Abstract
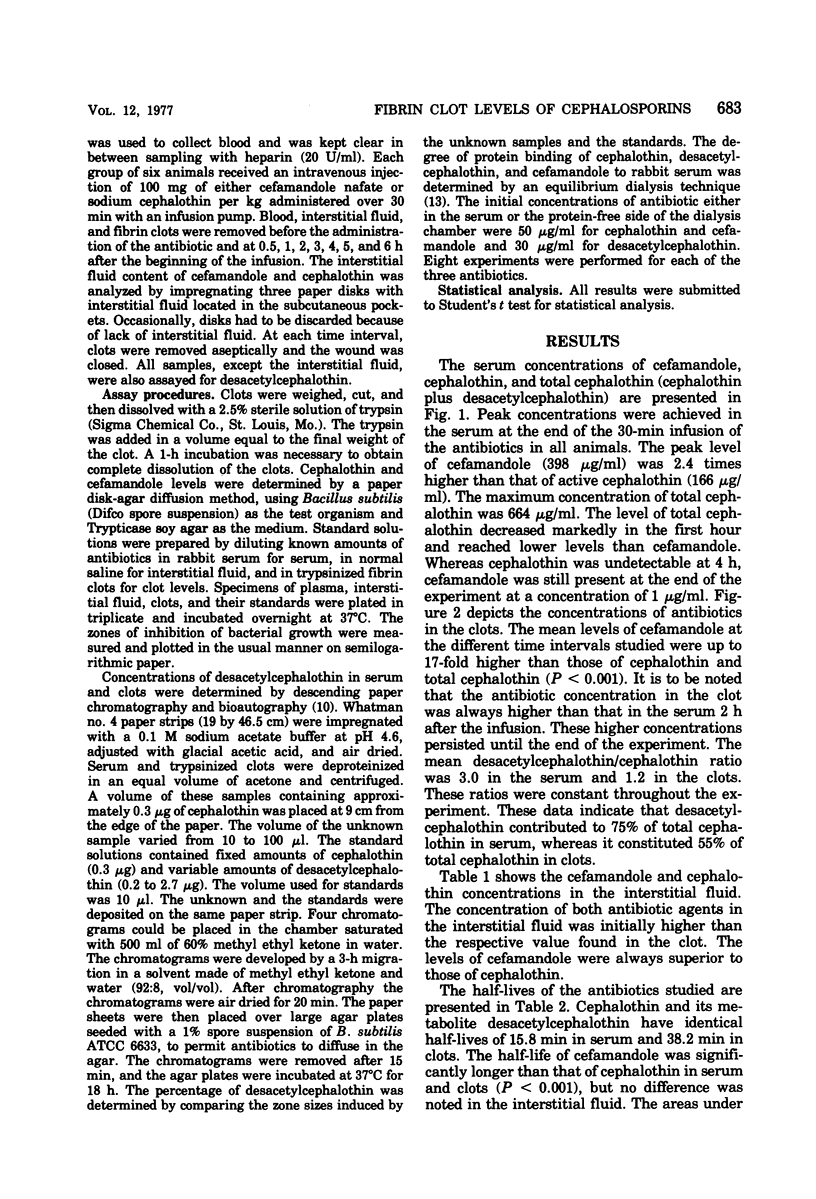
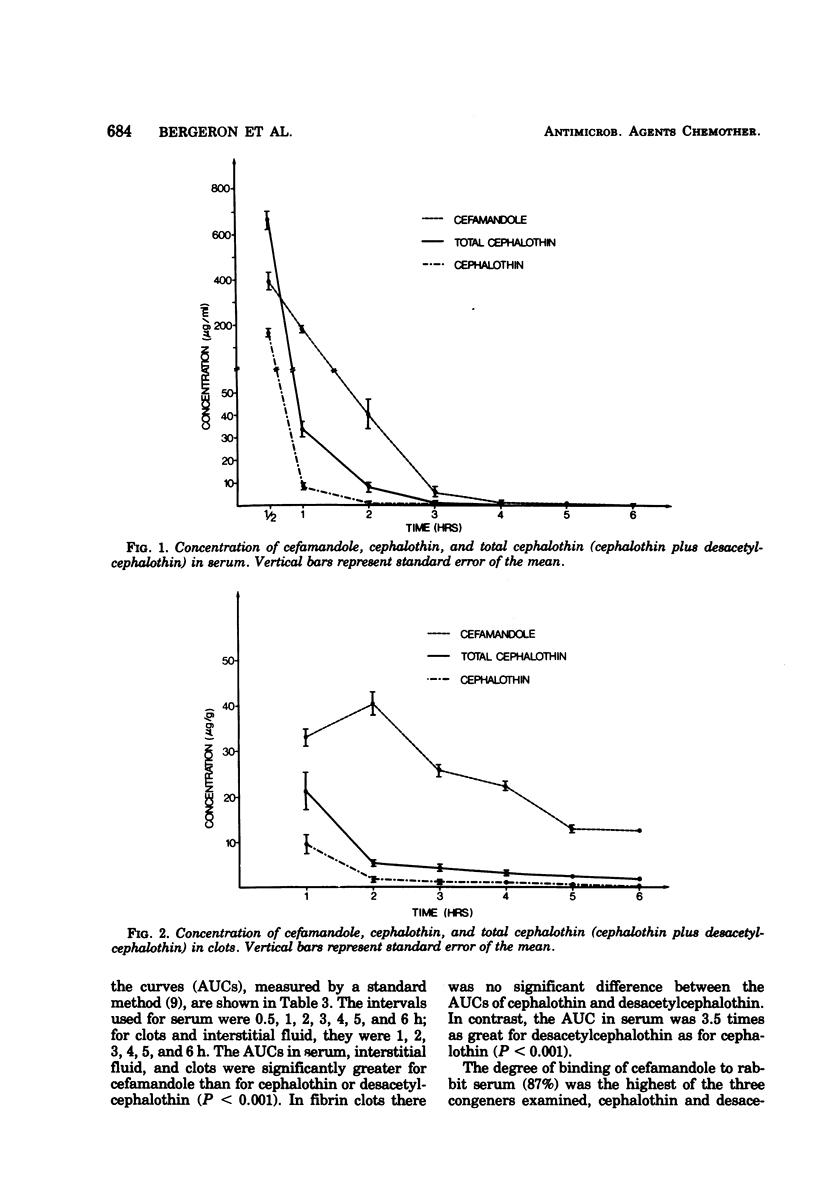
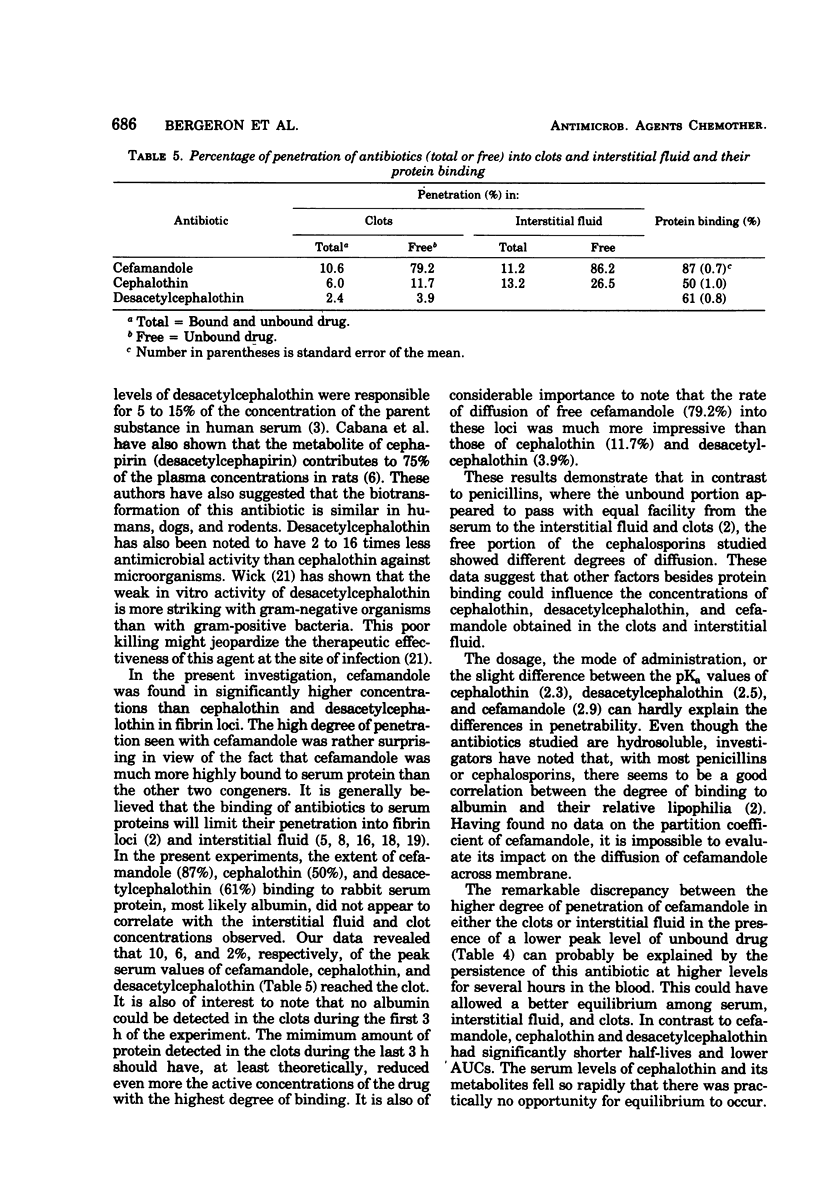
The conversion of cephalothin into a less active metabolite (desacetylcephalothin) might influence its distribution in tissues. An experimental rabbit model devised to determine concentrations of antibiotics in subcutaneous fibrin clots was used in this study. Groups of five to six animals received 100-mg/kg intravenous injections of either cefamandole or cephalothin. One hour after the injection, the concentration of cefamandole in serum was 20 times higher than that of cephalothin. Whereas cephalothin was undetectable at 4 h, cefamandole was still detectable at the end of the experiment. The half-lives of cephalothin and cefamandole in serum were 16 and 27 min, respectively. The concentration of cefamandole found in fibrin clots was severalfold higher than that of cephalothin. The half-life of cefamandole in clots (81 min) was superior to that of cephalothin (38 min). Although concentrations of both antibiotics were higher in serum than in clots at 1 h, the concentrations of these drugs in the clots persisted at higher levels throughout the next 5 h of the experiment. The extent of binding of cefamandole (87%) to rabbit serum was greater than that of cephalothin (50%). At least 55% of cephalothin was metabolized in vivo into its less active metabolite desacetylcephalothin. This metabolite was found in higher proportion in the serum (75%) than in the clots (55%). Whereas only 12% of the free (unbound) cephalothin reached the clots, 78% of the free cefamandole was found in the clots. This lower level of penetration of unbound cephalothin might be explained by the short half-life of this antibiotic, not permitting equilibrium to occur.
