Summary
Background
The contemporary associations of type 2 diabetes with a wide range of incident cardiovascular diseases have not been compared. We aimed to study associations between type 2 diabetes and 12 initial manifestations of cardiovascular disease.
Methods
We used linked primary care, hospital admission, disease registry, and death certificate records from the CALIBER programme, which links data for people in England recorded in four electronic health data sources. We included people who were (or turned) 30 years or older between Jan 1, 1998, to March 25, 2010, who were free from cardiovascular disease at baseline. The primary endpoint was the first record of one of 12 cardiovascular presentations in any of the data sources. We compared cumulative incidence curves for the initial presentation of cardiovascular disease and used Cox models to estimate cause-specific hazard ratios (HRs). This study is registered at ClinicalTrials.gov (NCT01804439).
Findings
Our cohort consisted of 1 921 260 individuals, of whom 1 887 062 (98·2%) did not have diabetes and 34 198 (1·8%) had type 2 diabetes. We observed 113 638 first presentations of cardiovascular disease during a median follow-up of 5·5 years (IQR 2·1–10·1). Of people with type 2 diabetes, 6137 (17·9%) had a first cardiovascular presentation, the most common of which were peripheral arterial disease (reported in 992 [16·2%] of 6137 patients) and heart failure (866 [14·1%] of 6137 patients). Type 2 diabetes was positively associated with peripheral arterial disease (adjusted HR 2·98 [95% CI 2·76–3·22]), ischaemic stroke (1·72 [1·52–1·95]), stable angina (1·62 [1·49–1·77]), heart failure (1·56 [1·45–1·69]), and non-fatal myocardial infarction (1·54 [1·42–1·67]), but was inversely associated with abdominal aortic aneurysm (0·46 [0·35–0·59]) and subarachnoid haemorrhage (0·48 [0·26–0.89]), and not associated with arrhythmia or sudden cardiac death (0·95 [0·76–1·19]).
Interpretation
Heart failure and peripheral arterial disease are the most common initial manifestations of cardiovascular disease in type 2 diabetes. The differences between relative risks of different cardiovascular diseases in patients with type 2 diabetes have implications for clinical risk assessment and trial design.
Funding
Wellcome Trust, National Institute for Health Research, and Medical Research Council.
Introduction
Patients with type 2 diabetes are at increased risk of cardiovascular diseases and associated clinical complications.1 Although type 2 diabetes has become an increasingly common disease, estimated to affect 380 million people worldwide by 2025,2 the incidence of myocardial infarction and stroke has declined rapidly during the past few decades. However, myocardial infarction and stroke continue to be chosen as primary outcomes of major type 2 diabetes trials (appendix).3 To reliably estimate the benefit of type 2 diabetes prevention and treatment in trials, or the future burden of type 2 diabetes-associated diseases for health-care planning, a better understanding of how type 2 diabetes affects the risk of other acute and chronic cardiovascular manifestations is needed.
Previous studies have not compared the relation between type 2 diabetes and a wide range of cardiovascular outcomes such as heart failure, peripheral arterial disease, abdominal aortic aneurysm, and ventricular arrhythmias in the same study, but have instead focused on a narrower range of disease outcomes, usually just one or two.4 Such comparisons need large study samples to reliably estimate associations for rare outcomes. Since early reports were published,5 results of several small studies have shown that the effect of type 2 diabetes on cardiovascular manifestations differs according to the specific cardiovascular outcome measured6 and the sex of the participant.7 However, these studies were not designed to reliably assess associations with several cardiovascular diseases or across population subgroups.
We have addressed these gaps in knowledge by establishing a large prospective cohort using linked electronic health records,8, 9 which combine information about diabetes diagnosis, risk factors, and medication use with future cardiovascular events. Our objective was to investigate and compare associations between type 2 diabetes and future risk of 12 of the most common initial cardiovascular presentations in men and women.
Methods
Study population
The study population was drawn from the CALIBER programme (CArdiovascular disease research using LInked Bespoke studies and Electronic health Records),9 which links four sources of electronic health data in England: primary care health records (coded diagnoses, clinical measurements, and prescriptions) from general practices contributing to the Clinical Practice Research Datalink (CPRD), coded hospital discharges (hospital episode statistics), the Myocardial Ischaemia National Audit Project (MINAP), and death registrations. Individuals were eligible for inclusion if they were (or turned) 30 years or older between Jan 1, 1998, and March 25, 2010, and if they had been registered for at least 1 year in a practice that met research data recording standards. We excluded individuals with a history of cardiovascular disease or if they had a record of pregnancy within 6 months of study entry (appendix).
Approval was granted by the independent scientific advisory committee of the Medicines and Healthcare products Regulatory Agency (protocol 12_117) and the MINAP Academic Group.
Procedures
We defined individuals as having diabetes at baseline (type 1, type 2, or uncertain type) on the basis of coded diagnoses recorded in CPRD or hospital episode statistics at or before study entry (appendix). Participants who developed new-onset diabetes during follow-up were analysed according to their baseline status of no diabetes. We compared people with type 2 diabetes to those without diabetes; we excluded people with type 1 diabetes or diabetes of uncertain type. In each participant with diabetes, we assessed glycaemic control by taking the mean of all the HbA1c measurements from 3 years before study entry to 3 years after, ignoring values occurring after an endpoint.
For continuous variables (BMI, HDL cholesterol, total cholesterol, and systolic blood pressure) we used, as a baseline value, the most recent measurement recorded in CPRD in the year before study entry, but included measurements outside this time window in imputation models. Social deprivation was included in models as quintiles of the index of multiple deprivation,10 a score calculated for each participant's neighbourhood on the basis of social indices such as income, education, and employment. Data recorded before study entry were used to classify participants as never smokers, ex-smokers, or current smokers at baseline.
