Abstract
Objective
Program implementers have argued that the increasing availability of anti-retroviral therapy (ART) will reduce the stigma of HIV. We analyzed data from Uganda to assess how HIV-related stigma has changed during a period of ART expansion.
Design
Serial cross-sectional surveys.
Methods
We analyzed data from the Uganda AIDS Rural Treatment Outcomes (UARTO) study during 2007-2012 to estimate trends in internalized stigma among people living with HIV (PLHIV) at the time of treatment initiation. We analyzed data from the Uganda Demographic and Health Surveys (DHS) from 2006 and 2011 to estimate trends in stigmatizing attitudes and anticipated stigma in the general population. We fitted regression models adjusted for socio-demographic characteristics, with year of data collection as the primary explanatory variable.
Results
We estimated an upward trend in internalized stigma among PLHIV presenting for treatment initiation (adjusted b=0.18; 95% CI, 0.06 to 0.30). In the general population, the odds of reporting anticipated stigma were greater in 2011 compared to 2006 (adjusted OR=1.80; 95% CI, 1.51 to 2.13), despite an apparent decline in stigmatizing attitudes (adjusted OR=0.62; 95% CI, 0.52 to 0.74).
Conclusions
Internalized stigma has increased over time among PLHIV in the setting of worsening anticipated stigma in the general population. Further study is needed to better understand the reasons for increasing HIV-related stigma in Uganda and its impact on HIV prevention efforts.
Keywords: Stigma, trends, incidence, HIV, Uganda
Introduction
In low- and middle-income countries (LMICs), HIV-related stigma has been associated with reduced uptake of voluntary counseling and testing[1,2] and increased sexual risk-taking behavior[3] in the general population. Among people living with HIV (PLHIV), stigma has been associated with emotional distress[4,5], decreased adherence to anti-retroviral therapy (ART)[6,7], and reduced likelihood of HIV status disclosure[8,9]. One argument for increasing access to ART was that doing so would reduce stigma[10,11] through improvements in physical health and HIV-related symptom burden[12] leading to economic rehabilitation and social reintegration[13,14]. However, the extent to which levels of HIV-related stigma have actually changed in LMICs during the past decade of treatment scale-up is unclear. A better understanding of temporal trends in stigma in LMICs would help elucidate the impact of ART availability on stigma and the potential need for interventions beyond ART to reduce stigma.
We attempted to address this question using serial cross-sections of data from two sources: the Uganda AIDS Rural Treatment Outcomes (UARTO) study, a longitudinal cohort study of PLHIV in southwestern Uganda who initiate ART upon enrollment; and the Uganda Demographic and Health Surveys (DHS)[15,16], which were nationally representative, population-based surveys conducted in Uganda in 2006 and 2011. Analyzing data from UARTO allowed us to examine temporal trends in internalized stigma among PLHIV newly initiating ART[17,18], while the DHS allowed us to examine trends in stigmatizing attitudes (i.e., expressions of social distance) [18,19] and fears about disclosure (i.e., anticipated stigma)[17,20] in the general population. We had two specific aims: (a) to estimate temporal trends in internalized stigma from 2007 to 2012 among PLHIV presenting for ART initiation; and (b) to understand temporal trends in stigmatizing attitudes and fears about disclosure among persons in the general community.
Methods
Uganda AIDS Rural Treatment Outcomes (UARTO) study
The UARTO study enrolls participants from the Mbarara Regional Referral Hospital Immune Suppression Syndrome Clinic, Mbarara, Uganda, an HIV clinic serving the Mbarara district (population 1.1 million, 92% in rural areas) and adjacent districts[21]. Participants were eligible for enrollment in the UARTO cohort if they were treatment-naïve and newly initiating ART, were at least 18 years of age, and lived within 60 kilometers of the clinic. 49% of patients who were approached for study participation agreed to be enrolled. At the pre-treatment baseline visit, participants underwent blood draws and structured interviews conducted in the local language, Runyankole. The scale for measuring internalized stigma (described in more detail below) was added to the study questionnaire beginning in August 2007. Therefore, only participants whose baseline visits occurred between August 2007 and December 2012 were included in this analysis.
Study staff obtained signed, or in case of illiteracy, thumbprint-indicated informed consent from all participants. Ethical approval for study procedures was obtained from ethical review committees at the University of California at San Francisco, San Francisco, California, USA, Partners Healthcare, Boston, Massachusetts, USA, and the Mbarara University of Science and Technology, Mbarara, Uganda. Consistent with national guidelines, we received clearance for the study from the Uganda National Council for Science and Technology, Kampala, Uganda, and from the Research Secretariat in the Office of the President, Kampala, Uganda.
