Abstract
Purpose
Pancreatic cancer is the fourth leading cause of cancer deaths and there currently is no reliable modality for the early detection of this disease. Here we identify cancer-specific promoter DNA methylation of BNC1 and ADAMTS1 as a promising biomarker detection strategy meriting investigation in pancreatic cancer.
Experimental Design
We used a genome-wide pharmacologic transcriptome approach to identify novel cancer-specific DNA methylation alterations in pancreatic cancer cell lines. Of 8 promising genes, we focused our studies on BNC1 and ADAMTS1 for further downstream analysis including methylation and expression. We used a nanoparticle-enabled MOB (Methylation On Beads) technology to detect early stage pancreatic cancers by analyzing DNA methylation in patient serum.
Results
We identified 2 novel genes, BNC1 (92%) and ADAMTS1, (68%) that showed a high frequency of methylation in pancreas cancers (n=143), up to 100% in PanIN-3 and 97% in Stage I invasive cancers. Using the nanoparticle-enabled MOB technology, these alterations could be detected in serum samples (n=42) from pancreas cancer patients, with a sensitivity for BNC1 of 79% (95%CI:66-91%) and for ADAMTS1 of 48% (95%CI:33-63%), while specificity was 89% for BNC1 (95%CI:76-100%) and 92% for ADAMTS1 (95%CI:82-100%). Overall sensitivity using both markers is 81% (95%CI:69-93%) and specificity is 85% (95%CI:71-99%).
Conclusions
Promoter DNA methylation of BNC1 and ADAMTS1 are potential biomarkers to detect early stage pancreatic cancers. Assaying the promoter methylation status of these genes in circulating DNA from serum is a promising strategy for early detection of pancreatic cancer and has the potential to improve mortality from this disease.
Keywords: DNA Methylation, Early detection biomarker, Pancreatic cancer, Cancer screening
Introduction
Pancreatic cancer is a deadly cancer with an overall 5-year survival rate of less than 5% and few improvements in survival over the last 3 decades.(1, 2) Pancreatic cancer currently ranks as the fourth leading cause of cancer related death in United States with an estimated 44,030 new cases and 37,660 deaths in 2011 and its incidence is rising.(3, 4) One of the major factors attributed to the dismal prognosis of pancreas cancer is delayed diagnosis such that only about 10% of patients are amenable to potential curative surgical resection.(4) However, long term 5-year survival is attainable in selected patients for whom surgical removal of early-stage disease is accomplished.(5, 6) Therefore, early detection of pancreatic cancer is thought to be the best modality for improving survival in this lethal disease.(7-10) At this time no reliable screening test currently exists for the early detection of this cancer.
Pancreatic cancer is characterized by multiple genetic and epigenetic changes.(11, 12) In recent years, it has become apparent that pancreatic cancer is as much a disease of mis-regulated epigenetics as it is a disease of DNA mutations.(11, 12) In particular, changes in DNA promoter methylation patterns could play a crucial role in tumorigenesis and cancer progression.(13) In order to address the need for both clinical diagnostics as well as therapeutics, many studies have employed DNA methylation analysis of specific genes for application in diagnostics of multiple cancers.(13, 14) Such diagnostic tests can, in principle, be used for early detection, for assessing prognosis, as predictors of response to therapy, and as a therapeutic targets. Early detection of disease results in an improved clinical outcome for most types of cancer.(15, 16) Therefore, much effort has been invested in developing efficient screening technologies for this purpose. Recently, there have been multiple successful reports of DNA methylation screening using various body fluids such as stool for detection of colorectal cancer,(17, 18) sputum for lung cancer(19) and urine for prostate cancer.(20) However, no screening tool is currently available for early detection in pancreatic cancer. This tumor type is often metastatic or locally advanced at initial diagnosis since patients often present with nonspecific gastrointestinal symptoms.(21) The development of an early stage screening modality for pancreatic cancer, for the use in particularly in high risk groups, would then have a potential impact in reducing mortality from this currently lethal disease.
Any optimal screening technology needs to be simple, easy to perform, cost-effective, noninvasive, and yield more benefit than harm. Such screening efforts have been in practice for more than a decade for a multitude of various cancers.(2) Currently, endoscopic ultrasound has shown promise as a screening tool for pancreatic cancer in high-risk patients, but it is available only in highly specialized centers and is an expensive and invasive modality that needs to be repeated at frequent intervals. (22, 23) In the current report, we now define the use of a genome-wide expression array technology to identify novel hypermethylated genes in pancreatic cancer for which assays of methylation status in serum DNA holds robust potential for early detection of this disease.
Materials and Methods
Cell culture, treatment, and transfection
Pancreatic cancer cell lines (Panc1, MIA-PaCa2, PL45, and Capan1) were obtained from ATCC and maintained under the recommended conditions. All cell lines were treated with the demethylating agent 5-aza-2’-deoxycytidine (DAC), Trichostatin-A (TSA), or saline (control), and cells were collected for DNA and RNA. DKO cells (HCT116 colon cancer cells with genetic disruption of DNMT1 and DNMT3b) were cultured as described previously. (24) Full length BNC1 cDNA was subcloned into the pIRES-neo3 expression vector. Panc-1 and MIA-PaCa2 cells were transfected with the Lipofectamine 2000 Reagent (INVITROGEN) according to the manufacturer's protocol. Panc-1 and MIA-PaCa2 cells were transfected with a control construct (empty vector) or BNC1-pIRESneo3, selected for 10 days with G418 (500μg/ml).
Gene Expression Microarray Analysis
Total RNA was harvested from log phase cells using TRIzol (Invitrogen) and the RNeasy kit (QIAGEN) according to the manufacturer's instructions, including a DNase digestion step. RNA was then used for the Agilent 4x44 genome-wide expression array. Data analysis was performed using previously reported techniques. (25)
In vitro cell proliferation, migration and invasion assays
Panc-1 and MIA-PaCa2 cells were seeded onto 96-well plates (5000 cells/well) and after 96 hours the cultures were pulsed for 6 hours with 0.3 μCi [methyl-3H] thymidine (Amersham Life Science) per well. Three independent experiments were performed. Proliferation was measured using liquid scintillation. Cell migration and invasion assays were performed using 24-well transwells (8μm pore size) coated with (invasion) or without (migration) matrigel (BD Biosciences). 20×104 Panc-1 and MIA-PaCa2 cells in 1% FBS-DMEM were seeded into the upper chamber, and DMEM containing 20% FBS was placed in the lower chamber. After 48 hours, cells on the lower surface of the membrane were fixed with methanol and stained with 1% Toluine Blue in 1% borax and the cells on the lower surface of the membrane were counted with the use of a light microscope. Transwell experiments were assessed in three replicate experiments.
Patient samples and study population
Pancreatic tissues were collected from 173 patients with formalin-fixed, paraffin-embedded (FFPE) tissues (Table 1). These included 123 tissue samples from patients with Stage I through Stage IV pancreatic cancer who underwent primary surgical resection at the Johns Hopkins Hospital (JHH) from 1998 to 2009 (median follow up of 6.4 years). For comparison, additional FFPE pancreatic tissues were obtained from patients who had undergone pancreatectomy for pancreatic cancer but had the surrounding premalignant lesion called pancreatic intraepithelial neoplasia (PanIN) (n=20) or for pancreatitis (n=30). Pathology was re-reviewed to confirm histology (C.A.I-D) (Table 1). Clinicopathologic characteristics and overall survival were checked using patient medical records. Total RNA and matched genomic DNA were obtained from 3 pancreatic cancer patient donors and 4 normal pancreatic tissue donors. (Biochain Institute, Hayward, CA)
Table 1.
