflibercept injection for neovascular glaucoma. clinicaltrials.gov/ct2/show/NCT01711879.
- Sedghipour MR, Mostafaei A, Taghavi Y. Low-dose subconjunctival bevacizumab to augment trabeculectomy for glaucoma. Clinical Ophthalmology. 2011;5(1):797–800. doi: 10.2147/OPTH.S17896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittstrom E, Holmberg H, Hvarfner C, Andreasson S. Clinical and electrophysiologic outcome in patients with neovascular glaucoma treated with and without bevacizumab. European Journal of Ophthalmology. 2012;22(4):563–74. doi: 10.5301/ejo.5000089. [DOI] [PubMed] [Google Scholar]
- Yazdani S, Hendi K, Pakravan M, Mahdavi M, Yaseri M. Intravitreal bevacizumab for neovascular glaucoma: a randomized controlled trial. Journal of Glaucoma. 2009;18(8):632–7. doi: 10.1097/IJG.0b013e3181997211. [DOI] [PubMed] [Google Scholar]
- Arcieri ES, Secches DJL, Paula JS, Barella KA, Arcieri RS, Jorge R, et al. Efficacy and safety of intravitreal bevacizumab in eyes with neovascular glaucoma undergoing Ahmed Glaucoma Valve implantation - preliminary report. ARVO. 2010:627/A471. doi: 10.1111/aos.12493. [DOI] [PubMed] [Google Scholar]
- Chakrabarti M, Chakrabarti A, Stephen V, John SR. Efficacy of combining intravitreal bevacizumab monotherapy with panretinal photocoagulation in early stages of neovascular glaucoma. American Academy of Ophthalmology. 2008:182. [Google Scholar]
- NCT01128699 [20 August 2013];Ahmed valve glaucoma implant with adjunctive subconjunctival bevacizumab in refractory glaucoma. clinicaltrials.gov/ct2/show/NCT01128699.
- Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. New England Journal of Medicine. 1994;331(22):1480–7. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- Andreoli CM, Miller JW. Anti-vascular endothelial growth factor therapy for ocular neovascular disease. Current Opinion in Ophthalmology. 2007;18(6):502–8. doi: 10.1097/ICU.0b013e3282f0ca54. [DOI] [PubMed] [Google Scholar]
- Assaad MH, Baerveldt G, Rockwood EJ. Glaucoma drainage devices: pros and cons. Current Opinion in Ophthalmology. 1999;10(2):147–53. doi: 10.1097/00055735-199904000-00012. [DOI] [PubMed] [Google Scholar]
- Avery RL. Regression of retinal and iris neovascularization after intravitreal bevacizumab (Avastin) treatment. Retina. 2006;26(3):352–4. doi: 10.1097/00006982-200603000-00016. [DOI] [PubMed] [Google Scholar]
- Blankenship GW. A clinical comparison of central and peripheral argon laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1988;95(2):170–7. doi: 10.1016/s0161-6420(88)33212-4. [DOI] [PubMed] [Google Scholar]
- Bloom PA, Tsai JC, Sharma K, Miller MH, Rice NS, Hitchings RA, et al. “Cyclodiode”. Trans-scleral diode laser cyclophotocoagulation in the treatment of advanced refractory glaucoma. Ophthalmology. 1997;104(9):1508–19. doi: 10.1016/s0161-6420(97)30109-2. [DOI] [PubMed] [Google Scholar]
- Boyer DS, Heier JS, Brown DM, Francom SF, Ianchulev T, Rubio RG. A Phase IIIb study to evaluate the safety of ranibizumab in subjects with neovascular age-related macular degeneration. Ophthalmology. 2009;116(9):1731–9. doi: 10.1016/j.ophtha.2009.05.024. [DOI] [PubMed] [Google Scholar]
- Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. New England Journal of Medicine. 2006;355(14):1432–44. doi: 10.1056/NEJMoa062655. [DOI] [PubMed] [Google Scholar]
- Chang TS, Bressler NM, Fine JT, Dolan CM, Ward J, Klesert TR, et al. Improved vision-related function after ranibizumab treatment of neovascular age-related macular degeneration: results of a randomized clinical trial. Archives of Ophthalmology. 2007;125(11):1460–9. doi: 10.1001/archopht.125.11.1460. [DOI] [PubMed] [Google Scholar]
