Abstract
Recent theoretical and empirical work suggests that adults with borderline personality disorder (BPD) have difficulty regulating both shame and anger, and that these emotions may be functionally related in clinically relevant ways (e.g., Schoenleber & Berenbaum, 2012b). The covariation of shame with anger-related emotions has important clinical implications for interventions targeting shame and uncontrolled anger in BPD. However, no studies have examined shame, anger, and their covariation in adolescents who may be at risk for developing BPD. Therefore, this study focuses on associations between BPD symptoms and patterns of covariation between daily experiences of shame and anger-related affects (i.e., hostile irritability) in a community sample of adolescent girls using ecological momentary assessment. Multilevel models revealed that girls with greater BPD symptoms who reported greater mean levels of shame across the week also tended to report more hostile irritability, even after controlling for guilt. Additionally, examination of within-person variability showed that girls with greater BPD symptoms reported more hostile irritability on occasions when they also reported greater concurrent shame, but this was only the case in girls of average socioeconomic status (i.e., those not receiving public assistance). Unlike shame, guilt was not associated with hostile irritability in girls with greater BPD symptoms. Results suggest that shame may be a key clinical target in the treatment of anger-related difficulties among adolescent girls with BPD symptoms.
Keywords: borderline personality disorder, shame, hostility, irritability, ecological momentary assessment
Symptoms of borderline personality disorder (BPD) are usually recognizable by adolescence and are associated with a host of poor long-term outcomes (Chanen & McCutcheon, 2013; Winograd, Cohen, & Chen, 2008). Although prevalence rates are similar across men and women in the general population, studies indicate higher rates of BPD among adolescent girls and young women in clinical and forensic settings, and greater distress and impairment in women with BPD as compared to their male counterparts (APA, 2013; Grant et al., 2008; Rosler, Retz, Yaqoobi, Burg, & Retz-Junginger, 2009). In addition, research has shown that BPD symptoms peak during mid-adolescence, between ages 14 and 17 (Bornovalova, Hicks, Iacono, & McGue, 2009). Research on the early manifestations and characteristics of BPD symptoms during mid-adolescence, especially in girls, is therefore critical in the effort to develop targeted prevention and treatment strategies (Chanen & McCutcheon, 2013).
Although BPD is associated with a range of negative affects, recent theoretical and empirical work suggests that adults with BPD have particular difficulties regulating shame and anger-related emotions (Berenson et al., 2011; Gratz et al., 2010; Linehan, 1993). Moreover, several authors have suggested that anger-related affects may be elicited in the context of intense shame among individuals with BPD, perhaps as a defensive attempt to deflect attention away from the shamed self and direct blame to others (Bateman & Fonagy, 2004; Schoenleber & Berenbaum, 2012b; Velotti, Elison, & Garofalo, 2014). According to these theorists, shame could be a prime driver of anger-related emotions and thus may be an important clinical target in the treatment of anger and aggression in those with BPD.
However, little empirical work has examined emotional dysfunction, let alone patterns of dysregulation and covariation of specific emotional states, among adolescents with emerging BPD symptoms. This is a significant gap considering that proneness to intense shame and anger is associated with poor outcomes and higher likelihood of future self-harm and suicide attempts in adults with BPD (Brodsky, Groves, Oquendo, Mann, & Stanley, 2006; Brown, Linehan, Comtois, Murray, & Chapman, 2009; Rusch et al., 2008; Welch & Linehan, 2002). In addition, both shame and anger are relevant to the fundamental difficulties with identity and relatedness that are believed by many to lie at the core of personality disorders (Bender, Morey, & Skodol, 2011; Skodol et al., 2011).
Shame-proneness and Shame-aversion in BPD
Shame is characterized by a feeling that one is inherently a bad or defective person (Lewis, 2000). Thus, shame involves a general and global negative evaluation of the whole self, which is closely aligned with the negative self-representations and self-concepts reported in those with BPD (Butler, Brown, Beck, & Grisham, 2002; Jovev & Jackson, 2004). A large body of research suggests that shame can be distinguished from guilt, a related yet distinct emotion characterized by feeling bad about specific actions or behaviors that are inconsistent with one's moral values (Lewis, 2000). Both shame and guilt involve negative self-evaluations, and are therefore often referred to as self-conscious emotions, but several studies have demonstrated that shame is more strongly associated with maladaptive behaviors and psychopathology than guilt (Bennett, Sullivan, & Lewis, 2010; Fergus, Valentiner, McGrath, & Jencius, 2010; Tangney, Wagner, & Gramzow, 1992b). In fact, many studies have shown that guilt is unrelated or even inversely related to problem behaviors after controlling for shame (Fergus et al., 2010; Tangney, Wagner, Fletcher, & Gramzow, 1992a; Tangney et al., 1992b).
A number of theorists and researchers have discussed shame as a central emotion in BPD (Linehan, 1993; Rizvi, Brown, Bohus, & Linehan, 2011; Rusch et al., 2007; Schoenleber & Berenbaum, 2012a). Rusch and colleagues (2007) found that adult BPD patients scored higher than healthy controls or patients with social phobia on both explicit and implicit measures of shame. Another study found that adult BPD patients reacted to negative evaluation in the laboratory with greater increases in shame, but not other emotions, relative to a clinical group without personality disorder (Gratz et al., 2010). In the first published study to our knowledge that has examined shame in relation to BPD symptoms in children or adolescents, Hawes, Helyer, Herlianto, and Willing (2012) found that the identity disturbance component of BPD features was associated with an implicit measure of shame-prone self-concept, but only among girls (ages 10-14). One study also found that although BPD symptoms in undergraduate students were positively associated with shame-proneness, they were negatively associated with guilt-proneness (Schoenleber & Berenbaum, 2012a), supporting distinctions between shame and guilt in their association with BPD. The same study also found that students with greater BPD symptoms reported high levels of shame aversion, i.e., experiencing shame as particularly painful and intolerable.
Anger-Related Emotions in BPD
Anger-related emotions, including irritability and hostility, are central components of emotion dysregulation in BPD and may serve as precursors to the development of the disorder (Carlotta, Borroni, Maffei, & Fossati, 2013; Crowell, Beauchaine, & Linehan, 2009; Stepp, Burke, Hipwell, & Loeber, 2012). For instance, research suggests that uncontrolled anger and affective instability are the most predictive criteria for distinguishing between adolescents with and without a BPD diagnosis (Becker, Grilo, Edell, & McGlashan, 2002). In addition, higher levels of anger, aggression, and impulsivity differentiated adolescent inpatients with BPD from those with major depressive disorder, and were associated with more suicidality in those with BPD (Horesh, Orbach, Gothelf, Efrati, & Apter, 2003). In a longitudinal study, adolescents who failed to show a normative reduction in hostility and exhibited increases in impulsive behaviors across ages 13 to 17 were at an increased risk for Cluster B personality disorders (Kobak, Zajac, & Smith, 2009). These findings underscore the importance of examining anger-related emotions in adolescents who may at risk for the development of BPD, as these difficulties are among the earliest of BPD-related traits to emerge and are prognostic of poor long-term outcomes.
