Abstract
The main complication of Perthes’ disease is femoral head deformation. Evidence from the literature highlights two important factors related to the cause and timing of this complication. (1) Extrusion of the femoral head appears to be a major factor that leads to femoral head deformation. (2) Deformation of the femoral head occurs in the latter part of the stage of fragmentation. The likelihood of preventing femoral head deformation is over 16 times higher if extrusion is reversed or prevented by the early stage of fragmentation than if done later. Several treatment options have been described in children who present later in the course of the disease but the outcomes of all these measures do not compare with those of early intervention.
Keywords: Containment, femoral head deformation, Perthes’ disease, prevention
MeSH terms: Prognosis treatment protocols, legg-calve, perthes, hip, children
INTRODUCTION
Perthes’ disease was described over a 100 years ago, but the aetiology of the disease has not been established, and there is no consensus on the optimal treatment. The major emphasis of this article is to highlight a rational approach of treatment that aims to prevent the femoral head from getting deformed by intervening early in the course of the disease. Treatment options later in the course of the disease have also been mentioned.
Aim of treatment
Perthes’ disease is a self-limiting disease of children characterized by interruption of the blood supply to the capital femoral epiphysis resulting in necrosis of the epiphysis. The vascular occlusion is temporary; complete re-vascularization of the epiphysis occurs over a period of 2-4 years if the child is under 12 years of age at onset of the disease.1,2 During the process of re-vascularization the necrotic bone is completely replaced by healthy new bone.3,4 In some children the disease heals without any sequelae and consequently no treatment is needed in these children. However, treatment is needed in a significant proportion of children in whom the femoral head is likely to get deformed while epiphyseal re-vascularization occurs. Secondary degenerative arthritis is likely to develop in mid-adult life if the femoral head does get deformed. The aim of treatment of these susceptible children should be to prevent the femoral head from getting deformed.
In order to achieve this aim, we need to understand what causes the femoral head to get deformed and when during the evolution of the disease irreversible deformation of the femoral head occurs.
PATHOGENESIS AND TIMING OF FEMORAL HEAD DEFORMATION
The bone necrosis that follows the vascular occlusion triggers changes in the soft tissue of the hip joint which include synovitis,5,6,7 articular cartilage hypertrophy8 and hypertrophy of the ligamentum teres.9 These soft tissue changes and muscle spasm cause the femoral head to extrude out laterally of the acetabulum. Stresses of weight-bearing and muscular contraction pass across the acetabular margin onto the extruded part of the avascular femoral head. Unlike normal healthy bone, the avascular bone is not capable of withstanding these physiological stresses and the trabeculae collapse; this results in irreversible femoral head deformation.10,11 Extrusion appears to be a prime factor that predisposes to femoral head deformation; the greater the extrusion, the greater the propensity for femoral head deformation. If more than 20% of the width of the epiphysis extrudes outside the acetabulum irreversible femoral head deformation is almost inevitable.12,13
The natural evolution of Perthes disease can be clearly identified on plain radiographs. The disease passes through the stages of avascular necrosis, fragmentation, and reconstitution (Stages I-III) before the disease finally heals (Stage IV).14 The stages of avascular necrosis, fragmentation, and reconstitution can be further divided into early and late stages [Stages Ia, Ib, IIa, IIb, IIIa and IIIb – Figure 1].13 In untreated children femoral head extrusion increases as the disease progresses; in the initial stages of the disease the increase in extrusion is gradual but extrusion abruptly increases in the late stage of fragmentation (Stage IIb), often exceeding the critical 20%. There is evidence that the femoral head deformation occurs during the late stage of fragmentation or in the early part of the stage of reconstitution.13 This vital knowledge enables us to divide the disease into an early part (i.e., before femoral head deformation begins) and the late part (i.e., after the femoral head has begun to deform). It follows that treatment aimed at preventing femoral head deformation must be instituted in the early part of the disease if it is to be effective. It needs to be emphasized that any treatment instituted at the late stage of fragmentation (Stage IIb) or thereafter is not preventive but either remedial or salvage in nature.
