Abstract
Despite China’s rapid progress improving water, sanitation and hygiene (WSH) access, in 2011, 471 million people lacked access to improved sanitation and 401 million to household piped water. Because certain infectious diseases are sensitive to changes in both climate and WSH conditions, we projected impacts of climate change on WSH-attributable diseases in China in 2020 and 2030 by coupling estimates of the temperature sensitivity of diarrheal diseases and three vector-borne diseases, temperature projections from global climate models, WSH-infrastructure development scenarios, and projected demographic changes. By 2030, climate change is projected to delay China’s rapid progress toward reducing WSH-attributable infectious disease burden by 8–85 months. This development delay summarizes the adverse impact of climate change on WSH-attributable infectious diseases in China, and can be used in other settings where a significant health burden may accompany future changes in climate even as the total burden of disease falls due to non-climate reasons.
Introduction
Globally in 2010, infectious diseases attributable to unsafe water, sanitation, and hygiene (WSH) were estimated to be responsible for 337,000 deaths and the loss of more than 21 million disability adjusted life-years (DALYs)1. WSH-attributable diseases include soil-transmitted helminth (STH) infections, schistosomiasis, diarrheal diseases (fully or partially preventable through improvements to WSH infrastructure), and vector-borne diseases such as malaria, dengue and Japanese encephalitis (associated with poor management of water resources, such as inadequate drainage and unsafe storage of domestic water)2–4. The distribution of the WSH-attributable disease burden is uneven, highlighting well-recognized global health disparities: 66% of the burden is borne by children under 5 years-old, driven primarily by premature mortality from diarrhea, and nearly three-quarters of this burden occurs in 15 developing countries1,5. In China, specifically, WSH-attributable disease burden is similarly concentrated in low-income provinces and in young children6. In addition to their morbidity and mortality, the sequelae of these diseases, such as malnutrition, stunting, impaired school performance, immunodeficiency, and impaired cognitive functioning, can hinder economic growth and development at a population level7,8.
While climate and weather relationships for many WSH-attributable diseases are not well-characterized, there are studies associating certain diseases with key environmental variables responsive to changes in climate, including temperature9,10, precipitation11,12, and relative humidity10,13. Shifts in temperature can impact transmission by influencing the replication rate and survival of pathogens and vectors in the environment14. Meanwhile, as climate change intensifies the hydrologic cycle15,16, heavy precipitation events can overwhelm existing water and sanitation systems, mobilizing pathogens17,18, and drought conditions can increase pathogen exposure by limiting the water available for hygiene and forcing populations to utilize contaminated water supplies19,20.
China has made tremendous progress reducing WSH-attributable diseases through decades-long improvements in water supply and sanitation21. Yet, while the Millennium Development Goal (MDG) for drinking water was met in 2009, the MDG for sanitation has been more difficult to achieve22, and considerable disparities remain6. China is known to have limited water resources—overall per capita supply is about 32% of the world average23—and thus is particularly vulnerable to risks associated with the impacts of climate change on water supply and quality, potentially slowing or even reversing some of the gains made through China’s recent rapid investments in infrastructure24. What is more, China is expected to experience large changes in climate over the coming decades: where average global temperatures are expected to increase by 0.5–4.4°C over 1990 levels by 210025, China is projected to experience a 3.9–6.0 °C increase26 and has already warmed 1.1°C over the past 50 years26.
Here, we quantify the change in the burden of WSH-attributable disease in response to projected changes in temperature in China in 2020 and 2030. We examine how these changes interact with concomitant changes in demographics and urbanization in China, and how uncertainty in both future climate conditions and future WSH infrastructure development (as depicted by the set of storylines described in Table 1) influence the estimated burden of WSH-attributable disease. This is, to our knowledge, the first estimate of infectious disease burden (expressed in units of DALYs per 1,000 population) that accounts for changes in both WSH infrastructure and climate, while also accounting for regional variations in baseline incidence and the varied impact of changes in temperature on diarrheal diseases across different WSH access scenarios (Table 2). The epidemiological literature quantifying relationships between WSH-attributable diseases and climatic variables is limited. Because our review found few studies quantifying relationships between WSH-attributable disease incidence and variation in precipitation or relative humidity (see Supplementary Information), we restricted our quantitative analysis to projected changes in temperature, and acknowledge that, even for this variable, available literature is limited.
Table 1.
The twelve storylines utilized in the analysis, developed by combining the three water and sanitation access development paths and four representative concentration pathway (RCP) scenarios.
| Storyline | RCP scenario | Water and sanitation access development path |
|---|---|---|
|
| ||
| 0.1 | Reference | Maintenance level |
| 0.2 | Linear (midline) | |
| 0.3 | Exponential | |
|
| ||
| 1.1 | 2.6 | Maintenance level |
| 1.2 | Linear (midline) | |
| 1.3 | Exponential | |
|
| ||
| 2.1 | 4.5 | Maintenance level |
| 2.2 | Linear (midline) | |
| 2.3 | Exponential | |
|
| ||
| 3.1 | 6.0 | Maintenance level |
| 3.2 | Linear (midline) | |
| 3.3 | Exponential | |
|
| ||
| 4.1 | 8.5 | Maintenance level |
| 4.2 | Linear (midline) | |
| 4.3 | Exponential | |
Table 2.
