Abstract
BACKGROUND AND PURPOSE
Opioids, such as morphine, are the most effective treatment for pain but their efficacy is diminished with the development of tolerance following repeated administration. Recently, we found that morphine activated ERK in opioid-tolerant but not in naïve rats, suggesting that morphine activation of μ-opioid receptors is altered following repeated morphine administration. Here, we have tested the hypothesis that μ-opioid receptor activation of ERK in the ventrolateral periaqueductal gray (vlPAG) is dependent on dynamin, a protein implicated in receptor endocytosis.
EXPERIMENTAL APPROACH
Rats were made tolerant to repeated microinjections of morphine into the vlPAG. The effects of dynamin on ERK activation and antinociception were assessed by microinjecting myristoylated dominant-negative dynamin peptide (Dyn-DN) or a scrambled control peptide into the vlPAG. Microinjection of a fluorescent dermorphin analogue (DERM-A594) into the vlPAG was used to monitor μ-opioid receptor internalization.
KEY RESULTS
Morphine did not activate ERK and Dyn-DN administration had no effect on morphine-induced antinociception in saline-pretreated rats. In contrast, morphine-induced ERK activation in morphine-pretreated rats that was blocked by Dyn-DN administration. Dyn-DN also inhibited morphine antinociception. Finally, morphine reduced DERM-A594 internalization only in morphine-tolerant rats indicating that μ-opioid receptors were internalized and unavailable to bind DERM-A594.
CONCLUSIONS AND IMPLICATIONS
Repeated morphine administration increased μ-opioid receptor activation of ERK signalling via a dynamin-dependent mechanism. These results demonstrate that the balance of agonist signalling to G-protein and dynamin-dependent pathways is altered, effectively changing the functional selectivity of the agonist-receptor complex.
LINKED ARTICLES
This article is part of a themed section on Opioids: New Pathways to Functional Selectivity. To view the other articles in this section visit http://dx.doi.org/10.1111/bph.2015.172.issue-2
Keywords: morphine, opioid, opiate, morphine tolerance, periaqueductal gray, endocytosis, ERK, functional selectivity, ligand bias
Introduction
The antinociceptive effects of opioids are limited by the development of tolerance with repeated administration. The mechanism for tolerance has been difficult to identify because many signalling adaptations correlate with the development of tolerance (Christie, 2008; Williams et al., 2013). Opioid agonist binding to μ-opioid receptors induces phosphorylation of the receptor by G-protein receptor kinases (GRKs) and recruitment of proteins, including β-arrestin and dynamin, involved in the internalization of the receptor (Goodman et al., 1996; receptor nomenclature follows Alexander et al., 2013a). Ligand-biased signalling of μ-opioid receptors (McPherson et al., 2010; Kelly, 2013a; b) has been observed where specific agonists preferentially couple to specific effectors. Few studies have addressed whether ligand-biased signalling is altered by repeated opioid administration and the development of tolerance.
The μ-opioid receptor belongs to a family of GPCRs demonstrated to signal from the plasma membrane or from endosomes following internalization (Murphy et al., 2009). The ability of opioids to induce tolerance varies inversely with agonist efficacy to induce antinociception and μ-opioid receptor internalization. Internalization, but not tolerance, readily occurs following acute administration of high-efficacy agonists, whereas low-efficacy agonists, such as morphine, produce pronounced tolerance and little internalization (Finn and Whistler, 2001; Grecksch et al., 2006; Pawar et al., 2007). The fact that morphine tolerance is attenuated in β-arrestin knock-out mice (Bohn et al., 2000) led to the hypothesis that endocytosis of μ-opioid receptors was necessary for morphine tolerance. However, endocytosis and recycling of receptors has been demonstrated to reduce the development of tolerance to opioids (Finn and Whistler, 2001; He et al., 2009). A potential resolution to this controversy is that the ability of morphine to induce μ-opioid internalization is enhanced with repeated administration. Morphine, upon binding to the μ-opioid receptors, does not recruit β-arrestin or induce internalization of μ-opioid receptors efficiently (Whistler and von Zastrow, 1998; Alvarez et al., 2002; Arttamangkul et al., 2008; He et al., 2009). However, recent results from our laboratory indicate that morphine potency for inhibition of presynaptic GABA release and activation of the postsynaptic G-protein-activated, inward-rectifier K channels (GIRK;Kir3.x; channel nomenclature follows Alexander et al., 2013b) is enhanced in ventrolateral periaqueductal gray (vlPAG) neurons following chronic morphine administration (Ingram et al., 1998; 2008). These findings suggest that morphine is a more potent μ-opioid receptor agonist following repeated administration and may recruit endocytic machinery necessary for internalization and activation of endosomal signalling pathways, such as the ERK pathway.
Consistent with this idea, morphine activated ERK in the PAG of morphine-tolerant rats more efficiently than in naïve rats (Macey et al., 2009), an effect seen in several different brain areas following chronic morphine administration (Ortiz et al., 1995; Berhow et al., 1996; Narita et al., 2002; Asensio et al., 2006). Given that ERK activation in many cell types is dependent on recruitment of β-arrestin and dynamin scaffolding proteins (Whistler et al., 1999; Zheng et al., 2008), we tested the hypothesis that the increased ability of morphine to activate ERK in tolerant rats was dependent on recruitment of dynamin following repeated morphine administration. Phosphorylated ERK (pERK) levels were measured in the presence of the dynamin dominant-negative peptide (Dyn-DN) microinjected directly into the vlPAG in saline- and morphine-pretreated rats. Dyn-DN inhibits receptor internalization by disrupting dynamin formation of the endosome (Grabs et al., 1997). The vlPAG is an important area for opioid antinociception and the development of tolerance (Tortorici et al., 1999; Lane et al., 2005; Morgan et al., 2006a). We found that μ-opioid receptor signalling via ERK was enhanced in morphine-tolerant rats in a dynamin-dependent manner and that prior exposure to morphine blocked internalization of DERM-A594, a fluorescent analogue of the potent and selective μ-opioid receptor agonist, in morphine-tolerant rats without affecting DERM-A594 internalization in saline-pretreated rats. Thus, repeated morphine treatment effectively changes the ‘apparent’ functional selectivity of the agonist-receptor complex from predominately dynamin-independent signalling to a dynamin-dependent pathway.
Methods
Animals
All animal care and experimental procedures complied with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the Institutional Animal Care and Use Committees at Washington State University or Oregon Health & Science University. All studies involving animals are reported in accordance with the ARRIVE guidelines for reporting experiments involving animals (Kilkenny et al., 2010; McGrath et al., 2010). A total of 157 animals were used in the experiments described here.
Experiments were performed in adult male Sprague Dawley rats (250–350 g; supplied by Animal Technologies, Livermore, CA, USA or Harlan Laboratories, Livermore, CA, USA).
Microinjections
Rats were anaesthetized with pentobarbital (60 mg·kg−1, i.p.) and implanted with a guide cannula (23 gauge, 9 mm long) aimed at the vlPAG (AP: +1.7 mm, ML: ±0.6 mm, DV: −5.0 mm from lambda) using stereotaxic techniques. The guide cannula was attached to two screws in the skull by dental cement. At the end of the surgery, a stylet was inserted to plug the guide cannula. The rat was maintained under a heat lamp until awake. Following surgery, rats were housed individually. The animal housing room was maintained on a reverse light/dark schedule (lights off at 0700 h) so rats could be tested during the active dark phase. Food and water were freely available at all times except during testing. Rats were handled daily before and after surgery. Experiments began at least 7 days after surgery.
Drugs were administered directly into the vlPAG through a 31 gauge injection cannula (0.25 mm OD and 0.127 mm ID) inserted into and extending 2 mm beyond the tip of the guide cannula. One day before testing, rats received a sham injection in which an injector was inserted into the guide cannula but no drug was administered. This procedure reduces responses resulting from mechanical stimulation of neurons on the test day and habituates the rat to the microinjection procedure. Testing with drug administration began 1 day later. Drugs were microinjected at a rate of 0.1 μL per 10 s while the rat was gently restrained by hand. The injection cannula remained in place for an additional 20 s to minimize backflow of the drug up the cannula track. Following the injection, the stylet was replaced and the rat was returned to its home cage.
Testing of antinociceptive behaviour
All behavioural assessments were conducted using the hot plate test which consisted of measuring the time taken (latency) to lick a hind paw when the rat was placed on a hot (52.5°C) plate. The rat was removed from the hot plate if no response occurred before the cut-off of 50 s. Animals with baseline hot plate latencies greater than 20 s were omitted from the study (n = 6). Only rats with the injection cannula in or on the border of the vlPAG were included in data analyses (Paxinos and Watson, 2005). A total of 36 rats were omitted due to cannula placements outside of vlPAG.