- Deeks JJ, Higgins JPT, Altman DG, Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration; 2011. Chapter 9: Analysing data and undertaking meta-analyses. Available from www.cochrane-handbook.org. [Google Scholar]
- Delgado MF, Dickens CJ, Iwach AG, Novack GD, Nychka DS, Wong PC, et al. Long-term results of noncontact neodymium:yttrium-aluminum-garnet cyclophotocoagulation in neovascular glaucoma. Ophthalmology. 2003;110(5):895–9. doi: 10.1016/S0161-6420(03)00103-9. [DOI] [PubMed] [Google Scholar]
- Doft BH, Blankenship G. Retinopathy risk factor regression after laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1984;91(12):1453–7. doi: 10.1016/s0161-6420(84)34123-9. [DOI] [PubMed] [Google Scholar]
- Ehlers JP, Spirn MJ, Lam A, Sivalingam A, Samuel MA, Tasman W. Combination intravitreal bevacizumab/ panretinal photocoagulation versus panretinal photocoagulation alone in the treatment of neovascular glaucoma. Retina. 2008;28(5):696–702. doi: 10.1097/IAE.0b013e3181679c0b. [DOI] [PubMed] [Google Scholar]
- Feibel RM, Bigger JF. Rubeosis iridis and neovascular glaucoma. Evaluation of cyclocryotherapy. American Journal of Ophthalmology. 1972;74(5):862–7. doi: 10.1016/0002-9394(72)91206-8. [DOI] [PubMed] [Google Scholar]
- Gandhi JS. Use of antivascular agents for neovascular glaucoma: benefits beyond pressure?. Clinical and Experimental Ophthalmology. 2008;36(1):102–3. doi: 10.1111/j.1442-9071.2007.01667.x. [DOI] [PubMed] [Google Scholar]
- Gheith ME, Siam GA, de Barros DS, Garg SJ, Moster MR. Role of intravitreal bevacizumab in neovascular glaucoma. Journal of Ocular Pharmacology and Therapeutics. 2007;23(5):487–91. doi: 10.1089/jop.2007.0036. [DOI] [PubMed] [Google Scholar]
- Grisanti S, Biester S, Peters S, Tatar O, Ziemssen F, Bartz-Schmidt KU. Intracameral bevacizumab for iris rubeosis. American Journal of Ophthalmology. 2006;142(1):158–60. doi: 10.1016/j.ajo.2006.02.045. [DOI] [PubMed] [Google Scholar]
- Grover S, Gupta S, Sharma R, Brar VS, Chalam KV. Intracameral bevacizumab effectively reduces aqueous vascular endothelial growth factor concentrations in neovascular glaucoma. British Journal of Ophthalmology. 2009;93(2):273–4. doi: 10.1136/bjo.2008.145714. [DOI] [PubMed] [Google Scholar]
- Hayreh SS, Klugman MR, Podhajsky P, Servais GE, Perkins ES. Argon laser panretinal photocoagulation in ischemic central retinal vein occlusion. A 10-year prospective study. Graefe's Archive for Clinical and Experimental Ophthalmology. 1990;228(4):281–96. doi: 10.1007/BF00920049. [DOI] [PubMed] [Google Scholar]
- Hayreh SS. Management of central retinal vein occlusion. Ophthalmologica. 2003;217(3):167–88. doi: 10.1159/000068980. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Sterne JAC, Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration; 2011. Chapter 8: Assessing risk of bias in included studies. Available from www.cochrane-handbook.org. [Google Scholar]
- Higgins JPT, Deeks JJ, Altman DG, Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration; 2011. Chapter 16: Special topics in statistics. Available from www.cochrane-handbook.org. [Google Scholar]
- Iliev ME, Domig D, Wolf-Schnurrbursch U, Wolf S, Sarra GM. Intravitreal bevacizumab (Avastin) in the treatment of neovascular glaucoma. American Journal of Ophthalmology. 2006;142(6):1054–6. doi: 10.1016/j.ajo.2006.06.066. [DOI] [PubMed] [Google Scholar]
