Abstract
Objectives
To examine the effect of the new legislation on partial sickness benefit on subsequent work participation of Finns with long-term sickness absence. Additionally, we investigated whether the effect differed by sex, age or diagnostic category.
Design
A register-based quasi-experimental study compared the intervention (partial sick leave) group with the comparison (full sick leave) group regarding their pre-post differences in the outcome. The preintervention and postintervention period each consisted of 365 days.
Setting
Nationwide, individual-level data on the beneficiaries of partial or full sickness benefit in 2008 were obtained from national sickness insurance, pension and earnings registers.
Participants
1738 persons in the intervention and 56 754 persons in the comparison group.
Outcome
Work participation, measured as the proportion (%) of time within 365 days when participants were gainfully employed and did not receive either partial or full ill-health-related or unemployment benefits.
Results
Although work participation declined in both groups, the decline was 5% (absolute difference-in-differences) smaller in the intervention than in the comparison group, with a minor sex difference. The beneficial effect of partial sick leave was seen especially among those aged 45–54 (5%) and 55–65 (6%) and in mental disorders (13%). When the groups were rendered more exchangeable (propensity score matching on age, sex, diagnostic category, income, occupation, insurance district, work participation, sickness absence, rehabilitation periods and unemployment, prior to intervention and their interaction terms), the effects on work participation were doubled and seen in all age groups and in other diagnostic categories than traumas.
Conclusions
The results suggest that the new legislation has potential to increase work participation of the population with long-term sickness absence in Finland. If applied in a larger scale, partial sick leave may turn out to be a useful tool in reducing withdrawal of workers from the labour market due to health reasons.
Keywords: partial sick leave, sick leave, work disability, population registers
Strengths and limitations of this study.
Applying nationally representative population register-based data with valid information on the payment of health-related and unemployment-related allowances in Finland.
Applying a quasi-experimental study design with difference-in-differences and propensity score analysis to control for selection on both observed and unobserved factors.
Registers provided only a limited number of background characteristics.
Introduction
The need to increase work participation of working age people is currently a matter of concern in many Western countries. In Finland, delayed or lacking labour market attachment of young people, absence from work during later years and early exit from labour market have all raised alarm. To counteract these trends, an active labour market policy has been adopted, including the introduction of partial social security benefits and other tools to increase the so-called flexicurity of the labour market.1 In Finland, legislation on partial sickness benefit was introduced in 2007. The new benefit allowed for the first time to combine part-time sick leave with part-time work.
The Finnish social insurance is based on the Nordic Model. Everyone aged between 16 and 67, non-retired and living permanently in the country (employees, self-employed, students, unemployed job seekers and those on sabbatical or alternation leave) and also non-residents, working for at least 4 months in Finland, are covered by statutory sickness insurance. The sickness allowances are financed by employers, employees and the state; and are administrated by the Social Insurance Institution of Finland (SII). Statutory benefits can rest on previous earnings or benefits or the minimum allowance can be granted. For the earnings-related occupational sickness benefits, a minimum of 3 months of employment is required.
At present, the Finnish national sickness benefit scheme includes a full and a partial sickness benefit. A medical certificate is an absolute requirement for the two sickness benefits to be granted. In order to be eligible for the partial benefit, an employee has to be eligible for a full benefit as well, but according to medical judgement, partial return to work (RTW) is safe enough. Partial sick leave is thus alternative to full sick leave and it is always medically certified. During the first years after introducing the partial sickness benefit in Finland, a partial sick leave had to be directly preceded by a period of full sick leave of at least 60 days and the partial sickness benefit could be granted from a minimum of 12 to a maximum of 72 working days. During partial sick leave, work time and salary are reduced by 40–60% of the regular and work tasks can be modified, if necessary. The employee and the employer sign a fixed-term work contract for the part-time work. In Finland, the use of partial sick leave is voluntary for the individual. The employer, as well, is entitled to decline the use of the benefit in case the work arrangements needed at the work place are not feasible.
Sickness absence rates are in many countries higher among women compared with men.2 Also, partial sick leave has been more frequently used by women.3 It is known that sickness absence increases with age.2 It is also recognised that challenges of RTW are different, for example, in musculoskeletal diseases and mental disorders. In the latter category, the outflow from disability benefits due to recovery has been lower.4
The current evidence on the effects of partial sick leave on RTW or work participation is partly inconsistent. In the other Nordic countries, partial sick leave has been found to increase the likelihood of return to regular working hours5 6 and to be associated with higher subsequent employment rate.7 No effect of active sick leave (RTW to modified duties) on the average number of sick leave days or long-term disability had been detected in a Norwegian cluster randomised controlled trial.8 There is some discrepancy in the findings on the effectiveness of partial sick leave in mental disorders. A Danish study9 found no effect, whereas a Swedish study10 reported a weak effect of partial sick leave on full recovery in the beginning of work disability due to mental disorders, and a stronger effect when partial sick leave was assigned after 60 days of full sick leave.
