Abstract
BACKGROUND
Myc-positive B-cell non-Hodgkin lymphoma (NHL) with or without a B-cell chronic lymphocytic leukemia/lymphoma 2 (BCL2) rearrangement is associated with inferior progression-free survival (PFS) and overall survival (OS). In this study, the authors reviewed the outcomes of patients with myc-positive and double-hit NHL at The Ohio State University.
METHODS
All patients who had non-Burkitt, aggressive B-cell NHL from 2008 to 2011 were assessed for the t(14;18) translocation and for v-myc avian myelocytomatosis viral oncogene homolog (CMYC) rearrangements at diagnosis, and all myc-positive patients were included in the current analysis. Associations with clinical characteristics were described, and univariable and multivariable models were used to assess correlations between clinical variables and outcomes.
RESULTS
Of 49 myc-positive patients, 29 patients also had BCL2 rearrangements (double-hit NHL). No patients underwent autologous stem cell transplantation in first remission. For all myc-positive patients, the median PFS was 16.6 months, and the median OS was 37.7 months. For patients who had double-hit NHL, the median PFS was 8 months, and the median OS was 12.5 months; whereas the median PFS and OS were not reached for myc-positive patients. A complete response (CR) after front-line therapy, the presence of t(14;18), International Prognostic Index (IPI) group, and age were associated with PFS; whereas only the achievement of a CR and age >60 years were associated with OS in the multivariable setting. The median PFS was 3.3 months, and the median and OS was 7.0 months for patients who did not attain a CR; and the medians were not reached for patients who achieved a CR (P <.00001).
CONCLUSIONS
The achievement of a CR with front-line therapy is associated with a prolonged PFS and OS in patients with myc-positive NHL, even after adjusting for type of initial therapy, histology, age, IPI, or the presence of a concurrent BCL2 translocation.
Keywords: non-Hodgkin lymphoma, B-cell lymphoma, C-myc genes, immunoglobulin heavy chain genes
INTRODUCTION
Rearrangements involving v-myc avian myelocytomatosis viral oncogene homolog (CMYC) and B-cell chronic lymphocytic leukemia/lymphoma 2 (BCL2) have been associated with adverse outcomes in aggressive B-cell non-Hodgkin lymphoma (NHL). CMYC rearrangements are identified in 5% to 13% of newly diagnosed cases of aggressive B-cell NHL.1–4 Patients who had lymphomas harboring a CMYC rearrangement (ie, myc-positive) were associated with decreased 5-year progression-free survival (PFS) (31%; P = .006) and overall survival (OS) (33%; P = .016) compared with myc-negative patients in a series of 135 patients who had diffuse large B-cell lymphoma (DLBCL) treated with combined rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).1 Myc-positive patients with BCL2 (or BCL6) rearrangements (double-hit NHL) have a particularly poor prognosis, and standard therapy is not effective for these patients. In a review of 20 patients who had double-hit NHL, the median OS of 4.5 months was significantly shorter than that in matched controls with Burkitt lymphoma (P = .002) or DLBCL (P = .04).5 Another series of 54 patients with double-hit NHL included 36 patients who had B-cell lymphoma unclassifiable between Burkitt lymphoma and diffuse large B-cell lymphoma (BCLU), 17 patients who had DLBCL, and 1 patient who had follicular lymphoma. Fifty-nine percent of those patients died within 6 months of diagnosis after treatment with combined cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) (n = 23); R-CHOP (n = 11); autologous stem cell transplantation (n = 6); or palliative therapy (n = 14).6 Green et al identified 193 patients with DLBCL, including 11 with double-hit NHL, and those patients had a median PFS of 6 months and an OS of 13 months when they received R-CHOP7; whereas another series identified 14 patients with double-hit DLBCL who had a 5-year PFS rate of 18% and an OS rate of 27% among those who received R-CHOP.3
Given the poor prognosis for these patients, novel therapeutic approaches are being examined. In one trial, 12 patients who received dose-adjusted (DA) rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (DA-R-EPOCH) had a median PFS of 21 months compared with 6 months for patients who received R-CHOP (n = 15) and 6 months for patients who received rituximab, cyclophosphamide, vincristine, doxorubicin, and methotrexate alternating with rituximab, ifosfamide, etoposide, cytarabine (R-CODOX-M/R-IVAC) (n = 6)8; and, in another trial, 6 patients with myc-positive DLBCL who received DA-R-EPOCH had a 2-year PFS rate of 83%.9 However, Jaglal et al identified a survival advantage for patients with BCLU who received R-CHOP compared with patients who received other regimens in a series of 31 patients (including some with MYC, BCL2, and BCL6 rearrangements), with a median OS of 33 months using R-CHOP versus 17 months using the other regimens (P = .048).10 Other approaches in these patients include consolidation with autologous stem cell transplantation in first remission. We reviewed the outcomes of patients with myc-positive and double-hit NHL at our institution, where autologous stem cell transplantation in first remission is not offered, and all patients with newly diagnosed DLBCL and BCLU are evaluated for CMYC and BCL2 rearrangements.
