Abstract
Traumatic injury remains an unacceptably high contributor to morbidity and mortality rates across the United States. Gender-specific research in trauma and emergency resuscitation has become a rising priority. In concert with the 2014 Academic Emergency Medicine consensus conference “Gender-specific Research in Emergency Care: Investigate, Understand, and Translate How Gender Affects Patient Outcomes,” a consensus-building group consisting of experts in emergency medicine, critical care, traumatology, anesthesiology, and public health convened to generate research recommendations and priority questions to be answered and thus move the field forward. Nominal group technique was used for the consensus-building process and a combination of face-to-face meetings, monthly conference calls, e-mail discussions, and preconference surveys were used to refine the research questions. The resulting research agenda focuses on opportunities to improve patient outcomes by expanding research in sex- and gender-specific emergency care in the field of traumatic injury and resuscitation.
Each year, trauma accounts for 42 million emergency department (ED) visits and 2 million hospital admissions across the nation. It remains the primary cause of death (47% of all deaths) for young individuals (age 1 to 44 years).1 The resulting loss of productive life-years related to trauma exceeds that of any other disease. Trauma systems and trauma care can significantly improve survival and function.
Different trauma outcomes have been identified based on sex, with relative protection afforded to females in most studies. Researchers are now beginning to study novel sex- and gender-specific perspectives in the areas of acute care research, including the specific area of traumatic injury and resuscitation.2 However, these studies have significant limitations, including their retrospective design and the use of data from large trauma registries.3 Furthermore, systematic reviews and meta-analyses on sex disparities in trauma sample only a small amount of the total literature published, which skews the conclusions. Few trauma outcomes studies present data separately by sex, and the bias against publishing negative studies persists. Sex-specific issues in traumatic injury and resuscitation are therefore important to address.
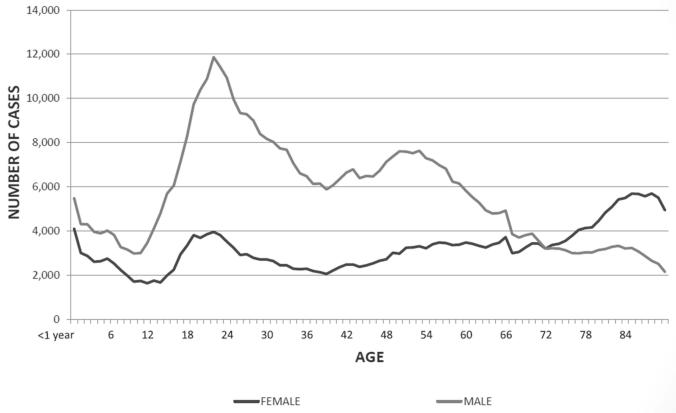
When addressing sex-specific research priorities in traumatic injury and resuscitation, it is important to recognize significant sex-based differences in injury patterns. In 2010, females sustained fewer than half of the fatal injuries in the United States (Table 1), but women and men had similar incidences of nonfatal injuries (Table 2). Male gender is associated with higher case fatality rates when stratified by age, but not by injury type or severity (Table 3, Figures 1 and 2). The design of trauma prevention strategies requires a true appreciation of the significant sex differences in specific injury patterns and outcomes.
Table 1.
Age-adjusted Fatal Injury Rates (per 100,000) All Ages, United States, 2010
| Cause of Death | Female | Male |
|---|---|---|
| All injuries | 33.96 | 81.73 |
| Unintentional | 25.49 | 51.45 |
| Violence | 7.24 | 28.63 |
| Homicide | 2.25 | 8.58 |
| Suicide | 4.99 | 19.78 |
| Transportation* | 6.56 | 16.28 |
| Fall | 6.43 | 10.26 |
Transportation includes cars, motorcycles, bicycles, and pedestrians.
Data from www.cdc.gov/injury/wisqars.
Table 2.
Age-adjusted Nonfatal Injury Rates (per 100,000), All Ages, United States, 2012
| Cause | Female | Male |
|---|---|---|
| All injuries | 9,269.89 | 11,141.01 |
| All unintentional injuries | 8622.94 | 10,285.25 |
| Violence | 855.76 | 646.94 |
| Assault | 449.75 | 672.91 |
| Sexual assault | 49.44 | 5.12 |
| Transportation* | 1277.16 | 1382.76 |
| Self-harm | 188.06 | 127.81 |
Transportation includes cars, motorcycles, bicycles, and pedestrians.