In a randomised controlled trial among persons with musculoskeletal disorders, we found that early part-time sick leave predicted faster sustained RTW than full sick leave.11 The beneficial effect of partial sick leave on work retention was also observed at population level.12 13 Partial sick leave was associated in the short term with decreased work retention, in terms of increased subsequent sickness absence. In the long-term it was associated with increased work retention, in terms of increased subsequent use of partial disability pension and decreased use of full disability pension. These findings imply the necessity to use an outcome that simultaneously accounts for different indicators of work participation. Some of these previous observational studies have suffered from limited data samples and narrow generalisability of findings,5 9 self-reported data9 and incomprehensive operationalisation and measurement of work participation.5 6 10 12 13
In order for policymakers to be able to make well-informed decisions in the area of social and health policies, scientific evaluation of the effectiveness of population-level interventions, for example, introducing new legislation or policy change is needed.14 Natural or quasi-experiments have successfully been used in connection with various population-level interventions in the field of public health when planned experimentation, that is, manipulation of exposure, has not been possible.15 In the field of work-disability research, this approach has, however, been rare.2
This study examined the effects of the new Finnish legislation that enabled the use of partial sickness benefit on subsequent work participation. For this, we compared beneficiaries of partial sickness benefit with those receiving full sickness benefit a year after the law on partial sick leave was enacted. We utilised a quasi-experimental design with an integrated measure of work participation. Analyses were carried out in an individual-level register-based data representative of the Finnish working population with long-term sickness absence. We examined whether the effects of partial sick leave on subsequent work participation differed by sex, age or diagnostic category of the benefit receivers.
Methods
Study design and setting
The population-level intervention of interest in this study was the introduction of partial sick leave in Finland in 2007. We conducted a quasi-experimental study following recent guidelines on evaluating population health interventions.15 This design was chosen to minimise the effect of measured and unmeasured confounding. We compared the intervention (partial sick leave) group with the comparison (full sick leave) group regarding their pre-post differences in work participation. The preintervention (T1) and postintervention (T2) study period each consisted of 365 days. A wash-out period of 1 year was set preintervention and postintervention (figure 1) in order to obtain a robust effect of the intervention on work participation. These time windows were allowed to move according to the timing of the individual's sick leave period.
Figure 1.
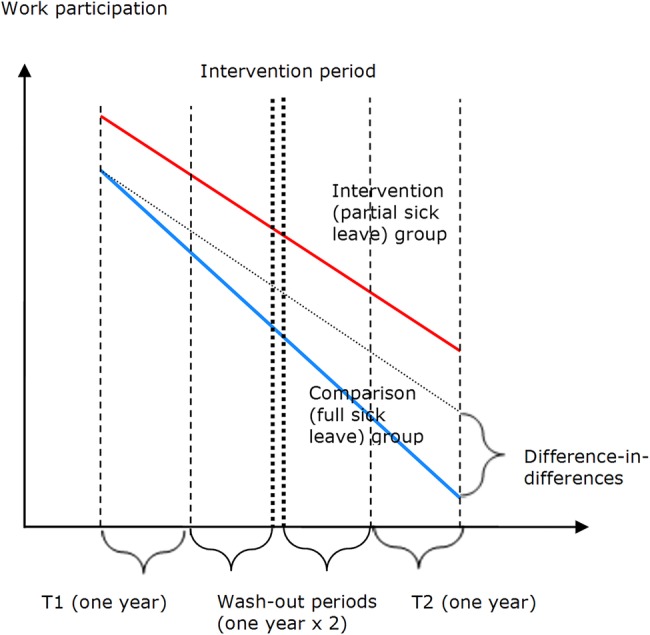
Schematic presentation of the study design and difference-in-differences method. (T1 corresponds to preintervention period, T2 corresponds to postintervention period).
Individual-level data were derived from the national sickness insurance register of the SII and the pension and earnings registers of the Finnish Centre for Pensions. Data from these three registers were linked on the basis of social security numbers of the participants. The social insurance register provided information on all medically certified and compensated sickness absence spells, temporary and permanent national disability pensions, and old-age pensions in Finland. The registers of the Finnish Centre for Pensions contained information on employment periods, earnings-related pensions and unsalaried periods due to disability, rehabilitation or unemployment. Written consent from the individuals was not needed as only encrypted register data were obtained by the researchers carrying out the analyses in the Finnish Institute of Occupational Health.
Participants
Participants that were granted a partial sickness benefit (intervention group) were compared with those who received a full sickness benefit (comparison group). A total sample of individuals who had received either partial sickness benefit (n=1838) or full sickness benefit (n=67 086) in 2007–2008 and whose compensated sickness absence period had ended between 1 January and 31 December 2008 was drawn from the national sickness insurance register. Since a full-time sickness absence of 60 working days had to precede a partial sick leave, only those with full sick leave ending with an uninterrupted period of at least 60 days of payment of the benefit were included in the total sample. Thus, in our sample, receivers of full sickness benefit had not received partial sickness benefit, but they would have been entitled to it as for the length of the preceding fulltime sickness absence.