Figure 1.
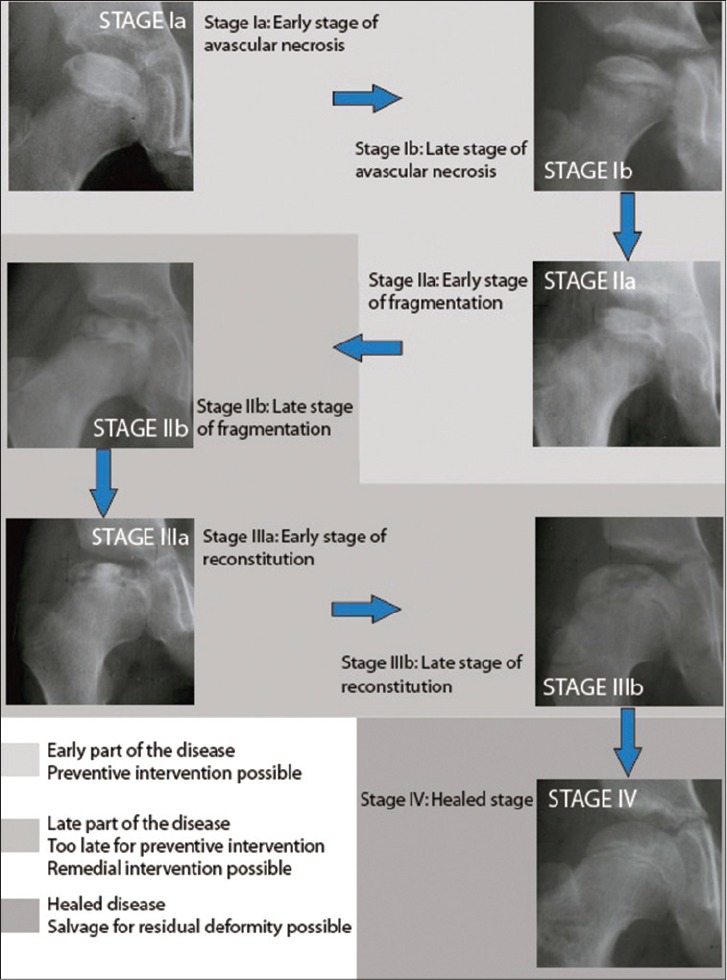
The stages of evolution of Perthes’ disease. The early part of the disease is from the onset till Stage IIa (early fragmentation stage). The late part of the disease is from Stage IIb to Stage IIIb. Intervention aimed at preventing femoral head deformation is only feasible during the early part of the disease
TREATMENT OF PERTHES’: EARLY IN THE COURSE OF THE DISEASE
Treatment early in the course of the disease (i.e. from the onset to the early stage of fragmentation) attempts to prevent the femoral head from bearing forces across the acetabular margin by either preventing or reversing extrusion of the femoral head by “containment.”
Containment is the term used to describe any intervention that places the antero-lateral part of the femoral epiphysis well into the acetabulum thereby protecting the vulnerable part of the epiphysis from being subjected to deforming stresses. Containment can be achieved by two different methods; the first involves keeping the hip in abduction and internal rotation or in abduction and flexion by casting, bracing or by surgery on the femur. Alternatively, containment can be achieved by an osteotomy of the pelvis that re-orients the acetabulum such that it covers the antero-lateral part of the femoral epiphysis (e.g. Salter osteotomy, triple innominate osteotomy) or by creating a bony shelf over the extruded part of the epiphysis [Figure 2].
Figure 2.