MATERIALS AND METHODS
Patients
All patients with untreated, de novo, aggressive B-cell NHL (DLBCL or BCLU) who were positive for a CMYC rearrangement by fluorescence in situ hybridization (FISH) between January 2008 and December 2011 were included. Patients who had follicular, Burkitt, or transformed NHL and those who had CMYC rearrangements identified only at relapse were not included.
Pathologic Evaluation and FISH
All formalin-fixed, paraffin-embedded lymph node samples from patients with aggressive B-cell NHL that were identified between January 2008 and December 2011 were evaluated prospectively at the time of diagnosis for the presence of a CMYC rearrangement by FISH using a CMYC dual-color, break-apart probe (Abbott Molecular, Des Plains, Ill). Patients were also screened for the immunoglobulin heavy locus (IGH)/BCL2 translocation using a dual-color, dual-fusion translocation probe (Abbott Molecular). The diagnostic specimens also were reviewed centrally by hematopathologists.
Response Assessment
Response was determined at the completion of therapy by the treating physician. In addition, all available interim (n = 25) and post-treatment (n = 21) positron emission tomography (PET)/computed tomography (CT) studies were centrally reviewed by 1 nuclear medicine physician who was blinded to the initial interpretation of the scans, and response was assessed with the Deauville criteria using hepatic uptake as the reference.11
Statistical Analyses
Clinical, demographic, and pathologic characteristics were assessed and summarized across all patients as well as between those with versus without a BCL2 rearrangement. Associations of myc-positive NHL versus double-hit NHL with these characteristics were evaluated using Fisher exact tests for categorical variables and Wilcoxon rank-sum tests for continuous variables. PFS and OS were calculated from the date of diagnosis to the date of disease progression and/or death; and progression-free patients who remained alive were censored at the time of their last follow-up. Univariable Cox regression models were used to assess the correlations of characteristics with PFS and OS. The characteristics or markers that were significant in the univariate setting were carried forward for evaluation in the multivariable setting, and best subsets modeling and concordance statistics were used to assess the best models for PFS and OS. Agreement on results from PET/CT for interim scans versus post-treatment scans was evaluated using a Kappa statistic.12 For all analyses, statistical significance was defined as P <.05. All analyses were conducted using the statistical program R (version 2.15.2 GUI 1.53 Leopard build 64-bit; R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Patients and Disease Characteristics
Forty-nine patients were identified who had CMYC rearrangements, 29 patients had double-hit NHL (59%), 14 patients were myc-positive without a BCL2 rearrangement, and 6 patients were myc-positive but were not assessed for BCL2 rearrangement. Thirty-seven patients (76%) were diagnosed with DLBCL, 11 patients (22%) had BCLU, and 1 patient (2%) was unable to be classified. The patients with double-hit NHL tended to present with higher stage disease (P = .086) and with higher IPI scores (P = .005) compared with patients who did not have a BCL2 rearrangement. Remaining clinical characteristics are described in Table 1.
TABLE 1.
Demographic and Clinical Characteristics of Patients With Myc-Positive and Double-Hit Non-Hodgkin Lymphoma
| Characteristic | No. of Patients (%) | |||
|---|---|---|---|---|
|
| ||||
| Overall, N = 49 | Myc-Positive NHL, N = 20 | Double-Hit NHL, N = 29 | P | |
| Age: Median [range], y | 62 [23–83] | 61 [34–83] | 64 [23–79] | .82 |
| Men | 27 (55) | 13 (65) | 14 (48) | .39 |
| Disease stage | .045 | |||
| I | 2 (4) | 2 (10) | 0 (0) | |
| II | 7 (14) | 5 (25) | 2 (7) | |
| III | 11 (22) | 5 (25) | 6 (21) | |
| IV | 29 (59) | 8 (40) | 21 (72) | |
| B-symptoms | 27 (55) | 11 (55) | 16 (55) | .99 |
| Ki-67: Median [range], % | 90 [45–100] | 90 [45–100] | 90 [50–100] | .76 |
| IPI | .005 | |||
| 0–1 | 6 (16) | 6 (38) | 0 (0) | |
| 2–4 | 19 (50) | 7 (44) | 12 (55) | |
| 4–5 | 13 (34) | 3 (19) | 10 (45) | |
| Bulky disease >5 cm | 26 (53) | 10 (50) | 16 (55) | .77 |
| BM Involvement, no (%) | 10 (20) | 4 (20) | 6 (21) | .99 |
| Morphology | .75 | |||
| DLBCL | 36 (73) | 15 (75) | 21 (72) | |
| BCLU | 11 (22) | 5 (25) | 6 (21) | |
| Not classified | 2 (4) | 0 (0) | 2 (7) | |
| Induction therapy | .008 | |||
| R-CHOP | 17 (35) | 12 (60) | 5 (17) | |
| R-EPOCH | 17 (35) | 3 (15) | 14 (48) | |
| Burkitt likea | 11(22) | 3 (15) | 8 (28) | |
| Other | 4 (8) | 2 (10) | 2 (7) | |
| Transplantation in first remission | 0 (0) | 0 (0) | 0 (0) | NS |
Abbreviations: BCLU, B-cell lymphoma unclassifiable with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma; BM, bone marrow; DLBCL, diffuse large B-cell lymphoma; IPI, International Prognostic Index; NS, nonsignificant; R-CHOP, rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; R-EPOCH, rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin.
