Abstract
Importance
Reperfusion times for ST elevation myocardial infarction (STEMI) occurring in outpatients have improved significantly, but quality improvement efforts have largely ignored STEMI occurring in hospitalized patients (inpatient-onset STEMI).
Objective
To define the incidence and variables associated with treatment and outcomes of patients who develop STEMI during hospitalization for conditions other than acute coronary syndromes (ACS).
Design, Setting and Participants
STEMIs were identified in the 2008–2011 California State Inpatient Database.
Exposure
STEMI were classified as inpatient-onset or outpatient-onset based on present-on-admission codes. Patients who developed STEMI after being hospitalized for ACS were excluded from the analysis.
Main Outcome Measures
Regression models were used to evaluate associations between location of onset of STEMI, resource utilization and outcomes. Adjustments were made for patient age, sex, comorbidities and hospital characteristics.
Results
62021 STEMIs were identified from 303 hospitals of which 3068 (4.9%) occurred in patients hospitalized for non-ACS indications. Inpatient-onset STEMI patients were older (71.5 ± 13.5 vs 64.9 ± 14.1 years; p < 0.001) and more frequently female (47.4% vs 32%; p < 0.001) than outpatient-onset STEMI. Inpatient-onset STEMI had higher in-hospital mortality (33.6% vs 9.2%; adjusted odds ratio (AOR) = 3.05; 95% CI, 2.76 to 3.38; p < 0.001), were less likely to be discharged home (33.7% vs 69.4%; AOR = 0.38; 95% CI, 0.34 to 0.42; p < 0.001), and were less likely to undergo cardiac catheterization (33.8% vs 77.8%; AOR = 0.19; 95% CI, 0.16 to 0.21; p < 0.001) or percutaneous coronary intervention (21.6% vs 65%; AOR = 0.23; 95% CI, 0.21 to 0.26; p < 0.001). Length of stay (13.4 ± 17.8 vs 4.7 ± 6.3 days; adjusted multiplicative effect (AME) = 2.51; 95% CI, 2.35 to 2.69; p < 0.001) and inpatient charges ($245000 ± 258700 vs $129000 ± 129800; AME = 2.09; 95% CI, 1.93 to 2.28; p < 0.001) were higher for inpatient-onset STEMI.
Conclusions and Relevance
Patients who developed STEMI while hospitalized for a non-ACS condition, compared to those with onset of STEMI as an outpatient, were less likely to undergo invasive testing or intervention and had a higher in-hospital mortality rate.
Keywords: Myocardial infarction, STEMI, percutaneous coronary intervention, surgical procedures, inpatient-onset STEMI
INTRODUCTION
Early reperfusion with percutaneous coronary intervention (PCI) or thrombolytic therapy remains the primary goal in the initial treatment of eligible patients presenting to a hospital with ST-elevation myocardial infarction (STEMI). Over the last decade, recognition that this strategy is of critical importance has prompted the development of a number of regional and national initiatives to facilitate and improve systems of care for STEMI. These initiatives, including the North Carolina Reperfusion of Acute Myocardial Infarction in Carolina Emergency Department (RACE) initiative1, the American College of Cardiology (ACC) D2B Alliance2 and the American Heart Association (AHA) Mission: Lifeline initiative3, have enhanced recognition, reduced time to treatment, improved systems of care, and facilitated access of patients to PCI-capable facilities. Consequently, national median door to balloon times improved by over 30 minutes between 2005 and 2010.4
These initiatives have focused exclusively on patients who develop STEMI outside of a hospital setting (outpatient-onset STEMI), and little is known about the incidence and outcomes of STEMI in patients hospitalized for non-acute coronary syndrome (ACS) conditions (inpatient-onset STEMI). In fact, large national databases set up for quality improvement such as the NCDR (National Cardiovascular Data Registry) ACTION Registry–GWTG (Get With The Guidelines) exclude patients who develop STEMI while already hospitalized.5
In a recent single center study, we found that patients who develop inpatient-onset STEMI were older and more often female, had more comorbidities, were less likely to receive reperfusion therapy, had longer ECG to first device activation times, and were less likely to survive than patients with an outpatient STEMI.6 In the current study, we aimed to define the incidence and outcomes of inpatient-onset STEMI in a large multi-center cohort. In addition, we sought to understand the variables that are associated with the development of inpatient-onset STEMI, which may be potential targets for strategies to improve processes and systems of care for this population.
METHODS
Data Source
We examined admissions to non-federal hospitals in the state of California using 2008–2011 discharge data from the State Inpatient Database (CA-SID), which were obtained from the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality.7 The CA-SID is an all-payer administrative database including 100% of the state’s inpatient discharge records. For the purpose of this study, all records were used except those from stand-alone psychiatric hospitals, stand-alone physical and substance use rehabilitation facilities, and individuals under the age of 18 years. Each CA-SID record includes: 1. basic demographic information, including age, gender, race, and primary payer; 2. up to 30 International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) diagnosis codes; 3. up to 21 ICD-9-CM procedure codes; and 4. outcome information, such as discharge disposition, length of stay, and inpatient charges. The CA-SID contains an indicator of whether each discharge diagnosis code was present on admission which enabled the classification of each STEMI as inpatient-onset or outpatient-onset. CA-SID (covering approximately 12% of the US population) was used rather than a national sample because the Nationwide Inpatient Sample does not contain present on admission information, which would have made it unsuitable for this analysis.
