Abstract
Missing in Metastasis (MIM), also known as MTSS1, is a scaffold protein that is down-regulated in multiple metastatic cancer cell lines compared to non-metastatic counterparts. MIM regulates cytoskeletal dynamics and actin polymerization, and has been implicated in the control of cell motility and invasion. MIM has also been shown to bind to a receptor PTP, PTPδ, an interaction that may provide a link between tyrosine phosphorylation-dependent signaling and metastasis. We used shRNA-mediated gene silencing to investigate the consequences of loss of MIM on the migration and invasion of the MCF10A mammary epithelial cell model of breast cancer. We observed that suppression of MIM by RNAi enhanced migration and invasion of MCF10A cells, effects that were associated with increased levels of PTPδ. Furthermore, analysis of human clinical data indicated that PTPδ was elevated in breast cancer samples when compared to normal tissue. We demonstrated that the SRC protein tyrosine kinase is a direct substrate of PTPδ and, upon suppression of MIM, we observed changes in the phosphorylation status of SRC, in particular the inhibitory site (Tyr 527) was hypophosphorylated, whereas the activating autophosphorylation site (Tyr 416) was hyperphosphorylated. Thus, the absence of MIM led to PTPδ-mediated activation of SRC. Finally, the SRC inhibitor SU6656 counteracted the effects of MIM suppression on cell motility and invasion. This study illustrates that both SRC and PTPδ have the potential to be therapeutic targets for metastatic tumors associated with loss of MIM.
Keywords: Missing in Metastasis, MTSS1, PTPδ, SRC, breast cancer, cell migration, cell invasion, metastasis
INTRODUCTION
According to the American Cancer Society (Breast Cancer Facts and Figures 2013–2014), approximately 233,000 women will be diagnosed with invasive breast cancer in the USA in 2014, which is predicted to lead to 40,000 deaths. It is expected that breast cancer will account for 29% of all new cancers diagnosed in women. Metastasis, the spread of cancer from the primary tumor to remote sites, is the major cause of fatality, resulting in about 90% of deaths [1]. The pathophysiology of metastasis encompasses release of cells from the primary tumor site, transport of the cells in the blood vessels or the lymphatic system, attachment to the remote site, and invasion and colonization of secondary site [2]. Therefore, it is of utmost importance to gain an understanding the mechanisms that facilitate the invasive transition in breast cancer and the complex processes that underlie changes in cell migration and cell invasion. Although considerable attention has focused on the oncogenes and tumor suppressors that trigger the establishment of primary tumors, it is now apparent that there is also a class of metastasis suppressor genes, the products of which exert a regulatory influence at each step in the development of a metastatic state without affecting growth of the primary tumor [3]. Missing in Metastasis (MIM), also referred to as MTSS1, is one such metastasis suppressor, with potential roles in the control of cellular migration and invasion. MIM is expressed in a diverse range of tissues and is down-regulated in several cancers, including breast [4–8]. Thus it has been proposed that loss of MIM function may promote the metastatic potential of cancer cells.
MIM is a multi-domain protein, the structure of which suggests a scaffolding function [9]. The presence of WH2 and IMD domains implies a functional link with the actin cytoskeleton and recruitment of MIM to specific cytoskeletal networks. Such interactions implicate MIM in cytoskeletal changes that underlie regulation of metastasis. The central segment of MIM is rich in proline, serine, and threonine residues, and plays an important regulatory role in MIM function. Importantly, this central segment of MIM binds to several key cellular proteins, including association with the receptor protein tyrosine phosphatase (RPTP) family protein, PTPδ [10]. Interaction studies using the yeast two-hybrid approach and analysis of MIM interaction with recombinant PTPδ illustrate that MIM binds to the cytoplasmic domain of PTPδ [10]. Since RPTPs are known to regulate tyrosine phosphorylation-dependent signaling, this MIM-PTPδ interaction may provide a functional link that influences the signal transduction events that underlie the establishment of an invasive state.
The RPTPs are transmembrane proteins that have the potential to regulate signaling through ligand-controlled protein tyrosine dephosphorylation [11, 12]. The LAR-like RPTPs are a subfamily of these receptor-like proteins that have been extensively characterized in neurons, and have been directly implicated in axon growth regulation in invertebrates [13]. The LAR-like PTPs (LAR, PTPσ, PTPδ) contain two intracellular phosphatase domains and an extracellular segment consisting of Ig-like and fibronectin type III like domains, commonly found in cell adhesion molecules [11]. This structural architecture implies that LAR-like phosphatases may function in integrating tyrosine phosphorylation-dependent cellular signaling with cell-cell and cell-matrix interactions. In fact, LAR-like RPTPs have been implicated in biological processes that rely upon regulated cell-cell and cell-matrix contact, such as control of neuronal pathfinding [14, 15]. LAR localizes to the ends of focal adhesions, implicating LAR-like RPTPs in their disassembly [16]. Signaling events downstream of LAR-like RPTPs that regulate axonal guidance involve Rho-GTPase-dependent cytoskeletal remodeling [17]. It has also been demonstrated, using LAR−/− mice, that LAR plays a significant role in the signaling events responsible for mammary gland development and function [18]. Overall, this suggests that RPTPs, in particular those of the LAR subfamily, might be important regulators of signaling in breast cancer.
The LAR-like enzyme PTPδ is also expressed in the central nervous system, where it is concentrated in growth cones of elongating processes [19]. PTPδ is a homophilic cell adhesion molecule [20]. These homophilic interactions serve to promote neuronal adhesion and neurite outgrowth [20, 21]. PTPδ has been suggested to be a tumor suppressor due to its inactivation in a number of human cancers, including head and neck, melanoma, lung cancer and neuroblastoma [22–24]. Multiple mutations have been identified in tumors that may compromise not only activity, but also the function of the extracellular segment [22]. Chromosome 9p, which harbors the PTPRD (gene encoding PTPδ), is also a frequent target of microdeletion in primary tumors and is subject to chromosome shedding in 6% of tumors studied [25, 26]. In contrast to genomic studies, PTPδ loss of function in mice is associated with impaired learning, but has not been reported to increase tumor incidence [27]. Furthermore, reconstitution studies failed to demonstrate a growth suppressive function for PTPδ [28]. Therefore, consistent with the complex role of other PTPs in cancer [29, 30], it appears that the function of PTPδ may be context-dependent. In this study, we have expanded the potential roles of PTPδ in cancer by testing the hypothesis that it functions in the regulation of tyrosine phosphorylation-dependent signaling events that underlie cell motility and cell invasion in MIM-negative cells. We present evidence that suppression of MIM led to increased expression of PTPδ, which enhanced invasion of breast epithelial cells through activation of the protein tyrosine kinase SRC. These data define a mechanism by which MIM may exert activity as a metastasis suppressor through regulating tyrosine phosphorylation-dependent signaling in breast epithelial cells.
EXPERIMENTAL PROCEDURES
Antibodies
Anti-PTPδ antibody was from Novus Biologicals. Stained tissue sections in the Human Protein Atlas were generated using the same antibody. Antibodies to SRC-pTyr 527, SRC-pTyr 416 and total SRC protein, Cortactin–pTyr 421, and total Cortactin, as well as antibodies to MIM, were from Cell Signaling Technology.
Cell culture
MCF-10A cells were obtained from ATCC (Manassas, VA) and cultured in Dulbecco’s modified Eagle medium (DMEM)–F-12 (Invitrogen) supplemented with 5% donor horse serum, 20 ng/ml epidermal growth factor (EGF), 10 μg/ml insulin, 100 ng/ml hydrocortisone, 100 ng/ml cholera toxin, 100 U/ml penicillin, and 100 μg/ml streptomycin. Growth factor-reduced Matrigel was purchased from BD Biosciences.
Generation of cells expressing shRNA targeting MIM and PTPδ
For stable suppression of MIM in MCF10A cells, we expressed a pMLP retroviral vector (in a pMSCV backbone) using the targeting sequences TCTTCTGCAGCTTCAGCGT and TCTTTTTGATCTCATGCCG incorporated into the sequence of the human microRNA-30 (miR30). The infected cells were selected using puromycin (1–2 μg). For double selection, PTPRD shRNA, using the targeting sequence TGCATACATCTTAGACTCT, was subcloned in pMSCV hygro and selected using hygromycin (100 μg/ml). pcDF1-PTPRD (plasmid 25642) was ordered from Addgene. Infections were carried out as previously described [22]. The GST-PTPδ fusion construct in pGEX vector was a kind gift from Dr. Timothy Chan. Inactive (C1553S) and substrate-trapping (D1521A) mutations were engineered into pcDF1-PTPRD and pGEX-PTPRD constructs using site-directed mutagenesis (Quickchange II XL kit from Stratagene) as directed by the manufacturer. The coding sequences were verified by DNA sequencing.
