Abstract
Background:
Pregnancy tumor histologically coincides with oral pyogenic granuloma. It is a reactive hemorrhagic swelling that mostly occurs in gingiva of pregnant women and can cause some complications. Considering the lack of knowledge regarding its prevalence, this study aimed to determine the frequency and characteristics of pyogenic granuloma in pregnant women presenting to Tehran/Iran Medical Centers in 2013.
Materials and Methods:
In this descriptive cross-sectional study, a total of 923 pregnant women with a mean age of 27.7 ± 4.7 years were selected among those presenting to Tehran Medical Centers using consecutive sampling and clinical examination. Data were collected through interview and filling out a data form. Related variables were evaluated, and if the lesion was present, its clinical and histological characteristics were recorded. Data were analyzed and reported using relative and absolute frequency indices.
Results:
Of 923 pregnant women presenting only 2 (0.22%) had clinical and histological signs and symptoms of pyogenic granuloma. Both lesions had a firm consistency and were seen on maxillary gingiva. The lesions were not ulcerative, but both had bleeding.
Conclusion:
Considering the frequency of pyogenic granuloma in previous studies, it can be concluded that the prevalence of this lesion in pregnant women presenting to Tehran Medical Centers in 2013 is lower than previous studies.
Keywords: Gingiva, pregnant women, prevalence, pyogenic granuloma
Introduction
The pregnancy tumor is a particular type of pyogenic granuloma. Affected women are usually in their 3rd-9th month of pregnancy.1,2 Pyogenic granuloma occurs in anatomic location of gingiva in 5% of pregnancies;3 thus, the name pregnancy tumor or granuloma gravidarum.4 Hormonal imbalance following pregnancy affects the host response to irritation.5 However, bacterial plaque and gingival inflammation are necessary for hormonal changes causing gingivitis.6 These lesions may also interfere with the patient’s mastication.7 Owing to specific tissue structure, pyogenic granuloma lesions are usually ulcerative and tend to bleed8-10 causing secondary complications namely oral infection. If not diagnosed, inappropriate treatments like administration of unnecessary drugs may be used and be dangerous.11,12 Chronic stimulation is one etiology that can be hardly diagnosed. However, the location of these lesions being close to the gingival margin indicates that calculus, food residues and restoration overhangs are important stimuli that need to be eliminated after surgical resection of the lesion.8 However, definite etiologic factors of pyogenic granuloma have yet to be fully identified, and genetic, local and immunologic factors may also play a role in this respect.4,13
Preventive measures include adherence to oral hygiene instructions, dental plaque removal and use of the soft toothbrush by pregnant women. In the case of uncontrollable bleeding, the choice of treatment should be made based on patient’s specific condition.14 Surgical and periodontal treatments should be performed if possible.15 After surgery, the recurrence rate has been reported to be 16%16 and re-operation is inevitable in some cases.4,5,17
Chamani et al.18 reported the prevalence of gingival pregnancy tumor to be 4.2% among pregnant women presenting to Kerman/Iran Medical Centers. This rate was reported to be 4.5% by Khatibi et al., among patients presenting to one medical center in Tehran.19 Because previous studies reported the prevalence of this lesion just from one medical center and in some of them the number of the samples was low and no biopsy was conducted in confirmation of the diagnosis, the present study aimed to determine the prevalence of pyogenic granuloma in pregnant women presenting to several medical centers in Tehran in 2013.
Materials and Methods
This descriptive cross-sectional study was conducted among pregnant women presenting to five hospitals, as well as one clinic and a private office in 2012. We selected these centers from different areas of Tehran in order not to over-estimate or underestimate the prevalence rate. One hospital was selected from the west, one hospital and the private office were selected from the center, one hospital was selected from the south, the clinic from the southeast, one hospital from the northeast and the last from the north of Tehran. Patients were selected by consecutive sampling based on the admission ratio of each of the selected centers. A data form was specifically designed for this study by an oral medicine specialist and filled out by interviewing and clinical examination of patients. Any pedunculated or sessile red or pink prominent lesion with soft or firm consistency developed at any time following the onset of pregnancy were recorded as the primary diagnosis of pyogenic granuloma, and then biopsy was done as confirmation. Pink lesions had to have a history of color change from red to pink. Patients who also reported loosening and mobility of the adjacent teeth or those with a suspicious systematic history in favor of malignancy, HIV infection or hormonal imbalance (like hyperparathyroidism) were excluded from the study. The validity of the design and content of the data form was evaluated and confirmed by three oral medicine specialists. Number and percentage of patients based on number of previous pregnancies, gender of fetus, number of tooth brushings per day, use of dental floss and mouthwash, pattern of dental visits, consumption of oral contraceptive pills (OCPs), presence of supra gingival calculus at different areas and presence of pyogenic granuloma were reported on the data form. Also, the mean and standard deviation of patients’ age and fetal age were determined and reported.