Associations between Shame and Anger-related Emotions
Not only are shame and anger prominent emotional experiences in BPD, but some authors have suggested that shame and anger may be functionally related in clinically important ways (Schoenleber & Berenbaum, 2012b; Velotti et al., 2014). Beyond the BPD literature, social psychologists have written extensively on the potential for shame to evoke simultaneous anger and aggression (e.g., Gilligan, 1997; Lutwak, Panish, Ferrari, & Razzino, 2001; Tangney et al., 1992a). In various samples across developmental stages (i.e., childhood through adulthood), shame has been shown to generate hostile and aggressive behaviorial responses (Bennett, Sullivan, & Lewis, 2005; Scheel et al., 2013; Thomaes, Bushman, Stegge, & Olthof, 2008), whereas guilt has been associated with constructive responses to anger such as cognitive reappraisals and nonhostile corrective actions (Tangney, Wagner, Hill-Barlow, Marschall, & Gramzow, 1996).
Although no studies currently exist with adolescents, recent evidence suggests that shame has a particularly strong association with anger and aggression in adults with BPD. For instance, shame-proneness has been associated with anger and hostility, as well as chronic suicidal ideation, suicide attempts, and self-injurious behavior in adult BPD patients (Brodsky et al., 2006; Brown et al., 2009; Rizvi et al., 2011; Rizvi & Linehan, 2005; Rusch et al., 2007, 2008; Welch & Linehan, 2002). Moreover, a recent study found that adults with BPD reacted to shame induction in the laboratory with greater increases in anger and more sustained anger than depressed patients or healthy controls (Scheel et al., 2013), implying that BPD may be associated with the simultaneous co-occurrence of anger with shame. It has been suggested that externalized anger is one of several maladaptive strategies for avoiding or deflecting intense shame, and that individuals with BPD symptoms may be more likely to instantaneously convert shame to anger-related affects due to their tendency toward shame-aversion, i.e., experiencing shame as intolerable (Schoenleber & Berenbaum, 2012a). Thus, anger may co-occur with shame among individuals with BPD, perhaps as a defensive attempt to deflect attention away from the shamed self and direct blame to others (Schoenleber & Berenbaum, 2012b).
Goals and Hypotheses of the Current Study
In summary, experiences of shame and anger, and the momentary covariation of shame and anger-related emotions, are clinically significant but understudied aspects of BPD, and are therefore the focus of the current study. Using ecological momentary assessment (EMA) of affective experiences across a one-week period, we examined individual differences in BPD symptoms as a potential moderator of associations between experiences of shame and anger-related emotions (operationalized as a composite of irritability and hostility, referred to hereafter as hostile irritability) in daily life after controlling for experiences of guilt. The use of EMA is a significant improvement over previous studies of shame and angry affects in BPD by providing intensive repeated measures that allow for the disentangling of between-person differences in dispositional affect (i.e., mean levels over the course of the week) and within-person fluctuations or variability in affective states. In addition, the diverse community sample provides significant variability in race and socioeconomic status (SES), which are often not explored in clinical studies but may have important implications for culturally sensitive theory and practice. We examined the covariation between concurrent reports of affects rather than time-lagged relationships because clinical theory and past research suggest that shame can instantaneously or very quickly lead to angry affects, suggesting a momentary co-occurrence of these affective experiences rather than time-lagged relationships (Bennett et al., 2005; Scheel et al., 2013; Thomaes et al., 2008).
In accordance with the theoretical and empirical literature reviewed above, our hypotheses were as follows: 1) Between-person differences in mean levels of shame over the course of the week (i.e., dispositional shame or shame-proneness), and not guilt, will be positively associated with hostile irritability, but only among those with greater BPD symptoms; and 2) Within-person momentary reports of shame, and not guilt, will be positively associated with contemporaneous reports of hostile irritability, but only among those with greater BPD symptoms. In addition, considering the diverse study sample and previous studies demonstrating associations between sociodemographic factors such as low SES and anger, aggression, and psychopathology (Conger et al., 1994; Evans, 2004; Evans & English, 2002), we also took the opportunity to explore race and SES as potential moderators of these hypothesized relationships.
Method
Participants and Recruitment Procedures
One hundred and fourteen 16-year-old girls with a wide range of BPD symptoms were recruited from the ongoing Pittsburgh Girls Study (PGS) for a substudy on girls' personality development. The ongoing PGS involves an urban community sample of four age cohorts of girls who were ages 5-8 at the first assessment in 2000/2001 and have been followed with annual assessments since that time. The PGS sample was identified by oversampling from low-income neighborhoods, such that neighborhoods in which at least 25% of families were living at or below poverty level were fully enumerated and a random selection of 50% of households in all other neighborhoods were enumerated. Of the 2,875 eligible families that were contacted to determine interest in study participation, 2,450 families (85%) agreed to participate in the PGS and provided informed consent (see Keenan et al., 2010 for further details on PGS study design).
One hundred and fourteen girls were selected from the larger PGS for participation in the current substudy in 2010-2012 (girls in cohort 7 in 2010, cohort 6 in 2011, and cohort 5 in 2012). To obtain a sample with a high degree of variability in core symptoms of BPD, girls were recruited based on their self reports on the Affective Instability subscale of the Personality Assessment Inventory (PAI-AI; Morey, 1991), which assesses a core symptom of BPD and was administered as part of the main PGS annual assessment battery. Approximately one-third of girls who were recruited for the current substudy screened high on affective instability (scores > 11 on the PAI-AI), and the remainder of the sample was randomly selected from girls endorsing low to medium levels of affective instability (scores ≤ 11). This sampling strategy was intended to produce a sample with a wide range of BPD symptoms (affective instability as well as associated symptoms consistent with BPD such as impulsivity, chaotic interpersonal relationships, intense and inappropriate anger, self-harm, and identity disturbance).
Out of the 114 girls who were recruited for this substudy, 89 completed diagnostic interviews for personality disorders and a seven-day EMA protocol. Thus, 89 girls are included in the current analyses. The 89 girls who participated did not significantly differ from the 25 who did not participate in terms of race, SES, PAI-AI scores, or number of BPD symptoms. Reflecting the demographic characteristics of the PGS, this sample was racially and socioeconomically diverse (67% African American, 33% Caucasian; 53% of families reported receiving some form of public assistance in the last year, e.g., WIC, food stamps, welfare, temporary assistance for needy families).
Assessment Procedures and Measures
Participants completed semi-structured interviews for Axis I and II disorders in the laboratory, followed by a one-week cellular phone-based EMA protocol in their home environments. All study procedures were approved by the University Institutional Review Board. Participants were compensated for their participation.
