Abstract
Activin A is a member of the TGFβ superfamily. Activin A and TGFβ have multiple common downstream targets and have been described to merge in their intracellular signaling cascades and function. We have previously demonstrated that coordinated loss of E-cadherin and TGFβ receptor II results in epithelial cell invasion. When grown in three-dimensional organotypic reconstruct cultures, esophageal keratinocytes expressing dominant-negative mutants of E-cadherin and TGFβ receptor II showed activated Smad2 in the absence of functional TGFβ receptor II. However, we could show increased levels of Activin A secretion, and Activin A was able to induce Smad2 phosphorylation. Growth factor secretion can activate autocrine and paracrine signaling, which affects crosstalk between the epithelial compartment and the surrounding microenvironment. We show that treatment with the Act A antagonist Follistatin or with a neutralizing Activin A antibody can increase cell invasion in organotypic cultures in a fibroblast- and MMP-dependent manner. Similarly, suppression of Activin A with shRNA increases cell invasion and tumorigenesis in vivo. Therefore, we conclude that maintaining a delicate balance of Activin A expression is critical for homeostasis in the esophageal microenvironment.
Keywords: esophageal squamous cell carcinoma, TGFβ, BMP signaling, cell invasion
Introduction
Activin A (Act A), like other members of the TGFβ superfamily, is a regulator of embryonic development and tumorigenesis [1–3]. Act A binds to type II activin receptors, ActRII/IIB, that have intrinsic serine/threonine kinase activity. Binding of Act A results in the recruitment of activin receptor type I, Alk4, and the subsequent phosphorylation and activation of Smad 2/3 [4, 5]. TGFβ and Activin signaling intersect at the level of Smad2/3 resulting in common downstream effector activation.
Previous research has shown that coordinated loss of E-cadherin and TGFβ receptor II (TβRII) occurs in the majority of esophageal squamous cell cancers [6]. Based upon this evidence, we have established an organotypic culture model system utilizing esophageal keratinocytes expressing dominant-negative mutants of E-cadherin and TβRII to investigate the biological consequences of their loss. Keratinocytes expressing dominant-negative forms of E-cadherin and TβRII and tumor tissues with coordinated loss of E-cadherin and TβRII retained the expression of phosphorylated Smad2, thus suggesting that Act A compensates for the loss of TGFβ signaling and induces the activation of Smad2.
Similar to TGFβ, Act A is described as having pro- and anti-tumorigenic functions. Members of the TGFβ family, including Act A, can downregulate E-cadherin promoting cell invasion [7]. Our previous study showed increased cell invasion in Boyden chamber assays in response to Act A stimulation through an E-cadherin-dependent increase of the CD44 variant form in the esophageal cancer cell line TE11 [8]. In the current study, we further demonstrate the increased secretion of Act A in invasive organotypic cultures. Act A can suppress proliferation in different tumor cells [9–11], mainly through the induction of p15INK4B [12], while others describe an oncogenic role for Act A [3, 13–16]. From these reports and similar observations made for TGFβ1, which also has been shown to have dual functions [17, 18], Act A is likely to have a role in the regulation of epithelial homeostasis. Interestingly, other studies demonstrated that Act A is necessary for the maintenance of self-renewal in human embryonic stem cells through the induction of Oct4, Nanog, Nodal, Wnt3, FGF-2, and by suppressing BMP signaling [19]. These observations illustrate Act A function as a mediator of stemness with the potential for being a cancer stem cell marker [20, 21]. Furthermore, suppression of Id2, a downstream target of Act A and TGFβ1, is central to the induction of epithelial-mesenchymal-transition [22], a mechanism known to induce single-cell invasion, which is antagonized by BMP. Another Act A target, Id1, regulates epidermal homeostasis [23]. However, the role of Id1 in proliferation could only be demonstrated in three-dimensional cultures, not in monolayer experiments [23].
To better understand the complex role of Act A in esophageal cell invasion, we employed three-dimensional organotypic cultures to reconstitute the epithelium with squamous esophageal epithelial cells expressing wild-type full-length E-cadherin, dominant-negative mutant E-cadherin or dominant-negative mutant E-cadherin and TGFβ receptor II (ECdnT). We found that Act A secretion is increased in ECdnT cells. In addition, altered cell invasion of ECdnT cell in vitro was dependent upon fibroblasts and MMP activation. In vivo we show that loss of Act A can initiate tumorigenesis using xenograft models. Overall, our data indicate that Act A concentrations contribute to the homeostasis in the esophageal microenvironment and in the absence of functional TGFβ signaling can shift the balance towards tumor invasiveness.
Material and methods
Cell culture and tissues
Primary esophageal epithelial cells (keratinocytes) from normal human esophagus were established as described previously [6]. Fetal esophageal fibroblasts were isolated as previously described [6] and head-and-neck cancer-associated fibroblasts were purchased from Asterand (Detroit, MI). Fibroblasts were grown in DMEM with 5% fetal bovine serum (FBS, Hyclone, Thermo Fisher Scientific, Waltham, MA), 100 units/mL penicillin, and 100 µg/mL streptomycin (Gibco, Invitrogen, Carlsbad, CA). HUVEC cells were grown in EBM-2 basal media (Lonza Biosciences, Walkersville, MD) supplemented with endothelial growth medium 2 (EGM-2) growth factors (Lonza Biosciences, Walkersville, MD).
A tissue microarray with 83 spotted squamous esophageal tissues, AccuMax Tissue Microarray, was purchased from ISU Abxis (distributed by Accurate Chem, Westbury, NY).
Lentivirus infection
shRNA-mediated loss of Act A in esophageal squamous cells was performed using shRNA directed towards three different target sequences. Act A shRNA and control pGIPZ plasmids were purchased from Thermo Scientific. Virus was generated using HEK293T cells. Cells were then transduced and sorted using flow cytometry prior to experimental use.
Xenograft animal experiments
The current study protocol was reviewed and approved by the Vanderbilt University Animal Care and Use Committee. Briefly, a total of 1×106 cells (INHBA-high and normal esophageal fibroblasts) were suspended in 150µl of Matrigel (BD Bioscience, Franklin Lakes, NJ) and kept on ice prior to subcutaneous injection into the flanks of 8–10 week old female NOD/SCID mice (The Jackson Laboratory, Bar Harbor, ME). Tumor growth was monitored weekly by caliper measurements.
Organotypic Culture
Organotypic reconstructs were grown as previously described [6] with the exception that each culture was rinsed in 1×PBS and incubated with Epidermalization 3 medium lacking serum for two more days before harvesting. The following treatments were added to the organotypic cultures at the time of epithelial seeding and renewed with every media change: Five ng/ml recombinant human TGFβ1, 10ng/ml Activin A, 100 ng/ml Follistatin and 600 ng/ml neutralizing antibody against Activin A (all from R&D Systems, Minneapolis, MN), or 1 µM A83-01 (Tocris, Bristol, UK) and 1 µM GM6001 (Millipore EMD, Billerica, MA). Puromycin treatment at 5 µg/ml on day 5 was applied to induce fibroblast cell death. The culture matrix was washed serially with PBS, before the epithelial cells were seeded.
Spheroid formation
Spheroid assays were performed as described previously [6]. In brief, cells were resuspended in 2% Matrigel and then cultured on a Matrigel layer in chamber slides (Nalge Nunc, Naperville, IL). Cells were fixed in 4% paraformaldehyde (Fisher Scientific, Hampton, NJ) overnight at 4°C. Incubation with Alexa568–conjugated phalloidin was overnight at 4°C.
Proliferation assays
Cells were plated at 500 cells per well in a 96-well plate for proliferation assays. WST-1 reagent (Roche, Nutley, NJ) was added to each well at the time points indicated and incubated at 37°C for a minimum of 1 hour. Absorbance measurements at 450nm were taken using a BioTek Synergy 4 plate reader (Winooski, VT). Measurements were taken in 24-hour increments.
Immunofluorescence
Organotypic culture tissue, previously fixed in formalin for 24 hours and embedded in paraffin, was sectioned at 5µm, deparaffinized and heated in 1× TBE buffer in a pressure cooker for 12 min for antigen retrieval. Samples were blocked in 1× PBS with 5% Bovine Serum Albumin (Sigma-Aldrich, Saint- Louis, MO) for 1 hour prior to incubation with primaries antibody in 1× PBS-BSA 5% overnight at 4°C. Tissues were then rinsed three times in PBS and incubated with secondary antibodies in 1× PBS BSA 5% for 1 hour at room temperature. After additional rinses with PBS, the sections were mounted with Vectashield mounting medium containing DAPI (Vector Laboratories, Burlingame, CA). Images were taken on a Zeiss microscope, using Axiocam and Axiovision software (Carl Zeiss Microscopy, Thornwood, NY).
Immunohistochemistry for TβRII and pSmad2 in the tissue microarrays and OTC samples was done using the Vectastain Elite kit (Vector Laboratories, Burlingame, CA) following the manufacturer's protocol.
Western Blot
Western blots were performed as previously described [8]. The results are representative of at least three independent experiments.
Flow cytometry
Flow cytometry was used to separate lentivirus-transduced from the non-transduced population based upon GFP+ status. Gates were set to divide high and low GFP+ expressing cells. Flow cytometry experiments were performed using a BD AriaIII flow cytometer (BD Biosciences, Franklin Lakes, NJ) in the VMC Flow Cytometry Shared Resource. After sorting, the cells were returned to culture for future experiments.