Clinical information for primary pancreatic samples
| Pancreas Primary Tumors |
||||||
|---|---|---|---|---|---|---|
| Normal (N=4) | PanINs (N=20) | Stage I (N=38) | Stage II (N=78) | Stage III (N=5) | Stage IV (N=2) | |
| Median Survival (months) | 137.3 | 42.4 | 17.8 | 13.9 | 19.6 | |
| Gender | ||||||
| Male | 3 (75%) | 9 (45%) | 9 (23.7%) | 44 (57%) | 1 (20%) | 2 (100%) |
| Female | 1 (25%) | 11 (55%) | 29 (76.3%) | 34 (43%) | 4 (80%) | 0.0% |
| Grade | ||||||
| Well Differentiated | 9 (45%) | 3 (7.9%) | 4 (5.1%) | 1 (20%) | 0 (0%) | |
| Moderately Differentiated | 8 (40%) | 23 (60.5%) | 41 (52%) | 4 (40%) | 1 (50%) | |
| Poorly Differentiated | 3 (15%) | 12 (31.6%) | 33 (42.9%) | 4 (40%) | 1 (50%) | |
Pre-operative CA 19-9 levels were investigated in our patient population. 45.1% of patients in our cohort had pre-operative CA 19-9 levels measured. The range for normal CA 19-9 at our institution is 0-36 U/mL and values greater than 36 was considered elevated and abnormal.
DNA Methylation Analysis
Primer pairs for methylation analysis were designed using MSPPrimer (http://www.mspprimer.org). All primer sequences are listed in Supplementary Table S1. DNA was extracted using the standard phenol-chloroform extraction method. Bisulfite modification of genomic DNA was carried out using the EZ DNA Methylation Kit (Zymo Research). Conventional methylation-specific PCR (MSP) was then performed as previously described on all FFPE samples. (26)
Quantitative methylation specific PCR (qMSP) was performed on all cell lines and FFPE tissues from normal pancreas, (n=14) chronic pancreatitis (n=30), PanIN (n=20) and pancreatic tumors (n=12). The Power SYBR Green PCR kit (Applied Biosystems) was used and the amplification conditions consisted of an initial 10-min denaturation step at 95 °C, followed by 40 cycles of denaturation at 95 °C for 15 s and annealing and extension for 30 s and 60 s, respectively. An ABI StepOnePlusReal-Time PCR System was used (Applied Biosystems), and for quantification the comparative cycle threshold (Ct) method was used, normalizing the Ct values for the indicated gene to the Ct values of unmethylated reaction relative to a methylated reaction sample.
Gene expression Analysis
Quantitative expression (qPCR) analysis was performed on all cell lines and samples with matched total RNA and genomic DNA. Expression primers were designed using the open access program Primer3 (http://frodo.wi.mit.edu/primer3). Total RNA was extracted using the RNeasy Mini Kit (QIAGEN), treated with DNase (QIAGEN). Superscript III first strand cDNA synthesis kit (Invitrogen) was used according to the manufacturer's instructions. Expression analysis was performed by qPCR using 1μl of cDNA as template and JumpStart Red Taq DNA Polymerase (SIGMA) for amplification. Quantification of the Ct method was used, normalizing the Ct values for the indicated gene to the Ct values of GAPDH relative to that of the mean of 4 normal pancreas samples.(27)
Pancreatic cancer patient serum samples
Patient serum samples were obtained from individuals with pancreatic cancer prior to undergoing surgical treatment at the JHH after obtaining informed consent from 2007 to 2009. Matching tumor samples were drawn from the pathology archives of the JHH in accordance with all rules and regulations of the Institutional Review Board (IRB) and as per HIPAA compliance. A total of 42 serum samples were tested from patients with invasive pancreas cancers and 23 of which had matching FFPE tissue available. Additionally, 26 serum samples were obtained from normal, healthy volunteers to serve as controls.
Methylation On Beads (MOB) method
MOB is a recently developed nanotechnology that permits capture, retention, and bisulfite treatment of minute amounts of DNA. (28) This type methodology is ideal for examining DNA in body fluids including stool, sputum and serum. MOB was performed as previously described.(29, 30) DNA methylation was detected as described above.
Statistical analysis
Unless otherwise noted, experiments were carried out in triplicate and data are presented as the mean± standard margin of error (SEM). For quantitative MSP analysis, BNC1 and ADAMSTS1 promoter methylation was considered positive if the methylation value was greater than twice that of the average of 4 normal pancreas samples. The Student t-test was used for analyses of [3H]thymidine incorporation and anchorage-independent cell growth. The Mann–Whitney rank sum test was used to analyze data obtained in the colony formation, migration, and invasion assays. All p-values are two-sided, and p-values less than or equal to 0.05 were considered statistically significant. Statistical calculations were carried out using GraphPad Prism4 software.
The Cancer Genome Atlas Analysis
Forty pancreatic cancer samples were publically available in The Cancer Genome Atlas (TCGA) with matched expression data via RNAseq version 2 and methylation data via the Illumina Infinium 450K platform. Level 3 data, which is normalized by TCGA, was used for analysis. Linear regression modeling was used to fit the data and a pair-wise, two-sided Pearson's correlation coefficient was calculated and graphed using R: A language and environment for statistical computing. (31)
Results
Identification of cancer-specific promoter DNA methylation in pancreatic cancer
To identify novel DNA methylation biomarkers in pancreatic cancer, we used our previously established human transcriptome-wide microarray screen in four different human pancreatic cancer cell lines (PL45, MIA-PaCa2, Panc1, and Capan1) to detect genes silenced by promoter hypermethylation (25). This assay employs a genome-wide pharmacologic strategy using DAC and TSA to re-express genes silenced in association with abnormal promoter CpG island DNA methylation.(25, 32) We initially identified a total of 1,427 unique genes in all four cell lines which met the criteria for candidate hypermethylated genes in the pancreatic cancer cell lines (Supplementary Fig. S1)
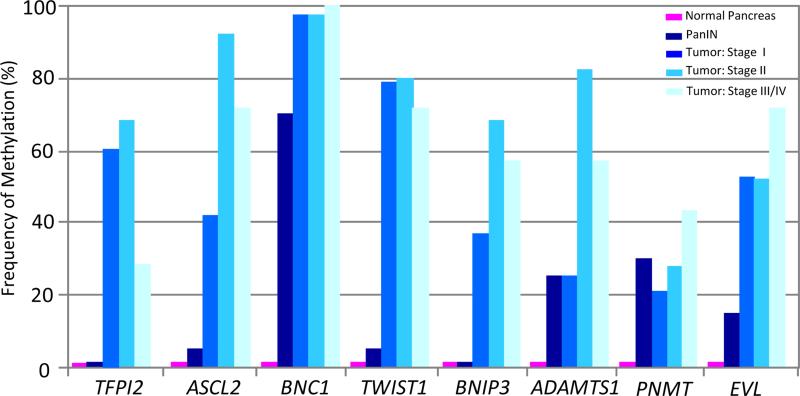
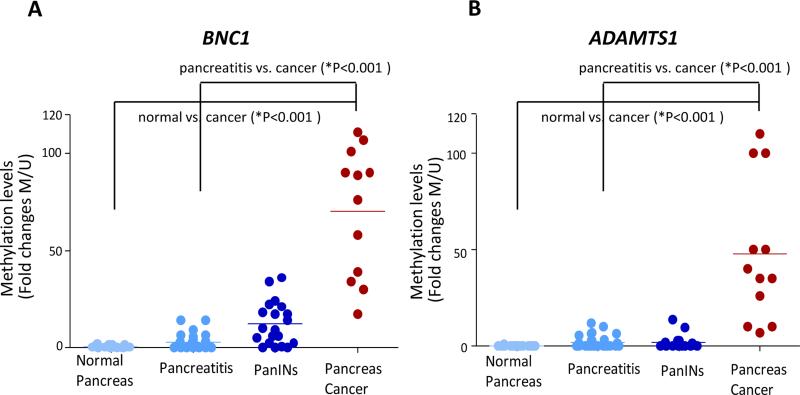
In order to filter down to genes that only showed cancer specific methylation, we used the following experimental validation criteria based on our prior studies (33): 1) methylation in pancreas cancer cell lines associated with loss of expression; 2) presence of gene expression in normal pancreas tissue; 3) no or low methylation in normal pancreatic tissues (cancer-free tissues); and 4) methylation present in primary pancreatic cancers. Eight genes (TFPI2, ASCL2, BNC1, TWIST1, BNIP3, ADAMTS1, PNMT, and EVL) fulfilled the above criteria on our initial screen, displaying cancer-specific methylation in primary pancreatic cancers (Fig. 1).
Fig. 1.
Methylation frequencies of the 8 genes in a series of pancreatic cancer patients (stage I-IV; n=147); along with normal pancreas from non-cancerous patients (n=4) and pancreatic intraepithelial neoplasia (PanIN) (n=20; ranging from PanIN-1 to -3).