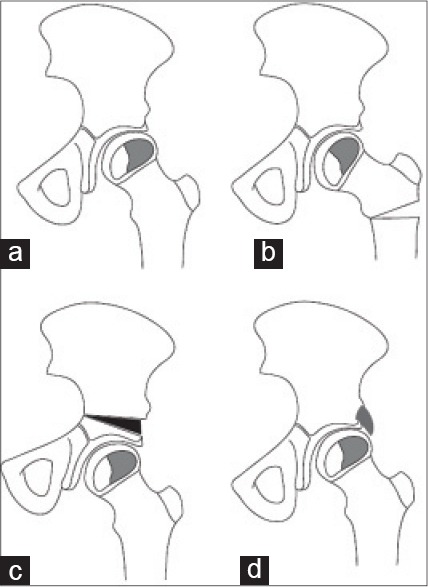
Schematic diagram of surgical options for containment of an extruded avascular femoral epiphysis (a) include proximal femoral varus osteotomy (b) innominate osteotomy (c) and shelf procedure (d)
Extrusion invariably occurs sooner or later in children over the age of 7 years at the onset of the disease13,15 and hence containment should be ensured as soon as the disease is diagnosed. In children under 7 years at the onset of the disease extrusion may or may not occur; these children need to be monitored closely with anteroposterior and frog-lateral radiographs, every 3 or 4 months and containment ensured as soon as extrusion is identified without any delay. Most children who are under the age of 5 years at the onset of the disease have a favorable prognosis but some fare badly.16,17 Containment will be needed even in these young children if extrusion occurs.17
Though the importance of containment in the early part of the disease was emphasized repeatedly by several authors this has often been ignored.18,19,20,21,22 It is important that their advice is followed as the odds ratio of avoiding femoral head deformation is 16.58 times higher if containment is achieved early in the disease (Stage IIa or earlier) than if it is achieved late in the disease (Stage IIb or later).23
The range of motion should be restored before effective containment can be achieved. Skin traction for a week usually restores motion. If this fails a broom-stick cast in wide abduction can be applied under general anesthesia and retained for 6 weeks; hip motion improves once the cast is removed.
The effect of surgical containment lasts throughout the course of the disease, but the containment effect of bracing or casting is present only as long as the device is worn. Since the propensity for femoral head deformation persists till the early stage of reconstitution (Stage IIIa) the brace or splint must be worn till the disease has progressed beyond this point but need not be continued till complete healing of the disease has occurred.24
The author advocates avoiding weight-bearing in addition to containment as some reports suggest that combining weight relief with containment may be beneficial.25
TREATMENT PLANNING
The factors to take into consideration to decide the treatment include:
The age of the child at the onset of symptoms
The presence of extrusion of the femoral head
The range of motion of the hip
The stage of evolution of the disease.26
The outline of treatment that takes these variables into consideration is shown in Table 1.
Table 1.
Outline of decision-making for treatment of Perthes’ disease early in the course of the disease
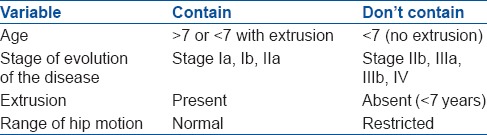
Two factors widely used for treatment planning, the status of the lateral pillar (Herring's grading) and the extent of epiphyseal involvement (Caterall's grouping) have not been included in the decision-making scheme outlined in table. This is because treatment needs to be initiated well before the stage of fragmentation when these two variables can be identified with some degree of certainty.27
Children may not qualify for containment based on the decision-making outline shown in Table 1; these include children who do not need containment as the prognosis is good (e.g., a 6-year-old child in Stage IIa with no extrusion) and children who are denied containment since it is too late for containment to be of benefit (children in Stage IIb or later). Both these groups of children need no active intervention but should be followed up till skeletal maturity to evaluate their outcome.
What is the effect of containment?
Several studies suggest that children over the age of 6 years at onset of the disease and in whom more than half the epiphysis is avascular are likely to benefit from containment.28,29,30,31,32,33,34,35,36 The chances of retaining a spherical femoral head with minimal coxa magna are greater when containment is performed.
Contrary to earlier views that surgical containment has no effect on the healing process37,38 it has been shown that the duration of the disease is significantly shortened with a third of children by-passing the stage of fragmentation when a varus osteotomy is performed in the stage of avascular necrosis.32
How much of containment is needed?