Assessment of BPD Symptoms
BPD symptoms were assessed dimensionally using the Structured Clinical Interview for DSM-IV Personality Disorders (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997), a semi-structured interview with established reliability and validity for assessing the presence and severity of personality disorders in adolescents. Interviewers were post-baccalaureat, masters, or doctoral-level clinicians who were trained to reliability by the corresponding author (SDS). The nine items corresponding to individual DSM-5 diagnostic criteria for BPD were rated on a 0-3 scale (0 = not present, 1 = subthreshold, 2 = present, 3 = strongly present). Per DSM-5 (APA, 2013) guidelines for the diagnosis of personality disorder in adolescence, symptoms were only rated “present” if they were present for at least the past year and judged to be pervasive, persistent, and unlikely to be limited to developmental stage or an episode of another disorder. The nine BPD items were summed to yield a dimensional score for BPD symptoms, which was used as a continuous measure of BPD symptoms.
Twenty-two participants' SIDP-IV interviews (25% of the analyzed sample) were videotaped and rated by at least one additional independent rater for calculation of interrater reliability. The number of raters per case ranged from 2 to 6 (N = 14 cases had 2 raters, 4 had 3 raters, 2 had 4 raters, and the remaining 2 had 5 and 6 raters). ICC's were calculated based on one-way random effect models for the unequal number of raters per case, and demonstrated excellent interdiagnostician agreement for BPD dimensional scores (ICC = .91). The distribution of BPD criteria that were met above clinical threshold (i.e., items scored ≥ 2) is presented in Table 1. The prevalence of diagnosable BPD in the current study sample (4.5%) is within the range found in other community adolescent samples (e.g., 3-6%; Chabrol et al., 2004; Zanarini, 2003). Consistent with previous studies with adolescent samples (e.g., Becker et al., 2002; Zanarini et al., 2011), intense anger and affective instability were the most frequently met BPD criteria in this sample.
Table 1. Distribution of BPD symptoms met above threshold in study sample (N = 89).
| BPD criterion | N | % |
|---|---|---|
| 1. Efforts to avoid abandonment | 2 | 2.2 |
| 2. Unstable relationships | 8 | 9.0 |
| 3. Identity disturbance | 3 | 3.4 |
| 4. Impulsivity | 11 | 12.4 |
| 5. Suicide/self-harm behavior | 4 | 4.5 |
| 6. Affective instability | 25 | 28.1 |
| 7. Chronic emptiness | 11 | 12.4 |
| 8. Intense anger | 33 | 37.1 |
| 9. Paranoid/dissociative | 9 | 10.1 |
| BPD symptom counts (# criteria) | ||
| 0 | 47 | 52.8 |
| 1 | 11 | 12.4 |
| 2 | 13 | 14.6 |
| 3 | 7 | 7.9 |
| 4 | 7 | 7.9 |
| 5 | 4 | 4.5 |
Note. Criteria were counted as present (i.e., above threshold) based on item scores ≥ 2 on the Structured Clinical Interview for DSM-IV Personality Disorders (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997).
Ecological Momentary Assessment of Affect
After completion of diagnostic interviews, participants were given modified, answer-only cellular telephones to use during the EMA protocol. Based on their reported wake and sleep times and activity schedules, participants were scheduled to receive a maximum of four calls from research staff per day over the course of seven days (maximum of 28 calls across the week). Due to some participants' after-school activities and work schedules, there was individual variability in the number of planned calls per day, as further described below. At each call, participants were asked questions about their current mood, activities, and location. For mood items (Happy, Sad, Nervous, Excited, Scared, Ashamed, Irritable, Hostile, Guilty, Alert), girls were asked to rate how they had been feeling in the last 15 minutes on a 5-point Likert scale (1 = very slight or not at all; 5 = extremely). Similar procedures have been successfully used in previous EMA studies with child and adolescent samples (e.g., Primack et al., 2011; Silk et al., 2011). As with these previous studies, participants could not take calls during school hours. However, previous studies have been limited to evening and weekend assessments, and we improved on this by including a morning call. On school days, call 1 was before school, and calls 2-4 were after school up until 10:00pm. On weekends, call 1 was within an hour of the girl's reported awakening time, and calls 2-4 were scheduled at equal intervals across the day until 10:00pm. If a participant missed the first call, second and third attempts to reach the participant were made, each in 10-minute intervals.
Although 93 girls agreed to participate in the EMA protocol, data were excluded from three girls who completed less than seven calls over the course of the week (i.e., less than one call per day on average) and from one girl who did not complete diagnostic interviews, leaving a sample of 89 girls who were included in this report. The current analyses included 1569 phone calls (M = 17.81 successful calls per person; SD = 4.06; Range = 7-27). The mean number of planned phone calls per person was 20.67 (SD = 3.82) and the compliance rate (i.e., percentage of planned calls that were successful) was 86.31% (SD = 12.37%; Median = 90.5% Range = 35% to 100%). Neither the number of calls planned nor individual compliance rates were significantly associated with any study variables (r's ≤ .15, ns), nor did these factors emerge as significant covariates in any of the models tested. As expected considering the inability to assess girls during school or work hours, there was wide variability in the time lags between assessments (M = 8.84 hrs, SD = 8.84, Range = 0.17–70.53 hrs). For the majority of assessments (78%), girls reported being at home at the time of assessment. Reported activities included media use (28%); family, peer, or school-related activities (24%); personal care or eating (18%); chores, shopping, outdoor activities, or transportation (18%); and either sleeping or doing “nothing” (12%).
The current analysis uses participants' ratings on four emotions that directly pertain to our study hypotheses: Ashamed, Guilty, Irritable, and Hostile. Ratings of irritability and hostility were highly correlated (r = .65, p < .001) and loaded on the same factor in an exploratory factor analysis (EFA). Bivariate correlations also suggested that hostility and irritability were related to other study variables in similar ways (e.g., with shame, r's = .45 and .48, which did not significantly differ, z = 0.39, ns; and with guilt, r's = .39 and .33, z = 0.72, ns). Ratings of hostility and irritability were therefore combined into a single “hostile irritability” score by calculating the mean of these ratings for each person at each occasion. Models were also tested with hostility and irritability as separate dependent variables, and results were generally the same across these constructs, supporting their combination to streamline analyses and results. Although ratings of shame and guilt were also highly correlated (r = .77, p < .001), they loaded on separate factors in an EFA and showed differential relationships with other study variables (e.g., shame was significantly associated with BPD symptoms, r = .29, p < .01, but guilt was not, r = .09, ns, and these correlations differed significantly from one another, z = 2.82, p < .005; and shame was more strongly associated with hostile irritability, r = .52, than was guilt, r = .38, z = 2.20, p < .05). These findings are consistent with previous research suggesting distinctions between shame and guilt in their associations with psychopathology (Bennett et al., 2010; Fergus et al., 2010; Tangney et al., 1992b). Shame and guilt were therefore treated as separate constructs, allowing us to examine their differential effects on hostile irritability. Because shame, guilt, and hostile irritability ratings were positively skewed, they were log-transformed prior to analysis.
