Abstract
BACKGROUND
The predictive value of ascending aortic distensibility (AAD) for mortality and hard cardiovascular disease (CVD) events is not fully established.
OBJECTIVES
We sought to assess the utility of AAD to predict mortality and incident CVD events beyond conventional risk factors in the Multi-Ethnic Study of Atherosclerosis (MESA).
METHODS
AAD was measured with magnetic resonance imaging at baseline in 3,675 MESA participants free of overt CVD. Cox proportional-hazards regression was used to evaluate risk of death, heart failure (HF), and incident CVD in relation to AAD, CVD risk factors, indices of subclinical atherosclerosis, and Framingham risk score.
RESULTS
There were 246 deaths and 171 hard CVD (myocardial infarction, resuscitated cardiac arrest, stroke and cardiovascular [CV] death) and 88 HF events over a median 8.5-year follow-up. Decreased AAD was associated with increased all-cause mortality with a hazard ratio (HR) for the first verus fifth quintile of AAD of 2.7 (p = 0.008) independent of age, sex, ethnicity, other CVD risk factors, and indices of subclinical atherosclerosis. Overall, subjects with lowest AAD had an independent 2-fold risk of hard CVD events. Decreased AAD was associated with CV events in low-to-intermediate CVD risk individuals with an HR for the first quintile of AAD of 5.3 (p = 0.03) as well as with incident HF but not after full adjustment.
CONCLUSIONS
Decreased proximal aorta distensibility significantly predicts all-cause mortality and hard CV events among individuals without overt CVD. AAD may help refine risk stratification, especially among asymptomatic, low-to-intermediate risk individuals.
Keywords: aortic stiffness, cardiovascular risk, magnetic resonance imaging, mortality
Introduction
Conventional risk factors associated with atherosclerosis are major determinants of cardiovascular disease (CVD). Recently, a complement to this classic view was proposed and termed the vascular aging continuum, starting from age-related arterial stiffening leading to cardiac disease and heart failure (HF) and also to microvascular disease of the brain and kidneys with resulting disability and eventually death (1).
The direct measurement of aortic stiffness as a marker of early arterial damage may be important. Although the usual onset of CVD appears in middle and older age, a large body of evidence suggests that subclinical vascular and cardiac alterations start much earlier in life (2–6). Global arterial stiffness measured as carotid-femoral pulse wave velocity (PWV) may independently predict incident cardiovascular events among patients as well as in the general population separate from traditional CVD risk factors (7). Subsequently, reference values and determinants of PWV in healthy individuals, with and without CVD risk factors, have been described for large populations (8) and recently included in guidelines (9). In healthy humans, reduced ascending aortic distensibility has been shown to be an early marker of subclinical vascular alteration. However, little is known of the prognostic value of altered proximal aortic function, which is responsible for most of the mechanical buffering and cushioning in the circulatory system, thus influencing ventricular-vascular coupling (10). Recently, Maroules et al. reported modest associations of aortic distensibility with a composite of soft and hard cardiovascular endpoints in the Dallas Heart Study (11), while thoracic aorta compliance, measured by transesophageal echocardiography, may be comparable to carotid-femoral PWV for predicting mortality (12).
We postulated that a direct measure of aortic function – ascending aortic distensibility (AAD) – using magnetic resonance imaging (MRI) (13),, may be directly related to hard cardiovascular events and mortality, independent of classic CVD risk factors. Thus, the aim of our study was to determine the prognostic value of AAD beyond established indices of subclinical atherosclerosis and conventional risk factors included in the global Framingham risk score. To this end, we measured aortic distensibility and ascertained the post-scan occurrence of hard CVD events in participants within the Multi-Ethnic Study of Atherosclerosis (MESA) cohort.
METHODS
The MESA study (14) is a population-based sample of 6,814 men and women aged 45 to 84 years without clinical CVD at time of enrollment who identified themselves as white, African-American, Hispanic, or Chinese from 6 U.S. communities (Baltimore, New York, Minneapolis, Winston-Salem, Los Angeles, and Chicago). Out of 5,098 participants who took part in the cardiovascular MRI exam, 3,675 subjects underwent suitable AAD measurements for analysis. The study was approved by the institutional review boards at all recruiting field centers and all participants provided written informed consent.
AORTIC AND CARDIAC MRI
MRI was performed using 1.5-T whole-body MRI scanners as previously described (15). In summary, gradient echo phase-contrast cine MRI with electrocardiographic gating was performed to evaluate aortic distensibility. Images of the ascending and descending aorta were obtained in the transverse plane perpendicular to the aortic lumen at the level of the right pulmonary artery. Imaging parameters included repetition time: 10 ms; echo time: 1.9 ms; field of view: 34 cm; slice thickness: 8 mm; matrix: 256 × 224; temporal resolution: 20 ms; encoding velocity: 150 cm/s; and bandwidth: 32 kHz.
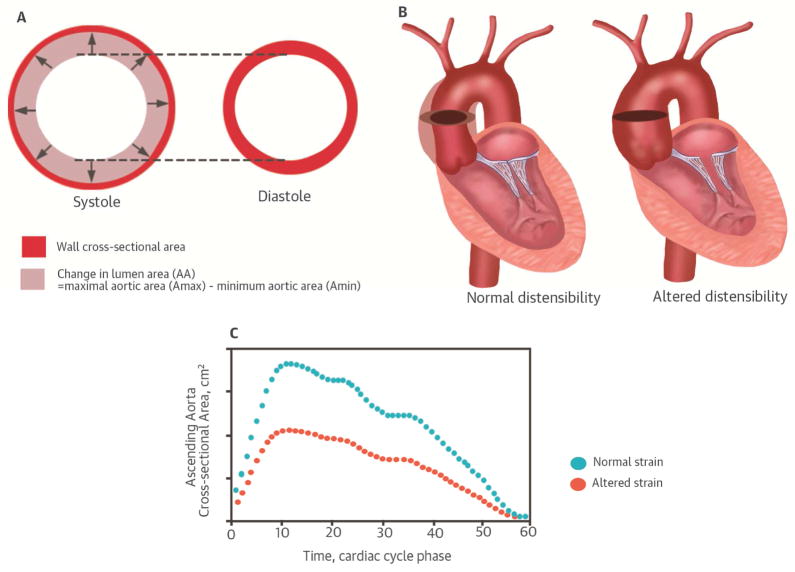
As illustrated in Figure 1, cross-sectional lumen areas of the ascending aorta were determined using a semi-automated contouring method with previously reported inter-reader reproducibility (16). The maximal (Amax) and minimal (Amin) aortic areas and change in aortic area defined as ΔA = (Amax-Amin) were used to calculate the distensibility of the ascending aorta (AAD) in each subject as follows, with PP being pulse pressure (in mmHg): AAD = ΔA/(Amin x PP) in 10−3 mmHg−1.