Kim et al. suggest that a modest varus angulation of 10-15° is sufficient to obtain adequate containment by a femoral varus osteotomy;39 the author prefers to create a varus angulation of 20° [Figure 3].26,32
Figure 3.
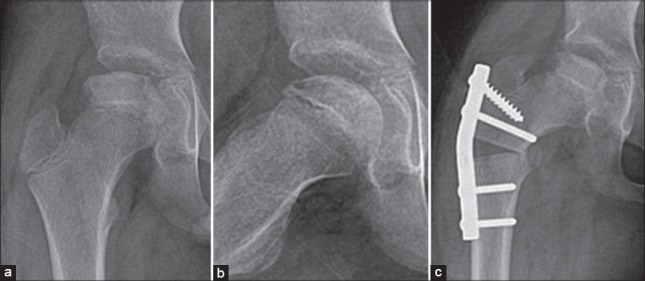
Anteroposterior (a) and frog leg lateral (b) radiographs of the hip of an 11-year-old boy with Perthes’ disease in the early stage of the disease. An open wedge varus osteotomy with 20° of angulation has been performed (c)
Excellent containment can be obtained with the triple pelvic osteotomy; however, there is a risk of over-coverage and pincer impingement. The acetabular fragment must not be rotated so far as to increase the CE angle beyond 44° when a triple pelvic osteotomy is performed.40
There are no studies that attempt to determine how large a shelf is required to provide adequate containment without causing impingement.
TREATMENT OF PERTHES’: LATE IN THE COURSE OF THE DISEASE (REMEDIAL SURGERY)
Treatment in the late part of the stage of fragmentation or in the early part of the stage of reconstitution attempts to minimize the effects of early deformation of the femoral head that has already occurred. At this stage, some children have a reduced range of motion (particularly abduction) and attempted abduction results in hinging.41 A valgus femoral osteotomy overcomes the hinging and brings a more congruent surface of the femoral head under the acetabulum.42 The operation should be performed in the advanced stage of reconstitution rather than in the late part of the fragmentation stage because sufficient reconstitution of the femoral head should have occurred enough to withstand weight-bearing stresses without getting deformed.42 A valgus osteotomy will increase uncovering of the femoral head, and this can be addressed with a shelf procedure.41 However, the shelf procedure should be delayed in the younger child as the acetabular cover may improve spontaneously once the abnormal forces on the lateral rim of the acetabulum while hinging are relieved by the valgus osteotomy.41
The valgus osteotomy when performed for hinge abduction relieves pain and improves functional scores but only in a small proportion of hips (~10%) will the femoral head remain spherical and end up as Stulberg Class I or II (spherical head); the majority will fall into Class III and IV (non-spherical).41,42 The role of containment at this phase of the disease remains uncertain.43,44
Arthrodiatasis and epiphyseal drilling
Apart from containment (which is most widely practiced) some surgeons have attempted arthrodiatasis or joint distraction with an external fixator in an attempt to unload the hip and facilitate the restoration of epiphyseal height.45,46 The reported results have not been sufficiently encouraging to recommend this as the procedure of choice.46 Yet another approach has been to drill the epiphysis in the hope that this will hasten re-vascularization; reports on the long term outcome of this method of treatment are awaited.47
TREATMENT OF THE SEQUELAE OF THE DISEASE (SALVAGE SURGERY)
In recent times, there has been enthusiasm to attempt to re-shape the deformed femoral head and the acetabulum following Perthes’ disease by safe surgical dislocation of the hip.48,49,50 Abnormalities such as cam impingement, pincer impingement, functional retroversion and greater trochanteric and lesser trochanteric impingement have all been noted and addressed. The surgical procedures performed on young adults are included under what is termed as “joint preserving surgery.”48 Reduction of pain, increased joint motion and improved strength of the hip abductors have been reported after such intervention. Survival analysis demonstrated that 61% of the patients had not undergone a total hip replacement 8 years after the surgery, while 39% had already undergone hip replacement by this time. It remains to be seen how much longer the surviving hips will function to decide if these procedures do really preserve the hip. A longer followup is clearly needed to answer this question particularly because a study from Norway noted that a third of young adults undergoing total hip replacement for degenerative joint disease secondary to Perthes disease had undergone ‘joint preserving surgery’ prior to the hip replacement.51
Treatment of established degenerative joint disease following Legg-Calvé-Perthes disease
Total hip replacement is required once secondary degenerative arthritis develops.52 The surgery may need to be modified to deal with structural changes in the proximal femur and the acetabulum that follows Perthes’ disease. A higher rate of complications had been noted in some series, but the survival rate of the prosthesis is good.53,54,55 Responses to a standard health-related quality of life questionnaire showed that the patients who underwent total hip replacement for the sequelae of Perthes’ disease had reduced quality of life.53 These observations underscore the overwhelming reason for early preventive intervention in order to preserve the sphericity of the femoral head during the early part of Perthes’ disease.