Since eligibility for a partial sickness benefit required a prior work contract, we excluded from the analyses those who did not have any employment periods (n=2 and n=4923) during the entire study period. We additionally excluded those who had died (n=24 in the partial sick leave group and n=2600 in the full sick leave group) or moved to old age pension (n=1 and n=354, respectively), had not turned 16 at the time of the first data collection period (T1; n=3) or whose sickness absence periods (ending in 2008) extended beyond the time frame of data collection (n=66 and n=1024). The final sample included 1738 participants in the partial sick leave group and 56 754 participants in the full sick leave group. We focused our analyses in the four main diagnostic groups in which partial sickness benefit has most frequently been used, that is, musculoskeletal diseases, mental disorders, traumas and tumours (M, F, S and T, and C and D categories in ICD-10, respectively). All other diagnoses were merged in one group.
Outcome measure
Work participation was operationalised as the time the individuals were likely to have actually participated in gainful employment. It was approximated as the proportion (%) of time within 365 days when participants had an employment contract and did not receive either partial or full ill-health-related benefits (sickness benefits, rehabilitation allowances, disability pensions), or unemployment benefits. Work participation was calculated for T1 and T2. It was assumed that when receiving partial benefits, the participants worked half of the work time (which is typically the case in Finland).
Covariates
Data on sex, dates of birth and death, insurance district (region), annual gross income in 2007, diagnostic codes (ICD-10) and occupational branch were obtained from the sickness insurance register. Information on occupation was available for all participants in the intervention group and for a random sample of 7.7% of the participants in the comparison group.
Data analyses
The distributions of all variables were compared between the total full sickness benefit group (n=67 086) and the subsample of those participants in the full sickness benefit group for whom the registers provided information on occupational branch (n=4347). Since no differences in the distributions were detected, we assumed that information on occupational branch was missing at random. Multiple imputation was used to compensate for the missing data on occupational branch in the comparison group. For this, we generated multiple-imputed data sets (n=10) using the proc mi of SAS. The imputation model included all covariates.
Propensity score (PS) with 1:1 matching was used to match individuals on the probability that they would belong to the intervention (partial sick leave) group. Individuals that were matched to each other had equal or nearly equal (close enough) estimated PSs.
Difference-in-differences (DID) and PS analyses are methods that are complementary to each other and can be applied in causal inference to counter selection bias and confounding.16 We applied the DID method alone and in combination with PS matching. Combining methods to counter bias and confounding from different sources and comparing the results have been encouraged.15 The DID method can be applied to control the fixed unobserved individual differences and common trends.
The DID method allows one to estimate the difference in pre-post, within participant, differences between the intervention and the comparison group. The effect of partial sick leave on work participation was consequently estimated as the difference in pre-post differences (differences between T2 and T1) between partial and full sick leave groups. The effect was estimated using the general linear model (GLM) with repeated measures design. An F-statistic for the interaction term between the group assignment and change of work participation in time was applied as the DID statistic.
PS is defined as a conditional probability of being exposed to a certain intervention given observed covariates.15 17 18 It is applied to balance the covariates in two groups and thus to reduce bias. We computed PS (ie, probability of being exposed to partial sick leave) by logistic regression for all participants. The following set of variables and their interaction terms were included in the logistic regression model: age, sex, diagnostic category, income, occupation, insurance district, and work participation, sickness absence, rehabilitation periods and unemployment at T1. The best fit model was chosen.
Thereafter, we matched the partial sick leave and full sick leave groups on the estimated PS using local optimal (greedy) algorithm.19 The matching was performed within (sex × diagnostic category) strata. Subsequently a DID analysis was also carried out in the matched subsample.
Several sensitivity analyses were carried out. The analyses were run separately for participants for whom the registers provided information on occupational branch and for the total sample in which imputed data on occupational branch were utilised for the comparison group. To examine the group difference in work participation at T1 (due to unemployment or sick leave) as source of reduced group comparability, the analyses were carried out separately among participants who did not receive unemployment benefits at T1 and among participants with 100% of work participation at T1.
Results
Descriptive characteristics of the study population
Information on the background characteristics of the intervention and comparison group in the total analysed sample is shown in table 1. Women constituted 71% of the partial sick leave group and 53% of the full sick leave group. Partial benefit was most common among those who were aged between 35 and 54, whereas full benefit was common among those aged from 45 to 65. The income level of those in the partial sick leave group was higher than of those in the full sick leave group. The partial sickness benefit was most often used in connection with mental disorders and musculoskeletal diseases, while the full benefit was most often used in musculoskeletal diseases. The use of the partial benefit was most frequent in social and healthcare services and administrative and office work, whereas the full benefit was most commonly used in industrial and service work. No large regional differences in the use of the benefits were detected.
Table 1.