Histology
Rats were anaesthetized with halothane, 5–10 min after the final hot plate test and perfused with saline and then formalin (10%). The brain was removed and placed in formalin (10%) in preparation for subsequent immunohistochemical and confocal analysis. The brain was sectioned coronally (60 μm) to identify the location of the injection site, defined as the end of the cannula track (Paxinos and Watson, 2005). Brain slices containing the vlPAG were incubated in 5% goat serum (Sigma-Aldrich, St. Louis, MO, USA), 3% BSA (Sigma-Aldrich) and 0.5% Triton X-100 (Sigma-Aldrich) for 1 h at room temperature. To label neurons, slices from Experiment 1 (see below) were stained with NeuroTrace Fluorescent 640/660 Nissl Stain (1/250, Molecular Probes, Eugene, OR, USA). Slices from Experiment 2 (see below) were incubated with mouse anti-NeuN antibodies (1/500, Chemicon, Temecula, CA, USA). In both experiments, slices were incubated with rabbit anti-phospho-ERK1/2 antibodies (1/300, Cell Signaling, Beverly, MA, USA) overnight, washed and then incubated in appropriate secondary antibodies [goat anti-rabbit IgG 488 Alexa Fluor conjugate (1/800, Invitrogen, Carlsbad, CA, USA) and/or goat anti-mouse IgG 555 (1/800, Invitrogen)]. All slices were thoroughly washed, mounted onto a slide with either SlowFade or Prolong Gold Antifade Reagents (Invitrogen), coverslipped and imaged with a Zeiss LSM510 META confocal microscope (Carl Zeiss MicroImaging, Inc., Thornwood, NY, USA).
Fluorescence intensity quantification
The pERK labelling was quantified in individual NeuN-labelled or NeuroTrace-labelled vlPAG neurons 100–200 μm adjacent to the aqueduct using Image J (NIH, Bethesda, MD, USA). Three fields from the same slice were analysed for each animal. The experimenter was unaware of the treatments during analysis. The pERK labelling and background labelling were calculated for each neuron using Image J (Schneider et al., 2012). The intensity of the background labelling was subtracted from the pERK labelling to obtain the final intensity for each neuron.
Experiment 1: activation of ERK following single injections of opioid agonists
Baseline hot plate nociception was assessed. Animals then received a single microinjection of one of the following: DERM-A594 [300 ng per 0.5 μL (0.32 mM); generous gift from Dr. Seksiri Arrtamangkul, Vollum Institute, OHSU] or its vehicle (0.5 μL of 32% DMSO in saline), saline (0.4 μL), dermorphin [2.2 μg per 0.4 μL (6.2 mM); Phoenix Pharmaceuticals, Burlingame, CA, USA], or one of two doses of morphine [10 μg (32.9 mM) or 22 μg per 0.4 μL (72.5 mM); Sigma-Aldrich]. The dose of DERM-A594 given was the highest dose possible because of solubility constraints. The hot plate test was performed 15 min following drug microinjections. Immediately after the hot plate test, the rat was killed and the brain was removed for histological analysis of pERK labelling.
Experiment 2: role of dynamin in ERK activation in tolerant rats
To determine the effect of dynamin inactivation on the time course of acute morphine-induced antinociception, rats were tested on the hot plate test to assess baseline hot plate latencies. Each rat was pretreated with either a microinjection of Dyn-DN (200 ng per 0.4 μL; Tocris Bioscience, Bristol, UK) or scrambled dynamin peptide (Dyn-scr; 200 ng per 0.4 μL; Tocris Bioscience) and tested on the hot plate 20 min prior to receiving a single microinjection of morphine (5 μg per 0.4 μL) or saline. Hot plate latencies were measured at 15, 30, 60, 90 and 120 min following injections. A separate study used the same procedure to test the ability of Dyn-DN peptide to block ERK activation after a single microinjection of a high dose of morphine (22 μg per 0.4 μL). Rats were perfused 20 min following microinjections and the brains were removed for immunohistochemistry.
To determine the effect of dynamin inactivation on the acute morphine dose response, rats were pretreated with either a microinjection of Dyn-DN (200 ng per 0.4 μL; Tocris Bioscience) or Dyn-scr (200 ng per 0.4 μL; Tocris Bioscience) 20 min prior to receiving microinjections of cumulative third-log doses (1, 2.2, 4.6, 10, 22 μg per 0.4 μL) at 20 min intervals. Hot plate latencies were measured 15 min following each microinjection.
To induce tolerance, animals received twice daily microinjections of morphine (5 μg per 0.4 μL) or saline on days 1 and 2. Baseline nociception was assessed using the hot plate test before and 15 min after the first set of microinjections of morphine or saline on day 1. On day 3, rats were pretreated with Dyn-DN (100 ng per 0.4 μL; Tocris Bioscience) or Dyn-scr (100 ng per 0.4 μL; Tocris Bioscience) 20 min prior to microinjection of morphine (10 μg per 0.4 μL) microinjections into the vlPAG. Nociception was assessed using the hot plate test 15 min after each injection. Immediately after the hot plate test, the rat was killed and the brain was removed for histological analysis of pERK labelling.
Experiment 3: morphine inhibition of DERM-A594 internalization
It is difficult to find a μ-opioid receptor antibody that specifically labels the PAG, so we used the fluorescent opioid peptide, DERM-A594 to measure μ-opioid receptor internalization. Microinjection of DERM-A594 into the vlPAG produces rapid internalization of μ-opioid receptors (Macey et al., 2010). We reasoned that if microinjection of morphine into the vlPAG induces μ-opioid receptor internalization in tolerant rats, then fewer μ-opioid receptors would be available for internalization to a subsequent microinjection of DERM-A594. Tolerance was induced by twice daily microinjections of morphine or saline for 2 days. Half of the rats in each group were injected with morphine (5 μg per 0.4 μL) or saline on day 3 and tested on the hot plate test 15 min later. DERM-A594 (300 ng per 0.5 μL) was microinjected into the vlPAG 30 min after morphine or saline injection and the brain was removed 10 min later. DERM-A594 labelling was quantified in individual NeuN-labelled vlPAG neurons 100–200 μm adjacent to the aqueduct using the Zeiss LSM Image Examiner program (Carl Zeiss MicroImaging, Inc.). The experimenter was unaware of the treatments during analyses. The fluorescence intensities of DERM-A594 and background labelling were calculated as the integrated density for each neuron using Image J (Schneider et al., 2012). The intensity of the background labelling was subtracted from the DERM-A594 labelling to obtain the final intensity for each neuron.
Data analysis
Values of hot plate latencies are shown as means ± SEM for the different treatment groups. The integrated density of fluorescence (from pERK or DERM-A594) was averaged (±SEM) for the total number of neurons in each treatment group (n = 4–7 rats per group; 20–24 neurons per rat). Statistical significance of differences between group means (for both hotplate and fluorescence assays) was determined by anova followed by Bonferroni's post hoc test, P < 0.05 (GraphPad Prism, La Jolla, CA, USA).
Results
Activation of ERK with acute opioid administration
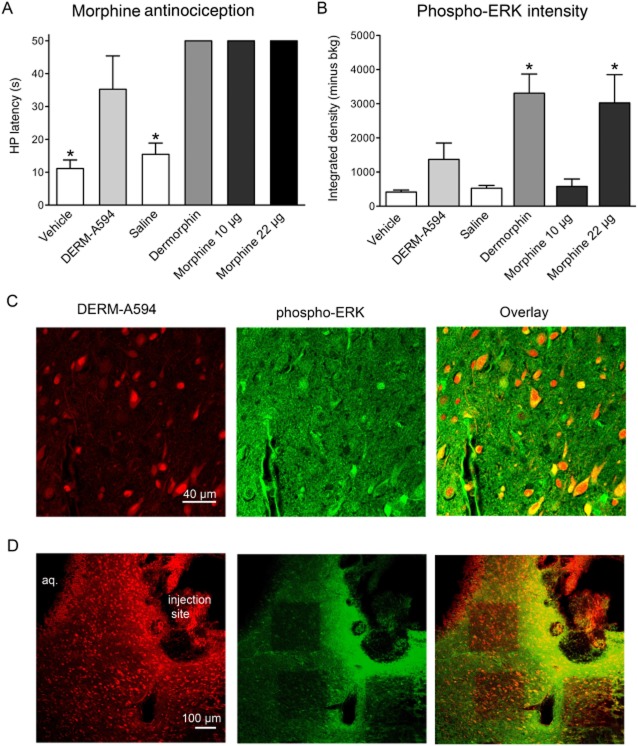
We compared the ability of dermorphin and morphine to activate ERK when microinjected into the vlPAG. We also compared a lower dose of the fluorescent dermorphin compound DERM-A594 (Arttamangkul et al., 2000; 2008; Macey et al., 2010). Microinjection of each agonist into the vlPAG caused a significant increase in hot plate latency at the doses given, compared with saline- or vehicle-treated controls [one-way anova; F(5,21) = 24.52, P < 0.05; Bonferroni's post hoc test, *P < 0.05; n = 3–5 rats per group; Figure 1A].
