Abstract
Objectives
lder adults frequently experience falls, at great cost to themselves and society. Older adults with cancer may be at greater risk for falls and have unique risk factors.
Materials and Methods
We undertook a systematic review of the available medical literature to examine the current evidence regarding factors associated with falls in older adults with cancer. PubMed, Embase, CINAHL, CENTRAL, DARE, Cochrane Database of Systematic Reviews and clinical trials.gov were searched using standardized terms for concepts of oncology/cancer, people 60 and older, screening, falls and diagnosis. Eligible studies included cohort or case-control studies or clinical trials in which all patients, or a subgroup of patients, had a diagnosis of cancer and in which falls were either the primary or secondary outcome.
Results
We identified 31 studies that met our inclusion criteria. Several studies suggest that falls are more common in older adults with a diagnosis of cancer than those without. Among the 11 studies that explored factors associated with outpatient falls, some risk factors for falls established in the general population were also associated with falls in older adults with cancer, including dependence in activities of daily living and prior falls. Other factors associated with falls in a general population, such as age, polypharmacy and opioid use, were not predictive of falls among oncology populations. Falls among older adults with cancer in the inpatient setting were associated with established risk factors for falls in people without cancer, but also with factors unique to an oncology population, such as brain metastases.
Conclusions
Falls in older adults with cancer are more common than in the general population, and are associated with risk factors unique to people with cancer. Further study is needed to establish methods of screening older adults with cancer for fall risk and ultimately implement interventions to reduce their risk of falls. Identifying which older adults with cancer are at greater risk for falls is a requisite step to ultimately intervene and prevent falls in this vulnerable population.
Keywords: Cancer, elderly, older adults, falls, geriatric assessment, outcomes
Introduction
Falls are common, costly and under-recognized events in the lives of older adults, and are the leading cause of traumatic mortality in this age group.(1) Nearly one in three older adults fall each year.(2) At least 10% of falls result in injuries(3), including head injuries and fractures; more subtly, falls are associated with fear of falling and functional decline.
Cancer is a disease of aging. The rising incidence of cancer, coupled with the aging of the population will result in an anticipated 67% increase in the incidence of cancer in older adults by 2030.(4) With the rising incidence of cancer in older adults who may be at greater risk for falls, attention to falls will be essential to meet the clinical needs of this growing population. The Institute of Medicine recently convened a committee to evaluate cancer care in older adults; their report, “Delivering High-Quality Cancer Care: Charting a Course for a System in Crisis,” highlighted the need to “ensure that the care of older adults with cancer is well coordinated and comprehensive.”(5) In order to ensure that older adults receive such comprehensive care, with attention to falls, we must determine whether older adults with cancer are at greater risk for falls, and what risk factors are associated with falls in this vulnerable population.
We therefore undertook a systematic review to examine the rate of falls and factors associated with falls, including demographics, comorbidities, functional status, medications and psychosocial factors, in older adults with cancer in both the inpatient and community setting.
Methods
Search Strategy
In the framework of the PRISMA guidelines (www.prisma-statement.org), in conjunction with a medical librarian (SF), two investigators (TMW, PD) searched the medical literature from PubMed 1946-, Embase 1947-, Cumulative Index for Nursing and Allied Health (CINAHL) 1937-, Cochrane Central Register of Controlled Trials (CENTRAL), Database of Abstracts of Reviews of Effects (DARE), Cochrane Database of Systematic Reviews, and clinicaltrials.gov. Standardized terms and keywords were combined in the search for the following concepts: oncology/cancer, people sixty and older, screening, falls and diagnosis (See Appendix 1 for full details of search strategy). All searches were completed in March 2014, and limited to English language using database supplied limits. All results were exported to EndNote. Duplicates were identified and removed. Inclusion criteria included manuscripts, abstracts or clinical trials examining falls in humans with cancer. Eligible studies included retrospective cohort studies, case-control studies, prospective cohort studies or clinical trials in which at least either all patients had cancer, or a diagnosis of cancer defined a subgroup, and falls were a primary or secondary outcome. Studies were excluded if they did not examine falls as an endpoint, did not include patients over age 60, or did not include patients with a diagnosis of cancer. Review articles were excluded. Two authors (TMW and PD) reviewed the titles and abstracts. Full manuscripts were obtained on a subset of articles and reviewed with the inclusion criteria. The references of selected relevant articles were hand-searched for any additional articles that met our inclusion criteria. No meta-analysis was planned a priori.
Two authors examined the eligible full manuscripts; data was extracted by author (PD) and double-checked by another (TMW). First author, year of publication, type of study, sample size, type of cancer included, type of cancer treatment (if specified), age of participants (mean or median, and standard deviation, if reported), and site of enrollment (inpatient or outpatient) or type of database were extracted and recorded in a Microsoft Excel database. Whether falls were assessed prospectively or retrospectively was recorded. The method of falls ascertainment or definition of falls used was recorded, if reported. The rate of falls and ascertainment period was recorded. In some cases, only the odds ratio for falls among patients with cancer relative to controls was reported, and this data was recorded. The rate of injurious falls was recorded, if reported.
Manuscripts were stratified into those that examined outpatient/community falls and those that examined inpatient falls. Studies that examined factors associated with or predictive of falls were identified. When an association between a predictor and falls was examined, the odds ratio for falls associated with each factor was recorded, if statistically significant. If the relationship was statistically significant but not reported as an odds ratio, then it was recorded as a qualitatively positive relationship.
In the outpatient falls strata, demographic information extracted included age, race and gender. Comorbidities included osteoporosis, arthritis, or overall comorbidity score. Functional measures included Eastern Cooperative Oncology Group (ECOG)(6) or Karnofsky (7) performance status, activities of daily living (ADLs), instrumental activities of daily living (IADLs), objective measures of physical performance, a prior history of falls, and use of an assistive device for walking. Psychosocial or cognitive factors included cognitive impairment, social support/marital status or depression. Measures of medication included the number of medications, or certain classes of medications, including antipsychotics, corticosteroids, benzodiazepines, and opiates. Factors associated with the cancer diagnosis or its treatment included pain, fatigue, anemia, androgen deprivation therapy, use of chemotherapy, cancer stage and the presence of brain metastases. Finally, other factors, including visual impairment, a positive screen on the Vulnerable Elders Survey-13(8) or nutritional risk were recorded.
In the inpatient falls strata, demographic information included age, race and gender. Comorbidities included cardiac disease, chronic kidney disease, chronic obstructive pulmonary disease or comorbidity scores. Functional measures included ECOG or Karnofsky performance status, ADLs, IADLs, measures of physical performance, prior history of falls, or use of an assistive device for walking. Psychosocial or cognitive factors recorded included cognitive impairment, delirium or depression. Medication factors included the number of medications, or certain classes of medications: antipsychotics, corticosteroids, benzodiazepines, and opiates. Factors associated with cancer or its treatment included pain, fatigue, anemia, chemotherapy, stage, brain metastases, and symptom score using the Edmonton Symptom Assessment Score. Other clinical factors (fever and blood pressure) were also recorded.