ELISA
Capture ELISAs for Act A and TGFβ1 were purchased from R&D Systems (Minneapolis, MN). The protocols were performed according to the manufacturers instructions.
Invasion assays
Matrigel-based invasion chamber assays were purchased from BD Biosciences (Franklin Lakes, NJ) and performed according to manufacturer’s direction. Act A was added either to the top insert or the bottom chamber to assess hapto- versus chemotactic invasion during 16–24 hours incubation.
For trans-endothelial invasion assays (XCELLigence system, Roche Diagnostics), Roche E-plates (Roche Diagnostics) were treated with 100 µl of 0.1% sterile gelatin (Sigma-Aldrich) overnight at 4°C. Plates were washed once with sterile PBS before the addition of HUVEC cells (Lonza Biosciences, Walkersville, MD). 25,000 HUVEC cells/100 µl were seeded on E-plates and incubated for 18 hours at 37°C. The cell index was monitored on the xCELLigence system while the monolayer was formed. Following the formation of the HUVEC monolayer, which is indicated by the plateau in the cell index, the endothelial cell growth medium EGM-2 was removed and 100 µl of RPMI containing 5% serum media was added. The cell index was monitored for 4 hours and allowed to stabilize. Then, esophageal epithelial cells pre-treated with Act A for 24 hours were added to each well at a density of 5,000 cells/100 µl. The cell index was normalized to the HUVEC monolayer and invasion was monitored over time as epithelial cells disrupt the endothelial cell layer (changes in initial slope). Rate of invasion of the cell lines were calculated in real time according to the RTCA software version 1.2.
Zymography
Zymography was performed as previously described [8]. Briefly, conditioned medium was separated by SDS-PAGE at 4°C in gel containing gelatin. The gels were then washed in Triton 2.5% (v/v) in ddH2O twice for 30 min and incubated overnight in at 37°C in a development buffer (0.05M Tris-HCl pH 8.8, 5mM CaCl2, 0.02% NaN3). Then, the gels were stained in 0.1% Coomassie blue R-250 for an hour and destained in methanol/acetic/acid/water solution (10%: 20%: 70%, v:v:v). Images were taken on Gel Doc XR system (Bio-Rad, Hercules, CA).
Antibodies and other reagents
Alexa 568-conjugated Phalloidin (Invitrogen, Carlsbad, CA), SMA (Sigma-Aldrich) and Podoplanin (eBioscience, San Diego, CA) were used for immunofluorescence. Anti-TβRII (clone L21) and PAI-1 (Santa Cruz Biotechnologies, Santa Cruz, CA), Ki67 (Vector Laboratories, Burlingame, CA). and phospho-Smad2 (Cell Signaling, Danvers, MA) were used for immunohistochemistry. Antibodies used to detect protein by Western blotting were E-cadherin (BD Transduction, Franklin Lakes, NJ), vimentin (Sigma-Aldrich, St. Louis, MO); total Smad 2, phospho-Smad2, were purchased from Cell Signaling Technologies (Danvers, MA); Alpha-tubulin from Abcam (Cambridge, MA).
Dataset analysis
Datasets made publicly available from Oncomine (http://www.oncomine.org/), GEO Datasets (http://www.ncbi.nlm.nih.gov/gds/; [24]), and NextBio (http://www.nextbio.com/b/nextbio.nb; [25]) were used to query clinical correlations with Act A (Supplemental Table 1). The collected information from each dataset was analyzed and visualized in Prism version 6.00 for Mac (GraphPad software, La Jolla, California, www.graphpad.com).
Biostatical analysis
Biostatistical was performed using Prism version 6.00 for Mac. In vitro and in vivo experiments were analyzed using Student’s t-tests or one-way ANOVAs. Statistical significance was set at p<0.05. All experiments were done in triplicates with at least 3 biological replicates.
Results
Increased epithelial cell invasion is associated with increased Act A secretion
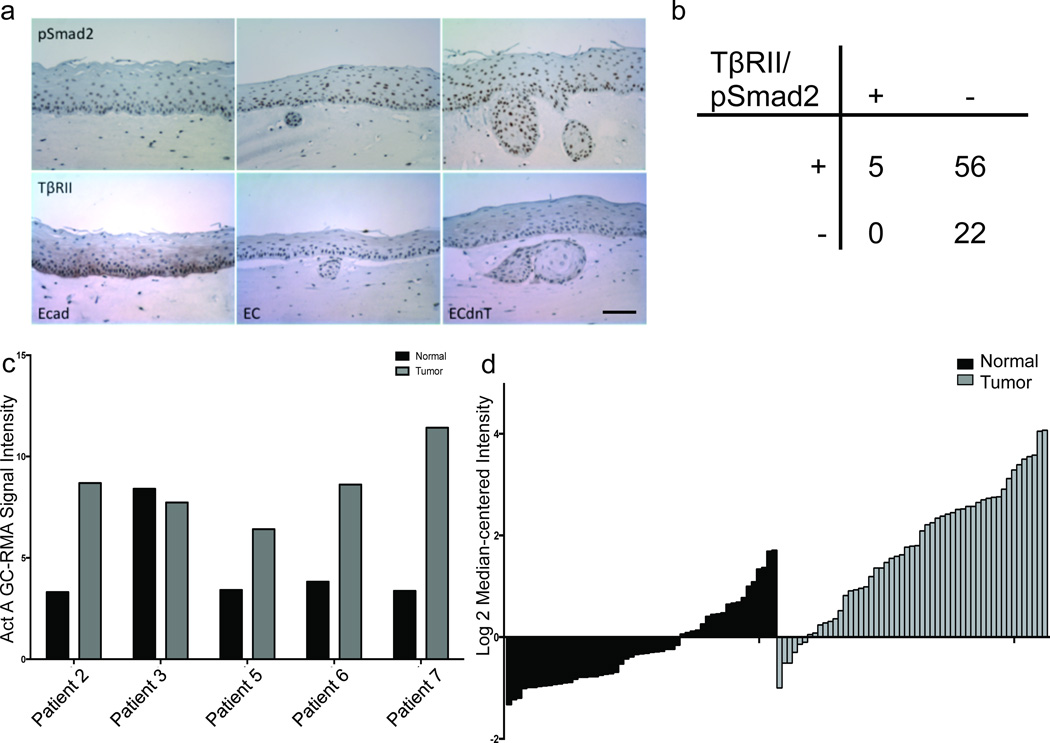
The R-Smads (Smad2 and Smad3) are common downstream mediators of both TGFβ and Activin signaling. We performed immunohistochemistry using antibodies against TβRII and pSmad2 to determine their expression in non-invasive and invasive organotypic cultures. Keratinocytes expressing wild-type E-cadherin (E) form a non-invasive epithelial sheet, while expression of dominant-negative E-cadherin (EC) or combined expression of dominant-negative E-cadherin and TβRII (ECdnT) leads to a gradual increase of invasiveness as shown previously [8]. We have previously shown that expression of dominant-negative E-cadherin correlates with lower TβRII levels in EC cells, potentially due to a lack of its stabilization at the cell membrane (6). Even though the signal for TβRII was lower in EC and ECdnT cells than in the normal control epithelium, represented by the E cells (Figure 1a), we observed a strong signal of nuclear pSmad2 in invasive ECdnT cells. Nuclear localization of pSmad2 in the absence of TβRII staining supports the notion that Smad2 can be activated and phosphorylated through a separate signaling pathway, when TβRII expression is low or disrupted. We subsequently analyzed 83 esophageal squamous cell carcinoma tissues for E-cadherin (6), TβRII and pSmad2 expression. Seventy-one percent of the tumor tissues retained Smad2 activation in the absence of TβRII (Figure 1b). To determine the levels of Act A gene expression in esophageal squamous cell carcinoma (ESCC), we analyzed published datasets and identified upregulation of Act A in ESCC tumor samples compared to normal tissues (Figure 1 c, d; Supplemental Table 1 [26, 27]).
Figure 1. Act A specifically stimulates phosphorylation of Smad2 and Act A upregulation is common in ESCC.
(a) Immunohistochemistry staining with antibody against phosphorylated Smad2 (pSmad2) and TGFβ receptor II (TβRII) showed increased nuclear signal for pSmad2 in the invasive ECdnT organotypic cultures. Scale bar 50 micron. (b) Analysis of immunohistochemistry staining for TβRII and pSmad2 in 83 ESCC cases in a tissue microarray shows no significant correlation. Fisher’s exact test, two tailed p= 0.3182. (c) Five paired normal adjacent and ESCC tissues (GSE17531) were analyzed for INHBA mRNA expression, which identified upregulation of INHBA in four ESCC samples. (d) Waterfall plot of a publically available dataset (GSE23400) represented upregulation of INHBA in the ESCC (grey bars) samples vs. normal (black bars).