FUTURE TRENDS
The treatment planning outlined here is based entirely on plain radiographic evaluation of the disease. Recent reports suggest that newer methods of magnetic resonance imaging (MRI) such as perfusion MRI may hold promise in treatment planning and currently studies evaluating the efficacy of these imaging techniques are underway.56,57
CONCLUSION
Treatment of Perthes disease should aim at preventing femoral head deformation, thereby minimizing the risk of secondary degenerative arthritis. This is possible in a large proportion of instances if the hip is contained early in the course of the disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Catterall A. Legg-Calvé-Perthes’ syndrome. Clin Orthop Relat Res. 1981;158:41–52. [PubMed] [Google Scholar]
- 2.Conway JJ. A scintigraphic classification of Legg-Calvé-Perthes disease. Semin Nucl Med. 1993;23:274–95. doi: 10.1016/s0001-2998(05)80109-6. [DOI] [PubMed] [Google Scholar]
- 3.Jensen OM, Lauritzen J. Legg-Calvé-Perthes’ disease. Morphological studies in two cases examined at necropsy. J Bone Joint Surg Br. 1976;58:332–8. doi: 10.1302/0301-620X.58B3.956251. [DOI] [PubMed] [Google Scholar]
- 4.Salter RB. Legg-Perthes disease: The scientific basis for the methods of treatment and their indications. Clin Orthop Relat Res. 1980;150:8–11. [PubMed] [Google Scholar]
- 5.Howorth MB. Coxa plana. J Bone Joint Surg Am. 1948;30A:601–20. [PubMed] [Google Scholar]
- 6.Matsoukas JA. Viral antibody titers to rubella in coxa plana or Perthes’ disease. Perthes diseases: Is it the late osseous redidua of a minor prenatal rubella? Acta Orthop Scand. 1975;46:957–62. doi: 10.3109/17453677508989284. [DOI] [PubMed] [Google Scholar]
- 7.Joseph B, Pydisetty RK. Chondrolysis and the stiff hip in Perthes’ disease: An immunological study. J Pediatr Orthop. 1996;16:15–9. doi: 10.1097/00004694-199601000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Joseph B. Morphological changes in the acetabulum in Perthes’ disease. J Bone Joint Surg Br. 1989;71:756–63. doi: 10.1302/0301-620X.71B5.2584244. [DOI] [PubMed] [Google Scholar]
- 9.Kamegaya M, Moriya H, Tsuchiya K, Akita T, Ogata S, Someya M. Arthrography of early Perthes’ disease. Swelling of the ligamentum teres as a cause of subluxation. J Bone Joint Surg Br. 1989;71:413–7. doi: 10.1302/0301-620X.71B3.2722932. [DOI] [PubMed] [Google Scholar]
- 10.Rab GT, DeNatale JS, Herrmann LR. Three-dimensional finite element analysis of Legg-Calve-Perthes disease. J Pediatr Orthop. 1982;2:39–44. doi: 10.1097/01241398-198202010-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ueo T, Tsutsumi S, Yamamuro T, Okumura H. Biomechanical analysis of Perthes’ disease using the finite element method: The role of swelling of articular cartilage. Arch Orthop Trauma Surg. 1987;106:202–8. doi: 10.1007/BF00450456. [DOI] [PubMed] [Google Scholar]
- 12.Griffin PP, Green NE, Beauchamp RD. Legg-Calvé-Perthes disease: Treatment and prognosis. Orthop Clin North Am. 1980;11:127–39. [PubMed] [Google Scholar]
- 13.Joseph B, Varghese G, Mulpuri K, Narasimha Rao K, Nair NS. Natural evolution of Perthes disease: A study of 610 children under 12 years of age at disease onset. J Pediatr Orthop. 2003;23:590–600. doi: 10.1097/00004694-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Waldenstrom H. The first stages of coxa plana. J Bone Joint Surg. 1938;20:559–66. [Google Scholar]