Figure 1.
Opioid agonists induce antinociception and ERK phosphorylation. (A) DERM-A594 microinjections [300 ng per 0.5 μL (0.32 mM); n = 3] significantly increased hot plate latencies, compared with vehicle-treated rats (32% DMSO; n = 3; *P < 0.05). Dermorphin [2.2 μg per 0.4 μL (6.9 mM); n = 4] and morphine [10 μg per 0.4 μL (33 mM), n = 5 and 22 μg per 0.4 μL (72.5 mM), n = 4] microinjections increased hot plate latencies to cut-off for all rats and were significantly different from saline (*P < 0.05). (B) Dermorphin significantly increased the intensity of pERK immunoreactivity compared with saline control animals. There was a trend towards increased pERK labelling for the lower concentration of the fluorescent DERM-A594. Similarly, the maximal concentration of morphine (22 μg) significantly increased the intensity of pERK labelling but an equally antinociceptive dose of morphine (10 μg) did not (*P < 0.05). (C) Confocal images from a representative slice showing that cells that internalized DERM-A594 in the vlPAG also showed pERK labelling. Neurons were defined by NeuroTrace staining. Scale bar is the same for all images. (D) Confocal images (10×) showing the whole field of vlPAG and three fields that were scanned for pERK analyses. The cerebral aqueduct (aq.) and injection site is noted on the DERM-A594 panel. Scale bar is the same for all images.
Slices from each animal were stained with NeuroTrace and immunostained with an antibody to pERK1/2. There was a significant overall effect of opioid treatment in the intensity of pERK labelling [F(5,19) = 6.271, P < 0.05; Figure 1B]. This effect was primarily driven by the increase in intensity in rats injected with dermorphin (n = 4) compared with saline (n = 3; Bonferroni's post hoc test, P < 0.05). The dose of DERM-A594 (n = 3) injected also caused an increase in pERK intensity, although this increase did not reach statistical significance compared with vehicle-treated rats (n = 4; Bonferroni's post hoc test, ns). Morphine (10 μg per 0.4 μL; n = 3) did not activate ERK compared with saline (Bonferroni's post hoc test, ns). However, a supramaximal antinociceptive dose of morphine (22 μg per 0.4 μL; n = 4) increased pERK labelling compared with saline and the lower dose of morphine (Bonferroni's post hoc tests, P < 0.05).
Opioids are known to hyperpolarize vlPAG neurons (Chieng and Christie, 1994; Osborne et al., 1996) and disinhibit PAG output neurons (Vaughan and Christie, 1997). Thus, it is not known whether activation of ERK by opioid agonists occurs in the cells expressing μ-opioid receptors or in cells that are activated by removing GABA inhibition. In order to test this, colocalization of internalized DERM-A594 and pERK was assessed (n = 3). We found that an average of 66 ± 11% of cells that had pERK1/2 intensities over background were also labelled with DERM-A594 (Figure 1C). These results indicate that a significant proportion of pERK labelled cells express μ-opioid receptors. The percentage is probably an underestimate considering the low dose of DERM-A594 used in these studies. The data also suggest that ERK activation may occur as a result of disinhibition. An example of a slice containing vlPAG and three separate fields assessed for DERM-A594 labelling and pERK staining is shown in Figure 1D. DERM-A594 labelling is brightest in the nucleus but it is not known why it trafficks so quickly to this portion of neurons or whether it trafficks with receptors. However, several laboratories in independent studies have confirmed that internalized DERM-A594 is dependent on binding to μ-opioid receptors with irreversible antagonists (Arttamangkul et al., 2006; Macey et al., 2010; Phillips et al., 2012).
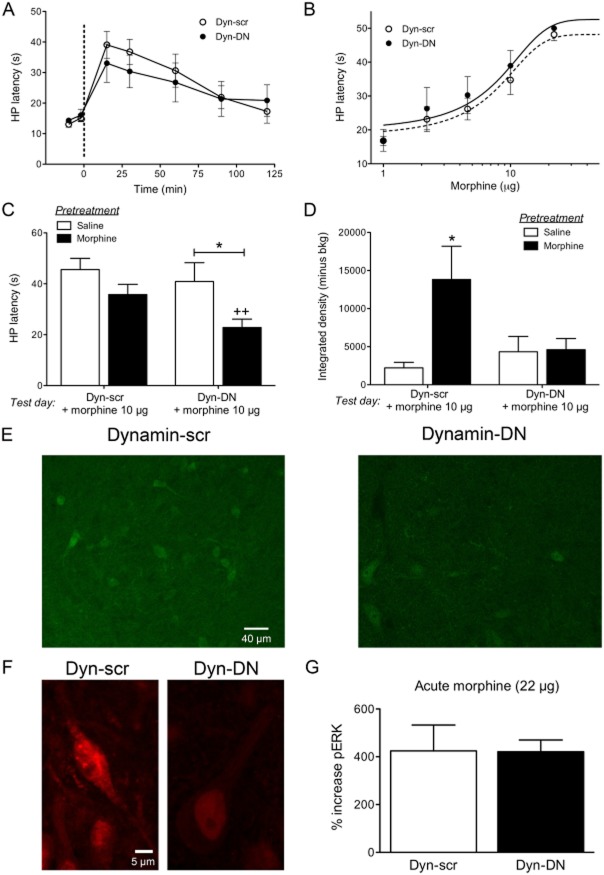
Activation of ERK in morphine-tolerant rats is dependent on dynamin
The effects of blocking dynamin activity on morphine antinociception were assessed using microinjections of Dyn-DN or the scrambled control peptide (Dyn-scr) 20 min prior to a single microinjection of morphine (5 μg per 0.4 μL). Rats were tested on the hot plate test 15, 30 60, 90 and 120 min following the microinjections (Figure 2A). There was no overall effect or effect of treatment [two-way repeated measures anova, F(1,15) = 4.636, P > 0.05]. Additional groups of rats were pretreated with Dyn-DN or Dyn-scr microinjections and then received cumulative doses of morphine. Rats were tested on the hot plate 15 min after each injection (Figure 2B). The D50 values were 7.8 (CI 3.8–11.8) for Dyn-scr and 5.8 (CI 1.9–9.7) for Dyn-DN [F(1,79) = 0.4712, P > 0.05] treated rats. These results show that inhibition of dynamin does not affect the ability of morphine to induce antinociception.
Figure 2.
Inhibition of dynamin reduces morphine antinociception and ERK activation in morphine-tolerant rats. (A) Rats were placed on the hot plate to determine their baseline latency, then were pretreated with Dyn-DN (n = 6) or Dyn-scr (n = 10) and tested on the hot plate 15 min later. Rats were then microinjected with a single dose of morphine (5 μg per 0.4 μL, used to induce tolerance in later studies). Hot plate latencies were tested at 15, 30, 60, 90 and 120 min. There was no effect of the Dyn-DN peptide on the time course of morphine antinociception. (B) Rats were pretreated with Dyn-DN (n = 7) or Dyn-scr (n = 10) microinjections followed by cumulative doses of morphine at 20 min intervals. Rats were tested on the hot plate 15 min following each morphine dose. There was no effect of the dynamin inhibitor peptide on the dose response to morphine in naïve animals. (C) Rats were pretreated with either saline or morphine (5 μg per 0.4 μL) twice daily for 2 days. On day 3, rats were microinjected with either Dyn-DN or Dyn-scr peptides 20 min prior to morphine (10 μg per 0.4 μL). There was a significant effect of pretreatment [two-way anova; F(1,26) = 8.721; P < 0.5]. In addition, hot plate latency was significantly attenuated by Dyn-DN in morphine-pretreated rats (n = 7) compared with saline (n = 5) (Bonferroni's post hoc test; *P < 0.05) and compared to morphine-pretreated + Dyn-scr (Bonferroni's post hoc test; ++P < 0.05). There was no difference in morphine- (n = 10) and saline- (n = 8) pretreated rats given Dyn-scr (Bonferroni's post hoc test; ns). (D) Brains from rats in (C) were removed 30 min after final morphine microinjection and immunostained with an antibody to phosphorylated ERK (pERK). There was an overall interaction [two-way anova; F(1,18) = 5.082); P < 0.05]. Morphine increased the intensity of pERK labelling in morphine-pretreated rats given Dyn-scr (n = 5) compared with saline-pretreated rats (n = 4; Bonferroni's post hoc test, *P < 0.05). Microinjection of Dyn-DN peptide blocked pERK labelling in morphine- (n = 8) pretreated rats so pERK labelling was not different from saline-pretreated rats (n = 5; Bonferroni's post hoc test, ns). (E) Confocal images showing pERK1/2 labelling in morphine-pretreated rats receiving Dyn-scr and Dyn-DN microinjections. Scale bar is the same for both images. (F) Confocal image (100×) showing a DERM-A594-labelled neuron (left panel) and the decreased DERM-A594 labelling in a rat that received Dyn-DN peptide prior to the DERM-A594 microinjection. (G) Rats received either Dyn-DN or Dyn-scr microinjections prior to a supramaximal dose of morphine (22 μg per 0.4 μL). Rats were perfused and brains removed 20 min later for pERK immunohistochemistry. There was no effect of the dynamin inhibitor peptide on pERK levels.