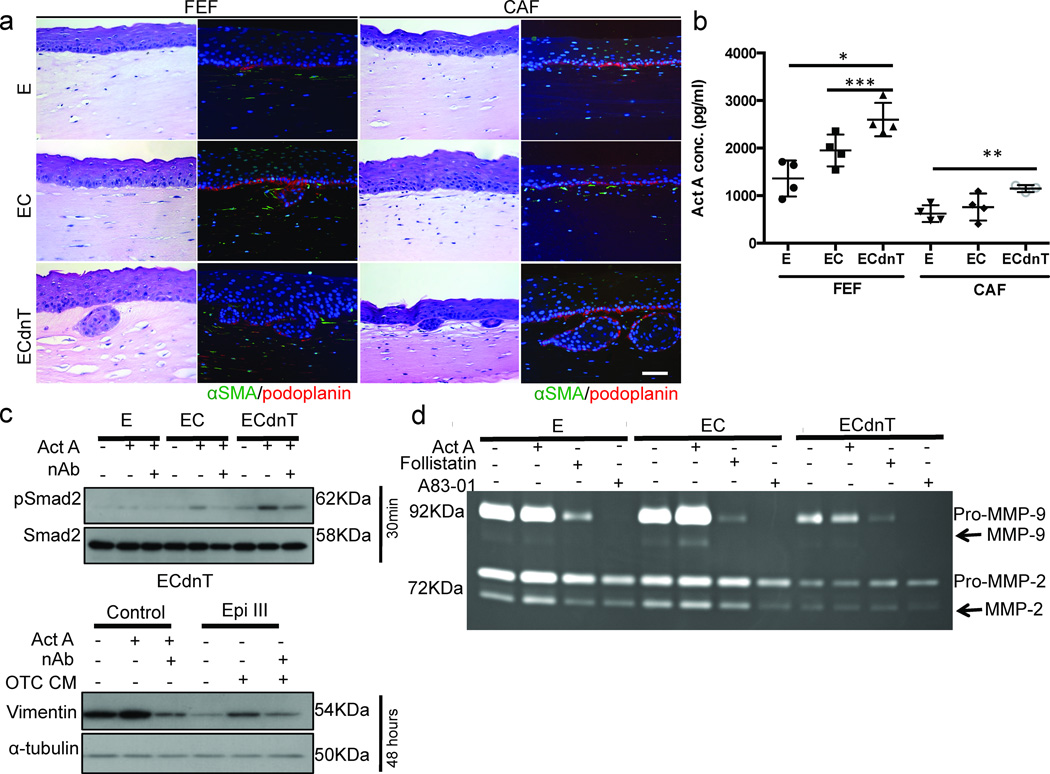
As esophageal epithelial cells invade in a fibroblast-dependent manner [6, 8], we employed organotypic cultures comparing the effects of the presence of embedded fetal esophageal fibroblasts (FEF) and cancer-associated fibroblasts (CAF) on cell invasion and Act A secretion (Figure 2a, b). E or EC cells grown in organotypic cultures with FEFs or CAFs had minimal invasive potential, while ECdnT cells showed cell invasion in either context (Figure 2a). Immunofluorescence staining with antibodies against the fibroblast-specific marker αSMA (green) exclusively labeled FEFs and CAFs in the matrix, while Podoplanin (red) expression, a putative marker of collective invasion, stained the basal membrane of the epithelial cells (Figure 2a).
Figure 2. Increased epithelial cell invasion is associated with higher levels of secreted Act A.
(a) Esophageal epithelial cells expressing wild-type full-length E-cadherin (E), dominant-negative mutant E-cadherin (EC) or dominant-negative mutant E-cadherin and TGFβ receptor II (ECdnT) were grown in organotypic cultures with either fetal esophageal fibroblasts (FEF) or cancer-associated fibroblasts (CAF) embedded in the underlying matrix. Immunofluorescence staining with antibody against αSMA (green) and podoplanin (red) showed similar expression pattern in the cultures. Scale bar is 50 micron. (b) Activin A concentration in conditioned media from organotypic cultures is higher in invasive cultures as measured using indirect ELISA. * p=0.003, ** p= 0.005, *** p=0.03 (c) Stimulation of epithelial cells with Act A in monolayer plastic culture demonstrated phosphorylation of Smad. Neutralizing antibody against Activin (nAb) prevented the induction of pSmad2 by Act A. Following stimulation with Act A or with conditioned media from organotypic culture increased expression of vimentin was detected after 48 hours by Western Blot. The increase was reversed in the presence of neutralizing antibody (nAb). (d) Inhibition with the Act A antagonist, Follistatin, or a pan-TGFβ inhibitor A83-01 suppressed MMP-9 secretion in E, EC and ECdnT cells as measured by gelatin zymography. Upper bands reflect pro-MMP, lower bands activated, cleaved MMP (arrow).
Since our analysis of human SCC samples implicated Act A in the regulation of Smad2 and cell invasion (Figure 1), we determined the levels of Act A in the conditioned media from organotypic cultures with different levels of invasion. We performed ELISA and observed a positive association between Act A secretion levels and epithelial cell invasion (Figure 2b). To test for specificity of Act A-mediated phosphorylation of Smad2 in this model system, we isolated protein from keratinocytes grown in a monolayer on plastic for Western Blot analysis. We compared protein lysates from conditions with Act A stimulation or neutralizing antibody to demonstrate that phosphorylation of Smad2 could be induced by Act A with high specificity. Increased signal for pSmad2 was detected following Act A stimulation, which was reduced in the presence of the neutralizing antibody. Similarly, treating ECdnT cells with Act A or conditioned media from organotypic cultures induced vimentin, a mesenchymal cytoskeleton component and a marker of tumor cell invasion. Conversely, Act A neutralizing antibody inhibited vimentin expression (Figure 2c).
We speculated that Act A may alter extracellular matrix degradation, since epithelial cell invasion is strongly associated with the digestion of the extracellular matrix by matrix metalloproteases. Therefore, we collected conditioned media from cells grown on monolayer and analyzed the secretion of the collagen-digesting matrix metalloproteases MMP-9 and MMP-2 using gelatin-zymography (Figure 2d). When using recombinant Follistatin, the endogenous inhibitor of Act A [28], or A83-01 (an inhibitor for ALK4, 5 and 7), MMP-9 secretion was reduced compared to untreated or Act A stimulated monolayer cultures (Figure 2d).
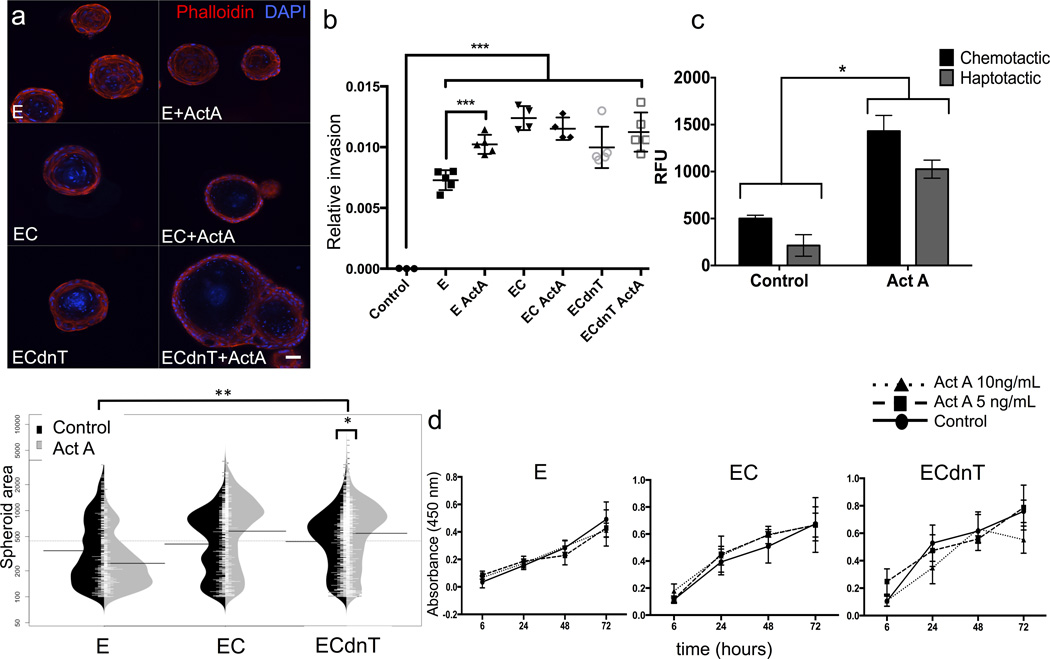
Stimulation with Act A increases spheroid size and cell invasion in vitro
To identify the functional consequences of Act A-mediated Smad2 signaling, we grew E, EC and ECdnT cells embedded in Matrigel to induce spheroid formation (Figure 3a). In the presence of Act A, ECdnT cells form more and larger spheroids compared to E and EC cells (Graph and Supplemental Table 2). In a trans-endothelial invasion assay (Figure 3b), we observed decreased impedance as a measure of cell invasion through the endothelial cell layer. Epithelial cells pre-treated with Act A were seeded on a layer of endothelial cells (HUVEC) and a significant disruption of the HUVEC layer was observed with Act A stimulation in normal E cells. More invasive EC and ECdnT cells disrupted the HUVEC layer to a comparable degree without or with Act A stimulation.
Figure 3. Stimulation with Act A increases spheroid size and cell invasion in vitro.