Analytic Procedures
Hypotheses were tested using multilevel structural equation modeling (MSEM) in Mplus version 7 (Muthén & Muthén, 2012) using full-information maximum likelihood estimation with robust standard errors (MLR estimator). MLR estimation can include missing data and produces unbiased parameter estimates and standard errors that are robust to moderate non-normality. As illustrated in Figure 1, the MSEM included the random intercept for hostile irritability, which captured individual differences in mean levels of hostile irritability across the week, and two random slopes (s1 and s2) reflecting momentary hostile irritability regressed on person-mean-centered repeated measures of momentary shame (“ShameW”) and guilt (“GuiltW”). The intercept of hostile irritability and the two slopes were then regressed on BPD symptom dimensional scores from the baseline assessment, minority race (0 = White; 1 = African American), and low SES at age 16 (0 = not receiving public assistance; 1 = receiving public assistance). We used the receipt of public assistance as a marker of low SES, as this variable was highly correlated with family income level (r = .66, p < .001) while being more sensitive than pure household income to family size and resources available to the family. The regression of BPD symptoms on slopes allowed us to test the hypothesis that individuals with greater BPD symptoms would show a stronger within-person coupling of momentary shame with contemporaneous hostile irritability. In addition, the intercept of hostile irritability was regressed on each individual's own mean levels of shame and guilt across the diary period (i.e., grand-mean-centered person means of shame and guilt, labeled as “ShameB” and “GuiltB”, respectively). Interaction terms for BPD×ShameB and BPD×GuiltB were also included as predictors of the intercept of hostile irritability to test the hypothesis that those with higher BPD symptoms and higher mean levels of shame (i.e., greater dispositional shame) across the week also tend to report higher levels of hostile irritability. All continuous between-person predictors (i.e., BPD symptoms, ShameB, and GuiltB) were grand-mean centered. We also included the BPD×Race and BPD×Low SES interaction terms in our initial model to explore whether effects varied as a function of demographic characteristics. BPD×Race was not a significant predictor in any part of the model, and was therefore dropped from the final analyses for parsimony. We probed significant interactions by testing the significance of simple slopes at selected values of the moderators (-/+1SD) and examining the regions of significance for such effects in accordance with Preacher, Curran, and Bauer (2006).
Figure 1.

Multilevel structural equation model illustrating within-person effects at level 1 and between-person effects at level 2. Filled circles represent random effects. s1 = slope of momentary hostile irritability regressed on momentary shame. s2 = slope of momentary hostile irritability regressed on momentary guilt. BPD = borderline personality disorder symptoms. Race, socioeconomic status (SES), and two-way interactions between level 2 covariates were also included in the model (see Table 3 for all regression coefficients), but are not included in the figure for ease of interpretation.
Results
Descriptive statistics (prior to centering and transformations) and correlations for all study variables are presented in Table 2. To test for multicollinearity, we ran a series of multiple regressions in which each predictor was regressed on all other predictors, and examined variance inflation factors (VIFs). All VIFs fell below 2.5, indicating that multicollinearity was not an issue (O'Brien, 2007).
Table 2. Descriptive statistics and intercorrelations for all study variables (N = 89).
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Race | ||||||
| 2. Low SES | .30** | |||||
| 3. BPD symptoms | .16 | .22* | ||||
| 4. Shame┼ | .03 | .01 | .29** | |||
| 5. Guilt┼ | -.05 | -.07 | .09 | .77*** | ||
| 6. Hostile Irritability┼ | .09 | .25* | .49** | .52*** | .38*** | |
|
| ||||||
| %/M | 67% | 53% | 3.87 | 1.06 | 1.08 | 1.36 |
| SD | 3.85 | 0.11 | 0.18 | 0.39 | ||
| Range | 0-15 | 1.00-1.53 | 1.00-2.16 | 1.00-2.94 | ||
| ICC | 0.06 | 0.19 | 0.29 | |||
Note. Race was coded 0 = White/Caucasion, 1 = African American. Low SES was coded 0 = no public assistance, 1 = receiving public assistance. Thus, percentages can be interpreted to mean that 67% of the sample was African American, and 53% had lower SES (i.e., receiving public assistance). BPD symptoms = borderline personality disorder dimensional scores, calculated based on the sum of the nine BPD item scores from the Structured Interview for DSM-IV Personality (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997). Hostile Irritability was calculated based on the mean of hostility and irritability ratings from ecological momentary assessment (EMA) protocol.
Descriptive statistics are presented for measures of shame, guilt, and hostile irritability aggregated within individuals across the entire EMA protocol. Thus, ranges for these measures represent the range of individual means across repeated measures, rather than the range of momentary scores (which ranged from 1 to 5). Means and correlations were computed prior to log transformation of affect variables.
p < .05.
p < .01.
p < .001.
Between-person Effects of Mean Levels of Shame and Guilt on Hostile irritability
Unstandardized coefficients from the final MSEM are presented in Table 3. BPD symptoms had a significant main effect on mean levels of hostile irritability, indicating that greater BPD symptoms were associated with greater hostile irritability. Individual differences in mean levels of shame (ShameB) were not associated with hostile irritability in the sample overall. However, as hypothesized, there was a significant interaction between BPD symptoms and ShameB. Simple slopes tests demonstrated that greater mean levels of shame were associated with greater hostile irritability among those with high BPD symptoms only (+1SD; B = 1.77, SE = 0.57, z = 3.10, p = .002) and not among those with medium (i.e., at the sample mean; B = 0.71, SE = 0.44, z = 1.62, p = .11) or low (-1SD; B = -0.34, SE = 0.57, z = -0.61, p = .54) BPD symptoms. The confidence interval for the simple slope at all conditional values of BPD symptoms indicated that the association between mean levels of shame and hostile irritability was significant at or above a grand-mean-centered BPD symptom value of 0.54, which corresponds to a raw BPD dimensional score of between 5 and 6 (or approximately 2 to 3 symptoms of BPD met above threshold). These effects were not moderated by SES.
Table 3. Multilevel structural equation model unstandardized regression coefficients.
| Fixed Effects | Dependent Variables | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Hostile Irritability (intercept) | Hostile Irritability on ShameW (s1) | Hostile Irritability on GuiltW (s2) | ||||
|
|
|
|
||||
| B | SE | B | SE | B | SE | |
| Intercept | 0.18*** | 0.03 | 0.20** | 0.08 | 0.11 | 0.12 |
| Race | <0.01 | 0.03 | 0.02 | 0.13 | -0.14 | 0.17 |
| Low SES | 0.07∼ | 0.04 | -0.15 | 0.15 | 0.38* | 0.17 |
| BPD symptoms | 0.01* | 0.01 | 0.04* | 0.02 | -0.02 | 0.03 |
| BPD × Low SES | <0.01 | 0.01 | -0.06* | 0.03 | -0.01 | 0.04 |
| ShameB | 0.71 | 0.44 | ||||
| GuiltB | 0.30 | 0.30 | ||||
| BPD × ShameB | 0.29** | 0.10 | ||||
| BPD × GuiltB | -0.14* | 0.09 | ||||
Note. Hostile Irritability was calculated based on the mean of hostility and irritability ratings from ecological momentary assessment (EMA) protocol. Race was coded 0 = White/Caucasion, 1 = African American. Low SES was coded 0 = no public assistance, 1 = receiving public assistance. BPD = borderline personality disorder symptoms. ShameW = within-person fluctuations in shame (person-mean-centered momentary shame ratings). GuiltW = within-person fluctuations in guilt (person-mean-centered momentary guilt ratings). ShameB = between-person differences in mean shame across the week (grand-mean-centered person means). GuiltB = between-person differences in mean guilt across the week (grand-mean-centered person means).
p < .10.
p < .05.
p < .01.
p < .001.