Cell migration and invasion assays
Cell motility was measured using Cell Culture Inserts (8.0-μm pore size) for six-well plates (BD Falcon). To visualize cell invasion, we used eight-well chamber slides (BD Biosciences) precoated with 70 μL of 1:1 mixture of Matrigel and Collagen I (BD Biosciences). On day 1, 4000 cells were grown per well in the presence of 5 ng/mL EGF [31]. Cell morphology was photographed on days 8 and 10. The phase images were taken by a Zeiss Axiovert 200M using AxioVison 4.4 software. To quantitate cell invasion, we used BD BioCoat Matrigel Invasion Chambers, 8.0-μm pore size. MCF10A cells (1 × 106) were grown in the insert. After 48 h, the cells retained inside the insert were removed, and those that migrated to the other side of the insert were fixed and stained with DAPI and counted.
Real Time Quantitative PCR
Total RNA from 70–80% cells was isolated using Trizol, DNase I treated and reverse transcribed using reverse transcriptase and random hexamers. QPCR was performed for PTPRD according to manufacturer’s recommendations (Applied Biosystems). The mean Cycle Threshold (Ct) value was used to calculate the gene expression. PCR products were normalized to beta-actin levels. Primers used for PTPRD were 5′-AGAGAGAAATGTCACCAATA-3′, 5′-AATTCCCTTAGGATATACTG-3′ and for actin were 5′-TCCCTGGAGAAGAGCTACG-3′, 5′-GTAGTTTCGTGCATGCCACA-3′.
Cycloheximide study
MCF10A cells expressing the appropriate shRNA were serum-starved overnight, followed by treatment with cycloheximide (100 μg/ml). Cell lysates were collected at the indicated times and protein concentrations were determined by Bradford. Equal amounts of lysates were loaded and proteins were resolved by SDS-PAGE and detected by immunoblotting.
Immunoprecipitation and immunoblotting
Cells were grown to 90% confluency in 10 cm plates, washed with cold 1 X phosphate buffered saline (PBS) and extracted using 800μl of lysis buffer consisting of 50mM Tris-HCl (pH 7.5), 150mM NaCl, 5mM EDTA, 1% Triton X-100, 0.1% sodium deoxycholate, 20mM β-glycerophosphate, 1mM sodium vanadate, 1mM sodium fluoride and protease inhibitor cocktail. All steps were carried out on ice or at 4°C. Cells were lysed for 1h, centrifuged at 12,000 × g for 10 min and protein concentrations were determined using the Bradford assay. Lysates (Total protein 1 mg) were pre-cleared for 60 min with protein A/G-Sepharose. The supernatants were first incubated for 60 min with appropriate antibodies and 10 μl of protein A/G Sepharose was then added for another 60 min. The immune complexes were pelleted at 3000 × g for 5 min and washed three times with cold lysis buffer. The beads were resuspended in 20 μl of 5X Laemmli sample buffer and heated at 95°C for 1 min. Proteins were resolved by SDS-PAGE and detected by immunoblotting.
Substrate trapping assay
Serum-starved MCF10A cells expressing wild type or substrate-trapping DA mutant of PTPδ were pretreated with 50 μM pervanadate for 30 minutes. Cells were rinsed with ice-cold PBS and lysed in 50 mM Tris-HCl, pH 7.5, 150 mM NaCl, 5 mM EDTA, 1% Triton X-100, 0.1% sodium deoxycholate, protease inhibitor tablet (EDTA-free, Roche). Dithiothreitol (DTT) was added to a final concentration of 10 mM and cells were lysed for 30 min on a rotating wheel at 4°C. Cell debris was centrifuged at 12,000 × g for 10 minutes and protein concentrations were determined by the method of Bradford. An equal amount of lysate (100 μg) was diluted in cold lysis buffer and pre-cleared for 30 min with anti-Flag-agarose beads. To test for PTPδ substrate-trapping capacity, lysates expressing either wild type or PTPδ trapping mutant were immunoprecipitated with PTPδ antibody. The PTPδ-substrate complexes were pelleted at 3000 × g for 5 min, washed 3 times with lysis buffer, resuspended in Laemmli sample buffer and binding of SRC was detected by immunoblotting.
In vitro phosphatase assay
GST-tagged wild type PTPδ and CS mutant were purified on GS-agarose [32]. The reduced enzyme was then incubated with immunoprecipitated SRC at 30°C for 30 min. The reaction was terminated with Laemmli sample buffer, proteins were resolved by SDS-PAGE and substrate dephosphorylation was visualized by immunoblotting.
RESULTS
Loss of MIM induced migration of mammary epithelial cells
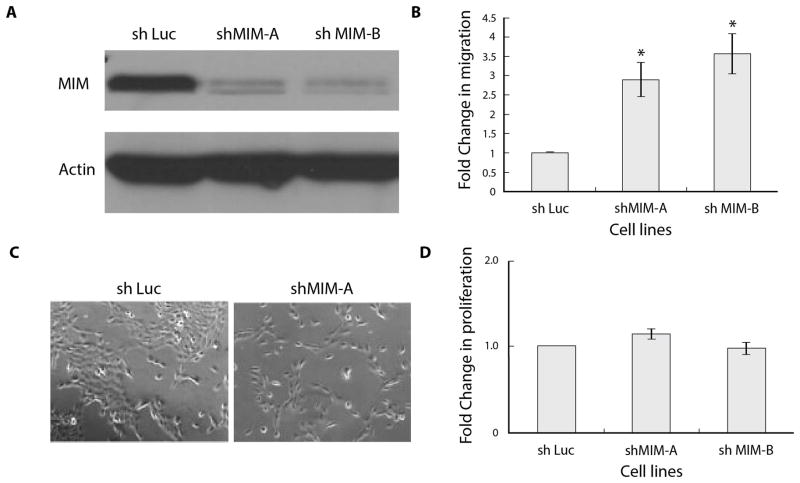
In breast carcinoma, the ability of tumor cells to migrate from the primary site and establish a secondary tumor is an early determinant of the transition from a benign to an invasive state. Although it has been reported that loss of MIM transcript correlates with the invasive state of breast cancer cell lines [4], the role of MIM during cell migration and cell invasion has not been elucidated. To investigate its role in the migration and invasion of mammary epithelial cells, we suppressed MIM using RNAi and generated stable MCF10A populations expressing MIM-directed shRNA. Depletion of MIM by two distinct shRNAs was validated by immunoblotting (Fig 1A) and the effects were investigated using a transwell migration assay. We observed that suppression of MIM resulted in up to a 4-fold increase in migration, compared to those cells stably expressing a control shRNA (Fig 1B). In addition, MCF10A cells normally form clusters when grown as sub-confluent cultures [33]; however, we observed that suppression of MIM led to a scattering phenotype with a preponderance of single cells that do not form clusters (Fig 1C). In contrast, we observed that suppression of MIM had no apparent effect on cell proliferation (Fig 1D).
Figure 1. Suppression of MIM induced an increase in mammary epithelial cell motility.
(A) RNAi-mediated suppression of MIM by shRNA, measured by immunoblotting cell lysates with antibodies to MIM. (B) MCF10A cells infected with control or two distinct MIM-directed shRNAs were seeded in transwell migration chambers, incubated for 48 h, and cells that had migrated were counted. The motility of the control cells was normalized to 1. Error bars represent S.E.M. (n=3). * denotes p value<0.05. (C) Scattering of MCF10A cells induced by suppression of MIM was visualized in sub-confluent culture. (D) MCF10 A cells infected with control or two distinct MIM-directed shRNAs were seeded in 96 well plates, incubated for 48h, and cell proliferation was measured using MTT reagent according to the manufacturer’s recommendations.
Loss of MIM induced invasion of mammary epithelial cells
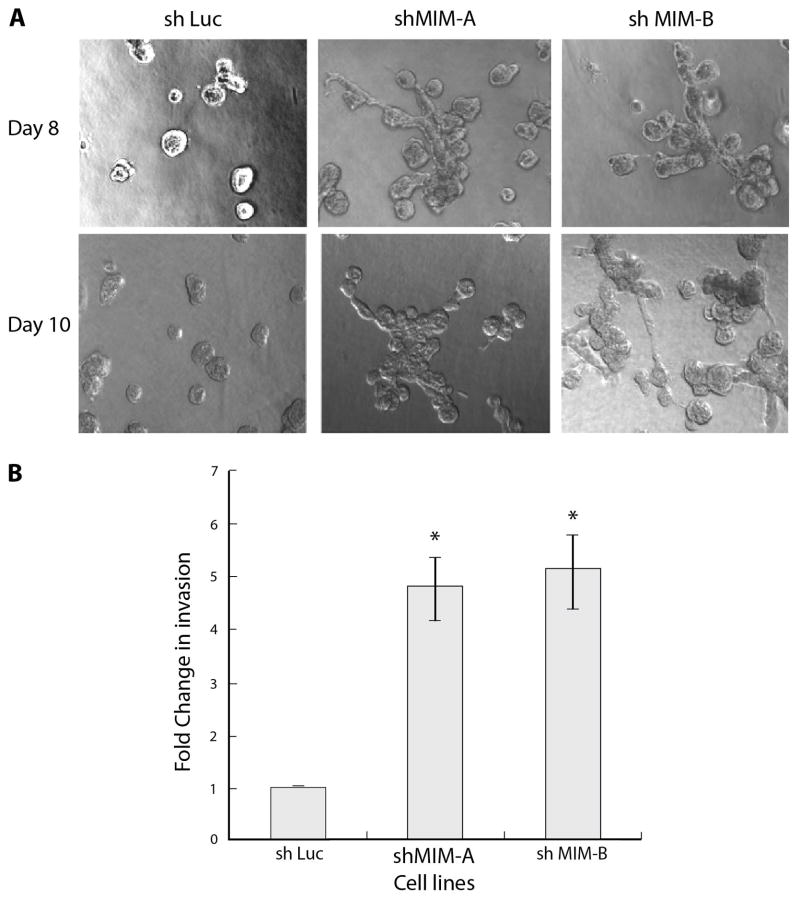
Given the intrinsic complexity of the invasion process, 2D culture systems are limited in their utility; however, 3D culture in modified Matrigel/Collagen matrices has permitted modeling of cell invasion [33]. Consistent with the migration assay, we observed that attenuation of MIM expression in MCF10A cells led to disorganized acinar structures and formation of cellular protrusions indicative of an invasive state (Fig 2A). In addition, we performed quantitative assays in transwell filters coated with Matrigel and observed that cells in which MIM was depleted displayed an ~5-fold increase in invasion compared with the parental cells (Fig 2B). These results are consistent with a role for MIM in regulating cell migration and invasion, both important features of metastasis.