Characteristics of participants in partial and full sick leave group at the time of intervention (n, %)
| Partial sick leave n=1738 | Full sick leave n=56 754 | |
|---|---|---|
| Sex (%) | ||
| Female | 1236 (71.1) | 30 058 (53.0) |
| Age (years) (%) | ||
| 16–34 | 217 (12.5) | 10 901 (19.2) |
| 35–44 | 430 (24.7) | 11 231 (19.8) |
| 45–54 | 753 (43.3) | 18 740 (33.0) |
| 55–65 | 338 (19.5) | 15 882 (28.0) |
| Mean (SD) | 46.2 (9.0) | 45.7 (11.3) |
| Annual gross income (€) (%) | ||
| −30 000 | 1237 (71.2) | 46 119 (81.3) |
| 30 001–60 000 | 409 (23.5) | 9593 (16.9) |
| 60 001– | 39 (2.2) | 732 (1.3) |
| Missing | 53 (3.1) | 310 (0.5) |
| Median | 24 618 | 20 668 |
| Diagnostic categories (%) | ||
| Mental disorders | 663 (38.2) | 14 255 (25.1) |
| Musculoskeletal diseases | 624 (35.9) | 20 613 (36.3) |
| Tumours | 112 (6.4) | 3031 (5.4) |
| Traumas | 136 (7.8) | 8416 (14.8) |
| Other | 203 (11.7) | 10 439 (18.4) |
| Insurance district (%) | ||
| Northern | 219 (12.6) | 7764 (13.7) |
| Western | 259 (14.9) | 7824 (13.8) |
| Eastern | 194 (11.2) | 8525 (15.0) |
| South-Western | 410 (23.6) | 13 254 (23.3) |
| Southern | 656 (37.7) | 19 349 (34.1) |
| Missing | 0 (0.0) | 38 (0.1) |
| Occupational branch (%) | (non-imputed subsample n=4347) | |
| Technical and scientific work, etc | 193 (11.1) | 409 (9.4) |
| Social and healthcare services | 516 (29.7) | 719 (16.5) |
| Administration and office work | 293 (16.9) | 413 (9.5) |
| Commercial work | 113 (6.5) | 288 (6.6) |
| Agriculture and forestry | 50 (2.9) | 214 (4.9) |
| Transport | 60 (3.4) | 269 (6.2) |
| Industrial and construction work, mining | 309 (17.8) | 1146 (26.4) |
| Service work | 204 (11.7) | 889 (20.5) |
DID in work participation between partial and full sick leave group
In both groups the level of work participation decreased during the follow-up, the absolute reduction being larger in the full sick leave group (−26.5%) as compared with the partial sick leave group (−21.2%; table 2). The absolute overall DID in work participation was 5.3% (95% CI 3.1% to 7.5%).
Table 2.
Comparison of work participation (%) between partial and full sick leave group (GLM repeated measures design)
| Work participation (%) |
||||||||
|---|---|---|---|---|---|---|---|---|
| n | Preintervention period (T1) Mean (95% CI) |
Postintervention period (T2) Mean (95% CI) |
Post-pre difference (T2-T1) Mean (95% CI) |
p Value | Difference in differences Mean (95% CI) |
F-statistic | p Value | |
| All* | ||||||||
| Partial sick leave | 1685 | 86.6 (85.2 to 88.1) | 65.4 (63.4 to 67.4) | −21.2 (−23.4 to −19.1) | 0.001 | 5.3 (3.1 to 7.5) | 22.8 | 0.001 |
| Full sick leave | 56 406 | 79.4 (79.1 to 79.6) | 52.9 (52.5 to 53.2) | −26.5 (−26.9 to −26.2) | 0.001 | |||
| Males† | ||||||||
| Partial sick leave | 490 | 86.6 (84.0 to 89.1) | 62.7 (59.0 to 66.5) | −23.9 (−27.9 to −19.9) | 0.001 | 6.3 (2.3 to 10.3) | 9.3 | 0.002 |
| Full sick leave | 26 507 | 80.3 (80.0 to 80.7) | 50.2 (49.7 to 50.7) | −30.1 (−30.7 to −29.6) | 0.001 | |||
| Females† | ||||||||
| Partial sick leave | 1195 | 85.4 (83.7 to 87.0) | 66.9 (64.6 to 69.3) | −18.4 (−21.0 to −15.9) | 0.001 | 4.9 (2.4 to 7.5) | 14.2 | 0.001 |
| Full sick leave | 29 889 | 78.6 (78.2 to 78.9) | 55.2 (54.7 to 55.7) | −23.4 (−23.9 to −22.9) | 0.001 | |||
| 16–34 years* | ||||||||
| Partial sick leave | 210 | 89.3 (85.8 to 92.8) | 75.5 (70.2 to 80.9) | −13.8 (−19.6 to −8.0) | 0.001 | 2.8 (−1.1 to 10.6) | 2.5 | 0.111 |
| Full sick leave | 10 759 | 84.6 (84.1 to 85.1) | 66.1 (65.3 to 66.8) | −16.6 (−20.8 to −12.5) | 0.001 | |||
| 35–44 years* | ||||||||
| Partial sick leave | 424 | 84.7 (81.9 to 87.5) | 68.1 (64.2 to 72.0) | −16.6 (−20.8 to −12.5) | 0.001 | 2.0 (−2.2 to 6.2) | 0.9 | 0.352 |
| Full sick leave | 11 177 | 78.4 (77.9 to 79.0) | 59.8 (59.1 to 60.5) | −18.6 (−19.4 to −17.8) | 0.001 | |||