(a) Esophageal epithelial cells, when grown embedded in 2% Matrigel, form spheroids. Immunofluorescence with Alexa568-conjugated Phalloidin stained the actin cytoskeleton, DAPI, blue, was used as a counterstain for nuclei. Scale bar is 50 micron. Stimulation with recombinant Act A increased spheroid size and number as quantified in the graph, * and ** p< 0.0001. (b) Trans-endothelial cell migration was measured after stimulation of esophageal epithelial cells with Act A, *** p<0.0001. (c) Haptotactic (stimulation in top chamber) and chemotactic (addition to the media in the bottom chamber) invasion of ECdnT cells in response to Act A was measured in Boyden chamber assays kSFM is media only control, *p< 0.0001. (d) Proliferation index was determined after stimulation with two concentrations of Act A using the WST assay. Cell proliferation was unchanged by stimulation with Act A.
When assessing Act A function in Boyden chamber invasion assays (Figure 3c), we added Act A either to the top chamber as a stimulant for the ECdnT cells or to the bottom as a chemoattractant. Act A increased haptotactic as well as chemotactic cell invasion. This observation was in line with our previous report that Act A increased cell invasion in esophageal cancer cell lines [8].
Finally, we show that the increased cell invasion is independent of cell proliferation, as WST-1 assays did not show differences in proliferation index in response to two different concentrations of Act A stimulation compared to untreated normal media (Figure 3d).
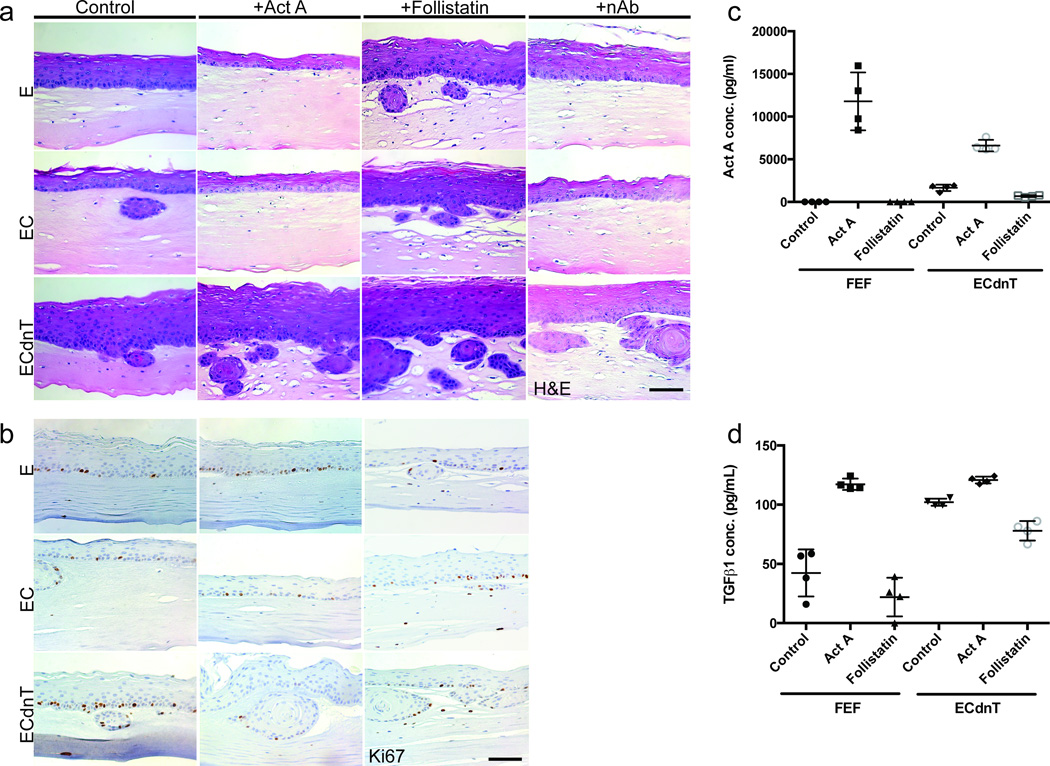
Imbalance of Act A induces epithelial cell invasion
Organotypic cultures allow us to measure the effects of the stromal compartment and epithelial cell homeostasis in a physiologically relevant context, while modifying signaling activation (Figure 4). As described earlier wild-type E-cadherin expressing cells grow as a normal stratified epithelium without invasion into the matrix (Figure 4a). When treated with Act A, epithelium formation of E cells remained unchanged (Figure 4a). However, the addition of Follistatin induced cell invasion, while Act A-neutralizing antibody did not. Similarly, EC cells, which have minimal invasive potential, show slightly increased invasion when treated with Follistatin. However, Act A treatment or addition of the neutralizing Act A-antibody prevented EC cell invasion. This strongly supports our idea that the cells are sensitive to changes in Act A and show differential responses when exposed to varying Act A concentrations in a context dependent manner.
Figure 4. Imbalance of Act A induces epithelial cell invasion.
(a) Esophageal epithelial cells expressing wild-type full-length E-cadherin (E), dominant-negative mutant E-cadherin (EC) or dominant-negative mutant E-cadherin and TGFβ receptor II (ECdnT) were grown in organotypic cultures in the presence of recombinant Activin A (Act A), its antagonist Follistatin or a neutralizing antibody against Activin A (nAb); H&E staining. Stimulation with Act A inhibited invasion of E and EC cells, but failed to suppress ECdnT cell invasion. Follistatin increased cell invasion in all cell types, while the neutralizing antibody prevented invasion of E and EC cells, without an effect on ECdnT cells. (b) Immunohistochemistry staining with ki67-antibody showed no differences in cell proliferation. Scale bars are 50 micron. (c) Indirect ELISA with antibody against Act A measured increased levels after addition of recombinant Act A in fibroblasts (FEF) and ECdnT. Untreated ECdnT cells (Control) secreted higher baseline levels of Act A than FEF, which were reduced by Follistatin. (d) TGFβ1 concentration was increased in response to stimulation with Act A and overall baseline secretion was higher in control ECdnT cells than fibroblasts as measured by indirect ELISA. Follistatin inhibited TGFβ1 secretion.
ECdnT cells have the highest potential for cell invasion and could be considered dysplastic or pre-malignant [8, unpublished data]. In contrast to E and EC cells, treatment with Act A did not inhibit ECdnT cell invasion. Conditions that disrupt Act A function, such as Follistatin treatment or Act A-neutralizing antibody, enhanced ECdnT cell invasion. Although the degree of cell invasion varied between the cell lines and treatment, the proliferation index as analyzed by staining for Ki67-positive cells was unchanged (Figure 4b). Again, invasion and changes in Act A signaling were not dependent on cell proliferation. However, as disruption of Act A signaling using Follistatin or the neutralizing Act A-antibody had differential effects, the balance of Act A signaling appeared to be integral for the induction of cell invasion.
In organotypic cultures, the respective treatments affected stromal as well as epithelial compartments. To analyze the role of Act A in autocrine and paracrine signaling, we determined Act A secretion levels in conditioned media from fibroblast and epithelial monolayer cultures stimulated with Act A or treated with the inhibitor Follistatin (Figure 4c). FEFs did not secret Act A, but exogenous addition of Act A could be detected by ELISA. Follistatin treatment had no effect on fibroblasts. Act A levels in ECdnTs indicate endogenous expression and secretion, which was reduced in the presence of Follistatin. Treatment with recombinant Act A elevated the levels measured by ELISA. Interestingly, TGFβ1 levels were influenced by Act A treatment in a similar pattern. Endogenous TGFβ1 secretion was at a detectable level in fibroblasts, albeit higher in ECdnTs. Follistatin reduced TGFβ1 secretion in both cell types. This may indicate a feedback mechanism of Act A and TGFβ signaling.