Parameter values for α, which describes the proportional change in the rate ratio of each WSH-attributable disease associated with a 1°C increase in surface temperature. α values are derived from a literature review and meta-analysis described in the Supplementary Information. (Modified from prior work6.)
| Disease | Water and sanitation access scenarioa | α value (95% CI) | |
| Diarrheal diseases | II | Centralized, treated drinking water is piped to each residence AND improved sanitation facilities are appropriately installedb,c | 0.077 (0.046, 0.108) |
| IV | Drinking water is available from centralized piped systems, but treatment is incomplete or nonexistent (partially improved) AND improved sanitation facilities are appropriately installedb,c | 0.080 (0.070, 0.090) | |
| V | Either improved sanitation facilities or partially improved drinking water is availableb,c,d | 0.030 (0.012, 0.050) | |
| VI | No improved or partially improved drinking water or improved sanitation is availableb,c | 0.056 (0.034, 0.078) | |
| Aggregate | 0.063 (0.039, 0.086) | ||
|
| |||
| Malaria | 0.125 (0.023, 0.227) | ||
|
| |||
| Dengue fever | 0.260 (−0.052, 0.572) | ||
|
| |||
| Japanese encephalitis | 0.079 (0.033, 0.126) | ||
Because baseline diarrhea risk and the impact of temperature on disease risk may depend on local conditions, α values for diarrheal diseases are shown for specific water and sanitation access scenarios as well as aggregated across all scenarios. Scenario-specific baseline rate ratios were obtained from prior work6: II = 2.5; IV = 4.5; V = 5.2; and VI = 11.2, using an idealized scenario with no transmission of diarrheal diseases from unsafe water or sanitation as the reference group.
Improved sanitation includes a sewer connection (typically seen in urban areas), a triple compartment septic tank, an anaerobic biogas digester, a double barrel funnel type septic tank, and a urine-separating toilet with a septic tank. The latter four designs, found in rural areas, reduce pathogen loads through extended residence times as well as physical and chemical inactivation of pathogens, depending on soil and weather conditions. Unimproved sanitation includes unprotected stool pits and the absence of any sanitation system.
Improved drinking water is defined as water that comes from centralized piped water systems that are treated regularly. Partially improved drinking water also comes from centralized piped water systems, but treatment is irregular or nonexistent. Untreated wells and surface water sources were classified as unimproved.
Combined scenarios Va and Vb6; see Supplementary Methods.
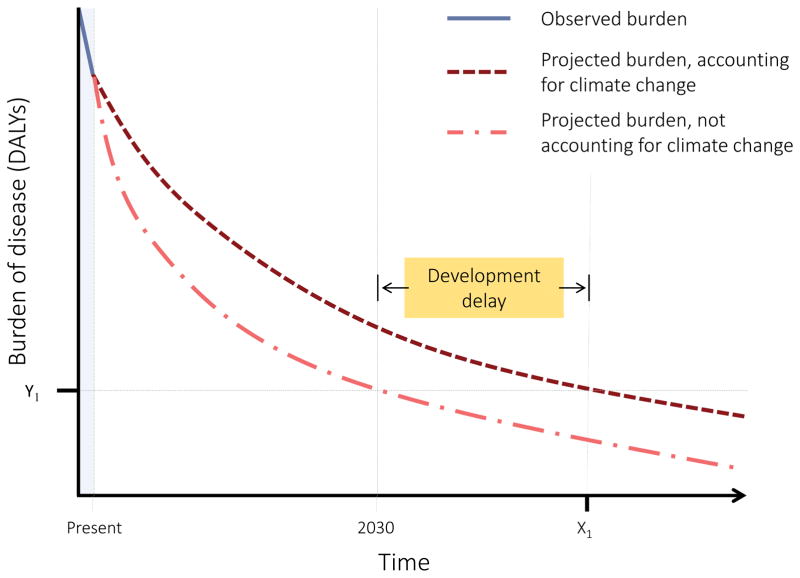
The impact of climate change was quantified as a development delay, defined as the length of time required for the country to reduce disease burden in the presence of climate change to the level projected in the absence of climate change. The development delay can be interpreted as the additional years of continued investment in infrastructure and personnel required in the presence of climate change to achieve the disease burden anticipated without climate change (Figure 1).
Figure 1.
Conceptual diagram of the development delay (highlighted) attributable to climate change in 2030. As the burden of disease falls in a given setting, the development delay associated with climate change at 2030 is the time beyond 2030 (i.e., X1 - 2030) required in the presence of climate change to achieve the burden of disease projected for 2030 without the impact of climate change (Y1). More generally, the development delay for a given year is calculated as the time that will pass before the burden of disease under climate change conditions will equal the burden of disease projected for that year without the impact of climate change. Negative delay values indicate the effect of climate change is to accelerate progress towards improved health.