| 45–54 years* | ||||||||
| Partial sick leave | 725 | 86.9 (84.7 to 89.0) | 65.7 (62.6 to 68.8) | −21.1 (−24.4 to −17.9) | 0.001 | 4.7 (1.4 to 8.0) | 7.9 | 0.005 |
| Full sick leave | 18 659 | 77.6 (77.2 to 78.1) | 51.8 (51.2 to 52.4) | −25.9 (−26.5 to −25.2) | 0.001 | |||
| 55–65 years* | ||||||||
| Partial sick leave | 326 | 89.6 (86.3 to 92.9) | 57.0 (52.3 to 61.7) | −32.6 (−37.7 to −27.5) | 0.001 | 5.7 (0.5 to 10.8) | 4.7 | 0.030 |
| Full sick leave | 15 811 | 78.5 (78.0 to 78.9) | 40.2 (39.5 to 40.8) | −38.3 (−39.0 to −37.6) | 0.001 | |||
| Musculoskeletal diseases‡ | ||||||||
| Partial sick leave | 598 | 87.0 (84.8 to 89.3) | 60.3 (57.0 to 63.6) | −26.7 (−30.3 to −23.2) | 0.001 | 0.7 (−2.9 to 4.3) | 0.1 | 0.712 |
| Full sick leave | 20 537 | 79.7 (79.4 to 80.1) | 52.3 (51.7 to 52.9) | −27.4 (−28.0 to −26.8) | 0.001 | |||
| Mental disorders‡ | ||||||||
| Partial sick leave | 645 | 84.6 (82.2 to 87.1) | 67.0 (63.8 to 70.3) | −17.6 (−21.3 to −13.9) | 0.001 | 12.8 (9.0 to 16.5) | 43.8 | 0.001 |
| Full sick leave | 14 136 | 74.6 (74.0 to 75.1) | 44.2 (43.5 to 44.9) | −30.4 (−31.1 to −29.6) | 0.001 | |||
| Traumas‡ | ||||||||
| Partial sick leave | 132 | 86.7 (82.0 to 91.3) | 68.1 (61.5 to 74.6) | −18.6 (−25.3 to −11.8) | 0.001 | −3.2 (−10.0 to 3.5) | 0.9 | 0.348 |
| Full sick leave | 8312 | 82.9 (82.3 to 91.3) | 67.6 (66.7 to 68.4) | −15.3 (−16.2 to −14.5) | 0.001 | |||
| Tumours‡ | ||||||||
| Partial sick leave | 109 | 90.6 (85.9 to 95.4) | 75.0 (67.4 to 82.5) | −15.7 (−23.5 to −7.9) | 0.001 | 5.3 (−2.6 to 13.2) | 1.7 | 0.190 |
| Full sick leave | 3021 | 87.2 (86.3 to 88.1) | 66.2 (64.8 to 67.6) | −21.0 (−22.4 to −19.5) | 0.001 | |||
| Other diagnostic categories‡ | ||||||||
| Partial sick leave | 201 | 87.4 (83.4 to 91.4) | 63.6 (57.8 to 69.4) | −23.8 (−30.0 to −17.6) | 0.001 | 6.2 (−0.05 to 12.5) | 3.8 | 0.052 |
| Full sick leave | 10 400 | 80.2 (79.6 to 80.7) | 50.1 (49.3 to 50.9) | −30.0 (−30.9 to −29.2) | 0.001 | |||
*Age, sex, income, diagnosis, occupational group, insurance district.
†Age, income, diagnosis, occupational group, insurance district.
‡Age, sex, income, occupational group, insurance district.
The DID in work participation tended to be larger in men than in women.
In all age categories, work participation declined more in the full than in the partial sick leave group. The difference in the decline was significant in age categories 45–54 and 55–65. There was no effect in those aged 35–44. In the youngest age category (16–34 years) the DID was large but statistically non-significant.
A statistically significantly larger effect (12.8%, 95% CI 9.0% to 16.5%) was found in mental disorders as compared with the other diagnostic categories.
The results found in the subsample of participants for whom the registers provided information on occupational branch were very similar to those in the total sample (data not shown). The exclusion of the participants who received unemployment benefits at T1 led to an absolute increase in the DID in work participation (DID 7.6%, 95% CI 5.4% to 9.7%). The DID in work participation increased further (DID 9.5%, 95% CI 6.8% to 12.1%) when participants with reduced work participation (for any reason) at T1 were excluded from the analyses.
DID in work participation in the PS-matched subsample
The matching procedure resulted in a total of 1660 matched pairs of participants. The PS matched partial sickness benefit receivers did not differ from full sickness benefit receivers with regard to age, gross income, number of unemployment days, sickness absence days, rehabilitation days or work participation at T1. There were some differences between the groups in the distribution of occupational branches and insurance districts (see online appendix table 1).