Figure 2. Suppression of MIM promoted mammary epithelial cell invasion.
(A) Induction of invasive structures in MCF10A cells in which MIM was suppressed by two distinct shRNAs. The micrographs were taken at Day 8 and Day 10 of 3D culture in Matrigel-collagen. Scale bar represents 100 μm. (B) MCF10A cells infected with control or two distinct MIM-directed shRNAs were seeded in transwell migration chambers in which the membrane was coated with Matrigel, incubated for 48 h, and cells that had migrated through the Matrigel coating were counted. Invasion by the control cells was normalized to 1. Error bars represent S.E.M. (n=3). * denotes p value<0.05
Loss of MIM induced an increase in mRNA and protein levels of PTPδ
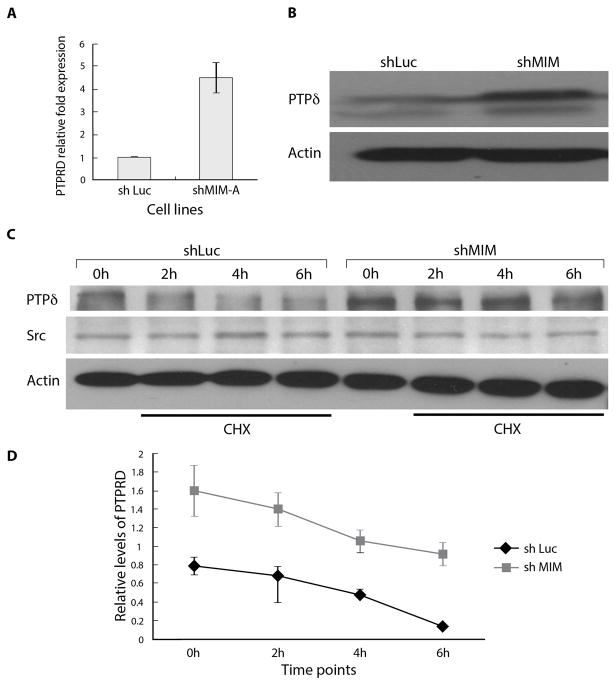
As MIM and PTPδ have been shown to be binding partners [10], this interaction may underlie a functional link between MIM and tyrosine phosphorylation-dependent signaling events associated with cell migration and invasion. We observed that the level of PTPδ mRNA (Fig 3A) and protein (Fig 3B) was elevated in cells in which MIM was suppressed compared to the control cells; however, the stability of PTPδ protein was apparently unaffected, as assessed by immunoblotting to measure PTPδ protein in cycloheximide-treated compared to control cells (Fig 3C & D).
Figure 3. Suppression of MIM increased the mRNA and protein levels of PTPδ.
(A) Quantitative real time PCR analysis of RNA extracted from cells expressing indicated shRNA to illustrate that MCF10A cells with MIM-directed shRNA is accompanied by increased levels of PTPRD mRNA. (B) Immunoblot of lysates expressing indicated shRNA to illustrate that treatment of MCF10A cells with MIM-directed shRNA is accompanied by increased levels of PTPδ. (C) Control and shMIM-expressing MCF10A cells were treated with cyclohexamide, and lysates were prepared at the indicated time points. The levels of PTPδ was assessed by immunoblotting (20 μg of total lysate protein). The levels of SRC were measured as a control. (D) Quantitation of PTPδ stability from three independent experiments is indicated. Error bars represent S.E.M.
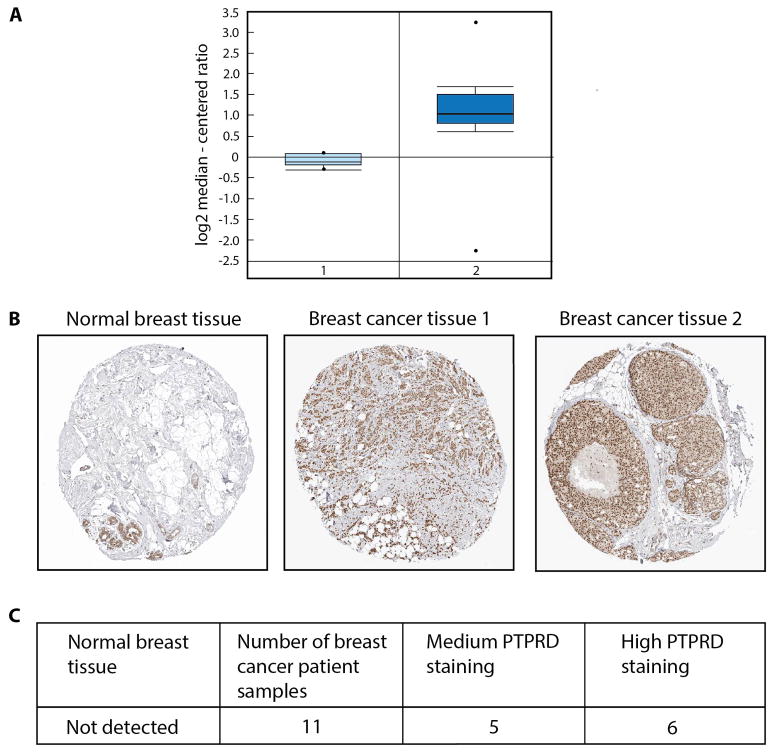
PTPδ expression in human breast cancer
To investigate whether there were alterations in the level of expression of PTPδ in human breast cancer, we analyzed microarray gene expression data from Finak et al [34] for the level of PTPδ mRNA in 53 breast tumor stroma samples, compared to 6 normal breast stroma samples (data available at www.oncomine.org). This revealed that PTPδ mRNA levels were elevated in the tumor samples when compared with the normal samples (Fig 4A, 2.4 fold change, P-value of 7.94E-15). We also investigated PTPδ protein expression using immunohistochemistry data from 11 patient samples that were available in the Human Protein Atlas [35] (www.proteinatlas.org). The normal breast tissue showed minimal staining for PTPδ (Fig 4B), whereas a patient with ductal carcinoma showed more intense staining for PTPδ. We observed high PTPδ staining in more than 50% of patient samples when compared with the normal tissues (Fig 4C). In addition, we attempted to determine whether there was a correlation between MIM expression and any clinical variables. However this proved to be intractable due to the genomic location of MIM, close to the c-MYC gene (hg18), which is part of a genomic region commonly amplified in breast cancer samples [36].
Figure 4. Expression of PTPδ in human tumor samples.
(A) PTPδ expression was analyzed in datasets from the Oncomine (Compendia Bioscience) database (http://www.oncomine.org). The Finak Breast dataset, which constituted 53 breast tumor stroma samples and 6 normal breast stroma samples that were analyzed on Agilent 44K microarrays, showed increased mRNA levels of PTPδ in the tumor samples (P value is 7.94E-15). (B) PTPδ protein expression data from the Human Protein Atlas (www.proteinatlas.org). Representative images of Immunohistochemistry staining for one sample of normal breast tissue and two breast cancer tissue specimens from patients are shown. (C) Table indicates PTPδ protein expression levels analyzed by immunohistochemistry in 11 patient samples, of which 5 patient samples showed medium and 6 patient samples showed high staining relative to the normal breast tissue.