BNC1 and ADAMTS1: Potential DNA methylation biomarker for early detection of pancreatic cancer
We examined the methylation status of all eight of our candidate genes in a large series of primary pancreatic tumor samples, (n=123; Stages 1-4; Table 1), normal pancreas (n=4) and premalignant PanINs (n=20) by MSP. The most frequently methylated gene was BNC1 (91%), followed by ADAMTS1 (67%), TWIST1 (67%), ASCL2 (65%), BNIP3 (49%), TFPI2 (54%), EVL (47%), and PNMT (27%) (Fig. 1). Interestingly, two of the genes, BNC1 (91%) and ADAMTS1 (67%) that demonstrated frequent methylation in this cohort of primary pancreatic cancer samples also showed frequent methylation in the precursor lesions of pancreatic cancer, PanIN lesion (BNC1: 70% (14/20); ADAMTS1: 25% (5/20), respectively) (Fig. 1).
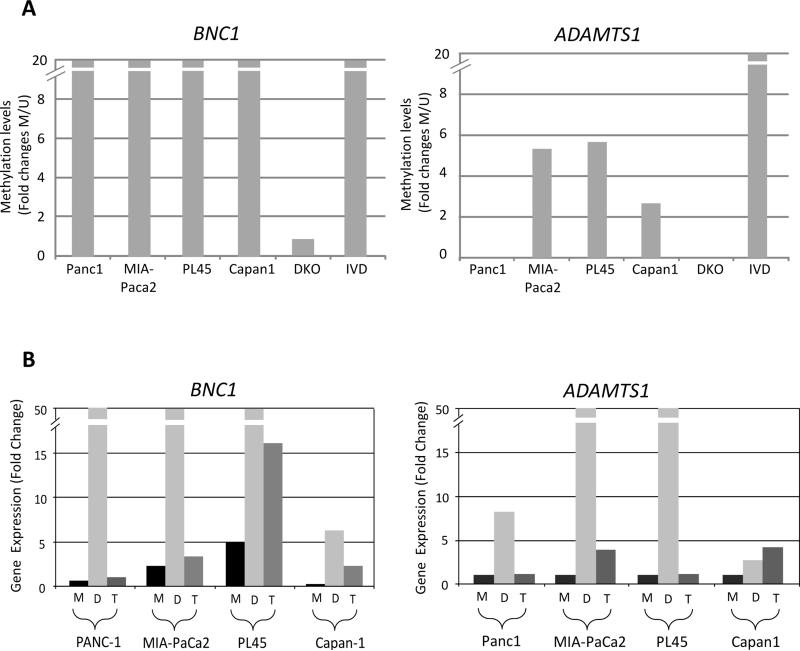
We verified the abnormal methylation status of BNC1 and ADAMTS1 through quantitative MSP analyses (Fig. 2A) and correlated this with expression patterns for these genes by qPCR (Fig. 2B). Both genes showed lack of endogenous gene expression and significant re-expression after DAC treatment in these cell lines. Treatment with a histone deacetylase inhibitor such as TSA resulted in minimal re-expression except in PL45 for BNC1 which may be regulated both by promoter DNA methylation and histone modifications (Fig. 2B). We also confirmed promoter-associated CpG island methylation in the BNC1 and ADAMTS1 promoter by bisulfite sequencing analysis in pancreatic cancer cell lines, primary pancreas cancer samples normal pancreatic tissue and in the DNMT1(−/−) DNMT3B(−/−) double knockout (DKO) which serves as a negative control. These analyses revealed dense methylation of both BNC1 and ADAMTS1 in the pancreatic cancer cell line and the primary pancreatic cancer and minimal or no methylation in normal pancreas samples and in DKO. These results are all consistent with our conventional and quantitative MSP analyses (Fig. 2. C and D).
Fig. 2.
(A-B) Silencing of BNC1 and ADAMTS1 genes in pancreatic cancer cell lines. (A) qMSP analysis of BNC1 and ADAMTS1 gene promoter region and correlation with (B) gene expression by qPCR in pancreatic cancer cell lines. IVD= in vitro methylated DNA. DKO=double knockout (DKO) HCT116 cells (DNMT1−/− and DNMT3b−/−). Quantitative PCR expression is shown as fold change ± standard error relative to mock-treated (M) cells during 5 μM 5-Aza-2’-deoxycytidine (DAC; D) and 300 nM Trichostatin A (TSA; T) treatments. Normal pancreas and DKO cells were used as controls. (C-D) Bisulfite sequencing analysis of CpG island in (C) BNC1 and (D) ADAMTS1 gene promoter region. Bisulfite sequencing analysis of the BNC1 (for Panc1) and ADAMTS1 (for MIA-PaCa2) genes in a pancreatic cancer cell line, a primary pancreatic cancer (stage II), normal pancreatic tissue and DKO cell line as a negative control. Open circles represent unmethylated CpG sites and filled circles represent methylated CpG sites with each row representing a single clone. TIS indicate transcriptional start site. Location of CpG sites (BST: upstream region from −331 to +36 for BNC1, +22 to +207 for ADAMTS1 relative to transcriptional start site). The red and blue bars represent MSP amplification and bisulfite amplification region, respectively.
Little is known about the role of epigenetic alterations in the precursor lesions of pancreatic cancer even though defining the timing of prevalence of DNA methylation events would be critical information for understanding pancreatic carcinogenesis, for early pancreatic cancer detection as well as for identification of novel targets for chemoprevention.(34) Identification of precursor lesions such as PanIN (or pancreatic carcinoma in situ) is thought to represent one of the best targets available for early detection and chemoprevention strategies for pancreatic cancer.(35) Specifically, BNC1 was also methylated in the tissues of PanIN-1 (5/9, 56%), PanIN-2 (6/8, 75%), and PanIN-3 (3/3, 100%) during PanIN progression (data not shown).
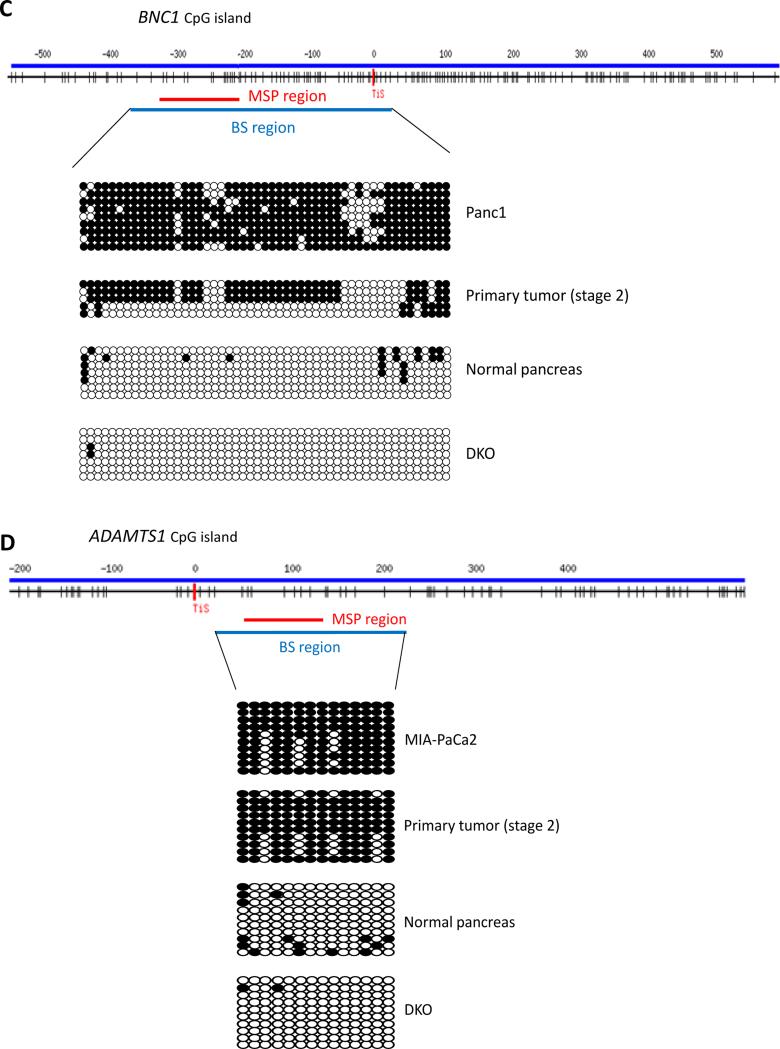
Next, we collected and analyzed a subset of tissue samples from patients diagnosed with non-cancerous diseases such as pancreatitis that may have confounding effects for using BNC1 and ADAMTS1 methylation status for early detection of pancreatic cancer. Patients with chronic pancreatitis are at a two- to 26-fold increased risk for developing pancreatic cancer.(4) However, chronic inflammatory conditions may also increase the frequency of methylation as a field defect which may then increase risk of subsequent malignancy.(36-38) We compared methylation of BNC1 and ADAMTS1 between different conditions (normal, pancreatitis, PanIN, and invasive cancers) using MSP analysis. As shown in Fig. 3, BNC1 (A) and ADAMTS1 (B) show statistically increased frequency of methylation when comparing normal pancreas tissues and invasive cancers (p<0.001; both BNC1 and ADAMTS1) as well as between chronic pancreatitis and invasive cancers (p<0.001, both BNC1 and ADAMTS1). There is a low frequency of BNC1 and ADAMTS1 methylation present in non-cancerous disease such as pancreatitis. More interestingly, there is significant quantitative difference between PanINs and invasive cancers on both genes (p<0.001 both BNC1 and ADAMTS1). However, BNC1 methylation could be detected in the earliest stages of pancreatic carcinogenesis such as PanIN-1, unlike the patterns seen for ADAMTS1 methylation whereby ADAMTS1 methylation is only seen in invasive cancers (data not shown), suggesting that the use of both genes may be optimal to determine the presence of invasive pancreatic cancer.