The primary outcome of interest was internalized stigma, as measured with the six-item Internalized AIDS-Related Stigma Scale (IARSS)[22]. The IARSS has demonstrated a coherent internal structure and good reliability and construct validity among PLHIV in Uganda[9,23]. Two scale items relate to concerns about disclosure (felt stigma)[24] and four items relate to feelings of shame and/or self-hatred[25] (see Table 1). Among study participants at enrollment, the estimated scale reliability coefficient for the IARSS was 0.89.
Table 1. Characteristics of participants in UARTO cohort at time of enrollment (n=329).
| Characteristic | Mean (SD) or no. (%) |
|---|---|
| Year of cohort entry | |
| 2007 | 51 (16%) |
| 2008 | 83 (25%) |
| 2009 | 37 (11%) |
| 2010 | 10 (3%) |
| 2011 | 78 (24%) |
| 2012 | 70 (21%) |
| Female | 229 (70%) |
| Age, years | 34 (10) |
| Achieved more than primary education | 80 (24%) |
| Married | 182 (55%) |
| Household asset index | -0.01 (2.0) |
| Employed | 243 (74%) |
| Travel time to/from clinic, minutes | 52 (41) |
| Body mass index | 22 (4) |
| CD4 cell count | 221 (152) |
| MOS-HIV physical health summary score | 53 (11) |
| HSCL-D score | 1.50 (0.52) |
| Probable depression (HSCL-D>1.75) | 81 (25%) |
| IARSS score | 1.54 (2.05) |
| Being HIV positive makes me feel dirty | 58 (18%) |
| I feel guilty that I am HIV positive | 88 (27%) |
| I am ashamed that I am HIV positive | 76 (23%) |
| I sometimes feel worthless because I am HIV positive | 45 (14%) |
| I hide my HIV status from others | 123 (37%) |
| It is difficult to tell people about my HIV infection | 116 (35%) |
Explanatory variables of interest measured at ART initiation included physical health status, CD4+ T-lymphocyte cell count, body mass index (BMI), depression symptom severity, and socio-demographic variables. Physical health status was measured using the Medical Outcomes Study-HIV Health Survey (MOS-HIV) Physical Health Summary (PHS) score[26]. Depression symptom severity was measured as a continuous variable using the depression sub-scale of the Hopkins Symptom Checklist (HSCL-D)[27]. The scale was adapted for the Ugandan context[28,29], with the four somatic items deleted to avoid possible overlap between symptoms of depression and symptoms of HIV infection[30]. Among study participants at enrollment, the estimated scale reliability coefficient for the modified HSCL-D was 0.86.
Socio-demographic variables included age, gender, educational attainment, marital status, household asset wealth, employment status, and travel time to/from clinic. Household asset wealth was measured by applying principal components analysis to a series of 25 binary variables for household-owned assets and housing characteristics[31]. The first principal component was retained and used to define the wealth index and was entered into the regression models as a continuous variable, with higher values indicating greater asset wealth. Self-reported travel time to/from clinic was included as a proxy for rural residence.
Uganda Demographic and Health Surveys (DHS)
The Uganda DHS are nationally-representative, population-based surveys that were conducted in Uganda in 2006 and 2011. Each iteration of the DHS used a stratified two-stage cluster sampling design based on the sampling frame from the 2002 Population Census. By design, the majority of participants were women. Details of the sampling procedures are included in the full published reports[15,16]. We limited our analyses to participants in the southwest region of Uganda (the region from which the participants in the UARTO study were drawn).
The primary outcomes of interest from the DHS were fears about disclosure and stigmatizing attitudes. Fear of disclosure was assessed by the question “If a member of your family got infected with the AIDS virus, would you want it to remain a secret or not?” Positive responses to this question reflect anticipated stigma in the general population[20]--similar to felt stigma that may be experienced by PLHIV[24]--or the expectation of rejection were one to test HIV positive and the test result revealed to others[17]. Stigmatizing attitudes were assessed by three questions: 1) “If a member of your family became sick with AIDS, would you be willing to care for her or him in your own household?”; 2) “ Would you buy fresh vegetables from a shopkeeper or vendor if you knew that this person had the AIDS virus?”; and 3) “In your opinion, if a female teacher has the AIDS virus but is not sick, should she be allowed to continue teaching in the school?” Positive responses to these questions reflect expressions of social distance[18], or an unwillingness to engage in certain forms of interaction with PLHIV (often motivated by instrumental concerns about casual transmission [19]). A binary composite variable was created from these three questions, equal to one if the participant expressed at least one stigmatizing attitude. As a sensitivity analysis, an ordinal composite variable was also created, with values ranging from zero (answering no to all three questions) to three (answering yes to all three questions).