FIGURE 1. Principle of local aortic stiffness: Distensibility of the Ascending Aorta.
During systole, the ascending aorta stores most of the left ventricular stroke volume, which is released downstream during diastole thereby transforming a pulsatile flow into a steadier flow. This cushioning effect allows minimizing energy expenditure. The relative change in aortic lumen area divided by pulse pressure defines distensibility (A). Comparative illustration of preserved (left) and altered (right) distensibility of the ascending aorta (B) and corresponding cross-sectional area to cardiac cycle time curves for preserved (blue) and altered (red) aortic distensibility (C).
Cardiac MRI was performed with measurements of left ventricular (LV) mass as previously described (17).
CVD RISK FACTORS AND MEASURES OF SUBCLINICAL ATHEROSCLEROSIS
During baseline examination, all participants completed standardized questionnaires to obtain information about smoking history, pack years of smoking, medication usage, diagnosis of high cholesterol, and diabetes. Height and weight were measured and resting systolic (SBP) and diastolic (DBP) blood pressures were measured 3 times with participants in the seated position with an automated oscillometric sphygmomanometer. The average of the last 2 measurements was used in analysis. Mean brachial blood pressure (MBP) was calculated as (2 DBP + SBP)/3. The ankle brachial pressure index (ABI) was calculated by dividing SBP at the ankle by brachial SBP as reported in (18). Heart rate was monitored and recorded at the time of the MRI exam. Total and high-density lipoprotein (HDL) cholesterol and glucose levels were measured from blood samples obtained after a 12-hour fast. Diabetes mellitus was defined as fasting glucose ≥126 mg/dl or use of insulin or oral hypoglycemic medication. Among those without diabetes, impaired fasting glucose was defined as fasting glucose from 100 to 125 mg/dl. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or current use of antihypertensive medications. Carotid artery intima-media thickness (IMT), a noninvasive measure of subclinical atherosclerosis, was reported to further characterize subclinical atherosclerosis. A composite Z score for overall maximal IMT was calculated by summing the two carotid IMT sites after normalization by the standard deviation of each measure and divided by the standard deviation of the sum (19). IMT of the right and left near and far walls of the common and internal carotid artery were measured by B-mode echography. Mean coronary artery calcium (CAC) score was measured by computed tomography as previously described (19).
The sex-specific global CVD Framingham 10-year risk was calculated as described by D’Agostino et al. (20), based on these risk factors at baseline: age, total cholesterol, HDL cholesterol, SBP, antihypertensive treatment, smoking, and diabetes.
FOLLOW-UP FOR CVD EVENTS AND DEATHS
Participants were followed for death and incident CVD events for an average 8.5 years from baseline examination. In addition to four follow-up MESA study examinations, a telephone interviewer contacted each participant every 9 to 12 months to inquire about all interim hospital admissions, CVD outpatient diagnoses, and deaths. Medical records were available for an estimated 99% of hospitalized CVD events and information on 97% of outpatient CVD diagnostic encounters. Events and incidence dates were adjudicated by 2 blinded physicians from the MESA study events committee using pre-specified criteria. Adjudication of events has been previously detailed (17). Hard CVD events in MESA were required to be symptomatic and included myocardial infarction (MI), resuscitated cardiac arrest, stroke, and cardiovascular death. Incident heart failure (HF) events were recorded. All deaths were identified. For potential CVD deaths, cause was assigned through committee review. For other deaths, the underlying cause was obtained through state or city vital statistics departments.
STATISTICAL ANALYSIS
Participant characteristics were reported according to outcome as percentages for categorical variables and means and standard deviations for continuous variables. Baseline characteristics were compared separately between both outcome groups (death and incident CVD) and the group without events using a Student t test for continuous variables and a chi-square test for categorical variables.
The relationships between AAD and time-to-death/time-to-CVD events and HF events were studied using univariate and multivariate Cox regression models. For the definition of time-to-death, subjects who were alive before loss-to-follow-up were treated as right censored. For the definition of time-to-CVD or HF events, subjects who did not have events (including CVD death) before loss-to-follow-up were treated as right censored. Univariate Cox proportional hazards regression models were first fitted for each time-to-event (time-to-death, time-to-CVD, time-to-HF) variable for quintiles of AAD without adjusting other covariates, as the effects of AAD on the hazard functions were nonlinear. Table 1 presents distribution of AAD values in quintiles. Subsequently, we studied the predictive value of AAD by quintiles for mortality, hard CVD, and HF compared to 1) constitutional factors; 2) cardiovascular (CV) risk factors; 3) measures of subclinical atherosclerosis individually and together (ABI, carotid IMT, CAC); and 4) LV hypertrophy (LVH). ABI was considered abnormal when <1.0 or ≥1.4 as previously determined to be related to outcome in MESA (18). LVH was defined as LV mass ≥90th percentile in the study population (197 g). We considered a 10-year CVD risk to be low or intermediate when <10%, corresponding to our cohort’s median of risk, and high when ≥10%. Constitutional variables of adjustment for multivariate Cox regression models included: age category, sex, weight, height, and ethnicity. CV risk factors used in further adjusting the models included MBP, antihypertensive medication (yes/no), diabetes (yes/no), total and HDL cholesterol, and cigarette smoking in pack-years. Kaplan-Meier estimates of the cumulative event-free distribution functions were calculated for time-to-mortality and time-to-CVD according to extreme quintiles of AAD. Values of p < 0.05 are considered statistically significant. Confidence intervals (CIs) are expressed as 95% CIs. All analyses were performed using Stata 12C (StataCorp, College Station, Texas).
TABLE 1.
Distribution of AAD Values by Quintiles
| AA Distensibility, 10−3 mm Hg−1 | Min | 25% | 50% | 75% | Max |
|---|---|---|---|---|---|
| AAD quintile 1 | 0.14 | 0.62 | 0.75 | 0.87 | 0.97 |
| AAD quintile 2 | 0.97 | 1.06 | 1.15 | 1.25 | 1.34 |
| AAD quintile 3 | 1.34 | 1.47 | 1.58 | 1.71 | 1.84 |
| AAD quintile 4 | 1.84 | 2.00 | 2.16 | 2.35 | 2.60 |
| AAD quintile 5 | 2.60 | 2.88 | 3.24 | 3.84 | 6.60 |
AAD = ascending aorta distensibility
RESULTS
PARTICIPANT CHARACTERISTICS AND CVD RISK PROFILE ACCORDING TO OUTCOME
Our analysis included the 3,675 MESA participants who had aortic distensibility measured by MRI. There were 246 deaths, 171 hard CV events, and 88 incident HF events over a median 8.5 years of follow-up. The participants’ mean age at baseline was 60 ± 10 (range: 44 to 84 years). Of the participants, 54% were female, 11% Chinese-American, 29% African American, 17% Hispanic, and 43% Caucasian. Table 2 shows baseline characteristics of participants according to events. MESA participants with aortic data tended more often to be Caucasian or African-American and female and, overall, have a moderately lower risk profile and subclinical atherosclerosis burden (IMT, ABI, CAC) than participants without aortic MRI. Although statistically significant in large population samples, these differences do not seem to be within clinically relevant ranges.