- 15.Muirhead-Allwood W, Catterall A. The treatment of Perthes’ disease. The results of a trial of management. J Bone Joint Surg Br. 1982;64:282–5. doi: 10.1302/0301-620X.64B3.7096392. [DOI] [PubMed] [Google Scholar]
- 16.Fabry K, Fabry G, Moens P. Legg-Calvé-Perthes disease in patients under 5 years of age does not always result in a good outcome. Personal experience and meta-analysis of the literature. J Pediatr Orthop B. 2003;12:222–7. doi: 10.1097/01.bpb.0000049583.53117.f7. [DOI] [PubMed] [Google Scholar]
- 17.Canavese F, Dimeglio A. Perthes’ disease: Prognosis in children under six years of age. J Bone Joint Surg Br. 2008;90:940–5. doi: 10.1302/0301-620X.90B7.20691. [DOI] [PubMed] [Google Scholar]
- 18.Axer A. Subtrochanteric osteotomy in the treatment of perthes’ disease: A preliminary report. J Bone Joint Surg Br. 1965;47:489–99. [PubMed] [Google Scholar]
- 19.Axer A, Gershuni DH, Hendel D, Mirovski Y. Indications for femoral osteotomy in Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 1980;150:78–87. [PubMed] [Google Scholar]
- 20.Heikkinen E, Puranen J. Evaluation of femoral osteotomy in the treatment of Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 1980;150:60–8. [PubMed] [Google Scholar]
- 21.Hoikka V, Poussa M, Yrjönen T, Osterman K. Intertrochanteric varus osteotomy for Perthes’ disease. Radiographic changes after 2-16-year followup of 126 hips. Acta Orthop Scand. 1991;62:549–53. doi: 10.3109/17453679108994494. [DOI] [PubMed] [Google Scholar]
- 22.Lack W, Feldner-Busztin H, Ritschl P, Ramach W. The results of surgical treatment for Perthes’ disease. J Pediatr Orthop. 1989;9:197–204. [PubMed] [Google Scholar]
- 23.Joseph B, Nair NS, Narasimha Rao K, Mulpuri K, Varghese G. Optimal timing for containment surgery for Perthes disease. J Pediatr Orthop. 2003;23:601–6. doi: 10.1097/00004694-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Thompson GH, Westin GW. Legg-Calvé-Perthes disease: Results of discontinuing treatment in the early reossification phase. Clin Orthop Relat Res. 1979;139:70–80. [PubMed] [Google Scholar]
- 25.Mintowt-Czyz W, Tayton K. Indication for weight relief and containment in the treatment of perthes’ disease. Acta Orthop Scand. 1983;54:439–45. doi: 10.3109/17453678308996598. [DOI] [PubMed] [Google Scholar]
- 26.Joseph B, Srinivas G, Thomas R. Management of Perthes disease of late onset in southern India. The evaluation of a surgical method. J Bone Joint Surg Br. 1996;78:625–30. [PubMed] [Google Scholar]
- 27.Joseph B, Price CT. Principles of containment treatment aimed at preventing femoral head deformation in Perthes disease. Orthop Clin North Am. 2011;42:317–27. doi: 10.1016/j.ocl.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 28.Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86-A:2121–34. [PubMed] [Google Scholar]
- 29.Stevens PM, Williams P, Menelaus M. Innominate osteotomy for Perthes’ disease. J Pediatr Orthop. 1981;1:47–54. doi: 10.1097/01241398-198101010-00007. [DOI] [PubMed] [Google Scholar]
- 30.Paterson DC, Leitch JM, Foster BK. Results of innominate osteotomy in the treatment of Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 1991;266:96–103. [PubMed] [Google Scholar]