Socio-demographic variables, including age, gender, educational attainment, marital status, household asset wealth[31], and employment status, were included in the analysis as potential confounders of the relationship between time and stigma. We also included a composite HIV knowledge variable equal to the number of correct responses to six questions about HIV prevention and transmission (Appendix 1).
Statistical Analysis
To summarize changes in internalized stigma at time of ART initiation among UARTO participants by year of cohort entry, we estimated mean stigma (IARSS) scores among participants with complete data on the variables of interest. To estimate changes in IARSS scores over time, we fitted a linear regression model with robust standard errors to the data with IARSS as the outcome variable and year of cohort entry as the explanatory variable. A statistically significant regression coefficient was considered evidence that stigma among PLHIV at ART initiation was changing over time. As an alternative parameterization, we fitted a linear regression model specifying time as a series of dummy variables for each 1-year period, using a Wald-type F test to test the joint statistical significance of the time dummy variables. Estimates were adjusted for socio-demographic characteristics measured at ART initiation as described above. To determine whether temporal trends in clinical factors at presentation could explain observed stigma trends in the UARTO cohort, we sequentially added clinical explanatory variables (BMI, CD4 count, PHS, and HSCL-D) to the regression model and then re-assessed the statistical significance of the regression coefficient for year of cohort entry.
To summarize changes in fears about disclosure and stigmatizing attitudes in the DHS sample (among respondents living in southwestern Uganda only), we merged the 2006 and 2011 datasets into a single dataset with year of DHS as a variable. We used two-sample tests of proportions to compare fears about disclosure and stigmatizing attitudes between 2006 and 2011. To adjust for changes in socio-demographic characteristics, we fitted logistic regression models to the data with year of DHS and socio-demographic variables as explanatory variables. Using these multivariable models, we then sought to identify whether changes in knowledge of HIV explained changes in stigma by adding the composite knowledge variable to the models and re-assessing the statistical significance of the year indicator.
All analyses were performed using SAS software (Version 9.3, SAS Institute, Cary, NC). Regression diagnostic procedures yielded no evidence of collinearity or overly-influential outliers in any of the models. Because our analyses of the DHS were limited to participants living in southwestern Uganda, we did not apply survey weights or clustering variables to obtain nationally representative estimates.
Results
Temporal trends in internalized stigma among UARTO participants
There were 229 women (70%) and 100 men (30%) in the sample for whom complete case data were available (see Appendix 2 for details). Due to a restructuring of study administration and interruption in salary support for study staff, recruitment was limited to ten participants in 2010. Baseline characteristics are described in Table 1.
Mean stigma scores by year of cohort entry are shown in Figure 1; in item-by-item analyses, statistically significant upward trends were observed for all items except for the item “I sometimes feel worthless because I am HIV positive” (b=0.02, p=0.06). In univariable analysis, a statistically significant positive association between year of entry and IARSS score was observed (b=0.17; 95% CI, 0.05-0.28). This suggests an 11.0% (0.17/1.54=0.11) increase per year, relative to the baseline value, in the mean internalized stigma score among newly enrolled participants at cohort entry. The alternative parameterization specifying time as a series of dummy variables was consistent with this finding, rejecting the null hypothesis that mean IARSS score at ART initiation was constant across time (F=3.77, p=0.003).
Figure 1. Mean IARSS scores by year of entry.
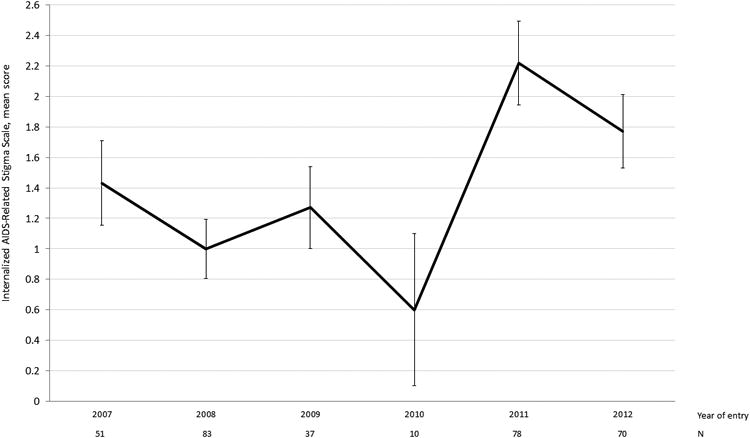
Bars represent standard errors.