TABLE 2.
Baseline Characteristics of MESA Participants According to Outcome
| Participants without aortic MRI n = 3,137 | Participants with aortic MRI n = 3,675 | No Event n = 3,316 | Deaths n = 246 | p Value† | Incident CVD n = 171 | p Value‡ | |
|---|---|---|---|---|---|---|---|
| Ethnicity | |||||||
| Caucasian | 33% | 43%* | 43% | 40% | 0.33 | 52% | 0.013 |
| Chinese American | 13% | 11%* | 11% | 5% | 0.002 | 4% | 0.004 |
| African American | 26% | 29%* | 29% | 42% | <0.001 | 29% | 0.87 |
| Hispanic | 28% | 17%* | 17% | 13% | 0.11 | 15% | 0.50 |
| CV Risk Profile | |||||||
| Age, yr | 64 ± 10 | 61 ± 10 | 60 ± 10 | 69 ± 10 | <0.001 | 67 ± 7 | <0.001 |
| Male/Female | 49%/51% | 46%/54% | 44%/56 | 57%/43 | <0.001 | 57%/43 | 0.002 |
| Height, cm | 166 ± 10 | 167 ± 10 | 167 ± 10 | 167 ± 10 | 0.95 | 168 ± 10 | 0.47 |
| Weight, kg | 80 ± 19 | 78 ± 16* | 78 ± 16 | 78 ± 17 | 0.67 | 81 ± 15 | 0.11 |
| BMI, kg/m−2 | 29 ± 6 | 28 ± 5* | 28 ± 5 | 28 ± 5 | 0.60 | 29 ± 5 | 0.15 |
| Hypertension, % | 49% | 42%* | 40% | 59% | <0.001 | 63% | <0.001 |
| Hypertension | 40% | 35%* | 33% | 51% | <0.001 | 51% | <0.001 |
| Medication, % | |||||||
| Smoking status, % | |||||||
| Never | 49% | 51% | 52% | 40% | <0.001 | 47% | 0.26 |
| Former | 38% | 36%* | 35% | 38% | 0.12 | 30% | 0.35 |
| Active | 13% | 13% | 12% | 21% | <0.001 | 23% | <0.001 |
| Diabetes status, % | |||||||
| Normal | 68% | 78%* | 79% | 65% | <0.001 | 63% | <0.001 |
| IFG | 17% | 12%* | 11% | 17% | 0.004 | 13% | 0.54 |
| Diabetes | 15% | 10%* | 10% | 17% | <0.001 | 22% | <0.001 |
| Total cholesterol, mg/dl | 194 ± 37 | 194 ± 35 | 194 ± 34 | 189 ± 37 | 0.01 | 197 ± 36 | 0.22 |
| HDL cholesterol, mg/dl | 50 ± 14 | 52 ± 15* | 52 ± 15 | 50 ± 15 | 0.104 | 48 ± 13 | <0.001 |
| Framingham 10-yr | 16.1 ± 9.7 | 13.1 ± 9.3* | 12.3 ± | 20.5 ± | <0.001 | 21.1 ± | <0.001 |
| Global risk, % | |||||||
| Seated brachial blood Pressures | |||||||
| SBP, mm Hg | 129 ± 22 | 125 ± 21 | 124 ± 21 | 133 ± 25 | <0.001 | 136 ± 23 | <0.001 |
| DBP, mm Hg | 72 ± 10 | 72 ± 10 | 72 ± 10 | 72 ± 11 | 0.96 | 75 ± 11 | <0.001 |
| PP, mm Hg | 57 ± 18 | 53 ± 17* | 52 ± 16 | 61 ± 19 | <0.001 | 61 ± 18 | <0.001 |
| Mean BP, mm Hg | 91 ± 13 | 90 ± 13 | 89 ± 12 | 92 ± 14 | <0.001 | 95 ± 14 | <0.001 |
| Brachial blood Pressures during MRI | |||||||
| SBP, mm Hg | n/a | 134 ± 21 | 133 ± 20 | 144 ± 23 | <0.001 | 143 ± 221 | <0.001 |
| DBP, mm Hg | n/a | 77 ± 13 | 77 ± 13 | 78 ± 12 | 0.51 | 79 ± 13 | 0.04 |
| PP, mm Hg | n/a | 57 ± 17 | 56 ± 17 | 66 ± 18 | <0.001 | 64 ± 17 | <0.001 |
| Mean BP, mm Hg | n/a | 96 ± 14 | 96 ± 14 | 100 ± 14 | <0.001 | 101 ± 14 | <0.001 |
| Heart rate, beats/min | 63.3 ± 9.9 | 62.9 ±* | 62.8 ± | 63.9 ±.1 | 0.09 | 64.5 ± 10.8 | 0.03 |
| Maximal internal arotid IMT, mm | 0.89 ± 0.20 | 0.86 ± 0.18* | 0.85 ± 0.18 | 0.96 ± 0.22 | <0.001 | 0.92 ± 0.17 | <0.001 |
| ABI | 1.114 ± 0.125 | 1.112 ± 0.116* | 1.118 ± 0.107 | 1.045 ± 79 | <0.001 | 1.062 ± 0.173 | <0.001 |
| CAC score, median (IQR) | 5 (0–120) | 0 (0–62)* | 0 (0–42) | 52 (0–300) | <0.001 | 93 (10–308) | <0.001 |
| LV mass by MRI, g | n/a | 120 ± 29 | 119 ± 28 | 129 ± 34 | <0.001 | 130 ± 32 | <0.001 |
| Ascending Aortic Function | |||||||
| AAD, 10−3 mmm Hg−1 | n/a | 1.86 ± 1.31 | 1.91 ± 1.34 | 1.36 ± 0.69 | <0.001 | 1.50 ± 1.04 | <0.001 |
Values are mean ± SD or % unless otherwise indicated.
p<0.05 for the difference between groups with and without available aortic MRI data in MESA;
p Value for the significance of the difference between group without events and the mortality group;
p Value for the significance of the difference between group without events and the group with incident CVD.