Fig. 3.
Quantitative MSP (qMSP) analysis of BNC1 and ADAMTS1 using real-time PCR. Normal pancreas (n=4 normal tissues, n=10 surrounding normal tissues), chronic pancreatitis samples (n=30), PanIN 1-3 (n=20), and stage II tumors (n=12), respectively. qMSP showed significantly increased frequency of methylation when comparing normal pancreas tissues and invasive cancers (p<0.001; both BNC1 and ADAMTS1) as well as between chronic pancreatitis and invasive cancers (p<0.001, both BNC1 and ADAMTS1). qMSP is shown as fold change for methylated signal relative to unmethylated signal. In qMSP analysis, signals for unmethylated (U) and methylated (M) DNA are shown for each sample. Horizontal bar indicates mean methylation level.
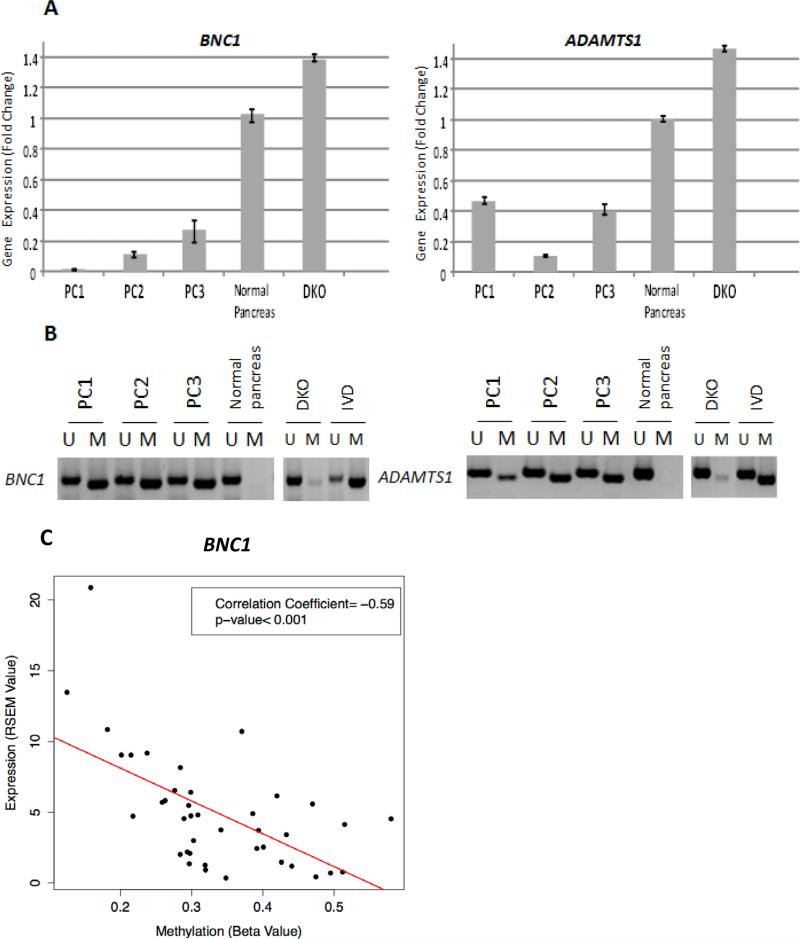
Correlation of BNC1 and ADAMTS1 methylation and gene expression in pancreas cancer
We examined whether methylation of promoter-associated CpG-islands of BNC1 and ADAMTS1 is associated with gene silencing by investigating BNC1 and ADAMTS1 mRNA expression in fresh pancreatic cancer tissues (n=4). Both BNC1 and ADAMTS1 mRNA levels in primary pancreatic cancers were significantly downregulated or silenced compared to normal pancreas mRNA as well as in DKO cells (p<0.001 BNC1 and ADAMTS1, t-test) (Fig. 4A). We also confirmed, by MSP analysis, that the down-regulation of gene expression was associated with DNA methylation of BNC1 and ADAMTS1 in these primary pancreas cancers. Normal pancreas had no methylation of either gene but expressed both genes (Fig. 4B). Investigation of methylation and expression in the larger TCGA dataset revealed ADAMTS1 did not have an adequate number of CpG island probes for evaluation. BNC1 methylation and expression were inversely correlated (correlation coefficient = −0.59, p-value <0.001) (Fig. 4C).
Fig. 4.
Down-regulation of BNC1 and ADAMTS1 gene expression in primary pancreas cancers. (A) Quantitative mRNA gene expression and (B) DNA methylation analysis of BNC1 and ADAMTS1 in pancreas cancers using qPCR and MSP analysis. PC1-3 indicates primary pancreatic cancer samples. Normal pancreas was used as a control. Expression and methylation are matched from each individual samples. MSP analysis, signals for unmethylated (U) and methylated (M) DNA are shown for each sample. IVD= in vitro methylated DNA. DKO=double knockout HCT116 cells (DNMT1−/− and DNMT3b−/). C) Correlation between methylation and expression in 41 samples from The Cancer Genome Atlas for BNC1. The solid line indicates the linear regression model for all points.
We also investigated the expression of BNC1 and ADAMTS1 in larger cohorts of primary pancreas cancers using previously published gene expression microarray data previously in Oncomine™(Compendia Bioscience, Ann Arbor, MI). The Oncomine™ database is a web-based data-mining platform aimed at facilitating gene discovery from genome-wide expression analyses in cancer (39). Interestingly, we found that both BNC1 and ADAMTS1 are significantly down-regulated in multiple independent primary pancreas cancers gene expression array data sets (Supplementary Table S2).