The results from the DID analysis in the PS-matched subsample are presented in table 3. The absolute overall DID was increased to 9.8% (95% CI 5.9% to 13.7%). A tendency for a larger DID in men than in women was also found in this subsample. The DID was still the largest in those participants aged over 45 years, but in contrast to the total sample an effect was seen in the younger age categories as well. Differences between the diagnostic categories were reduced as compared to the total sample. The largest effect was still found in mental disorders. In addition, a statistically significant DID was also found in musculoskeletal diseases and tumours. Further adjustment for the differences in the distribution of occupation and insurance district between the intervention and comparison group had no effect on the results of the DID analysis.
Table 3.
Comparison of work participation (%) between partial and full sick leave group
| Work participation (%) | ||||
|---|---|---|---|---|
| n (pairs) | Difference in differences Mean (95% CI) |
F-statistic | p Value | |
| All* | 1660 | 9.8 (5.9 to 13.7) | 60.8 | 0.0001 |
| Males† | 489 | 12.4 (6.9 to 17.9) | 28.1 | 0.002 |
| Females† | 1171 | 7.2 (3.1 to 11.4) | 34.0 | 0.0001 |
| 16–34 years* | 209 | 8.5 (0.5 to 16.6) | 9.5 | 0.002 |
| 35–44 years* | 422 | 6.7 (0.7 to 12.6) | 9.8 | 0.002 |
| 45–54 years* | 708 | 11.1 (6.3 to 15.9) | 30.3 | 0.0001 |
| 55–65 years* | 321 | 12.9 (6.5 to 19.4) | 12.2 | 0.001 |
| Musculoskeletal diseases‡ | 598 | 6.3 (1.5 to 11.2) | 6.0 | 0.015 |
| Mental disorders‡ | 621 | 18.9 (14.2 to 23.5) | 59.9 | 0.0001 |
| Traumas‡ | 131 | 0.3 (−9.3 to 9.9) | 0.0 | 0.99 |
| Tumours‡ | 109 | 12.5 (1.8 to 23.2) | 5.9 | 0.016 |
| Other diagnostic categories‡ | 201 | 11.1 (3.3 to 18.9) | 7.6 | 0.006 |
(GLM repeated measures design) in the PS-matched subsample.
*Age, sex, income, diagnosis, occupational group, insurance district.
†Age, income, diagnosis, occupational group, insurance district.
‡Age, sex, income, occupational group, insurance district.
PS, propensity score.
Discussion
Principal findings
We applied a quasi-experimental design to study the population-level effects of the introduction of partial sickness benefit in Finland among a working population with long-term sickness absence. It was found that partial sick leave had a positive effect on work participation. Although the overall work participation declined from T1 to T2, at the population level the decline was 5% (absolute difference) smaller among the receivers of partial sickness benefit (intervention group) than among the receivers of full sickness benefit (comparison group). The beneficial effect of partial sick leave was seen especially among those aged between 45–54 and 55–65 and in mental disorders. No major sex difference was detected. When the groups were rendered more exchangeable, the effect on work participation was doubled, and the effects were seen in other diagnostic categories than traumas and all age groups.
Validity of the study
An observational quasi-experimental study design can be applied to assess the effects of a planned event or intervention, when randomised controlled trials are neither ethical nor feasible. Observational studies can also better simulate real-world settings and offer more relevant information in view of policy-making.20 The internal validity of observational studies is lower than that of randomised controlled trials due to possible selection according to exposure. For this reason, an analytical approach called potential outcomes or counterfactual framework was chosen. The term refers to the fact that in an ideal situation the exposed would be compared to themselves when unexposed. Since this comparison is impossible, we need a comparable or exchangeable comparison group. We utilised two methods (DID and PS) that have been previously recommended and applied to control for selection on both observed factors and unobserved fixed factors.15 20 21
In the DID method, it is assumed that the unobserved characteristics in the studied groups are stable and that the outcomes would change identically in these groups in the absence of intervention. Consequently, the intervention and comparison groups should be identical, except for the intervention status. However, it is sufficient that the groups are closely, though not exactly, similar.15 We included in the comparison group only participants who would have been entitled to partial sickness benefit as for the length of the preceding sickness absence. We also applied a short wash-out period, to minimise the intragroup differences between the two time points. However, as full information on the eligibility of the participants for partial sickness benefit was not available in the registers (eg, severity of the health problem and degree of remaining workability), we utilised matching on PS to further increase the exchangeability of the groups. Moreover, at the time of the study, the national rates in sickness absence were rather stable. The unemployment rate in Finland was relatively low during the intervention in 2008 (6.4%), however the rates were similar at T1 (7.7–8.4%) and T2 (7.8–8.4%).