Full text
PDF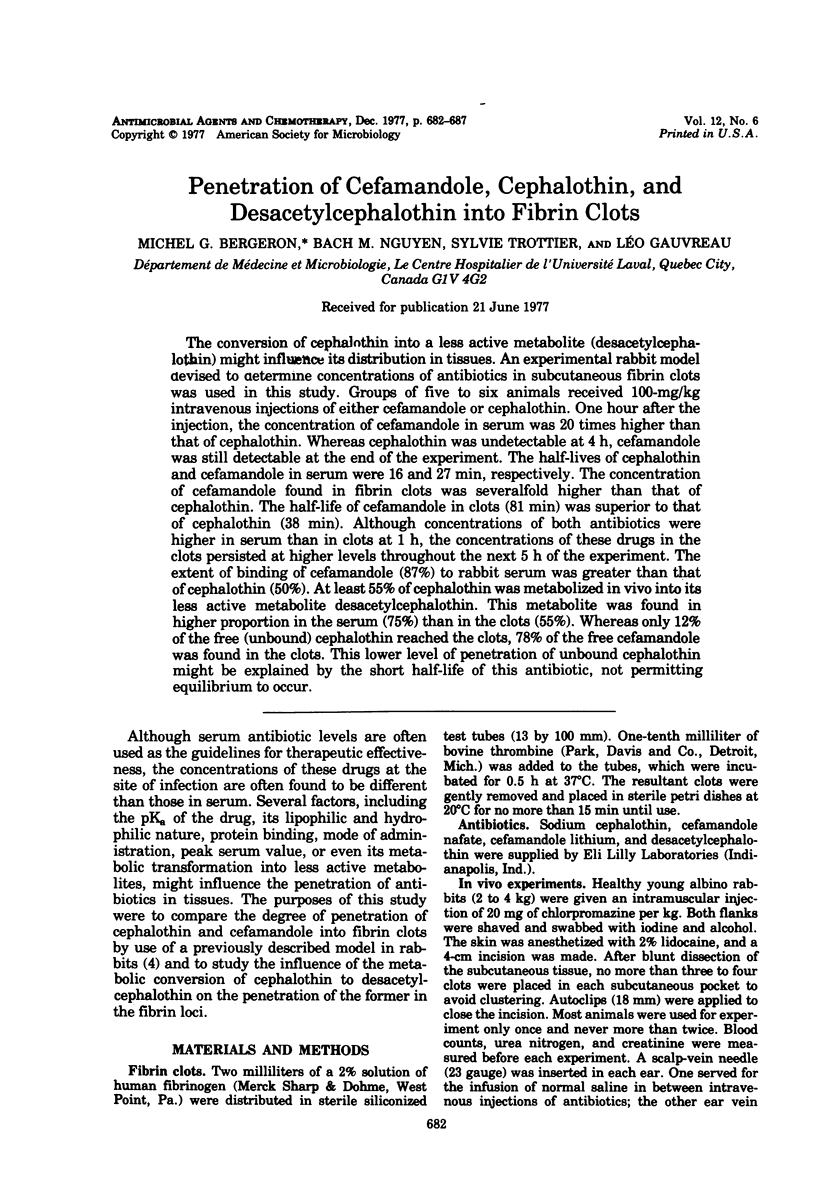
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BROWN D. M. TISSUE DISTRIBUTION OF PENICILLINS. Postgrad Med J. 1964 Dec;40:SUPPL–SUPPL:36. doi: 10.1136/pgmj.40.suppl.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barza M., Brusch J., Bergeron M. G., Weinstein L. Penetration of antibiotics into fibrin loci in vivo. 3. Intermittent vs. continuous infusion and the effect of probenecid. J Infect Dis. 1974 Jan;129(1):73–78. doi: 10.1093/infdis/129.1.73. [DOI] [PubMed] [Google Scholar]
- Barza M., Melethil S., Berger S., Ernst E. C. Comparative pharmacokinetics of cefamandole, cephapirin, and cephalothin in healthy subjects and effect of repeated dosing. Antimicrob Agents Chemother. 1976 Sep;10(3):421–425. doi: 10.1128/aac.10.3.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barza M., Samuelson T., Weinstein L. Penetration of antibiotics into fibrin loci in vivo. II. Comparison of nine antibiotics: effect of dose and degree of protein binding. J Infect Dis. 1974 Jan;129(1):66–72. doi: 10.1093/infdis/129.1.66. [DOI] [PubMed] [Google Scholar]
- Barza M., Weinstein L. Penetration of antibiotics into fibrin loci in vivo. I. Comparison of penetration of ampicillin into fibrin clots, abscesses, and "interstitial fluid". J Infect Dis. 1974 Jan;129(1):59–65. doi: 10.1093/infdis/129.1.59. [DOI] [PubMed] [Google Scholar]
- Cabana B. E., van Harken D. R., Hottendorf G. H. Comparative pharmacokinetics and metabolism of cephapirin in laboratory animals and humans. Antimicrob Agents Chemother. 1976 Aug;10(2):307–317. doi: 10.1128/aac.10.2.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher L. S., Chow A. W., Yoshikawa T. T., Guze L. B. Cephalothin and cephaloridine therapy for bacterial meningitis. Ann Intern Med. 1975 May;82(5):689–693. doi: 10.7326/0003-4819-82-5-689. [DOI] [PubMed] [Google Scholar]