Our earlier results showed evidence that another opioid agonist, dermorphin, induces dynamin-dependent antinociception (Macey et al., 2010) and that morphine preferentially activates ERK signalling in tolerant rats (Macey et al., 2009). Given that ERK signalling can be dynamin-dependent, we assessed whether Dyn-DN changed morphine-induced ERK activation and antinociception in morphine-tolerant rats. Rats were pretreated with either saline or morphine (5 μg per 0.4 μL) twice a day for 2 days to induce tolerance (Morgan et al., 2006b; Bobeck et al., 2012). The first microinjection of morphine on day 1 increased hot plate latencies (48 ± 2 s; n = 17) compared with rats injected with saline (13 ± 1 s; n = 13; t(28) = 18.10; P < 0.05). On day 3, morphine- and saline-pretreated rats received microinjections of either the Dyn-DN (100 ng per 0.4 μL) or Dyn-scr (100 ng per 0.4 μL) 20 min prior to morphine microinjection. All rats received morphine (10 μg per 0.4 μL) microinjections on the test day (Figure 2C). There was an effect of pretreatment on hot plate latencies [two-way anova; F(1,26) = 8.721; P < 0.05; Figure 2A] where morphine-pretreated rats had shorter hot plate latencies compared with saline controls. In saline-pretreated rats, microinjection of Dyn-DN or Dyn-scr did not alter the effect of morphine on hot plate latency. However, Dyn-DN significantly reduced hot plate latencies in morphine- compared with saline-pretreated rats (Bonferroni's post hoc test; P < 0.05). Dyn-DN also reduced the response to morphine compared with Dyn-scr [t-test, t(15) = 2.319, P < 0.05].
Brains from a subset of the animals tested for behaviour were fixed and sliced for pERK immunoreactivity (Figure 2D and E). There was a significant overall interaction between pretreatment and dynamin peptide injections [two-way anova interaction; F(1,18) = 5.082; P < 0.05]. There was a low level of pERK labelling in saline-pretreated rats given the Dyn-scr peptide and Dyn-DN peptide in the presence of morphine. However, morphine caused an increase in pERK in morphine-pretreated rats injected with Dyn-scr (Bonferroni's post hoc test, P < 0.05). Dyn-DN peptide blocked the increase in pERK labelling in morphine-pretreated rats and there was no difference in pERK intensity from saline-pretreated rats given Dyn-DN + morphine (Bonferroni's post hoc test, ns).
Given the increase in pERK intensity in naïve animals in response to the supramaximal dose of morphine (22 μg), we were also interested in further testing if the response was dynamin-dependent. Rats were pretreated with microinjections of Dyn-DN or Dyn-scr peptides 20 min prior to microinjections of morphine (22 μg per 0.4 μL). One rat received a microinjection of DERM-A594 to confirm that the Dyn-DN peptide attenuated internalization (Figure 2F). All rats were perfused 15 min after the final injections and tissue was processed for pERK staining. The high dose of morphine (22 μg) increased pERK integrated densities compared with rats that received saline but there was no effect of Dyn-DN peptide (422 ± 49% increase) compared with Dyn-scr-treated rats (425 ± 108% increase, Figure 2G). These results suggest that high doses of morphine induce pERK but it is dependent on other signalling pathways.
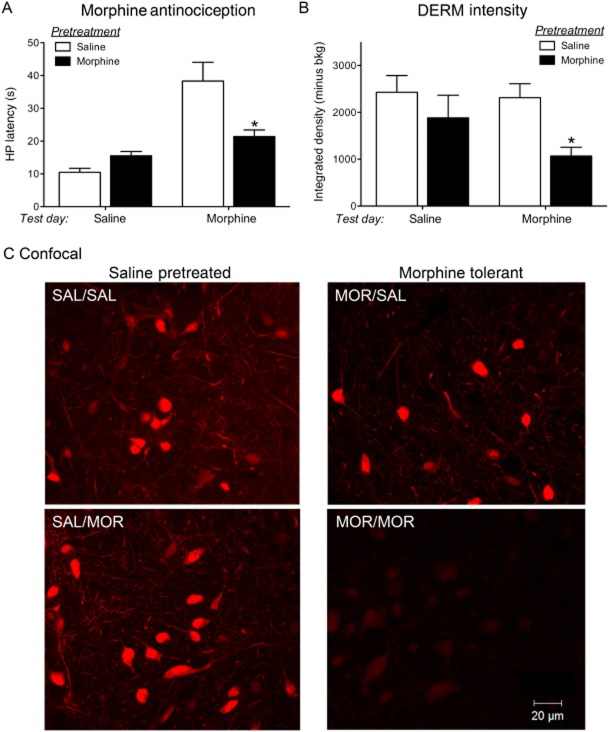
Morphine reduces DERM-A594 internalization in morphine-tolerant rats
Dynamin is a GTPase involved in endocytosis (Herskovits et al., 1993). The blockade of morphine-induced antinociception and ERK activation in morphine-tolerant rats by Dyn-DN administration suggested that morphine activation of μ-opioid receptors may induce endocytosis more readily after repeated morphine administration. We tested this hypothesis by analysing the effects of prior morphine exposure on DERM-A594 internalization. If morphine induces μ-opioid receptor internalization, then fewer μ-opioid receptors would be available to bind DERM-A594. Rats were pretreated with saline or morphine (5 μg per 0.4 μL) twice a day for 2 days to induce tolerance. On the test day, nociception was assessed 15 min after microinjection of either saline or morphine (5 μg per 0.4 μL). There was a significant interaction between pretreatment and test day injection [two-way anova interaction; F(1,27) = 17.06; P < 0.05; Figure 3A]. Hot plate latencies were significantly lower in morphine-pretreated rats as would be expected with the development of tolerance [pretreatment; F(1,27) = 5.005, P < 0.05]. Hot plate latencies were not different in saline- and morphine-pretreated rats given a saline injection on the test day (Bonferroni's post hoc test, ns). However, morphine-pretreated rats had significantly decreased hot plate latencies when challenged with morphine on the test day, compared with saline-pretreated rats (Bonferroni's post hoc test, P < 0.05). These results indicate that morphine-pretreated rats were tolerant to repeated morphine microinjections as we have shown many times previously (Tortorici et al., 1999; Morgan et al., 2006b; Bobeck et al., 2012).
Figure 3.
Morphine reduces DERM-A594 fluorescence in morphine-tolerant rats. (A) Rats were pretreated with either morphine (5 μg per 0.4 μL) or saline twice daily for 2 days. On day 3, rats received microinjections of saline or morphine (5 μg per 0.4 μL) and were tested on the hot plate. There was a significant overall interaction [two-way anova; F(1,27) = 17.06; P < 0.05]. Hot plate latencies were significantly reduced following morphine microinjections on the test day in morphine-tolerant rats (n = 11) compared with saline-pretreated rats (n = 5; Bonferroni's post hoc test; *P < 0.05). Saline microinjections on the test day did not affect latencies in saline- (n = 6) or morphine- (n = 8) pretreated rats (Bonferroni's post hoc test; ns). (B) Immediately after hot plate testing, all rats received microinjections of DERM-A594 (300 ng per 0.5 μL) and rats were perfused and brains were removed 10 min after microinjections. DERM-A594 intensity was significantly reduced in morphine- compared with saline-pretreated rats [pretreatment: F(1,21) = 6.943; P < 0.05]. Morphine injection on test day significantly reduced DERM-A594 intensity in morphine- (n = 6) compared with saline- (n = 9) pretreated rats (Bonferroni's post hoc test; *P < 0.05). There was no difference in saline- (n = 6) and morphine-pretreated rats (n = 4) when given saline on test day (Bonferroni's post hoc test, ns). (C) Representative confocal images from each group showing reduced DERM-A594 fluorescence in cell bodies and processes in morphine-tolerant rats that received a morphine microinjection prior to DERM-A594.