Projected climate exposures
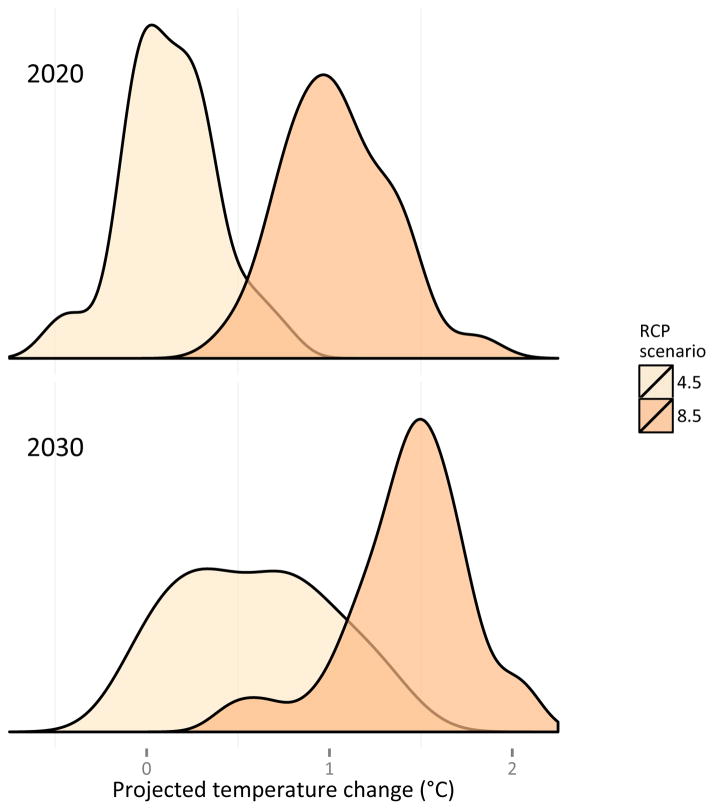
HadGEM2-ES model outputs for the four representative concentration pathway (RCP) scenarios were used to project provincial temperature deviation (Td) in 2020 and 2030 relative to the 2008 reference climate. The projected mean Td under RCP 2.6 indicates that China is expected to undergo 0.57°C of warming nationwide between 2008 and 2020 (see Supplementary Figure 2 and Supplementary Table 2). RCP 2.6 projects a total warming of 0.99°C between 2008 and 2030 (see Supplementary Figure 3 and Supplementary Table 3). Under RCP 8.5, the temperature increase reaches 1.0°Cand 1.38 °C by 2020 and 2030, respectively. Population exposure to the projected climate across China is shown in Figure 2, expressed as the distribution of the population-weighted temperature deviations, ΔTρ, in 2020 and 2030 (also see Supplementary Figure 4). In the Supplementary Results, the HadGEM2-ES model is compared against observations and against other CMIP5 models, and the regional representativeness of the semi-decadal analysis is assessed.
Figure 2.
Distribution of population-weighted provincial temperature deviations, ΔTρ, from 2008 under RCP 4.5 and RCP 8.5. The y-axis represents the proportion of provinces across China experiencing a given ΔTρ value.
Projected diarrheal and vector-borne disease burden
Disease- and province-specific baseline rates were propagated forward using the above projected temperature deviations for 2020 and 2030, disease-specific temperature response functions, and the WSH storylines in Table 1. The burden of WSH-attributable disease in all storylines was dominated by diarrheal diseases (Supplementary Table 4), similar to the results of our previous work6. The reference storyline 0.2, in which there is no climate change, accounted for projected urbanization, population growth and changes in population age distribution. Assuming a linear water and sanitation development path, this reference storyline projects a nationwide decrease in the burden of diarrheal diseases (in DALYs) of 51.3% between 2008 and 2020, and 63.7% between 2008 and 2030. On the same linear development path under RCP 2.6 (storyline 1.2), the decrease is 48.4% between 2008 and 2020, and 59.5% between 2008 and 2030. For RCP 8.5 (storyline 4.2), the decrease slows yet more, to 46.3% between 2008 and 2020, and 58.0% between 2008 and 2030. From 2008 to 2030, climate change is projected to slow the rate of decrease in diarrheal disease burden by 6.5% under RCP 2.6 and 8.9% under RCP 8.5.
Reference storyline results indicate that the total burden of malaria, dengue fever, and Japanese encephalitis is expected to decrease 6.6% by 2020 and 20.9% by 2030, without climate change. Under RCP scenario 2.6 the burden decreases 7.5% by 2020 and 16.4% by 2030. Under RCP 8.5, the burden decreases only 6.5% by 2020 and 15.1% by 2030. Thus, between 2008 and 2030 climate change slows the rate of decrease in vector-borne disease burden by 21.2% under RCP 2.6 and by 27.8% under RCP 8.5. Notably, in the case of dengue fever, the confidence interval for α included the null value (zero).
Quantification of climate change development delay
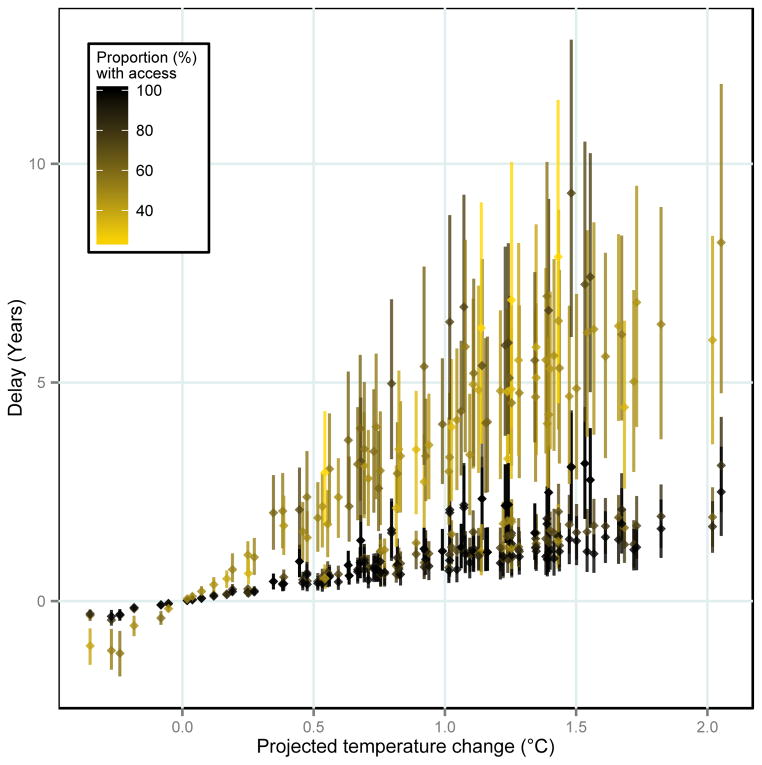
At the national level, by 2020 the development delay imposed on China by climate change (Table 3) ranges from 1.2 months (RCP 4.5 and exponential development path; storyline 2.3) to 48 months (RCP 8.5 and maintenance development path; storyline 4.1). By 2030, the delay ranges from 8 months (RCP 6.0 and exponential path; storyline 3.3) to 62 months (RCP 8.5 and maintenance path; storyline 4.1). However, the delay in 2030 ranged from 9 months (under RCP 4.5) to 21 months (under RCP 8.5) when assuming a linear water and sanitation development path that makes minimal assumptions about the future trend in infrastructure improvement in China beyond the trend observed from 1990 to 201227 (Table 3). On the same development path, the delay reaches 15 months under RCP 2.6, which is the climate change scenario consistent with the lowest greenhouse gas emissions28. The full range of development delays imposed by climate change, and the sensitivity of these values to changes in development paths, RCPs, and uncertainty in α, can be seen in Figure 3 and Supplementary Figure 9; geographical variation in delays across China is shown in Supplementary Figure 10.