After multivariable adjustment for baseline socio-demographic characteristics, the adjusted regression coefficient for year of cohort entry remained statistically significant (b=0.18; 95% CI, 0.06-0.30) (Table 2). The statistical significance remained unchanged with the addition of each of the clinical explanatory variables of interest (PHS, BMI, CD4 count, or HSCL-D) to the multivariable linear regression model, suggesting that changes over time in health status at ART initiation did not explain the observed trend towards increasing stigma.
Table 2. Linear regression estimates for the association between year of cohort entry and IARSS score, with covariates.
| Variable | Adjusted coefficient | 95% CI |
|---|---|---|
| Year of cohort entry | 0.177 | (0.056, 0.298) |
| Female | 0.203 | (-0.332, 0.737) |
| Age, per 10 years | -0.339 | (-0.576, -0.102) |
| Achieved secondary education | 0.323 | (-0.222, 0.868) |
| Unmarried | 0.244 | (-0.234, 0.722) |
| Asset index | 0.031 | (-0.090, 0.151) |
| Unemployed | 0.032 | (-0.485, 0.549) |
| Time to clinic, per minute | 0.006 | (0.0002, 0.011) |
Temporal trends in stigmatizing attitudes and fears of disclosure in southwestern Uganda
Complete case data (see Appendix 2) on persons living in southwestern Uganda were available on 1,141 participants in the 2006 DHS and 1,106 participants in the 2011 DHS (Table 3). Comparing 2006 and 2011, statistically significant differences were found in stigmatizing attitudes and fears about disclosure. Respondents in 2011 were more likely to display an accepting attitude on all three indicators of stigmatizing attitudes (59% vs. 46%, χ2=38.2, p<0.001). However, respondents in 2011 were also more likely to endorse fears about disclosure (61% vs. 47%, χ2=43.4, p<0.001). Adjustment for socio-demographic variables and HIV knowledge yielded no substantive changes in these findings (Table 4).
Table 3. Characteristics of participants in 2006 and 2011 DHS (southwest region, n=2247).
| Characteristic | Mean (SD) or no. (%) |
|---|---|
| Year of DHS | |
| 2006 | 1,141 (51%) |
| 2011 | 1,106 (49%) |
| Sociodemographic variables | |
| Female | 1,865 (78%) |
| Age, years | 29 (10) |
| Achieved more than primary education | 468 (21%) |
| Married | 1,355 (60%) |
| Wealth index | 0.03 (0.75) |
| Employed | 1,835 (82%) |
| Stigma and knowledge variables | |
| Expresses accepting attitude on all 3 stigmatizing attitudes indicators | 1,178 (52%) |
| Would want it kept secret if family member had HIV | 1,203 (54%) |
| No. of correct answers to 6 HIV knowledge questions | 4.8 (1.1) |
Table 4. Logistic regression estimates for the association between year of survey and stigma variables.
| Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | ||
| Expresses at least one stigmatizing attitude towards PLHIV | 2006 | Reference | Reference | ||
| 2011 | 0.59 | (0.50, 0.70) | 0.62 | (0.52, 0.74) | |
| Expresses concerns about HIV disclosure | 2006 | Reference | Reference | ||
| 2011 | 1.75 | (1.48, 2.07) | 1.80 | (1.51, 2.13) | |
Estimates have been adjusted for age, gender, educational attainment, marital status, household asset wealth, and employment status.
Discussion
In this analysis of data from southwestern Uganda, we observed an increase over time in internalized stigma among PLHIV initiating ART. This increase was not explained by compositional changes in socio-demographic characteristics, health status, or psychosocial well-being at treatment initiation. During the same time period, we observed that a significantly higher percentage of people in the general population endorsed fears about disclosure despite an apparent increase in accepting attitudes towards PLHIV. Our findings suggest that the expansion of ART alone may be insufficient to reduce HIV-related stigma and that further targeted efforts to counter stigma are necessary, such as educational campaigns[32], changes to laws or policies that institutionalize stigma[7], and/or livelihood interventions[10].
Our analysis of the 2006 and 2011 DHS suggests that anticipated stigma has worsened in the community despite a decline in stigmatizing attitudes towards PLHIV. What could explain these divergent trends in the general population? Social desirability bias may offer one potential explanation[33]. Namely, the widely disseminated HIV prevention campaigns in Uganda[34,35] may have sensitized people to knowing how they ought to feel about PLHIV without actually changing how they actually feel about PLHIV. This could potentially explain why anticipated stigma increased (i.e., respondents expressed fear of disclosure in the event of a hypothetical case of HIV infection in their family) even while indicators of stigmatizing attitudes declined (i.e., because respondents increasingly understand that they should endorse accepting attitudes towards PLHIV). An alternative interpretation is that, while respondents may have actually changed their own attitudes towards PLHIV, they may have perceived that others in society have not. Thus, the trend towards increasing acceptance of PLHIV may reflect respondents' true feelings, but the belief that such attitudes remain prevalent in society may result in persistent fears of disclosure.