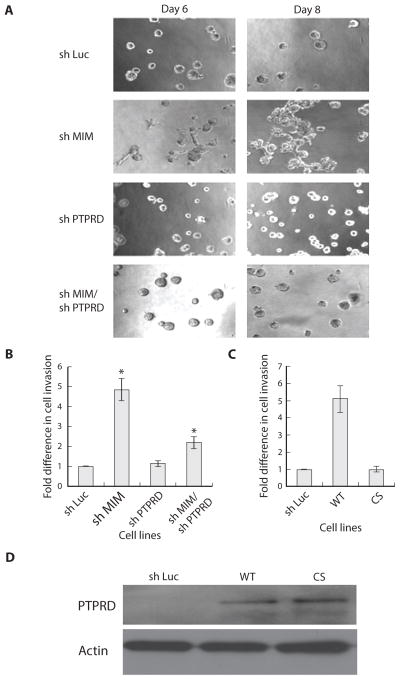
The invasion phenotype induced by loss of MIM was mediated by altered levels of PTPδ
To investigate the importance of PTPδ for the enhanced cell motility and invasion caused by MIM suppression, we generated cell lines co-expressing shRNA targeting both MIM and PTPδ. We observed no apparent effects on cell invasion of suppressing PTPδ alone, but the co-expression of both MIM and PTPδ-directed shRNAs resulted in abrogation of the invasion phenotype caused by suppression of MIM alone (Fig 5A). This illustrates that PTPδ is required for the MIM-dependent signaling events that underlie cell invasion.
Figure 5. The formation of invasive structures that accompanied suppression of MIM was abrogated by co-suppression of PTPδ.
(A) Phase images of the MCF10A acini expressing the indicated shRNA. (B) Co-suppression of PTPδ impaired cell invasion induced by suppression of MIM. (C) Expression of wild type active PTPδ, but not the catalytically inactive mutant form of the enzyme, was sufficient to induce cell invasion. In both B and C, cell invasion was quantitated using transwell chambers coated with Matrigel. Data are presented as change in cell invasion relative to the luciferase control. Error bars represent S.E.M. (n=3). * denotes p-value<0.05. (D) Expression of wild-type PTPδ and the CS mutant was determined by immunoblotting the lysates with PTPδ antibody.
We investigated further this effect of PTPδ on MIM signaling using quantitative invasion assays performed on transwell invasion chambers (Fig 5B). Suppression of MIM resulted in an ~5-fold increase in cell invasion that was partially blocked upon co-suppression of MIM and PTPδ. To determine whether the enzymatic activity of PTPδ was required for its effects on cell invasion, we generated stable cells in which wild type PTPδ and the catalytically inactive CS mutant were overexpressed and observed that wild-type PTPδ, but not the inactive CS mutant, resulted in an increase in cell invasion (Fig 5C & D). This indicated that elevated levels of PTPδ were sufficient to enhance invasion, highlighting further the importance of PTPδ in mediating MIM functions.
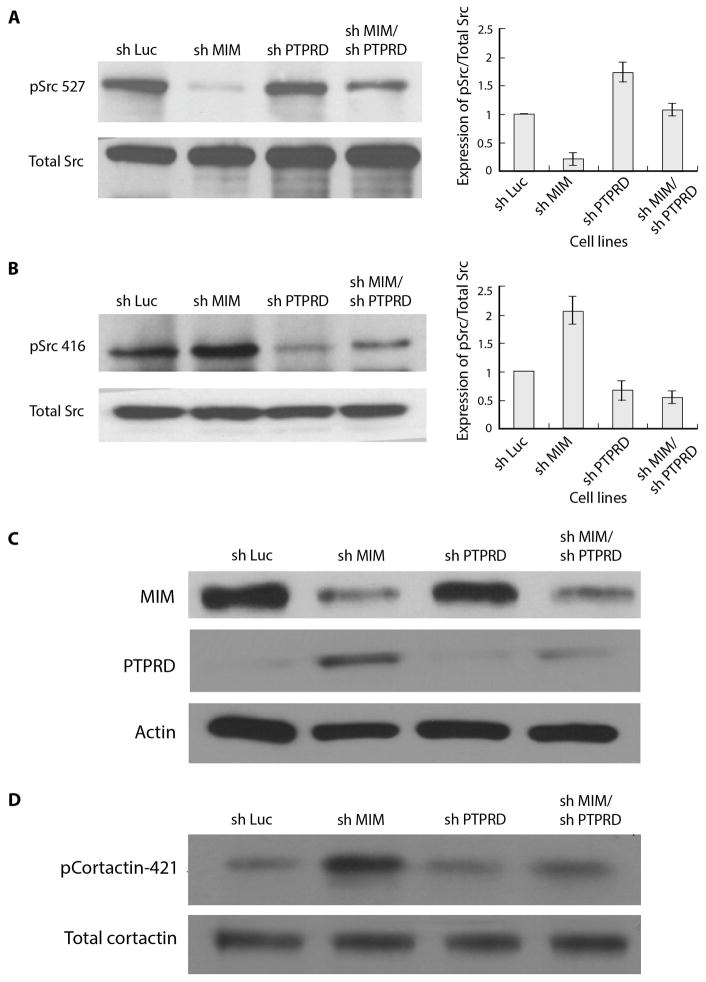
The invasion phenotype induced by loss of MIM was mediated by activation of SRC
MIM regulates sonic hedgehog signaling and promotes ciliogenesis by antagonizing SRC-dependent phosphorylation of cortactin [37]. SRC contains an N-terminal myristoyl group, an SH3 domain, an SH2 domain, a protein tyrosine kinase domain, and a C-terminal regulatory tail [38]. Under basal conditions, 90% of SRC is phosphorylated at Tyr 527 in the C-terminal tail, which undergoes intramolecular association with the SH2 domain, blocking substrate binding and thereby rendering SRC inactive [39]. Dephosphorylation of Tyr 527 represents an important mechanism for SRC activation, being accompanied by autophosphorylation at Tyr 416 in the activation loop, which promotes kinase activity. When we examined the phosphorylation status of SRC in MIM-depleted cells, we observed that phosphorylation at Tyr 527 was markedly decreased (Fig 6A), whereas autophosphorylation on Tyr 416 was enhanced (Fig 6B). These effects were accompanied by the expected changes in levels of MIM and PTPδ (Fig 6C). Furthermore, suppression of MIM was accompanied by enhanced phosphorylation of Tyr 421 in cortactin, a direct substrate of SRC (Fig 6D). These data are consistent with an activating role for PTPδ in the regulation of SRC.
Figure 6. Suppression of MIM led to activation of the protein tyrosine kinase SRC.
(A) SRC was immunoprecipitated from lysates of MCF10A cells expressing the indicated shRNA and blotted for the presence of phosphate on Tyr 527. Right panel: immunoblots from three independent experiments were quantitated. Error bars represent S.E.M (n=3). (B) SRC was immunoprecipitated from lysates of MCF10A cells expressing the indicated shRNA and blotted for the presence of phosphate on Tyr 416. Right panel: immunoblots from three independent experiments were quantitated. Error bars represent S.E.M (n=3). (C) RNAi-mediated suppression of MIM and PTPδ was measured by immunoblotting cell lysates with MIM and PTPδ antibodies, using actin as a loading control. (D) Cortactin was immunoprecipitated from lysates of MCF10A cells expressing the indicated shRNA and blotted for phosphorylation of Tyr 421.
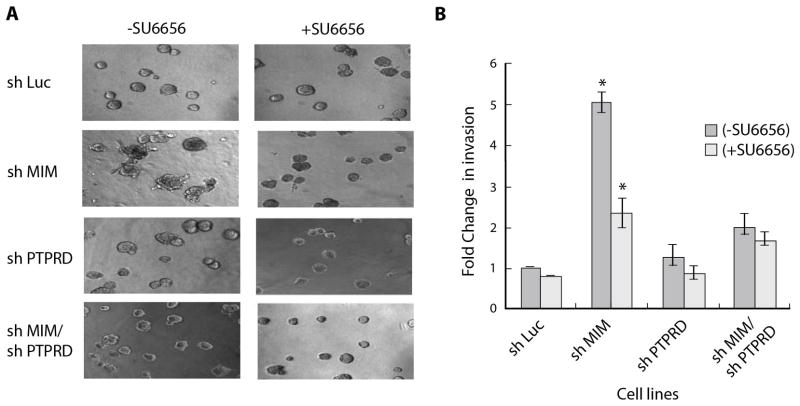
MIM functioned through SRC family kinases to regulate cell motility and invasion
To test whether SRC activity was essential for the enhanced cell invasion that accompanies MIM suppression, we tested the effect of the inhibitor SU6656 [40] on formation of invasive structures in 3D culture. We observed that this SRC inhibitor attenuated cell invasion that was induced by suppression of MIM (Fig 7A). Furthermore, inhibition of SRC with SU6656 was sufficient to antagonize the effect of MIM suppression measured in quantitative cell invasion assays (Fig 7B). These observations highlight the importance of SRC as a mediator of the effects of MIM loss on cell invasion.
Figure 7. Invasion induced by suppression of MIM was blocked by SU6656, an inhibitor of SRC.