Identification of STEMI-Related Hospital Stays
STEMI-related hospitalizations were identified using diagnosis codes 410.X1, excluding 410.71 (non-ST elevation myocardial infarction) and 410.91 (acute myocardial infarction not otherwise specified) in any position. The validity of using this approach for defining MI in administrative data has been previously documented.8 Admissions were classified as outpatient-onset or inpatient-onset STEMI based on present on admission codes (Figure 1). To improve identification of unambiguously inpatient-onset STEMI, we excluded patients with diagnosis codes present on admission that were consistent with non-ST elevation myocardial infarction or unstable angina (410.71, 411.1, 411.81, 411.89), as well as angina pectoris or chest pain (413.x, 768.50, 768.51, 786.59). For patients with STEMI recorded as present on admission, we excluded those who were admitted via transfer from another short stay hospital, since we could not discern whether the STEMI was incident at previous facility (inpatient-onset STEMI) or prior to admission to the previous facility (outpatient-onset STEMI).
Figure 1. Cohort flow diagram.
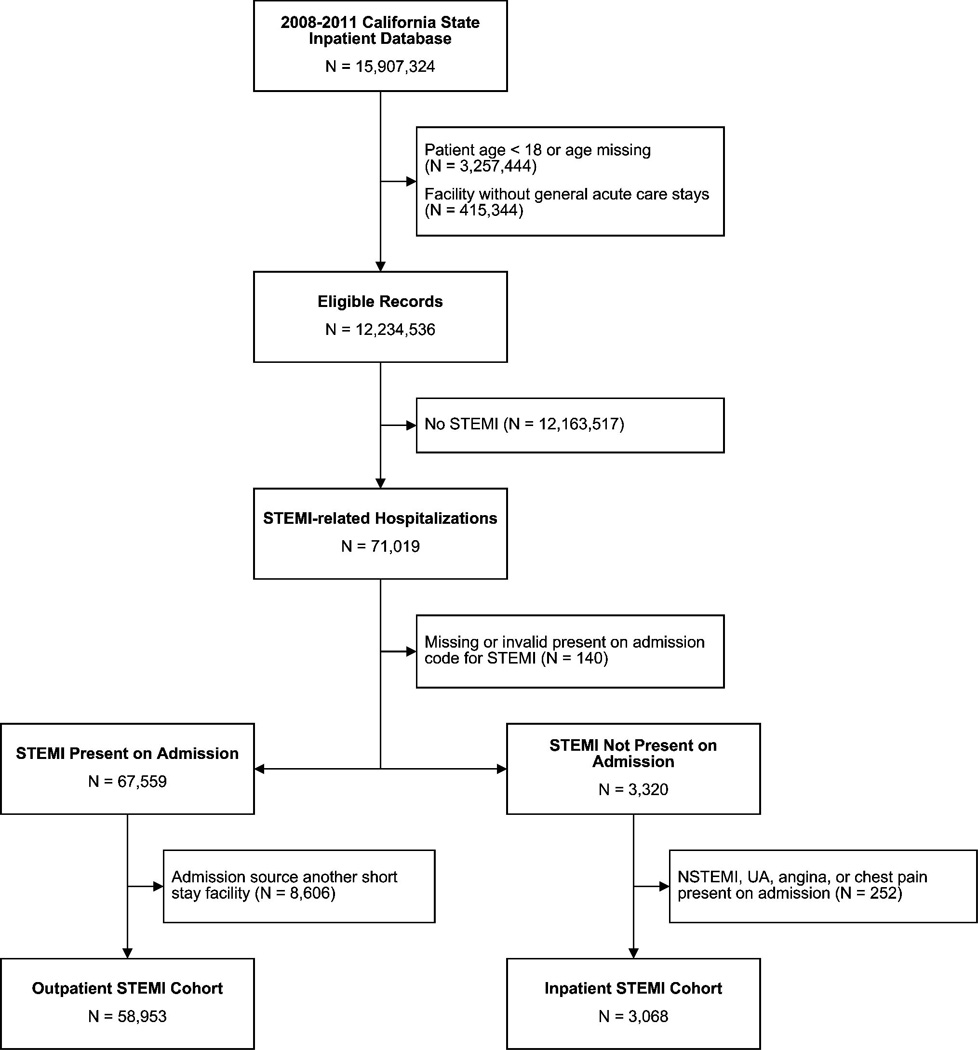
Flowchart of cohort identification [US = unstable angina, NSTEMI = non-STEMI].
Identification of cohort at risk of non-cardiac procedure-related inpatient-onset STEMI
In order to evaluate the association between surgical procedures and risk of inpatient-onset STEMI, we constructed a supplementary cohort, starting with all adult patients hospitalized in acute care hospitals. Patients listed as having ACS, angina, or chest pain present on admission were excluded. For the remaining patients, we examined ICD-9-CM procedure codes to identify receipt of non-cardiac surgical procedures listed in current ACC/AHA guidelines on perioperative cardiovascular care.9 Using these guidelines, ICD-9 procedure codes were assigned into three risk categories (low, intermediate and vascular/high risk) as well as cardiac surgeries (which were limited to the first two days following admission in an effort to identify cardiac surgeries likely preceding STEMI) by two investigators (H.B. and L.Z.) with review of assignments by a third (P.K.); a complete listing of grouped codes is provided in Supplementary Table 1. Admissions during which patients received multiple surgical procedures that fell into different categories were classified based on the highest risk surgical procedure. For patients who had a surgical procedure performed and developed a STEMI during the same hospitalization, the assumption was made that the STEMI occurred subsequent to the surgical procedure. It was felt unlikely that a surgical procedure would have been performed during the same hospitalization following a STEMI.