Data from http://www.cdc.gov/injury/wisqars.
Table 3.
Incident and Case Fatality Rate by Age and Sex
| Number |
Deaths |
Case Fatality Rate |
||||
|---|---|---|---|---|---|---|
| Age, years | Female | Male | Female | Male | Female | Male |
| <1 | 4,088 | 5,476 | 81 | 134 | 1.98 | 2.45 |
| 1–4 | 11,088 | 16,440 | 181 | 248 | 1.63 | 1.51 |
| 5–9 | 11,162 | 17,227 | 94 | 152 | 0.84 | 0.88 |
| 10–14 | 8,762 | 21,048 | 91 | 208 | 1.04 | 0.99 |
| 15 -19 | 16,002 | 41,555 | 347 | 1,298 | 2.17 | 3.12 |
| 20–24 | 18,360 | 55,069 | 425 | 2,205 | 2.31 | 4.00 |
| 25–34 | 26,124 | 81,276 | 657 | 3,089 | 2.51 | 3.80 |
| 35–44 | 22,970 | 63,349 | 621 | 2,265 | 2.70 | 3.58 |
| 45–54 | 30,267 | 72,496 | 809 | 2,757 | 2.67 | 3.80 |
| 55–64 | 33,949 | 57,295 | 963 | 2,783 | 2.84 | 4.86 |
| 65–74 | 33,378 | 36,406 | 1,198 | 2,356 | 3.59 | 6.47 |
| 75–84 | 47,084 | 31,372 | 2,477 | 3,057 | 5.26 | 9.74 |
| >84 | 49,264 | 21,512 | 3,386 | 2,694 | 6.87 | 12.52 |
| NK/NR | 10 | 49 | 7 | 25 | 70.00 | 51.02 |
| Total | 312,508 | 520,570 | 11,337 | 23,271 | 3.63 | 4.47 |
Reproduced with permission from the American College of Surgeons, from the National Trauma Data Bank 2013 Annual Report, based on 833,311 records from 2012 admission year from 805 U.S./Canadian hospitals. The complete report is available at www.cdc.gov/injury/wisqars. NK/NR = not known/not reported
Figure 1.
Trauma case fatality rate by age and sex (2013). Reproduced with permission by the American College of Surgeons, from the National Trauma Data Bank 2013 Annual Report, based on 833,311 records from 2012 admission year from 805 U.S./Canadian hospitals. The complete report is available at https://www.facs.org/quality-programs/trauma/ntdb.
Figure 2.
Trauma incidents by age and sex (2013). Reproduced with permission by the American College of Surgeons, from the National Trauma Data Bank 2013 Annual Report, based on 833,311 records from 2012 admission year from 805 U.S./Canadian hospitals. The complete report is available at https://www.facs.org/quality-programs/trauma/ntdb.
METHODS
An iterative consensus process using the nominal group technique was used to generate research priorities. Our workgroup consisted of members representing emergency medicine (EM), critical care, traumatology anesthesiology, and public health. Thirty-nine consensus attendees participated in the trauma breakout group and prioritized the proposed agenda using the Poll Everywhere voting method.
In this consensus article, we recommend the development and rigorous pursuit of four important themes of research focused on sex differences in traumatic injury and resuscitation: 1) prehospital and acute care (including how care providers’ gender influences patient outcomes); 2) trauma outcomes; 3) the influence of sex on coagulation, immunity, and inflammation; and 4) intermediate and long-term care. Consensus was reached for the questions in bold type in the research dimension sections for each of the recommendations. Questions not in boldface type were discussed extensively by the working group and were felt to be areas of considerable importance for research.
PREHOSPITAL AND ACUTE CARE
Recommendation 1
Determine specific factors that contribute to sex-based differences in trauma triage and transfer and acute care, and evaluate patient outcomes in relation to the sex composition of the trauma team.