Outcomes
The primary endpoint was the first record of one of the following 12 cardiovascular presentations in any of the data sources: stable angina, unstable angina, myocardial infarction, unheralded coronary death, heart failure, transient ischaemic attack, ischaemic stroke, subarachnoid haemorrhage, intracerebral haemorrhage, peripheral arterial disease, abdominal aortic aneurysm, and a composite outcome classified as arrhythmia or sudden cardiac death, which consisted of cardioversion, ventricular arrhythmia, implantable cardioverter defibrillator, cardiac arrest, or sudden cardiac death. Any events occurring after the first cardiovascular presentation were ignored. Endpoint definitions are described in the appendix and coding algorithms are available on the CALIBER portal. Secondary outcomes were cardiovascular mortality and all-cause mortality.
Statistical analysis
We plotted crude cumulative incidence curves for each cardiovascular endpoint for people with no diabetes and those with type 2 diabetes, using age as the timescale (appendix). Follow-up was censored at the occurrence of a primary endpoint, death, de-registration from the practice, or the last data collection for the practice, whichever occurred first.
We used multivariable Cox regression to calculate cause-specific hazards for associations between type 2 diabetes and initial presentations of cardiovascular disease. The proportional hazards assumption was verified by plotting Schoenfeld residuals (appendix). In the primary analysis, we compared individuals with type 2 diabetes to those without diabetes, adjusting for age, sex, BMI, deprivation, HDL cholesterol, total cholesterol, systolic blood pressure, smoking status, and prescription of statins or other antihypertensive medication in the year before study entry. The baseline hazard function of each model was stratified by general practice and sex, and we used multiple imputation to account for missing covariate data (appendix). We also did analyses adjusted for age and sex only, and analyses adjusted for age, sex, and cardiovascular risk factors. We assessed interactions with age and sex. In patients with type 2 diabetes, we estimated hazard ratios (HRs) by level of glycaemic control (HbA1c concentration). We grouped patients with type 2 diabetes into categories by HbA1c concentration, with cutoff points at 48 mmol/mol (6·5%, the threshold for diagnosis of diabetes),11 and 58 mmol/mol (7·5%, the recommended threshold for initiation of thiazolidinedione or insulin in type 2 diabetes in UK guidelines).12
15% of people with diabetes did not have a code for the type of diabetes (appendix) and were excluded from the primary analyses. To assess the effect of this potential misclassification bias, we did a sensitivity analysis comparing individuals with any diabetes diagnosis to those without diabetes (most patients with diabetes in a cohort of this age would have type 2 diabetes). We did sensitivity analyses ignoring endpoints recorded only in primary care (CPRD), restricted to fatal endpoints, or restricted to individuals who entered the study after 2004 (when recording of covariates would be expected to be more complete after introduction of the Quality and Outcomes Framework to incentivise good performance in the care of specified diseases).13 We did analyses using R 2.15.
This trial is registered with ClinicalTrials.gov, number NCT01804439.
Role of the funding source
The funder of the study had no role in the conduct of the study or study design, in the collection, analysis, or interpretation of the data, or in the writing of this report. ADS, SD, and ER had access to the raw data for this study. The corresponding author had full access to all of the data in the study and had final responsibility for the decision to submit for publication.
Results
The study cohort included 1 921 260 individuals, of whom 1 887 062 (98·2%) did not have diabetes and 34 198 (1·2%) had type 2 diabetes. People with type 2 diabetes had lower mean HDL cholesterol and higher mean BMI than people without diabetes (table). The use of statins and antihypertensive medication was greater in people with type 2 diabetes than in those without diabetes, and increased over time (table). People with type 2 diabetes were about twice as likely to be black or south Asian as those without diabetes (table).
Table.
Baseline characteristics of 1 921 260 people without cardiovascular diseases at baseline, according to sex and type 2 diabetes status
|
Women |
Men |
||||
|---|---|---|---|---|---|
| No diabetes (n=955 655) | Type 2 diabetes (n=15 805) | No diabetes (n=931 407) | Type 2 diabetes (n=18 393) | ||