Identification of STEMI-related treatments, comorbid conditions, and other covariates
Using the data provided in CA-SID records, several additional variables were constructed. Using ICD-9-CM procedure codes, we identified potentially STEMI-related treatments provided during the stay, including PCI (00.66, 36.01, 36.02, 36.05, 36.06, 36.07, 36.09) and cardiac catheterization (37.22, 37.23, 88.5x). Comorbid conditions were identified by applying Elixhauser comorbidity criteria to all diagnosis codes listed as present on admission.10 The original formulation of the Elixhauser criteria excludes comorbidities related to the diagnosis-related group assigned to the inpatient stay; because the objective in this analysis was to identify conditions other than STEMI that were present on admission, we removed this exclusion.
Development of a model of in-hospital mortality risk
We modeled the association between inpatient mortality and patient age, gender, procedural risk category and comorbid conditions, among those patients in the California database who did not experience an inpatient-onset STEMI. Using the resultant regression model, we estimated the risk of inpatient death among those patients who did experience an inpatient-onset STEMI, and divided these patients into four quartiles of risk for ease of presentation. We then evaluated the association between mortality and the use of PCI in patients in the different quartiles and then fit regression models allowing for interactions between interventional treatment strategies and the quartiles of patient risk.
Statistical Analyses
Unadjusted comparisons between inpatient-onset and outpatient-onset STEMI patients were made using t-tests for continuous variables and chi-squared tests for categorical variables as appropriate. To evaluate adjusted comparisons between location of STEMI onset and treatment (PCI and cardiac catheterization), outcomes (in-hospital death and discharge to home), and resource use (length of stay and inpatient charges), regression models were constructed using logistic regression for treatment and outcome endpoints, a negative binomial model for the length of stay endpoint, and a generalized linear model with log link and gamma distribution for the charges endpoint. All models were adjusted for patient age, gender, comorbid conditions present on admission and hospital characteristics (as listed in table 1). Unadjusted associations between the rate of non-cardiac surgical risk class and incidence of inpatient-onset STEMI were assessed using chi-squared tests, while adjusted results were reported using logistic regression. In order to account for potential correlation of patients within hospitals, clustered standard errors were used in adjusted regression models.
Table 1.
Baseline Characteristics for STEMI-related hospitalizations in California, 2008–2011
| Overall (N=62,021) |
Outpatient- onset STEMI (N=58,953) |
Inpatient-onset STEMI (N=3,068) |
p | |
|---|---|---|---|---|
| N (%) | ||||
| Patient Characteristics | ||||
| Age (years; mean (SD)) | 65.2 (14.1) | 64.9 (14.1) | 71.5 (13.5) | <0.001 |
| Female | 20,316 (32.8%) | 18,865 (32.0%) | 1,451 (47.4%) | <0.001 |
| Race / Ethnicity | <0.001 | |||
| White | 37,701 (63.8%) | 35,787 (63.7%) | 1,914 (64.9%) | |
| Black | 3,106 (5.3%) | 2,928 (5.2%) | 178 (6%) | |
| Hispanic | 11,391 (19.3%) | 10,913 (19.4%) | 478 (16.2%) | |
| Asian | 5,069 (8.6%) | 4,756 (8.5%) | 313 (10.6%) | |
| Native American | 38 (0.1%) | 35 (0.1%) | 3 (0.1%) | |
| Other | 1,812 (3.1%) | 1,749 (3.1%) | 63 (2.1%) | |
| CAD Risk Factors | ||||
| Hypertension | 40,692 (65.6%) | 38,588 (65.5%) | 2,104 (68.6%) | <0.001 |
| Diabetes w/o chronic complications | 15,526 (25%) | 14,814 (25.1%) | 712 (23.2%) | 0.02 |
| Diabetes w/ chronic complications | 3,538 (5.7%) | 3,195 (5.4%) | 343 (11.2%) | <0.001 |
| Obesity | 7,582 (12.2%) | 7,279 (12.3%) | 303 (9.9%) | <0.001 |
| Current Smoker | 14,337 (23.1%) | 14,032 (23.8%) | 305 (9.9%) | <0.001 |
| Former Smoker | 8,445 (13.6%) | 7,964 (13.5%) | 481 (15.7%) | <0.001 |
| Major Comorbid Conditions | ||||
| Congestive heart failure | 13,456 (21.7%) | 12,546 (21.3%) | 910 (29.7%) | <0.001 |
| Valvular disease | 5,358 (8.6%) | 4,941 (8.4%) | 417 (13.6%) | <0.001 |
| Pulmonary circulation disease | 1,598 (2.6%) | 1,427 (2.4%) | 171 (5.6%) | <0.001 |
| Peripheral vascular disease | 5,056 (8.2%) | 4,490 (7.8%) | 466 (15.2%) | <0.001 |