Induction of cell invasion by Act A is fibroblast- and MMP-dependent
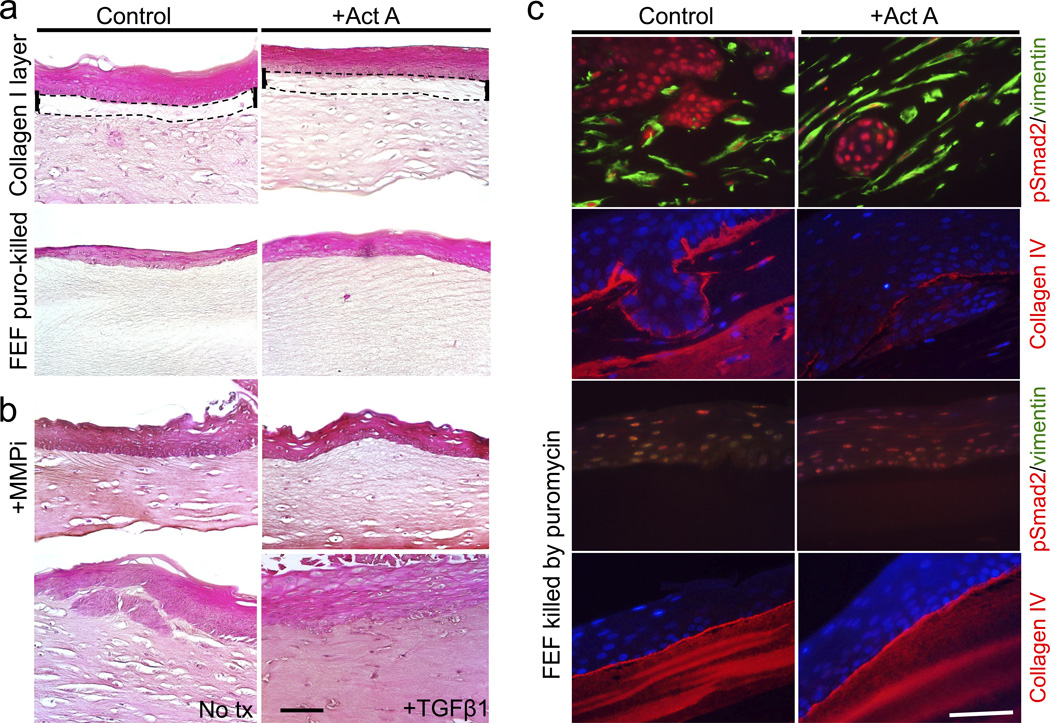
Epithelial cells grown in a monolayer on plastic have different gene expression patterns and behaviors compared to cells grown in a physiological context such as three-dimensional organotypic cultures. We have previously shown that fibroblast-secreted factors are necessary to induce cell invasion of ECdnT cells [8], yet we observed that Act A could initiate ECdnT invasion in Boyden chamber assays in the absence of fibroblasts or fibroblast-conditioned media (Figure 3b, c). We aimed to create an environment to address epithelial-fibroblast crosstalk and its effects on cell invasion. First, we overlayed the cellular matrix with a collagen I layer to prevent direct physical interaction of the epithelial cells with the embedded fibroblasts and potentially minimizing access to fibroblast-secreted factors (Figure 5a). ECdnT cells did not invade into the stroma in the presence of a collagen I layer, regardless if stimulated with Act A or not. As the collagen I layer could alter the pliability and stiffness of the matrix affecting cell invasion, we next performed the experiment without the collagen I layer, however, treated the stromal layer with puromycin to kill the embedded fibroblasts. Fibroblasts were allowed to crosslink and contract the collagen/Matrigel matrix during the initial 5 days of culture. Then, fibroblasts were killed by puromycin-treatment. ECdnT cells in the absence of fibroblasts did not invade into the extracellular matrix in control or Act A stimulated cultures (Figure 5a). This supports our previous observation that fibroblast paracrine signaling is important for epithelial cell invasion.
Figure 5. Regulation of cell invasion by Act A is fibroblast- and MMP-dependent.
(a) Separating the cellular matrix and epithelium of the organotypic cultures growing ECdnT cells through a collagen I layer, dashed lines, prevented cell invasion in the absence (control) and presence of Act A (+Act A). When the cellular matrix of the organotypic culture was treated with puromycin to kill the embedded fibroblasts before the ECdnT cells were seeded, epithelial formation occurred but invasion was inhibited with and without Act A stimulation. (b) Treatment of ECdnT organotypic cultures with a pan-MMP inhibitor, GM6001, suppressed cell invasion, which was not restored in the presence of Act A. Untreated (no tx) control ECdnT cells in organotypic culture invaded into the underlying matrix. TGFβ1 treatment inhibited epithelial cell invasion. Scale bars are 50 micron. (c) Immunohistochemistry showed nuclear localization of phosphorylated Smad (pSmad2, red) in control and Act A stimulated conditions. Collagen IV, red, was disrupted in invasive cultures after Act A treatment. Loss of the fibroblasts (FEF), labeled green with antibody against vimentin (no staining in the lower panels), had no effect on the nuclear localization of pSmad2. The collagen IV layer was not disrupted in non-invasive cultures in the absence of FEFs.
As MMP-9 secretion was induced by Act A treatment and correlated with increased cell invasion of ECdnT cells in organotypic cultures, we set out to determine if MMPs are necessary for Act A-induced ECdnT cell invasion. Using a pan-MMP activity inhibitor GM6001, we could abolish ECdnT cell invasion, which could not be restored by Act A addition (Figure 5b). This finding indicates that blocking MMP activity downstream of Act A disrupts the signaling cascade necessary for ECdnT cell invasion. As a control, we treated ECdnT cells with TGFβ1, which inhibited ECdnT cell invasion (Figure 5b). These data show that Act A and TGFβ1 have independent functions in this cell system, but also highlight the complexity of their balance. Immunofluorescence staining with antibodies against pSmad2 showed a strong nuclear signal in untreated control and Act A stimulated-organotypic cultures (Figure 5c). Collagen IV (red) is deposited at the basement membrane, but is disrupted after Act A treatment. The collagen IV layer is not disturbed in non-invasive conditions without fibroblasts regardless of Act A stimulation. Absence of fibroblasts (lack of vimentin-positive cells, green), while inhibiting cell invasion, only marginally diminished pSmad2-positive signal in the epithelial layer.
Act A knock-down results in cell invasion and tumorigenesis
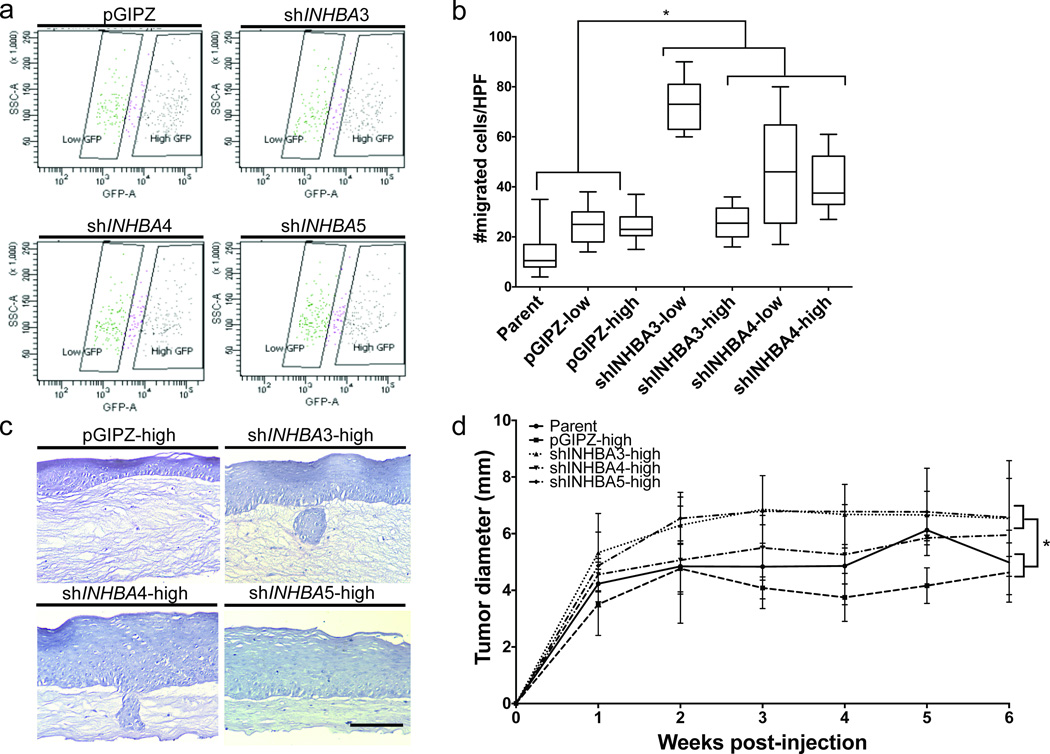
Our data obtained in monolayer and OTC cultures thus far suggest that the pro-invasive role of Act A is in part driven by the presence of fibroblasts and the induction of MMP expression. Therefore, we next set out to determine if ECdnT cells would exhibit an invasive phenotype without Act A secretion and signaling. To answer this question, ECdnT cells were transduced with three distinct clones to stably express shRNA specifically targeting Act A, shINHBA. Following transduction, the cells were sorted by flow cytometry to select for GFP-positive populations. To examine if Act A exerts distinct functions at different expression levels, we sorted the stable shRNA and empty vector control clones by GFP-low (shINHBA-low) and GFP-high (shINHBA-high) expression (Figure 6a; Supplemental Figure 1). In Boyden chamber migration assays, shINHBA-high and shINHBA-low cells showed increased chemotactic migration compared to parent and empty vector (pGIPZh) control cells (Figure 6b; Supplemental Figure 2a). shINHBA-high and shINHBA-low cells showed no proliferation differences compared to controls (Supplemental Figure 2b). Interestingly, shINHBA-low cells showed increased migration compared to shINHBA-high cells, suggesting a dose-dependent effect of Act A signaling. Dose-dependent effects of Act A signaling have been previously described, primarily in embryogenesis (Green and Smith, 1990; Green et al., 1992; Symes et al., 1994). Similarly to the effect observed in the Boyden chambers, organotypic reconstructs of shINHBA-high cells showed thicker epithelial cell layers and increased invasion into the underlying stroma compared to the pGIPZ-high control (Figure 6c).
Figure 6. shRNA-mediated loss of Act A promotes epithelial cell migration and invasion.
(a) ECdnT cells transduced with shRNA- Act A-GFP constructs (shINHBA3 through 5) were sorted by Flow Cytometry for positivity and low/high expression (left vs. right gating). (b) Boyden chamber migration assays were performed using shINHBA-high and shINHBA-low expressing cells. Both shINHBA-high and shINHBA-low showed overall increased in vitro migration compared to parent and empty vector (pGIPZ-high and -low) cells. Migrated cells are depicted as the number of cells counted per high-powered field. Analysis was performed using an one-way ANOVA and subsequent Student’s t-test. (c) shINHBA and empty vector control cells (pGIPZ-high) were grown in organotypic cultures with normal fetal esophageal fibroblasts. shINHBA cultures had increased epithelial cell layer thickness and increased collective cell invasion into the underlying stroma, compared to control cultures. Scale bar is 50 micron. (d) NOD/SCID flank injections were performed using shINHBA-high and control (parent and empty vector pGIPZ-high) cells, in co-culture with normal fetal esophageal fibroblasts. After six weeks post-injection, shINHBA-high cells showed overall greater tumor growth, compared to parent and pGIPZ-high control cells.