Quality Appraisal
We examined the quality of studies included in the review using the Newcastle-Ottawa Quality Assessment Scale for case-control and cohort studies (www.ohri.ca/programs/clinical_epidemiology/oxford.asp). Scores range from 0 to 9 stars based on criteria for selection, comparability and exposure assessment for case-control studies and selection, comparability and outcome assessment for cohort studies. Cross-sectional studies were appraised using a modification of the criteria for cohort studies (See Appendix 2 for details on modifications of the Newcastle-Ottawa scale applied for this study). Given that the outcome of falls is a potentially multiply-recurring outcome, it was assumed that the outcome of interest could have occurred prior to enrollment. Only cohort and case-control studies available in full manuscript form were subjected to quality appraisal using the Newcastle-Ottawa scale; abstracts, pilot studies, qualitative studies and ongoing trials were evaluated to the extent possible, but were not subjected to quality appraisal as the Newcastle-Ottawa scale was not designed for use in these studies.
Results
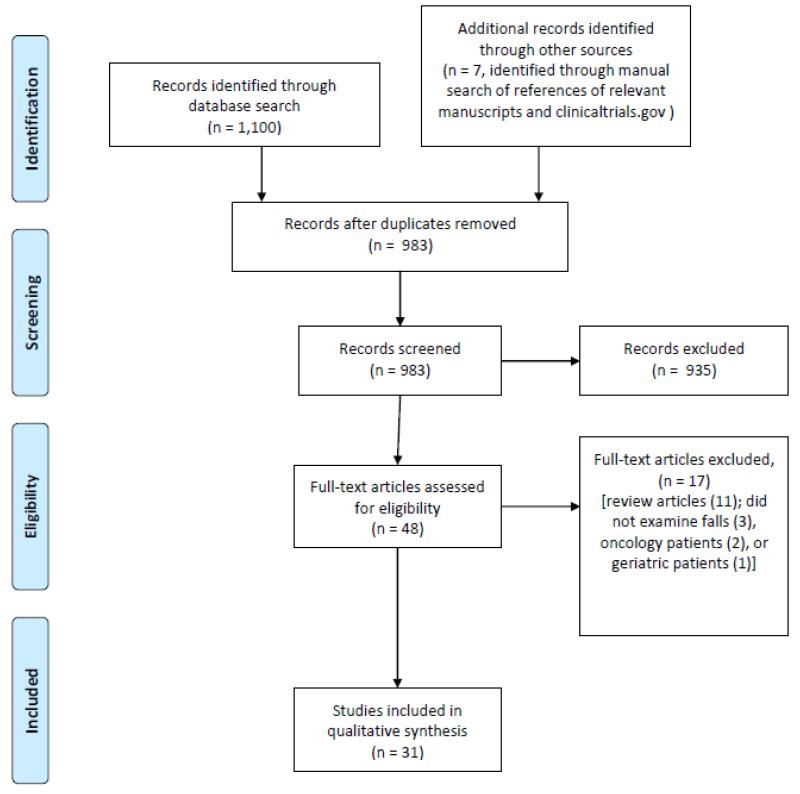
The initial search strategy identified 1,100 published articles. The authors also reviewed the references from selected articles to identify an additional 6 articles not located through the original search; 1 clinical trial.was identified on ClinicalTrials.gov. We used the automatic duplicate finder in EndNote and124 duplicates were identified and removed, for a total of 984 unique citations. Two authors (TMW, PD) reviewed the unique titles and abstracts to identify 41 potentially relevant articles, which were retrieved and the full manuscripts reviewed. These authors independently reviewed the articles for inclusion criteria. This resulted in a final list of 31 unduplicated studies (Figure 1).
Figure 1.
PRISMA flow diagram of phases of systematic review
The 31 studies were published in 19 unique journals (Table 1). Of note, the sample involved 26 teams of authors, with 141 different authors publishing evidence related to oncology falls in geriatric cancer patients. Funding was acknowledged in 14 of the studies by multiple sources including research grants, awards, and fellowships from the National Institute of Health, the National Cancer Institute, the Department of Health and Human Services, the Center for Disease Control, the Canadian Cancer Society, universities, and hospital foundations.
Table 1.
Characteristics of included studies and populations
| Author | Year | Type of Study |
Sample size | Type of cancer | Type of cancer treatment |
Age | Site of enrollment or source of database |
Falls assessment: retrospective or prospective |
How falls were assessed |
Fall rate (%) |
Injurious fall rate |
NOQAS Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bylow et al(15) | 2008 | Cohort | 50 (initial assessment) 40 (second assessment) |
Prostate | ADT | Mean 78 | Outpatient | Retrospective and prospective |
CGA falls screening |
20% in past 3 months |
NR | 4★ |
| Capone et al(23) |
2012 | Retrospectiv e case control |
288 | Hematology with or without bone marrow transplantation, solid tumor, brain tumor |
Any | Mean 60.9 (SD 13.7) |
Inpatient | Retrospective | Online event reporting tool completed by nurse managers |
3% | NR | 4★ |
| Flood et al (46) |
2006 | Retrospectiv e |
119 | Primary oncologic or hematologic diagnosis |
NR | Mean 74.1 | Inpatient | Retrospective | Medical data | 5% | NR | 4★ |
| Goodridge & Marr(24) |
2002 | Retrospectiv e |
357 | Any | NR | Mean 70.9 | Inpatient | Retrospective | Incident report forms |
27.5% | 43.9% | * |
| Hendrich et al(47) |
1995 | Retrospectiv e case control |
338 | NR | NR | NR | Inpatient | Retrospective | Incident reports/chart review |
OR 2.7 for cancer diagnosis |
NR | 7★ |
| Herndon et al(11) |
1997 | Population- based case- control |
1,158 | Any (except skin) |
NR | Range 65 and older |
Community | Retrospective | ICD9 CM codes for fall injuries |
OR 0.8 (0.5-1.2) for cancer patients relative to noncancer patients |
NR | 5★ |
| Hurria et al(31) |
2011 | Prospective cohort |
500 | Any | Chemotherap y |
Mean 73 (SD 6.2) |
Outpatient | Retrospective | Patient self- report |
18% in past 6 months |
NR | 6★ |
| Hussain et al(19) |
2010 | Prospective cohort |
260 | Prostate | ADT in one group, no ADT in one group |
Mean 68- 69 |
Outpatient | Retrospective | Patient self- report |
Baseline: 15% in past 12 months 12 month followup: 35% |
NR | 5★ |
| Kalsi et al(9) | 2013 | Cross- sectional |
417 | Urological, lung, breast, gynecological, hepatobiliary, and gastrointestinal malignancies |
NR | Mean 73.9 (SD 5.4) |
Outpatient | Retrospective | CGA postal questionnaire (CGA-GOLD), patient self- report |
13.3% | NR | * |
| Kelly et al(34) | 2003 | Case control | 11,390 | NR | NR | Mean 74.5 and 78.5 |
Administrative data |
Retrospective | Administrative data |
14% of fallers had cancer vs 12% of nonfallers; AOR 1.00 |
31.6 per 1,000 population per year |
6★ |
| Luce et al(48) | 2012 | Prospective | 211 | Any | NR | Mean 78 (SD 6) |
Inpatient/ outpatient |
Retrospective | CGA falls screening |
31% in past year |
29% | 3★ |
| Mohile et al(14) |
2011 | Retrospectiv e |
12,480 | Any | NR | Mean 76 | Medicare Current Benificiary Survey |
Retrospective | Self-report | 26.4%, AOR 1.17 |
NR | 6★ |
| O’Connell et al(27) |
2005 | Prospective cohort |
227 | NR | NR | Mean 67.7 (SD 13.8) |
Inpatient oncology or palliative care unit |
Prospective | Nurse report | 37% in 12 months prior to hospitaliza tion; 15% during hospitaliza tion |
NR | 4★ |
| O’Connell et al(43) |
2007 | Retrospectiv e and prospective case control |
Retrospectiv e: 377 Prospective: 34 |
NR | NR | Mean 73 (SD 15) |
Community or inpatient |
Retrospective and prospective |
FRAT | Cannot be determine d in case:contr ol study |
NR | 4★ |
| Overcash(17) | 2007 | Prospective cross- sectional (no follow-up period noted) |
165 | Any | Any | Mean 77.6 | Community | Prospective | AGS guidelines using the Kellogg International Work Group definition of falls |
21% | NR | 3★ |