| Paralysis | 1,313 (2.1%) | 1,134 (1.9%) | 179 (5.8%) | <0.001 |
| Other neurological disorders | 3,261 (5.3%) | 2,948 (5%) | 313 (10.2%) | <0.001 |
| Chronic pulmonary disease | 9,452 (15.2%) | 8,718 (14.8%) | 734 (23.9%) | <0.001 |
| Hypothyroidism | 4,861 (7.8%) | 4,483 (7.6%) | 378 (12.3%) | <0.001 |
| Renal failure | 7,880 (12.7%) | 7,075 (12%) | 805 (26.2%) | <0.001 |
| Liver disease | 1,104 (1.8%) | 964 (1.6%) | 140 (4.6%) | <0.001 |
| Acquired immune deficiency syndrome | 160 (0.3%) | 152 (0.3%) | 8 (0.3%) | 0.98 |
| Lymphoma | 296 (0.5%) | 257 (0.4%) | 39 (1.3%) | < 0.001 |
| Metastatic cancer | 738 (1.2%) | 552 (0.9%) | 186 (6.1%) | <0.001 |
| Solid tumor w/out metastasis | 921 (1.5%) | 811 (1.4%) | 110 (3.6%) | <0.001 |
| Peptic ulcer | 30 (0.1%) | 25 (0.1%) | 5 (0.2%) | 0.03 |
| Rheumatoid arthritis | 1,131 (1.8%) | 1,039 (1.8%) | 92 (3%) | <0.001 |
| Coagulopathy | 1,859 (3%) | 1,613 (2.7%) | 246 (8%) | <0.001 |
| Weight loss | 1,464 (2.4%) | 1,171 (2.0%) | 294 (9.6%) | <0.001 |
| Fluid and electrolyte disorders | 8,748 (14.1%) | 7,884 (13.4%) | 864 (28.2%) | <0.001 |
| Chronic blood loss anemia | 437 (0.7%) | 359 (0.6%) | 78 (2.5%) | <0.001 |
| Deficiency anemia | 8,144 (13.1%) | 7,296 (12.4%) | 848 (27.6%) | <0.001 |
| Depression | 2,907 (4.7%) | 2,694 (4.6%) | 213 (6.9%) | <0.001 |
| Psychosis | 1,286 (2.1%) | 1,175 (2.0%) | 111 (3.6%) | <0.001 |
| Alcohol abuse | 2,145 (3.5%) | 2,000 (3.4%) | 145 (4.7%) | <0.001 |
| Drug abuse | 1,906 (3.1%) | 1,842 (3.1)% | 64 (2.1%) | <0.001 |
| Hospital Characteristics | ||||
| PCI capability | 53,168 (85.7%) | 50,979 (86.5%) | 2,189 (71.4%) | <0.001 |
| Diagnostic cardiac catheterization only | 3,645 (5.9%) | 3,345 (5.7%) | 300 (9.8%) | <0.001 |
| Nocardiac catheterization capability | 5,208 (8.4%) | 4,629 (7.9%) | 579 (18.9%) | <0.001 |
| Facility Size (based on annual discharges) | <0.001 | |||
| Quartile 1 (lowest) | 419 (0.7%) | 340 (0.6%) | 79 (2.6%) | |
| Quartile 2 | 5,638 (9.1%) | 5,253 (8.9%) | 381 (12.4%) | |
| Quartile 3 | 16,667 (26.9%) | 15,821 (26.8%) | 846 (27.6%) | |
| Quartile 4 (highest) | 39,301 (63.4%) | 37,539 (63.7%) | 1,762 (57.4%) | |
P-values for comparison of outpatient-onset STEMI vs inpatient-onset STEMI by t-test for continuous variables and chisquared test for binary/categorical variables. Missing values in gender (59) and race (2904). ‘Other neurological disorders’ is a specific term defined by the Healthcare Cost and Utilization Project (HCUP). The mean and range for number of annual discharges was 1422 (172, 2228) for Quartile 1, 4561 (2249, 6111) for Quartile 2, 9627 (6112, 12680) for Quartile 3, 19392 (12762, 47502) for Quartile 4.
All inferential statistics were performed using an alpha level of 0.05. Significance testing was two-sided. Dataset construction was performed in SAS System, version 9.3 (SAS Institute, Cary, NC) and statistical analyses in Stata/SE, version 12.1 (Statacorp, College Station, TX). The University of North Carolina at Chapel Hill Institutional Review Board exempted this study from review.
RESULTS
Cohort characteristics
Between 2008 and 2011 in the state of California, there were approximately 12 million adult hospitalizations in acute care hospitals. After excluding patients who developed STEMI after being hospitalized for an ACS or had a STEMI present on transfer from another facility, 62021 patients were found to have had a STEMI that was either present on admission (outpatient-onset STEMI group) or occurred while hospitalized for a non-ACS condition (inpatient-onset STEMI group) from a total of 303 hospitals (Figure 1). Of these, 58953 (95.1%) were outpatient-onset STEMIs and 3068 (4.9%) were inpatient-onset STEMIs. The incidence of inpatient-onset STEMI was 2.7 per 10,000 admissions.
Comparison of inpatient-onset and outpatient-onset STEMI
Patients with inpatient-onset STEMI were older, more often female, and had more comorbidities including congestive heart failure, chronic lung disease, renal failure and peripheral vascular disease than patients with outpatient-onset STEMI (Table 1). The prevalence of hypertension was slightly higher, and the prevalence of diabetes without complication slightly lower, in the inpatient-onset STEMI group. The prevalence of diabetes with complications was more than twice as high in inpatient-onset STEMI compared to outpatient-onset STEMI.