The Burkitt-like therapies were rituximab, cyclophosphamide, vincristine, doxorubicin, methotrexate, ifosfamide, etoposide, and cytarabine (R-CODOX-M/R-IVAC) (n = 6); rituximab, hyperfractionated cyclophosphamide, vincristine, doxorubicin, dexamethasone, methotrexate, and cytarabine (R-Hyper-CVAD) (n = 4); or R-CHOP with high-dose methotrexate (n = 1).
Therapy Received
Initial therapy varied across patients and included R-CHOP (n = 17), DA-R-EPOCH (n = 17), a Burkitt-like regimen ([R-CODOXM/R-IVAC]; rituximab, hyperfractionated cyclophosphamide, vincristine, doxorubicin, dexamethasone, methotrexate, and cytarabine [R-Hyper-CVAD]; or R-CHOP with high-dose methotrexate; n = 11), or an alternative regimen (n = 4). Initial therapy was different between the 2 groups: the patients with double-hit NHL were more likely to receive DA-R-EPOCH or a Burkitt-like regimen, whereas myc-positive patients were more likely to receive R-CHOP (P = .013). In addition, morphology was significantly associated with induction regimen (P = .001), and patients who had BCLU were more likely to receive a Burkitt-like regimen (64% vs 11%) and were less likely to receive R-CHOP (9% vs 43%) compared with patients who had DLBCL.
Physician-Assessed Response to Therapy
Nine patients died before the first response assessment after 1 (n = 5), 2 (n = 3), or 3 (n = 1) cycles of therapy. Of the 40 remaining patients, 38 patients were assessed with PET/CT, 1 patient was assessed with CT, and 1 patient who had central nervous system disease was assessed with CT and brain magnetic resonance imaging. Twenty-nine of 49 treated patients (59%) achieved a complete response (CR) by physician assessment, and 20 did not (partial response [PR], n = 2; stable disease, n = 1; refractory disease, n = 8; death before assessment, n = 9). Both patients who did not undergo a PET/CT scan achieved a physician-assessed CR and were relapse-free at last follow-up. Thirteen of the 29 patients with double-hit NHL achieved a CR (45%; 95% confidence interval [CI], 26%–64%), including 7 patients who received DA-R-EPOCH, 3 patients who received R-CHOP, and 3 patients who received a Burkitt-like regimen. In 14 myc-positive only patients, 10 achieved a CR (71%; 95% CI, 42%–92%), including 6 who received R-CHOP, 1 who received DA-R-EPOCH, 2 who received a Burkitt-like regimen, and 1 who received other regimens. Decreased IPI (P = .002) and lack of B-symptoms (P = .02) at diagnosis were both associated with achievement of a CR in the univariate setting. CR was not significantly associated with morphology (P = .95), induction regimen (P >.70), or the presence of t(14;18) (P = .12) (see Table 2).
TABLE 2.
Characteristics of Patients With and Without Physician-Assessed Complete Response
| Characteristic | No. of Patients (%) | ||
|---|---|---|---|
|
| |||
| No Induction CR, n = 20 | Induction CR, n = 29 | P | |
| Translocation t(14;18) | .12 | ||
| No | 4 | 10 | |
| Yes | 16 | 13 | |
| IPI at diagnosis: Median [range] | 4 [2–5] | 2 [0–5] | .0003 |
| IPI group | .0012 | ||
| Low: 0–1 | 0 | 6 | |
| Intermediate: 2–3 | 5 | 14 | |
| High: 4–5 | 10 | 3 | |
| Sex | .57 | ||
| Women | 10 | 12 | |
| Men | 10 | 17 | |
| Age at diagnosis: Median [range], y | 64.5 [40–83] | 57 [23–82] | .014 |
| Age >60 y at diagnosis | .14 | ||
| No | 6 | 15 | |
| Yes | 14 | 13 | |
| B-symptoms | .04 | ||
| No | 5 | 17 | |
| Yes | 15 | 12 | |
| Ki-67: Median [range], % | 92.5 [60–100] | 85 [45–100] | .60 |
| Regimen group | .70 | ||
| Burkitt like | 5 | 6 | |
| R-CHOP | 5 | 12 | |
| R-EPOCH | 8 | 9 | |
| Other | 2 | 2 | |
| Morphology | .70 | ||
| BCLU | 4 | 7 | |
| DLBCL | 15 | 22 | |
| Other | 1 | 0 | |
| Bulky disease >5 cm | .077 | ||
| No | 5 | 14 | |
| Yes | 14 | 12 | |
| Elevated LDH | .26 | ||
| No | 2 | 7 | |
| Yes | 17 | 18 | |
| BM involvement | .99 | ||
| No | 15 | 22 | |
| Yes | 4 | 6 | |
Abbreviations: BCLU, B-cell lymphoma unclassifiable with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma; BM, bone marrow; CR, complete response; DLBCL, diffuse large B-cell lymphoma; IPI, International Prognostic Index; LDH, lactate dehydrogenase; R-CHOP, rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; R-EPOCH, rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin.