Following testing on the hot plate, all rats were microinjected with DERM-A594 (300 ng per 0.5 μL) into the vlPAG and the brains were removed 10 min later. Slices were analysed for fluorescence intensity of internalized DERM-A594 (Figure 3B and C). The intensity of DERM-A594 fluorescence was significantly decreased in morphine- compared with saline-pretreated rats [two-way anova pretreatment; F(1,21) = 6.943; P < 0.05]. Morphine microinjection prior to the DERM-A594 injection significantly decreased DERM-A594 intensity in morphine-tolerant rats compared with saline-pretreated rats (Bonferroni's post hoc test, P < 0.05). DERM-A594 intensity was similar in rats that received saline on test day, regardless of the pretreatment with saline or morphine (Bonferroni's post hoc test; ns).
Discussion
Our previous studies showed evidence that morphine activated MAP/ERK signalling selectively in morphine-tolerant rats (Macey et al., 2009). The results presented here extended this finding to show that ERK activation in morphine-tolerant rats was dynamin-dependent and that inhibition of dynamin decreased morphine-induced antinociception in morphine-tolerant rats without affecting antinociception in saline-pretreated rats. Our results also show that morphine interfered with internalization of the fluorescent dermorphin analogue, DERM-A594, in morphine-tolerant rats. Taken together, the results indicated that repeated morphine administration and the development of tolerance enhanced the ability of morphine to recruit dynamin, a GTPase involved in GPCR endocytosis (Herskovits et al., 1993; Vallee et al., 1993).
Role of ERK activation in opioid antinociception
Opioids induce antinociception in the vlPAG by inhibiting GABA release and disinhibiting PAG output neurons to the rostral ventromedial medulla (Heinricher and Ingram, 2008). Microinjections of the MEK/ERK inhibitor UO126 reduce morphine antinociception selectively in morphine-tolerant rats (Macey et al., 2009) indicating that activation of ERK enhances morphine antinociception. In this paper, we extend our earlier studies to show that antinociceptive doses of morphine (10 μg) did not induce ERK activation in control rats, but significantly increased ERK activation in rats pretreated with repeated injections of morphine. We also showed that the potent agonist dermorphin increased pERK with acute administration as expected from our earlier work showing dynamin-dependent dermorphin antinociception (Macey et al., 2010). Together, these results strongly support the hypothesis that dynamin and ERK activation are important signalling pathways that promote opioid antinociception in the vlPAG.
Functional selectivity of opioid agonists at μ-opioid receptors
There are many known opioid agonists that bind to the μ-opioid receptor and several of these have distinct potencies and efficacies for selected signalling pathways, known as ligand bias or functional selectivity (Kelly, 2013a). Morphine has long been known to initiate signalling cascades different from those of other opioid agonists, such as fentanyl and DAMGO (Connor et al., 2004; Kelly et al., 2008). Agonist-specific differences in internalization with acute administration have been observed (Stevens and Yaksh, 1989; Paronis and Holtzman, 1992; Duttaroy and Yoburn, 1995; Grecksch et al., 2006), and similar differences have been noted with ERK activation (Macey et al., 2006). Opioid agonists show ligand bias when tested for their ability to activate G-proteins, recruit β-arrestin or induce internalization (McPherson et al., 2010; Rivero et al., 2012) and this bias has been measured using various methods that are dependent on comparing agonist affinity and efficacy on these measures (Kenakin et al., 2012; Kelly, 2013a; b; Kenakin and Christopoulos, 2013). In this study, we showed that repeated morphine administration increased morphine signalling via ERK in a dynamin-dependent manner. Activation of the MAPK/ERK pathway by chronic morphine administration has been demonstrated in spinal cord (Horvath et al., 2010) and brain (Narita et al., 2002; Macey et al., 2006; 2009; Lin et al., 2010) and ERK signalling has been shown to be both internalization and dynamin-dependent in many cell types (Ignatova et al., 1999). However, in some cases dynamin-dependent μ-opioid receptor signalling appears to be independent of μ-opioid receptor internalization (Whistler et al., 1999; Kramer and Simon, 2000) suggesting that scaffolding proteins downstream of the μ-opioid receptor but prior to endocytosis could be involved in μ-opioid receptor activation of ERK. A G-protein-dependent pathway that is not dependent on dynamin or internalization also has been described in some cells (Rozenfeld and Devi, 2007; Zheng et al., 2008). This pathway may explain the increase in ERK activation observed with supramaximal morphine doses in naïve animals (Figure 1B) that was not inhibited in the presence of the Dyn-DN peptides (Figure 2G). It is also important to note that the supramaximal dose induces severe behavioural immobility suggestive of catatonia so ERK activation may occur through very different signalling pathways.
Our results indicate that acute morphine signalling is different from that of dermorphin. Dermorphin is a potent μ-opioid receptor agonist with high selectivity for μ-opioid receptors compared with δ-opioid receptors (de Castiglione and Rossi, 1985; Melchiorri and Negri, 1996). Dermorphin stimulates internalization of μ-opioid receptors that is blocked by inhibitors of dynamin (Macey et al., 2010), a GTPase involved in vesicle endocytosis that is recruited following GRK phosphorylation and binding of β-arrestin to the μ-opioid receptor (Herskovits et al., 1993; Daaka et al., 1998). Morphine is a partial agonist that is also more selective for μ- over δ-opioid receptors but does not efficiently recruit β-arrestin and dynamin to the receptor and does not induce internalization in most cell types (Whistler and von Zastrow, 1998). β-Arrestin binding to the β2-adrenoceptor is dependent on both agonist occupation and phosphorylation of the receptor by GRKs (Krasel et al., 2005). Therefore, agonist occupancy may be a key factor for GRK phosphorylation and recruitment of β-arrestin. The change in functional selectivity of morphine and its ability to recruit dynamin-dependent signalling pathways is consistent with our previous observations that morphine has increased potency at the μ-opioid receptor in tolerant rats (Ingram et al., 1998; 2008). These results support previous data demonstrating adaptive changes in μ-opioid receptor activation in the vlPAG associated with repeated administration of morphine. In tolerant rats, morphine activates GIRK channels with increased potency (Ingram et al., 2008) and desensitizes μ-opioid receptor coupling to GIRK channels more readily (Dang and Williams, 2004; Bagley et al., 2005a; Ingram et al., 2008). The μ-opioid receptor inhibition of adenylyl cyclase and Ca2+ channels are also altered following chronic morphine administration (Ingram et al., 1998; Bagley et al., 2005a; b). Moreover, the binding affinity of opioid agonists has been shown to increase after long-term exposure of μ-opioid receptor-expressing cells to morphine (Birdsong et al., 2013). These results imply that morphine binding to the μ-opioid receptor induces a different conformation of the receptor in tolerant rats that may expose different phosphorylation sites (Doll et al., 2011; 2012). The fact that changes are observed in multiple effector pathways and that the potency and/or efficacy of agonist activation of μ-opioid receptors is altered argues that changes occur in agonist binding and activation of the receptor, prior to activation of effector systems.
The change in functional selectivity of morphine may also arise from activation of heteromers of the μ-opioid receptor and δ-opioid receptor. Chronic morphine administration induces the expression of μ/δ-opioid receptor heteromers (Gupta et al., 2010), activation of which induces prolonged ERK signalling (Rozenfeld and Devi, 2007). δ-receptor agonists have no effect in naïve animals but inhibit presynaptic GABA release in the vlPAG after chronic morphine treatment (Hack et al., 2005). Interestingly, upregulation of δ-opioid receptor activity is dependent on expression of μ-opioid receptor and β-arrestin as inhibition of presynaptic GABA release mediated by δ-opioid receptors was not observed in μ-opioid receptor or β-arrestin knock-out mice (Hack et al., 2005).