| Age, years | 48·2 (16·2) | 64·7 (14·4) | 45·4 (14) | 60·8 (13) | |
| Social deprivation* | 184 942 (19·4%) | 4313 (27·3%) | 189 247 (20·3%) | 4285 (23·3%) | |
| Ethnic origin | |||||
| White | 503 274 (90·8%) | 9641 (81·8%) | 388 763 (90·5%) | 10 716 (82·4%) | |
| South Asian | 14 673 (2·6%) | 912 (7·7%) | 12 865 (3·0%) | 1041 (8·0%) | |
| Black | 16 722 (3·0%) | 748 (6·3%) | 13 148 (3·1%) | 670 (5·2%) | |
| Other | 19 328 (3·5%) | 491 (4·2%) | 14 640 (3·4%) | 579 (4·5%) | |
| Smoking status | |||||
| Current smoker | 130 946 (17·6%) | 2028 (14·4%) | 148 020 (23·7%) | 3327 (20·6%) | |
| Ex-smoker | 108 593 (11·4%) | 2927 (18·5%) | 109 538 (11·8%) | 5507 (29·9%) | |
| Never smoked | 506 383 (67·9%) | 9158 (64·9%) | 366 729 (58·7%) | 7327 (45·3%) | |
| Systolic blood pressure†, mm Hg | 127 (19·6) | 141 (19·7) | 133 (17·2) | 139 (17·6) | |
| Diastolic blood pressure†, mm Hg | 77·1 (10·3) | 79·5 (10·1) | 80·3 (10·0) | 80·5 (10·0) | |
| Total cholesterol†, mmol/L | 5·54 (1·14) | 5·08 (1·22) | 5·39 (1·11) | 4·77 (1·16) | |
| HDL cholesterol†, mmol/L | 1·57 (0·45) | 1·34 (0·39) | 1·28 (0·37) | 1·14 (0·33) | |
| BMI†, kg/m2 | 26·0 (5·59) | 30·5 (6·76) | 26·5 (4·43) | 29·3 (5·43) | |
| Random glucose concentration†, mmol/L | 5·35 (1·16) | 10·4 (4·93) | 5·56 (1·29) | 10·7 (4·78) | |
| Fasting glucose concentration†, mmol/L | 5·14 (0·75) | 8·72 (3·53) | 5·31 (0·79) | 9·1 (3·51) | |
| Glycaemic control‡ | |||||
| HbA1c recorded | 12 835 (1·3%) | 12 187 (77·1%) | 12 031 (1·3%) | 14 435 (78·5%) | |
| HbA1c, mmol/mol | 44·3 (14·7) | 59·3 (18·0) | 46·9 (16·3) | 60·5 (18·1) | |
| HbA1c <48 mmol/mol (6·5%) | 9468 (73·8%) | 3445 (28·3%) | 8030 (66·7%) | 3671 (25·4%) | |
| HbA1c 48–58 mmol/mol (6·5–7·5%) | 1854 (14·4%) | 3458 (28·4%) | 2004 (16·7%) | 4075 (28·2%) | |
| HbA1c ≥58 mmol/mol (7.5%) | 1513 (11·8%) | 5284 (43·4%) | 1997 (16·6%) | 6689 (46·3%) | |
| Diabetes treatment in year before study entry | |||||
| Diet only | NA | 4591 (29·0%) | NA | 5467 (29·7%) | |
| Metformin | 884 (0·1%) | 7714 (48·8%) | 106 (<0·1%) | 8764 (47·6%) | |
| Sulfonylurea | 133 (<0·1%) | 6241 (39·5%) | 124 (<0·1%) | 7526 (40·9%) | |
| Insulin | 189 (<0·1%) | 1939 (12·3%) | 77 (<0·1%) | 1882 (10·2%) | |
| Thiazolidinedione | 5 (<0·1%) | 962 (6·1%) | 6 (<0·1%) | 1225 (6·7%) | |
| DPP-4 inhibitor, meglitinide derivative, or GLP-1 receptor agonist | 1 (<0·1%) | 153 (1·0%) | 1 (<0·1%) | 182 (1·0%) | |
| Cardiovascular preventive treatment in year before study entry | |||||
| Statin | 18 233 (1·9%) | 5636 (35·7%) | 19 537 (2·1%) | 6680 (36·3%) | |
| Any antihypertensive medication | 156 098 (16·3%) | 9404 (59·5%) | 99 179 (10·6%) | 9898 (53·8%) | |
| ACE inhibitor | 59 412 (6·2%) | 5278 (33·4%) | 44 176 (4·7%) | 6333 (34·4%) | |
| Angiotensin receptor blocker | 7324 (0·8%) | 1357 (8·6%) | 5276 (0·6%) | 1263 (6·9%) | |
| β blocker | 54 861 (5·7%) | 2755 (17·4%) | 34 455 (3·7%) | 2730 (14·8%) | |
| Subset of patients entering the study from 2004 onwards | |||||
| Number of patients | 283 993 | 6900 | 293 890 | 8 212 | |
| Age, years | 43·6 (15·6) | 64·1 (15·7) | 41·4 (13·0) | 59·6 (13·7) | |
| HbA1c recorded‡ | 6191 (2·2%) | 6509 (94·3%) | 5677 (1·9%) | 7816 (95·2%) | |
| Statin prescription in year before study entry | 11 774 (4·1%) | 4383 (63·5%) | 13 059 (4·4%) | 5395 (65·7%) | |
| Antihypertensive prescription in year before study entry | 43 736 (15·4%) | 4663 (67·6%) | 33 535 (11·4%) | 5464 (66·5%) | |
| ACE inhibitor prescription in year before study entry | 20 577 (7·2%) | 2866 (41·5%) | 17 531 (6·0%) | 3776 (46·0%) | |
Data are mean (SD) or number (%). Proportion of participants with non-missing values of covariates: ethnic origin 52·5% (1 002 211 of 1 921 260 participants), smoking 72·9% (1 400 483 participants), systolic blood pressure 42·2% (811 591 participants), diastolic blood pressure 42·2% (811 591 participants), total cholesterol 8·3% (158 990 participants), HDL cholesterol 5·4% (103 809 participants), and BMI 30·3% (582 172 participants). NA=not applicable. ACE=angiotensin-converting enzyme.
Number (%) in most deprived quintile.
Most recent measurement within 1 year of study entry.
Mean HbA1c during the 3 years before or after study entry.
The prevalence of any type of diabetes in all individuals in CALIBER aged 40–50 years (with or without previous cardiovascular disease) was 1·52% (95% CI 1·47–1·57) in women and 2·25% (2·19–2·32) in men (appendix). During follow-up, 51 690 participants were newly diagnosed with diabetes, with a median time to diagnosis from study entry of 4·9 years (IQR 2·4–7·7).