Centrally Reviewed Post-Treatment and Interim PET/CT
Post-treatment PET/CT scans were available for central review from 25 of the 40 patients who completed induction therapy, including 16 patients who had documented double-hit NHL. Ten post-treatment PET/CT scans were negative by central review, including 7 from patients with double-hit NHL. Fifteen post-treatment PET/CT scans were positive by central review, including 9 from patients with double-hit NHL. Of 19 patients who achieved a physician-assessed CR and had post-treatment scans available, 9 were positive by central review, and all remain in remission at last follow-up after initial front-line therapy. Among these 9 patients, the maximum standard uptake value (SUV) for sites that were considered positive by central review ranged from 2.4 to 4.3, whereas the difference between active sites and liver uptake ranged from 0.5 to 1.5. The 6 remaining positive post-treatment PET/CT scans were from patients who had primary refractory disease (n = 5) or who achieved a physician-assessed PR (n = 1). All 5 refractory patients died within 15 months of diagnosis, and the patient who had a PR progressed and died 14 months after diagnosis.
Twenty-eight patients had centrally reviewed interim PET/CT scans, including 18 patients with double-hit NHL; these interim PET/CT scans were conducted after 2 (n = 12), 3 (n = 11), or 4 (n = 4) cycles of therapy. Twenty-three patients were positive on interim PET/CT scans, including 15 with double-hit NHL. Overall, 24 patients had both post-treatment and interim PET/CT scans available for central review; for 18 patients, the 2 scans were concordant; and, overall, the PET/CT results had moderate agreement between interim and post-treatment scans (kappa = 0.47; P = .02). Among all 28 patients who had an available interim PET/CT scan, the results of the interim scan accurately predicted the physician-assessed response at the completion of therapy in 14 patients. Although the negative predictive value of a negative interim PET/CT scan for end-of therapy response was 100%, the positive predictive value was only 26%.
PFS and OS Outcomes
At the time of these analyses, 24 patients had died, and the median follow-up was 28.5 months (range, 7.8–45.3 months) in living patients. The median PFS across all 49 myc-positive patients was 16.6 months (95% CI, 8 months to not yet reached [NR]). The median PFS for documented double-hit patients was 8 months (95% CI, 5.4 months to NR), whereas the median PFS for myc-positive only patients had not been reached (95% CI, 16.6 months to NR; P = .049) (Fig. 1A). Variables that were significantly associated with PFS included IPI (P = .0005), age (P = .001), and B-symptoms (P = .02) (see Table 3). Attainment of a physician-assessed CR to induction therapy was highly significant for PFS (P <.00001), and the median PFS for patients who achieved a CR had not been reached (95% CI, NR to NR) compared with 3.3 months (95% CI, 2.0–7.1 months) for patients who did not achieve a CR (P <.00001) (Fig. 2A). Nineteen of the 20 patients who did not achieve a CR progressed, and none survived to undergo transplantation. One patient was lost to follow-up at 14 months without evidence of relapse. Four of the 29 patients who had a physician-assessed CR relapsed at 6 months, 10 months, 11 months, and 17 months, although 2 patients were successfully salvaged by autologous transplantation and remained in remission. The median PFS for patients with documented double-hit NHL who achieved a CR had not yet been reached (95% CI, NR to NR) versus 3.9 months (95% CI, 1.8–8.0 months) for those who did not achieve a CR (P <.0001). In the 14 patients documented to not have t(14;18), the median PFS had not yet been reached in the 10 patients who achieved a CR (95% CI, NR to NR) versus a median PFS of 2.7 months in the 4 patients who did not achieve a CR (95% CI, 1.9 months to NR).
Figure 1.
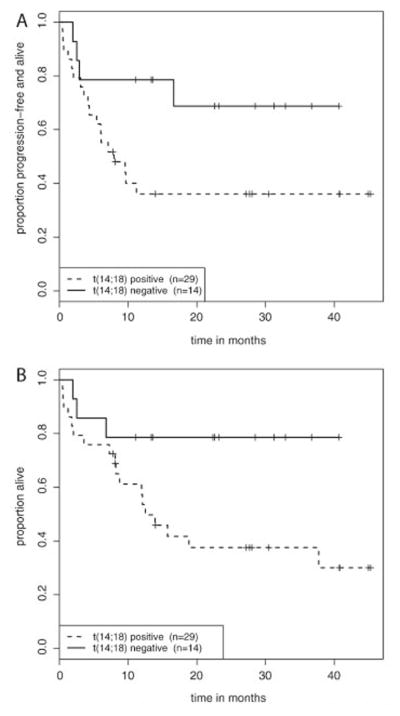
(A) Progression-free survival and (B) overall survival are illustrated for patients with myc-positive versus double-hit non-Hodgkin lymphoma.