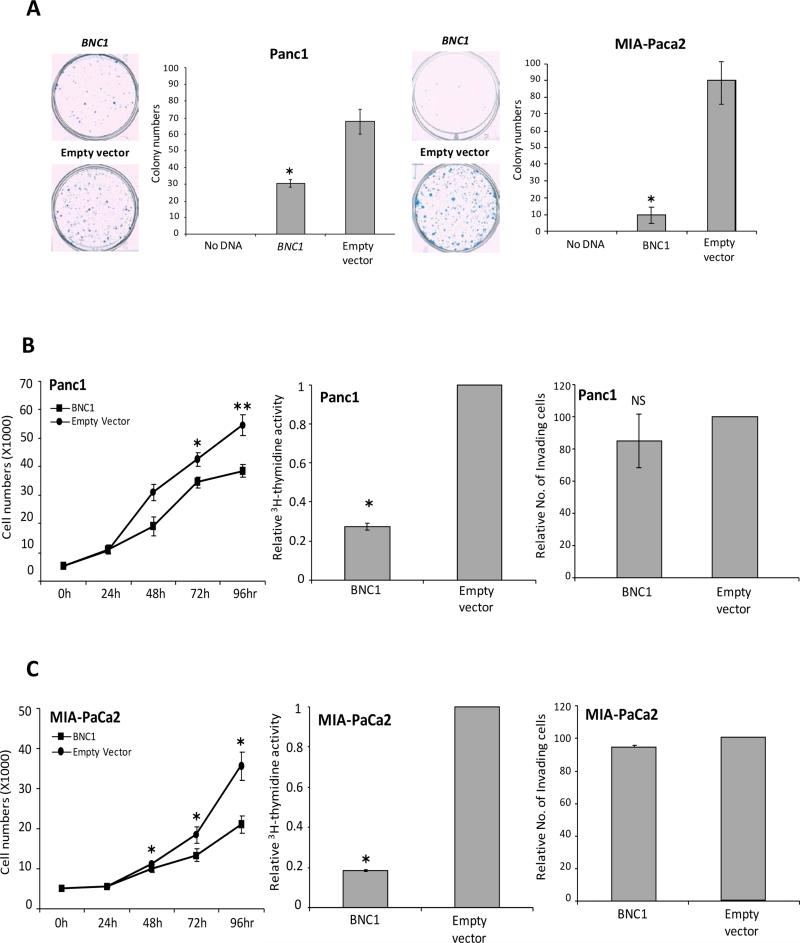
Tumor suppressive effects of BNC1 gene over-expression in pancreatic cancer cells
Since BNC1 appeared to be the most promising biomarker for early detection of pancreas cancer, we investigated whether this gene possesses tumor suppressive effects in pancreatic cancer cells in vitro. We transfected full-length BNC1 into Panc1 and MIA-PaCa2 cells lacking BNC1 expression (Supplementary Fig. S2). We then performed in vitro colony formation assays and found over-expression with BNC1 full-length gene induced a nearly 2.2-fold (Panc1) and 9-fold (MIA-PaCa2) reduction of G418-resistant colonies (Fig. 5A). In addition, there was a 73% (Panc1) and 82% (MIA-PaCa2) decrease in cell proliferation as measured by [3H] thymidine activity (Fig. 5B and 5C; left and middle panel). However, overexpression of BNC1 gene, as compared with control cells transfected with empty vector, had no effect on the migration and invasion capacities of Panc1 and MIA-PaCa2 cells as examined in the matrigel-coated transwell membrane assay (Fig. 5B and 5C; right panel). Taken together, these data suggest that BNC1 may have tumor-suppressive effects in human pancreatic cancer cells in vitro.
Fig. 5.
Functional assays of BNC1 gene in pancreatic cancer cells. (A) Colony formation in Panc1 and MIA-PaCa2 cells transfected with pcDNA3.1 or BNC1-pcDNA3.1 and grown for 2 weeks in medium containing G418. Results are plotted as the mean colony numbers relative to pcDNA3.1 transfectants in three independent experiments (Panc1; *p=0.0275, MIA-PaCa2; *p=0.0294). (B) Cell proliferation and invasion assays in Panc1 cells (C) Cell proliferation and invasion assays in MIA-PaCa2 cells. Left panel: BNC1 transfected Panc1 cells (BNC1-pcDNA3.1) were compared with control cells transfected with empty vector (pcDNA3.1). Results are plotted as the mean cells number in three different independent experiments (Panc1; *p=0.0469; 72 hrs, **p=0.0086; 96hrs: MIA-PaCa2, *p=0.0469; 48hrs, *p=0.0318; 72hrs, *p=0.0389; 96hrs). Middle panel: Cell proliferation measured by 3H-thymidine incorporation (Panc1; *p=0.0286, MIA-PaCa2; *p=0.0256). Right panel: Invasion of Panc1 and MIA-PaCa2 cells through matrigel-coated transwells relative to control cells transfected with empty vector in three independent experiments (NS: not statistically significant).
Detection of DNA methylation in pancreatic cancer patient sera using MOB technology
Since no reliable blood-based screening test exists for patients at high risk of pancreas cancer, the development of a non-invasive modality for cancer detection may improve mortality in this aggressive cancer.(40, 41) Recently, many studies have suggested that cancer-specific DNA methylation patterns can be found in detached tumor cells in bodily fluids and biopsies, or in free-floating DNA from cancer patients.(14, 42) Therefore, we examined, as a pilot study, whether we can detect presence of BNC1 and ADAMTS1 promoter DNA methylation in pancreatic cancer patient sera. We used a highly-sensitive nano-enabled assay, termed Methylation On Beads (MOB), which we have recently developed to improve the sensitivity of methylation detection (28). MOB incorporates DNA isolation and bisulfite conversion in a single tube process which minimizes the loss of sample and risk of contamination associated with separate processes.
We tested serum samples from a series of pancreatic cancer patients, stages I-IV (n=42) as well as a panel of sera from normal healthy individuals (n=26). Sensitivity was determined based on the stringent assumption that all patients with pancreas cancer would have DNA methylation of BNC1 and ADAMTS1 while the genes would be unmethylated in all healthy normal volunteers. We found that serum samples from 33 of the 42 patients with cancer had methylation for BNC1, while 20 of the 42 showed methylation for ADAMTS1. Overall, for all stages included, the sensitivity was determined to be 79% and 48% for BNC1 and ADAMTS1 respectively. Sensitivity of detection of stage I pancreatic cancers was 90% for both genes. Amongst the 26 normal serum samples, 3 of the normal samples showed methylation for BNC1 while 2 showed methylation for ADAMTS1. Specificity of detection was determined to be 89% for BNC1 and 92% for ADAMTS1 (Table 2). Use of both genes together for early detection improved sensitivity (81%, 95%CI: 69% to 93%) but not specificity (85%, 95%CI: 71% to 99%) compared to single gene methylation detection. Results in the corresponding FFPE tissue samples of pancreas cancer were higher for both genes, with 100% sensitivity and specificity for BNC1 and 79.2% sensitivity and 100% specificity for ADAMTS1.
Table 2.
Sensitivity and specificity of BNC1 and ADAMTS1 in pancreatic cancer patient serum samples
| BNC1 | ADAMTS1 | ||||
|---|---|---|---|---|---|
| Pancreatic Cancer |
Sensitivity(%)
|
||||
| Stage | n | Estimated Value | 95% CI | Estimated Value | 95% CI |
| I | 10 | 90% (9/10) | 90% (9/10) | ||
| II-IV | 32 | 75% (24/32) | 34% (11/32) | ||
| Total | 42 | 79% (33/42) | 66-91% | 48% (20/42) | 33-63% |
|
Specificity(%)
|
|||||
|---|---|---|---|---|---|
| Estimated Value | 95% CI | Estimated Value | 95% CI | ||
| Normal | 26 | 89% | 76-100% | 92% | 82-100% |
CI- confidence interval
DISCUSSION
In this study we used a genome-wide pharmacological approach to identify methylation of cancer-specific genes in pancreatic cell lines. We have used such an approach previously in both colorectal and breast cancer.(17, 25, 43) Defining the DNA hypermethylome has been useful to identify not only novel DNA methylation biomarker candidates but also tumor suppressor gene candidates.(33) DNA methylation biomarkers have obvious applications in diagnostics,(17, 18, 33) but can also contribute indirectly to therapeutics as predictors of response to therapy. (28) We initially identified 1,427 genes that are potentially silenced by DNA methylation in pancreatic cancer and then focused on those genes demonstrating cancer-specific methylation in primary tumors.(25) In-depth analysis was limited to BNC1 and ADAMTS1 which showed the highest frequency of methylation at 91.8% and 66.7%, respectively, in pancreatic cancer samples. Basonuclin (BNC1) is a zinc-finger transcription factor that interacts with the promoters of both RNA polymerases I and II. Bioinformatic analysis suggests that basonuclin target genes may be implicated in chromatin structure, transcription/DNA-binding, adhesion/cell–cell junction, signal transduction and intracellular transport.(44) Little is known about the biological role for BNC1 in human cancers. A recent report showed methylation of BNC1 in lung cancers suggested that silencing of BNC1 by promoter methylation might be of relevance to the diagnosis and management of cancers and also suggesting its biological role as a tumor suppressor gene (45). Indeed, we find that over-expression of BNC1 in the pancreatic cancer cell lines Panc1 and MIA-PaCa2 inhibited colony formation and cell proliferation in vitro. ADAMTS1 (A Disintegrin-like Metalloproteinase with Thrombospondin type 1 motif, 1), which is the prototypic member of the ADAMTS family, is widely expressed in various human tissues.(46) ADAMTS1 has been shown to be down-regulated in colorectal, breast, non-small cell lung cancer, prostate cancer, and pancreatic cancers.(47-51) In addition, it has been shown ADAMTS1 might have anti-angiogenic activity in cells (49). Our studies also show that we found that methylated ADAMTS1 was associated with a worse overall survival as compared to unmethylated ADAMTS1. This was significant by log-rank analysis (p=0.03) as well as by univariate Cox regression analysis (ADAMTS1 Unmethylated as reference, ADAMTS1 Methylated- Odds Ratio 1.6; Confidence Interval 1.03-2.52; p=0.03). (Supplementary Fig. S3)
Our principal goal in this study was to identify new genes in pancreatic cancer demonstrating tumor-specific methylation which could serve as early detection biomarkers. The poor accessibility of the pancreas along with the late presentation of symptoms have thwarted attempts at timely detection of this malignancy and contributes to high mortality rates such that pancreas cancer remains the fourth leading cause of cancer death in both men and women. (53) There have been limited improvements in the mortality from this disease over the past 30 years. (54) However, cancers such as breast and colorectal cancers, where screening has been in practice for early detection, have seen a decrease in cancer mortality (55). Therefore, development of cancer biomarkers for pancreatic cancer is the best hope for early detection and potentially improving mortality from this lethal cancer (14).