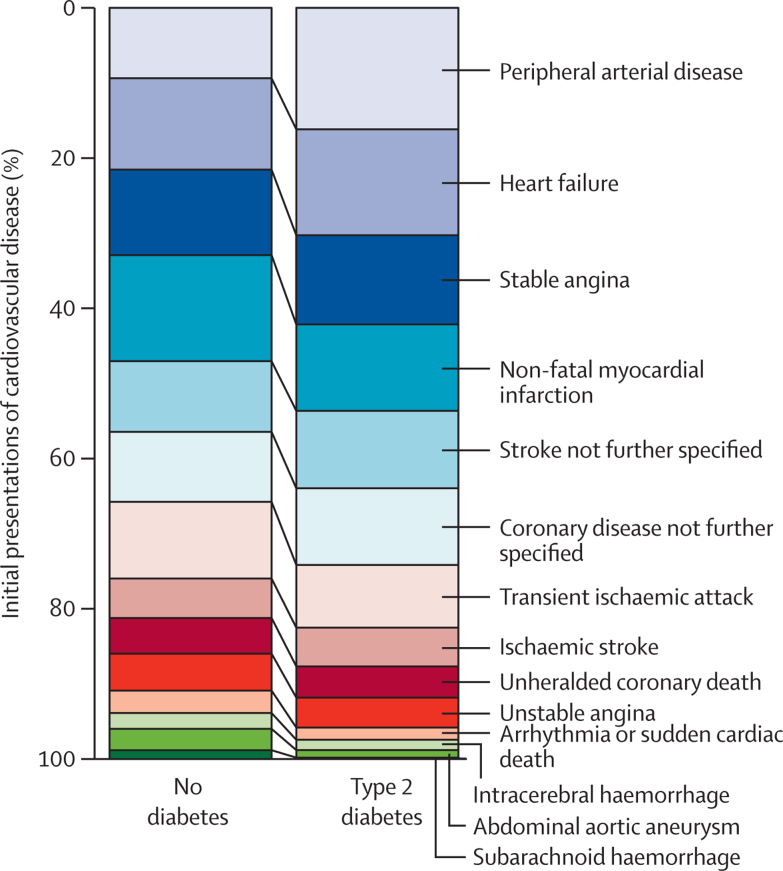
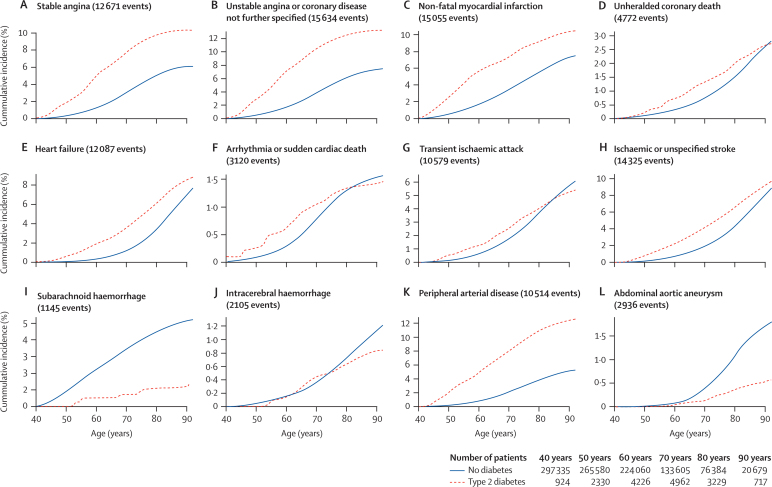
We analysed 113 638 cardiovascular events over 11·6 million person-years of follow-up (median follow-up 5·5 years [IQR 2·1–10·1]). Of these events, 6137 (5·4%) were in people with type 2 diabetes, who accrued 162 756 person-years of follow-up. Peripheral arterial disease was the first presentation in 992 (16·2%) of the 6137 patients with type 2 diabetes who had cardiovascular events, and heart failure was the first presentation in 866 (14·1%) of these patients (figure 1). By contrast, 10 074 (9·4%) of 107 501 people without diabetes presenting with cardiovascular events had peripheral arterial disease, and 13 072 (12·2%) had heart failure (appendix). Cumulative incidence curves show substantial differences in the direction and strength of the associations between each of the cardiovascular manifestations and type 2 diabetes (figure 2; appendix). The difference in the cumulative incidence of peripheral arterial disease between people with and without diabetes was the largest of all the cardiovascular diseases; a woman with type 2 diabetes at age 40 years had a 9·7% risk (95% CI 8·4–11·1) of developing peripheral arterial disease as her first presentation of cardiovascular disease by age 80 years; a woman without diabetes had a 3·2% risk (3·1–3·3). The corresponding figures for men were 11·7% (10·5–13·0) and 4·5% (4·4–4·7).
Figure 1.
Distribution of initial presentations of cardiovascular diseases
Distribution of initial presentations of cardiovascular disease in participants with and without type 2 diabetes and no history of cardiovascular disease.
Figure 2.
Cumulative incidence curves for the incidence of first presentation of 12 cardiovascular diseases in patients aged ≥40 years, by diabetes status
The curves begin at age 40 years rather than 30 years because 40 years is a typical age for a patient to develop type 2 diabetes.
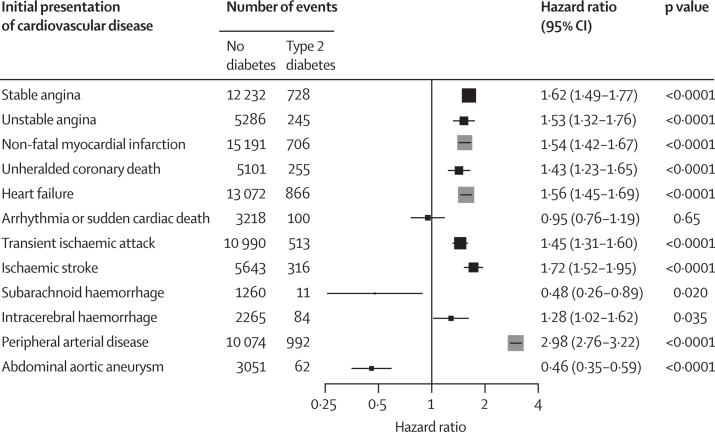
In multivariable Cox models, we noted strong positive associations between type 2 diabetes and peripheral arterial disease, ischaemic stroke, stable angina, heart failure, and non-fatal myocardial infarction (figure 3; appendix).