Within-Person Effects of Momentary Shame and Guilt on Hostile Irritability
In the overall sample, within-person momentary shame (ShameW), but not guilt (GuiltW), was positively associated with concurrent ratings of hostile irritability. Thus, in the sample overall, higher ratings of shame (and not guilt) tended to co-occur with greater concurrent reports of hostile irritability. As hypothesized, there was a main effect of BPD symptoms on the relationship between momentary shame and hostile irritability (s1), indicating that girls with greater BPD symptoms tended to report greater hostile irritability on occasions when they also reported more shame; however, there was also a significant interaction between BPD and SES. As illustrated in Figure 2, only girls with higher BPD symptoms and average SES (i.e., those not receiving public assistance) reported greater hostile irritability on occasions when they also reported experiencing more shame (B = 0.36, SE = 0.13, z = 2.66, p = .008). The confidence interval for the simple slope at all conditional values of BPD symptoms for girls with average SES indicated that the positive within-person momentary association between shame and hostile irritability was significant at or above a grand-mean-centered BPD symptom value of -1.87, which corresponds to a raw BPD dimensional score of about 2 (or approximately 1 symptom of BPD met above threshold, or 2 symptoms met at sub-threshold). Within-person associations between momentary shame and hostile irritability were not significantly different from zero among those with high BPD symptoms and low SES nor among those with low BPD symptoms (-1SD), regardless of SES (all ps > .05).
Figure 2.
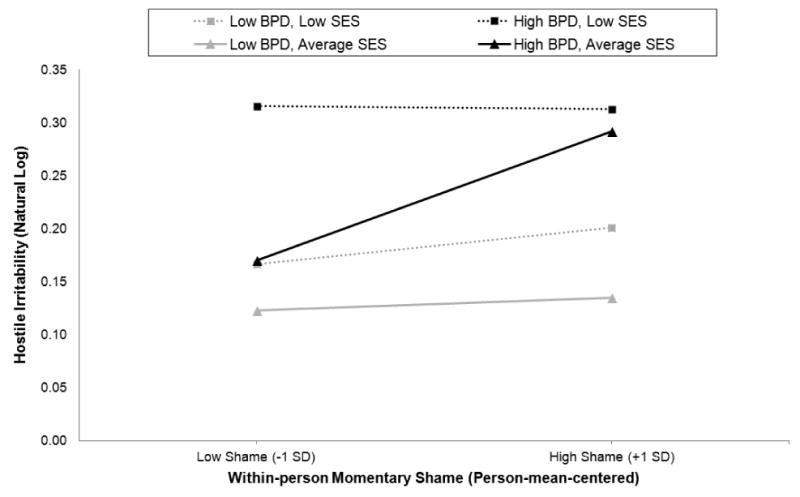
Within-person associations between momentary shame and concurrent momentary hostile irritability (log-transformed) as a function of borderline personality disorder (BPD) symptoms and socioeconomic status (SES). Lines represent model-estimated simple slopes at - 1SD and +1SD from the mean of BPD symptoms and at low (i.e., receiving public assistance) and average (i.e., not receiving public assistance) SES levels. The association between momentary shame (within-person deviations from individual means) and hostile irritability is only significant (i.e., different from zero, p < .05) among girls with high BPD symptoms and average SES (solid black line).
As hypothesized, BPD symptoms were not significantly associated with the coupling of guilt with hostile irritability either at between- or within-person levels. Unexpectedly, however, girls with low SES showed a stronger within-person association of momentary guilt (and not shame) with concurrent hostile irritability, regardless of BPD symptoms. Simple slopes tests revealed that momentary guilt was only significantly associated with hostile irritability for girls with low SES (B = 0.49, SE = 0.21, z = 2.27, p = .02), and not among girls with average SES (B = 0.11, SE = 0.12, z = 0.92, p = .36).
In a supplemental analysis, we examined whether results differed if BPD dimensional scores were calculated without including the “intense anger” criterion. This step allowed us to explore whether the coupling of shame with hostile irritability is only stronger among those with anger-related BPD symptoms, or if these results generalize to other BPD symptoms such as affective instability or impulsivity. All results and substantive interpretations remained the same in this supplemental analysis, suggesting that shame is positively associated with hostile irritability among those with greater non-anger-related BPD symptoms such as affective instability and impulsivity. However, the association between low SES and overall hostile irritability became significant (B = 0.07, SE = 0.04, z = 1.97, p < .05), whereas it was not significant in the above results (p = .06). Further details from this analysis are available upon request from the first author.
Discussion
We examined whether BPD symptoms in a diverse community sample of adolescent girls predicted associations between experiences of shame and anger-related emotions (i.e., hostile irritability) in daily life. Results generally supported hypothesized associations between shame and anger-related affects in those with greater BPD symptoms and demonstrated important distinctions between shame and guilt in this regard. Specifically, consistent with our hypotheses, mean levels of shame, and not guilt, over the course of the week were associated with greater hostile irritability, but only in girls with high levels BPD symptoms. In addition, as hypothesized, girls with greater BPD symptoms tended to report more hostile irritability on occasions when they also reported experiencing more shame, but not on occasions when they reported more guilt. However, the within-person coupling of momentary shame with hostile irritability was only found among those girls with greater BPD symptoms and average SES (i.e., those not receiving public assistance). This within-person link between shame and hostile irritability emerged among girls of average SES with as few as one symptom of BPD met above threshold, or two symptoms at subthreshold.
Our finding that shame, and not guilt, was associated with hostile irritability in girls with higher BPD symptoms is consistent with studies that have demonstrated negligible or even negative associations between guilt and psychopathology or anger-related emotions after controlling for shame (Tangney et al., 1992a, 1992b). However, this is the first study to our knowledge to examine the momentary within-person associations between shame, guilt, and angry affects using intensive repeated measures. Our results extend previous findings by demonstrating that the within-person momentary covariation of shame and guilt with anger-related emotions in adolescent girls depends on their level of BPD symptoms and SES, such that momentary shame (but not guilt) is associated with simultaneous anger-related emotions only in girls with greater BPD symptoms and average SES.
Consistent with recent literature reviews suggesting that shame confers greater vulnerability to angry reactivity and aggression (e.g., Schoenleber & Berenbaum, 2012b; Velotti et al., 2014), our results imply that shame and anger-related emotions may be functionally related in adolescent girls with BPD symptoms, even in those with BPD symptoms at subthreshold levels. Perhaps due to features such as rejection sensitivity and a fragile sense of self, individuals with BPD can be particularly prone to intense shame while also experiencing shame as highly intolerable and threatening to their sense of self and relatedness to others (Velotti et al., 2014). Thus, they might be more likely to externalize blame and react angrily in efforts to regulate shame and regain a sense of control. Although it is possible that shame may emerge as a consequence of being more hostile and irritable (e.g., feeling bad about being grumpy), previous research suggests that anger-related emotions co-occur simultaneously with shame, as opposed to occurring as a consequence of shame (Bennett et al., 2005; Scheel et al., 2013; Thomaes et al., 2008; Velotti et al., 2014). Nonetheless, the temporal relationships between shame and anger should be explored in future studies with more frequent daily measurements of affect with shorter and less variable time lags between assessments.