Prior studies have identified possible targets for aberrant DNA methylation in pancreatic cancers. Identification of PanIN using methylation patterns was described by Sato and colleagues with methylation frequency ranging from 13-30% for a panel of genes and suggested that their set of genes might also be utilized for early detection.(56) Herein, we suggest that promoter methylation of BNC1 and ADAMTS1 may comprise a more promising method of detection of early stage pancreatic cancer as they provide a much greater sensitivity. To our knowledge, BNC1 and ADAMTS1 have not been previously described as a DNA methylation biomarkers in pancreatic cancers. In addition, we saw that methylation of these genes were able to detect early stage pancreatic cancers at higher frequencies than the current blood-based test, CA 19-9. In detail, the median CA 19-9 for all patients was 114.5 U/mL. The rate of abnormal and elevated CA 19-9 in all invasive cancers was 70%. This increased with increasing stage. 52% of Stage I cancers had an elevated CA 19-9. This increased to 73.7% of Stage II cancers and 100% of Stage III and IV cancers. In all instances the combination of methylation of ADAMTS1 and BNC1 showed improved sensitivity compared to CA 19-9. (Table 3) This suggests that methylation of these genes may be useful for screening of high risk individuals including patients with patients with family history of pancreatic cancer, hereditary pancreatitis, familial syndromes such as BRCA1/2 mutation families, Peutz-Jeghers syndrome or hereditary nonpolyposis colorectal cancer, cystic fibrosis or familial atypical multiple mole syndrome (57).
Table 3.
Comparison of BNC1 and ADAMTS1 methylation and CA 19-9
| Stage | BNC1 | ADAMTS1 | ADAMTS1 and BNC1 Combined | CA 19-9 |
|---|---|---|---|---|
| PanIN (n=20) | 70% | 25% | 75% | 20% |
| Stage I (n=38) | 97% | 63% | 97% | 52% |
| Stage II (n=78) | 96% | 82% | 96% | 73.7% |
| Stage III & IV (n=7) | 100% | 57% | 100% | 100% |
The rates of methylation for either BNC1, ADAMTS1 or BNC1 or ADAMTS1 were identified for PanIN and invasive pancreatic cancers, Stage I, Stage II, and Stage III&IV. Any methylation was considered to be a positive test. CA 19-9 levels were derived from patients who had evaluation of a CA 19-9 level prior to surgery. Any value 37 U/mL and greater was considered to be positive.
Ideally, methods for cancer screening should be easy to perform, cost-effective, noninvasive, and provide a benefit to patients. Blood-based biomarkers fulfill the first three requirements. However, development of such technology requires an ultrasensitive strategy. In a pilot study, we now show that screening with a highly sensitive nano-based technology allows sensitive and specific detection of invasive cancers. Using our two biomarkers (BNC1 and ADAMTS1), we are able to detect very early stages of pancreatic cancer, with high sensitivity and specificity. Not only have we achieved, in these first studies, higher sensitivities than previously reported for serum hypermethylation markers, but our technology also has the potential to constitute a cost-effective approach for screening of selected, highest risk individuals in the general population for cancers. Additionally, our nano-based MOB detection method serves to significantly reduce the quantity of serum necessary for analysis.(58)
The implementation of BNC1 and ADAMTS1 for screening will require testing in a larger prospective study. We anticipate that the methylation level of these two genes (BNC1 and ADAMTS1) may be used alone, or in combination with other standard methods, to characterize the neoplasia. For example, methods for detecting BNC1 or ADAMTS1 promoter methylation could be carried out prior to or concurrently with testing for mutations common to pancreatic cancer such as KRAS (57) PALB2 (58) or GNAS (59) mutations to improve cancer specificity and sensitivity. Further diagnostic testing could then be initiated to localize the pathology based on their risk profiles including imaging studies such as CT or MRI scans and/or endoscopic studies. As one example, a patient with an extensive family history of pancreatic cancer who tests positive for methylation of BNC1 and ADAMTS1 and also has KRAS mutations could then be tested with CT imaging to evaluate for pancreas neoplasms and or endoscopic screening. Moreover, serial screening in serum of these genes methylation status could also provide an estimate of an individual patient cancer risk. However, this would need to be established in future studies.
In conclusion, to our knowledge, this is the first study to describe the utility of BNC1 and ADAMTS1 promoter methylation as biomarkers in pancreatic cancer. These genes are methylated at high frequencies in pancreatic cancer and are unmethylated in normal pancreatic tissues. Furthermore, we are able to detect the methylation of these genes in the serum of patients with pancreatic cancer. Our data strongly suggests that BNC1 and ADAMTS1 promoter methylation is potentially useful as a sensitive and specific noninvasive modality for identifying individuals at risk for pancreatic cancer.
Supplementary Material
Translational Relevance.
Pancreatic cancer is a deadly cancer with an overall 5-year survival rate of less than 5%. No significant improvements in survival have been observed over the last three decades. Early detection of pancreatic cancer is thought to be the best hope for improving survival in this lethal disease. We have identified a high frequency of methylation of BNC1 and ADAMTS1 in invasive pancreas cancers at 97%. In addition, using Methylation On Beads (MOB) technology, BNC1 and ADAMTS1 promoter methylation in pancreatic cancer patient sera can be detected with high sensitivity and specificity. Detection of methylated BNC1 may serve as a new early detection biomarker for the screening of pancreatic cancer patients and has the potential to improve mortality from this lethal cancer.
Acknowledgements
We would like to thank Sharon Metzger-Gaud, Theresa Sanlorenzo-Caswell and the Johns Hopkins Cancer Registry for assistance with the primary cancer database. We would like to thank Kathy Bender and Rickey Moore for administrative support.
Grant Support
This study is supported by NIH NCI K23CA127141, U54CA151838, R01CA155305, P30CA006973, T32CA126607, CA058184, NIEHS R01 ES011858 the American College of Surgeons/Society of University Surgeons Career Development Award, the Lustgarten Foundation, the Miriam & Sheldon G. Adelson Medical Research Foundation, and the National R&D program (50596) through the Dongnam Institute of Radiological & Medical Sciences (DIRAMS) funded by the Korean Ministry of Education, Science and Technology.
Footnotes
Conflicts of Interest: The authors have no conflicts to disclose.
Authors’ Contributions:
Study design and drafting of manuscript: Yi, J.M., Guzzetta, AA, Ahuja, N., Baylin S.; Analysis and interpretation of data: Yi, J.M., Bailey V.J., Guzzetta, A.A., Chiappinelli, K.B., Ahuja N., Herman, J.G., Baylin S.B.; Statistical Analysis: Guzzetta, A.A. and Downing, S.R Critical revision of the manuscript for important intellectual content: Yi, J.M., Guzzetta. A.A., Bailey V.J., Chiappinelli, K.B., Wang, T.H., Ahuja N., Herman J.G., Baylin S.B.: Technical or Material support: Downing, S.R., Van Neste L., Chiappinelli, K.B., Herrera, A., Keeley, B.P., Pappou, E., Wolfgang, C., Iacobuzio-Donahue C.A., Goggins, M.G.: Funding: Ahuja N. and Baylin S.B.