In turn, the persistence of fears about disclosure in the community could adversely affect PLHIV through two hypothesized social psychological mechanisms (explained by Link[18] in the context of mental illness stigma). First, during socialization, PLHIV may devalue themselves because they see themselves as belonging to a person group that most others in the general population view negatively. Second, PLHIV who are concerned about the stigmatizing attitudes held by others will engage in negative defenses such as covering and isolation. Either or both of these mechanisms could explain why internalized stigma among PLHIV increased over time.
It remains unclear whether our findings reflect trends in other populations in sub-Saharan Africa. Program implementers from Partners in Health[11,36] as well as investigators in South Africa[37], Botswana[20], Uganda[10,12], and Malawi[38], have argued that the increasing availability of ART should be associated with reduced levels of stigma in the general population. This experience has not been observed universally. For example, Maughan-Brown[39] found an increase in several dimensions of stigma among the general population of South Africa in 2003-2006 despite ART expansion. This finding may be related to the idea that ART does little to counter persistent blaming attitudes and feelings of moral outrage in the community; indeed, ART may be perceived as allowing PLHIV to appear healthy enough to engage in promiscuous behaviors and spread HIV[39-41]. Niehaus[42], on the other hand, argued that any association with perceived deviance provides an insufficient explanation for persisting negative attitudes towards PLHIV. Lack of trust among the general population in the efficacy and sustainability of ART may also mitigate the positive effects of ART expansion on stigma[43,44]. Finally, Maughan-Brown studied only the earliest period of treatment expansion. With additional observation periods, it is possible that the trends observed in his study would have changed.
We contend that there is reason to believe that our findings may be unique to Uganda and that the persistence of stigma may be related to the country's status as the only country in sub-Saharan Africa to have experienced an increasing incidence of HIV in the past decade[45,46]. Formerly hailed as an HIV/AIDS “success story”[47], Uganda's achievements in controlling the spread of HIV have stalled as the number of new infections per year in Uganda has increased from approximately 69,000 in 2001 to 120,000 in 2012[45]. There is growing concern that the recent drafting of anti-homosexuality legislation may have increased HIV-related stigma and discouraged people from being tested and treated[48-50]. Moreover, many observers fear that HIV-related stigma will be further exacerbated by recently-passed legislation that criminalizes “willful” HIV transmission and permits medical providers to disclose a patient's HIV status to others[49,51]. Given the urgent need to reduce new HIV infections and HIV-related deaths in Uganda, further investigation into the relationship between stigma and persistently high HIV incidence as well as interventions to reduce HIV-related stigma may be warranted.
There are several limitations to our study. First, our data are derived from a single region of Uganda. Regional heterogeneity in stigmatizing attitudes has been described[52]. Furthermore, as discussed above, it is uncertain whether our findings represent a trend unique to Uganda or reflect trends that exist in other LMICs. The IARSS scores in the UARTO cohort (mean=1.5) appeared to be lower compared to those obtained in surveys conducted in South Africa (mean=3.0) and Swaziland (mean=2.2)[22]. These differences may be due to the fact that those data were collected in hyperendemic settings during an earlier time period compared to the UARTO cohort. Second, our measures of anticipated stigma and social distance, which are also used as core indicators for monitoring the HIV epidemic by the Joint United Nations Programme on HIV/AIDS[53], describe hypothetical situations that survey respondents could have misunderstood without being provided with further information. Although this limitation is well-known[33,54], it would only lead to biased estimates of temporal trends in stigma if respondents' comprehension of these specific questions were also systematically changing over time. Third, the study sample of PLHIV consisted primarily of women. However, this is typical of other HIV cohorts in sub-Saharan Africa. For example, in the meta-analysis of more than 200,000 PLHIV by Druyts et al.[55], nearly two-thirds of participants were women. Similar findings were reported by Muula et al.[56] Fourth, we were unable to evaluate the role of health care providers' attitudes toward PLHIV as a contributing factor to the increase in internalized stigma among PLHIV; although participants in the UARTO cohort were ART-naïve, about half of them had had previous contact with HIV providers. Because disrespect of PLHIV among providers in sub-Saharan Africa has been shown to be a potentially important cause of disengagement from HIV care[57], further study on trends in health care providers' attitudes would be helpful in understanding the reasons for increasing internalized stigma among PLHIV.