- 31.Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes’ disease: A prospective study of 368 patients with five-year followup. J Bone Joint Surg Br. 2008;90:1364–71. doi: 10.1302/0301-620X.90B10.20649. [DOI] [PubMed] [Google Scholar]
- 32.Joseph B, Rao N, Mulpuri K, Varghese G, Nair S. How does a femoral varus osteotomy alter the natural evolution of Perthes’ disease? J Pediatr Orthop B. 2005;14:10–5. doi: 10.1097/01202412-200501000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Wichlacz W, Sotirow B, Sionek A, Czop A. The surgical treatment of children with Perthes’ disease: 26 years of experience. Ortop Traumatol Rehabil. 2004;6:718–27. [PubMed] [Google Scholar]
- 34.Saran N, Varghese R, Mulpuri K. Do femoral or salter innominate osteotomies improve femoral head sphericity in Legg-Calvé-Perthes disease? A meta-analysis. Clin Orthop Relat Res. 2012;470:2383–93. doi: 10.1007/s11999-012-2326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Terjesen T, Wiig O, Svenningsen S. Varus femoral osteotomy improves sphericity of the femoral head in older children with severe form of Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 2012;470:2394–401. doi: 10.1007/s11999-011-2181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bowen JR, Guille JT, Jeong C, Worananarat P, Oh CW, Rodriquez A, et al. Labral support shelf arthroplasty for containment in early stages of Legg-Calve-Perthes disease. J Pediatr Orthop. 2011;31:S206–11. doi: 10.1097/BPO.0b013e31822910ba. [DOI] [PubMed] [Google Scholar]
- 37.Marklund T, Tillberg B. Coxa plana: A radiological comparison of the rate of healing with conservative measures and after osteotomy. J Bone Joint Surg Br. 1976;58:25–30. doi: 10.1302/0301-620X.58B1.1270492. [DOI] [PubMed] [Google Scholar]
- 38.Iwasaki K. The change in venous circulation of the proximal part of the femur after varus osteotomy in Perthes’ disease. J Jpn Orthop Assoc. 1986;60:237–49. [PubMed] [Google Scholar]
- 39.Kim HK, da Cunha AM, Browne R, Kim HT, Herring JA. How much varus is optimal with proximal femoral osteotomy to preserve the femoral head in Legg-Calvé-Perthes disease? J Bone Joint Surg Am. 2011;93:341–7. doi: 10.2106/JBJS.J.00830. [DOI] [PubMed] [Google Scholar]
- 40.Hosalkar H, Munhoz da Cunha AL, Baldwin K, Ziebarth K, Wenger DR. Triple innominate osteotomy for Legg-Calvé-Perthes disease in children: Does the lateral coverage change with time? Clin Orthop Relat Res. 2012;470:2402–10. doi: 10.1007/s11999-011-2189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi IH, Yoo WJ, Cho TJ, Moon HJ. The role of valgus osteotomy in LCPD. J Pediatr Orthop. 2011;31(2 Suppl):S217–22. doi: 10.1097/BPO.0b013e318223b404. [DOI] [PubMed] [Google Scholar]
- 42.de Gheldere A, Eastwood DM. Valgus osteotomy for hinge abduction. Orthop Clin North Am. 2011;42:349–54. doi: 10.1016/j.ocl.2011.04.005. vi. [DOI] [PubMed] [Google Scholar]
- 43.Reinker KA. Shelf and/or reduction and containment surgery. Orthop Clin North Am. 2011;42:355–9. doi: 10.1016/j.ocl.2011.03.003. vii. [DOI] [PubMed] [Google Scholar]
- 44.Chang JH, Kuo KN, Huang SC. Outcomes in advanced Legg-Calvé-Perthes disease treated with the Staheli procedure. J Surg Res. 2011;168:237–42. doi: 10.1016/j.jss.2009.09.056. [DOI] [PubMed] [Google Scholar]