References
- 1.Jemal ASR, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–49. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Klapman J MM. Early detection of pancreatic cancer: why, who, and how to screen. Cancer Control. 2008;15:280–7. doi: 10.1177/107327480801500402. [DOI] [PubMed] [Google Scholar]
- 3.Siegel RWE, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. A Cancer Journal for Clinicians. 2011;61:212–36. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 4.Gemmel CEA, Helmstädter L, Riemann JF. Pancreatic cancer screening: state of the art. Expert Rev Gastroenterol Hepatol. 2009;3:89–96. doi: 10.1586/17474124.3.1.89. [DOI] [PubMed] [Google Scholar]
- 5.Yeo CJCJ, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA, Hruban RH, Ord SE, Sauter PK, Coleman J, Zahurak ML, Grochow LB, Abrams RA. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Annual of Surgery. 1997;226:248–57. doi: 10.1097/00000658-199709000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, et al. 1423 Pancreaticoduodenectomies for Pancreatic Cancer: A Single-Institution Experience. Journal of Gastrointestinal Surgery. 2006;10:1199–211. doi: 10.1016/j.gassur.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 7.Greenhalf W, Neoptolemos JP. Increasing survival rates of patients with pancreatic cancer by earlier identification. Nat Clin Prac Oncol. 2006;3:346–7. doi: 10.1038/ncponc0483. [DOI] [PubMed] [Google Scholar]
- 8.Misek DEPT, Lubman DM, Simeone DM. Early detection and biomarkers in pancreatic cancer. Journal of the National Conprehensive Cancer Network. 2007;5:1034–41. doi: 10.6004/jnccn.2007.0086. [DOI] [PubMed] [Google Scholar]
- 9.Michael G. Molecular markers of early pancreatic cancer. Journal of Clinical Oncology. 2005;23:4524–31. doi: 10.1200/JCO.2005.19.711. [DOI] [PubMed] [Google Scholar]
- 10.Wilentz REHR. Pathology of cancer of the pancreas. Surgical Oncology Clinics of North America. 1998;7:43–65. [PubMed] [Google Scholar]
- 11.Ueki TTM, Sohn T, Yeo CJ, Issa JP, Hruban RH, Goggins M. Hypermethylation of multiple genes in pancreatic adenocarcinoma. Cancer Research. 2000;60:1835–9. [PubMed] [Google Scholar]
- 12.Jones S, Zhang X, Parsons DW, Lin JC-H, Leary RJ, Angenendt P, et al. Core Signaling Pathways in Human Pancreatic Cancers Revealed by Global Genomic Analyses. Science. 2008;321:1801–6. doi: 10.1126/science.1164368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones PA, Baylin SB. The Epigenomics of Cancer. Cell. 2007;128:683–92. doi: 10.1016/j.cell.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laird PW. The power and the promise of DNA methylation markers. Nat Rev Cancer. 2003;3:253–66. doi: 10.1038/nrc1045. [DOI] [PubMed] [Google Scholar]
- 15.Jemal A, Center MM, DeSantis C, Ward EM. Global Patterns of Cancer Incidence and Mortality Rates and Trends. Cancer Epidemiology Biomarkers & Prevention. 2010;19:1893–907. doi: 10.1158/1055-9965.EPI-10-0437. [DOI] [PubMed] [Google Scholar]
- 16.Jemal AWE, Thun M. Declining death rates reflect progress against cancer. PLoS One. 2010;5:e9584. doi: 10.1371/journal.pone.0009584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glockner SC, Dhir M, Yi JM, McGarvey KE, Van Neste L, Louwagie J, et al. Methylation of TFPI2 in Stool DNA: A Potential Novel Biomarker for the Detection of Colorectal Cancer. Cancer Research. 2009;69:4691–9. doi: 10.1158/0008-5472.CAN-08-0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Melotte V, Lentjes MHFM, van den Bosch SM, Hellebrekers DMEI, de Hoon JPJ, Wouters KAD, et al. N-Myc Downstream-Regulated Gene 4 (NDRG4): A Candidate Tumor Suppressor Gene and Potential Biomarker for Colorectal Cancer. Journal of the National Cancer Institute. 2009;101:916–27. doi: 10.1093/jnci/djp131. [DOI] [PubMed] [Google Scholar]
- 19.Anglim PPGJ, Koss MN, Hagen JA, Turla S, Campan M, Weisenberger DJ, Laird PW, Siegmund KD, Laird-Offringa IA. Identification of a panel of sensitive and specific DNA methylation markers for squamous cell lung cancer. Molecular Cancer. 2008;7:62. doi: 10.1186/1476-4598-7-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoque MO. DNA methylation changes in prostate cancer: current developments and future clinical implementation. Expert Review of Molecular Diagnostics. 2009;9:243–57. doi: 10.1586/erm.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koopmann J, Rosenzweig CNW, Zhang Z, Canto MI, Brown DA, Hunter M, et al. Serum Markers in Patients with Resectable Pancreatic Adenocarcinoma: Macrophage Inhibitory Cytokine 1 versus CA19-9. Clinical Cancer Research. 2006;12:442–6. doi: 10.1158/1078-0432.CCR-05-0564. [DOI] [PubMed] [Google Scholar]
- 22.Larghi A, Verna EC, Lecca PG, Costamagna G. Screening for Pancreatic Cancer in High-Risk Individuals: A Call for Endoscopic Ultrasound. Clinical Cancer Research. 2009;15:1907–14. doi: 10.1158/1078-0432.CCR-08-1966. [DOI] [PubMed] [Google Scholar]
- 23.Canto MI, Goggins M, Yeo CJ, Griffin C, Axilbund JE, Brune K, et al. Screening for pancreatic neoplasia in high-risk individuals: an EUS-based approach. Clinical Gastroenterology and Hepatology. 2004;2:606–21. doi: 10.1016/s1542-3565(04)00244-7. [DOI] [PubMed] [Google Scholar]
- 24.Rhee I, Bachman KE, Park BH, Jair KW, Yen RW, Schuebel KE, et al. DNMT1 and DNMT3b cooperate to silence genes in human cancer cells. Nature. 2002;416:552–6. doi: 10.1038/416552a. [DOI] [PubMed] [Google Scholar]
- 25.Schuebel KE, Chen W, Cope L, Glöckner SC, Suzuki H, Yi JM, Chan TA, Neste LV, Criekinge WV, Bosch SV, van Engeland M, Ting AH, Jair K, Yu W, Toyota M, Imai K, Ahuja N, Herman JG, Baylin SB. Comparing the DNA Hypermethylome with Gene Mutations in Human Colorectal Cancer. PLoS Genetics. 2007;3:1709–23. doi: 10.1371/journal.pgen.0030157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herman JG, Graff JR, Myohanen S, Nelkin BD, Baylin SB. Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci U S A. 1996;93:9821–6. doi: 10.1073/pnas.93.18.9821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–8. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 28.Bailey VJ, Zhang Y, Keeley BP, Yin C, Pelosky KL, Brock M, et al. Single-Tube Analysis of DNA Methylation with Silica Superparamagnetic Beads. Clinical Chemistry. 2010;56:1022–5. doi: 10.1373/clinchem.2009.140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bailey VJ, Easwaran H, Zhang Y, Griffiths E, Belinsky SA, Herman JG, et al. MS-qFRET: a quantum dot-based method for analysis of DNA methylation. Genome Res. 2009;19:1455–61. doi: 10.1101/gr.088831.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bailey VJ, Keeley BP, Razavi CR, Griffiths E, Carraway HE, Wang TH. DNA methylation detection using MS-qFRET, a quantum dot-based nanoassay. Methods. 2010;52:237–41. doi: 10.1016/j.ymeth.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 31.R: A Language and Environment for Statistical Computing. 2.14.0 ed. R Development Core Team; Vienna, Austria: 2011. [Google Scholar]