In conclusion, in this study of rural southwestern Uganda, we found evidence for a temporal trend of increasing stigma among PLHIV presenting for ART initiation as well as persisting anticipated stigma among the general population. Despite the growing availability of ART, which has allowed increasing numbers of PLHIV to restore physical health and rehabilitate economically and socially, these forms of stigma remain highly prevalent and may have worsened. Our findings underscore the need to better understand reasons for persistent stigma in the era of ART expansion and more effective methods to reduce stigma among PLHIV and in the general population.
Supplementary Material
Acknowledgments
The authors thank the participants of the Uganda AIDS Rural Treatment Outcomes Study who contributed valuable time and information.
Source of Funding: The UARTO Study was funded by U.S. National Institutes of Health (NIH) R01MH054907, P30AI27763, and K23MH079713. The authors also acknowledge the following additional sources of support: NIH T32AI007433 (Chan), K23MH099916 (Siedner), K23MH087228 (Haberer), U01CA066529 (Martin), P30AI060354 (Mayer), K24MH087227 (Bangsberg), K23MH096620 (Tsai), David Brudnoy Scholar Award (Chan), and the Burke Family Foundation (Weiser). Dr. Mayer has also received unrestricted research grants from Merck, Gilead, and Bristol Meyers Squibb.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
Author Contributions: B.T.C. performed the statistical analyses and drafted the manuscript. S.D.W., Y.B., J.E.H., P.W.H., J.N.M., and D.R.B. conceived the design of the study. B.T.C., S.D.W., D.R.B., and A.C.T. conceived the design of the specific analyses presented in this manuscript. A.R.M. provided assistance with data management. All authors were involved in revisions of the paper for critical intellectual content and approved the final version.
References
- 1.Hutchinson PL, Mahlalela X. Utilization of voluntary counseling and testing services in the Eastern Cape, South Africa. AIDS Care. 2006;18:446–55. doi: 10.1080/09540120500213511. [DOI] [PubMed] [Google Scholar]
- 2.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79:442–7. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Skinner D, et al. AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape Town, South Africa. Ann Behav Med. 2012;43:362–71. doi: 10.1007/s12160-012-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64:1823–31. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74:2012–9. doi: 10.1016/j.socscimed.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyer S, Clerc I, Bonono CR, Marcellin F, Bilé PC, Ventelou B. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: Individual and healthcare supply-related factors. Soc Sci Med. 2011;72:1383–92. doi: 10.1016/j.socscimed.2011.02.030. [DOI] [PubMed] [Google Scholar]
- 7.Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16:18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Norman A, Chopra M, Kadiyala S. Factors related to HIV disclosure in 2 South African communities. Am J Public Health. 2007;97:1775–81. doi: 10.2105/AJPH.2005.082511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013;46:285–94. doi: 10.1007/s12160-013-9514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsai AC, Bangsberg DR, Weiser SD. Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Med. 2013;10:e1001557. doi: 10.1371/journal.pmed.1001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farmer P, Léandre F, Mukherjee JS, Claude M, Nevil P, Smith-Fawzi MC, et al. Community-based approaches to HIV treatment in resource-poor settings. Lancet. 2001;358:404–9. doi: 10.1016/s0140-6736(01)05550-7. [DOI] [PubMed] [Google Scholar]
- 12.Tsai AC, Bangsberg DR, Bwana M, Haberer JE, Frongillo EA, Muzoora C, et al. How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS Behav. 2013;17:2725–31. doi: 10.1007/s10461-013-0503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venkataramani AS, Thirumurthy H, Haberer JE, Boum Y, Siedner MJ, Kembabazi A, et al. CD4+ cell count at antiretroviral therapy initiation and economic restoration in rural Uganda. AIDS. 2014;28:1221–6. doi: 10.1097/QAD.0000000000000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell C, Skovdal M, Madanhire C, Mugurungi O, Gregson S, Nyamukapa C. “We, the AIDS people…”: how antiretroviral therapy enables Zimbabweans living with HIV/AIDS to cope with stigma. Am J Public Health. 2011;101:1004–10. doi: 10.2105/AJPH.2010.202838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uganda Bureau of Statistics (UBOS) and ICF International Inc. Uganda Demographic and Health Survey 2011. Kampala, Uganda: UBOS and Calverton, Maryland: ICF International Inc; 2012. [Google Scholar]