TABLE 3.
Univariate Analysis of the Factors Associated With Progression-Free and Overall Survival
| Factor | PFS | OS | ||
|---|---|---|---|---|
|
| ||||
| HR | P | HR | P | |
| Translocation t(14;18) | 2.85 | .049 | 3.41 | .037 |
| Induction CR | 0.038 | <.00001 | 0.013 | <.00001 |
| IPI at diagnosis | 2.67 | .0002 | 2.3 | .0004 |
| IPI groupa | 6.28 | .00014 | 4.22 | .0013 |
| Men | 0.85 | .69 | 0.78 | .57 |
| Age at diagnosis | 1.05 | .006 | 1.06 | .002 |
| Age >60 y at diagnosis | 2.52 | .045 | 3.05 | .02 |
| B-symptoms | 2.73 | .02 | 3.10 | .014 |
| Ki-67 | 1.001 | .92 | 1.01 | .48 |
| Regimen groupb | ||||
| R-CHOP | 0.88 | .82 | 0.58 | .38 |
| R-EPOCH | 1.32 | .62 | 1.22 | .73 |
| Other | 2.2 | .35 | 1.97 | .36 |
| DLBCL vs BCLU | 1.24 | .67 | 0.92 | .86 |
| Bulky disease >5 cm | 1.60 | .31 | 1.63 | .30 |
| Elevated LDH | 2.37 | .25 | 1.87 | .32 |
| BM involvement | 1.55 | .36 | 1.44 | .48 |
Abbreviations: BCLU, B-cell lymphoma unclassifiable with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma; BM, bone marrow; CR, complete response; DLBCL, diffuse large B-cell lymphoma; HR, hazard ratio; IPI, International Prognostic Index; LDH, lactate dehydrogenase; OS, overall survival; PFS, progression-free survival; R-CHOP, rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; R-EPOCH, rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin.
IPI group was treated as an ordinal variable (low vs intermediate vs high).
The reference group was patients who received Burkitt-like regimens.
Figure 2.
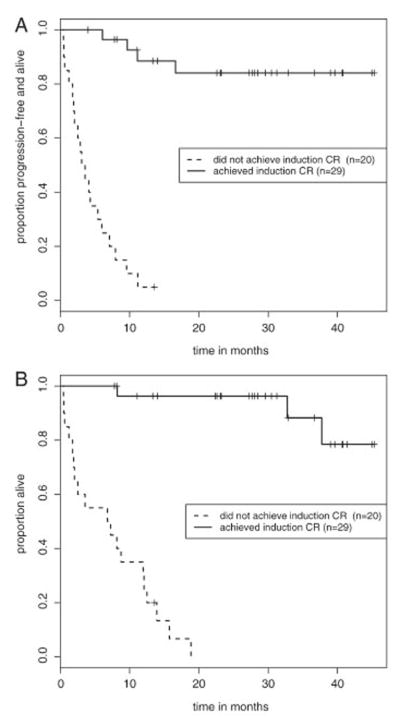
(A) Progression-free survival and (B) overall survival are illustrated for patients with myc-positive and double-hit non-Hodgkin lymphoma based on the achievement of physician-assessed complete response (CR).
The median OS for the entire cohort was 37.7 months (95% CI, 13.9 months to NR). The median OS for those with double-hit NHL was 12.5 months (95% CI, 8.2 months to NR), and the estimated medians and CIs for OS were not yet reached for the myc-positive patients without documented t(14;18) as well as those with documented absence of t(14;18). The documented presence or absence of t(14;18) was significantly associated with OS (P = .037) (Fig. 1B). In the univariate setting, increased IPI (P = .0005), increased age at diagnosis (P = .015), the presence of B-symptoms (P = 0.014), and failure to achieve a CR (P <.00001) were significantly associated with shortened OS (see Table 3). The median OS for those patients who did not achieve a physician-assessed CR was 7.0 months (95% CI, 2.0–12.5 months) compared with a median not reached for those who did achieve a CR (95% CI, NR to NR; P <.00001) (Fig. 2B).