The physiological consequence of this adaptive change in morphine signalling at μ-opioid receptors is important for differences in interpretation of recent studies on tolerance. Current cellular models of tolerance focus on regulatory mechanisms of μ-opioid receptors, including desensitization and internalization (Christie, 2008; Williams et al., 2013). Support for these models include data generated from β-arrestin knock-out mice (Bohn et al., 2000) and mice expressing a knock-in mutant μ-opioid receptor that internalizes to morphine (Kim et al., 2008) that do not develop tolerance to opioids. These findings indicate that proteins involved in μ-opioid receptor desensitization and internalization are critically involved in tolerance to morphine. However, many studies have shown that acute morphine administration is not effective at recruiting proteins involved in μ-opioid receptor desensitization and endocytosis (Whistler and von Zastrow, 1998; Finn and Whistler, 2001). Although acute morphine is not capable of inducing significant μ-opioid receptor internalization (Keith et al., 1996; Sternini et al., 1996; Whistler and von Zastrow, 1999) or activating dynamin-dependent ERK signalling (Macey et al., 2006; 2009), our results suggest that morphine does induce μ-opioid receptor internalization and stimulate dynamin-dependent ERK phosphorylation after repeated administration of morphine. Loss of μ-opioid receptors on the plasma membrane has been demonstrated in the brain (Drake et al., 2005) and guinea pig ileum (Patierno et al., 2011) following chronic morphine administration. Alternatively, dynamin inhibitors may disrupt the development of adaptations to repeated opioid administration (Madhavan et al., 2010) or disrupt μ-opioid receptor signalling in tolerant animals that is not dependent on internalization (Whistler and von Zastrow, 1999; Whistler et al., 1999). Indeed, additional morphine signalling pathways have been identified that are disrupted in β-arrestin knock-out mice (Bradaia et al., 2005; Mittal et al., 2012). Our data are also consistent with the interpretation that there is an increased affinity of morphine for μ-opioid receptors (Ingram et al., 1998; 2008; Birdsong et al., 2013). Increased competition of morphine with DERM-A594 would also result in decreased DERM-A594 fluorescence in tolerant rats after a morphine challenge. In either case, morphine activation of μ-opioid receptors, in morphine-tolerant rats, recruits dynamin-dependent processes that are important in mediating antinociception.
In summary, our results demonstrate that for a single opioid agonist, morphine, the balance between activation of different effector signalling pathways is altered by repeated administration. These changes in μ-opioid receptor signalling are associated with the development of antinociceptive tolerance observed in the vlPAG. Future studies will address the role of ligand-biased endosomal μ-opioid receptor signalling in the vlPAG and the role of ERK signalling in the cellular mechanisms underlying μ-opioid receptor-mediated antinociception.
Acknowledgments
This study was supported in part by the National Institute of Drug Abuse [DA023318 (T. A. M.) and DA027625 (M. M. M. and S. L. I.)]. The assistance of Drs. Sue Aicher and Deb Hegarty for use of the confocal microscope and Dr. Seksiri Arttamangkul for a generous gift of DERM-A594 is greatly appreciated.
Glossary
Abbreviations
- Dyn-DN
dominant-negative dynamin peptide
- Dyn-scr
scrambled dynamin peptide
- GRK
G-protein receptor kinase
- vlPAG
ventrolateral periaqueductal gray
Author contributions
T.A.M., M.M.M. and S.L.I. conceived the study. T.A.M., E.N.B., K.L.S. and S.L.I. designed the study, collected data and analysed experiments. T.A.M. and S.L.I. wrote the manuscript and all authors edited the final version of the manuscript.
Conflict of interest
The authors state that there are no conflicts of interest associated with this work.
References
- Alexander SPH, Benson HE, Faccenda E, Pawson AJ, Sharman JL, Spedding M, et al. The Concise Guide to PHARMACOLOGY 2013/14: G Protein-Coupled Receptors. Br J Pharmacol. 2013a;170:1459–1581. doi: 10.1111/bph.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander SPH, Benson HE, Faccenda E, Pawson AJ, Sharman JL, Catterall WA, et al. The Concise Guide to PHARMACOLOGY 2013/14: Ion Channels. Br J Pharmacol. 2013b;170:1607–1651. doi: 10.1111/bph.12447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez VA, Arttamangkul S, Dang V, Salem A, Whistler JL, Von Zastrow M, et al. mu-Opioid receptors: ligand-dependent activation of potassium conductance, desensitization, and internalization. J Neurosci. 2002;22:5769–5776. doi: 10.1523/JNEUROSCI.22-13-05769.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arttamangkul S, Alvarez-Maubecin V, Thomas G, Williams JT, Grandy DK. Binding and internalization of fluorescent opioid peptide conjugates in living cells. Mol Pharmacol. 2000;58:1570–1580. doi: 10.1124/mol.58.6.1570. [DOI] [PubMed] [Google Scholar]
- Arttamangkul S, Torrecilla M, Kobayashi K, Okano H, Williams JT. Separation of mu-opioid receptor desensitization and internalization: endogenous receptors in primary neuronal cultures. J Neurosci. 2006;26:4118–4125. doi: 10.1523/JNEUROSCI.0303-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arttamangkul S, Quillinan N, Low MJ, von Zastrow M, Pintar J, Williams JT. Differential activation and trafficking of micro-opioid receptors in brain slices. Mol Pharmacol. 2008;74:972–979. doi: 10.1124/mol.108.048512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asensio VJ, Miralles A, Garcia-Sevilla JA. Stimulation of mitogen-activated protein kinase kinases (MEK1/2) by mu-, delta- and kappa-opioid receptor agonists in the rat brain: regulation by chronic morphine and opioid withdrawal. Eur J Pharmacol. 2006;539:49–56. doi: 10.1016/j.ejphar.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Bagley EE, Chieng BC, Christie MJ, Connor M. Opioid tolerance in periaqueductal gray neurons isolated from mice chronically treated with morphine. Br J Pharmacol. 2005a;146:68–76. doi: 10.1038/sj.bjp.0706315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagley EE, Gerke MB, Vaughan CW, Hack SP, Christie MJ. GABA transporter currents activated by protein kinase A excite midbrain neurons during opioid withdrawal. Neuron. 2005b;45:433–445. doi: 10.1016/j.neuron.2004.12.049. [DOI] [PubMed] [Google Scholar]
- Berhow MT, Hiroi N, Nestler EJ. Regulation of ERK (extracellular signal regulated kinase), part of the neurotrophin signal transduction cascade, in the rat mesolimbic dopamine system by chronic exposure to morphine or cocaine. J Neurosci. 1996;16:4707–4715. doi: 10.1523/JNEUROSCI.16-15-04707.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birdsong WT, Arttamangkul S, Clark MJ, Cheng K, Rice KC, Traynor JR, et al. Increased agonist affinity at the mu-opioid receptor induced by prolonged agonist exposure. J Neurosci. 2013;33:4118–4127. doi: 10.1523/JNEUROSCI.4187-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobeck EN, Haseman RA, Hong D, Ingram SL, Morgan MM. Differential development of antinociceptive tolerance to morphine and fentanyl is not linked to efficacy in the ventrolateral periaqueductal gray of the rat. J Pain. 2012;13:799–807. doi: 10.1016/j.jpain.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohn LM, Gainetdinov RR, Lin FT, Lefkowitz RJ, Caron MG. Mu-opioid receptor desensitization by beta-arrestin-2 determines morphine tolerance but not dependence. Nature. 2000;408:720–723. doi: 10.1038/35047086. [DOI] [PubMed] [Google Scholar]
- Bradaia A, Berton F, Ferrari S, Luscher C. beta-Arrestin2, interacting with phosphodiesterase 4, regulates synaptic release probability and presynaptic inhibition by opioids. Proc Natl Acad Sci U S A. 2005;102:3034–3039. doi: 10.1073/pnas.0406632102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Castiglione R, Rossi AC. Structure-activity relationships of dermorphin synthetic analogues. Peptides. 1985;6(Suppl. 3):117–125. doi: 10.1016/0196-9781(85)90361-4. [DOI] [PubMed] [Google Scholar]