(A) Phase images of cells treated in the presence or absence of SU6656 (5μM) taken at Day 6. (B) The invasion of the MCF10A cells that expressed the indicated shRNAs was quantitated in coated transwell chambers in the absence or presence of SU6656 (5μM). Data are presented as change in cell invasion relative to the luciferase control in the absence of SU6656. Error bars represent S.E.M (n=3). *denotes p value<0.005
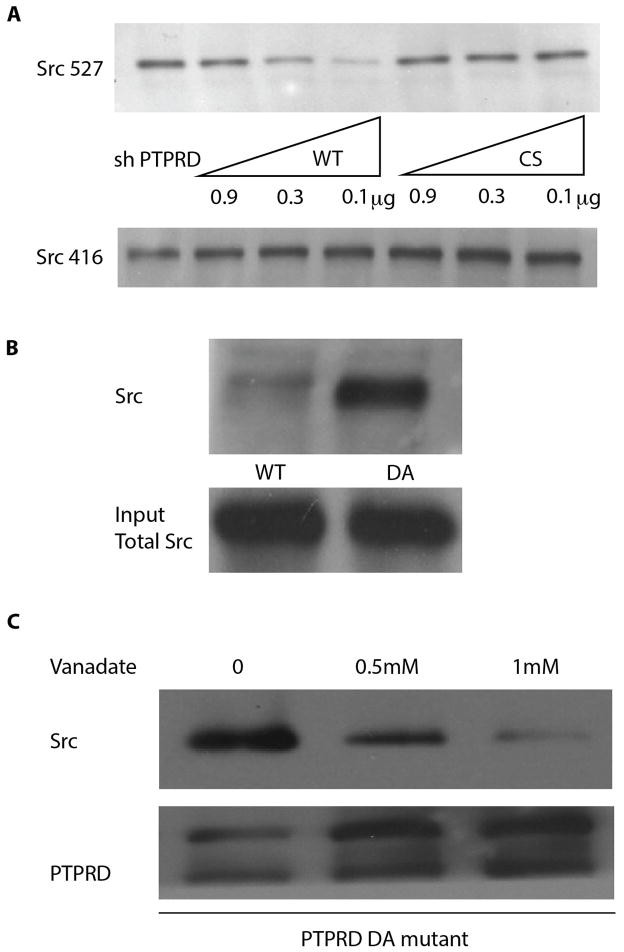
SRC was a direct substrate of PTPδ
To test whether there was an enzyme-substrate relationship, we investigated whether PTPδ directly dephosphorylated SRC in vitro. We immunoprecipitated SRC from lysates of pervanadate-treated MCF10A cells that expressed shRNA directed against either PTPδ (to promote phosphorylation at Tyr 527) or MIM (to promote phosphorylation at Tyr 416). The immunoprecipitated SRC was then incubated with wild-type, active PTPδ or the catalytically dead CS mutant, and the extent of dephosphorylation was measured using specific antibodies. Immunoblots revealed that PTPδ specifically dephosphorylated SRC at Tyr 527 (Fig 8A).
Figure 8. Identification of SRC as a direct substrate of PTPδ.
(A) SRC was immunoprecipitated from lysates from MCF10A cells treated either with shPTPRD (for enhanced phosphorylation of Tyr 527) or shMIM (for enhanced phosphorylation of Tyr 416). The immunoprecipitates were treated with recombinant PTPδ, either active wild type (WT) or inactive (CS) mutant proteins, as indicated. Proteins were resolved by SDS-PAGE and immunoblotted using phospho-specific antibodies to Tyr 527 and Tyr 416. (B) MCF10A cells expressing WT and DA mutant were treated with 50 μM pervanadate for 30 minutes. PTPδ was immunoprecipitated, then protein complexes were analyzed by SDS-PAGE and immunoblotted with anti-SRC antibody. (C) Immunoblot analysis of the association of SRC with PTPδ substrate trapping mutant from cell lysates prepared in the absence and presence of vanadate (0.5mM and 1mM).
Earlier work from our laboratory revealed that mutation of Asp 181 to Ala abolishes the catalytic activity of PTP1B, but maintains its binding affinity for substrates, thus producing a substrate-trapping mutant form of the enzyme [41]. Using this strategy we generated a substrate-trapping mutant form of PTPδ. Wild type PTPδ and the substrate-trapping (DA) mutant were expressed in MCF10A cells, immunoprecipitated from cell lysates and probed with an anti-SRC antibody. A stable interaction between the trapping mutant and SRC was observed, but not between wild type PTPδ and SRC (Fig 8B). To examine whether the interaction of SRC with the PTPδ substrate-trapping mutant occurred through the PTP active site, we included sodium orthovanadate. Vanadate is a competitive inhibitor and transition state analog of phosphate that binds at the PTP active site and competes with substrate for binding to the enzyme [42]. We observed that the interaction of SRC with PTPδ was inhibited by vanadate (Fig 8C). In summary, these data illustrate that the effects of suppressing MIM on cell migration and invasion are mediated by the direct dephosphorylation and activation of SRC by PTPδ.
DISCUSSION
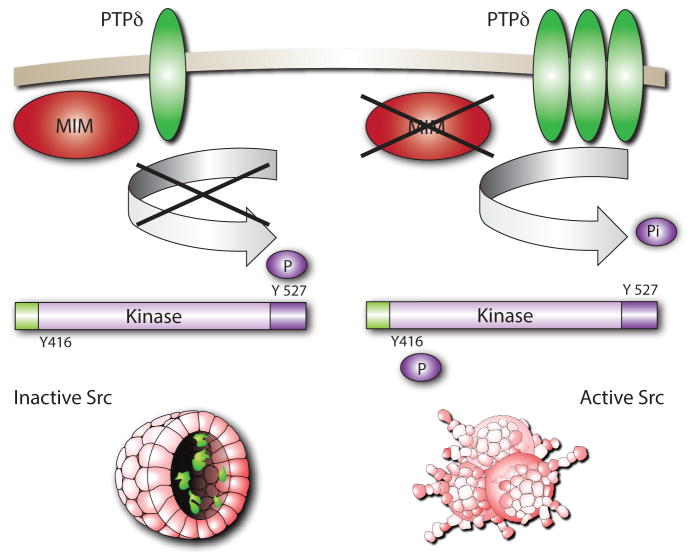
Our data demonstrate that the increased levels of PTPδ in MIM-depleted cells provide a direct link to tyrosine phosphorylation-dependent signaling and the switch to a more invasive state. On this basis, we propose a model that illustrates a mechanism by which MIM and PTPδ may regulate breast epithelial cell motility and invasion (Fig 9). In the absence of MIM, the levels of PTPδ protein were increased, which in turn promoted dephosphorylation of Tyr 527, the inhibitory site in the C-terminal tail of SRC. This was associated with autophosphorylation at Tyr 416 and activation of SRC. These data suggest that under normal conditions, MIM functions to suppress the levels of PTPδ and thereby to suppress SRC activation, motility and invasion of breast epithelial cells.
Figure 9.
Model to explain the relationship between expression of MIM and PTPδ-induced activation of SRC.
MIM as a metastasis suppressor
Metastasis is a major cause of morbidity and mortality in developed countries. Mortality associated with breast cancer has declined considerably due to early diagnosis and improvements in current therapies. Nevertheless, disease recurrence and the transition to metastasis still remain a challenge. MIM is widely expressed in human and mouse tissues, suggesting a potential to exert effects broadly in multiple cancer contexts. It was originally defined by the fact that its transcript was missing in metastatic cells, but not in the non-metastatic counterparts, with methylation of CpG islands thought to play an important role in silencing. Consequently, a biomarker such as MIM may prove to be a valuable tool for detection of metastasis. Furthermore, loss of MIM, and the activation of PTPδ/SRC-dependent signaling, may define a signature that would permit specific targeting of that population of metastatic cells. However, expression analyses have revealed situations in which MIM may be down-regulated more generally in tumor cells, rather than exclusively in metastasis [9]. Nevertheless, the absence of MIM could still provide a defining signature that would facilitate specific targeting of such tumor cells.
PTPδ as a SRC phosphatase
SRC is a critical regulator of signaling pathways that affect cell migration, adhesion and invasion. We have demonstrated that the enhanced cell migration and cell invasion that is a consequence of suppression of MIM resulted from increased levels of PTPδ, which catalyzed the dephosphorylation and activation of SRC. As such, PTPδ joins those members of the PTP family with the ability to regulate the activation status of SRC. PTP-mediated regulation of SRC is complex, due to the ability of these enzymes to control the phosphorylation status of both activating and inhibitory sites. Initially, expression of another receptor PTP, PTPα, was shown to transform rat embryo fibroblasts through dephosphorylation and activation of SRC [43]. The prototypic receptor PTP, CD45, was also shown to act positively to promote antigen receptor signaling through dephosphorylation and activation of SRC family PTKs [11, 12]. Non-transmembrane PTPs, including PTP1B [44] have also been reported to function as activators of SRC by dephosphorylating the C-terminal Tyr 527 residue. In contrast, other phosphatases, such as PTPN23 [45] and PTP-BAS [46], have been shown to dephosphorylate SRC at its autophosphorylation site, thus antagonizing SRC activity. Therefore, the members of the PTP family offer a mechanism for fine control over the signaling function of SRC. Overexpression of SRC is observed in many cancers, including breast cancer [47]; however, overexpression or hyperactivation of SRC in transgenic mouse models is not sufficient to induce a higher grade of breast tumor and metastasis [48]. In contrast, transgenic overexpression of SRC in a p21−/− background dramatically induces tumor growth and metastasis, suggesting that the combination with a second hit may augment the transforming activity of SRC [49]. Considering the positive effect of PTPδ on SRC activity, loss of MIM may promote tumor growth and metastasis particularly in breast tumors in which SRC is overexpressed.