Finally, as we were able to observe an effect of after loss of Act A in epithelial cells in vitro, we set out to explore functional consequences of Act A suppression in vivo. Utilizing a Matrigel-plug xenograft model, we subcutaneously injected shINHBA-high, pGIPZ-high, and parent ECdnT cells with FEF into the flanks of female NOD/SCID mice. After six weeks of growth, mice injected with shINHBA-high cells had larger tumors compared to pGIPZ-high and parental control cells (Figure 6d). Therefore, we conclude that Act A function is context- and concentration-dependent and can either promote or inhibit epithelial cell migration, invasion, and tumor growth.
Discussion
Keratinocyte differentiation in the esophagus has much in common with other squamous tissues, such as the interfollicular skin and the oropharynx, making the esophagus an outstanding model to understand squamous epithelial homeostasis and disease [29–31]. We have previously shown that the coordinated loss of the cell adhesion molecule E-cadherin and TGFβ receptor II is a frequent event in esophageal squamous cell cancer and results in increased cell invasion [6]. Esophageal cancer has a high mortality rate, with 5-year survival remaining static at 19% [32] and the current treatment options for patients are restricted. The identification of mechanisms that disrupt esophageal homeostasis advances our understanding of the development and progression of pre-neoplastic lesions and has clinical significance.
Little is known about Act A and its involvement in esophageal disease. Act A expression is associated with lymph node metastasis, staging, poor patient prognosis [33], and concomitant upregulation of N-cadherin [34]. Act A has been associated with ESCC aggressiveness. This increase in aggressiveness is accompanied by increased proliferation [35] and MMP-7 activity [36]. We observed increased epithelial levels of MMP-9 in response to Act A stimulation, while MMP-2, which is mainly secreted by the fibroblasts in our system (data not shown), remained largely unaffected. While treatment with Follistatin and A83-01 enhanced cell invasion, it results in reduced MMP-9 and MMP-2 secretion as well as activity, indicating that other mechanisms are involved in cell invasion independent of MMP-9 and MMP-2 (unpublished data). Analysis of publicly available datasets identified frequent upregulation of Act A, but does not allow us to identify which subcellular compartment (tumor or stromal) is responsible Act A expression or secretion. Our data indicate that Act A exerts paracrine function on the fibroblasts resulting in a feedback loop required for epithelial cell invasion, since depletion of the fibroblasts in the organotypic cultures inhibits Act A-mediated cell invasion.
Our unique opportunity to analyze Act A function using three-dimensional organotypic cultures is highlighted by the differences in Act A signaling regulation as measured by its target Id1 in monolayer and three-dimensional cultures [23]. Act A and TGFβ overlap in their intracellular signaling cascades [24] and function, as demonstrated by deletions of TGFβ2, TGFβ3 and the Act A subunit, ActivinβA, which result in cleft palate defects in the respective mouse models [25–28]. Furthermore, analysis of the Act A and TGFβ-induced transcriptome demonstrate multiple common downstream targets [37]. Mutations in the TGFβ/BMP signaling axis are frequent events in different types of cancer: Similar to a 10-bp polyadenine tract within the TGFβ receptor type II gene that results in a frameshift mutation in GI cancers, a biallelic mutation in ACVR2 has been identified in colorectal and pancreatic cancer [38]. ACVR1B is mutated in pancreatic cancer [39]. In a majority of sporadic colorectal cancers, BMPR2 expression is impaired [40]. BAMBI (BMP and Activin Membrane-bound Inhibitor) is upregulated in colorectal cancer and is under direct regulation of the Wnt pathway [41] and is part of a gene expression profile that predicts metastasis [42].
Interestingly, stimulation of organotypic cultures with TGFβ1 resulted in suppressed ECdnT invasion, while recombinant Act A was unable to inhibit cell invasion. Treatment with Act A or Act A-neutralizing antibody had no effect in “normal” organotypic epithelia retaining E-cadherin expression and intact TGFβ signaling. In these normal epithelial cells, only the addition of Follistatin induced cell invasion demonstrating the importance of a balance between the Act A-mediated signaling and BMP pathways. Follistatin, while binding Act A with high affinity, can also antagonize BMP signaling, in particular BMP-2, -4, -7 and -11, as well as myostatin. BMPs, like Act A, signal through surface receptor complexes containing type I (ALK2 ALK3 and ALK6) and type II (BMPRII, ActRII, ActRIIB) receptors. While the BMPs, particularly BMP2 and BMP4, have higher affinity for their type I receptors, they can still stimulate signaling through the shared type II receptors [5]. These observations indicate that changes in the balance between Act A- and BMP mediated signaling can affect the phenotype in a context-dependent manner. ECdnT organotypic cultures, which model a pre-malignant phenotype, showed enhanced invasion in the presence of neutralizing antibody and Follistatin compared to untreated cells. While neutralizing Act A in EC cells suppressed invasion it failed to inhibit ECdnT cell invasion indicating that more invasive cells might be less responsive to the invasion-suppressive functions of Act A. Follistatin on the other hand increased invasion in all cell lines tested.
Follistatin is an antagonist of myostatin (GDF-8) in addition to inhibiting Act A. In an analysis of publically available esophageal and head-and-neck squamous cell carcinoma datasets (GDS2520, GDS3838) myostatin unlike INHBA is not differentially expressed in cancer compared to normal tissues. There is no evidence in the literature that myostatin contributes to collective invasion or the initiation of ESCC, however, myostatin is a key player in later stages of cancer progression through its role in cancer cachexia [43, 44].
High serum levels of Follistatin have been detected in patients with ovarian [45] and metastatic prostate cancer [46]. In oral squamous cell carcinoma, serum levels of Follistatin and Act A were not significantly different in the tumor patients compared to control groups [47]. Interestingly, Follistatin, as well as Act A, were overexpressed in tumor tissues from these patients. In the same study, Act A expression was shown to correlate with poor prognosis overall and disease-free survival, while Follistatin was not [47]. This observation further highlights that Follistatin may have independent roles other than antagonizing Activin A. In other studies, however, Follistatin upregulation has been positively correlated with cell motility, invasion and metastasis [48], while other groups have demonstrated that Follistatin can also inhibit experimental metastasis in SCID mice [49].
Knock-down of Act A in ECdnT cells using shRNA demonstrates epithelial cell-dependent effects of Act A, whereas the response of the stromal cells remains unaltered. Furthermore, cells with low levels of Act A knock-down were more invasive than with high levels of suppression indicating a dose-dependent phenotype. As the observations for the use of neutralizing antibody in the different cell lines appear contradictory, a possible explanation is that final Act A activity may vary following neutralization and, therefore, initiate differential cellular responses. Increased invasion and tumor initiation as observed with ECdnT cells supports the notion that endogenous Act A may suppress tumor initiation. Based on mouse models targeting Act A expression in the skin, it has been shown that Act A overexpression leads to epidermal hyperplasia [50]. However, when Act A-overexpressing mice were bred with transgenic animals carrying a dominant-negative deletion of the kinase-domain in the ActRIB, hyperplasia, hyperproliferation and abnormal keratinocyte organization could be rescued [45]. These data elude to the importance of Act A levels in the regulation of epithelial architecture. Interestingly, the same group observed differential results for Act A effects in vitro and in vivo, not only in regard to epithelial cell proliferation, but also migration. Act A promoted migration in the wounded skin, but showed no pro-migratory effect in vitro [43].
These observations, along with our results, indicate that Follistatin and shRNA against Act A could increase invasion and tumorigenesis depending on the cellular context. Exogenous Act A treatment in the background of mutant TβRII did not inhibit cell invasion, an additional hint at signal regulation through Act A gradients. Previous research regarding the role of Act A in embryogenesis may allow for the elucidation of the functional consequences of Act A during tumorigenesis, as the reactivation of essential developmental pathways have been found to contribute significantly to cancer initiation and development. Xenopus models have shown the dose-dependent effect of Act A in endo-mesoderm development. Act A induces specific gene expression signatures at increasing concentrations, thus inducing distinct cell fates [51–54]. This process occurs through long-range Act A diffusion through the extracellular matrix, and has been shown to signal in a cell-specific manner [52,55]. The effect of Act A is further complicated through its intermingling with additional signaling pathways, such as Wnt [56]. Therefore, based upon our and previous studies, we conclude that the balance of Act A concentration is crucial to exert its potentially dose-dependent dual function on invasion and growth.
Of note, laser-capture microdissected RNA expression analysis of invasive untreated ECdnT cells identified changes in multiple members of the TGFβ family (Supplemental Table 3). Most of these targets have been validated in mass-spectrometry analysis using conditioned media from ECdnT organotypic cultures. While BMP-2 itself was downregulated, Gremlin 1 was found to be upregulated. Similarly, the inhibitory pseudo-receptor BAMBI and latent-binding protein 1 were upregulated indicating potential TGFβ signaling suppression. Further, Activin inhibitors such as Follistatin and Follistatin-like were downregulated. These observations further highlight the importance of maintaining the equilibrium between intersecting pathways in the regulation of cell invasion and potentially tumorigenesis.