Patients were selected from the waiting list of medical centers or their medical records, and their verbal consent was obtained for participation in the study. Under adequate lighting and using a dental mirror, the gingivae, vestibule, alveolar mucosa, lips, floor of the mouth, pharynx, gingiva, buccal mucosa, dorsal, ventral and lateral tongue surfaces and soft and hard palate were examined by a clinician for detection of pyogenic granuloma. Diagnosis of pyogenic granuloma was made based on the clinical manifestation of lesions, and histopathological examinations were carried out in Shahid Beheshti Medical School to rule out peripheral giant cell granuloma and the peripheral fibroma with calcification.
Results
In this study, 923 pregnant women were evaluated. Patients were in the age range of 17-41 years (mean age of 27.7 ± 4.7 years). The fetal age was in the range of 6-39 weeks (mean of 25.8 ± 9.5). Only 548 subjects had the fetal gender determined; out of which, 287 (52.4%) were males and 261 (47.6%) were females; 569 subjects (61.6%) were experiencing their first pregnancy, 262 (28.4%) had their second pregnancy, 74 (8.0%) their third, 15 (1.6%) their fourth and 3 (0.3%) their fifth pregnancy.
Distribution of subjects based on their tooth brushing pattern, use of dental floss and mouthwash is shown in Graphs 1-3.
Graph 1.
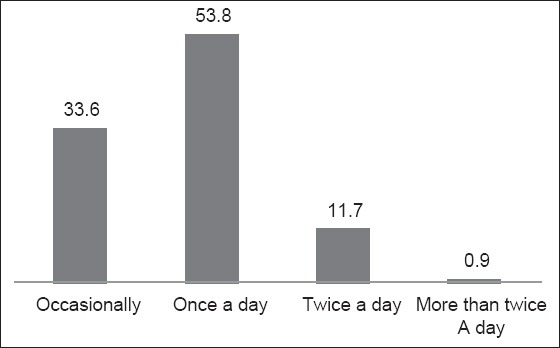
The frequency distribution of number of tooth brushings per day by the understudy pregnant women.
Graph 3.
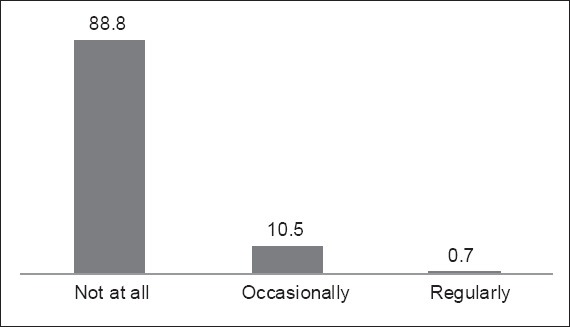
The frequency distribution of using mouthwash by the understudy pregnant women.
Graph 2.
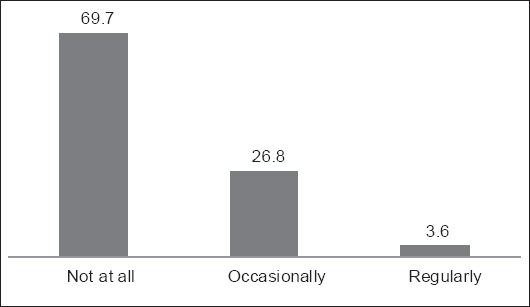
The frequency distribution of using dental floss by the understudy pregnant women.
Pattern of visiting a dentist was every 6 months in 3 (0.3%), once a year in 23 (2.5%), once every 2 years in 160 (17.3%) and less in 737 (79.8%) subjects. Consumption of OCPs was reported by 170 (18.4%) subjects; 753 (81.6%) did not report consumption of OCPs.