Table 3.
Estimated burden of WSH-attributable disease in China in 2020 and 2030, presented across storylines constituting water and sanitation access development paths and RCP scenarios. The development delay attributable to climate change in 2020 and 2030 is presented for each of the twelve storylines. The 95% confidence intervals generated from a meta-analysis of α values drawn from the literature were propagated through the full analysis reported here (95% CIs).
| Storyline | RCP scenario | Water and sanitation access development path | 2020 | 2030 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Burden of disease (millions of DALYs) | 95% CI | Development delay (months) | 95% CI | Burden of disease (millions of DALYs) | 95% CI | Development delay (months) | 95% CI | |||
|
| ||||||||||
| 0.1 | reference | Maintenance level | 2.42 | N/A | N/A | N/A | 2.10 | N/A | N/A | N/A |
| 0.2 | Linear (midline) | 1.36 | N/A | N/A | N/A | 1.02 | N/A | N/A | N/A | |
| 0.3 | Exponential | 1.21 | N/A | N/A | N/A | 0.82 | N/A | N/A | N/A | |
|
| ||||||||||
| 1.1 | 2.6 | Maintenance level | 2.53 | (2.49 to 2.57) | 28.7 | (17.7, 40.6) | 2.26 | (2.20 to 2.33) | 45.3 | (27.5, 63.7) |
| 1.2 | Linear (midline) | 1.44 | (1.41 to 1.47) | 7.3 | (4.8, 10.0) | 1.13 | (1.09 to 1.18) | 15.1 | (9.5, 20.8) | |
| 1.3 | Exponential | 1.28 | (1.25 to 1.31) | 6.2 | (3.9, 8.6) | 0.93 | (0.88 to 0.97) | 13.1 | (8.1, 18.4) | |
|
| ||||||||||
| 2.1 | 4.5 | Maintenance level | 2.45 | (2.44 to 2.46) | 5.9 | (3.7, 8.7) | 2.20 | (2.16 to 2.23) | 26.2 | (16.1, 36.8) |
| 2.2 | Linear (midline) | 1.38 | (1.37 to 1.39) | 1.6 | (1.1, 2.3) | 1.08 | (1.06 to 1.11) | 8.7 | (5.5, 12.2) | |
| 2.3 | Exponential | 1.22 | (1.22 to 1.23) | 1.2 | (0.8, 1.9) | 0.88 | (0.86 to 0.91) | 7.8 | (4.8, 10.9) | |
|
| ||||||||||
| 3.1 | 6.0 | Maintenance level | 2.45 | (2.44 to 2.47) | 7.9 | (5.0, 11.5) | 2.20 | (2.16 to 2.24) | 27.8 | (17.1, 38.9) |
| 3.2 | Linear (midline) | 1.38 | (1.37 to 1.39) | 1.9 | (1.3, 2.8) | 1.09 | (1.06 to 1.12) | 9.3 | (5.9, 12.9) | |
| 3.3 | Exponential | 1.23 | (1.22 to 1.24) | 1.7 | (1.1, 2.5) | 0.88 | (0.86 to 0.91) | 8.1 | (5.0, 11.4) | |
|
| ||||||||||
| 4.1 | 8.5 | Maintenance level | 2.60 | (2.53 to 2.67) | 48.2 | (29.2, 68.3) | 2.32 | (2.23 to 2.41) | 62.0 | (37.4, 87.3) |
| 4.2 | Linear (midline) | 1.50 | (1.45 to 1.55) | 12.7 | (8.5, 17.1) | 1.18 | (1.12 to 1.24) | 20.8 | (13.1, 28.6) | |
| 4.3 | Exponential | 1.33 | (1.29 to 1.38) | 10.6 | (6.8, 14.7) | 0.97 | (0.91 to 1.03) | 18.0 | (11.0, 25.1) | |
Figure 3.
Province-specific development delay values shown as a function of the temperature deviation from 2008 to 2030. The proportion of the population with access to improved water and sanitation in 2030 is indicated by the color scale. Dots represent delays calculated using mean α; whiskers express the 95% confidence intervals derived from the pooled α effect measures from the meta-analysis; separate dots/whiskers are shown for each storyline for each province. Shanghai, Beijing, and Tianjin are not shown.