| Overcash & Beckstead(20) |
2008 | Prospective cross- sectional (no follow-up period noted) |
352 (297 had cancer) |
Any (except skin) |
Chemotherap y or none |
Mean 78- 80 |
Outpatient | Retrospective | CGA falls screening |
29.5% in past year |
NR | 5★ |
| Overcash & Rivera(21) |
2008 | Prospective | 20 | Any | NR | Mean 75.5 | Outpatient | Retrospective | AGS guidelines, Kellogg International work group definition of falls, and patient self- report |
65% in past year, 79% in past 3 months, 60% since cancer diagnosis |
NR | 3★ |
| Overcash et al(49) |
2010 | Prospective qualitative (semi- structured interviews) |
20 | Any | Varied | Mean 76.4 | Community | Retrospective | Patient self- report |
100% | NR | * |
| Pautex(26) | 2008 | Retrospectiv e |
198 | Advanced cancer |
Varied | Mean 71 (SD 12.1) |
Inpatient palliative care |
Retrospective | Institutional incident report form |
18.2% | NR | 6★ |
| Pearse(25) | 2004 | Retrospectiv e and prospective |
Prospective: 102 |
NR | NR | Mean 67 (prospecti ve) |
Inpatient hospice | Retrospective | Review of accident forms |
22.5% | NR | 7★ |
| Potter et al(50) | 2012 | Pilot intervention |
38 patient-caregiver dyads |
NR | NR | Mean 65 | Inpatient | Retrospective and prospective |
Fall diaries | 40.9% in 3 months before interventio n; 18.2% in 4 months after intevention |
NR | * |
| Puts et al(16) | 2013 | Prospective cohort |
112 | Lung, breast, colorectal, lymphoma, myeloma |
Varied | Mean 74.2 (SD 6) |
Outpatient | Prospective | CGA falls screening |
19% in past 6 months |
NR | 7★ |
| Spoelstra et al(51) |
2010 | Retrospectiv e cross- sectional |
6,912 (911 with cancer) |
NR | NR | Range 65- 101 |
Community | Retrospective | MDS | 27.5% (overall sample) |
NR | 6★ |
| Spoelstra et al(12) |
2010 | Retrospectiv e cross- sectional |
7,448 total (967 with cancer) |
NR | NR | Range 65 and older |
Community | Retrospective | MDS: number of falls over past 6 months |
27.2% | NR | 5★ |
| Spoelstra et al(13) |
2013 | Retrospectiv e |
9,481 | NR | NR | Mean 77 | Outpatient | Retrospective | Patient self- report |
33% in those with cancer vs 30% in those without (p=0.01) OR 1.16 on MVA |
NR | 5★ |
| Steer et al(52) | 2012 | Cross- sectional |
155 | Any | NR | Mean 78 (range 70- 95) |
Outpatient | Retrospective | GA | 20% | NR | * |
| Stone et al(10) | 2012 | Prospective | 185 | Metastatic or locoregionally advanced cancer |
NR | Mean 68 (SD 12.6) |
Inpatient or outpatient |
Prospective | Patient self- report |
50.3% | 21.1% | 7★ |
| To et al(53) | 2010 | Cross- sectional |
200 | Gastrointestinal , lung, genitourinary, breast, other |
Varied | Mean 76.7 (range 70- 92) |
Outpatient | Retrospective | GA | 22% | NR | 3★ |
| Tofthagen et al(22) |
2012 | Prospective | 109 | Any | Taxane or Platinum chemotherapy |
Mean 58.4 (SD 11.8) |
Outpatient | Retrospective | CIPNAT | 19.3% since treatment |
NR | 4★ |
| Ward et al(18) | 2014 | Retrospectiv e |
65,311 | Breast, colon, lung, prostate |
Chemotherap y |
65 and older |
SEER-Medicare | Retrospective | ICD-9 CM codes related to fall injuries |
NR | 9.15 per 1000 person- months for patients receiving neurotoxic doublet |
7★ |
| Winters- Stone(54) |
Trial in progre ss |
Randomized trial |
429 | Stage I-IIIC cancer other than brain or spinal cord |
Completed chemotherapy <3 months prior |
Eligibility: age 50-75 years |
Outpatient | Prospective | Monthly self- report |
Trial in progress |
Trial in progress |
* |
NOQAS, Newcastle-Ottawa Quality Assessment Scale; ADT, Androgen Deprivation Therapy; CGA, Comprehensive Geriatric Assessment; NR, not reported; ICD-9 CM, International Classification of Diseases, Ninth Revision, Clinical Modification; FRAT, Fall Risk Assessment Tool; AGS, American Geriatrics Society; MDS, Minimum Data Set; GA, Geriatric Assessment; CIPNAT, Chemotherapy-Induced Peripheral Neuropathy Assessment Tool; SEER, Surveillance, Epidemiology, and End Results;
unscored
Risk and prevalence of falls in outpatients with cancer
Studies varied widely with regard to how falls were assessed. Most studies assessed falls retrospectively over various or unspecified time periods. The rate of falls ranged from 13% (time period unspecified) in a cross-sectional study of older adults undergoing a screening geriatric assessment (9) to 50.3% over 6 months in a prospective cohort of older adults with cancer enrolled in a palliative care program.(10) Most studies of older adults of cancer reported a rate of falls between 20-30% in time periods of 3-12 months (Table 1).
Several studies compared the risk of falls between patients with cancer and those without. Some found a greater risk of falls among older adults with cancer, while others did not. In a population based case-control study, Herndon et al demonstrated no difference in the risk of fall-related injuries among older adults with a self-reported history of cancer relative to those without a reported history of cancer [odds ratio (OR 0.8 [95% Confidence Intervals (CI) 0.5-1.2].(11) Similarly, in a cohort of low-income community-dwelling elders, a diagnosis of cancer was not a statistically significant predictor of falls.(12) Yet in another study, Spoelstra et al found that the rate of falls was 33% among those with cancer, versus 30% among those without, resulting in an odds ratio for falls of 1.16 (95% CI 1.01-1.33, p=0.03).(13) Mohile et al showed in a large population-based study that the rate of falls in those with a diagnosis of cancer was 26.4% versus 21.9% in those with no cancer [Adjusted OR 1.17 (95% CI 1.04-1.32)].(14) All of these studies were performed in cohorts of patients with a history of cancer in whom current treatment or cancer stage and status were not reported.
Factors associated with falls in patients with cancer (outpatients)
We examined factors associated with or predictive of falls in older adults with cancer (Table 2). Most of the studies examined cross-sectional associations between a retrospective report of falls and current clinical and treatment factors. A few prospectively evaluated falls.(10,15,16) No factors were consistently associated with falls across studies.
Table 2.