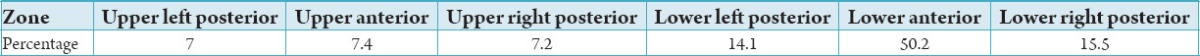
Dental calculus was present in the buccal area in 19 (2.1%), in the lingual area in 425 (46.0%) and in both buccal and lingual areas in 29 (3.1%) subjects. Table 1 summarizes the distribution of dental calculus at different areas of the dental arch.
Table 1.
Distribution of dental calculus in pregnant women.
Overall, two patients had pyogenic granuloma, and its diagnosis was histopathologically confirmed.
Patient one with pyogenic granuloma was a 29-year-old housewife with a sessile lesion with a firm consistency measuring 1.5 × 1 mm. The lesion was located in the labial and palatal gingival surfaces of maxillary incisors. It was red in color and had a smooth surface without tenderness. It was not ulcerative and had no induration at the base of the lesion. The lesion was hemorrhagic, and patient’s oral hygiene status was poor. The patient reported tooth brushing once a day and no use of dental floss or mouthwash.
The second patient with pyogenic granuloma was a 24-year-old housewife with no specific dental history. The patient was in her first pregnancy, and the fetal age was 4 months. The lesion was located in between the maxillary left central and lateral incisors. The lesion was unlobulated with pink to red color. The patient had calculus in every sextant of her teeth. The lesion surface was smooth and sessile without tenderness or ulceration. The base of the lesion had no induration, and the lesion had apparent bleeding.
Discussion
In the present study, of 923 pregnant women, 2 (0.22%) had clinical and histopathological signs and symptoms of PG.
Khatibi et al., in their study in 2013 reported the prevalence rate of PG to be 4.5% (72 out of 1600 pregnant women) among pregnant women presenting to one hospital in Tehran/Iran. This frequency was higher than ours.19 Alexanian and Rakhshanfar in 2001 also evaluated the prevalence of PG in the same hospital in Tehran and reported its prevalence rate to be 4%, which is similar to the abovementioned study but higher than our rate.20 Chamani et al. reported the prevalence rate of PG to be 4.2% among pregnant women presenting to Kerman/Iran medical centers. This rate is also close to the above-mentioned rate and higher than ours.18 Saebi and Robati in 1993 evaluated the periodontal tissue of pregnant women presenting to the Mashhad/Iran University of Medical Sciences and estimated the prevalence rate of PG to be 10%.21 The obtained higher rate in their study may be attributed to the fact that their study was conducted on patients’ dental records in the archives of the university, and the patients were not clinically examined. Saebi and Haghgoyan in 2000 evaluated the prevalence of periodontal disease among pregnant women presenting to one hospital in Tehran and reported the prevalence of PG to be 2%. This rate is closer to our obtained value.22
Our obtained value was lower than the reported prevalence rates in previous studies. One reason for this lower rate may be biopsy of lesions and their histological confirmation. Some researchers like Chamani et al.18 did not histopathologically examine the lesions, which may be responsible for the higher prevalence rate reported by them. Ideally, the diagnosis of pregnancy tumor should be made by histopathological analysis.4 However, obtaining patient consent for biopsy is always problematic in epidemiological studies. Moreover, in our study, subjects were selected from different districts of Tehran and different cultural and socioeconomic status of subjects may also play a role in this regard.
In our study, both cases of PG had a firm consistency, which is in accord with the results of previous studies.23 Some studies have not mentioned the consistency of lesions. However, it should be noted that the consistency of lesions depends on the age of the lesion. As the lesion matures, collagen fibers increase and the lesion becomes firmer.