Risks factors associated with inpatient-onset STEMI
Both procedural and patient-level factors were associated with onset of STEMI in hospitalized patients (Table 2). After adjustment, those patients who underwent any surgical procedure as part of their hospitalization had a higher risk of inpatient-onset STEMI compared to those that did not (OR 2.36, 95% CI, 2.17 to 2.58). The risk of inpatient-onset STEMI was lowest in patients with no procedure and highest in patients undergoing cardiac surgical procedures (Table 3). In total, 49.6% of inpatient-onset STEMIs occurred following a surgical procedure. Congestive heart failure, metastatic cancer, coagulopathy, low risk surgery, valvular disease and peripheral vascular disease were other variables associated with developing inpatient-onset STEMI. In adjusted models in which hospitals were divided into quartiles based on number of annual discharges, facility size was not associated with occurrence of inpatient-onset STEMI (p = 0.63)
Table 2.
Associations between patient demographic and clinical characteristics and occurrence of STEMI during hospitalizations for non-acute coronary syndrome conditions
| Adjusted Odds Ratio [95% CI] | P value | |
|---|---|---|
| Cardiac Surgery* | 24.44 [19.41, 30.78] | < 0.001 |
| High Risk/Vascular Surgery* | 3.48 [2.82, 4.30] | < 0.001 |
| Intermediate risk surgery* | 2.15 [1.4, 2.38] | < 0.001 |
| Low risk surgery* | 1.56 [1.37, 1.79] | < 0.001 |
| Age (per year) | 1.03 [1.03, 1.04] | < 0.001 |
| Female gender | 0.76 [0.71, 0.82] | < 0.001 |
| Comorbid Conditions** | ||
| AIDS | 1.41 [0.76, 2.61] | 0.28 |
| Chronic pulmonary disease | 1.10 [1.00, 1.21] | 0.04 |
| Coagulopathy | 1.58 [1.37, 1.82] | < 0.001 |
| Congestive heart failure | 1.71 [1.53, 1.91] | < 0.001 |
| Diabetes w/o chronic complications | 1.19 [1.09, 1.30] | < 0.001 |
| Diabetes w/ chronic complications | 1.26 [1.09, 1.45] | 0.002 |
| Fluid and electrolyte disorders | 1.29 [1.19, 1.40] | < 0.001 |
| Hypertension | 1.21 [1.10, 1.32] | < 0.001 |
| Hypothyroidism | 0.85 [0.76, 0.96] | 0.008 |
| Liver disease | 1.02 [0.84, 1.23] | 0.87 |
| Lymphoma | 1.15 [0.84, 1.57] | 0.39 |
| Metastatic cancer | 1.74 [1.50, 2.02] | < 0.001 |
| Obesity | 1.00 [0.89, 1.13] | 0.97 |
| Paralysis | 1.37 [1.18, 1.59] | < 0.001 |
| Peptic ulcer Disease | 2.05 [0.89, 4.76] | 0.09 |
| Peripheral vascular disease | 1.46 [1.31, 1.63] | < 0.001 |
| Pulmonary circulation disease | 0.94 [0.78, 1.12] | 0.48 |
| Renal failure | 1.15 [1.04, 1.26] | 0.005 |
| Rheumatoid arthritis | 1.14 [0.95, 1.38] | 0.17 |
| Solid tumor w/out metastasis | 1.23 [1.02, 1.48] | 0.03 |
| Valvular disease | 1.36 [1.21, 1.52] | < 0.001 |
| Weight loss | 1.26 [1.09, 1.45] | 0.002 |
Adjustment was made for the variables listed in the table, smoking status, facility characteristics, chronic blood loss anemia, deficiency anemia, psychosis, alcohol abuse, drug abuse and calendar year.
The comparator group is hospitalized patients who did not undergo surgery.
For all variables, comparator group were those patients without STEMI
Table 3.
Covariate-adjusted incidence of STEMI, stratified by ACC/AHA procedural risk classification (per 10000 admissions)
| No Surgery | 2.0 ± 0.1 |
| Low risk surgery* | 3.1± 0.2 |
| Intermediate risk surgery* | 4.2 ± 0.2 |
| High Risk/Vascular Surgery* | 6.9 ± 0.7 |
| Cardiac Surgery | 47.7 ± 5.2 |
Treatment, clinical outcomes and resource utilization of inpatient-onset STEMI
In unadjusted analyses, patients with inpatient-onset STEMI had worse outcomes and greater resource utilization than patients with outpatient-onset STEMI (Table 4). After adjustment for age, gender, co-morbidities and hospital characteristics, inpatient-onset STEMI patients were less likely to undergo cardiac catheterization (OR = 0.19; 95% CI, 0.16 to 0.21; p < 0.001) or PCI (OR = 0.23; 95% CI, 0.21 to 0.26; p < 0.001) than outpatient-onset STEMI (table 5). Inpatient-onset STEMI patients consumed greater resources as indicated by longer length of stay (multiplicative factor = 2.51; 95% CI, 2.35 to 2.69; p < 0.001) and inpatient charges (multiplicative factor = 2.09; 95% CI, 1.93 to 2.28; p < 0.001). Adjusted in-hospital mortality was more than three times as high for inpatient-onset STEMI (OR = 3.05; 95% CI, 2.76 to 3.38; p < 0.001) and patients were much less likely to be discharged home following an inpatient-onset STEMI (OR = 0.38; 95% CI, 0.34 to 0.42; p < 0.001).