Factors associated with outpatient falls in older adults with cancer
| Study | Odds Ratio for Falls | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | Comorbidities | Function | Psychosocial/ Cognitive |
Medications | Cancer/Treatment Factors | Other | |||||||||||||||||||||||||
| Age | Race | Gender | Osteoporosis | Arthritis | Comorbidities | Neuropathy | Performance Status | ADL | IADL | Physical performance measures§ |
Prior falls | Use of assistive device for walking |
Cognitive Impairment | Social support | Depression | Number of medications |
Antipsychotics | Corticosteroids | Benzodiazepines | Opiates | Pain | Fatigue | Anemia | ADT duration | Chemotherapy | Cancer Stage | Brain metastases | Visual impairment | VES13 | Nutrition | |
| Bylow(15) | ○ | ○ | ○ | ○ | ○ | ■ | ○ | ○ | 4.7† | ■ | ○ | ○ | 7.1† | ■ | ■ | ○ | ■ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ■ | ○ | ■ | ○ | ○ | 5.4‡ | ■ |
| Overcash 2007(17) |
■ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | † * | † * | ○ | ○ | ○ | † * | ○ | † * | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Hussain(19) | ○ | ○ | ○ | ○ | 2.4‡ | ■ | ○ | ○ | ■ | ■ | ■ | 4.2‡ | ○ | ○ | 0.4‡ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ■ | ■ | ○ | ○ | ○ | ○ | ○ | ○ |
| Overcash 2008a(20) |
○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | 1.4† | ○ | ○ | ○ | ○ | 1.1† | ○ | 0.9† | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Overcash 2008b(20) |
○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | 3.4† | ○ | ○ | ○ | ○ | ■ | ○ | ■ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Puts(16) | ○ | ○ | ■ | ○ | ○ | ■ | ○ | ■ | ■ | ■ | ○ | ■ | ○ | ■ | ■ | ■ | ○ | ○ | ○ | ■ | ■ | ○ | ■ | ○ | ○ | ■ | ■ | ○ | ■ | ○ | ■ |
| Stone(10)** | ■ | ○ | ■ | ○ | ○ | ■ | ■ | ○ | ○ | ○ | ■ | 1.3‡ | ○ | ○ | ○ | ■ | ■ | ■ | ■ | 1.0/ mg‡ |
■ | 2.0‡ | ■ | ○ | ○ | ○ | ○ | ■ | ■ | ○ | ○ |
| Ward(18)*** | 1.7‡d | 0.5‡e 0.7‡f |
1.5‡g | 1.3‡ | ○ | 1.4‡h | ■ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | 1.3‡i | 1.6‡j | ○ | ○ | ○ | ○ |
| Spoelstra(13) | ○ | 0.8‡e | ■ | ○ | ○ | 1.1‡ | ○ | ○ | ■ | ○ | ○ | ○ | ○ | 1.5‡ | ■ | 1.3‡ | ○ | ○ | ○ | ■ | ○ | 1.4‡ | ○ | ○ | ○ | ○ | ■ | ○ | ■ | ○ | 1.6‡k |
| Overcash & Rivera(21) |
○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | AUC 0.85l |
○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Tofthagen(22) | ○ | ○ | ○ | ○ | ○ | ○ | 1.4‡m | ○ | ○ | ■ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | 1.3‡m | ■ | ○ | ○ | ○ | ○ | |
Impaired gait, AbnormalTimed Up and Go Test or grip strength
p<0.05 on univariate analysis
p<0.05 on multivariate analysis
Odds ratio not reported; relationship statistically significant as analyzed.
Hazard ratios reported
Hazard ratios for falls with injury
Not evaluated
■ Not significant
ADL, activities of daily living; IADL, instrumental activities of daily living; ADT, androgen deprivation therapy; VES13, Vulnerable Elders Survey-13;
Group with history of cancer, but no current cancer treatment
Group with cancer currently receiving treatment
for age <80 relative to younger patients
for black race relative to white race
for Asian race relative to white race
for female gender
for Charlson Comorbidity Index score of 2 or greater relative to 0
for neurotoxic doublet chemotherapy relative to non-neurotoxic chemotherapy
for Stage IV relative to Stage I
for weight loss relative to none
area under the curve of Timed Up and Go Test for association with falls within 1 year or 3 months
for loss of balance
per cycle of chemo
Several studies examined if demographic factors, such as age (10,17,18), race (13,18), and gender (10,13,16,18), were associated with falls. Of these studies, one study found that individuals over the age of 80 were more likely to experience falls with injuries than individuals younger than 80 [Odds Ratio (OR) 1.18 (95% Confidence Intervals 1.07-1.25) for age 70-74; OR 1.32 (95% CI 1.2-1.46) for age 75-79 and OR 1.71 (95% CI 1.54-1.89) for age 80 or older], (18). Two studies found that people of white race were significantly more likely to fall or experience injurious falls than people of black or Asian race [OR 0.76 (95% CI 0.61-0.96) for falls for black people relative to others; OR 0.54 (95% CI 0.46-0.64) for injurious falls for black race relative to white; OR 0.71 (95% CI 0.59-0.87) for injurious falls for Asian race relative to white].(13,18) One study showed that women had a significantly greater odds of injurious falls than men [OR 1.54 (95% CI 1.43-1.57)].(18)
A number of geriatric syndromes were among the factors associated with falls in the studies evaluated. Two studies (13,18) found that comorbidities were significantly associated with falls [OR 1.07 (95% CI 1.04-1.12) for any comorbidity versus none; OR 1.35 (95% CI 1.24-1.47) for risk of injurious falls in people with a Charlson Comorbidity score of 2 or more vs. none], while others did not.(10,15,16,19). Measures of functional status were significantly associated with falls, particularly scores on Activities of Daily Living (ADL), Instrumental Activities of Daily Living (IADL), physical performance measures, and prior falls. Dependence in ADLs was associated with between a 40% to nearly five-fold increased odds of falls.(15,17,20) Scores IADLs were significantly correlated with falls [Pearson product moment correlation coefficient −0.238, p<0.05].(17) The Timed Up and Go test significantly correlated with falls within 1 year in one study [Pearson product moment correlation coefficient 0.58, p=0.01].(21) Self-report of prior falls was associated with between a 30% and four-fold increased odds of falls.(10,19)
Psychosocial and cognitive issues including cognitive impairment, marital status, and depression were significantly associated with falls as well. Cognitive impairment, as measured by the MMSE or 5-minute recall, was associated with 12-53% greater odds of falls. (13,17,20) The availability of social support, evidenced by married marital status, was associated with a 60% lower odds of falls [OR 0.42 (95% CI 0.19-0.93)].(19) The score on the geriatric depression scale was significantly associated with falls [Pearson product moment correlation coefficient 0.116, p<0.05](17), while use of antidepressants was associated with a 29% increased risk of falls.(13) Although the use of certain medications such as antipsychotics (10), corticosteroids (10), and opiates (10,16) were not found to significantly predict falls in the community setting, benzodiazepine use was significantly associated with falls in a dose-dependent fashion [Hazard Ratio (HR) 1.05/mg daily diazepam dose equivalent (95% CI 1.01-1.09)].(10)
Cancer symptoms or treatment factors were examined for their associations with falls in a number of studies. Pain and chemotherapy type were significantly related to falls. Patient-report of daily pain was associated with a 44% greater odds of falls [OR 1.44 (95% CI 1.32-1.59)] in one study, and an 87% greater odd of falls in another [OR 1.87 (95% CI 1.03-3.4)].(10,13) Increasing numbers of cycles of neurotoxic chemotherapy were associated with greater risk of falls [OR 1.3/cycle (95% CI 1.01-1.75)] and neurotoxic doublets were associated with injurious falls [OR 1.28 (95% CI 1.12-1.45)]. (18,22) However, other symptoms and treatment factors, including fatigue (10,16), anemia (19), androgen deprivation therapy (ADT) duration (15,19), and brain metastases (10), were not significantly associated with falls. Visual impairment was not significantly related to falls in oncology populations.(10,13,16)
Hospital and inpatient hospice fall rate in patients with cancer
A number of studies examined falls in individuals with cancer while in an inpatient acute care hospital or inpatient hospice/palliative care setting. Studies varied widely with regards to how falls were assessed. Most studies assessed falls retrospectively during a patient’s hospital stay, although some studies assessed falls both prospectively and retrospectively. The rate of falls ranged from 3% in a retrospective case control study (average length of stay for fallers was 15 days) (23) to 27.5% in a in a retrospective study of patients in a palliative care unit (average length of stay for fallers was 46 days) (24). Most studies of older adults with cancer reported a rate of falls in the inpatient setting between 15-23% (see Table 1).