- Gardner W. G., Prior R. B., Perkins R. L. Fluid and pharmacological dynamics in a subcutaneous chamber implanted in rats. Antimicrob Agents Chemother. 1973 Aug;4(2):196–197. doi: 10.1128/aac.4.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon C., Regamey C., Kirby W. M. Comparative clinical pharmacology of amoxicillin and ampicillin administered orally. Antimicrob Agents Chemother. 1972 Jun;1(6):504–507. doi: 10.1128/aac.1.6.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoehn M. M., Murphy H. W., Pugh C. T., Davis N. E. Paper chromatographic techniques for the determination of cephalothin and desacetylcephalothin in body fluids. Appl Microbiol. 1970 Nov;20(5):734–736. doi: 10.1128/am.20.5.734-736.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby W. M., De Maine J. B., Serrill W. S. Pharmacokinetics of the cephalosporins in healthy volunteers and uremic patients. Postgrad Med J. 1971 Feb;47(Suppl):41–46. [PubMed] [Google Scholar]
- LEE C. C., HERR E. B., Jr, ANDERSON R. C. Pharmacological and toxicological studies on cephalotin. Clin Med (Northfield) 1963 Jun;70:1123–1138. [PubMed] [Google Scholar]
- Molavi A., Barza M., Cole W., Berman H., Weinstein L. In vitro assessment of tobramycin, a new aminoglycoside with anti-Pseudomonas activity. Chemotherapy. 1973;18(1):7–16. doi: 10.1159/000221242. [DOI] [PubMed] [Google Scholar]
- Strausbaugh L. J., Mandaleris C. D., Sande M. A. Cefamandole and ampicillin therapy in experimental Haemophilus influenzae meningitis. J Infect Dis. 1977 Feb;135(2):210–216. doi: 10.1093/infdis/135.2.210. [DOI] [PubMed] [Google Scholar]
- Tan J. S., Trott A., Phair J. P., Watanakunakorn C. A method for measurement of antibiotics in human interstitial fluid. J Infect Dis. 1972 Nov;126(5):492–497. doi: 10.1093/infdis/126.5.492. [DOI] [PubMed] [Google Scholar]
- Vianna N. J., Kaye D. Penetration of cephalothin into the spinal fluid. Am J Med Sci. 1967 Aug;254(2):216–220. doi: 10.1097/00000441-196708000-00012. [DOI] [PubMed] [Google Scholar]
- Waterman N. G., Kastan L. B. Interstitial fluid and serum antibiotic concentrations. Arch Surg. 1972 Aug;105(2):192–196. doi: 10.1001/archsurg.1972.04180080046008. [DOI] [PubMed] [Google Scholar]
- Waterman N. G., Raff M. J., Scharfenberger L., Barnwell P. A. Protein binding and concentrations of cephaloridine and cefazolin in serum and interstitial fluid of dogs. J Infect Dis. 1976 Jun;133(6):642–647. doi: 10.1093/infdis/133.6.642. [DOI] [PubMed] [Google Scholar]