Although the effects of SES observed in this study were not hypothesized, they warrant discussion and interpretation. It is noteworthy that the predicted relationship between momentary shame and hostile irritability only emerged among girls with high BPD symptoms and average SES. As shown in Figure 2, girls with high BPD symptoms and low SES reported high levels of hostile irritability regardless of their concurrent levels of shame. There may be a ceiling effect for the high-BPD and low SES girls, whose hostile irritability is so high that there is little room to increase as a function of shame. These results may imply that the additive combination of BPD symptoms with poverty represents a high degree of cumulative risk (e.g., see Evans, Li, & Whipple, 2013) that predisposes adolescent girls to higher levels of hostile irritability, independent of shame. Previous research has documented associations between economic adversity and exposure to hostility, aggression, and violence both at home and in the community, which in turn influences the development of adjustment problems in children, including hostile and aggressive behavior (e.g., Conger et al., 1994; Evans & English, 2002). BPD symptoms may further compound this risk by virtue of higher trait anger and aggression, thereby predisposing these girls to higher levels of hostile irritability for reasons that are independent of concurrent levels of shame. There may also be aspects of living in an average to high SES environment, such as invalidation of the child's emotions or behaviors that do not meet familial expectations (Linehan, 1993), that could promote experiences of shame in those with BPD symptoms. This is an interesting possibility to explore in future studies.
As hypothesized, BPD symptoms did not predict a stronger coupling of guilt with hostile irritability, but we unexpectedly found that low SES was associated with a stronger within-person coupling of momentary guilt with hostile irritability, regardless of BPD level. This contrasts with findings from previous studies indicating that guilt is not associated with anger or aggression after controlling for shame (for review, see Velotti et al., 2014). However, one study has found that shame-free guilt is linked to higher internalizing and externalizing symptoms in early adolescent girls but not boys (Ferguson, Stegge, Miller, & Olsen, 1999). The authors suggest that this may be due to a gender paradox, i.e., as compared to boys, girls tend to receive harsher consequences from their environment and to express more remorse and regret for their delinquent behavior. Perhaps girls living in poverty may try to cover or regulate this guilt with anger-related emotions; conversely, they might feel guilty for acting in an irritable or hostile manner. Alternatively, girls with limited family resources may differ in their level of understanding, interpretation, and daily usage of words like “shame” and “guilt” due to differences in emotion socialization and/or education, obscuring distinctions between these constructs in their self reports. Although we can only speculate about these potential explanations, they suggest that SES deserves further investigation in studies of BPD in the effort to develop more culturally sensitive prevention strategies.
The current study fills important gaps in previous research by examining not only mean levels of affective experiences but also momentary patterns of covariation between self-conscious and anger-related affects in relation to BPD symptoms. The assessment of daily affective experiences using EMA methodology is ideal for examining these within-person processes with greater ecological validity than laboratory-based assessment on a single occasion. On a related note, the intensive repeated measures of affect allowed us to use a statistical approach that improves upon past studies by disaggregating between- and within-persons effects so that relations between both trait and state levels of shame and angry emotions could be examined. Further, the diverse adolescent community sample is advantageous and novel because BPD-related pathology has generally been understudied in adolescents with sociodemographic risk factors such as low SES. Although this introduces heterogeneity and statistical power may be limited to detect moderation effects, the diverse sample allowed us to explore whether the hypothesized relations between shame and anger-related emotions in adolescents with BPD symptoms differed across racial and socioeconomic strata.
On the other hand, this study has several limitations that should be noted. The inability to assess girls during school and work hours restricts ecological validity, and these are social contexts in which adolescent girls may have been most prone to experiencing intense shame and anger-related emotions. There were also insufficient assessments in close enough succession to one another to examine the temporal sequence of affective experiences. In order to establish whether shame precedes angry affects, or vice-versa, it would be necessary to sample affective experiences at a much higher frequency and resolution (i.e., several assessments within minutes of each other). Furthermore, we relied on single items to assess complex affective constructs, and it is unclear how girls understood or interpreted these emotion words when making their ratings. This is common in EMA studies (Scollon, Kim-Prieto, & Diener, 2003; Stone & Shiffman, 1994), in which it is necessary to reduce the number of items in order to alleviate participant burden and increase compliance with intensive repeated measures. However, this limitation may be mitigated by recent evidence for the validity and reliability of single-item measures (Dollinger & Malmquist, 2009; Hoeppner, Kelly, Urbanoski, & Slaymaker, 2011), and the consistency of our results distinguishing between shame and guilt with previous studies using multiple-item measures of these constructs suggests that our measures have validity. Finally, given the adolescent community sample of only girls, these results may not generalize to males, adults, or to treatment-seeking individuals with a diagnosis of BPD.
Despite these limitations, there are several implications of these results for clinical assessment and interventions. First, our results suggest that shame could be a key clinical target for interventions aimed at preventing or reducing angry or aggressive behavior in adolescent girls with BPD symptoms. Clinicians should be aware of the possibility that hostility, irritability, or other anger-related emotions might mask underlying experiences of intense shame, or at least co-occur with them. Angry emotions may be more noticeable on the surface, whereas shame could be hidden and may go unnoticed, especially in the context of hostile behavior. Careful assessment of shame experiences, particularly in those who demonstrate angry or hostile affects, may be warranted in order to adequately validate and directly target intense shame. Accurate validation of such underlying shame experiences may help to mitigate angry affects and allow for the introduction of more adaptive ways of coping with shame. Clinical interventions that are designed to target shame, such as compassion focused therapy (Gilbert, 2011), elements of dialectical behavior therapy (e.g., opposite action, mindfulness, and acceptance; Rizvi et al., 2011), and some relational or object relations approaches (Stadter, 2011), may be particularly helpful in reducing the intensity of shame and maladaptive reactions to experiences of shame, including anger and aggression directed at self or others (Velotti et al., 2014). Finally, our results suggest that these affective processes may operate differently in girls from low-SES backgrounds, highlighting the importance of considering the influence of family-level adversity in research and clinical assessment.
Acknowledgments
This research and the efforts of the authors were supported by grants from the National Institute of Mental Health (K01 MH086713, PI: Stepp; R01 MH56630, PI: Loeber; R01 MH056888, PI: Pilkonis; K01 MH101289, PI: Scott; F32 MH097311, PI: Scott; F31 MH093991, PI: Whalen; K01 MH097091, PI: Hallquist), the National Institute on Drug Abuse (R01 DA012237, PI: Chung), and by funding from the Office of Juvenile Justice and Delinquency Prevention, the FISA Foundation and the Falk Fund.