Several studies compared the length of hospital stay between fallers and non-fallers. Fallers tended to have longer hospital stays than non-fallers. In a case-control study, Capone et al demonstrated that the average length of stay for fallers was 15 days while the average stay for those that did not fall was 7 days.(23) Similarly, in a study by Pease, fallers were found to have an average stay of 23 days compared to non-fallers who had a mean stay of 19 days.(25) A retrospective study by Goodridge and Marr found that fallers had a mean stay of 46 days while those that did not fall had an average stay of 19 days.(24)
Factors associated with inpatient falls in patients with cancer
These studies of inpatient falls sought to identify factors associated with falls (Table 3). Several analyzed whether demographic factors such as age (24-26) or gender (24-26) were related to inpatient falls in an oncology population. In a retrospective study of inpatients by Goodridge and Marr, age and gender were significantly associated with falls: patients who fell were, on average, 3.5 years older than those who did not fall, and men were 70% more likely to fall (p=0.04).(24) None of the studies examined evaluated race as a predictor of inpatient falls.
Table 3.
Factors associated with inpatient falls in older adults with cancer
| Study | Odds Ratio for Falls | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | Comorbidities | Function | Psychosocial/ Cognitive |
Medications | Cancer/Treatment Factors | Other | ||||||||||||||||||||||||
| Age | Race | Gender | Cardiac disease | Chronic Kidney Disease |
COPD | Comorbidities | Performance Status | ADL | IADL | Physical performance measures§ |
Prior falls | Use of assistive device for walking |
Cognitive Impairment | Delirium | Depression | Number of medications |
Antipsychotics | Corticosteroids | Benzodiazepines | Opiates | Pain | Fatigue | Anemia | Chemotherapy | Metastases/Stage | Brain metastases | ESAS Score | Fever | Blood pressure | |
| Capone(23) | ○ | ○ | ○ | 1.8 | 2.7 | ○ | ○ | ○ | ○ | ○ | 11.6 | 9.5 | 11.3 | 10.5 | ○ | 2.8a | ○ | 4.9 | 2.8 | 2.2 | 3.3b | 0.09 | ○ | 2.0 | ○ | 4.8 | 7.5 | ○ | 7.2 | ○ |
| O’Connell 2007(43) |
○ | ○ | ○ | ○ | ○ | ○ | ○ | ■ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| O’Connell 2005(27) |
○ | ○ | ○ | ○ | ○ | ○ | ○ | † * | ○ | ○ | † * | ■ | ○ | † * | † * | ○ | ○ | ○ | ○ | ○ | ○ | ○ | † * | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Pearse(25) | ■ | ○ | ■ | ○ | ○ | ○ | ■ | ○ | ■ | ○ | ○ | ■ | ■ | 12.8‡ | ○ | ○ | ■ | ○ | ○ | ■ | ■ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | 0.96‡ c |
| Pautex(26) | ■ | ○ | ■ | ○ | ○ | 5.4 | ○ | ○ | ○ | ■ | ○ | ○ | ○ | ■ | † * | ■ | ○ | † * | ■ | ■ | ■ | ○ | ○ | ■ | ■ | ○ | ○ | ○ | ○ | ○ |
| Goodridge &Marr(24) |
† * | ○ | 1.7†d | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ■ e | ○ | ○ | ■ e | ○ | ■ e | ○ | ■ e | ○ | ○ | ○ | ○ | ○ | ○ | † * f | ○ | ○ |
Impaired gait or weak grip strength
p<0.05 on univariate analysis
p<0.05 on multivariate analysis
Not evaluated
Evaluated, and not significant
Odds ratio not reported; relationship statistically significant as analyzed.
COPD, chronic obstructive pulmonary disease; ADL, activities of daily living; IADL, instrumental activities of daily living; ESAS , Edmonton Symptom Assessment Scale
Antidepressant use
as part of summary drug score including antidepressants, anxiolytics, benzodiazepines, corticosteroids, and opiates.
per mmHg supine systolic blood pressure
males relative to females
comparison between those who fell once versus repeatedly
Patients who fell once had greater symptom scores than those who fell repeatedly
Geriatric domains, including comorbidities, functional status and physical function, medications, cognition and depression, were associated with inpatient falls. Specific comorbidities, including cardiac disease (40% prevalence in nonfallers vs 54% in fallers, p=0.019)(23), chronic kidney disease (5% prevalence in nonfallers versus 12% in fallers, p=0.03) (23), chronic obstructive pulmonary disease [Adjusted OR 5.42 (95% CI 1.16-25.3)](26), were significantly associated with falls. Use of an assistive device for walking was strongly associated with falls in one study [OR 11.34 (95% CI 2.52-50.94)].(23) Prior falls were also strongly associated with inpatient falls [OR 9.51 (95% CI 2.64-34.22)].(23) Measures of functional status using the Activities of Daily Living and Instrumental Activities of Daily Living scales were not significantly associated with inpatient falls.(25,26) Patients who fell had a higher mean score on the Eastern Cooperative Oncology Group (ECOG) performance status scale(6) with a mean score of 2.61 ± standard deviation (SD) 0.78 versus 1.53 + SD 1.19 among those who did not experience an inpatient fall.(27) Physical performance measures were consistently associated with inpatient falls(23,27); in one study, patients with poor impaired gait had an 11-fold greater risk of falls than those with normal gait.