- Katz GJ, Higginbotham EJ, Lichter PR, Skuta GL, Musch DC, Bergstrom TJ, et al. Mitomycin C versus 5-fluorouracil in high-risk glaucoma filtering surgery. Extended follow-up. Ophthalmology. 1995;102(9):1263–9. doi: 10.1016/s0161-6420(95)30875-5. [DOI] [PubMed] [Google Scholar]
- Kitnarong N, Chindasub P, Metheetrairut A. Surgical outcome of intravitreal bevacizumab and filtration surgery in neovascular glaucoma. Advances in Therapy. 2008;25(5):438–43. doi: 10.1007/s12325-008-0047-5. [DOI] [PubMed] [Google Scholar]
- Kiuchi Y, Nakae K, Saito Y, Ito S, Ito N. Pars plana vitrectomy and panretinal photocoagulation combined with trabeculectomy for successful treatment of neovascular glaucoma. Graefe's Archive for Clinical and Experimental Ophthalmology. 2006;244(12):1627–32. doi: 10.1007/s00417-006-0321-7. [DOI] [PubMed] [Google Scholar]
- Kotecha A, Spratt A, Ogunbowale L, dell'Omo R, Kulkarni A, Bunce C, Franks WA. Intravitreal bevacizumab in refractory neovascular glaucoma: a prospective, observational case series. Archives of Ophthalmology. 2011;129(2):145–50. doi: 10.1001/archophthalmol.2010.350. [DOI] [PubMed] [Google Scholar]
- Kovacic Z, Ivanisevic M, Rogosic V, Plavec A, Karelovic D. Cyclocryocoagulation in treatment of neovascular glaucoma [Ciklokriokoagulacija u lijecenju neovaskularnoga glaukoma]. Lijecnicki Vjesnik. 2004;126(9-10):240–2. [PubMed] [Google Scholar]
- Lalwani GA, Rosenfeld PJ, Fung AE, Dubovy SR, Michels S, Feuer W, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. American Journal of Ophthalmology. 2009;148(1):43–58. doi: 10.1016/j.ajo.2009.01.024. [DOI] [PubMed] [Google Scholar]
- Martínez-Carpio PA, Bonafonte-Márquez E, Heredia-García CD, Bonafonte-Royo S. Efficacy and safety of intravitreal injection of bevacizumab in the treatment of neovascular glaucoma: systematic review [Eficacia y seguridad de la inyección intravítrea de bevacizumab en el tratamiento del glaucoma neovascular: revisión sistemática]. Archivos de la Socidad Espanola de Oftalmologia. 2008;83(10):579–88. doi: 10.4321/s0365-66912008001000004. [DOI] [PubMed] [Google Scholar]
- Meyer CF, Eter N, Holz FG. Ranibizumab in patients with subfoveal choroidal neovascularization secondary to age-related macular degeneration. Interim results from the SUSTAIN trial (abstract). Investigative Ophthalmology and Visual Science. 2008 E-abstract 273. [Google Scholar]
- Minckler D, Vedula SS, Li T, Mathew M, Ayyala R, Francis B. Aqueous shunts for glaucoma. Cochrane Database of Systematic Reviews. 2006;(2) doi: 10.1002/14651858.CD004918.pub2. [DOI: 10.1002/ 14651858.CD004918.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00406471 [9 November 2012];Rubeosis anti-VEGF (RAVE) trial for ischemic central retinal vein occlusion. doi: 10.1097/IAE.0000000000000191. clinicaltrials.gov/ct2/show/NCT00406471. [DOI] [PubMed]
- Ohnishi Y, Ishibashi T, Sagawa T. Fluorescein gonioangiography in diabetic neovascularisation. Graefe's Archive for Clinical and Experimental Ophthalmology. 1994;232(4):199–204. doi: 10.1007/BF00184005. [DOI] [PubMed] [Google Scholar]
- Oshima Y, Sakaguchi H, Gomi F, Tano Y. Regression of iris neovascularization after intravitreal injection of bevacizumab in patients with proliferative diabetic retinopathy. American Journal of Ophthalmology. 2006;142(1):155–8. doi: 10.1016/j.ajo.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Pagenstecher M. Contribution to the teachings of hemorrhagic glaucoma [Beitrage zur Lehre vom hämorrhagischen Glaucom]. Graefe's Archive for Clinical and Experimental Ophthalmology. 1871;17:98–130. [Google Scholar]