We utilised nationwide population data with comprehensive individual-level register-based information on ill-health-related and unemployment-related absences from work. Personal identification (social security) numbers enabled linking information from three different source registers. These registers have originally been established for administrative purposes, but the data can also be used for research.22 Among the advantages of register-based studies is a low likelihood of selection and attrition bias. The source registers of this study provided valid information on the receivers and payment days of the benefits. A limitation of the registers is that they typically provide only a limited number of background characteristics of the participants and other covariates. The process of assignment to partial sick leave is not random. Most likely it is complex and affected by many actors (the patient, physician, employer and workplace) for which information cannot be found in the national registers. Nevertheless, the factors that were included in the analyses have earlier been found to be important predictors of the use of health-related social security benefits and also associated with work disability and RTW.
Information on diagnoses for sickness benefits was also retrieved from registers and had been based on medical assessment. In case of a long-term sickness absence (lasting more than 60 days) in Finland, the sickness benefit is paid in shorter periods, each being covered with a separate medical certificate. Diagnostic codes are transferred from these certificates to the administrative registers. We used the latest (and presumably the most accurate) diagnostic code provided for each long-term sickness absence in 2007–2008. Data on occupational branch had to be imputed for the majority of participants in the comparison group. Nevertheless, the sensitivity analyses suggested that using imputed data on occupation did not affect the results. In contrast to earlier studies on the topic, work participation was approximated in the current study by taking simultaneously into account the rate of different ill-health-related and unemployment-related benefits. We operationalised work participation as proportion of time within a year of not receiving ill-health-related or unemployment benefits. Hence, we had a relatively comprehensive indicator of the availability of the participants for the labour market.
Results in relation to earlier findings
The overall results of this study are congruent with earlier findings, indicating positive effects of partial sick leave on RTW and work retention.5–7 12 We found that partial sick leave had a positive effect on future work participation especially in mental disorders, but the results of the analyses in the subgroup suggested that the overall effect in the total sample might be underestimated.
Our findings on the usefulness of partial sick leave in mental disorders, though not directly comparable, are congruent with a study showing the beneficial effects of partial sick leave on RTW in mental disorders after 60 days of full sick leave, 10 but differ from an earlier study reporting no effect.9 The literature suggests that returning and continuing at work may be more challenging for those with mental disorders than those with somatic problems (eg, musculoskeletal diseases).23–25 In addition, the outflow from disability benefits due to recovery has been lower among those with mental disorders than with musculoskeletal diseases.4 However, in our previous study we found an effect of partial sick leave on work disability pension in both diagnostic categories, the effect tending to be larger in mental disorders than in musculoskeletal diseases.12 The diagnostic groups of musculoskeletal diseases and mental disorders may differ in the degree of comparability of the partial and full sick leave groups with regard to the background characteristics, severity of the health problem and remaining work ability, number of sickness absences as well as in transition to rehabilitation and unemployment. When the exchangeability of the groups was increased with PS matching, a beneficial effect on work participation was detected also in persons with musculoskeletal diseases and those with tumours.
Sickness absence is known to increase with age.26 In addition, it has been found that RTW after long-term sickness absence is less likely at higher ages.27 28 Partial sick leave was found to be most frequently used and also most effective among middle-aged and older workers. It may well be that work arrangements associated with partial sick leave are more easily implemented by employees in a more established or stable work situation.
Conclusions
The overall results of the effectiveness of partial sick leave on work participation suggest that the new legislation on partial sickness benefit introduced in 2007 has the potential to increase work participation of the working population with long-term sickness absence in Finland. A positive effect was seen especially in mental disorders. In the future—if applied in a larger scale—partial sick leave may turn out to be an effective tool in reducing temporary and permanent withdrawal of workers from the labour market due to health reasons.
Supplementary Material
Footnotes
Contributors: JK, SS, EV-J, LJV and AK designed the study. All authors were involved in data collection. JK, SS and AK conducted the analyses, all contributed to the interpretation of the results and JK, SS and EV-J drafted the manuscript. All authors accepted the final version of the manuscript.