PTPδ as a tumor suppressor or oncogene
When one considers the prevalence of PTKs as oncoproteins, it was anticipated that PTPs, through their catalysis of the complementary dephosphorylation step, would serve as tumor suppressors. Now we know that several PTPs exert a tumor suppressor function. In fact, detailed sequence analyses of members of the PTP family have revealed a wide variety of mutations in PTP genes in various cancers [50]. The PTPRD gene, encoding PTPδ, is one such example [22, 23]. In this case, in addition to mutations that would be predicted to inactivate catalytic function, the clustering of mutations in the portion of the gene encoding the extracellular segment of the protein highlights the potential importance of interactions with ligands in the regulation of activity. Nevertheless, it is also now apparent that PTPs have the capacity to function positively to promote signaling. Furthermore, aberrant upregulation of PTP genes has been detected in multiple cancers, indicative of an oncogenic function [11, 12]. An excellent example is the SH2 domain-containing PTP SHP2, which is encoded by the PTPN11 gene. SHP2, which normally facilitates RAS activation, exists in a low activity state under basal conditions and is activated following interaction of its SH2 domains with pTyr residues on proteins that target the PTP to signaling complexes. Activating somatic mutations in PTPN11/SHP2 allow the enzyme to adopt the active conformation in the absence of the normal stimulus and have been associated with hyperactivation of MAPK and other signaling pathways and increased risk of sporadic childhood malignancies, such as juvenile myelomonocytic leukemia and acute myeloid leukemia [51]. Another example is the PTPN1 gene, which is located at chromosome 20q13, a region that is frequently amplified in breast cancer and associated with poor prognosis. It has also been reported that PTP1B is over-expressed in breast tumors together with the oncoprotein tyrosine kinase HER2. Mice expressing activated alleles of HER2 in mammary glands develop multiple mammary tumors and frequent metastases to the lung; however, when such mice were crossed with Ptpn1-knockout mice, tumor development was delayed and the incidence of lung metastases was decreased [52, 53]. Conversely, targeted overexpression of PTP1B alone was sufficient to drive mammary tumorigenesis in mice [52], illustrating that it can play a positive role in promoting signaling events associated with breast tumorigenesis. A similar tumor-promoting role was suggested in prostate cancer [54]. Nevertheless, SHP2 functions as a tumor suppressor in cartilage [55] and PTP1B has also been shown to exhibit tumor suppressive effects, for example in lymphomagenesis in a p53-deficient background [56]. Consequently, there is precedent for members of the PTP family to function as a tumor suppressor, a tumor promoter or both, depending upon context.
To date, somatic mutations in the PTPRD gene have been reported in diverse tumors [22, 24] and germline mutations of PTPRD have been found in metastatic Ewing sarcoma [57]. Also, PTPδ has been reported to exhibit tumor suppressor activity through inhibition of STAT3 activation [24]. Nevertheless, there have been conflicting reports of both tumor suppressor and tumor promoter functions of PTPδ in neuroblastoma [24, 28]. Our study is consistent with a tumor promoting function of PTPδ through dephosphorylation and activation of SRC. Data from the Human Protein Atlas, which indicated elevated expression of PTPδ in tumor samples from patients, compared to normal breast tissue, are also consistent with such a positive role in the regulation of signaling in breast cancer cells. This raises the exciting possibility that such positively acting PTPs as PTPδ may prove to be important therapeutic targets for new ways to intervene in cancer.
Therapeutic implications and conclusions
SRC has been established as a critical regulator of multiple signaling pathways involved in cell proliferation, survival, angiogenesis and metastasis [58]. Elevated levels and activity of SRC protein have been reported in several cancers, including breast cancer, and the extent of overexpression and hyperactivation correlates with metastatic potential, particularly in colon and breast cancer [59]. In addition, SRC activation has been associated with increased signaling through growth factor receptors, GPCRs or hormone receptors and influences multiple stages of tumor growth and progression [60]. Consequently, multiple SRC inhibitors are currently being assessed as therapeutics [61]. Although these approaches show potential, all PTK-directed therapies have encountered the problems of limited response and acquired resistance [62], and combinatorial approaches are being considered to try and overcome this. Combinatorial therapies involving SRC inhibitors and chemotherapy are in trials in various settings of metastatic cancer [63]; however, combination strategies that facilitate a more targeted intervention in particular signaling pathways may be of greatest benefit. In addition, it will be extremely important to identify those patient populations that would benefit most from SRC-directed therapies. Overall, this study suggests that patients with tumor or metastatic lesions defined by loss of MIM may be one such population. Furthermore, our work suggests that targeting such metastases with combinations of inhibitors of SRC and PTPδ may be more effective in abrogating the signals that underlie aberrant cell invasion than targeting either the PTK or the PTP alone. Although several members of the PTP family have been validated as therapeutic targets, they remain underexploited in large part due to the challenge of developing active site-directed inhibitors with drug development potential. Nevertheless, recent studies have highlighted the potential importance of dimerization in the inactivation of receptor PTPs [64, 65]. Consequently it may be possible to design agents that target the extracellular segment of RPTPs and antagonize RPTP function indirectly via regulation of dimerization. This raises the possibility of producing therapeutic agents that act via the extracellular segment of PTPδ, which may offer a new approach, together with inhibitors of SRC, to targeting specifically the MIM-depleted population of metastatic cells.
Acknowledgments
We thank Dr. Timothy Chan (Memorial Sloan Kettering Cancer Center, NY) for providing us with a GST-PTPRD construct and Dr. Todd Waldman (Georgetown University, Washington DC) for the pcdF1-PTPRD construct. We thank Dr. Gaofeng Fan, Dr. Michael Feigin and Dr. Senthil Muthuswamy for helpful discussions. Also, we thank James Duffy from the CSHL Graphics Department for assistance with the figures.
FUNDING
This research was supported by NIH grant CA53840 to N.K.T. and the CSHL Cancer Centre Support Grant CA45508. N.K.T. is also grateful for support from the following foundations: Joni Gladowsky Breast Cancer Foundation, The Don Monti Memorial Research Foundation, Hansen Memorial Foundation, West Islip Breast Cancer Coalition for Long Island, Glen Cove CARES, Find a Cure Today (FACT), Constance Silveri, Robertson Research Fund and the Masthead Cove Yacht Club Carol Marcincuk Fund.
ABBREVIATIONS
- MIM
Missing in Metastasis/MTSS1
- PTP
protein tyrosine phosphatase
- PTK
protein tyrosine kinase
- shRNA
short hairpin RNA
Footnotes
AUTHOR CONTRIBUTIONS
FC performed the experiments, FC, RL and NKT designed the experiments, analyzed and interpreted the data and wrote the manuscript. NKT directed the study.
COMPETING FINANCIAL INTERETS
All contributors declare that they have no financial or other conflicts of interest.