- The Nordic Cochrane Centre, The Cochrane Collaboration . Review Manager (RevMan). 5.2. The Nordic Cochrane Centre, The Cochrane Collaboration; Copenhagen: 2012. [Google Scholar]
- Rogell GD. Incremental panretinal photocoagulation. Results in treating proliferative diabetic retinopathy. Retina. 1983;3(4):308–11. doi: 10.1097/00006982-198300340-00015. [DOI] [PubMed] [Google Scholar]
- Sone H, Okuda Y, Kawakami Y, Hanatani M, Suzuki H, Kozawa T, et al. Vascular endothelial growth factor level in aqueous humor of diabetic patients with rubeotic glaucoma is markedly elevated. Diabetes Care. 1996;19(11):1306–7. doi: 10.2337/diacare.19.11.1306b. [DOI] [PubMed] [Google Scholar]
- Tripathi RC, Li J, Tripathi BJ, Chalam KV, Adamis AP. Increased level of vascular endothelial growth factor in aqueous humor of patients with neovascular glaucoma. Ophthalmology. 1998;105(2):232–7. doi: 10.1016/s0161-6420(98)92782-8. [DOI] [PubMed] [Google Scholar]
- Tsai JC, Feuer WJ, Parrish RK, 2nd, Grajewski AL. 5-Fluorouracil filtering surgery and neovascular glaucoma. Long-term follow-up of the original pilot study. Ophthalmology. 1995;102(6):887–92. doi: 10.1016/s0161-6420(95)30938-4. [DOI] [PubMed] [Google Scholar]
- Tsai JT, Wand M. Chapter 213: Neovascular Glaucoma. In: Alm A, Grosskreutz C, editors. Albert and Jakobiec’s Principles and Practice of Ophthalmology. 3rd Edition. Vol. 2. Saunders Elsevier; Canada: 2008. p. 2689. [Google Scholar]
- Vasudev D, Blair MP, Galasso J, Kapur R, Vajaranant T. Intravitreal bevacizumab for neovascular glaucoma. Journal of Ocular Pharmacology and Therapeutics. 2009;25(5):453–8. doi: 10.1089/jop.2009.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VEGF Inhibition Study in Ocular Neovascularization (V.I.S.I.O.N.) Clinical Trial Group. D'Amico DJ, Masonson HN, Patel M, Adamis AP, Cunningham ET, Jr, et al. Pegaptanib sodium for neovascular age-related macular degeneration: two-year safety results of the two prospective, multicenter, controlled clinical trials. Ophthalmology. 2006;113(6):992–1001. doi: 10.1016/j.ophtha.2006.02.027. [DOI] [PubMed] [Google Scholar]
- Wakabayashi T, Oshima Y, Sakaguchi H, Ikuno Y, Miki A, Gomi F, et al. Intravitreal bevacizumab to treat iris neovascularization and neovascular glaucoma secondary to ischemic retinal diseases in 41 consecutive cases. Ophthalmology. 2008;115(9):1571–80. doi: 10.1016/j.ophtha.2008.02.026. [DOI] [PubMed] [Google Scholar]
- Wilkins M, Indar A, Wormald R. Intraoperative Mitomycin C for glaucoma surgery. Cochrane Database of Systematic Reviews. 2005;(4) doi: 10.1002/14651858.CD002897.pub2. [DOI: 10.1002/14651858.CD002897.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wormald R, Wilkins M, Bunce C. Postoperative 5-Fluorouracil for glaucoma surgery. Cochrane Database of Systematic. Reviews. 2001;(3) doi: 10.1002/14651858.CD001132. [DOI: 10.1002/14651858.CD001132] [DOI] [PubMed] [Google Scholar]
- Yalvac IS, Eksioglu U, Satana B, Duman S. Long-term results of Ahmed glaucoma valve and Molteno implant in neovascular glaucoma. Eye. 2007;21(1):65–70. doi: 10.1038/sj.eye.6702125. [DOI] [PubMed] [Google Scholar]
- Yazdani S, Hendi K, Pakravan M. Intravitreal bevacizumab (Avastin) injection for neovascular glaucoma. Journal of Glaucoma. 2007;16(5):437–9. doi: 10.1097/IJG.0b013e3180457c47. [DOI] [PubMed] [Google Scholar]
- Simha A, Braganza A, Abraham L, Samuel P, Lindsley K. Anti-vascular endothelial growth factor for neovascular glaucoma. Cochrane Database of Systematic Reviews. 2009;(3) doi: 10.1002/14651858.CD007920.pub2. [DOI: 10.1002/14651858.CD007920] [DOI] [PMC free article] [PubMed] [Google Scholar]