References
- American Psychiatric Association [APA] Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Bateman A, Fonagy A. Psychotherapy for borderline personality disorder: Mentalization-based treatment. Oxford, UK: Oxford University Press; 2004. [Google Scholar]
- Becker DF, Grilo CM, Edell WS, McGlashan TH. Diagnostic efficiency of borderline personality disorder criteria in hospitalized adolescents: Comparison with hospitalized adults. American Journal of Psychiatry. 2002;159(12):2042–2047. doi: 10.1176/appi.ajp.159.12.2042. [DOI] [PubMed] [Google Scholar]
- Bender DS, Morey LC, Skodol AE. Toward a model for assessing level of personality functioning in DSM–5, part I: A review of theory and methods. Journal of Personality Assessessment. 2011;93(4):332–346. doi: 10.1080/00223891.2011.583808. [DOI] [PubMed] [Google Scholar]
- Bennett DS, Sullivan MW, Lewis M. Young children's adjustment as a function of maltreatment, shame, and anger. Child Maltreatment. 2005;10(4):311–323. doi: 10.1177/1077559505278619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett DS, Sullivan MW, Lewis M. Neglected children, shame-proneness, and depressive symptoms. Child Maltreatment. 2010;15(4):305–314. doi: 10.1177/1077559510379634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson KR, Downey G, Rafiaeli E, Coifman KG, Paquin NL. The rejection-rage contingency in borderline personality disorder. Journal of Abnormal Psychology. 2011;120(3):681–690. doi: 10.1037/a0023335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathology. 2009;21(Special Issue 04):1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodsky BS, Groves SA, Oquendo MA, Mann JJ, Stanley B. Interpersonal precipitants and suicide attempts in borderline personality disorder. Suicide and Life-Threatening Behavior. 2006;36(3):313–322. doi: 10.1521/suli.2006.36.3.313. [DOI] [PubMed] [Google Scholar]
- Brown MZ, Linehan MM, Comtois KA, Murray A, Chapman AL. Shame as a prospective predictor of self-inflicted injury in borderline personality disorder: A multi-modal analysis. Behaviour Research and Therapy. 2009;47(10):815–822. doi: 10.1016/j.brat.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler AC, Brown GK, Beck AT, Grisham J. Assessment of dysfunctional beliefs in borderline personality disorder. Behaviour Research and Therapy. 2002;40:1231–1240. doi: 10.1016/s0005-7967(02)00031-1. [DOI] [PubMed] [Google Scholar]
- Carlotta D, Borroni S, Maffei C, Fossati A. On the relationship between retrospective childhood adhd symptoms and adult bpd features: The mediating role of action-oriented personality traits. Comprehensive Psychiatry. 2013;54(7):943–952. doi: 10.1016/j.comppsych.2013.03.025. [DOI] [PubMed] [Google Scholar]
- Chabrol H, Montovany A, Ducongé E, Kallmeyer A, Mullet E, Leichsenring F. Factor structure of the borderline personality inventory in adolescents. European Journal of Psychological Assessment. 2004;20(1):59–65. [Google Scholar]
- Chabrol H, Montovany A, Ducongé E, Kallmeyer A, Mullet E, Leichsenring F. Factor structure of the borderline personality inventory in adolescents. European Journal of Psychological Assessment. 2004;20(1):59–65. [Google Scholar]
- Chanen AM, McCutcheon L. Prevention and early intervention for borderline personality disorder: Current status and recent evidence. British Journal of Psychiatry. 2013;54:s24–29. doi: 10.1192/bjp.bp.112.119180. [DOI] [PubMed] [Google Scholar]
- Conger RD, Ge X, Elder GH, Jr, Lorenz FO, Simons RL. Economic stress, coercive family process, and developmental problems of adolescents. Child Development. 1994;65(2):541–561. [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending linehan's theory. Psychological Bulletin. 2009;135(3):495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dollinger SJ, Malmquist D. Reliability and validity of single-item self-reports: With special relevance to college students' alcohol use, religiosity, study, and social life. The Journal of General Psychology. 2009;136:231–242. doi: 10.3200/GENP.136.3.231-242. [DOI] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. American Psychologist. 2004;59(2):77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Evans GW, English K. The environment of poverty: Multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Development. 2002;73(4):1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychological Bulletin. 2013;139(6):1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- Fergus TA, Valentiner DP, McGrath PB, Jencius S. Shame- and guilt-proneness: Relationships with anxiety disorder symptoms in a clinical sample. Journal of Anxiety Disorders. 2010;24(8):811–815. doi: 10.1016/j.janxdis.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Ferguson TJ, Stegge H, Miller ER, Olsen ME. Guilt, shame, and symptoms in children. Developmental Psychology. 1999;35(2):347–357. doi: 10.1037//0012-1649.35.2.347. [DOI] [PubMed] [Google Scholar]
- Gilbert P. Shame in psychotherapy and the role of compassion focused therapy. In: D RL, Tangney JP, editors. Shame in the therapy hour. Washington, DC, US: American Psychological Association; 2011. pp. 325–354. [Google Scholar]
- Gilligan J. Violence : Reflections on a national epidemic. 1st Vintage Books. New York: Vintage Books; 1997. [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Ruan WJ. Prevalence, correlates, disability, and comorbidity of dsm-iv borderline personality disorder: Results from the wave 2 national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2008;69(4):533–450. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotional reactivity and delayed emotional recovery in borderline personality disorder: The role of shame. Comprehensive Psychiatry. 2010;51(3):272–285. doi: 10.1016/j.comppsych.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Hawes DJ, Helyer R, Herlianto EC, Willing J. Borderline personality features and implicit shame-prone self-concept in middle childhood and early adolescence. Journal of Clinical Child and Adolescent Psychology. 2012;42(3):302–308. doi: 10.1080/15374416.2012.723264. [DOI] [PubMed] [Google Scholar]
- Hoeppner BB, Kelly JF, Urbanoski KA, Slaymaker V. Comparative utility of a single-item versus multiple-item measure of self-efficacy in predicting relapse among young adults. Journal of Substance Abuse Treatment. 2011;41(3):305–312. doi: 10.1016/j.jsat.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh N, Orbach I, Gothelf D, Efrati M, Apter A. Comparison of the suicidal behavior of adolescent inpatients with borderline personality disorder and major depression. Journal of Nervous and Mental Disease. 2003;191(9):582–588. doi: 10.1097/01.nmd.0000087184.56009.61. [DOI] [PubMed] [Google Scholar]