Among the 22 patients who have died, 18 had double-hit NHL, 3 were documented as myc-positive only, and 1 was myc-positive with unknown t(14;18) status. Causes of death included progressive disease (n = 12), organ failure (n = 3), sepsis/infection (n = 4), cardiac arrest (n = 1), and unknown causes (n = 2). Nineteen of the 20 patients who failed to achieve a CR have died. Three of the 29 patients who achieved a physician-assessed CR died 2 months after a relapse, 28 months after relapse and 5 courses of salvage chemotherapy, and of unknown causes 33 months after diagnosis with no evidence of relapse. In 9 patients who died early before response assessment, induction therapies included hyperfractionated cyclophosphamide (n = 2), R-Hyper-CVAD (n = 2), R-CHOP (n = 3), and DA-R-EPOCH (n= 2).
Multivariable Analyses
In multivariable analyses, we evaluated the influence of achieving a CR and having documented double-hit NHL (excluding those with unknown t[14;18] status) on PFS and OS while adjusting for IPI, age at diagnosis, and the presence of B symptoms; in the end, the optimal models for both PFS and OS only adjusted for whether or not age at diagnosis was >60 years (Table 4). In the multivariable model for PFS, achievement of CR was significantly associated with increased PFS (hazard ratio [HR], 0.027; P <.00001), and documented double-hit NHL status was still significantly associated with a worse prognosis (HR, 4.46; P = .033) as was age at diagnosis >60 years (HR, 4.98; P = .004). In multivariable analyses for OS, achieving a CR was significant and was associated with improved survival (HR, 0.01; P = .00002) as well as whether or not the patient was aged >60 years at diagnosis (HR, 4.46; P = .009). Even when the 6 patients with unknown t(14;18) status were included as myc-positive patients in the OS model, the results did not change. Evaluations of the PFS and OS distributions based on both double-hit NHL status and achievement of CR are illustrated in Figure 3.
TABLE 4.
Multivariable Analysis of the Factors Associated With Progression-Free Survival
| Factor | PFS | OS | ||
|---|---|---|---|---|
|
| ||||
| HR | P | HR | P | |
| Induction CR | 0.027 | <.00001 | 0.01 | .00002 |
| Translocation t(14;18) | 4.46 | .033 | – | – |
| Age >60 y at diagnosis | 4.98 | .004 | 4.46 | .009 |
Abbreviations: CR, complete response; HR, hazard ratio; OS, overall survival; PFS, progression-free survival.
Figure 3.
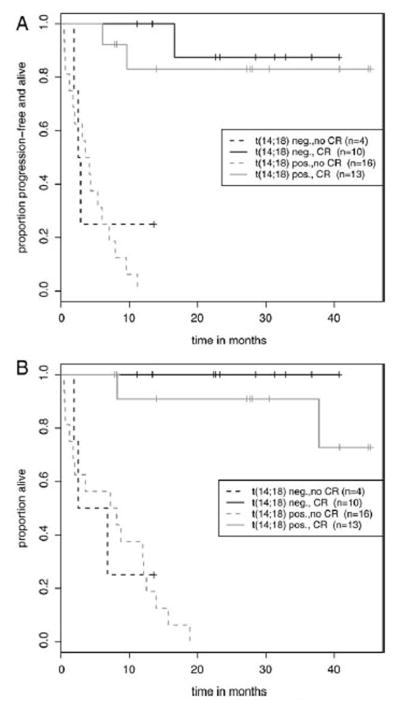
(A) Progression-free survival and (B) overall survival are illustrated for patients with non-Hodgkin lymphoma (NHL) who were myc-positive and achieved a complete response (CR) versus those who were myc-positive and did not achieve a CR and for patients who had double-hit NHL and achieved a CR versus those who had double-hit NHL (t(14;18) pos.) and did not achieve a CR. t(14;18) neg. denotes patients who did not have double-hit NHL.
DISCUSSION
Our retrospective studies indicate that 59% of patients with myc-positive and double-hit lymphomas can achieve a CR with initial therapy, and the estimated 2-year PFS rate was 81% (95% CI, 68%–98%) for the patients who achieved a CR. Even with double-hit lymphoma, 45% of these patients were able to achieve a CR with an estimated 2-year PFS rate of 83% (95% CI, 64%–99%). In our series, morphology and induction regimen were not associated with CR, PFS, or OS. Although documented double-hit NHL, IPI, age at diagnosis, and the presence of B-symptoms were associated with OS in univariable analysis, only CR was independently associated with OS in multivariable analysis, suggesting that initial response to front-line therapy is an important prognostic factor. This independent association of CR with PFS and OS was significant despite the removal of 6 patients from the analysis who were myc-positive but did not have an assessment for t(14;18). Whereas t(14;18) status and age remained significant in the multivariable setting for PFS, their significance was borderline (P = .046 and P = .045, respectively); achievement of CR was a clear and strong prognostic factor (P = .0006).