- Chieng B, Christie MJ. Hyperpolarization by opioids acting on mu-receptors of a sub-population of rat periaqueductal gray neurones in vitro. Br J Pharmacol. 1994;113:121–128. doi: 10.1111/j.1476-5381.1994.tb16183.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie MJ. Cellular neuroadaptations to chronic opioids: tolerance, withdrawal and addiction. Br J Pharmacol. 2008;154:384–396. doi: 10.1038/bjp.2008.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor M, Osborne PB, Christie MJ. μ-opioid receptor desensitization: is morphine different? Br J Pharmacol. 2004;143:685–696. doi: 10.1038/sj.bjp.0705938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daaka Y, Luttrell LM, Ahn S, Della Rocca GJ, Ferguson SS, Caron MG, et al. Essential role for G protein-coupled receptor endocytosis in the activation of mitogen-activated protein kinase. J Biol Chem. 1998;273:685–688. doi: 10.1074/jbc.273.2.685. [DOI] [PubMed] [Google Scholar]
- Dang VC, Williams JT. Chronic morphine treatment reduces recovery from opioid desensitization. J Neurosci. 2004;24:7699–7706. doi: 10.1523/JNEUROSCI.2499-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll C, Konietzko J, Poll F, Koch T, Hollt V, Schulz S. Agonist-selective patterns of micro-opioid receptor phosphorylation revealed by phosphosite-specific antibodies. Br J Pharmacol. 2011;164:298–307. doi: 10.1111/j.1476-5381.2011.01382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll C, Poll F, Peuker K, Loktev A, Gluck L, Schulz S. Deciphering micro-opioid receptor phosphorylation and dephosphorylation in HEK293 cells. Br J Pharmacol. 2012;167:1259–1270. doi: 10.1111/j.1476-5381.2012.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake CT, Aicher SA, Montalmant FL, Milner TA. Redistribution of mu-opioid receptors in C1 adrenergic neurons following chronic administration of morphine. Exp Neurol. 2005;196:365–372. doi: 10.1016/j.expneurol.2005.08.012. [DOI] [PubMed] [Google Scholar]
- Duttaroy A, Yoburn BC. The effect of intrinsic efficacy on opioid tolerance. Anesthesiology. 1995;82:1226–1236. doi: 10.1097/00000542-199505000-00018. [DOI] [PubMed] [Google Scholar]
- Finn AK, Whistler JL. Endocytosis of the mu opioid receptor reduces tolerance and a cellular hallmark of opiate withdrawal. Neuron. 2001;32:829–839. doi: 10.1016/s0896-6273(01)00517-7. [DOI] [PubMed] [Google Scholar]
- Goodman CB, Emilien B, Becketts K, Cadet JL, Rothman RB. Downregulation of mu-opioid binding sites following chronic administration of neuropeptide FF (NPFF) and morphine. Peptides. 1996;17:389–397. doi: 10.1016/0196-9781(96)00002-2. [DOI] [PubMed] [Google Scholar]
- Grabs D, Slepnev VI, Songyang Z, David C, Lynch M, Cantley LC, et al. The SH3 domain of amphiphysin binds the proline-rich domain of dynamin at a single site that defines a new SH3 binding consensus sequence. J Biol Chem. 1997;272:13419–13425. doi: 10.1074/jbc.272.20.13419. [DOI] [PubMed] [Google Scholar]
- Grecksch G, Bartzsch K, Widera A, Becker A, Hollt V, Koch T. Development of tolerance and sensitization to different opioid agonists in rats. Psychopharmacology (Berl) 2006;186:177–184. doi: 10.1007/s00213-006-0365-8. [DOI] [PubMed] [Google Scholar]
- Gupta A, Mulder J, Gomes I, Rozenfeld R, Bushlin I, Ong E, et al. Increased abundance of opioid receptor heteromers after chronic morphine administration. Sci Signal. 2010;3:ra54. doi: 10.1126/scisignal.2000807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hack SP, Bagley EE, Chieng BC, Christie MJ. Induction of delta-opioid receptor function in the midbrain after chronic morphine treatment. J Neurosci. 2005;25:3192–3198. doi: 10.1523/JNEUROSCI.4585-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He L, Kim JA, Whistler JL. Biomarkers of morphine tolerance and dependence are prevented by morphine-induced endocytosis of a mutant mu-opioid receptor. FASEB J. 2009;23:4327–4334. doi: 10.1096/fj.09-133223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinricher MM, Ingram SL. The brainstem and nociceptive modulation. In: Bushnell MC, Basbaum AI, editors. The Senses: A Comprehensive Reference. Vol. 5. San Diego, CA: Academic Press; 2008. pp. 593–626. [Google Scholar]
- Herskovits JS, Burgess CC, Obar RA, Vallee RB. Effects of mutant rat dynamin on endocytosis. J Cell Biol. 1993;122:565–578. doi: 10.1083/jcb.122.3.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath RJ, Landry RP, Romero-Sandoval EA, DeLeo JA. Morphine tolerance attenuates the resolution of postoperative pain and enhances spinal microglial p38 and extracellular receptor kinase phosphorylation. Neuroscience. 2010;169:843–854. doi: 10.1016/j.neuroscience.2010.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignatova EG, Belcheva MM, Bohn LM, Neuman MC, Coscia CJ. Requirement of receptor internalization for opioid stimulation of mitogen-activated protein kinase: biochemical and immunofluorescence confocal microscopic evidence. J Neurosci. 1999;19:56–63. doi: 10.1523/JNEUROSCI.19-01-00056.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram SL, Vaughan CW, Bagley EE, Connor M, Christie MJ. Enhanced opioid efficacy in opioid dependence is caused by an altered signal transduction pathway. J Neurosci. 1998;18:10269–10276. doi: 10.1523/JNEUROSCI.18-24-10269.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram SL, Macey TA, Fossum EN, Morgan MM. Tolerance to repeated morphine administration is associated with increased potency of opioid agonists. Neuropsychopharmacology. 2008;33:2494–2504. doi: 10.1038/sj.npp.1301634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keith DE, Murray SR, Zaki PA, Chu PC, Lissin DV, Kang L, et al. Morphine activates opioid receptors without causing their rapid internalization. J Biol Chem. 1996;271:19021–19024. doi: 10.1074/jbc.271.32.19021. [DOI] [PubMed] [Google Scholar]
- Kelly E. Efficacy and ligand bias at the mu-opioid receptor. Br J Pharmacol. 2013a;169:1430–1446. doi: 10.1111/bph.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly E. Ligand bias at the mu-opioid receptor. Biochem Soc Trans. 2013b;41:218–224. doi: 10.1042/BST20120331. [DOI] [PubMed] [Google Scholar]
- Kelly E, Bailey CP, Henderson G. Agonist-selective mechanisms of GPCR desensitization. Br J Pharmacol. 2008;153(Suppl. 1):S379–S388. doi: 10.1038/sj.bjp.0707604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenakin T, Christopoulos A. Measurements of ligand bias and functional affinity. Nat Rev Drug Discov. 2013;12:483–484. doi: 10.1038/nrd3954-c2. [DOI] [PubMed] [Google Scholar]
- Kenakin T, Watson C, Muniz-Medina V, Christopoulos A, Novick S. A simple method for quantifying functional selectivity and agonist bias. ACS Chem Neurosci. 2012;3:193–203. doi: 10.1021/cn200111m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilkenny C, Browne W, Cuthill IC, Emerson M, Altman DG. Animal research: Reporting in vivo experiments: The ARRIVE guidelines. Br J Pharmacol. 2010;160:1577–1579. doi: 10.1111/j.1476-5381.2010.00872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JA, Bartlett S, He L, Nielsen CK, Chang AM, Kharazia V, et al. Morphine-induced receptor endocytosis in a novel knockin mouse reduces tolerance and dependence. Curr Biol. 2008;18:129–135. doi: 10.1016/j.cub.2007.12.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer HK, Simon EJ. mu and delta-opioid receptor agonists induce mitogen-activated protein kinase (MAPK) activation in the absence of receptor internalization. Neuropharmacology. 2000;39:1707–1719. doi: 10.1016/s0028-3908(99)00243-9. [DOI] [PubMed] [Google Scholar]
- Krasel C, Bunemann M, Lorenz K, Lohse MJ. Beta-arrestin binding to the beta2-adrenergic receptor requires both receptor phosphorylation and receptor activation. J Biol Chem. 2005;280:9528–9535. doi: 10.1074/jbc.M413078200. [DOI] [PubMed] [Google Scholar]
- Lane DA, Patel PA, Morgan MM. Evidence for an intrinsic mechanism of antinociceptive tolerance within the ventrolateral periaqueductal gray of rats. Neuroscience. 2005;135:227–234. doi: 10.1016/j.neuroscience.2005.06.014. [DOI] [PubMed] [Google Scholar]
- Lin X, Wang Q, Ji J, Yu LC. Role of MEK-ERK pathway in morphine-induced conditioned place preference in ventral tegmental area of rats. J Neurosci Res. 2010;88:1595–1604. doi: 10.1002/jnr.22326. [DOI] [PubMed] [Google Scholar]