References
- 1.Weigelt B, Peterse JL, van‘t Veer LJ. Breast cancer metastasis: markers and models. Nat Rev Cancer. 2005;5:591–602. doi: 10.1038/nrc1670. [DOI] [PubMed] [Google Scholar]
- 2.Valastyan S, Weinberg RA. Tumor metastasis: molecular insights and evolving paradigms. Cell. 2011;147:275–292. doi: 10.1016/j.cell.2011.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith SC, Theodorescu D. Learning therapeutic lessons from metastasis suppressor proteins. Nat Rev Cancer. 2009;9:253–264. doi: 10.1038/nrc2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parr C, Jiang WG. Metastasis suppressor 1 (MTSS1) demonstrates prognostic value and anti-metastatic properties in breast cancer. Eur J Cancer. 2009;45:1673–1683. doi: 10.1016/j.ejca.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 5.Lee YG, Macoska JA, Korenchuk S, Pienta KJ. MIM, a potential metastasis suppressor gene in bladder cancer. Neoplasia. 2002;4:291–294. doi: 10.1038/sj.neo.7900231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nixdorf S, Grimm MO, Loberg R, Marreiros A, Russell PJ, Pienta KJ, Jackson P. Expression and regulation of MIM (Missing In Metastasis), a novel putative metastasis suppressor gene, and MIM-B, in bladder cancer cell lines. Cancer Lett. 2004;215:209–220. doi: 10.1016/j.canlet.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Xie F, Ye L, Ta M, Zhang L, Jiang WG. MTSS1: a multifunctional protein and its role in cancer invasion and metastasis. Front Biosci (Schol Ed) 2011;3:621–631. doi: 10.2741/s175. [DOI] [PubMed] [Google Scholar]
- 8.Mertz KD, Pathria G, Wagner C, Saarikangas J, Sboner A, Romanov J, Gschaider M, Lenz F, Neumann F, Schreiner W, Nemethova M, Glassmann A, Lappalainen P, Stingl G, Small JV, Fink D, Chin L, Wagner SN. MTSS1 is a metastasis driver in a subset of human melanomas. Nat Commun. 2014;5:3465. doi: 10.1038/ncomms4465. [DOI] [PubMed] [Google Scholar]
- 9.Machesky LM, Johnston SA. MIM: a multifunctional scaffold protein. J Mol Med (Berl) 2007;85:569–576. doi: 10.1007/s00109-007-0207-0. [DOI] [PubMed] [Google Scholar]
- 10.Woodings JA, Sharp SJ, Machesky LM. MIM-B, a putative metastasis suppressor protein, binds to actin and to protein tyrosine phosphatase delta. Biochem J. 2003;371:463–471. doi: 10.1042/BJ20021962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tonks NK. Protein tyrosine phosphatases: from genes, to function, to disease. Nat Rev Mol Cell Biol. 2006;7:833–846. doi: 10.1038/nrm2039. [DOI] [PubMed] [Google Scholar]
- 12.Tonks NK. Protein tyrosine phosphatases--from housekeeping enzymes to master regulators of signal transduction. The FEBS journal. 2013;280:346–378. doi: 10.1111/febs.12077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hendriks WJ, Elson A, Harroch S, Pulido R, Stoker A, den Hertog J. Protein tyrosine phosphatases in health and disease. FEBS J. 2013;280:708–730. doi: 10.1111/febs.12000. [DOI] [PubMed] [Google Scholar]
- 14.Stepanek L, Stoker AW, Stoeckli E, Bixby JL. Receptor tyrosine phosphatases guide vertebrate motor axons during development. J Neurosci. 2005;25:3813–3823. doi: 10.1523/JNEUROSCI.4531-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uetani N, Chagnon MJ, Kennedy TE, Iwakura Y, Tremblay ML. Mammalian motoneuron axon targeting requires receptor protein tyrosine phosphatases sigma and delta. J Neurosci. 2006;26:5872–5880. doi: 10.1523/JNEUROSCI.0386-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Serra-Pages C, Kedersha NL, Fazikas L, Medley Q, Debant A, Streuli M. The LAR transmembrane protein tyrosine phosphatase and a coiled-coil LAR-interacting protein co-localize at focal adhesions. EMBO J. 1995;14:2827–2838. doi: 10.1002/j.1460-2075.1995.tb07282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krueger NX, VanVactor D, Wan HI, Gelbart WM, Goodman CS, Saito H. The transmembrane tyrosine phosphatase DLAR controls motor axon guidance in Drosophila. Cell. 1996;84:611–622. doi: 10.1016/s0092-8674(00)81036-3. [DOI] [PubMed] [Google Scholar]
- 18.Schaapveld RQ, Schepens JT, Robinson GW, Attema J, Oerlemans FT, Fransen JA, Streuli M, Wieringa B, Hennighausen L, Hendriks WJ. Impaired mammary gland development and function in mice lacking LAR receptor-like tyrosine phosphatase activity. Dev Biol. 1997;188:134–146. doi: 10.1006/dbio.1997.8630. [DOI] [PubMed] [Google Scholar]
- 19.Sun QL, Wang J, Bookman RJ, Bixby JL. Growth cone steering by receptor tyrosine phosphatase delta defines a distinct class of guidance cue. Mol Cell Neurosci. 2000;16:686–695. doi: 10.1006/mcne.2000.0893. [DOI] [PubMed] [Google Scholar]
- 20.Wang J, Bixby JL. Receptor tyrosine phosphatase-delta is a homophilic, neurite-promoting cell adhesion molecule for CNS neurons. Mol Cell Neurosci. 1999;14:370–384. doi: 10.1006/mcne.1999.0789. [DOI] [PubMed] [Google Scholar]
- 21.Gonzalez-Brito MR, Bixby JL. Differential activities in adhesion and neurite growth of fibronectin type III repeats in the PTP-delta extracellular domain. Int J Dev Neurosci. 2006;24:425–429. doi: 10.1016/j.ijdevneu.2006.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Solomon DA, Kim JS, Cronin JC, Sibenaller Z, Ryken T, Rosenberg SA, Ressom H, Jean W, Bigner D, Yan H, Samuels Y, Waldman T. Mutational inactivation of PTPRD in glioblastoma multiforme and malignant melanoma. Cancer Res. 2008;68:10300–10306. doi: 10.1158/0008-5472.CAN-08-3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambert SR, Harwood CA, Purdie KJ, Gulati A, Matin RN, Romanowska M, Cerio R, Kelsell DP, Leigh IM, Proby CM. Metastatic cutaneous squamous cell carcinoma shows frequent deletion in the protein tyrosine phosphatase receptor Type D gene. Int J Cancer. 2012;131:E216–226. doi: 10.1002/ijc.27333. [DOI] [PubMed] [Google Scholar]
- 24.Veeriah S, Brennan C, Meng S, Singh B, Fagin JA, Solit DB, Paty PB, Rohle D, Vivanco I, Chmielecki J, Pao W, Ladanyi M, Gerald WL, Liau L, Cloughesy TC, Mischel PS, Sander C, Taylor B, Schultz N, Major J, Heguy A, Fang F, Mellinghoff IK, Chan TA. The tyrosine phosphatase PTPRD is a tumor suppressor that is frequently inactivated and mutated in glioblastoma and other human cancers. Proc Natl Acad Sci U S A. 2009;106:9435–9440. doi: 10.1073/pnas.0900571106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stallings RL, Nair P, Maris JM, Catchpoole D, McDermott M, O’Meara A, Breatnach F. High-resolution analysis of chromosomal breakpoints and genomic instability identifies PTPRD as a candidate tumor suppressor gene in neuroblastoma. Cancer Res. 2006;66:3673–3680. doi: 10.1158/0008-5472.CAN-05-4154. [DOI] [PubMed] [Google Scholar]
- 26.Molenaar JJ, Koster J, Zwijnenburg DA, van Sluis P, Valentijn LJ, van der Ploeg I, Hamdi M, van Nes J, Westerman BA, van Arkel J, Ebus ME, Haneveld F, Lakeman A, Schild L, Molenaar P, Stroeken P, van Noesel MM, Ora I, Santo EE, Caron HN, Westerhout EM, Versteeg R. Sequencing of neuroblastoma identifies chromothripsis and defects in neuritogenesis genes. Nature. 2012;483:589–593. doi: 10.1038/nature10910. [DOI] [PubMed] [Google Scholar]
- 27.Uetani N, Kato K, Ogura H, Mizuno K, Kawano K, Mikoshiba K, Yakura H, Asano M, Iwakura Y. Impaired learning with enhanced hippocampal long-term potentiation in PTPdelta-deficient mice. EMBO J. 2000;19:2775–2785. doi: 10.1093/emboj/19.12.2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clark O, Schmidt F, Coles CH, Tchetchelnitski V, Stoker AW. Functional analysis of the putative tumor suppressor PTPRD in neuroblastoma cells. Cancer Investigation. 2012;30:422–432. doi: 10.3109/07357907.2012.675383. [DOI] [PubMed] [Google Scholar]
- 29.Li S, Hsu DD, Wang H, Feng GS. Dual faces of SH2-containing protein-tyrosine phosphatase Shp2/PTPN11 in tumorigenesis. Frontiers of medicine. 2012;6:275–279. doi: 10.1007/s11684-012-0216-4. [DOI] [PubMed] [Google Scholar]
- 30.Lessard L, Stuible M, Tremblay ML. The two faces of PTP1B in cancer. Biochim Biophys Acta. 2010;1804:613–619. doi: 10.1016/j.bbapap.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 31.Xiang B, Muthuswamy SK. Using three-dimensional acinar structures for molecular and cell biological assays. Methods in enzymology. 2006;406:692–701. doi: 10.1016/S0076-6879(06)06054-X. [DOI] [PubMed] [Google Scholar]
- 32.Iizuka M, Inoue Y, Murata K, Kimura A. Purification and some properties of glutathione S-transferase from Escherichia coli B. J Bacteriol. 1989;171:6039–6042. doi: 10.1128/jb.171.11.6039-6042.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Debnath J, Muthuswamy SK, Brugge JS. Morphogenesis and oncogenesis of MCF-10A mammary epithelial acini grown in three-dimensional basement membrane cultures. Methods. 2003;30:256–268. doi: 10.1016/s1046-2023(03)00032-x. [DOI] [PubMed] [Google Scholar]