Table 4.
Treatments and outcomes in STEMI patients depending on the location of onset
| Overall (N=62,021) |
Outpatient (N=58,953) |
Inpatient (N=3,068) |
Unadjusted OR |
Adjusted OR |
p | |
|---|---|---|---|---|---|---|
| N (%) or Mean (SD) | ||||||
| Inpatient Mortality (%) | 6,476 (10.4) | 5,446 (9.2) | 1,030 (33.6) | 4.95 [4.52, 5.43] | 3.05 [2.76,3.38] | <0.001 |
| Length of hospital stay (days) | 5.2 (7.6) | 4.7 (6.3) | 13.4 (17.8) | 2.83 [2.67, 3.01] | 2.51 [2.35,2.69] | <0.001 |
| Hospital charges ($1000s) | 134.5 (140.8) | 129.0 (129.8) | 245.0 (258.7) | 1.90 [1.76, 2.05] | 2.09 [1.93,2.28] | <0.001 |
| Patients discharged home (%) | 41,914 (67.6) | 40,880 (69.4) | 1,034 (33.7) | 0.22 [0.20, 0.25] | 0.38 [0.34,0.42] | <0.001 |
| Use of cardiac catheterization (%) | 46,918 (75.7) | 45,881 (77.8) | 1,037 (33.8) | 0.15 [0.13, 0.17] | 0.19 [0.16,0.21] | <0.001 |
| Use of PCI (%) | 38,979 (62.9) | 38,317 (65.0) | 662 (21.6) | 0.15 [0.13, 0.17] | 0.23 [0.21,0.26] | <0.001 |
Results presented as odds ratios for death, home, percutaneous coronary intervention (PCI), and cardiac catheterization and multiplicative effect (e.g., 2.0 = doubling) for length of stay and charges outcomes. Adjustment was made for patient age, gender, facility characteristics and comorbid conditions present on admission. PCI: Percutaneous Coronary Intervention. Missing values for mortality (2), Length of hospital stay (3), Hospital Charges (5043)
Table 5.
Use of PCI and mortality in inpatient-onset STEMI patients stratified by risk of in-hospital mortality
| Quartile 1 (N=766) |
Quartile 2 (N=766) |
Quartile 3 (N=766) |
Quartile 4 (N=766) |
|
|---|---|---|---|---|
| Predicted mortality rate mean (minimum – maximum) | 1.1% (0.2%–1.7%) | 2.4% (1.7%–3.2%) | 4.4% (3.2%–6.1%) | 12.8% (6.1%–58.2%) |
| Use of cardiac catheterization n (mean [95% confidence interval]) | 358 (46.7% [43.2%, 50.3%]) | 287 (37.5% [34.0%, 41.0%]) | 212 (27.7% [24.5%, 31.0%]) | 179 (23.4% [20.4%, 26.5%]) |
| Use of PCI n (mean [95% confidence interval]) | 242 (31.6% [28.3%, 35.0%]) | 184 (24.0% [21.0%, 27.2%]) | 127 (16.6% [14.0%, 19.4%]) | 109 (14.3% [11.8%, 16.9%]) |
| Mortality without PCI n (mean [95% confidence interval]) | 138 (26.3% [22.6%, 30.3%]) | 208 (35.7% [31.8%, 39.8%]) | 256 (40.0% [36.2%, 44.0%]) | 294 (44.8% [41.0%, 48.7%]) |
| Mortality with PCI n (mean [95% confidence interval]) | 26 (10.7% [7.1%, 15.3%]) | 39 (21.2% [15.5%, 27.8%]) | 30 (23.6% [16.5%, 32.0%]) | 36 (33.0% [24.3%, 42.7%]) |
The association between in-hospital mortality and patient age, gender, procedural risk category, and comorbid conditions was modeled among those patients in the California database who did not experience an inpatient STEMI. Using the resultant regression model, the risk of in-hospital death was determined among those patients with an inpatient STEMI and the patients were divided into four quartiles of risk. For all quartiles, mortality was higher without PCI than with PCI (p < 0.001). [PCI = percutaneous coronary intervention]
The association of PCI with survival
To determine whether the use of PCI and/or mortality in patients treated with PCI varied with risk, inpatient-onset STEMI patients were divided into quartiles of increasing risk of in-hospital mortality using a model developed from those patients in the California database who did not experience an inpatient-onset STEMI. The use of invasive procedures (cardiac catheterization and PCI) decreased in higher risk quartiles (Table 6). However, patients who received PCI had higher survival in all quartiles versus those that did not (Table 6). Specifically, the odds ratio of mortality associated with PCI in quartile 1 (lowest risk) was 0.26 (95% CI: 0.16, 0.40), in quartile 2 was 0.37 (95% CI: 0.28, 0.52), in quartile 3 was 0.34 (95% CI: 0.23, 0.50), and in quartile 4 was 0.57 (95% CI: 0.41, 0.79). A test of linear trend for differences across quartile was non-significant (p = 0.10); in pairwise comparisons only the comparison between quartile 4 and 1 was statistically significant (p = 0.003).