ABI = ankle brachial index; BMI = body mass index; BP = blood pressure; CAC = coronary artery calcium; CV = cardiovascular; CVD = cardiovascular disease; DBP = diastolic blood pressure; HDL = high-density lipoprotein; IFG = impaired fasting glucose; IMT = intima media thickness; IQR = interquartile range; LV = left ventricular; MRI = magnetic resonance imaging; PP = pulse pressure; SBP = systolic blood pressure; other abbreviations as in Table 1.
Overall, the most frequent hard CV events were MI (n = 85), stroke (n = 63), and CV death (n = 52) (multiple events possible). There was, proportionally to the group without incident CVD or death, an increased proportion of Caucasians among those who developed CVD and a higher proportion of African-Americans among those who died. Subjects who died were older, more often male, hypertensive, active smokers, and diabetic or with impaired fasting glucose; body size, body mass index (BMI), and heart rate were not different between the 2 groups. Subjects who died had slightly higher total cholesterol but similar HDL cholesterol and increased SBP and PP but similar DBP than subjects without events. Subjects with incident CVD were older, more often male, hypertensive, active smokers, and diabetic, plus more likely to have increased weight (+10 kg on average) and BMI (+1 point) than subjects without events. While total cholesterol was not increased in the CVD group, HDL cholesterol was significantly lower and all components of blood pressure (systolic, diastolic, pulse pressure) were increased compared to the group without events and heart rate was slightly higher. AAD and ABI were lower and carotid IMT, CAC, and LV mass significantly higher in both event groups compared to participants without events (Table 2).
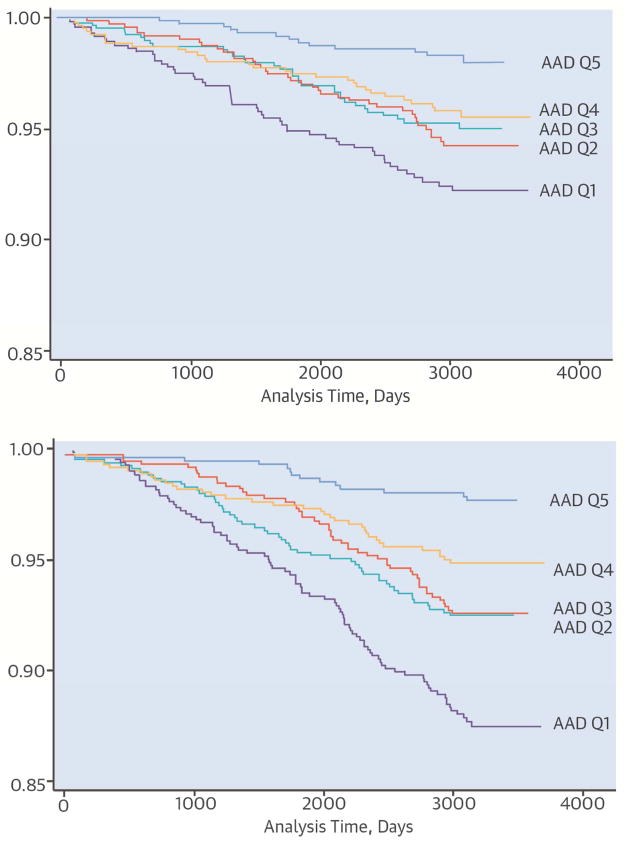
RELATIONSHIP OF AAD TO MORTALITY
The absolute rate of death was 9.3% and incidence rate 0.04 per 1,000 person-years in participants with the lowest levels of aortic distensibility (Q1) compared to 1.5% and 0.003 per 1,000 person-years in participants with greatest aortic distensibility (Q5) (p < 0.001). The Kaplan-Meier analysis (Central Ilustration, upper panel) showed a significant decrease in survival in the Q1 group compared to participants with the most preserved aortic distensibility (p < 0.001). The difference in survival between Q1 and Q5 of AAD was marked and consistently significant over time. The hazard ratio (HR) for death among Q1 participants was significantly increased at 6.5 compared to Q5 participants in univariate analysis (p < 0.001), 2.7 after adjustment for age, sex, ethnicity, and body size and 2.7 after further adjustment for smoking, antihypertensive medication, diabetes, and MBP (all p < 0.01; Table 3). This result was not substantially changed when adjusting for brachial systolic or PP instead of mean pressure. Furthermore, this result remained consistent in the fully-adjusted model after further individual or grouped adjustment for ABI, presence of CAC, carotid IMT, and presence of LVH (all p ≤ 0.01; Table 3).
TABLE 3.
Relationship of Proximal Aortic Stiffness to Incident Mortality
| Cox Models for All-cause Mortality
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted Model 1 | Adjusted Model 2 | Adjusted Model 3 | |||||
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| AAD quintile 1 | 6.5 (2.4–12.3) | <0.001 | 2.7 (1.3–5.2) | 0.005 | 2.7 (1.3–5.7) | 0.008 | 2.3 (1.2–4.4) | 0.009 |
| AAD quintile 2 | 4.0 (2.1–7.7) | <0.001 | 1.9 (1.0–3.9) | 0.07 | 2.1 (0.9–3.0) | 0.06 | 1.7 (0.9–3.3) | 0.11 |
| AAD quintile 3 | 4.1 (2.1–8.0) | <0.001 | 2.5 (1.3–5.0) | 0.007 | 2.6 (1.3–5.6) | 0.01 | 2.2 (1.2–4.3) | 0.01 |
| AAD quintile 4 | 2.7 (1.4–5.5) | 0.004 | 2.1 (1.0–4.2) | 0.04 | 2.2 (1.1–4.7) | 0.03 | 1.9 (1.0–3.7) | 0.04 |
| AAD quintile 5 | 1.0 (reference) | 1.0 (reference) | ||||||
|
| ||||||||
| ABI (<1.0 or ≥1.4) | 2.6 (2.0–3.5) | <0.001 | 2.1 (1.6–2.9) | <0.001 | 1.9 (1.4–2.6) | <0.001 | 1.8 (1.3–2.4) | <0.001 |
| AAD quintile 1 | 6.0 (3.3–10.7) | <0.001 | 2.8 (1.5–5.1) | 0.001 | 2.5 (1.3–4.7) | 0.005 | ||
|
| ||||||||
| Carotid IMT | 1.4 (1.3–1.6) | <0.001 | 1.4 (1.2–1.6) | <0.001 | 1.3 (1.2–1.5) | <0.001 | 1.1 (0.6–2.3) | 0.36 |
| AAD quintile 1 | 2.2 (1.1–4.3) | 0.02 | 2.3 (1.2–4.6) | 0.01 | 2.5 (1.2–5.3) | 0.01 | ||
|
| ||||||||
| CAC (present) | 2.4 (1.8–3.3) | <0.001 | 1.5 (1.0–2.1) | 0.03 | 1.5 (1.1–2.1) | 0.02 | 1.3 (1.0–1.9) | 0.07 |
| AAD quintile 1 | 5.0 (2.6–9.5) | <0.001 | 2.5 (1.2–4.9) | 0.009 | 2.7 (1.3–5.6) | 0.009 | ||
|
| ||||||||
| LVH | 1.6 (1.1–2.3) | 0.02 | 1.7 (1.1–2.7) | 0.01 | 1.7 (1.1–2.7) | 0.01 | ||
| AAD quintile 1 | 6.2 (3.3–11.7) | <0.001 | 2.4 (1.2–4.7) | 0.01 | 2.6 (1.2–5.5) | 0.01 | ||
AAD Quintile 1 corresponds to highest and Quintile 5 to lowest aortic stiffness. Adjustment was performed for the following risk factors: Model 1 = age, sex, weight, height, ethnicity; Model 2 = Model 1 + mean BP, smoking, antihypertensive medication, total cholesterol, HDL cholesterol and diabetes; individual tests of AAD vs. measures of atherosclerosis ABI, carotid IMT, presence of CAC defined as Agatston score >0, and LV hypertrophy defined as LV mass above 90th percentile are provided. Model 3 = Model 2 + adjustment for all measures of subclinical atherosclerosis (ABI, IMT, CAC).