- Jovev M, Jackson HJ. Early maladaptive schemas in personality disordered individuals. Journal of Personality Disorders. 2004;18(5):467–478. doi: 10.1521/pedi.18.5.467.51325. [DOI] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, McTigue K. The Pittsburgh Girls Study: Overview and initial findings. Journal of Clinical Child and Adolescent Psychology. 2010;39(4):506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak R, Zajac K, Smith C. Adolescent attachment and trajectories of hostile–impulsive behavior: Implications for the development of personality disorders. Dev Psychopathol. 2009;21(Special Issue 03):839–851. doi: 10.1017/S0954579409000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis M. Self-conscious emotions: Embarrassment, pride, shame, and guilt. In: Lewis M, Haviland-Jones J, editors. Handbook of emotions. 2nd. New York, NY: Guilford; 2000. pp. 623–636. [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Lutwak N, Panish JB, Ferrari JR, Razzino BE. Shame and guilt and their relationship to positive expectations and anger expressiveness. Adolescence. 2001;36(144):641–653. [PubMed] [Google Scholar]
- Morey LC. Personality assessment inventory: Professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Muthén BO, Muthén LK. Mplus user's guide. 7th. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- O'Brien RM. A caution regarding rules of thumb for variance inflation factors. Quality and Quantity. 2007;41(5):673–690. [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured interview for DSM-IV personality. Washington, D.C.: American Psychiatric Press; 1997. [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31(4):437–448. [Google Scholar]
- Primack BA, Silk JS, DeLozier CR, Shadel WG, Carpentier FRD, Dahl RE, Switzer GE. Using ecological momentary assessment to determine media use by individuals with and without major depressive disorder. Archives of Pediatric and Adolescent Medicine. 2011;165(4):360–365. doi: 10.1001/archpediatrics.2011.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Brown MZ, Bohus M, Linehan MM. The role of shame in the development and treatment of borderline personality disorder. In: D RL, Tangney JP, editors. Shame in the therapy hour. Washington, DC: American Psychological Association; US; 2011. pp. 237–260. [Google Scholar]
- Rizvi SL, Linehan MM. The treatment of maladaptive shame in borderline personality disorder: A pilot study of “opposite action”. Cognitive and Behavioral Practice. 2005;12(4):437–447. [Google Scholar]
- Rosler M, Retz W, Yaqoobi K, Burg E, Retz-Junginger P. Attention deficit/hyperactivity disorder in female offenders: Prevalence, psychiatric comorbidity and psychosocial implications. European Archives of Psychiatry and Clinical Neuroscience. 2009;259(2):98–105. doi: 10.1007/s00406-008-0841-8. [DOI] [PubMed] [Google Scholar]
- Rusch N, Lieb K, Gottler I, Hermann C, Schramm E, Richter H, Bohus M. Shame and implicit self-concept in women with borderline personality disorder. American Journal of Psychiatry. 2007;164(3):500–508. doi: 10.1176/ajp.2007.164.3.500. [DOI] [PubMed] [Google Scholar]
- Rusch N, Schiel S, Corrigan PW, Leihener F, Jacob GA, Olschewski M, Bohus M. Predictors of dropout from inpatient dialectical behavior therapy among women with borderline personality disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2008;39(4):497–503. doi: 10.1016/j.jbtep.2007.11.006. [DOI] [PubMed] [Google Scholar]
- Scheel CN, Schneid EM, Tuescher O, Lieb K, Tuschen-Caffier B, Jacob GA. Effects of shame induction in borderline personality disorder. Cognitive Therapy and Research. 2013:1–9. [Google Scholar]
- Schoenleber M, Berenbaum H. Aversion and proneness to shame in self- and informant-reported personality disorder symptoms. Personality Disorders: Theory, Research, and Treatment. 2012a;3(3):294–304. doi: 10.1037/a0025654. [DOI] [PubMed] [Google Scholar]
- Schoenleber M, Berenbaum H. Shame regulation in personality pathology. Journal of Abnormal Psychology. 2012b;121(2):433–446. doi: 10.1037/a0025281. [DOI] [PubMed] [Google Scholar]
- Scollon C, Kim-Prieto C, Diener E. Experience sampling: Promises and pitfalls, strengths and weaknesses. Journal of Happiness Studies. 2003;4(1):5–34. [Google Scholar]
- Silk JS, Forbes EE, Whalen DJ, Jakubcak JL, Thompson WK, Ryan ND, Dahl RE. Daily emotional dynamics in depressed youth: A cell phone ecological momentary assessment study. Journal of Experimental Child Psychology. 2011;110(2):241–257. doi: 10.1016/j.jecp.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, Bender DS, Morey LC, Clark LA, Oldham JM, Alarcon RD, Siever LJ. Personality disorder types proposed for DSM-5. Journal of Personality Disorders. 2011;25(2):136–169. doi: 10.1521/pedi.2011.25.2.136. [DOI] [PubMed] [Google Scholar]
- Stadter M. The inner world of shaming and ashamed: An object relations perspective and therapeutic approach. In: D RL, Tangney JP, editors. Shame in the therapy hour. Washington, DC, US: American Psychological Association; 2011. pp. 45–68. [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. Journal of Abnormal Child Psychology. 2012;40(1):7–20. doi: 10.1007/s10802-011-9530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (ema) in behavorial medicine. Annals of Behavioral Medicine. 1994;16(3):199–202. [Google Scholar]
- Tangney JP, Wagner P, Fletcher C, Gramzow R. Shamed into anger? The relation of shame and guilt to anger and self-reported aggression. Journal of Personality and Social Psychology. 1992a;62(4):669–675. doi: 10.1037//0022-3514.62.4.669. [DOI] [PubMed] [Google Scholar]
- Tangney JP, Wagner P, Gramzow R. Proneness to shame, proneness to guilt, and psychopathology. Journal of Abnormal Psychology. 1992b;101(3):469–478. doi: 10.1037//0021-843x.101.3.469. [DOI] [PubMed] [Google Scholar]
- Tangney JP, Wagner PE, Hill-Barlow D, Marschall DE, Gramzow R. Relation of shame and guilt to constructive versus destructive responses to anger across the lifespan. Journal of Personality and Social Psychology. 1996;70(4):797–809. doi: 10.1037//0022-3514.70.4.797. [DOI] [PubMed] [Google Scholar]
- Thomaes S, Bushman BJ, Stegge H, Olthof T. Trumping shame by blasts of noise: Narcissism, self-esteem, shame, and aggression in young adolescents. Child Development. 2008;79(6):1792–1801. doi: 10.1111/j.1467-8624.2008.01226.x. [DOI] [PubMed] [Google Scholar]
- Velotti P, Elison J, Garofalo C. Shame and aggression: Different trajectories and implications. Aggression and Violent Behavior 2014 [Google Scholar]
- Welch SS, Linehan MM. High-risk situations associated with parasuicide and drug use in borderline personality disorder. Journal of Personality Disorders. 2002;16(6):561–569. doi: 10.1521/pedi.16.6.561.22141. [DOI] [PubMed] [Google Scholar]
- Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: Prognosis for functioning over 20 years. Journal of Child Psychology and Psychiatry. 2008;49(9):933–941. doi: 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. American Journal of Psychiatry. 2003;160(2):274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Horwood J, Wolke D, Waylen A, Fitzmaurice G, Grant BF. Prevalence of DSM-IV borderline personality disorder in two community samples: 6,330 English 11-year-olds and 34,653 American adults. Journal of Personality Disorders. 2011;25(5):607–619. doi: 10.1521/pedi.2011.25.5.607. [DOI] [PMC free article] [PubMed] [Google Scholar]