Cognitive impairment was strongly associated with falls in three of four studies which evaluated the association, with ten- to twelve-fold greater odds of falls in patients with cognitive impairment or impaired orientation.(23,25-27) One study showed that antidepressant use was associated with falls [OR 2.85 (95% CI 1.42-5.73)]. (23) Delirium was associated with falls in both studies in which it was examined [Crude OR 2.24 (95% CI 1.08-4.64); Adjusted OR 2.25 (95% CI 0.98-5.17)].(26,27) The number of medications taken was not significantly related to falls.(23) Certain medications were noted to be significantly associated with falls, including antipsychotics [Adjusted OR 1.94 (95% CI 1.06-6.54)] (26), corticosteroids [OR 2.85 (95% CI 1.65-4.9] (23), benzodiazepines [OR 2.15 (95% CI 1.09-4.23)] (23), and opiates.(23)
Factors related to cancer stage and symptoms were examined. Interestingly, pain was protective against inpatient falls in one study [OR 0.09 (95% CI 0.05-0.71)].(23) Self-reported fatigue was associated with greater likelihood of falls.(27) Anemia requiring a blood transfusion was significantly associated with falls [OR 2.36 (95% CI 1.25-4.46)].(23) The presence of any metastases was associated with a significantly greater risk of falls [OR 4.76 (95% CI 2.78-8.17)], as was the presence of brain or central nervous system metastases [OR 7.52 (95% CI 2.76-20.46)].(23) Patients who fell only once reported greater symptom burden on the Edmonton Symptom Assessment Scale (ESAS) than those who fell repeatedly, suggesting that patients in less distress, with consequently increased activity, were the ones who fell more frequently.(24) The presence of fever [OR 7.19 (95% CI 2.06 - 25.11)] and lower blood pressure [OR 0.96/mmHg (95% CI 0.93-0.99)] were also significantly associated with inpatient falls.(23,25)
Discussion
By 2020, falls will cost the healthcare system nearly $55 billion.(28) Falls are associated with injuries, including head trauma, fractures, contusions, dislocations and other internal injuries. Further, they are associated with fear of falling, loss of confidence, going out less often,(29) functional decline,(30) and nursing home placement.(3) Among older adults with cancer, prior falls are associated with increased risk for chemotherapy toxicity and death.(31,32) Identifying older adults at risk for falls is important since interventions, including exercise, home safety modifications and medication adjustments, can decrease the rate of falls in community-dwelling older adults. (33)
In this systematic review, we identified 31 unique studies examining falls in older adults with cancer. Our review suggests that falls in older adults with cancer may be more common than among community-dwelling older adults without a diagnosis of cancer.(13,14) The rate of falls reported varied widely with the population studied, with the method of falls assessment and with duration of follow-up. This variability in methods undoubtedly contributed to inconsistency in conclusions about whether or not falls are more common in older adults with cancer. The two studies supporting an increased risk of falls were large cohort studies, with over 20,000 participants combined and with falls ascertained by participant report. They reported remarkably similar adjusted odds ratios of 1.16-1.17.(13,14) Conversely, a large study of over 11,000 patients failed to find an increased risk of falls in patients with cancer when falls were ascertained using administrative data.(34) Thus, the method of falls ascertainment may impact the results.
We identified that some factors established as risk factors in the general population were also associated with falls in oncology populations. For example, white race is associated with a greater risk for falls in both the general population and in oncology populations.(13,30,35) Dependence in ADLs is associated with greater risk for falls in community-dwelling individuals(36,37), and it retains its association with falls in oncology populations.(15,17,20)
Some risk factors established in the general population, however, were not found to be associated with falls in oncology populations. While this may be related to methods of ascertaining falls (see discussion below) or small sample size, this raises the question of whether falls in older adults with cancer require different methods of risk stratification than the general population. Increasing age is associated with increased risk for falls in the general population (36-38), but was found not to be associated with falls in two studies of patients with cancer.(10,17) It may be that cancer treatment accelerates frailty such that chronological age is no longer an important predictor of falls in an oncology population. Ward et al, however, did find an association between age and injurious falls in older adults with cancer using the SEER-Medicare database.(18) Measures of physical performance failed to predict falls in 2 of 3 studies of patients with cancer.(10,19,21) In general populations, measures of physical performance, such as the Timed Up and Go (TUG) Test, are very sensitive and specific for determining which individuals are at greater risk for falls. However, Stone et al found no significant association between TUG time and prospectively ascertained falls on multivariate analysis. It may be that a single baseline assessment of physical performance fails to predict falls because the health status of vulnerable older adults with cancer can change rapidly. For example, among older adults, nearly one in five (16.7%) develop new dependence in daily activities between the first and second cycle of chemotherapy, demonstrating that there can be rapid changes in functional status, which are not predicted by baseline TUG.(39)
Finally, we found that there are risk factors for falls that are unique to a population of patients with cancer. These include certain chemotherapeutic agents (18,22) and advanced cancer stage (18). In a prospective cohort study, Stone et al found the presence of brain metastases to be associated with falls on univariate analysis, though not multivariate analysis.(10) Among inpatients in a retrospective cohort study, the presence of brain metastases and primary brain tumors were associated with falls, after controlling for other established risk factors such as impaired gait.(23) Thus, accurately identifying older adults with cancer at risk for falls will require examination of factors unique to a population with cancer, such as cancer stage and treatment.
In our study, we stratified the studies by location of falls. Inpatient and outpatient falls have different contributing environmental factors and risk factors. Factors associated with falls in the inpatient setting may not be associated with falls in the outpatient setting.(40) Inpatient fall outcomes are often reported as falls per person-days rather than the overall risk or rate. Thus, the literature on inpatient versus outpatient falls is best examined separately.
There are several limitations to our study. Most of the studies ascertained falls retrospectively and did not report using an established definition of falls. The Prevention of Falls Europe and Outcomes Consensus Group (PROFANE) performed a systematic review of definitions of falls and methods of falls ascertainment.(41) The consensus definition of falls is “an unexpected event in which the participant comes to rest on the ground, floor, or lower level,” and the preferred wording for questions about falls is “have you had any fall, including a slip or a trip in which you lost your balance and landed on the floor or ground or lower level?”(42) PROFANE also advises that falls should be ascertained prospectively via daily recording. Only a few studies included in our systematic review utilized prospective ascertainment of falls(10,15,17,27,43) or standard definitions of falls.(17,21) Retrospective assessment of falls will be subject to recall bias. Overcash et al. demonstrated bias in retrospective recall of falls: some of the same participants who reported falls in the prior 3 months reported no falls in the prior year.(21) Underreporting of falls may have resulted in lower estimates of fall rates in the studies in this systematic review. The highest outpatient fall rate was seen in the prospective cohort study by Stone et al. This study, with prospective ascertainment of falls using weekly interviews, demonstrated a fall rate of 50% in 6-months of follow. (10) While this study specifically enrolled a vulnerable population, its findings also underscore the necessity of prospective ascertainment of falls.
Patients with cancer often receive much of their healthcare in the oncology clinic, particularly while receiving treatment, creating the imperative that this common problem be addressed in the oncology setting. Given financial constraints and time pressures, risk screening for falls in oncology must be unobtrusive and streamlined.(44,45) Studies of falls in oncology should employ definitions and methodologies that have been established by consensus in falls research in the general population of older adults.(41) Further, risk assessment may need to be ongoing in older adults with cancer; in a prospective cohort of older adults receiving chemotherapy, one in five of older adults developed new dependence in their activities of daily living between their first and second cycles of chemotherapy.(39) Given that ADL dependence is associated with falls in several studies of older adults with cancer,(15,17,20) nearly one in five older adults with cancer will develop a new risk factor for falls subsequent to starting chemotherapy. Thus, the fall risk in an older adult with cancer is unlikely to be static and may need to be assessed on an ongoing basis to identify those who may benefit from interventions to reduce the risk of falls.(33) An intervention study that screens potential participants for risk at a single time point may miss a significant number of patients who develop risk factors over their disease and treatment course. Future intervention studies aiming to prevent falls in older adults with cancer may require adaptive trial designs that incorporate this dynamic risk assessment into enrollment and stratification. Prospective study of an individual patient’s risk factors over time is necessary to confirm the utility of ongoing risk assessment.