In summary, we showed that overexpression and exogenous Act A treatment result in MMP-dependent invasion requiring the presence of fibroblasts. However, as Follistatin induced epithelial cell invasion and knock-down of Act A similarly resulted in enhanced cell invasion and tumorigenesis, we propose that low levels of Act A result in elevated motility or invasive potential, while high Act A levels depending on the cellular context results in less invasion. In conclusion, shifting the balance between Act A and Follistatin can disrupt epithelial homeostasis.
Supplementary Material
Acknowledgements
This work was supported by the National Institute of Health (DK94900, DK091491). The use of Research Cores is supported by the Vanderbilt Ingram Cancer Center (P30 CA68485) and the Vanderbilt Digestive Disease Research Center (P30 DK058404). We like to thank Connie Weaver for performing the Xcelligence trans-endothelial cell invasion assays and Rainelli B. Koumangoye for editing of the manuscript.
Abbreviations
- ActR
Activin A, Act A; Activin receptors
- E
wild-type full-length E-cadherin
- EC
dominant-negative mutant E-cadherin
- ECdnT
dominant-negative mutant E-cadherin and TGFβ receptor II
- nAb
neutralizing antibody
Footnotes
Conflict of interest statement: The authors declare no conflict of interest.
Dislosure/Duality of Interest
The authors have no duality of interests to disclose.
References
- 1.Larsson J, Karlsson S. The role of Smad signaling in hematopoiesis. Oncogene. 2005;24:5676–5692. doi: 10.1038/sj.onc.1208920. [DOI] [PubMed] [Google Scholar]
- 2.Thisse B, Wright CV, Thisse C. Activin- and Nodal-related factors control antero-posterior patterning of the zebrafish embryo. Nature. 2000;403:425–428. doi: 10.1038/35000200. [DOI] [PubMed] [Google Scholar]
- 3.Wildi S, Kleeff J, Maruyama H, Maurer CA, Buchler MW, Korc M. Overexpression of activin A in stage IV colorectal cancer. Gut. 2001;49:409–417. doi: 10.1136/gut.49.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harrison CA, Gray PC, Fischer WH, Donaldson C, Choe S, Vale W. An activin mutant with disrupted ALK4 binding blocks signaling via type II receptors. J Biol Chem. 2004;279:28036–28044. doi: 10.1074/jbc.M402782200. [DOI] [PubMed] [Google Scholar]
- 5.Harrison CA, Wiater E, Gray PC, Greenwald J, Choe S, Vale W. Modulation of activin and BMP signaling. Mol Cell Endocrinol. 2004;225:19–24. doi: 10.1016/j.mce.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Andl CD, Fargnoli BB, Okawa T, Bowser M, Takaoka M, Nakagawa H, Klein-Szanto A, Hua X, Herlyn M, Rustgi AK. Coordinated functions of E-cadherin and transforming growth factor beta receptor II in vitro and in vivo. Cancer Res. 2006;66:9878–9885. doi: 10.1158/0008-5472.CAN-05-4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferreira MC, Witz CA, Hammes LS, Kirma N, Petraglia F, Schenken RS, Reis FM. Activin A increases invasiveness of endometrial cells in an in vitro model of human peritoneum. Mol Hum Reprod. 2008;14:301–307. doi: 10.1093/molehr/gan016. [DOI] [PubMed] [Google Scholar]
- 8.Le Bras GF, Allison GL, Richards NF, Ansari SS, Washington MK, Andl CD. CD44 upregulation in E-cadherin-negative esophageal cancers results in cell invasion. PLoS One. 2011;6:e27063. doi: 10.1371/journal.pone.0027063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burdette JE, Jeruss JS, Kurley SJ, Lee EJ, Woodruff TK. Activin A mediates growth inhibition and cell cycle arrest through Smads in human breast cancer cells. Cancer Research. 2005;65:7968–7975. doi: 10.1158/0008-5472.CAN-04-3553. [DOI] [PubMed] [Google Scholar]
- 10.Danila DC, Inder WJ, Zhang X, Alexander JM, Swearingen B, Hedley-Whyte ET, Klibanski A. Activin effects on neoplastic proliferation of human pituitary tumors. J Clin Endocrinol Metab. 2000;85:1009–1015. doi: 10.1210/jcem.85.3.6473. [DOI] [PubMed] [Google Scholar]
- 11.Reis FM, Luisi S, Carneiro MM, Cobellis L, Federico M, Camargos AF, Petraglia F. Activin, inhibin and the human breast. Mol Cell Endocrinol. 2004;225:77–82. doi: 10.1016/j.mce.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 12.Ho J, de Guise C, Kim C, Lemay S, Wang XF, Lebrun JJ. Activin induces hepatocyte cell growth arrest through induction of the cyclin-dependent kinase inhibitor p15INK4B and Sp1. Cell Signal. 2004;16:693–701. doi: 10.1016/j.cellsig.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Kleeff J, Ishiwata T, Friess H, Buchler MW, Korc M. Concomitant over-expression of activin/inhibin beta subunits and their receptors in human pancreatic cancer. Int J Cancer. 1998;77:860–868. doi: 10.1002/(sici)1097-0215(19980911)77:6<860::aid-ijc11>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 14.Thomas TZ, Wang H, Niclasen P, O'Bryan MK, Evans LW, Groome NP, Pedersen J, Risbridger GP. Expression and localization of activin subunits and Follistatins in tissues from men with high grade prostate cancer. J Clin Endocrinol Metab. 1997;82:3851–3858. doi: 10.1210/jcem.82.11.4374. [DOI] [PubMed] [Google Scholar]
- 15.Woodruff TK. Role of inhibins and activins in ovarian cancer. Cancer Treat Res. 2002;107:293–302. doi: 10.1007/978-1-4757-3587-1_14. [DOI] [PubMed] [Google Scholar]
- 16.Yoshinaga K, Yamashita K, Mimori K, Tanaka F, Inoue H, Mori M. Activin a causes cancer cell aggressiveness in esophageal squamous cell carcinoma cells. Ann Surg Oncol. 2008;15:96–103. doi: 10.1245/s10434-007-9631-1. [DOI] [PubMed] [Google Scholar]
- 17.Rahimi RA, Leof EB. TGF-beta signaling: a tale of two responses. J Cell Biochem. 2007;102:593–608. doi: 10.1002/jcb.21501. [DOI] [PubMed] [Google Scholar]
- 18.Roberts AB, Wakefield LM. The two faces of transforming growth factor beta in carcinogenesis. Proc Natl Acad Sci U S A. 2003;100:8621–8623. doi: 10.1073/pnas.1633291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xiao L, Yuan X, Sharkis SJ. Activin A maintains self-renewal and regulates fibroblast growth factor, Wnt, and bone morphogenic protein pathways in human embryonic stem cells. Stem Cells. 2006;24:1476–1486. doi: 10.1634/stemcells.2005-0299. [DOI] [PubMed] [Google Scholar]
- 20.Katoh M. Network of WNT and Other Regulatory Signaling Cascades in Pluripotent Stem Cells and Cancer Stem Cells. Curr Pharm Biotechnol. 2011;12:160–170. doi: 10.2174/138920111794295710. [DOI] [PubMed] [Google Scholar]
- 21.Lewis MT. The more things change… the more things change: developmental plasticity of tumor-initiating mammary epithelial cells. Breast Cancer Res. 2010;12:101. doi: 10.1186/bcr2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kowanetz M, Valcourt U, Bergstrom R, Heldin CH, Moustakas A. Id2 and Id3 define the potency of cell proliferation and differentiation responses to transforming growth factor beta and bone morphogenetic protein. Mol Cell Biol. 2004;24:4241–4254. doi: 10.1128/MCB.24.10.4241-4254.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rotzer D, Krampert M, Sulyok S, Braun S, Stark HJ, Boukamp P, Werner S. Id proteins: novel targets of activin action, which regulate epidermal homeostasis. Oncogene. 2006;25:2070–2081. doi: 10.1038/sj.onc.1209230. [DOI] [PubMed] [Google Scholar]
- 24.Edgar R, Domrachev M, Lash AE. Gene Expression Omnibus: NCBI gene expression and hybridization array data repository. Nucleic Acids Res. 2002;30:207–210. doi: 10.1093/nar/30.1.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kupershmidt I, Su QJ, Grewal A, Sunaresh S, Halperin I, Flynn J, Shekar M, Wang H, Park J, Cui W, Wall GD, Wisotzkey R, Alag S, Akhtari S, Ronaghi M. Ontology-based meta-analysis of global collections of high-throughput public data. PLoS One. 2010;29:e13066. doi: 10.1371/journal.pone.0013066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee JJ, Natsuizaka M, Ohashi S, Wong GS, Takaoka M, Michaylira CZ, Budo D, Tobias JW, Kanai M, Shirakawa Y, Naomoto Y, Klein-Szanto AJ, Haase VH, Nakagawa H. Hypoxia activates the cyclooxygenase-2-prostaglandin E synthase axis. Carcinogenesis. 2010;31:427–434. doi: 10.1093/carcin/bgp326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Su H, Hu N, Yang HH, Wang C, Takikita M, Wang QH, Giffen C, Clifford R, Hewitt SM, Shou JZ, Goldstein AM, Lee MP, Taylor PR. Global gene expression profiling and validation in esophageal squamous cell carcinoma and its association with clinical phenotypes. Clin Cancer Res. 2011;17:2955–2966. doi: 10.1158/1078-0432.CCR-10-2724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eijken M, Swagemakers S, Koedam M, Steenbergen C, Derkx P, Uitterlinden AG, van der Spek PJ, Visser JA, de Jong FH, Pols HA, et al. The activin A-Follistatin system: potent regulator of human extracellular matrix mineralization. FASEB J. 2007;21:2949–2960. doi: 10.1096/fj.07-8080com. [DOI] [PubMed] [Google Scholar]