COMMENT
This multi-center study confirms previously published studies6,11,12 demonstrating increased mortality for patients who develop inpatient-onset STEMI compared to outpatient-onset STEMI. To the best of our knowledge, the present study is the largest of its kind and the only multi-center study specifically assessing the incidence and variables associated with outcomes of patients developing STEMI while hospitalized for a non-ACS condition.
In California between 2008 and 2011, patients developing inpatient-onset STEMI had a more than 3-fold increase in in-hospital mortality compared to outpatient-onset STEMI (33.6% versus 9.2%; p < 0.001). In our own recent single center study of patients developing inpatient-onset STEMI after admission for other non-ACS conditions, mortality was 39.6% for inpatient-onset STEMI versus 4% for outpatient-onset STEMI6. In the Maximal Individual TheRapy in Acute myocardial infarction (MITRA) study, which prospectively registered 5,888 patients with STEMI in 54 hospitals in Southwest Germany, inpatient-onset STEMI had a two-fold higher in-hospital mortality compared to outpatient-onset STEMI (27.3% versus 13.9%).11 Unlike the present study, the MITRA study included inpatient-onset STEMIs who were admitted with either stable or unstable angina. A retrospective study of 7,054 veterans hospitalized for acute MI (STEMI and non-STEMI) in 127 Veterans Affairs Hospitals between July 2003 and August 2004, found that the 792 (11.2 %) inpatient-onset acute MIs were at a much higher risk of in-hospital and 30-day mortality compared to outpatient-onset acute MI.13 Recently, data from 3,795 consecutive STEMI patients treated at a single center between March 2003 and January 2013 were reported.12 The 83 inpatient-onset STEMIs that were described had a higher 1-year mortality compared to outpatient-onset STEMIs that presented via emergency medical services (16.9% versus 10.3%).
The difference in mortality in the current study between inpatient-onset STEMI and outpatient-onset STEMI is at least partially related to those already hospitalized being older, having more comorbid conditions and having a concurrent illness or recent surgery. However, significant differences in outcomes remained after adjustment for age, gender and comorbidities. While it is impossible to completely adjust for confounders in an observational study, other potential reasons for differences in mortality should be considered. One of these is the lower utilization of cardiac catheterization and primary PCI in inpatient-onset STEMI. While primary PCI has not been studied in inpatient-onset STEMI, data from outpatient-onset STEMI show that reperfusion in general, and primary PCI in particular, improves outcomes.14,15 While the inpatient-onset STEMI population has a higher percentage of patients, compared to outpatient-onset STEMI, who are not candidates for primary PCI because of excessive risk of bleeding, acute neurological symptoms, family and/or patient wishes and/or severe comorbidities,6 there are few data to guide these decisions.
This study demonstrates that mortality associated with inpatient-onset STEMI progressively increased in patients deemed at higher risk (based upon a model developed from those patients in the California database who did not experience an inpatient-onset STEMI). Invasive procedures were used less frequently in inpatient-onset STEMI in higher risk quartiles but the use of PCI was associated with higher rates of survival in all risk quartiles, suggesting that in appropriately selected patients, PCI may be of benefit even among patients with comorbid conditions that increase their risk of mortality.
The question of how to improve outcomes and define optimum treatment in hospitalized patients who experience a STEMI is an area that merits more attention and concern. While there have been improvements in treatment times and clinical outcomes in outpatients who have onset of STEMI, few initiatives have focused on optimizing care of hospitalized patients with onset of STEMI after admission. Previous studies11–13, including our own6, point towards the likelihood that process measures, such as time from onset of symptoms to ECG and time from symptom onset to device deployment, play an important role in outcomes in this population. Extrapolation of data from outpatient-onset STEMI would suggest any benefit with reperfusion would be dependent on the rapidity of restoring flow.14,15 Thus, for patients who are candidates for reperfusion, it is likely that delays in initiating treatment have a negative impact on outcomes. In our earlier study, we found significant delays in recognition of inpatient-onset STEMI, obtaining an ECG, interpreting the ECG and making the decision to perform emergency coronary angiography.6 In contrast to these delays observed with recognition and decision-making, once the STEMI team was activated, there was no difference in reperfusion times between inpatient-onset and outpatient-onset STEMI. Garberich et al., reporting data from a single center registry of patients diagnosed with STEMI after hospital admission, showed that implementation of a standard STEMI protocol for inpatient-onset STEMI resulted in a reduction in in-hospital mortality (from 15.4% to 5.3%) with a moderate decrease in median reperfusion times (from 85 min to 67 min).11 These data demonstrate that systems designed to improve care of inpatient-onset STEMI can have a significant beneficial impact on mortality.
There is no regional or national database that collects information on process measures in inpatient-onset STEMI. In fact, large national databases set up for quality improvement specifically exclude patients that develop STEMI while already hospitalized. Development of a reporting infrastructure, either through existing databases or programs established for this purpose, is needed to enhance our understanding of inpatient-onset STEMI.
Multivariable analysis identified several ‘risk factors’ associated with inpatient-onset STEMI. There were the traditional risk factors associated with cardiovascular disease including age, male gender, diabetes, hypertension, and peripheral vascular disease. There were also several factors that have not previously been associated with acute MI including paralysis, hypothyroidism, weight loss and metastatic cancer. These results remained significant after adjustment for age, gender and comorbidities. Further studies are needed to define what role these conditions play in increasing the risk of acute coronary thrombosis.