RELATIONSHIP OF AAD TO CVD EVENTS
The absolute and incident rates of hard CVD were respectively 6.7% and 0.03 per 1,000 person-years in Q1 participants compared to 1.4% and 0.005 per 1000 person-years in Q5 participants (p < 0.001). The Kaplan-Meier analysis showed a significant decrease in CVD-free survival in the Q1 group compared to subjects with preserved aortic distensibility (Central Illustration, Lower panel). The difference in incident CVD between Q1 and Q5 of AAD was constant, notable, and significant over time. However, some degree of nonlinearity in HR distribution was present across intermediate quintiles of AAD. The HR for CVD in relationship to the degree of aortic stiffness is summarized in Table 4.
TABLE 4.
Relationship of Proximal Aortic Stiffness to Incident Hard CVD
| Cox Models for Incident Hard CVD
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted Model 1 | Adjusted Model 2 | Adjusted Model 3 | |||||
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| AAD quintile 1 | 5.7 (2.8–11.7) | <0.001 | 3.3 (1.5–7.0) | 0.002 | 2.2 (1.0–4.8) | 0.04 | 1.9 (0.9–3.8) | 0.09 |
| AAD quintile 2 | 3.6 (1.7–7.5) | 0.001 | 2.2 (1.0–4.8) | 0.05 | 1.8 (0.8–4.0) | 0.14 | 1.8 (0.9–3.7) | 0.10 |
| AAD quintile 3 | 3.6 (1.7–7.5) | 0.001 | 2.6 (1.2–5.6) | 0.01 | 2.2 (1.1–5.0) | 0.04 | 1.9 (0.9–3.9) | 0.07 |
| AAD quintile 4 | 3.0 (1.4–6.3) | 0.005 | 2.4 (1.1–5.2) | 0.02 | 2.2 (1.0–4.8) | 0.04 | 1.9 (0.9–3.9) | 0.07 |
| AAD quintile 5 | 1.0 (reference) | 1.0 (reference) | ||||||
|
| ||||||||
| ABI (<1.0 or ≥1.4) | 2.5 (1.7–3.5) | <0.001 | 2.2 (1.6–3.2) | <0.001 | 1.9 (1.3–2.7) | 0.001 | 1.8 (1.2–2.5) | 0.003 |
| AAD quintile 1 | 4.1 (2.2–7.6) | <0.001 | 2.5 (1.3–5.0) | 0.007 | 1.8 (0.9–3.5) | 0.11 | ||
|
| ||||||||
| Carotid IMT | 1.4 (1.2–1.6) | <0.001 | 1.2 (1.0–1.4) | 0.05 | 1.1 (0.9–1.3) | 0.41 | 0.6 (0.2–1.5) | 0.27 |
| AAD quintile 1 | 4.7 (2.2–10.2) | <0.001 | 3.4 (1.5–7.7) | 0.002 | 2.4 (1.1–5.5) | 0.03 | ||
|
| ||||||||
| CAC (present) | 4.3 (2.9–6.5) | <0.001 | 3.2 (2.1–5.0) | <0.001 | 3.0 (1.9–4.7) | <0.001 | 2.7 1.8–4.2) | <0.001 |
| AAD quintile 1 | 3.9 (1.9–8.0) | <0.001 | 3.0 (1.4–6.5) | 0.004 | 2.1 (0.9–4.5) | 0.07 | ||
|
| ||||||||
| LVH | 1.8 (1.2–2.7) | 0.009 | 1.6 (1.0–2.6) | 0.05 | 1.6 (0.9–2.5) | 0.07 | ||
| AAD quintile 1 | 5.5 (2.7–11.3) | <0.001 | 3.1 (1.4–56.8) | 0.004 | 2.1 (1.0–4.7) | 0.06 | ||
AAD Quintile 1 corresponds to highest and Quintile 5 to lowest aortic stiffness. Adjustment was performed for the following risk factors: Model 1 = age, sex, weight, height, ethnicity; Model 2 = Model 1 + mean BP, smoking, antihypertensive medication, total cholesterol, HDL cholesterol and diabetes; Individual tests of AAD vs. measures of atherosclerosis ABI, carotid IMT, presence of CAC defined as Agatston score>0 and LV hypertrophy defined as LV mass above 90th percentile are provided. Model 3 = Model 2 + adjustment for all measures of subclinical atherosclerosis (ABI, IMT, CAC). Abbreviations as in Tables 1, 2, and 3.
Q1 participants had an unadjusted HR for incident CVD of 5.7 (p < 0.001); 3.3 (p = 0.002) after adjustment for age, body size, and ethnicity; and 2.2 in the fully-adjusted model on CV risk factors including MBP. A similar result was found when adjusting for brachial SBP or PP instead of MBP.