- 16.Uganda Bureau of Statistics (UBOS) and ICF International Inc. Uganda Demographic and Health Survey 2006. Calverton, Maryland, USA: UBOS and Macro International Inc; 2007. [Google Scholar]
- 17.Link BG. Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review. 1987;52:96–112. [Google Scholar]
- 18.Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92:1461–500. [Google Scholar]
- 19.Pryor JB, Reeder GD, Vinacco R, Kott TL. The instrumental and symbolic functions of attitudes towards persons with AIDS. J Appl Soc Psychol. 1989;19:377–404. [Google Scholar]
- 20.Wolfe WR, Weiser SD, Leiter K, Steward WT, Percy-de Korte F, Phaladze N, et al. The impact of universal access to antiretroviral therapy on HIV stigma in Botswana. Am J Public Health. 2008;98:1865–71. doi: 10.2105/AJPH.2007.122044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Geng EH, Bwana MB, Kabakyenga J, Muyindike W, Emenyonu NI, Musinguzi N, et al. Diminishing availability of publicly funded slots for antiretroviral initiation among HIV-infected ART-eligible patients in Uganda. PLoS ONE. 2010;5:e14098. doi: 10.1371/journal.pone.0014098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21:87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- 23.Tsai AC, Weiser SD, Steward WT, Mukiibi NFB, Kawuma A, Kembabazi A, et al. Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS Behav. 2013;17:427–33. doi: 10.1007/s10461-012-0281-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scambler G, Hopkins A. Being epileptic: coming to terms with stigma. Sociol Health Illn. 1986;8:26–43. [Google Scholar]
- 25.Scheff TJ. Being mentally ill: a sociological theory. Chicago: Aldine Pub. Co; 1966. [Google Scholar]
- 26.Wu AW, Rubin HR, Mathews WC, Ware JE, Brysk LT, Hardy WD, et al. A health status questionnaire using 30 items from the Medical Outcomes Study. Preliminary validation in persons with early HIV infection. Med Care. 1991;29:786–98. doi: 10.1097/00005650-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Mod Probl Pharmacopsychiatry. 1974;7:79–110. doi: 10.1159/000395070. [DOI] [PubMed] [Google Scholar]
- 28.Bolton P. Cross-cultural validity and reliability testing of a standard psychiatric assessment instrument without a gold standard. J Nerv Ment Dis. 2001;189:238–42. doi: 10.1097/00005053-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Bolton P, Ndogoni L. Cross-cultural assessment of trauma-related mental illness (Phase II) Baltimore: [cited 2013 Nov 15]. Internet. Available from: http://www.certi.org/publications/policy/ugandafinahreport.htm. [Google Scholar]
- 30.Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188:662–70. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data--or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 32.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16:18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nyblade L, MacQuarrie K, Phillip F, Kwesigabo G, Mbwambo J, Ndega J. In: Measuring HIV stigma: results of a field test in Tanzania. US Agency for International Development, editor. Washington, DC: 2005. [cited 2014 Feb 18]. Internet. Available from: http://www.icrw.org/files/publications/Working-Report-Measuring-HIV-Stigma-Results-of-a-Field-Test-in-Tanzania.pdf. [Google Scholar]
- 34.Green EC, Halperin DT, Nantulya V, Hogle JA. Uganda's HIV prevention success: the role of sexual behavior change and the national response. AIDS Behav. 2006;10:335–46. doi: 10.1007/s10461-006-9073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Walque D. How does the impact of an HIV/AIDS information campaign vary with educational attainment? Evidence from rural Uganda. J Dev Econ. 2007;84:686–714. [Google Scholar]
- 36.Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health. 2005;95:53–9. doi: 10.2105/AJPH.2003.028563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mall S, Middelkoop K, Mark D, Wood R, Bekker LG. Changing patterns in HIV/AIDS stigma and uptake of voluntary counselling and testing services: the results of two consecutive community surveys conducted in the Western Cape, South Africa. AIDS Care. 2013;25:194–201. doi: 10.1080/09540121.2012.689810. [DOI] [PubMed] [Google Scholar]
- 38.Baranov V, Bennett D, Kohler HP. The indirect impact of antiretroviral therapy; Northeast Universities Development Consortium Conference; Hanover, New Hampshire. 2012. [Google Scholar]