- 32.Chan TA GS, Yi JM, Chen W, Van Neste L, Cope L, Herman JG, Velculescu V, Schuebel KE, Ahuja N, Baylin SB. Convergence of mutation and epigenetic alterations identifies common genes in cancer that predict for poor prognosis. PLoS Medicine. 2008;5:0823–38. doi: 10.1371/journal.pmed.0050114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yi JM, Dhir M, Van Neste L, Downing SR, Jeschke J, Glöckner SC, et al. Genomic and Epigenomic Integration Identifies a Prognostic Signature in Colon Cancer. Clinical Cancer Research. 2011;17:1535–45. doi: 10.1158/1078-0432.CCR-10-2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hruban RH, Goggins M, Parsons J, Kern SE. Progression Model for Pancreatic Cancer. Clinical Cancer Research. 2000;6:2969–72. [PubMed] [Google Scholar]
- 35.Hruban RH CM, Yeo CJ. Prevention of pancreatic cancer and strategies for management of familial pancreatic cancer. Digestive Diseases. 2001;19:76–84. doi: 10.1159/000050656. [DOI] [PubMed] [Google Scholar]
- 36.Issa JP, Ahuja N, Toyota M, Bronner MP, Brentnall TA. Accelerated Age-related CpG Island Methylation in Ulcerative Colitis. Cancer Res. 2001;61:3573–7. [PubMed] [Google Scholar]
- 37.Dhir M, Montgomery E, Glöckner S, Schuebel K, Hooker C, Herman J, et al. Epigenetic Regulation of WNT Signaling Pathway Genes in Inflammatory Bowel Disease (IBD) Associated Neoplasia. Journal of Gastrointestinal Surgery. 2008;12:1745–53. doi: 10.1007/s11605-008-0633-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hahn MA, Hahn T, Lee D-H, Esworthy RS, Kim B-w, Riggs AD, et al. Methylation of Polycomb Target Genes in Intestinal Cancer Is Mediated by Inflammation. Cancer Research. 2008;68:10280–9. doi: 10.1158/0008-5472.CAN-08-1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rhodes DR YJ, Shanker K, Deshpande N, Varambally R, Ghosh D, Barrette T, Pandey A, Chinnaiyan AM. ONCOMINE: a cancer microarray database and integrated data-mining platform. Neoplasia. 2004;6:1–6. doi: 10.1016/s1476-5586(04)80047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fry LC, Monkemuller K, Malfertheiner P. Molecular markers of pancreatic cancer: development and clinical relevance. Langenbecks Arch Surg. 2008;393:883–90. doi: 10.1007/s00423-007-0276-0. [DOI] [PubMed] [Google Scholar]
- 41.Ballehaninna UK, Chamberlain RS. The clinical utility of serum CA 19-9 in the diagnosis, prognosis and management of pancreatic adenocarcinoma: An evidence based appraisal. J Gastrointest Oncol. 2012;3:105–19. doi: 10.3978/j.issn.2078-6891.2011.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sidransky D. Emerging molecular markers of cancer. Nat Rev Cancer. 2002;2:210–9. doi: 10.1038/nrc755. [DOI] [PubMed] [Google Scholar]
- 43.Jeschke J, Van Neste L, Glockner SC, Dhir M, Calmon MF, Deregowski V, et al. Biomarkers for detection and prognosis of breast cancer identified by a functional hypermethylome screen. Epigenetics. 2012;7:701–9. doi: 10.4161/epi.20445. [DOI] [PubMed] [Google Scholar]
- 44.Wang J, Zhang S, Schultz RM, Tseng H. Search for basonuclin target genes. Biochemical and Biophysical Research Communications. 2006;348:1261–71. doi: 10.1016/j.bbrc.2006.07.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shames DSGL, Gao B, Sato M, Lewis CM, Shivapurkar N, Jiang A, Perou CM, Kim YH, Pollack JR, Fong KM, Lam CL, Wong M, Shyr Y, Nanda R, Olopade OI, Gerald W, Euhus DM, Shay JW, Gazdar AF, Minna JD. A genome-wide screen for promoter methylation in lung cancer identifies novel methylation markers for multiple malignancies. PLoS Medicine. 2006;3:e486. doi: 10.1371/journal.pmed.0030486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Porter S, Clark IM, Kevorkian L, Edwards DR. The ADAMTS metalloproteinases. Biochemical Journal. 2005;386:15–27. doi: 10.1042/BJ20040424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Masui T, Hosotani R, Tsuji S, Miyamoto Y, Yasuda S, Ida J, et al. Expression of METH-1 and METH-2 in Pancreatic Cancer. Clinical Cancer Research. 2001;7:3437–43. [PubMed] [Google Scholar]
- 48.Porter S, Scott SD, Sassoon EM, Williams MR, Jones JL, Girling AC, et al. Dysregulated Expression of Adamalysin-Thrombospondin Genes in Human Breast Carcinoma. Clinical Cancer Research. 2004;10:2429–40. doi: 10.1158/1078-0432.ccr-0398-3. [DOI] [PubMed] [Google Scholar]
- 49.Choi JE, Kim DS, Kim EJ, Chae MH, Cha SI, Kim CH, et al. Aberrant methylation of ADAMTS1 in non-small cell lung cancer. Cancer Genet Cytogenet. 2008;187:80–4. doi: 10.1016/j.cancergencyto.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 50.Yegnasubramanian S, Wu Z, Haffner MC, Esopi D, Aryee MJ, Badrinath R, et al. Chromosome-wide mapping of DNA methylation patterns in normal and malignant prostate cells reveals pervasive methylation of gene-associated and conserved intergenic sequences. BMC Genomics. 2011;12:313. doi: 10.1186/1471-2164-12-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahlquist T, Lind GE, Costa VL, Meling GI, Vatn M, Hoff GS, et al. Gene methylation profiles of normal mucosa, and benign and malignant colorectal tumors identify early onset markers. Mol Cancer. 2008;7:94. doi: 10.1186/1476-4598-7-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vázquez FHG, Ortega MA, Lane TF, Oikemus S, Lombardo M, Iruela-Arispe ML. METH-1, a human ortholog of ADAMTS-1, and METH-2 are members of a new family of proteins with angio-inhibitory activity. Journal of Biological Chemistry. 1999;274:23349–57. doi: 10.1074/jbc.274.33.23349. [DOI] [PubMed] [Google Scholar]
- 53.Vincent AHJ, Schulick R, Hruban RH, Goggins M. Pancreatic Cancer. Lancet. 2011;378:607–20. doi: 10.1016/S0140-6736(10)62307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Winter JMBM, Tang LH, D'Angelica MI, Dematteo RP, Fong Y, Kimstra DS, Jamaqin WR, Allen PJ. Survival after resection of pancreatic adenocarcinoma: results from a single institution over three decades. Annals of Surgical Oncology. 2012;19:165–75. doi: 10.1245/s10434-011-1900-3. [DOI] [PubMed] [Google Scholar]
- 55.Jemal ASR, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 56.Sato N, Maitra A, Fukushima N, van Heek NT, Matsubayashi H, Iacobuzio-Donahue CA, et al. Frequent Hypomethylation of Multiple Genes Overexpressed in Pancreatic Ductal Adenocarcinoma. Cancer Research. 2003;63:4158–66. [PubMed] [Google Scholar]
- 57.Brune KHS, Li A, Yashida S, Abe T, Griffith M, Yang D, Omura N, Eshleman J, canto M, Sculick R, Klein AP, Hruban RH, Iacobuzio-Donahue C, Goggins M. Genetic and epigenetic alterations of familiar pancreatic cancers. Cancer Epidemiol Biomarkers Prev. 2008;17:3536–42. doi: 10.1158/1055-9965.EPI-08-0630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jones Sn, Hruban RH, Kamiyama M, Borges M, Zhang X, Parsons DW, et al. Exomic Sequencing Identifies PALB2 as a Pancreatic Cancer Susceptibility Gene. Science. 2009;324:217. doi: 10.1126/science.1171202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wu J, Matthaei H, Maitra A, Dal Molin M, Wood LD, Eshleman JR, et al. Recurrent GNAS Mutations Define an Unexpected Pathway for Pancreatic Cyst Development. Science Translational Medicine. 2011;3:92ra66–92ra66. doi: 10.1126/scitranslmed.3002543. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.