Overall, increased aortic stiffness predicted CVD in the unadjusted and minimally-adjusted models independent of the individual effect of ABI, carotid IMT, presence of CAC, or LVH (Table 4). In the fully-adjusted models, AAD remained predictive of CVD after further adjustment for carotid IMT, which itself was not a significant predictor. However, AAD did not reach significance as a predictor of CVD when ABI and CAC where added individually or together to the fully-adjusted models. Neither AAD nor LVH were significant predictors in the fully-adjusted models when entered together.
When stratified according to Framingham risk category (Table 5), AAD significantly predicted CVD in low-to-intermediate-risk individuals (10-year CVD risk <10%) with an HR of 8.9 (p = 0.001) in univariate analysis and 5.3 (p = 0.03) in the fully-adjusted model, but did not reach significance in high-risk individuals (10-year CVD risk ≥10%). Additionally, reduced aortic distensibility remained a significant predictor of incident CVD in the adjusted model in low-to-intermediate-risk individuals even after further individual or grouped adjustment for ABI, CAC, and carotid IMT and after individual adjustment for LVH. Notably, ABI remained a significant predictor of CVD in low-to-intermediate-risk individuals whereas CAC, carotid IMT, and LVH did not (Table 5).
TABLE 5.
Relationship Between AAD and Incident Hard CVD According to Global Framingham Risk Category
| Cox Models for Incident Hard CVD According to Risk Category
|
||||||||
|---|---|---|---|---|---|---|---|---|
| 10-year CVD risk <10% | 10-year CVD risk ≥10% | |||||||
| Unadjusted | Adjusted* | Unadjusted | Adjusted* | |||||
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| ABI (<1.0 or ≥1.4) | 4.7 (2.1–10.4) | <0.001 | 5.4 (2.2–13.0) | <0.001 | 1.9 (1.3–2.8) | 0.001 | 1.6 (1.1–2.4) | 0.02 |
| AAD quintile 1 | 6.7 (2.1–22.1) | 0.001 | 5.8 (1.6–21.2) | 0.008 | 1.7 (0.8–3.6) | 0.17 | 1.3 (0.6–2.9) | 0.52 |
|
| ||||||||
| Carotid IMT | 1.7 (1.0–2.9) | 0.03 | 1.6 (0.9–2.9) | 0.09 | 1.2 (1.0–1.4) | 0.05 | 1.0 (0.9–1.2) | 0.71 |
| AAD quintile 1 | 7.0 (1.8–26.9) | 0.005 | 4.7 (1.1–20.6) | 0.04 | 2.5 (1.0–6.5) | 0.05 | 2.0 (0.7–5.4) | 0.18 |
|
| ||||||||
| CAC (present) | 2.6 (1.2–5.7) | 0.02 | 2.1 (0.9–5.1) | 0.11 | 3.6 (2.2–5.9) | <0.001 | 3.3 (1.9–5.6) | <0.001 |
|
| ||||||||
| AAD quintile 1 | 7.8 (2.1–29.6) | 0.003 | 5.0 (1.2–21.7) | 0.03 | 2.1 (0.9–5.0) | 0.09 | 1.6 (0.7–4.1) | 0.30 |
|
| ||||||||
| ABI+IMT+CAC† | - | - | - | - | - | - | - | - |
| AAD quintile 1 | 6.3 (1.9–20.8) | 0.003 | 5.8 (1.6–21.1) | 0.008 | 1.8 (0.8–4.0) | 0.16 | 1.5 (0.6–3.5) | 0.37 |
|
| ||||||||
| LVH | 2.7 (0.8–9.2) | 0.10 | 4.8 (1.0–22.5) | 0.05 | 1.3 (0.8–2.1) | 0.21 | 1.5 (0.9–2.5) | 0.15 |
| AAD quintile 1 | 9.5 (2.3–34.9) | 0.001 | 5.0 (1.2–22.1) | 0.03 | 2.3 (1.0–5.4) | 0.05 | 1.6 (0.6–4.2) | 0.30 |
Quintile 1 corresponds to highest and Quintile 5 to lowest aortic stiffness.
Fully adjusted model on age, sex, weight, height, ethnicity, mean BP, smoking, antihypertensive medication, total cholesterol, HDL cholesterol, and diabetes.
Incident HF was associated with altered AAD (Q1) in the univariate model with a HR of 6.0 (95% CI: 2.1–17.4; p = 0.001), but this relationship failed to reach significance in the intermediate- and fully-adjusted models (respectively HR: 2.1; p = 0.18 and HR: 1.4; p = 0.56).
DISCUSSION
We studied proximal aortic distensibility in a large sample from the MESA study. Altered distensibility of the ascending aorta was associated with increased risk of 1) all-cause mortality independent of age and traditional CVD risk factors and 2) incident CVD independent of age and traditional CVD risk factors in otherwise low-to–moderate-risk participants. After adjustment for traditional CV risk factors, individuals with markedly altered AAD for their age group had a 2-fold increase in risk of all-cause death in comparison with individuals with preserved aortic distensibility. Additionally, individuals with high aortic stiffness had an almost 4-fold increase in risk of incident CVD compared to individuals with preserved aortic elasticity if they had a low-to-intermediate CVD risk profile at baseline. However, high aortic stiffness only marginally predicted higher CVD in individuals with a high baseline CVD risk profile. This is the first report to demonstrate independent association of aortic distensibility with mortality and hard CVD events.
Important target organs, such as the heart and brain, are directly linked both anatomically and physiologically to the central elastic arterial sector composed of the ascending aorta, aortic arch, and carotid arteries. In this regard, the predictive value of carotid-femoral PWV, a global estimate of arterial stiffness, has been established in the general population and in CVD patients (7, 21–24). The importance of the proximal aorta in the buffering function of systolic load and therefore in preserving vascular-ventricular coupling is paramount (25–28). Age is a main determinant of arterial structural and functional changes, and subclinical alteration of proximal aortic function can occur early. However, the complex interplay between structural and functional changes in both the aorta and left ventricle through vascular-ventricular coupling is mainly driven by the aging process and further aggravated by atherosclerosis, whose prevalence also increases with age. The proximal aorta dilates and elongates during normal aging secondary to structural wall changes that include thinning and fragmentation of elastin fibers within the media. This process ultimately leads to arterial stiffness and increased afterload on the left ventricle with consequent LVH as well as systolic and diastolic dysfunction (27,28). Hundley et al. showed the relationship between aortic stiffness and impaired exercise capacity in the elderly (29) and Fernandes et al. (4) have shown the relationship between increased carotid stiffness and subclinical alteration in LV systolic and diastolic myocardial deformation in the MESA study.