- Macey TA, Lowe JD, Chavkin C. Mu opioid receptor activation of ERK1/2 is GRK3 and arrestin dependent in striatal neurons. J Biol Chem. 2006;281:34515–34524. doi: 10.1074/jbc.M604278200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macey TA, Bobeck EN, Hegarty DM, Aicher SA, Ingram SL, Morgan MM. Extracellular signal-regulated kinase 1/2 activation counteracts morphine tolerance in the periaqueductal gray of the rat. J Pharmacol Exp Ther. 2009;331:412–418. doi: 10.1124/jpet.109.152157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macey TA, Ingram SL, Bobeck EN, Hegarty DM, Aicher SA, Arttamangkul S, et al. Opioid receptor internalization contributes to dermorphin-mediated antinociception. Neuroscience. 2010;168:543–550. doi: 10.1016/j.neuroscience.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhavan A, He L, Stuber GD, Bonci A, Whistler JL. micro-Opioid receptor endocytosis prevents adaptations in ventral tegmental area GABA transmission induced during naloxone-precipitated morphine withdrawal. J Neurosci. 2010;30:3276–3286. doi: 10.1523/JNEUROSCI.4634-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath J, Drummond G, Kilkenny C, Wainwright C. Guidelines for reporting experiments involving animals: the ARRIVE guidelines. Br J Pharmacol. 2010;160:1573–1576. doi: 10.1111/j.1476-5381.2010.00873.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson J, Rivero G, Baptist M, Llorente J, Al-Sabah S, Krasel C, et al. mu-opioid receptors: correlation of agonist efficacy for signalling with ability to activate internalization. Mol Pharmacol. 2010;78:756–766. doi: 10.1124/mol.110.066613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchiorri P, Negri L. The dermorphin peptide family. Gen Pharmacol. 1996;27:1099–1107. doi: 10.1016/0306-3623(95)02149-3. [DOI] [PubMed] [Google Scholar]
- Mittal N, Tan M, Egbuta O, Desai N, Crawford C, Xie CW, et al. Evidence that behavioral phenotypes of morphine in beta-arr2-/- mice are due to the unmasking of JNK signaling. Neuropsychopharmacology. 2012;37:1953–1962. doi: 10.1038/npp.2012.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D, Liu Y, Roberts DC. Rapid and persistent sensitization to the reinforcing effects of cocaine. Neuropsychopharmacology. 2006a;31:121–128. doi: 10.1038/sj.npp.1300773. [DOI] [PubMed] [Google Scholar]
- Morgan MM, Fossum EN, Levine CS, Ingram SL. Antinociceptive tolerance revealed by cumulative intracranial microinjections of morphine into the periaqueductal gray in the rat. Pharmacol Biochem Behav. 2006b;85:214–219. doi: 10.1016/j.pbb.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Murphy JE, Padilla BE, Hasdemir B, Cottrell GS, Bunnett NW. Endosomes: a legitimate platform for the signaling train. Proc Natl Acad Sci U S A. 2009;106:17615–17622. doi: 10.1073/pnas.0906541106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narita M, Ioka M, Suzuki M, Narita M, Suzuki T. Effect of repeated administration of morphine on the activity of extracellular signal regulated kinase in the mouse brain. Neurosci Lett. 2002;324:97–100. doi: 10.1016/s0304-3940(02)00141-6. [DOI] [PubMed] [Google Scholar]
- Ortiz J, Harris HW, Guitart X, Terwilliger RZ, Haycock JW, Nestler EJ. Extracellular signal-regulated protein kinases (ERKs) and ERK kinase (MEK) in brain: regional distribution and regulation by chronic morphine. J Neurosci. 1995;15:1285–1297. doi: 10.1523/JNEUROSCI.15-02-01285.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne PB, Vaughan CW, Wilson HI, Christie MJ. Opioid inhibition of rat periaqueductal grey neurones with identified projections to rostral ventromedial medulla in vitro. J Physiol. 1996;490:383–389. doi: 10.1113/jphysiol.1996.sp021152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paronis CA, Holtzman SG. Development of tolerance to the analgesic activity of mu agonists after continuous infusion of morphine, meperidine or fentanyl in rats. J Pharmacol Exp Ther. 1992;262:1–9. [PubMed] [Google Scholar]
- Patierno S, Anselmi L, Jaramillo I, Scott D, Garcia R, Sternini C. Morphine induces mu opioid receptor endocytosis in guinea pig enteric neurons following prolonged receptor activation. Gastroenterology. 2011;140:618–626. doi: 10.1053/j.gastro.2010.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawar M, Kumar P, Sunkaraneni S, Sirohi S, Walker EA, Yoburn BC. Opioid agonist efficacy predicts the magnitude of tolerance and the regulation of mu-opioid receptors and dynamin-2. Eur J Pharmacol. 2007;563:92–101. doi: 10.1016/j.ejphar.2007.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paxinos G, Watson C. The Rat Brain in Stereotaxic Coordinates. 5th edn. Burlington, MA: Elsevier Academic Press; 2005. [Google Scholar]
- Phillips RS, Cleary DR, Nalwalk JW, Arttamangkul S, Hough LB, Heinricher MM. Pain-facilitating medullary neurons contribute to opioid-induced respiratory depression. J Neurophysiol. 2012;108:2393–2404. doi: 10.1152/jn.00563.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivero G, Llorente J, McPherson J, Cooke A, Mundell SJ, McArdle CA, et al. Endomorphin-2: a biased agonist at the mu-opioid receptor. Mol Pharmacol. 2012;82:178–188. doi: 10.1124/mol.112.078659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozenfeld R, Devi LA. Receptor heterodimerization leads to a switch in signaling: beta-arrestin2-mediated ERK activation by mu-delta opioid receptor heterodimers. FASEB J. 2007;21:2455–2465. doi: 10.1096/fj.06-7793com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternini C, Spann M, Anton B, Keith DE, Jr, Bunnett NW, von Zastrow M, et al. Agonist-selective endocytosis of mu opioid receptor by neurons in vivo. Proc Natl Acad Sci U S A. 1996;93:9241–9246. doi: 10.1073/pnas.93.17.9241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens CW, Yaksh TL. Potency of infused spinal antinociceptive agents is inversely related to magnitude of tolerance after continuous infusion. J Pharmacol Exp Ther. 1989;250:1–8. [PubMed] [Google Scholar]
- Tortorici V, Robbins CS, Morgan MM. Tolerance to the antinociceptive effect of morphine microinjections into the ventral but not lateral-dorsal periaqueductal gray of the rat. Behav Neurosci. 1999;113:833–839. doi: 10.1037//0735-7044.113.4.833. [DOI] [PubMed] [Google Scholar]
- Vallee RB, Herskovits JS, Aghajanian JG, Burgess CC, Shpetner HS. Dynamin, a GTPase involved in the initial stages of endocytosis. Ciba Found Symp. 1993;176:185–193. doi: 10.1002/9780470514450.ch12. discussion 193–197. [DOI] [PubMed] [Google Scholar]
- Vaughan CW, Christie MJ. Presynaptic inhibitory action of opioids on synaptic transmission in the rat periaqueductal grey in vitro. J Physiol. 1997;498:463–472. doi: 10.1113/jphysiol.1997.sp021872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whistler JL, von Zastrow M. Morphine-activated opioid receptors elude desensitization by beta-arrestin. Proc Natl Acad Sci U S A. 1998;95:9914–9919. doi: 10.1073/pnas.95.17.9914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whistler JL, von Zastrow M. Dissociation of functional roles of dynamin in receptor-mediated endocytosis and mitogenic signal transduction. J Biol Chem. 1999;274:24575–24578. doi: 10.1074/jbc.274.35.24575. [DOI] [PubMed] [Google Scholar]
- Whistler JL, Chuang HH, Chu P, Jan LY, von Zastrow M. Functional dissociation of mu opioid receptor signaling and endocytosis: implications for the biology of opiate tolerance and addiction. Neuron. 1999;23:737–746. doi: 10.1016/s0896-6273(01)80032-5. [DOI] [PubMed] [Google Scholar]
- Williams JT, Ingram SL, Henderson G, Chavkin C, von Zastrow M, Schulz S, et al. Regulation of mu-opioid receptors: desensitization, phosphorylation, internalization, and tolerance. Pharmacol Rev. 2013;65:223–254. doi: 10.1124/pr.112.005942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Chu J, Qiu Y, Loh HH, Law PY. Agonist-selective signaling is determined by the receptor location within the membrane domains. Proc Natl Acad Sci U S A. 2008;105:9421–9426. doi: 10.1073/pnas.0802253105. [DOI] [PMC free article] [PubMed] [Google Scholar]