Figure 3.
Association of type 2 diabetes with 12 cardiovascular diseases in patients aged ≥30 years
Adjusted hazard ratios (HRs) for different initial presentations of cardiovascular diseases associated with type 2 diabetes, adjusted for age, sex, BMI, deprivation, HDL cholesterol, total cholesterol, systolic blood pressure, smoking status, and statin and antihypertensive drug prescriptions. Two non-specific components of the primary endpoint are not shown in the figure for simplicity (they are inprecisely recorded versions of one of the 12 initial presentations): coronary disease not further specified, HR 1·58 (95% CI 1·45–1·73), p<0·0001; stroke not further specified 1·64 (1·48–1·81), p<0·0001.
By contrast, type 2 diabetes was inversely associated with abdominal aortic aneurysm and subarachnoid haemorrhage (figure 3). No statistically significant association between arrhythmia or sudden cardiac death and type 2 diabetes was noted (figure 3). The strengths of associations were slightly attenuated by adjustment for risk factors and medication compared with the model adjusted for age and sex only (appendix).
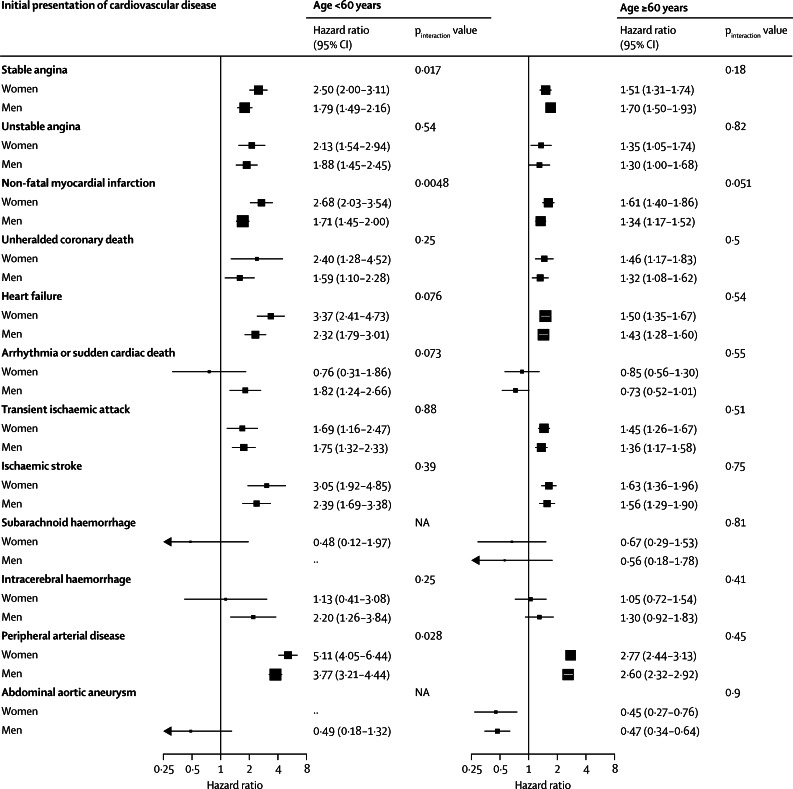
For individuals aged 40 years without cardiovascular disease, the overall estimated risk of developing any cardiovascular disease by age 80 years was 30·7% (95% CI 30·3–31·0) for women without diabetes and 44·3% (43·8–44·7) for men without diabetes, compared with 58·2% (54·9–61·4) for women with type 2 diabetes and 67·4% (64·4–70·4) for men with type 2 diabetes (appendix). We observed a slightly greater risk of non-fatal myocardial infarction associated with type 2 diabetes in women younger than 60 years than in men younger than 60 years, but noted no other statistically significant differences between sexes (figure 4). Associations between type 2 diabetes and coronary endpoints, transient ischaemic attack, ischaemic stroke, and peripheral arterial disease were significantly stronger in younger age groups than in older age groups (appendix). HRs for type 2 diabetes and cardiovascular endpoints were consistent across ethnic groups for the common endpoints such as heart failure, stable angina, and peripheral arterial disease, but the results for less common endpoints were imprecise because of the small number of events (data not shown).
Figure 4.
Hazard ratios for association of type 2 diabetes with 12 cardiovascular diseases by sex and age
Hazard ratios by sex and age group for the association of different initial presentations of cardiovascular disease with type 2 diabetes, adjusted for age, BMI, deprivation, HDL cholesterol, total cholesterol, systolic blood pressure, smoking status, and statin and antihypertensive drug prescriptions. NA=not applicable.
In individuals with type 2 diabetes, the risk of cardiovascular diseases associated with the presence of type 2 diabetes was highest for those with an HbA1c concentration of 58 mmol/mol (7·5%) or higher or those in whom HbA1c had not been recorded (appendix). Individuals with type 2 diabetes and an HbA1c concentration of less than 48 mmol/mol (6·5%) had an increased risk of peripheral arterial disease (HR 1·82, 95% CI 1·52–2·18) and ischaemic stroke (1·53, 1·18–1·98), but no greater risk of any of the other cardiovascular diseases (appendix).