In conclusion, falls in older adults with cancer may be more common than in the general population of older adults, with a 16-17% increased risk of falls. With the aging of the population and the increasing number of cancer survivors, we can anticipate growing numbers of older adults with a diagnosis of cancer suffering falls and at risk for fall-related injuries, which are potentially preventable. Identifying older adults with cancer at risk for falls may require considering both risk factors established in the general population, such as ADL dependence, and risk factors unique to an oncology population, such as certain chemotherapeutic agents and advanced cancer stage. By addressing these risk factors and factoring in the rapidity with which older adults with cancer experience changes in health status due to treatment or the disease itself, we can hope to intervene appropriately and prevent falls in these vulnerable individuals. Clinicians caring for older adults should be aware of their patients’ risk for falls and familiar with resources such as physical therapy or home safety evaluation/modification, which can reduce the risk and rate of falls. Future study is needed to determine what is the best method for screening for falls risk in older adults with cancer, and to determine whether interventions are effective in reducing the risk of falls.
Supplementary Material
Acknowledgements
Dr. Wildes’ research is supported by Grant Number 1K12CA167540 through the National Cancer Institute (NCI) at the National Institutes of Health (NIH) and Grant Number UL1 TR000448 through the Clinical and Translational Science Award (CTSA) program of the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCI, NCATS or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.CDC Fatalities and Injuries from Falls Among Older Adults -- United States, 1993-2003 and 2001-2005. Morbidity and Mortality Weekly Report. 2006;55(45):1221–4. [PubMed] [Google Scholar]
- 2.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA: The Journal of the American Medical Association. 2007;297(1):77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 4.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of Cancer Incidence in the United States: Burdens Upon an Aging, Changing Nation. Journal of Clinical Oncology. 2009;27(17):2758–65. doi: 10.1200/JCO.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- 5.Hurria A, Naylor M, Cohen HJ. Improving the quality of cancer care in an aging population: recommendations from an IOM report. JAMA: The Journal of the American Medical Association. 2013;310(17):1795–6. doi: 10.1001/jama.2013.280416. [DOI] [PubMed] [Google Scholar]
- 6.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. American Journal of Clinical Oncology. 1982;5(6):649–55. [PubMed] [Google Scholar]
- 7.Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. Journal of Clinical Oncology. 1984;2(3):187–93. doi: 10.1200/JCO.1984.2.3.187. [DOI] [PubMed] [Google Scholar]
- 8.Saliba D, Elliott M, Rubenstein LZ, Solomon DH, Young RT, Kamberg CJ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. Journal of the American Geriatrics Society. 2001;49(12):1691–9. doi: 10.1046/j.1532-5415.2001.49281.x. [DOI] [PubMed] [Google Scholar]
- 9.Kalsi T, Babic-Illman G. Feasibility, utility of comprehensive geriatric assessment screening via postal questionnaire (CGA-GOLD) in older people with cancer. European Geriatric Medicine. 2013;4:P250. doi: 10.1111/ecc.12509. [DOI] [PubMed] [Google Scholar]
- 10.Stone CA, Lawlor PG, Savva GM, Bennett K, Kenny RA. Prospective study of falls and risk factors for falls in adults with advanced cancer. Journal of Clinical Oncology. 2012;30(17):2128–33. doi: 10.1200/JCO.2011.40.7791. [DOI] [PubMed] [Google Scholar]
- 11.Herndon JG, Helmick CG, Sattin RW, Stevens JA, DeVito C, Wingo PA. Chronic medical conditions and risk of fall injury events at home in older adults. Journal of the American Geriatrics Society. 1997;45(6):739–43. doi: 10.1111/j.1532-5415.1997.tb01480.x. [DOI] [PubMed] [Google Scholar]
- 12.Spoelstra S, Given B, Eye von A, Given C. Falls in the community-dwelling elderly with a history of cancer. Cancer Nurs. 2010;33(2):149–55. doi: 10.1097/NCC.0b013e3181bbbe8a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spoelstra SL, Given BA, Schutte DL, Sikorskii A, You M, Given CW. Do older adults with cancer fall more often? A comparative analysis of falls in those with and without cancer. Oncol Nurs Forum. 2013;40(2):E69–78. doi: 10.1188/13.ONF.E69-E78. [DOI] [PubMed] [Google Scholar]
- 14.Mohile SG, Fan L, Reeve E, Jean-Pierre P, Mustian K, Peppone L, et al. Association of cancer with geriatric syndromes in older Medicare beneficiaries. J Clin Oncol. 2011;29(11):1458–64. doi: 10.1200/JCO.2010.31.6695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bylow K, Dale W, Mustian K, stadler WM, Rodin M, Hall W, et al. Falls and Physical Performance Deficits in Older Patients With Prostate Cancer Undergoing Androgen Deprivation Therapy. Urology. 2008;72(2):422–7. doi: 10.1016/j.urology.2008.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puts MTE, Monette J, Girre V, Wolfson C, Monette M, Batist G, et al. The fall rate of older community-dwelling cancer patients. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2013;21(3):775–83. doi: 10.1007/s00520-012-1579-4. [DOI] [PubMed] [Google Scholar]
- 17.Overcash J. Prediction of falls in older adults with cancer: a preliminary study. Oncol Nurs Forum. 2007;34(2):341–6. doi: 10.1188/07.ONF.341-346. [DOI] [PubMed] [Google Scholar]
- 18.Ward PR, Wong MD, Moore R, Naeim A. Fall-related injuries in elderly cancer patients treated with neurotoxic chemotherapy: a retrospective cohort study. Journal of Geriatric oncology. 2014;5(1):57–64. doi: 10.1016/j.jgo.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Hussain S, Breunis H, Timilshina N, Alibhai SM. Falls in men on androgen deprivation therapy for prostate cancer. Journal of Geriatric Oncology. 2010;1(1):32–9. doi: 10.1016/j.critrevonc.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Overcash JA, Beckstead J. Predicting falls in older patients using components of a comprehensive geriatric assessment. Clin J Oncol Nurs. 2008;12(6):941–9. doi: 10.1188/08.CJON.941-949. [DOI] [PubMed] [Google Scholar]
- 21.Overcash JA, Rivera HR. Physical performance evaluation of older cancer patients: a preliminary study. Critical Reviews in Oncology / Hematology. 2008;68(3):233–41. doi: 10.1016/j.critrevonc.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Tofthagen C, Overcash J, Kip K. Falls in persons with chemotherapy-induced peripheral neuropathy. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2012;20(3):583–9. doi: 10.1007/s00520-011-1127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Capone LJ, Albert NM, Bena JF, Tang AS. Predictors of a fall event in hospitalized patients with cancer. Oncol Nurs Forum. 2012;39(5):E407–15. doi: 10.1188/12.ONF.E407-E415. [DOI] [PubMed] [Google Scholar]
- 24.Goodridge D, Marr H. Factors associated with falls in an inpatient palliative care unit: an exploratory study. Int J Palliat Nurs. 2002;8(11):548–56. doi: 10.12968/ijpn.2002.8.11.10897. [DOI] [PubMed] [Google Scholar]