One patient with PG in our study had heavy calculus. Both cases had poor oral hygiene and did not use dental floss or mouthwash. In a study by Shademan et al., in 2009 of all cases with a known etiology, dental calculus and poor oral hygiene were among the most common predisposing factors.23 Chronic gingival and inflammatory stimuli due to poor oral hygiene have also been suggested as the most important predisposing factors. Textbooks have reported poor oral hygiene as a predisposing factor for PG.12,15 Presence of deep or peusopockets, presence of calculus and inappropriate restorations or crowns invading the periodontal space and compromising its health also play a direct role in development of pregnancy tumor.12 Moreover, considering the special hormonal changes in pregnant women and their direct impact on gingival inflammation, periodontal problems and consequent complications like pregnancy tumor may be anticipated.12
Both PG lesions detected in our study were in the maxillary gingiva. Lawoyin et al., in 1997 studied 38 cases of oral PG lesions in Ibadan, Nigeria and showed that gingiva was the most commonly involved site (74%).24 Saravana in 2009 demonstrated that 55% of PG lesions involved the maxilla, and 83% occurred in the gingiva.25 In another study in Jordan, the gingiva was found to be the most commonly affected site by PG (44.4%).26 Krishnapillai et al., in 2012 evaluated the characteristics of oral PG in patients presenting to a teaching hospital in South India and indicated that 50.23% of lesions occurred in the maxillary gingiva and 46.53% in the mandibular gingiva.27 Chamani et al., in their study in 2009 among pregnant women presenting to Kerman Medical Centers showed that anterior maxilla, especially the facial gingiva and the embrasure in between the maxillary second premolar and first molar teeth were the most commonly involved sites.18 Shademan et al., in 2009 reported that the PG oral lesions were most commonly found in the anterior maxilla (34.7%), posterior maxilla (22.1%), anterior mandible (20%) and posterior mandible (15.7%).23 Furthermore in the study by Khatibi et al., in 2013 all lesions occurred in the gingiva and 66 lesions were in the maxilla and 6 in the mandible.19
The prevalence rate of PG is variable at different sites in the oral cavity and seems to be influenced by the presence of adequate connective tissue in the area, response rate to inflammation due to different factors, degree of susceptibility of the area to trauma or stimuli, absence of abnormal dentition, malocclusion and inappropriate restorations and poor oral hygiene.23
Usually, the lesion is not tender, but hemorrhagic because of high vascularity and ulcerative surface of the lesion. In our study, both patients with PG showed signs of bleeding. Rapid growth is another characteristic of PG necessitating its prompt assessment by a clinician to rule out malignancies. In long-lasting lesions of PG, displacement of the adjacent teeth may also be seen.23
Conclusion
Despite in this study the prevalence of pregnancy tumor of the gingiva is lower than previous, considering the high prevalence of periodontal disease and caries in our community as well as the risk of PG among pregnant women and complications that these lesions can cause, dental clinicians and obstetrician-gynecologists have the responsibility to enhance the public knowledge regarding the importance of oral hygiene especially during pregnancy.
Acknowledgement
This article was based on a undergraduate thesis by Tabatabaei Nejad which was successfully complete under the supervision of Dr. Taheri and with the close co-operation of the Oral Medicine Department of Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Footnotes
Source of Support: Nil
Conflict of Interest: None
References
- 1.Terezhalmy GT, Riley CK, Moore WS. Focal epithelial hyperplasia (Heck's disease) Quintessence Int. 2001;32(8):664–5. [PubMed] [Google Scholar]
- 2.Wang PH, Chao HT, Lee WL, Yuan CC, Ng HT. Severe bleeding from a pregnancy tumor. A case report. J Reprod Med. 1997;42(6):359–62. [PubMed] [Google Scholar]
- 3.Sills ES, Zegarelli DJ, Hoschander MM, Strider WE. Clinical diagnosis and management of hormonally responsive oral pregnancy tumor (pyogenic granuloma) J Reprod Med. 1996;41(7):467–70. [PubMed] [Google Scholar]