Overall, results were robust to a range of modifications explored in our sensitivity analyses, including a comparison of people with any diabetes versus no diabetes (appendix). Results did not differ when primary care data were omitted as a source of endpoint information, apart from a slightly stronger association between type 2 diabetes and heart failure (HR 2·15 [95% CI 1·96–2·36] when primary care data were omitted vs 1·56 [1·45–1·69] when included; appendix). Type 2 diabetes was strongly associated with composite cardiovascular mortality and all-cause mortality (appendix).
Discussion
This population-based, contemporary study of nearly 2 million individuals with a median follow-up of 5·5 years provides strong evidence that associations between type 2 diabetes and 12 specific cardiovascular disease outcomes differ in terms of direction and magnitude of effects. Our findings draw attention to the high absolute and relative risks of incident peripheral arterial disease, heart failure, and stable angina in people with type 2 diabetes,1, 11 diseases that differ in preventive strategies and that often are poorly represented in the primary endpoint of randomised trials.
Peripheral arterial disease is one of the most common first presentations of cardiovascular disease, consistent with the increase in prevalence between 2000 and 2010 reported in a systematic review.14 Furthermore, of the 12 diseases studied, peripheral arterial disease showed the strongest association with type 2 diabetes, with an adjusted HR of 2·98 (95% CI 2·76–3·22), consistent with previous studies.14 Heart failure was also one of the most common first presentations (accounting for 14·4% of events in people with type 2 diabetes). Our definition excludes heart failure occurring after acute myocardial infarction, but we have to interpret this result with caution because we know that our data sources miss some cases of myocardial infarction.15 Possible mechanisms might include long-term hypertension, chronic hyperglycaemia, microvascular disease, glycosylation of myocardial proteins, diabetic nephropathy, and autonomic neuropathy.1 Similar to the meta-analysis of cohort studies in the Emerging Risk Factors Collaboration,4 we noted a weaker association of cardiovascular disease with type 2 diabetes in people 60 years or older than in younger people.
A novel finding was the association of type 2 diabetes with reduced incidence of two major aneurysmal diseases: abdominal aortic aneurysm and subarachnoid haemorrrhage. An inverse association between diabetes and abdominal aortic aneurysm has been suggested by cross-sectional studies of abdominal aortic aneurysm screening and case-control studies,6, 16, 17 but evidence from large prospective cohort studies has been mixed.18, 19 With 3113 abdominal aortic aneurysm events, our study is one of the largest cohort studies investigating this outcome,18, 19 and makes a substantial contribution to the evidence for a possible causal relation.
No previous cohort study has been large enough to investigate the association of type 2 diabetes with subarachnoid haemorrhage, but several case-control studies are consistent with our results (panel).20 These findings support the need to identify potential mechanisms that might have therapeutic implications. Such mechanisms might include diabetes-mediated changes in the vascular extracellular matrix, such as glycation of the extracellular matrix and covalent cross-linking between elastin and collagen in the aortic wall.21
Panel. Research in context.
Systematic review
We did a scientific literature search for population-based cohort studies that examined the association of two or more incident cardiovascular diseases in people with and without type 2 diabetes. We searched Embase and Medline for articles in English published within the past 10 years using the search terms “diabetes”, “occur*” or “association” or “incidence” or “onset” or “risk”, “prospective” or “cohort”, and terms for each of the individual diseases of interest as well as general terms for cardiovascular disease. We found a large meta-analysis of 102 cohort studies by the Emerging Risk Factors Collaboration,4 and meta-analyses of sex differences in the associations of diabetes with stroke27 and coronary heart disease.7 These meta-analyses did not differentiate between type of diabetes, and studied only a few cardiovascular diseases (coronary artery disease, stroke, vascular death). We found no cohort studies that reported the distribution of a large number of different initial presentations of cardiovascular disease in patients with type 2 diabetes.
Interpretation
Our study builds on the findings of previous cohort studies and meta-analyses showing that diabetes is strongly associated with increased risk of many atherosclerotic cardiovascular diseases. We show that this specifically holds true for type 2 diabetes, and that peripheral arterial disease and heart failure are the most common initial presentations of cardiovascular disease in patients with type 2 diabetes. We corroborate previous smaller studies in showing that type 2 diabetes is associated with reduced risk of abdominal aortic aneurysm and possibly subarachnoid haemorrhage. These findings have implications for disease modelling and clinical risk assessment.
Several studies have shown that type 2 diabetes is associated with out-of-hospital cardiac arrest and sudden cardiac death,22, 23 and an important unanswered question has been the extent to which this effect is mediated by incident diseases known to increase arrhythmic risk such as myocardial infarction and heart failure. In this study we looked at the initial presentation of cardiovascular disease—ie, arrhythmia with no previous myocardial infarction or heart failure—and our finding of no association suggests that the higher risk of cardiac arrest with type 2 diabetes is mediated by atherosclerotic coronary disease.
Sex differences in the effect of diabetes on coronary heart disease have been the subject of several reviews and meta-analyses.24 Although the absolute risk for coronary heart disease morbidity and mortality is lower in women than in men, the relative risk associated with diabetes has generally been reported to be higher in women,7, 25, 26 potentially due to their adverse risk-factor profile.26 The most recent meta-analysis of prospective studies focusing on diabetes reported relative risks for incident coronary heart disease of 2·63 for women and 1·85 for men with diabetes.7 Sex differences in the association of type 2 diabetes with outcomes other than coronary heart disease have less often been reported, with conflicting results for stroke.27, 28 In participants younger than 60 years, we noted weak evidence of a slightly stronger association of type 2 diabetes with myocardial infarction in women than in men—which is consistent with previous reports—but no other sex differences in associations between type 2 diabetes and cardiovascular outcomes.24
Our finding that HbA1c concentrations were associated with the risk of many cardiovascular diseases strengthens the case for the causal relevance of blood glucose in type 2 diabetes-related cardiovascular disease. These associations were particularly strong for peripheral arterial disease, and persisted even in participants with an HbA1c concentration of less than 48 mmol/mol (6·5%), suggesting that risk is not controlled in this group. Individuals in whom HbA1c had not been measured were at higher risk, consistent with measurement being a marker of overall quality of care.