Aortic dilatation and elongation associated with aortic stiffening (30) lead to a static aortic volume increase partly compensating for the loss of proximal aortic elasticity (systolic cushioning function and diastolic recoil; Figure 1). Until advanced age, or earlier as a result of lifelong aggravating factors such as hypertension, diabetes, or CVD, both aortic and LV function decline proportionally such that the vascular-ventricular coupling is preserved. However, when aortic stiffness is very high, aortic and cardiac complications may occur secondary to a sharp increase in arterial load. This may explain in part why this study and others found extreme aorta stiffness values to be the most relevant in predicting adverse outcomes. However, a specific cut-point has not been defined.
Additionally, flow alterations secondary to large-artery structural and functional modifications are transmitted to smaller arteries and may lead to cardiac, cerebral, and renal microvascular damage and subsequent target organ failure. The resulting global vascular aging continuum may account for the strong association between altered AAD and all-cause mortality beyond CVD’s specific role.
Our results are consistent with prior studies on global measures of aortic stiffness such as the Framingham community-based data of Mitchell et al. (22) regarding superiority of a direct measure of aortic stiffness over conventional brachial systolic or pulse pressure to predict all-cause mortality or incident CVD over time. However, we did not assess the relative value of central versus peripheral blood pressure in this relationship. Additionally, we have found that the highest stiffness group is the most significantly related to adverse outcome with an unevenly graded relationship between outcome and degree of stiffness in intermediate stiffness categories. We found the comparison of the highest and lowest quintiles of AAD to be consistently and strongly different over time in relation to outcome, whereas quintiles 2 through 4 exhibited some degree of crossing between cumulative event curves in the initial half of the follow-up period.
Although direct comparison is not possible with results from the meta-analysis of Vlachopoulos et al. (7) on predicting all-cause mortality and incident CVD because of differing predictor variables (PWV vs. AAD), categorization, and adjustment, it is interesting to note that our findings are consistent. In particular, the relative risk for all-cause mortality was 1.9 (95% CI: 1.60 to 2.24) in their study versus an HR of 2.3 in the present study. In contrast, however, they found marked stiffness to confer higher risk in the subgroup with a higher baseline risk than in low-risk individuals. This can be explained by the notably different definition of risk and sample selection. Indeed, the high-risk group in the Framingham cohort included subjects with known coronary artery disease, renal disease, hypertension, and diabetes, whereas our large sample of the MESA cohort, while representative of MESA participants overall, included participants without overt CVD, fewer diabetics, and no end-stage renal disease patients. Compared to esults by Maroules et al. using MRI in a general population sample of the Dallas Heart Study (11), hazard ratios relating AAD to cardiovascular outcome were higher in our study. This may best be explained by somewhat lower power due to a relatively lower sample size (n = 2,122) and follow-up time in a generally younger cohort with lower prevalence of CV risk factors yielding fewer events than in MESA. Furthermore, primary endpoint definition was significantly different between studies; the primary composite endpoint in Maroules et al. included soft events (hospitalizations for unstable angina, atrial fibrillation, revascularization), whereas we focused only on hard events.
A powerful general CV risk assessment score predicting 10-year risk for CVD in the Framingham study has been established for primary care use (20). Our study shows that AAD is a strong predictor of incident CVD and therefore a potentially useful risk-evaluation criterion in low-to-intermediate-risk individuals; its value in high-risk individuals is more limited. We found that belonging to the highest aortic stiffness category was significantly related to incident CVD with an HR of 1.9 when considering the global CV risk score integrating all traditional risk factors and 2.4 when considering individuals with 10-year CVD risk <10%. Furthermore, when all risk factors were studied individually or together, AAD remained an independent predictor of CVD in the low-to-intermediate-risk sub-cohort, albeit not among those with a baseline global risk score ≥10%.
STUDY LIMITATIONS
Not all participants in the MESA study had aortic MRI and so our study was limited to a subgroup of 3,677/5,098 or 72% of the participants who had an MRI exam and 3,677/6,814 (54%) of the whole MESA cohort. Risk factors were slightly less prevalent in the subgroup of MESA participants with aortic distensibility data compared to other participants. Nevertheless, this remains the largest reported sample of proximal aorta distensibility using MRI in any population. Additionally, the semi-automated contour registration process used to determine aortic areas during the cardiac cycle required a degree of manual intervention, and future studies may benefit from automated segmentation methods. Finally, the number of events remains relatively low and available data lack the statistical power to allow us to discriminate the potential predictive value of AAD for individual events such as HF in this cohort.
CONCLUSIONS
Decreased ascending aorta distensibility significantly predicts all-cause mortality and incident CVD events among individuals without overt CVD. The predictive value of proximal aortic stiffness for CVD is highest in subjects with low-to-intermediate global CV risk in whom risk evaluation could be useful. These findings support the hypothesis that the loss of proximal aortic distensibility is an important early marker of the vascular aging continuum intertwined with atherosclerosis leading to subclinical target organ damage and, ultimately, increased morbidity and mortality.
FIGURE 2. Measurement of Aortic Distensibility in MRI.
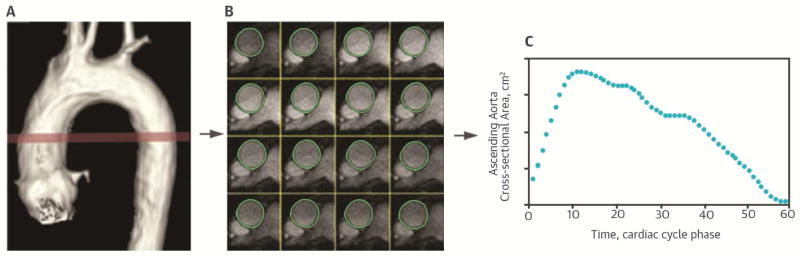
Magnetic resonance imaging (MRI) shows 3-dimensional reconstruction of the thoracic aorta with transverse aortic dynamic acquisition plane (red) (A). Result of the semi-automated segmentation of the ascending aorta (green contour) (B). Resulting cross- sectional area to cardiac cycle time curve (C).
FIGURE 3. CENTRAL ILLUSTRATION Cumulative Event-Free Probabilities for Survival and Survival Free of CVD.
The cumulative event-free probabilities for survival (A) and survival free of incident hard cardiovascular disease (CVD) (B) display similar patterns according to extreme quintiles of ascending aorta distensibility (AAD).
PERSPECTIVES.
Competency in Medical Knowledge
Proximal aortic stiffness can be assessed by magnetic resonance imaging and is an important determinant of circulatory efficiency. Alterations in proximal aortic function are an early marker of cardiovascular aging, atherosclerosis, and other forms of cardiovascular disease.
Translational Outlook
Longitudinal studies are needed to assess the relative value of various indices of aortic and vascular function, including distensibility, as predictors of clinical outcomes.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at www.mesa-nhlbi.org. The MESA study was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung and Blood Institute.