- 39.Maughan-Brown B. Stigma rises despite antiretroviral roll-out: a longitudinal analysis in South Africa. Soc Sci Med. 2010;70:368–74. doi: 10.1016/j.socscimed.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 40.Roura M, Urassa M, Busza J, Mbata D, Wringe A, Zaba B. Scaling up stigma? The effects of antiretroviral roll-out on stigma and HIV testing. Early evidence from rural Tanzania. Sex Transm Infect. 2009;85:308–12. doi: 10.1136/sti.2008.033183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ezekiel MJ, Talle A, Juma JM, Klepp KI. “When in the body, it makes you look fat and HIV negative”: the constitution of antiretroviral therapy in local discourse among youth in Kahe, Tanzania. Soc Sci Med. 2009;68:957–64. doi: 10.1016/j.socscimed.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 42.Niehaus I. Death before dying: understanding AIDS stigma in the South African lowveld. J Southern Afr Stud. 2007;33:845–860. [Google Scholar]
- 43.Agnarson AM, Masanja H, Ekström AM, Eriksen J, Tomson G, Thorson A. Challenges to ART scale-up in a rural district in Tanzania: stigma and distrust among Tanzanian health care workers, people living with HIV and community members. Trop Med Int Health. 2010;15:1000–7. doi: 10.1111/j.1365-3156.2010.02587.x. [DOI] [PubMed] [Google Scholar]
- 44.Bogart LM, Kalichman SC, Simbayi LC. Endorsement of a genocidal HIV conspiracy as a barrier to HIV testing in South Africa. J Acquir Immune Defic Syndr. 2008;49:115–6. doi: 10.1097/QAI.0b013e318181b889. [DOI] [PubMed] [Google Scholar]
- 45.UNAIDS. [cited 2014 Apr 30];Global report: UNAIDS report on the global AIDS epidemic 2013. 2013 Internet. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf.
- 46.Murray CJL, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:1005–1070. doi: 10.1016/S0140-6736(14)60844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Parkhurst JO. The Ugandan success story? Evidence and claims of HIV-1 prevention. Lancet. 2002;360:78–80. doi: 10.1016/S0140-6736(02)09340-6. [DOI] [PubMed] [Google Scholar]
- 48.Human Rights Watch. Uganda: “Anti-homosexuality” bill threatens liberties and human rights defenders. [cited 2014 Aug 25];2009 Internet. Available from: http://www.hrw.org/news/2009/10/15/uganda-anti-homosexuality-bill-threatens-liberties-and-human-rights-defenders.
- 49.Burki T. The changing tide in Uganda's HIV control. Lancet Infect Dis. 2014;14:555–6. doi: 10.1016/s1473-3099(14)70815-1. [DOI] [PubMed] [Google Scholar]
- 50.Devi S. Uganda takes “another step backward” with HIV bill. Lancet. 2014;383:1960. doi: 10.1016/s0140-6736(14)60941-7. [DOI] [PubMed] [Google Scholar]
- 51.Human Rights Watch. Uganda: Deeply Flawed HIV Bill Approved. [cited 2014 May 20];2014 Internet. Available from: http://www.hrw.org/news/2014/05/13/uganda-deeply-flawed-hiv-bill-approved.
- 52.Akullian A, Kohler P, Kinuthia J, Laserson K, Mills LA, Okanda J, et al. Geographic distribution of HIV stigma among women of childbearing age in rural Kenya. AIDS. 2014;28:1665–72. doi: 10.1097/QAD.0000000000000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.UNAIDS. National AIDS programmes: a guide to monitoring and evaluation. Geneva: 2000. [cited 2014 Feb 18]. Internet. Available from: http://www.who.int/hiv/pub/me/pubnap/en/ [Google Scholar]
- 54.Yoder PS, Nyblade L. Comprehension of questions in the Tanzania AIDS Indicator Survey. ORC Macro; Calverton: 2004. [cited 2014 Feb 18]. Internet. Available from: http://pdf.usaid.gov/pdf_docs/PNADC460.pdf. [Google Scholar]
- 55.Druyts E, Dybul M, Kanters S, Nachega J, Birungi J, Ford N, et al. Male sex and the risk of mortality among individuals enrolled in antiretroviral therapy programs in Africa: a systematic review and meta-analysis. AIDS. 2013;27:417–25. doi: 10.1097/QAD.0b013e328359b89b. [DOI] [PubMed] [Google Scholar]
- 56.Muula AS, Ngulube TJ, Siziya S, Makupe CM, Umar E, Prozesky HW, et al. Gender distribution of adult patients on highly active antiretroviral therapy (HAART) in Southern Africa: a systematic review. BMC Public Health. 2007;7:63. doi: 10.1186/1471-2458-7-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ware NC, Wyatt MA, Geng EH, Kaaya SF, Agbaji OO, Muyindike WR, et al. Toward an understanding of disengagement from HIV treatment and care in sub-Saharan Africa: a qualitative study. PLoS Med. 2013;10:e1001369. doi: 10.1371/journal.pmed.1001369. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