Sensitivity and uncertainty analyses
We analyzed the sensitivity of the diarrheal disease results to employing an aggregate α, versus α values stratified by four water and sanitation access scenarios (Table 2). Compared with using the aggregate α, stratified values generally yielded slightly higher estimates for diarrheal disease burden (2020 range: 0.04% lower to 1.19% higher; 2030 range: 0.44% lower to 2.85% higher; see Supplementary Results). Propagation of 95% confidence intervals for the aggregate α values for each disease category (Table 2) yielded a change in the projected nationwide burden of WSH-attributable disease in 2020 of less than 3.6% of the total burden, and less than 6.1% of the projected disease burden in 2030 (Table 3). For both time periods and under all storylines, there was an increase in WSH-attributable disease burden relative to the reference storyline even at the lower bound of each estimate.
The storylines that included the maintenance level water and sanitation development path yielded projected WSH-attributable disease burdens that were 76–79% greater in 2020 and 98–104% greater in 2030 when compared with the respective storylines using linear development paths. Likewise, when compared to linear development path storylines, storylines consistent with an exponential development path projected a nationwide disease burden that was 11–12% lower in 2020 and 18–19% lower in 2030 (Table 3).
Discussion and conclusions
This analysis represents the first assessment of the impact of climate change on WSH-attributable diseases a cross China. The country’s demographic and epidemiologic transitions, as well as changes to water and sanitation infrastructure, are expected to rapidly decrease the burden of infectious disease29. Our findings indicate that climate change will blunt this progress, even while controlling for demographic changes, infrastructure development, and urbanization (Figure 3 and Supplementary Figure 10).
The development delay imposed by climate change in 2030 amounts to 15 months under RCP 2.6 and 21 months under RCP 8.5, assuming a linear water and sanitation development path. In other words, in the presence of climate change, China loses on the order of 1–2 years of progress in reducing the burden of diarrheal and other WSH-attributable diseases; an additional 15 to 21 months of continued infrastructure investment, urbanization, and demographic shifts will be required in order to achieve the decrease in disease burden if not for climate change. Under a storyline assuming high emissions (RCP 8.5) and a maintenance development path, this development delay increases to over 5 years by 2030. Under the most aggressive (exponential) water and sanitation development path, the development delay by 2030 is 13 months under RCP 2.6 and 18 months under RCP 8.5.
After RCP 8.5, RCP 2.6 produces the next longest development delay, despite being the scenario consistent with the lowest concentration of greenhouse gases in 2100. The apparent paradox is the result of the radiative forcing pattern experienced under RCP 2.628, which peaks at 3.1 W/m2 in the mid-21st century. Thus, our timeframe captures a period during which the projected Td (°C) for China is greater under RCP 2.6 than under RCPs 4.5 or 6.0 (see Supplementary Figures 2, 3 and 4), before the projected decline in radiative forcing occurs28. This reinforces the need, when carrying out impact studies, to carefully consider the time frame over which impacts are being estimated in the context of the time course of warming projected by the scenarios used.
There were two potential sources of uncertainty in our analysis. The first was the rate at which improved water and sanitation access will increase. The three development paths presented represent increasingly ambitious policy options for China’s future investment in water and sanitation infrastructure. The linear path was consistent with China’s recent development as described by the WHO and UNICEF Joint Monitoring Program27, and thus was considered the midline estimate for our analysis. The most conservative estimate, the maintenance level path, assumed that access to improved water and sanitation was held constant at 2008 levels. This may seem unrealistic for a rapidly developing country, yet China’s unprecedented rural-to-urban migration, and its population growth30, will necessitate tremendous investments to maintain 2008 levels of access, particularly in urban areas. However, even if China were to exponentially increase the proportion of the population with access to improved water and sanitation as in the most liberal path, we project 8–18 months (depending on RCP) of development delay due to climate change by 2030.
Of interest, for diarrheal diseases the highest pooled estimates of α that we derived from the literature were not associated with low water and sanitation access scenarios. This may be due to the fact that α estimates across water and sanitation access scenarios are based on very few studies. However, the use of an aggregate α, which pooled a larger number of studies, instead of stratified values had little impact on our estimates of diarrheal disease burden (changing estimates by −0.04% to 2.85%). It is also possible that settings with higher baseline exposures because of poorer infrastructure may have lower α estimates because the physiologic response is blunted (i.e., a hormetic effect). Still, for reasons unrelated to scenario-specific α estimates, our analysis illustrates the limits of adaptation in provinces where access to improved water and sanitation is very high. Populations in these settings have reached their capacity to adapt through improving water and sanitation infrastructure, and our analysis projects large delays attributable to climate change in such provinces (Supplementary Figure 9, panel a). These findings raise the question of how adaptation afforded through other means (e.g., improving health systems) might be used to overcome the burden of disease attributable to climate change in regions that are able to achieve complete access to improved water and sanitation infrastructure, and, more generally, how high and low resource populations may both be impacted by climate stressors.
The second source of potential uncertainty was the HadGEM2-ES model output we used to generate our projections. The model accounts for the direct and indirect effects of aerosols, the impact of iron deposition on ecosystems, ozone, methane, and oxidants on tropospheric chemistry. The HadGEM2-ES model has been thoroughly evaluated against a variety of observed data and found to realistically represent near surface temperature, even in the presence of its complex Earth system model components.31 In this study, we further evaluated the model’s temperature outputs over the baseline period (2006–2010), and found that HadGEM2-ES performed comparable to other CMIP5 models when temperatures are compared to observations (Supplementary Results). Our projected temperature change across China from 2008 to 2030 was consistent with the IPCC AR5 projections over the same time period32 (Supplementary Results). We acknowledge the HadGEM2-ES model as a source of uncertainty even still, but note that a full analysis of this source of uncertainty was beyond the scope of this study.