ABBREVIATIONS
- AAD
ascending aorta distensibility
- CVD
cardiovascular disease
- MESA
Multi-Ethnic Study of Atherosclerosis
- MRI
magnetic resonance imaging
- ABI
ankle brachial ndex
- IMT
intima media thickness
- MBP
mean brachial pressure
- PWV
pulse wave velocity
- LVH
left ventricular hypertrophy
Footnotes
Disclosures: MESA Study Funding Source: NHLBI, contracts N01-HC-95159 through N01-HC-95169. No conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.O’Rourke MF, Safar ME, Dzau V. The Cardiovascular Continuum extended: Aging effects on the aorta and microvasculature. Vascular Medicine. 2010;15:461–8. doi: 10.1177/1358863X10382946. [DOI] [PubMed] [Google Scholar]
- 2.Redheuil A, Yu W-C, Wu CO, et al. Reduced ascending aortic strain and distensibility: earliest manifestations of vascular aging in humans. Hypertension. 2010;55:319–26. doi: 10.1161/HYPERTENSIONAHA.109.141275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng S, Fernandes VRS, Bluemke DA, McClelland RL, Kronmal RA, Lima JAC. Age-Related Left Ventricular Remodeling and Associated Risk for Cardiovascular Outcomes: The Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2009;2:191–8. doi: 10.1161/CIRCIMAGING.108.819938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernandes VR, Polak JF, Cheng S, et al. Arterial stiffness is associated with regional ventricular systolic and diastolic dysfunction: the Multi-Ethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol. 2008;28:194–201. doi: 10.1161/ATVBAHA.107.156950. [DOI] [PubMed] [Google Scholar]
- 5.Fernandes VR, Polak JF, Edvardsen T, et al. Subclinical atherosclerosis and incipient regional myocardial dysfunction in asymptomatic individuals: the Multi-Ethnic Study of Atherosclerosis (MESA) J Am Coll Cardiol. 2006;47:2420–8. doi: 10.1016/j.jacc.2005.12.075. [DOI] [PubMed] [Google Scholar]
- 6.Heckbert SR, Post W, Pearson GD, et al. Traditional cardiovascular risk factors in relation to left ventricular mass, volume, and systolic function by cardiac magnetic resonance imaging: the Multiethnic Study of Atherosclerosis. J Am Coll Cardiol. 2006;48:2285–92. doi: 10.1016/j.jacc.2006.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of Cardiovascular Events and All-Cause Mortality With Arterial Stiffness: A Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2010;55:1318–27. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 8.[No authors listed] The Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: “establishing normal and reference values. Eur Heart J. 2010;31:2338–50. doi: 10.1093/eurheartj/ehq165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 10.Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 11.Maroules CD, Khera A, Ayers C, et al. Cardiovascular outcome associations among cardiovascular magnetic resonance measures of arterial stiffness: the Dallas heart study. J Cardiovasc Magn Reson. 2014;16:33. doi: 10.1186/1532-429X-16-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Go OD, Safar ME, Smulyan H. Assessment of Aortic Stiffness by Transesophageal Echocardiography. Echocardiography. 2014;31:1105–12. doi: 10.1111/echo.12528. [DOI] [PubMed] [Google Scholar]
- 13.Redheuil A. Cardiovascular aging: Insights from local and regional measures of aortic stiffness using magnetic resonance imaging. Artery Res. 2014;8:66–72. [Google Scholar]
- 14.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 15.Malayeri AA, Natori S, Bahrami H, et al. Relation of aortic wall thickness and distensibility to cardiovascular risk factors (from the Multi-Ethnic Study of Atherosclerosis [MESA]) Am J Cardiol. 2008;102:491–6. doi: 10.1016/j.amjcard.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turkbey EB, Jain A, Johnson C, et al. Determinants and normal values of ascending aortic diameter by age, gender, and race/ethnicity in the multi-ethnic study of atherosclerosis (MESA) J Magn Reson Imaging. 2014;39:360–8. doi: 10.1002/jmri.24183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bluemke DA, Kronmal RA, Lima JA, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–55. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Criqui MH, McClelland RL, McDermott MM, et al. The ankle-brachial index and incident cardiovascular events in the MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2010;56:1506–12. doi: 10.1016/j.jacc.2010.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Folsom AR, Kronmal RA, Detrano RC, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–9. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D’Agostino RBS, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 21.Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 22.Mitchell GF, Hwang S-J, Vasan RS, et al. Arterial Stiffness and Cardiovascular Events: The Framingham Heart Study. Circulation. 2010;121:505–11. doi: 10.1161/CIRCULATIONAHA.109.886655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blacher J, Asmar R, Djane S, London GM, Safar ME. Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension. 1999;33:1111–7. doi: 10.1161/01.hyp.33.5.1111. [DOI] [PubMed] [Google Scholar]
- 24.Boutouyrie P, Tropeano AI, Asmar R, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension. 2002;39:10–5. doi: 10.1161/hy0102.099031. [DOI] [PubMed] [Google Scholar]
- 25.O’Rourke M. Arterial stiffening and vascular/ventricular interaction. J Hum Hypertens. 1994;8 (Suppl 1):S9–15. [PubMed] [Google Scholar]
- 26.Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part I: aging arteries: a “set up” for vascular disease. Circulation. 2003;107:139–46. doi: 10.1161/01.cir.0000048892.83521.58. [DOI] [PubMed] [Google Scholar]
- 27.Nichols WW, O’Rourke MF, Avolio AP, et al. Effects of age on ventricular-vascular coupling. Am J Cardiol. 1985;55:1179–84. doi: 10.1016/0002-9149(85)90659-9. [DOI] [PubMed] [Google Scholar]
- 28.Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer RJ, Kass DA. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation. 2005;112:2254–62. doi: 10.1161/CIRCULATIONAHA.105.541078. [DOI] [PubMed] [Google Scholar]
- 29.Hundley WG, Kitzman DW, Morgan TM, et al. Cardiac cycle-dependent changes in aortic area and distensibility are reduced in older patients with isolated diastolic heart failure and correlate with exercise intolerance. J Am Coll Cardiol. 2001;38:796–802. doi: 10.1016/s0735-1097(01)01447-4. [DOI] [PubMed] [Google Scholar]
- 30.Redheuil A, Yu W-C, Mousseaux E, et al. Age-Related Changes in Aortic Arch Geometry: Relationship With Proximal Aortic Function and Left Ventricular Mass and Remodeling. J Am Coll Cardiol. 2011;58:1262–70. doi: 10.1016/j.jacc.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]