- 34.Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A, Hallett M, Park M. Stromal gene expression predicts clinical outcome in breast cancer. Nat Med. 2008;14:518–527. doi: 10.1038/nm1764. [DOI] [PubMed] [Google Scholar]
- 35.Uhlen M, Oksvold P, Fagerberg L, Lundberg E, Jonasson K, Forsberg M, Zwahlen M, Kampf C, Wester K, Hober S, Wernerus H, Bjorling L, Ponten F. Towards a knowledge-based Human Protein Atlas. Nature biotechnology. 2010;28:1248–1250. doi: 10.1038/nbt1210-1248. [DOI] [PubMed] [Google Scholar]
- 36.Parris TZ, Kovacs A, Hajizadeh S, Nemes S, Semaan M, Levin M, Karlsson P, Helou K. Frequent MYC coamplification and DNA hypomethylation of multiple genes on 8q in 8p11-p12-amplified breast carcinomas. Oncogenesis. 2014;3:e95. doi: 10.1038/oncsis.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bershteyn M, Atwood SX, Woo WM, Li M, Oro AE. MIM and cortactin antagonism regulates ciliogenesis and hedgehog signaling. Developmental cell. 2010;19:270–283. doi: 10.1016/j.devcel.2010.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roskoski R., Jr Src kinase regulation by phosphorylation and dephosphorylation. Biochem Biophys Res Commun. 2005;331:1–14. doi: 10.1016/j.bbrc.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 39.Zheng XM, Resnick RJ, Shalloway D. A phosphotyrosine displacement mechanism for activation of Src by PTPalpha. EMBO J. 2000;19:964–978. doi: 10.1093/emboj/19.5.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blake RA, Broome MA, Liu X, Wu J, Gishizky M, Sun L, Courtneidge SA. SU6656, a selective src family kinase inhibitor, used to probe growth factor signaling. Mol Cell Biol. 2000;20:9018–9027. doi: 10.1128/mcb.20.23.9018-9027.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Flint AJ, Tiganis T, Barford D, Tonks NK. Development of “substrate-trapping” mutants to identify physiological substrates of protein tyrosine phosphatases. Proc Natl Acad Sci U S A. 1997;94:1680–1685. doi: 10.1073/pnas.94.5.1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huyer G, Liu S, Kelly J, Moffat J, Payette P, Kennedy B, Tsaprailis G, Gresser MJ, Ramachandran C. Mechanism of inhibition of protein-tyrosine phosphatases by vanadate and pervanadate. J Biol Chem. 1997;272:843–851. doi: 10.1074/jbc.272.2.843. [DOI] [PubMed] [Google Scholar]
- 43.Zheng XM, Wang Y, Pallen CJ. Cell transformation and activation of pp60c-src by overexpression of a protein tyrosine phosphatase. Nature. 1992;359:336–339. doi: 10.1038/359336a0. [DOI] [PubMed] [Google Scholar]
- 44.Bjorge JD, Pang A, Fujita DJ. Identification of protein-tyrosine phosphatase 1B as the major tyrosine phosphatase activity capable of dephosphorylating and activating c-Src in several human breast cancer cell lines. The Journal of biological chemistry. 2000;275:41439–41446. doi: 10.1074/jbc.M004852200. [DOI] [PubMed] [Google Scholar]
- 45.Lin G, Aranda V, Muthuswamy SK, Tonks NK. Identification of PTPN23 as a novel regulator of cell invasion in mammary epithelial cells from a loss-of-function screen of the ‘PTP-ome’. Genes & development. 2011;25:1412–1425. doi: 10.1101/gad.2018911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Palmer A, Zimmer M, Erdmann KS, Eulenburg V, Porthin A, Heumann R, Deutsch U, Klein R. EphrinB phosphorylation and reverse signaling: regulation by Src kinases and PTP-BL phosphatase. Mol Cell. 2002;9:725–737. doi: 10.1016/s1097-2765(02)00488-4. [DOI] [PubMed] [Google Scholar]
- 47.Irby RB, Yeatman TJ. Role of Src expression and activation in human cancer. Oncogene. 2000;19:5636–5642. doi: 10.1038/sj.onc.1203912. [DOI] [PubMed] [Google Scholar]
- 48.Dimri M, Naramura M, Duan L, Chen J, Ortega-Cava C, Chen G, Goswami R, Fernandes N, Gao Q, Dimri GP, Band V, Band H. Modeling breast cancer-associated c-Src and EGFR overexpression in human MECs: c-Src and EGFR cooperatively promote aberrant three-dimensional acinar structure and invasive behavior. Cancer Res. 2007;67:4164–4172. doi: 10.1158/0008-5472.CAN-06-2580. [DOI] [PubMed] [Google Scholar]
- 49.Kline CL, Jackson R, Engelman R, Pledger WJ, Yeatman TJ, Irby RB. Src kinase induces tumor formation in the c-SRC C57BL/6 mouse. Int J Cancer. 2008;122:2665–2673. doi: 10.1002/ijc.23445. [DOI] [PubMed] [Google Scholar]
- 50.Julien SG, Dube N, Hardy S, Tremblay ML. Inside the human cancer tyrosine phosphatome. Nat Rev Cancer. 2011;11:35–49. doi: 10.1038/nrc2980. [DOI] [PubMed] [Google Scholar]
- 51.Tartaglia M, Niemeyer CM, Fragale A, Song X, Buechner J, Jung A, Hahlen K, Hasle H, Licht JD, Gelb BD. Somatic mutations in PTPN11 in juvenile myelomonocytic leukemia, myelodysplastic syndromes and acute myeloid leukemia. Nat Genet. 2003;34:148–150. doi: 10.1038/ng1156. [DOI] [PubMed] [Google Scholar]
- 52.Julien SG, Dube N, Read M, Penney J, Paquet M, Han Y, Kennedy BP, Muller WJ, Tremblay ML. Protein tyrosine phosphatase 1B deficiency or inhibition delays ErbB2-induced mammary tumorigenesis and protects from lung metastasis. Nat Genet. 2007;39:338–346. doi: 10.1038/ng1963. [DOI] [PubMed] [Google Scholar]
- 53.Bentires-Alj M, Neel BG. Protein-tyrosine phosphatase 1B is required for HER2/Neu-induced breast cancer. Cancer Res. 2007;67:2420–2424. doi: 10.1158/0008-5472.CAN-06-4610. [DOI] [PubMed] [Google Scholar]
- 54.Lessard L, Labbe DP, Deblois G, Begin LR, Hardy S, Mes-Masson AM, Saad F, Trotman LC, Giguere V, Tremblay ML. PTP1B is an androgen receptor-regulated phosphatase that promotes the progression of prostate cancer. Cancer Res. 2012;72:1529–1537. doi: 10.1158/0008-5472.CAN-11-2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang W, Wang J, Moore DC, Liang H, Dooner M, Wu Q, Terek R, Chen Q, Ehrlich MG, Quesenberry PJ, Neel BG. Ptpn11 deletion in a novel progenitor causes metachondromatosis by inducing hedgehog signalling. Nature. 2013;499:491–495. doi: 10.1038/nature12396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dube N, Bourdeau A, Heinonen KM, Cheng A, Loy AL, Tremblay ML. Genetic ablation of protein tyrosine phosphatase 1B accelerates lymphomagenesis of p53-null mice through the regulation of B-cell development. Cancer Res. 2005;65:10088–10095. doi: 10.1158/0008-5472.CAN-05-1353. [DOI] [PubMed] [Google Scholar]
- 57.Jiang Y, Janku F, Subbiah V, Angelo LS, Naing A, Anderson PM, Herzog CE, Fu S, Benjamin RS, Kurzrock R. Germline PTPRD mutations in Ewing sarcoma: biologic and clinical implications. Oncotarget. 2013;4:884–889. doi: 10.18632/oncotarget.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim LC, Song L, Haura EB. Src kinases as therapeutic targets for cancer. Nat Rev Clin Oncol. 2009;6:587–595. doi: 10.1038/nrclinonc.2009.129. [DOI] [PubMed] [Google Scholar]
- 59.Elsberger B. Translational evidence on the role of Src kinase and activated Src kinase in invasive breast cancer. Crit Rev Oncol Hematol. 2014;89:343–351. doi: 10.1016/j.critrevonc.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 60.Tice DA, Biscardi JS, Nickles AL, Parsons SJ. Mechanism of biological synergy between cellular Src and epidermal growth factor receptor. Proc Natl Acad Sci U S A. 1999;96:1415–1420. doi: 10.1073/pnas.96.4.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hiscox S, Nicholson RI. Src inhibitors in breast cancer therapy. Expert opinion on therapeutic targets. 2008;12:757–767. doi: 10.1517/14728222.12.6.757. [DOI] [PubMed] [Google Scholar]
- 62.Sierra JR, Cepero V, Giordano S. Molecular mechanisms of acquired resistance to tyrosine kinase targeted therapy. Mol Cancer. 2010;9:75. doi: 10.1186/1476-4598-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang S, Huang WC, Zhang L, Zhang C, Lowery FJ, Ding Z, Guo H, Wang H, Huang S, Sahin AA, Aldape KD, Steeg PS, Yu D. SRC family kinases as novel therapeutic targets to treat breast cancer brain metastases. Cancer Res. 2013;73:5764–5774. doi: 10.1158/0008-5472.CAN-12-1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hower AE, Beltran PJ, Bixby JL. Dimerization of tyrosine phosphatase PTPRO decreases its activity and ability to inactivate TrkC. J Neurochem. 2009;110:1635–1647. doi: 10.1111/j.1471-4159.2009.06261.x. [DOI] [PubMed] [Google Scholar]
- 65.den Hertog J, Ostman A, Bohmer FD. Protein tyrosine phosphatases: regulatory mechanisms. FEBS J. 2008;275:831–847. doi: 10.1111/j.1742-4658.2008.06247.x. [DOI] [PubMed] [Google Scholar]