Our results support the use of clinically collected real-world cohorts from electronic health records to provide such evidence of absolute and relative risks of different disease outcomes in people with type 2 diabetes, and to complement findings from conventional investigator-led cohort studies,4 which typically are smaller, not contemporary, and have less external validity.
Our results will help to inform drug development and the design of trials in type 2 diabetes. Trials3 have often included acute myocardial infarction and acute stroke as their primary event endpoints, because of a previous perception that these outcomes were the main disease burdens in type 2 diabetes, or that they are easier to ascertain and validate than chronic disease endpoints. We propose that chronic disease endpoints such as heart failure, peripheral arterial disease, and stable angina are important to consider in the choice of primary endpoint because they are common, have a high morbidity burden, and might have different treatment effects from myocardial infarction or stroke.
Although a strength of this study is the ability to differentiate a wide range of cardiovascular diseases in a validated electronic health record linkage, the accuracy and amount of phenotypic detail recorded in such databases is limited. Residual confounding due to diet, physical activity, stress, and environmental factors might be a potential source of bias. Although coding for type 2 diabetes is prone to error in clinical practice,29 coding error is unlikely to be an important source of bias in our study because our analyses, based on the diagnostic11 marker of HbA1c, were consistent with the overall results. The age-specific prevalences of type 2 diabetes we estimated are similar to those from a national survey done at a similar time to our study.30 Error might occur in the recording of the cardiovascular outcomes; however, those that are more reliably coded (such as non-fatal myocardial infarction) might therefore be expected to show stronger associations with type 2 diabetes than diseases that are less reliably coded (such as stable angina). The fact that we did not observe this potential result suggests that the heterogeneity is real. We noted similar associations with type 2 diabetes when endpoint ascertainment was restricted to hospital admissions and deaths, which was reassuring. Our lifetime risks were somewhat artificial, because they were based on extrapolation of event rates reported in people entering the cohort at different ages, but this design did mean that they were more contemporaneous than estimates from long-term follow-up of cohorts diagnosed decades ago.
Heart failure and peripheral arterial disease are the most common initial manifestations of cardiovascular disease in type 2 diabetes. The differences between relative risks of different cardiovascular diseases in patients with type 2 diabetes have implications for clinical risk assessment and trial design.
Acknowledgments
Acknowledgments
This study was supported by the National Institute for Health Research (RP-PG-0407-10314, PI HH), Wellcome Trust (WT 086091/Z/08/Z, PI HH), the Medical Research Prognosis Research Strategy Partnership (G0902393/99558, PI HH) and the Farr Institute of Health Informatics Research, funded by The Medical Research Council (K006584/1, PI HH), in partnership with Arthritis Research UK, the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council, the Engineering and Physical Sciences Research Council, the National Institute of Health Research, the National Institute for Social Care and Health Research (Welsh Assembly Government), the Chief Scientist Office (Scottish Government Health Directorates), and the Wellcome Trust. LS is supported by a senior clinical fellowship from the Wellcome Trust (098504). ADS is supported by a Wellcome Trust clinical research training fellowship (0938/30/Z/10/Z). CPG is funded by the National Institute for Health Research (NIHR/CS/009/004) as a Clinician Scientist and Honorary Consultant Cardiologist. SD is supported by a University College London Provost's Strategic Development Fund fellowship. AT acknowledges support of Barts and the London Cardiovascular Biomedical Research Unit, funded by the National Institute for Health Research. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the National Institute for Health Research or the UK Department of Health.
Contributors
ADS and ER analysed and interpreted the data. ADS drafted the report. SD prepared the data. HH was the principal investigator and had the original research idea. CL, ER, SD, MP-R, CPG, JD, LS, AT, and HH contributed to interpretation of results, and critically reviewed and commented on the report. All authors saw and approved the final version. ADS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Declaration of interests
ADS and his institution have received grants from the Wellcome Trust; and his institution has received grants from the Medical Research Council (MRC) and National Institute for Health Research (NIHR). ER's institution has received grants from the Wellcome Trust, MRC, and NIHR. SD reports grants from the NIHR and Wellcome Trust; and personal fees from University College London Provosts Strategic Development Fund Fellowship. LS has received grants from the Wellcome Trust, MRC, and NIHR; and personal fees from GlaxoSmithKline. AT has received a grant from the NIHR grant programme. HH's institution has received grants from the MRC, Wellcome Trust, British Heart Foundation, NIHR, National Institute for Social Care and Health Research, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Chief Scientist Office, Cancer Research UK and Arthritis Research UK; fees for consultancy from AstraZeneca; and payment for lectures including service on speakers bureaus from Erasmus Summer School. All other authors declare no competing interests.