Funding: The study received financial support from the Social Insurance Institution of Finland (grant no: 67/26/2011).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Philips ER, Alloja J, Krillo K et al. Approaches to flexicurity: EU-models. European foundation for the improvement of living and working conditions, 2007. [Google Scholar]
- 2.OECD. Sickness, disability and work: breaking the barriers: a synthesis of findings across OECD countries. OECD Publishing, 2010. [Google Scholar]
- 3.Kausto J, Miranda H, Martimo K-P et al. Partial sick leave—review of its use, effects and feasibility in the Nordic countries. Scand J Work Environ Health 2008;34:239–49. 10.5271/sjweh.1266 [DOI] [PubMed] [Google Scholar]
- 4.OECD. Sick on the job? Myths and realities about mental health and work, in mental health and work. OECD Publishing, 2012. [Google Scholar]
- 5.Andren D, Svensson M. Part-time sick leave as a treatment method for individuals with musculoskeletal disorders. J Occup Rehabil 2012;22:418–26. 10.1007/s10926-011-9348-7 [DOI] [PubMed] [Google Scholar]
- 6.Hogelund J, Holm A, McIntosh J. Does graded return-to-work improve sick-listed workers’ chance of returning to regular working hours? J Health Econ 2010;29:158–69. 10.1016/j.jhealeco.2009.11.009 [DOI] [PubMed] [Google Scholar]
- 7.Markussen S, Mykletun A, Roed K. The case for presenteeism—Evidence from Norway's sickness insurance program. J Public Econ 2012;96:959–72. 10.1016/j.jpubeco.2012.08.008 [DOI] [Google Scholar]
- 8.Scheel IB, Hagen KB, Herrin J et al. Blind faith? The effects of promoting active sick leave for back pain patients: a cluster-randomized controlled trial. Spine 2002;27:2734–40. 10.1097/00007632-200212010-00014 [DOI] [PubMed] [Google Scholar]
- 9.Hogelund J, Holm A, Eplov LF. The effect of part-time sick leave for employees with mental disorders. J Ment Health Policy Econ 2012;15:157–0. [PubMed] [Google Scholar]
- 10.Andren D. Does part-time sick leave help individuals with mental disorders recover lost work capacity? J Occup Rehabil 2014;24:344–60. 10.1007/s10926-013-9467-4 [DOI] [PubMed] [Google Scholar]
- 11.Viikari-Juntura E, Kausto J, Shiri R et al. Return to work after early part-time sick leave due to musculoskeletal disorders: a randomized controlled trial. Scand J Work Environ Health 2012;38:134–3. 10.5271/sjweh.3258 [DOI] [PubMed] [Google Scholar]
- 12.Kausto J, Solovieva S, Virta LJ et al. Partial sick leave associated with disability pension: propensity score approach in a register-based cohort study. BMJ Open 2012;2:e001752. 10.1136/bmjopen-2012-001752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kausto J, Virta L, Luukkonen R et al. Associations between partial sickness benefit and disability pensions: initial findings of a Finnish nationwide register study. BMC Public Health 2010;10:361. 10.1186/1471-2458-10-361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grimshaw J, et al. Experimental and quasi-experimental designs for evaluating guideline implementation strategies. Fam Pract 2000;17(Suppl 1):S11–16. 10.1093/fampra/17.suppl_1.S11 [DOI] [PubMed] [Google Scholar]
- 15.Craig P, Cooper C, Gunnell D et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health 2012;66:1182–6. 10.1136/jech-2011-200375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ding YY. Risk adjustment: towards achieving meaningful comparison of health outcomes in the real world. Ann Acad Med Singapore 2009;38:552–7. [PubMed] [Google Scholar]
- 17.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998;17:2265–81. [DOI] [PubMed] [Google Scholar]
- 18.Pattanayak CW, Rubin DB, Zell ER. Propensity score methods for creating covariate balance in observational studies. Rev Esp Cardiol (Engl Ed) 2011;64:897–903. 10.1016/j.recesp.2011.06.008 [DOI] [PubMed] [Google Scholar]
- 19.Coca-Perraillon M. Local and global optimal propensity score matching. SAS Global Forum 2007;185:1–9. [Google Scholar]
- 20.Remler DK, Van Ryzin GG. Research methods in practice. Strategies for description and causation. SAGE Publications, Inc., 2011:616. [Google Scholar]
- 21.Gebel M, Vossemer J. The impact of employment transitions on health in Germany. A difference-in-differences propensity score matching approach. Soc Sci Med 2014;108:128–36. 10.1016/j.socscimed.2014.02.039 [DOI] [PubMed] [Google Scholar]
- 22.Gissler M, Haukka J. Finnish health and social welfare registers in epidemiological research. Norsk Epidemiologi 2004;14:113–20. [Google Scholar]
- 23.Briand C, Durand M-J, St-Arnaud L et al. Work and mental health: learning from return-to-work rehabilitation programs designed for workers with musculoskeletal disorders. Int J Law Psychiatry 2007;30:444–57. 10.1016/j.ijlp.2007.06.014 [DOI] [PubMed] [Google Scholar]
- 24.Thornicroft G, Brohan E, Kassam A et al. Reducing stigma and discrimination: candidate interventions. Int J Ment Health Syst 2008;2:3. 10.1186/1752-4458-2-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Oostrom SH, Anema JR, Terluin B et al. Development of a workplace intervention for sick-listed employees with stress-related mental disorders: intervention mapping as a useful tool. BMC Health Serv Res 2007;7:127. 10.1186/1472-6963-7-127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allebeck P, Mastekaasa A. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 5. Risk factors for sick leave—general studies. Scand J Public Health Suppl 2004;63:49–108. 10.1080/14034950410021853 [DOI] [PubMed] [Google Scholar]
- 27.Steenstra IA. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med 2005;62:851–60. 10.1136/oem.2004.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cornelius LR, van der Klink JJL, Groothoff JW et al. Prognostic factors of long-term disability due to mental disorders: a systematic review. J Occup Rehabil 2010;21:259–74. 10.1007/s10926-010-9261-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