- 4.Neville BW, Damm DD, Allen CM, Bouqout JE. 3rd ed. St. Louis: Saunders; 2009. Oral &Maxillofacial Pathology; pp. 517–23. [Google Scholar]
- 5.Eversole LR. 3rd ed. Hamilton: BC Decker; 2002. Clinical Outline of Oral Pathology: Diagnosis and Treatment; pp. 113–4. [Google Scholar]
- 6.Sooriyamoorthy M, Gower DB. Hormonal influences on gingival tissue: Relationship to periodontal disease. J Clin Periodontol. 1989;16(4):201–8. doi: 10.1111/j.1600-051x.1989.tb01642.x. [DOI] [PubMed] [Google Scholar]
- 7.Tumini V, Di Placido G, D’Archivio D, Del Giglio Matarazzo A. Hyperplastic gingival lesions in pregnancy. I. Epidemiology, pathology and clinical aspects. Minerva Stomatol. 1998;47(4):159–67. [PubMed] [Google Scholar]
- 8.Greenberg MS, Glick M, Ship JA. 11th ed. Hamilton: BC Decker; 2008. Burket's Oral Medicine; pp. 133–7. [Google Scholar]
- 9.Gondivkar SM, Gadbail A, Chole R. Oral pregnancy tumor. Contemp Clin Dent. 2010;1(3):190–2. doi: 10.4103/0976-237X.72792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adeyemo WL, Hassan OO, Ajayi OF. Pregnancy-associated pyogenic granuloma of the lip: A case report. Niger J Med. 2011;20(1):179–80. [PubMed] [Google Scholar]
- 11.Ababneh K, Al-Khateeb T. Aggressive pregnancy tumor mimicking a malignant neoplasm: A case report. J Contemp Dent Pract. 2009;10(6):E072–8. [PubMed] [Google Scholar]
- 12.Caranza FA, Newmans MG. 8thed. Ch. 1. Vol. 14. Philadelphia: Saunders; 1996. Clinical Periodontology; p. 11. (192-4). 380-4. [Google Scholar]
- 13.Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16(1):79–82. doi: 10.4103/0973-029X.92978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steelman R, Holmes D. Pregnancy tumor in a 16-year-old: Case report and treatment considerations. J Clin Pediatr Dent. 1992;16(3):217–8. [PubMed] [Google Scholar]
- 15.Greenberg MS, Glick M. 10th ed. Hamilton: BC Decker, WB Saunders; 2003. Burket's Oral Medicine: Diagnosis and Treatment; pp. 141–2. [Google Scholar]
- 16.Taira JW, Hill TL, Everett MA. Lobular capillary hemangioma (pyogenic granuloma) with satellitosis. J Am Acad Dermatol. 1992;27:297–300. doi: 10.1016/0190-9622(92)70184-h. [DOI] [PubMed] [Google Scholar]
- 17.Regezi JA, Sciubba JJ, Jordan RC. 4th ed. Philadelphia: WB Saunders; 2003. Oral Pathology: Clinical Pathologic Considerations; pp. 115–6. [Google Scholar]
- 18.Chamani G, Navvabi N, Abdollahzadeh SH. The frequency of pregancny tumor in pregnant mothers. Dent J Shiraz Med Sci Univ. 2009;10:79–82. [Google Scholar]
- 19.Khatibi M, Niroomanesh SH, Abhari SY, Falakaflaki N. The frequency of pyogenic granuloma and the related factors in patients referred to MirzaKuchek Khan Hospital in Tehran during 2010-2011. Iran Obstet Gynecol Infertil. 2013;16:1–6. [Google Scholar]
- 20.Alexanian E, Rakhshannfar S. Prevalence of pyogenic granuloma in pregnant woman referred to Tehran MirzaKuchak Khan Hospital. J Shahid Beheshti Univ Med Sci Dent Coll. 2001;83:111–7. [Google Scholar]
- 21.Saebi KH, Robati B. Evaluation of periodontium tissue in pregnancy period in referred patient to Mashhad dental University. J Mashhad Univ Med Sci Dent Coll. 1993;14:165–71. [Google Scholar]
- 22.Saebi KH, Haghgoyan SH. Prevalence of periodontal disease in pregnancy in pregnant women referred to Mirza Kuchak Khan Hospital. J Shahid Beheshti Univ Med Sci Dent Coll. 2000;5:67–73. [Google Scholar]
- 23.Shademan N, farzin ebrahimi S, jafari S. Pyogenic granuloma: A review of clinical characteristics of 95 Cases. 3. 2009;17(83):59–66. [Google Scholar]
- 24.Lawoyin JO, Arotiba JT, Dosumu OO. Oral pyogenic granuloma: A review of 38cases from Ibadan, Nigeria. Br J Oral Maxillofac Surg. 1997;35(3):185–9. doi: 10.1016/s0266-4356(97)90561-1. [DOI] [PubMed] [Google Scholar]
- 25.Saravana GH. Oral pyogenic granuloma: A review of 137 cases. Br J Oral Maxillofac Surg. 2009;47(4):318–9. doi: 10.1016/j.bjoms.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Al-Khateeb T, Ababneh K. Oral pyogenic granuloma in Jordanians: A retrospective analysis of 108 cases. J Oral Maxillofac Surg. 2003;61(11):1285–8. doi: 10.1016/s0278-2391(03)00729-8. [DOI] [PubMed] [Google Scholar]
- 27.Krishnapillai R, Punnoose K, Angadi PV, Koneru A. Oral pyogenic granuloma – A review of 215 cases in a South Indian Teaching Hospital, Karnataka, over a period of 20 years. Oral Maxillofac Surg. 2012;16(3):305–9. doi: 10.1007/s10006-012-0315-z. [DOI] [PubMed] [Google Scholar]