There are other potential sources of bias, but where possible we sought to direct the influence of our analytical assumptions toward the null. For instance, we assumed that any urban population had access to improved water and sanitation, despite several studies suggesting urban centers in China suffer from overwhelmed and inadequate water treatment facilities and inconsistent provision of piped water8,21. Furthermore, we limited our consideration to a small subset of WSH-related sequelae associated with climate change, and we did not include the WSH-related impacts of changes in precipitation levels, shifts in variability of temperature, sea level rise, salt-water intrusion, subsidence, flooding events, destruction of existing infrastructure, increased Urban Heat Island effect, or drought on the incidence of WSH-attributable disease26,33. Thus, the baseline burden of diarrheal diseases presented in our prior analysis is likely an underestimate, as are the results of the analysis presented here.
Our analysis required the assumption that response functions representing the relationship between temperature and WSH-attributable diseases derived elsewhere apply to the population being studied, though we adjusted these functions to match provincial-level infrastructure differences. As part of an effort to stand otherwise on the firmest foundation, we limited our consideration to the most common, linear models of WSH-attributable disease incidence response to temperature, despite the limited plausibility of such simple relationships34, and limited our description of climate change to changes in temperature, as these have the strongest support in the literature. As our understanding of the complex relationships between climate, WSH-attributable disease and development matures, these decisions bear revisiting in future analyses.
Across the diseases and storylines analyzed here, our findings are consistent with the assertion that climate change has the potential to delay China’s heretofore rapid progress toward decreasing the burden of WSH-attributable disease. The development delay is projected to be eight months or greater by 2030 if linear increases in water and sanitation infrastructure are continued, amounting to over 400,000 DALYs lost that would have been prevented by climate change mitigation. During the delay period, China would need to continue to make financial investments in human capital and physical infrastructure at the same rate provided from 1990 to 2012 just to counter the effect of climate change.
Despite the assumption that national development progresses with a concomitant increase in per capita greenhouse gas emissions35, the present analysis indicates the need to acknowledge the net delay in development that climate change, driven by said emissions, will impose. Delays in development as characterized by our analysis come at a potentially large cost—China’s investments in improved water and sanitation infrastructure from 2006 to 2010 amounted to approximately US$10.8 billion per year36—and these are in addition to the direct and indirect costs of the burden of WSH-attributable disease itself, which is estimated to cost China as much as US$11 billion per year37. The impact of climate change on WSH-attributable disease extends beyond the burden of disease discussed here; this analysis focused on only one family of health impacts associated with climate change, and thus the true development delay imposed by climate change on China is likely much larger.
Methods
Comparative risk assessment methods were used to estimate the burden of disease attributable to changes in temperature associated with climate change1,38,39. Previous estimates of the 2008 burden of disease attributable to unsafe WSH in each of the 31 provincial level administrative districts within China6, derived from data sources detailed in the Supplement (Supplementary Methods), served as the baseline in this provincial-level analysis. Following previous work5, WSH-attributable disease was defined to include diseases resulting from consumption of contaminated water; poor personal, domestic, or agricultural hygiene associated with a lack of access to clean or adequate water; and direct contact with water-dwelling vectors or pathogens due to unsafe water resource management.
To account for uncertainty in both future climate conditions and future infrastructure development, we constructed 12 storylines (Table 1) by combining output from 4 representative concentration pathways (RCPs)28 and 3 water and sanitation access projections corresponding to low, intermediate, and high investment options. The three water and sanitation access projections, termed ‘development paths’ herein and detailed in Supplementary Figure 1, assume: (1) maintenance level of current access; (2) a linear rate of increase in the proportion of the population with access; and (3) an exponential rate of increase in the proportion of the population with access (Supplementary Methods). Projections of the burden of WSH-attributable disease were estimated accounting for demographic trends by projecting the population distribution in 200040 (at approximately 1.0 km x 1.0 km resolution) to 2020 and 2030 using province-specific growth and urbanization rates41,42 (Supplementary Results Tables 2 and 3).
Monthly temperature projections under RCP 2.6, RCP 4.5, RCP 6.0, and RCP 8.5 generated by the HadGEM2-ES (1.25° latitude x 1.875° longitude) global climate model43 were obtained from the CMIP544. For each RCP, the semi-decadal mean monthly surface air temperature deviation in 2020 from a 2008 reference climate was calculated for each province, ρ, in China (Tdρ,2020, °C; Supplementary Methods, equation 2.1). Tdρ,2030 was calculated in an analogous fashion. A separate evaluation was carried out using 53CMIP5 ensemble members to assess the degree to which the reference period was representative, and to evaluate how results might differ using alternative CMIP5 models/members (Supplementary Results). To account for the uneven distribution of population across provinces, a population-weighted exposure to changing temperature, ΔTρ (°C), was calculated for each province, ρ (Supplementary Methods, equation 2.2).
A systematic literature review was conducted to identify studies quantifying the relationship between climate components and incidence of WSH-attributable diseases. The effect estimates from reviewed literature were aggregated45 to estimate the change in rate ratios for diarrheal diseases, malaria, dengue fever, and Japanese encephalitis in response to a 1°C increase in mean temperature (defined herein as α) using standard random effects meta-analysis techniques45 as detailed in Supplementary Methods (Supplementary Table 1). Because the impact (α) of increases in temperature on diarrheal diseases may vary depending on specific WSH infrastructure access, rate ratios obtained from the literature review were matched to China-specific water and sanitation access scenarios (Table 2, Supplementary Table 1). These α values were combined with the 2020 and 2030 ΔTρ values to obtain adjusted RRs for each province, disease, and WSH scenario (Supplementary Information, equation 1.1).