Patients in our series with myc-positive NHL but without t(14;18), many of whom received treatment with R-CHOP, had not reached a median PFS after >2 years of follow-up. These findings are in contrast to the series by Savage et al and 3 additional series of 100 to 245 patients with DLBCL, of which 11 to 35 patients were myc-positive, and myc-positive patients had inferior PFS and OS.1,13–15 A review of 57 patients with BCLU, including 30 who were myc-positive, indicated that myc-positive patients had shortened PFS with R-CHOP compared with more intensive regimens (P = .0358).16 Because our series did not include a group without CMYC rearrangements, definitive comparisons cannot be made with myc-negative patients. However, our data suggest that patients with myc-positive DLBCL without t(14;18) may not require intensification of therapy, especially in the absence of other clinical risk factors.
Many centers incorporate autologous transplantation in first remission for all of their patients with double-hit NHL, which, based on our current study, may not be necessary for patients who achieve a CR. None of our patients who failed to achieve a CR responded to salvage therapy or underwent autologous transplantation. Therefore, earlier recognition of these poor responders may be necessary. Unfortunately, in our trial, interim PET studies or other pretreatment characteristics like stage, IPI, etc, did not readily predict which patients were unlikely to respond. In addition, 9 patients died during initial induction therapy, highlighting the truly dismal prognosis for these patients and the limited time available to alter therapy to favorably impact disease outcomes.
We recognize the limitations of relying on a physician assessment of response using a PET/CT scan at the time of therapy; therefore, we included a central review of all available interim and post-treatment PET/CT scans by 1 nuclear medicine physician. It is noteworthy that 9 patients who were deemed to be in CR after completing therapy by their treating physician actually had a positive post-treatment PET/CT scan by central review. None of these patients have relapsed, suggesting that using standard criteria without clinical assessment may expose patients inappropriately to additional therapy.
Although our limited sample makes it challenging to draw conclusions regarding the impact of an interim PET/CT scan, its prognostic value in patients with aggressive NHL remains unclear. Cashen et al reported a series of 50 patients with DLBCL who received R-CHOP and underwent interim PET/CT scans. In that study, a positive PET/CT scan, interpreted according to International Harmonization Project criteria,17 had only a 42% positive predictive value for relapse.18 Pregno and colleagues evaluated 88 patients with DLBCL who received R-CHOP, and interim PET/CT scans had only a 36% positive predictive value for progression.19 Interim PET/CT scans in our series had a positive predictive value of 26%, again suggesting that prolonged remission is possible despite a positive interim PET/CT result.
Recent data have suggested that the translocation partner for CMYC may influence outcome, because those patients who have a nonimmunoglobulin gene translocation partner may have prolonged PFS.20 In addition, myc and bcl2 overexpression by immunohistochemistry (IHC) has also been associated with inferior PFS and OS. Green and colleagues identified 29% of patients in their series with overexpression of both Myc and Bcl2 proteins, and this was associated with shorter OS and PFS compared with patients who had 1 or 0 proteins overexpressed.7 Johnson et al evaluated 307 patients with DLBCL in a training set and a validation set. In that study, Myc was overexpressed in 100 patients, whereas FISH indicated that only 12% of patients were myc-positive. Overexpression by IHC of both myc and bcl2 was associated with inferior PFS and OS (P <.05).3 Consequently, assessment by IHC may identify a larger group of patients who are at increased risk for poor outcomes that may not be identified through FISH alone. However, it may not be feasible to treat so many patients with more intensive therapy when a large portion may otherwise achieve a CR with standard R-CHOP.3,7 Given the retrospective nature of our study, these specific analyses were not routinely performed.
In conclusion, myc-positive and double-hit NHLs continue to present therapeutic challenges. Here, we have identified a subset of patients who achieved a CR and experienced prolonged remissions, whereas those who failed to do so had dismal outcomes. The development of effective front-line regimens is needed, as salvage opportunities are limited because of rapid disease progression and early death. In addition, the identification of risk factors for patients associated with a failure to achieve a CR will aid in determining which patients with myc-positive NHL should receive standard front-line therapy versus those who are more suited for experimental approaches.