- 45.Aly TA, Amin OA. Arthrodiatasis for the treatment of Perthes’ disease. Orthopedics. 2009;32:817. doi: 10.3928/01477447-20090922-15. [DOI] [PubMed] [Google Scholar]
- 46.Segev E, Ezra E, Wientroub S, Yaniv M, Hayek S, Hemo Y. Treatment of severe late-onset Perthes’ disease with soft tissue release and articulated hip distraction: Revisited at skeletal maturity. J Child Orthop. 2007;1:229–35. doi: 10.1007/s11832-007-0046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Herrera-Soto JA, Price CT. Core decompression for juvenile osteonecrosis. Orthop Clin North Am. 2011;42:429–36. doi: 10.1016/j.ocl.2011.04.004. ix. [DOI] [PubMed] [Google Scholar]
- 48.Leunig M, Ganz R. Relative neck lengthening and intracapital osteotomy for severe Perthes and Perthes-like deformities. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S62–7. [PubMed] [Google Scholar]
- 49.Albers CE, Steppacher SD, Ganz R, Siebenrock KA, Tannast M. Joint-preserving surgery improves pain, range of motion, and abductor strength after Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 2012;470:2450–61. doi: 10.1007/s11999-012-2345-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim YJ, Novais EN. Diagnosis and treatment of femoroacetabular impingement in Legg-Calvé-Perthes disease. J Pediatr Orthop. 2011;31:S235–40. doi: 10.1097/BPO.0b013e3182260252. [DOI] [PubMed] [Google Scholar]
- 51.Lehmann TG, Engesaeter IØ, Laborie LB, Lie SA, Rosendahl K, Engesaeter LB. Total hip arthroplasty in young adults, with focus on Perthes’ disease and slipped capital femoral epiphysis: Followup of 540 subjects reported to the Norwegian Arthroplasty Register during 1987-2007. Acta Orthop. 2012;83:159–64. doi: 10.3109/17453674.2011.641105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Froberg L, Christensen F, Pedersen NW, Overgaard S. The need for total hip arthroplasty in Perthes disease: A long-term study. Clin Orthop Relat Res. 2011;469:1134–40. doi: 10.1007/s11999-010-1566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Traina F, De Fine M, Sudanese A, Calderoni PP, Tassinari E, Toni A. Long term results of total hip replacement in patients with Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 2011;93:e25. doi: 10.2106/JBJS.J.00648. [DOI] [PubMed] [Google Scholar]
- 54.Kim J, Cho YJ, Kim HJ. Role of total hip arthroplasty and resurfacing in Legg-Calvé-Perthes disease. J Pediatr Orthop. 2011;31(2 Suppl):S241–4. doi: 10.1097/BPO.0b013e318223b489. [DOI] [PubMed] [Google Scholar]
- 55.Costa CR, Johnson AJ, Naziri Q, Mont MA. Review of total hip resurfacing and total hip arthroplasty in young patients who had Legg-Calvé-Perthes disease. Orthop Clin North Am. 2011;42:419–22. doi: 10.1016/j.ocl.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 56.Du J, Lu A, Dempsey M, Herring JA, Kim HK. MR perfusion index as a quantitative method of evaluating epiphyseal perfusion in Legg-Calve-Perthes disease and correlation with short-term radiographic outcome: A preliminary study. J Pediatr Orthop. 2013;33:707–13. doi: 10.1097/BPO.0b013e3182a05dc1. [DOI] [PubMed] [Google Scholar]
- 57.Sankar WN, Thomas S, Castañeda P, Hong T, Shore BJ, Kim HK, et al. Feasibility and Safety of perfusion MRI for Legg-Calvé-Perthes Disease. J Pediatr Orthop. doi: 10.1097/BPO.0000000000000179. Epub ahead of print. [DOI] [PubMed] [Google Scholar]