We found that the risk of inpatient-onset STEMI increased with the complexity of surgical procedures as defined by the 2007 ACC/AHA peri-operative guidelines (unchanged in the 2009 focused update).9 These results mimic studies designed to identify patients at risk for peri-operative myocardial infarction and provide further evidence of the discriminative power of the categories defined by the guidelines.
Limitations
Our study has several limitations. It is a retrospective, observational analysis, and identification of STEMI cases and location of onset were based on administrative data rather than adjudicated endpoints. The dataset does not have information on admitting diagnoses, elective versus urgent admission or on mortality following discharge. It is possible that the numbers presented here underrepresent the problem as patients with inpatient-onset STEMI might have died prior to diagnosis. Unobserved case mix measures likely confound the estimated association between inpatient-onset STEMI and mortality. If the unobserved case mix severity is greater for inpatient STEMI, then our results may overestimate the effect of having an inpatient STEMI on mortality and other outcomes. Furthermore, incomplete coding of comorbid conditions on hospital claims may limit our ability to completely control for severity of disease. The estimated associations remain large however even after adjustment for observed covariates, suggesting that some portion of the difference in outcomes may be due to delayed recognition and/or lack of revascularization in inpatient STEMI. The database does not have information on cause specific mortality, so it is unknown whether mortality was related to the STEMI. The most recent data in the CA-SID at the time of this study were from 2011 and it is unknown whether the study findings reflect current outcomes. We chose to focus on PCI as a reperfusion strategy because the limitations of the administrative database prevented us from determining how many STEMI patients were treated with thrombolytic therapy. Thrombolytic therapy is commonly used to treat select outpatient-onset STEMI at facilities that do not have PCI capability. Unfortunately, the limitations of the database also prevented us from determining how many inpatient-onset STEMI would not have been candidates for thrombolytic therapy because of elevated bleeding risk.
CONCLUSIONS
In this multi-center, observational study, approximately 5% (2.7 per 10,000 admissions) of all STEMIs occurred in patients hospitalized for non-ACS conditions. Patients who developed STEMI while hospitalized for a non-ACS condition, compared to those with onset of STEMI as an outpatient, were less likely to undergo invasive testing or intervention and had a higher in-hospital mortality rate.
Supplementary Material
ACKNOWLEDGEMENTS
The California State Inpatient Database is a product of the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality, in partnership with the California Office of Statewide Health Planning and Development. Dr. Federspiel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
FUNDING SOURCES
Data acquisition and Dr. Federspiel’s effort were supported by grants F30-HL110483 from the National Heart, Lung, and Blood Institute and T32-GM008719 from the National Institute of General Medical Sciences. The funding organizations had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Footnotes
Presented in abstract form at the American Heart Association Scientific Sessions 2013
DISCLOSURES
None
REFERENCES
- 1.Jollis JG, Roettig ML, Aluko AO, et al. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA. 2007 Nov 28;298(20):2371–2380. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 2.Krumholz HM, Bradley EH, Nallamothu BK, et al. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008 Feb;1(1):97–104. doi: 10.1016/j.jcin.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation. 2007 Jul 10;116(2):217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Herrin J, Miller LE, et al. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011 Aug 30;124(9):1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (acute coronary treatment and intervention outcomes network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circulation. Cardiovascular quality and outcomes. 2009 Sep;2(5):491–499. doi: 10.1161/CIRCOUTCOMES.108.847145. [DOI] [PubMed] [Google Scholar]
- 6.Dai X, Bumgarner J, Spangler A, Meredith D, Smith SC, Stouffer GA. Acute ST-elevation myocardial infarction in patients hospitalized for noncardiac conditions. Journal of the American Heart Association. 2013 Apr;2(2):e000004. doi: 10.1161/JAHA.113.000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases (SID) Rockville, MD: Agency for Healthcare Research and Quality; 2005–2009. [PubMed] [Google Scholar]
- 8.McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PLoS One. 2014 Mar 28;9(3):e92286. doi: 10.1371/journal.pone.0092286. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. J. Am. Coll. Cardiol. 2007 Oct 23;50(17):e159–e241. doi: 10.1016/j.jacc.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med. Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Zahn R, Schiele R, Seidl K, et al. Acute myocardial infarction occurring in versus out of the hospital: patient characteristics and clinical outcome. Maximal Individual TheRapy in Acute Myocardial Infarction (MITRA) Study Group. J. Am. Coll. Cardiol. 2000 Jun;35(7):1820–1826. doi: 10.1016/s0735-1097(00)00629-x. [DOI] [PubMed] [Google Scholar]
- 12.Garberich RF, Traverse JH, Claussen MT, et al. ST-Elevation Myocardial Infarction Diagnosed After Hospital Admission. Circulation. 2014 Mar 18;129(11):1225–1232. doi: 10.1161/CIRCULATIONAHA.113.005568. [DOI] [PubMed] [Google Scholar]
- 13.Maynard C, Lowy E, Rumsfeld J, et al. The prevalence and outcomes of in-hospital acute myocardial infarction in the Department of Veterans Affairs Health System. Arch Intern Med. 2006 Jul 10;166(13):1410–1416. doi: 10.1001/archinte.166.13.1410. [DOI] [PubMed] [Google Scholar]
- 14.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004 Mar 16;109(10):1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 15.McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 2006 Jun 6;47(11):2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