Acknowledgments
FUNDING SUPPORT
No specific funding was disclosed.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
References
- 1.Savage KJ, Johnson NA, Ben-Neriah S, et al. MYC gene rearrangements are associated with a poor prognosis in diffuse large B-cell lymphoma patients treated with R-CHOP chemotherapy. Blood. 2009;114:3533–3537. doi: 10.1182/blood-2009-05-220095. [DOI] [PubMed] [Google Scholar]
- 2.Cuccuini W, Briere J, Mounier N, et al. MYC+ diffuse large B-cell lymphoma is not salvaged by classical R-ICE or R-DHAP followed by BEAM plus autologous stem cell transplantation. Blood. 2012;119:4619–4624. doi: 10.1182/blood-2012-01-406033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson NA, Slack GW, Savage KJ, et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol. 2012;30:3452–3459. doi: 10.1200/JCO.2011.41.0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horn H, Ziepert M, Becher C, et al. MYC status in concert with BCL2 and BCL6 expression predicts outcome in diffuse large B-cell lymphoma. Blood. 2013;121:2253–2263. doi: 10.1182/blood-2012-06-435842. [DOI] [PubMed] [Google Scholar]
- 5.Snuderl M, Kolman OK, Chen YB, et al. B-cell lymphomas with concurrent IGH-BCL2 and MYC rearrangements are aggressive neoplasms with clinical and pathologic features distinct from Burkitt lymphoma and diffuse large B-cell lymphoma. Am J Surg Pathol. 2010;34:327–340. doi: 10.1097/PAS.0b013e3181cd3aeb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson NA, Savage KJ, Ludkovski O, et al. Lymphomas with concurrent BCL2 and MYC translocations: the critical factors associated with survival. Blood. 2009;114:2273–2279. doi: 10.1182/blood-2009-03-212191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Green TM, Young KH, Visco C, et al. Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol. 2012;30:3460–3467. doi: 10.1200/JCO.2011.41.4342. [DOI] [PubMed] [Google Scholar]
- 8.Abramson JS, Barnes JA, Feng Y, et al. Double hit lymphomas: evaluation of prognostic factors and impact of therapy [abstract] Blood (ASH Annual Meeting Abstracts) 2012;120:Abstract 1619. [Google Scholar]
- 9.Dunleavy K, Pittaluga S, Wayne AS. MYC+ aggressive-B-cell lymphomas: novel therapy of untreated Burkitt lymphoma (BL) and MYC+ diffuse large B-cell lymphoma (DLBCL) with DA-EPOCH-R [abstract] Ann Oncol. 2011;22(suppl 4):106. Abstract 071. [Google Scholar]
- 10.Jaglal MV, Peker D, Tao JG, Cultrera JL. Double and triple hit diffuse large B cell lymphomas and first line therapy [abstract] Blood (ASH Annual Meeting Abstracts) 2012;120:Abstract 4885. [Google Scholar]
- 11.Meignan M, Gallamini A, Haioun C, Polliack A. Report on the Second International Workshop on interim positron emission tomography in lymphoma held in Menton, France, 8–9 April 2010. Leuk Lymphoma. 2010;51:2171–2180. doi: 10.3109/10428194.2010.529208. [DOI] [PubMed] [Google Scholar]
- 12.Fleiss JL, Levin BA, Paik MC. Statistical Methods for Rates and Proportions. 3. Hoboken, NJ: Wiley-Interscience; 2003. [Google Scholar]
- 13.Barrans S, Crouch S, Smith A, et al. Rearrangement of MYC is associated with poor prognosis in patients with diffuse large B-cell lymphoma treated in the era of rituximab. J Clin Oncol. 2010;28:3360–3365. doi: 10.1200/JCO.2009.26.3947. [DOI] [PubMed] [Google Scholar]
- 14.Kojima M, Nishikii H, Takizawa J, et al. MYC rearrangements are useful for predicting outcomes following rituximab and chemotherapy: multicenter analysis of Japanese patients with diffuse large B-cell lymphoma. Leuk Lymphoma. 2013;54:2149–2154. doi: 10.3109/10428194.2013.771398. [DOI] [PubMed] [Google Scholar]
- 15.Akyurek N, Uner A, Benekli M, Barista I. Prognostic significance of MYC, BCL2, and BCL6 rearrangements in patients with diffuse large B-cell lymphoma treated with cyclophosphamide, doxorubicin, vincristine, and prednisone plus rituximab. Cancer. 2012;118:4173–4183. doi: 10.1002/cncr.27396. [DOI] [PubMed] [Google Scholar]
- 16.Lin P, Dickason TJ, Fayad LE, et al. Prognostic value of MYC rearrangement in cases of B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma. Cancer. 2012;118:1566–1573. doi: 10.1002/cncr.26433. [DOI] [PubMed] [Google Scholar]
- 17.Juweid ME, Stroobants S, Hoekstra OS, et al. Use of positron emission tomography for response assessment of lymphoma: consensus of the Imaging Subcommittee of International Harmonization Project in Lymphoma. J Clin Oncol. 2007;25:571–578. doi: 10.1200/JCO.2006.08.2305. [DOI] [PubMed] [Google Scholar]
- 18.Cashen AF, Dehdashti F, Luo J, Homb A, Siegel BA, Bartlett NL. 18F-FDG PET/CT for early response assessment in diffuse large B-cell lymphoma: poor predictive value of international harmonization project interpretation. J Nucl Med. 2011;52:386–392. doi: 10.2967/jnumed.110.082586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pregno P, Chiappella A, Bello M, et al. Interim 18-FDG-PET/CT failed to predict the outcome in diffuse large B-cell lymphoma patients treated at the diagnosis with rituximab-CHOP. Blood. 2012;119:2066–2073. doi: 10.1182/blood-2011-06-359943. [DOI] [PubMed] [Google Scholar]
- 20.Pedersen MO, Gang AO, Poulsen TS, et al. MYC translocation partner determines survival in double-hit BCL2/MYC lymphoma. APMIS. 2012;120:6–7. [Google Scholar]