- 25.Pearse H, Nicholson L, Bennett M. Falls in hospices: a cancer network observational study of fall rates and risk factors. Palliat Med. 2004;18(5):478–81. doi: 10.1191/0269216304pm903oa. [DOI] [PubMed] [Google Scholar]
- 26.Pautex S, Herrmann FR, Zulian GB. Factors associated with falls in patients with cancer hospitalized for palliative care. J Palliat Med. 2008;11(6):878–84. doi: 10.1089/jpm.2007.0241. [DOI] [PubMed] [Google Scholar]
- 27.O’Connell B, Cockayne M, Wellman D, Baker L. Fall risk factors and the nature of falls in inpatient oncology and palliative care settings. Contemp Nurse. 2005;18(3):247–57. doi: 10.5172/conu.18.3.247. [DOI] [PubMed] [Google Scholar]
- 28.Englander F, Hodson TJ, Terregrossa RA. Economic dimensions of slip and fall injuries. J Forensic Sci. 1996;41(5):733–46. [PubMed] [Google Scholar]
- 29.Collerton J, Kingston A, Bond J, Davies K, Eccles MP, Jagger C, et al. The personal and health service impact of falls in 85 year olds: cross-sectional findings from the Newcastle 85+ cohort study. PLoS ONE. 2012;7(3):e33078. doi: 10.1371/journal.pone.0033078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. Journal of the American Geriatrics Society. 2002;50(8):1329–35. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 31.Hurria A, Togawa K, Mohile SG, Owusu C, Klepin HD, Gross CP, et al. Predicting Chemotherapy Toxicity in Older Adults With Cancer: A Prospective Multicenter Study. Journal of Clinical Oncology. 2011;29(25):3457–65. doi: 10.1200/JCO.2011.34.7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wildes TM, Ruwe AP, Fournier C, Gao F, Carson KR, Piccirillo JF, et al. Geriatric assessment is associated with completion of chemotherapy, toxicity, and survival in older adults with cancer. Journal of Geriatric oncology. 2013;4(3):227–34. doi: 10.1016/j.jgo.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kelly KD, Pickett W, Yiannakoulias N, Rowe BH, Schopflocher DP, Svenson L, et al. Medication use and falls in community-dwelling older persons. Age and Ageing. 2003;32(5):503–9. doi: 10.1093/ageing/afg081. [DOI] [PubMed] [Google Scholar]
- 35.Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther. 2009;89(4):324–32. doi: 10.2522/ptj.20070107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cesari M, Landi F, Torre S, Onder G, Lattanzio F, Bernabei R, Oxford University Press Prevalence and risk factors for falls in an older community-dwelling population. J Gerontol A Biol Sci Med Sci. 2002;57(11):M722–6. doi: 10.1093/gerona/57.11.m722. [DOI] [PubMed] [Google Scholar]
- 37.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 38.Rossat A, Fantino B, Nitenberg C, Annweiler C, Poujol L, Herrmann FR, et al. Risk factors for falling in community-dwelling older adults: which of them are associated with the recurrence of falls? J Nutr Health Aging. 2010;14(9):787–91. doi: 10.1007/s12603-010-0089-7. [DOI] [PubMed] [Google Scholar]
- 39.Hoppe S, Rainfray M, Fonck M, Hoppenreys L, Blanc J-F, Ceccaldi J, et al. Functional decline in older patients with cancer receiving first-line chemotherapy. Journal of Clinical Oncology. 2013;31(31):3877–82. doi: 10.1200/JCO.2012.47.7430. [DOI] [PubMed] [Google Scholar]
- 40.Morrison G, Lee H-L, Kuys SS, Clarke J, Bew P, Haines TP. Changes in falls risk factors for geriatric diagnostic groups across inpatient, outpatient and domiciliary rehabilitation settings. Disabil Rehabil. 2011;33(11):900–7. doi: 10.3109/09638288.2010.514019. [DOI] [PubMed] [Google Scholar]
- 41.Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C, PROFANE-Group Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age and Ageing. 2006;35(1):5–10. doi: 10.1093/ageing/afi218. [DOI] [PubMed] [Google Scholar]
- 42.Lamb SE, Jørstad-Stein EC, Hauer K, Becker C. Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. Journal of the American Geriatrics Society. 2005;53(9):1618–22. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 43.O’Connell BO, Baker L, Gaskin CJ, Hawkins MT. Risk items associated with patient falls in oncology and medical settings. J Nurs Care Qual. 2007;22(2):130–7. doi: 10.1097/01.NCQ.0000263102.06311.a9. [DOI] [PubMed] [Google Scholar]
- 44.Balogh EP, Ganz PA, Murphy SB, Nass SJ, Ferrell BR, Stovall E. Patient-centered cancer treatment planning: improving the quality of oncology care. Summary of an Institute of Medicine workshop. Oncologist. 2011;16(12):1800–5. doi: 10.1634/theoncologist.2011-0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sifer-Rivière L, Girre V, Gisselbrecht M, Saint-Jean O. Physicians’ perceptions of cancer care for elderly patients: A qualitative sociological study based on a pilot geriatric oncology program. Critical Reviews in Oncology / Hematology. 2010;75(1):58–69. doi: 10.1016/j.critrevonc.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 46.Flood KL, Carroll MB, Le CV, Ball L, Esker DA, Carr DB. Geriatric syndromes in elderly patients admitted to an oncology-acute care for elders unit. Journal of Clinical Oncology. 2006;24(15):2298–303. doi: 10.1200/JCO.2005.02.8514. [DOI] [PubMed] [Google Scholar]
- 47.Hendrich A, Nyhuis A, Kippenbrock T, Soja ME. Hospital falls: development of a predictive model for clinical practice. Appl Nurs Res. 1995;8(3):129–39. doi: 10.1016/s0897-1897(95)80592-3. [DOI] [PubMed] [Google Scholar]
- 48.Luce S, De Breucker S, Van Gossum A, Demols A, Mekinda Z, Ena G, et al. How to identify older patients with cancer who should benefit from comprehensive geriatric assessment? Journal of Geriatric Oncology. 2012;3(4):351–8. [Google Scholar]
- 49.Overcash JA, Rivera HR, Van Schaick J. An analysis of falls experienced by older adult patients diagnosed with cancer. Oncol Nurs Forum. 2010;37(5):573–80. doi: 10.1188/10.ONF.573-580. [DOI] [PubMed] [Google Scholar]
- 50.Potter P, Olsen S, Kuhrik M, Kuhrik N, Huntley LR. A DVD program on fall prevention skills training for cancer family caregivers. J Cancer Educ. 2012;27(1):83–90. doi: 10.1007/s13187-011-0283-2. [DOI] [PubMed] [Google Scholar]
- 51.Spoelstra S, Given B, Eye von A, Given C. Fall risk in community-dwelling elderly cancer survivors: a predictive model for gerontological nurses. J Gerontol Nurs. 2010;36(2):52–60. doi: 10.3928/00989134-20100108-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Steer C, O’Connor J, Underhill C, Donnelly J, Myers R, Eek R, et al. Care coordination in the older adult with cancer (CCOAC)- a pilot study of supportive care screening and intervention in an Australian regional oncology practice. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2012;S111:466. [Google Scholar]
- 53.To T, Okera M, Prouse J, Prowse RJ, Singhal N. Infancy of an Australian geriatric oncology program—characteristics of the first 200 patients. Journal of Geriatric Oncology. 2010;1(2):81–6. [Google Scholar]
- 54.Winterstone KM, Li F, Horak F, Luoh S-W, Bennett JA, Nail L, et al. Comparison of tai chi vs. strength training for fall prevention among female cancer survivors: study protocol for the GET FIT trial. BMC Cancer. BioMed Central Ltd. 2012;12(1):577. doi: 10.1186/1471-2407-12-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.