Supplementary Material
References
- 1.Rydén L, Grant PJ, Anker SD. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34:3035–3087. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 2.van Dieren S, Beulens JW, van der Schouw YT, Grobbee DE, Neal B. The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil. 2010;17:s3–s8. doi: 10.1097/01.hjr.0000368191.86614.5a. [DOI] [PubMed] [Google Scholar]
- 3.Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317–1326. doi: 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 4.Emerging Risk Factors Collaboration Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kannel WB, McGee DL. Diabetes and cardiovascular disease: the Framingham study. JAMA. 1979;241:2035–2038. doi: 10.1001/jama.241.19.2035. [DOI] [PubMed] [Google Scholar]
- 6.Nordon IM, Hinchliffe RJ, Loftus IM, Thompson MM. Pathophysiology and epidemiology of abdominal aortic aneurysms. Nat Rev Cardiol. 2011;8:92–102. doi: 10.1038/nrcardio.2010.180. [DOI] [PubMed] [Google Scholar]
- 7.Peters SAE, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57:1542–1551. doi: 10.1007/s00125-014-3260-6. [DOI] [PubMed] [Google Scholar]
- 8.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383:1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Denaxas SC, George J, Herrett E, et al. Data resource profile: cardiovascular disease research using linked bespoke studies and electronic health records (CALIBER) Int J Epidemiol. 2012;41:1625–1638. doi: 10.1093/ije/dys188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department for Communities and Local Government English indices of deprivation 2010: technical report. https://www.gov.uk/government/publications/english-indices-of-deprivation-2010-technical-report (accessed June 24, 2014).
- 11.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(suppl 1):S81–S90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 12.National Collaborating Centre for Chronic Conditions . Type 2 diabetes: national clinical guideline for management in primary and secondary care (update) Royal College of Physicians; London, UK: 2008. [PubMed] [Google Scholar]
- 13.Health and Social Care Information Centre. Department of Health Quality and outcomes framework. http://www.hscic.gov.uk/qof (accessed June 24, 2014).
- 14.Fowkes FGR, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382:1329–1340. doi: 10.1016/S0140-6736(13)61249-0. [DOI] [PubMed] [Google Scholar]
- 15.Herrett E, Shah AD, Boggon R, et al. Completeness and diagnostic validity of recording acute myocardial infarction events in primary care, hospital care, disease registry, and national mortality records: cohort study. BMJ. 2013;346:f2350. doi: 10.1136/bmj.f2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kent KC, Zwolak RM, Egorova NN. Analysis of risk factors for abdominal aortic aneurysm in a cohort of more than 3 million individuals. J Vasc Surg. 2010;52:539–548. doi: 10.1016/j.jvs.2010.05.090. [DOI] [PubMed] [Google Scholar]
- 17.De Rango P, Farchioni L, Fiorucci B, Lenti M. Diabetes and abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2014;47:243–261. doi: 10.1016/j.ejvs.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Ohrlander T, Merlo J, Ohlsson H, Sonesson B, Acosta S. Socioeconomic position, comorbidity, and mortality in aortic aneurysms: a 13-year prospective cohort study. Ann Vasc Surg. 2012;26:312–321. doi: 10.1016/j.avsg.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 19.Iribarren C1, Darbinian JA, Go AS, Fireman BH, Lee CD, Grey DP. Traditional and novel risk factors for clinically diagnosed abdominal aortic aneurysm: the Kaiser multiphasic health checkup cohort study. Ann Epidemiol. 2007;17:669–678. doi: 10.1016/j.annepidem.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Feigin VL, Rinkel GJ, Lawes CM, et al. Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies. Stroke. 2005;36:2773–2780. doi: 10.1161/01.STR.0000190838.02954.e8. [DOI] [PubMed] [Google Scholar]
- 21.Shantikumar S, Ajjan R, Porter KE, Scott DJ. Diabetes and the abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2010;39:200–207. doi: 10.1016/j.ejvs.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Siscovick DS, Sotoodehnia N, Rea TD, Raghunathan TE, Jouven X, Lemaitre RN. Type 2 diabetes mellitus and the risk of sudden cardiac arrest in the community. Rev Endocr Metab Disord. 2010;11:53–59. doi: 10.1007/s11154-010-9133-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kucharska-Newton AM, Couper DJ, Pankow JS, et al. Diabetes and the risk of sudden cardiac death, the Atherosclerosis Risk in Communities study. Acta Diabetol. 2010;47(suppl 1):161–168. doi: 10.1007/s00592-009-0157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rivellese AA, Riccardi G, Vaccaro O. Cardiovascular risk in women with diabetes. Nutr Metab Cardiovasc Dis. 2010;20:474–480. doi: 10.1016/j.numecd.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 25.Lee WL, Cheung AM, Cape D, Zinman B. Impact of diabetes on coronary artery disease in women and men: a meta-analysis of prospective studies. Diabetes Care. 2000;23:962–968. doi: 10.2337/diacare.23.7.962. [DOI] [PubMed] [Google Scholar]
- 26.Kanaya AM, Grady D, Barrett-Connor E. Explaining the sex difference in coronary heart disease mortality among patients with type 2 diabetes mellitus: a meta-analysis. Arch Intern Med. 2002;162:1737–1745. doi: 10.1001/archinte.162.15.1737. [DOI] [PubMed] [Google Scholar]
- 27.Peters SAE, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775 385 individuals and 12 539 strokes. Lancet. 2014;383:1973–1980. doi: 10.1016/S0140-6736(14)60040-4. [DOI] [PubMed] [Google Scholar]
- 28.Mulnier HE, Seaman HE, Raleigh VS, et al. Risk of stroke in people with type 2 diabetes in the UK: a study using the General Practice Research Database. Diabetologia. 2006;49:2859–2865. doi: 10.1007/s00125-006-0493-z. [DOI] [PubMed] [Google Scholar]
- 29.de Lusignan S, Sadek N, Mulnier H, Tahir A, Russell-Jones D, Khunti K. Miscoding, misclassification and misdiagnosis of diabetes in primary care. Diabet Med. 2012;29:181–189. doi: 10.1111/j.1464-5491.2011.03419.x. [DOI] [PubMed] [Google Scholar]
- 30.Shelton N. In: Health Survey for England 2003, volume 2: risk factors for cardiovascular disease. Sproston K, Primatesta P, editors. Department of Health; London, UK: 2004. Diabetes. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.