Age- and sex-specific estimates of incidence and mortality were then estimated for each province using the 2020 and 2030 adjusted RRs (Supplementary Methods). The overall burden of WSH-attributable disease (in DALYs per 1,000 population) was calculated under each of twelve storylines (Table 1) for 2020 and 2030 using the age- and sex-specific incidence and mortality counts. DALYs were calculated assuming non-uniform age-weighting and 3% discounting, with disability weights and disease durations drawn from established sources6,46 (Supplementary Methods). The burden of WSH-attributable disease projected under each storyline was then compared to the burden of disease anticipated in 2020 and 2030 without the impact of climate change. The impact of climate change on China’s ongoing progress reducing WSH-attributable disease was summarized as a development delay, δ, which expresses the additional time (in months) that a province would be required to continue to provide infrastructure improvement, health investments, and other efforts in order to attain the burden of WSH-attributable disease predicted under a scenario without the impact of climate change (see Figure 1 and Supplementary Methods). To quantify the impact of the uncertainty in the parent studies on our final results, the 95% confidence intervals of α values identified during the literature review were combined using standard, random effects meta-analysis techniques45 and were propagated through the analysis.
Supplementary Material
Acknowledgments
This work was supported in part by the Chemical, Bioengineering, Environmental, and Transport Systems Division of the National Science Foundation under grant no. 1249250, by the Division of Earth Sciences of the National Science Foundation under grant no. 1360330, by the National Institute for Allergy and Infectious Disease (K01AI091864) and by the Global Health Institute at Emory University. Yang Liu was supported in part by the Centers for Disease Control and Prevention (U01EH000405) and the National Institutes of Health (R21ES020225). Song Liang was supported in part by US EPA Science to Achieve Results grant (RD835192010) and by Emerging Pathogens Institute, University of Florida. Yang Gao was supported in part by the Office of Science of the U.S. Department of Energy as part of the Regional and Global Climate Modeling Program. The Pacific Northwest National Laboratory is operated for DOE by Battelle Memorial Institute (DE-AC05-76RL01830).
Footnotes
Author Contributions
MH, JHB, EJC, SL, HL, WL, JJH and JVR conceived and designed the experiments; MH, JHB, SL, YG and JVR performed the experiments; MH, JHB, YG and JVR analyzed the data; MH, JHB, EJC, SL, HL, WL, MCF, YL, JJH and JVR contributed materials/analysis tools; and MH, JHB, EJC, SL, HL, WL, MCF, YL, YG, JJH and JVR wrote the paper.
References
- 1.Lim SS, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pruss-Ustun A, Corvalan C. How much disease burden can be prevented by environmental interventions? Epidemiology. 2007;18:167–178. doi: 10.1097/01.ede.0000239647.26389.80. [DOI] [PubMed] [Google Scholar]
- 3.Pruss A, Kay D, Fewtrell L, Bartram J. Estimating the burden of disease from water, sanitation, and hygiene at a global level. Environmental Health Perspectives. 2002;110:537–542. doi: 10.1289/ehp.110-1240845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fewtrell L, Prüss-Üstün A, Bos R, Gore F, Bartram J. Water, sanitation and hygiene: quantifying the health impact at national and local levels in countries with incomplete water supply and sanitation coverage. World Health Organization; 2007. [Google Scholar]
- 5.Pruss-Ustun A, Bos R, Gore F, Bartram J. Safer water, better health: costs, benefits and sustainability of interventions to protect and promote health. Geneva: 2008. [Google Scholar]
- 6.Carlton EJ, et al. Regional disparities in the burden of disease attributable to unsafe water and poor sanitation in China. Bull World Health Organ. 2012;90:578–587. doi: 10.2471/BLT.11.098343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaible UE, Kaufmann SH. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007;4:e115. doi: 10.1371/journal.pmed.0040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartram J, Cairncross S. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med. 2010;7:e1000367. doi: 10.1371/journal.pmed.1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y, Bi P, Hiller JE. Meteorological variables and malaria in a Chinese temperate city: A twenty-year time-series data analysis. Environ Int. 2010;36:439–445. doi: 10.1016/j.envint.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Checkley W, et al. Effects of El Nino and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet. 2000;355:442–450. doi: 10.1016/s0140-6736(00)82010-3. [DOI] [PubMed] [Google Scholar]
- 11.Hashizume M, Dewan AM, Sunahara T, Rahman MZ, Yamamoto T. Hydroclimatological variability and dengue transmission in Dhaka, Bangladesh: a time-series study. BMC Infect Dis. 2012;12:98. doi: 10.1186/1471-2334-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cann KF, Thomas DR, Salmon RL, Wyn-Jones AP, Kay D. Extreme water-related weather events and waterborne disease. Epidemiol Infect. 2013;141:671–686. doi: 10.1017/S0950268812001653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hales S, de Wet N, Maindonald J, Woodward A. Potential effect of population and climate changes on global distribution of dengue fever: an empirical model. Lancet. 2002;360:830–834. doi: 10.1016/S0140-6736(02)09964-6. [DOI] [PubMed] [Google Scholar]
- 14.Altizer S, Ostfeld RS, Johnson PT, Kutz S, Harvell CD. Climate change and infectious diseases: from evidence to a predictive framework. Science. 2013;341:514–519. doi: 10.1126/science.1239401. [DOI] [PubMed] [Google Scholar]