- 29.Fuchs E, Horsley V. More than one way to skin. Genes Dev. 2008;22:976–985. doi: 10.1101/gad.1645908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seery JP. Stem cells of the oesophageal epithelium. J Cell Sci. 2002;115:1783–1789. doi: 10.1242/jcs.115.9.1783. [DOI] [PubMed] [Google Scholar]
- 31.Squier CA, Kremer MJ. Biology of oral mucosa and esophagus. J Natl Cancer Inst Monogr. 2001:7–15. doi: 10.1093/oxfordjournals.jncimonographs.a003443. [DOI] [PubMed] [Google Scholar]
- 32.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics 2014. A Cancer Journal for Clinicians. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 33.Yoshinaga K, Mimori K, Yamashita K, Utsunomiya T, Inoue H, Mori M. Clinical significance of the expression of activin A in esophageal carcinoma. Int J Oncol. 2003;22:75–80. [PubMed] [Google Scholar]
- 34.Yoshinaga K, Inoue H, Utsunomiya T, Sonoda H, Masuda T, Mimori K, Tanaka Y, Mori M. N-cadherin is regulated by activin A and associated with tumor aggressiveness in esophageal carcinoma. Clin Cancer Res. 2004;10:5702–5707. doi: 10.1158/1078-0432.CCR-03-0262. [DOI] [PubMed] [Google Scholar]
- 35.Yoshinaga K, Yamashita K, Mimori K, Tanaka F, Inoue H, Mori M. Activin a causes cancer cell aggressiveness in esophageal squamous cell carcinoma cells. Ann Surg Oncol. 2008;15:96–103. doi: 10.1245/s10434-007-9631-1. [DOI] [PubMed] [Google Scholar]
- 36.Yoshinaga K, Mimori K, Inoue H, Kamohara Y, Yamashita K, Tanaka F, Mori M. Activin A enhances MMP-7 activity via the transcription factor AP-1 in an esophageal squamous cell carcinoma cell line. Int J Oncol. 2008;33:453–459. [PubMed] [Google Scholar]
- 37.Sanford LP, Ormsby I, Gittenberger-de Groot AC, Sariola H, Friedman R, Boivin GP, Cardell EL, Doetschman T. TGFbeta2 knockout mice have multiple developmental defects that are non-overlapping with other TGFbeta knockout phenotypes. Development. 1997;124:2659–2670. doi: 10.1242/dev.124.13.2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hempen PM, Zhang L, Bansal RK, Iacobuzio-Donahue CA, Murphy KM, Maitra A, Vogelstein B, Whitehead RH, Markowitz SD, Willson JK, et al. Evidence of selection for clones having genetic inactivation of the activin A type II receptor (ACVR2) gene in gastrointestinal cancers. Cancer Res. 2003;63:994–999. [PubMed] [Google Scholar]
- 39.Su GH, Bansal R, Murphy KM, Montgomery E, Yeo CJ, Hruban RH, Kern SE. ACVR1B (ALK4, activin receptor type 1B) gene mutations in pancreatic carcinoma. Proc Natl Acad Sci U S A. 2001;98:3254–3257. doi: 10.1073/pnas.051484398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kodach LL, Wiercinska E, de Miranda NF, Bleuming SA, Musler AR, Peppelenbosch MP, Dekker E, van den Brink GR, van Noesel CJ, Morreau H, et al. The bone morphogenetic protein pathway is inactivated in the majority of sporadic colorectal cancers. Gastroenterology. 2008;134:1332–1341. doi: 10.1053/j.gastro.2008.02.059. [DOI] [PubMed] [Google Scholar]
- 41.Sekiya T, Adachi S, Kohu K, Yamada T, Higuchi O, Furukawa Y, Nakamura Y, Nakamura T, Tashiro K, Kuhara S, et al. Identification of BMP and activin membrane-bound inhibitor (BAMBI), an inhibitor of transforming growth factor-beta signaling, as a target of the beta-catenin pathway in colorectal tumor cells. J Biol Chem. 2004;279:6840–6846. doi: 10.1074/jbc.M310876200. [DOI] [PubMed] [Google Scholar]
- 42.Fritzmann J, Morkel M, Besser D, Budczies J, Kosel F, Brembeck FH, Stein U, Fichtner I, Schlag PM, Birchmeier W. A colorectal cancer expression profile that includes transforming growth factor beta inhibitor BAMBI predicts metastatic potential. Gastroenterology. 2009;137:165–175. doi: 10.1053/j.gastro.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 43.Tisdale MJ. Mechanisms of cancer cachexia. Physiol Rev. 2009;330:171–179. doi: 10.1152/physrev.00016.2008. [DOI] [PubMed] [Google Scholar]
- 44.Massague J. TGFbeta in Cancer. Cell. 2008;134:215–230. doi: 10.1016/j.cell.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ren P, Chen FF, Liu HY, Cui XL, Sun Y, Guan JL, Liu ZH, Liu JG, Wang YN. High serum levels of Follistatin in patients with ovarian cancer. J Int Med Res. 2012;40:877–886. doi: 10.1177/147323001204000306. [DOI] [PubMed] [Google Scholar]
- 46.Tumminello FM, Badalamenti G, Fulfaro F, Incorvaia L, Crescimanno M, Flandina C, Sepporta MV, Leto G. Serum Follistatin in patients with prostate cancer metastatic to the bone. Clin Exp Metastasis. 2010;27:549–555. doi: 10.1007/s10585-010-9344-x. [DOI] [PubMed] [Google Scholar]
- 47.Chang KP, Kao HK, Liang Y, Cheng MH, Chang YL, Liu SC, Lin YC, Ko TY, Lee YS, Tsai CL, Wang TH, Hao SP, Tsai CN. Overexpression of activin A in oral squamous cell carcinoma: association with poor prognosis and tumor progression. Ann Surg Oncol. 2010;17:1945–1956. doi: 10.1245/s10434-010-0926-2. [DOI] [PubMed] [Google Scholar]
- 48.Chen M, Sinha M, Luxon BA, Bresnick AR, O'Connor KL. Integrin alpha6beta4 controls the expression of genes associated with cell motility, invasion, and metastasis, including S100A4/metastasin. J Biol Chem. 2009;284:1484–1494. doi: 10.1074/jbc.M803997200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ogino H, Yano S, Kakiuchi S, Muguruma H, Ikuta K, Hanibuchi M, Uehara H, Tsuchida K, Sugino H, Sone S. Follistatin suppresses the production of experimental multiple-organ metastasis by small cell lung cancer cells in natural killer cell-depleted SCID mice. Clin Cancer Res. 2008;14:660–667. doi: 10.1158/1078-0432.CCR-07-1221. [DOI] [PubMed] [Google Scholar]
- 50.Bamberger C, Schärer A, Antsiferova M, Tychsen B, Pankow S, Müller M, Rülicke T, Paus R, Werner S. Activin controls skin morphogenesis and wound repair predominantly via stromal cells and in a concentration-dependent manner via keratinoctyes. Am J Pathol. 2005;167:733–747. doi: 10.1016/S0002-9440(10)62047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saka Y, Smith JC. A mechanism for the sharp transition of morphogen gradient interpretation in Xenopus. BMC Dev. Biol. 2007;7:4. doi: 10.1186/1471-213X-7-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McDowell N, Gurdon JB. Activin as a morphogen in Xenopus mesoderm induction. Semin. Cell Dev. Biol. 1999;10:311–317. doi: 10.1006/scdb.1999.0307. [DOI] [PubMed] [Google Scholar]
- 53.Gurdon JB, Harger P, Mitchell A, Lemaire P. Activin signalling and response to a morphogen gradient. Nature. 1994;371:487–492. doi: 10.1038/371487a0. [DOI] [PubMed] [Google Scholar]
- 54.Symes K, Yordán C, Mercola M. Morphological differences in Xenopus embryonic mesodermal cells are specified as an early response to distinct threshold concentrations of activin. Development. 1994;120:2339–2346. doi: 10.1242/dev.120.8.2339. [DOI] [PubMed] [Google Scholar]
- 55.Jones CM, Armes N, Smith JC. Signalling by TGF- family members: short-range effects of Xnr-2 and BMP-4 contrast with the long-range effects of activin. Current Biology. 1996;6:1468–1475. doi: 10.1016/s0960-9822(96)00751-8. [DOI] [PubMed] [Google Scholar]
- 56.Crease DJ, Dyson S, Gurdon JB. Cooperation between the activin and Wnt pathways in the spatial control of organizer gene expression. Proc. Natl. Acad. Sci. U.S.A. 1998;95:4398–4403. doi: 10.1073/pnas.95.8.4398. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.