- 15.Wetherald RT, Manabe S. Simulation of hydrologic changes associated with global warming. Journal of Geophysical Research-Atmospheres. 2002;107 doi: 10.1029/2001jd001195. [DOI] [Google Scholar]
- 16.Meehl GA, Stocker TF. Global Climate Projections. Climate Change 2007: The Physical Science Basis. 2007:747–845. [Google Scholar]
- 17.World Health Organization & Department for International Development. Summary and policy implications Vision 2030: the resilience of water supply and sanitation in the face of climate change. Geneva, Switzerland: 2009. [Google Scholar]
- 18.Curriero FC, Patz J, Rose JB, Lele S. The Association Between Extreme Precipitation and Waterborne Disease Outbreaks in the United States, 1948–1994. Am J Public Health. 2001;91:1194–1199. doi: 10.2105/ajph.91.8.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burr ML, Davis AR, Zbijowski AG. Diarrhoea and the drought. Public Health. 1978;92:86–87. doi: 10.1016/s0033-3506(78)80034-1. [DOI] [PubMed] [Google Scholar]
- 20.Fewtrell L, Colford JM. Water, Sanitation and Hygiene: Interventions and Diarrhoea. 2004 [PubMed] [Google Scholar]
- 21.Zhang J, et al. Environmental health in China: progress towards clean air and safe water. Lancet. 2010;375:1110–1119. doi: 10.1016/S0140-6736(10)60062-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United Nations. The Millenium Development Goals Report. New York: 2013. [Google Scholar]
- 23.The World Bank. The Little Green Data Book 2010. The World Bank; Washington, D.C: 2010. [Google Scholar]
- 24.Remais JV, Zhang J. Environmental lessons from China: finding promising policies in unlikely places. Environ Health Perspect. 2011;119:893–895. doi: 10.1289/ehp.1003024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Vuuren DP, et al. Temperature increase of 21st century mitigation scenarios. Proc Natl Acad Sci U S A. 2008;105:15258–15262. doi: 10.1073/pnas.0711129105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ding YH, et al. Detection, causes and projection of climate change over China: An overview of recent progress. Advances in Atmospheric Sciences. 2007;24:954–971. doi: 10.1007/s00376-007-0954-4. [DOI] [Google Scholar]
- 27.WHO/UNICEF Joint Monitoring Program. China: estimates on the use of water sources and sanitation facilities (1980–2012) World Health Organization; 2014. [Google Scholar]
- 28.Vuuren DP, et al. The representative concentration pathways: an overview. Climatic Change. 2011;109:5–31. doi: 10.1007/s10584-011-0148-z. [DOI] [Google Scholar]
- 29.Cook IG, Dummer TJ. Changing health in China: re-evaluating the epidemiological transition model. Health Policy. 2004;67:329–343. doi: 10.1016/j.healthpol.2003.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gong P, et al. Urbanisation and health in China. Lancet. 2012;379:843–852. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martin GM, et al. The HadGEM2 family of Met Office Unified Model climate configurations. Geoscientific Model Development. 2011;4:723–757. doi: 10.5194/gmd-4-723-2011. [DOI] [Google Scholar]
- 32.IPCC. Climate Change 2013: The Physical Science Basis: Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; Cambridge: 2013. [Google Scholar]
- 33.Jones GW. Southeast Asian Urbanization and the Growth of Mega-Urban Regions. Journal of Population Research. 2002;19:119–136. [Google Scholar]
- 34.Kolstad EW, Johansson KA. Uncertainties associated with quantifying climate change impacts on human health: a case study for diarrhea. Environ Health Perspect. 2011;119:299–305. doi: 10.1289/ehp.1002060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chang C-C. A multivariate causality test of carbon dioxide emissions, energy consumption and economic growth in China. Applied Energy. 2010;87:3533–3537. doi: 10.1016/j.apenergy.2010.05.004. [DOI] [Google Scholar]
- 36.World Bank. Policy Note: Concessionary financing programs for the water and sanitation sector. Report No. 56105. 2009 [Google Scholar]
- 37.Hutton G, Rodriguez UE, Naptitupulu L, Thang P, Kov P. Economic Impacts of Sanitation in South Asia. World Bank; 2008. [Google Scholar]
- 38.McMichael AJ, et al. In: Comparitive Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Vol. 1. Ch 20. World Health Organization; 2004. pp. 1543–1649. [Google Scholar]
- 39.Campbell-Lendrum D, Woodruff R. Comparative risk assessment of the burden of disease from climate change. Environ Health Perspect. 2006;114:1935–1941. doi: 10.1289/ehp.8432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.CIESIN & CIAT. Gridded Population of the World. CIESIN, Columbia University; Palisades, New York: 2011. [Google Scholar]
- 41.Landoni M. Two scenarios on Chinese population dynamics based on a multiregional projection model. Duke University; 2006. [Google Scholar]
- 42.Toth F, Cao G, Hizynyik E. Regional population projections for China. Report No. IR-03-042. International Institute for Applied Systems Analysis; 2003. [Google Scholar]
- 43.Met Office Hadley Centre & Instituto Nacional de Pesquisas Espaciais. US Department of Energy Program for Climate Model Diagnosis and Intercomparison. 2012. [Google Scholar]
- 44.Taylor KE, Stouffer RJ, Meehl GA. An Overview of CMIP5 and the Experiment Design. Bulletin of the American Meteorological Society. 2012;93:485–498. doi: 10.1175/bams-d-11-00094.1. [DOI] [Google Scholar]
- 45.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random effects models for meta-analysis. Research Synthesis Methods. 2010:97–111. doi: 10.1002/jsrm.12. [DOI] [PubMed] [Google Scholar]
- 46.Murray CLJ, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Harvard University Press; 1996. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.