Discussion
Initial triage to a trauma center leads to better overall outcomes.4 A recent population-based analysis confirmed that the initial transport of trauma patients to nontrauma centers was associated with a 30% increase in mortality during the first 48 hours after injury.5 Additional studies documented a survival benefit among patients who were taken initially to nontertiary trauma centers but later transferred to tertiary trauma centers versus patients who stayed at a nontertiary hospital, even after adjusting for variables affecting the likelihood of transfer. Although the survival benefit was larger for patients treated at a Level I trauma center, Level II trauma centers in a region with few tertiary trauma resources demonstrated a measurable benefit as well.6
Sex differences in access to trauma care have been identified in the prehospital setting, favoring better outcomes for men.7 The reasons might be related to perceived differences in injury severity, assumptions about the likelihood of benefiting from trauma center care, or subconscious gender bias. Additional studies are warranted to study these differences.
In addition to examining patient sex as a variable, it is important to consider the sex of the providers and its effect on trauma teams and trauma patient outcomes. This aspect of research has had minimal investigation in the medical context. It is unknown if a better understanding of team functioning and leadership translates to improved patient outcomes in the trauma setting and if the influence of sex as an essential variable should be investigated in trauma team leadership style and group dynamics.
Research Questions
What are the factors in the acute care trauma system (prehospital and ED) that contribute to sex-based differences in triage and acute treatment of the trauma patient?
Do differences in the behaviors of male and female trauma team leaders and team members affect patient outcomes, perceptions of leadership, and team dynamics?
Are trauma patient outcomes based on congruence if the doctor and patient are of the same sex or different sexes?
Evidence Summary
There is evidence that women are less likely than their male counterparts to be triaged to trauma centers despite having similar severities of injury.7 Both provider and acute care delivery system factors may have a role in explaining the differences in triage decisions according to sex and gender.5 More research is needed to delineate factors related to sex and gender that contribute to disparities in triage decisions for traumatically injured patients.
A Canadian population-based retrospective cohort analysis of severely injured adults (Injury Severity Score > 15, n = 26,861, 35% women) found that women with similar severities of injury to the male cohort were less likely to be triaged to trauma centers in direct transport from the scene and from nontrauma EDs.7 The women in this study were older and had more comorbid conditions. More women had falls from standing in this study, while more men fell from heights. These differences were controlled for in the analysis, but the difference in frequency of triage to a trauma center persisted. Emergency medical services personnel were less likely to transport females from the field to trauma centers (odds ratio [OR] = 0.88, 95% confidence interval [CI] = 0.81 to 0.97). Similarly, physicians were less likely to transfer females to trauma centers (OR = 0.85, 95% CI = 0.73 to 0.99).
Gender role stereotypes may also play a role in health care team dynamics. Studies have indicated that males enact “instrumental” traits and females enact “expressive” traits (Table 4). When reviewers were blinded to the sex of a person during case-based scenarios in nonmedical settings, they made assumptions about the sex of the person based on his or her described attributes. Perceived female leaders using feminine (gender-consistent) style were more highly rated by their peers than perceived female leaders using a masculine (gender-inconsistent) style. In the case of the perceived male leader, the ratings were higher when the style was gender-consistent and when he used a gender-inconsistent style that was in keeping with transformational leadership (Table 4).
Table 4.
Summary of Traditional Gender-related Characteristics
| Characteristic | Female | Male |
|---|---|---|
| Gender-typical traits | Expressive (helpful, understanding, compassionate, sensitive to others’ needs) |
Instrumental (independent, competitive, decisive, aggressive, dominant) |
| Gender-typical behavior | Communal (friendly, unselfish, concerned with others, expressive) |
Agentic (independent, masterful, assertive, instrumentally competent) |
| Leadership style | Transformational (interpersonal, democratic) |
Translational (task oriented, autocratic) |
Table constructed through incorporation of existing gender literature.
Collaborative nurse—physician relationships are associated with decreased risk-adjusted mortality rates and length of stay, fewer negative patient outcomes, and enhanced patient satisfaction in an intensive care unit (ICU) environment.8,9 Unfortunately, disparity has been shown in physician and nurse perceptions of teamwork and communication.10
A collaboration survey was administered to team members after patient resuscitation in a trauma center over a 1-year period.11 Of 92 participants, 61% were physicians and 46% were male. Most practitioners reported high scores for collaboration and satisfaction. Physicians and males rated team collaboration and satisfaction with decisions higher than nurses and females in all domains; however, since gender and profession were highly correlated (32 of 39 physicians were male and 32 of 34 nurses were female), these pilot data make it difficult to separate gender from team member position and warrants more study, which is currently ongoing at the R Adams Cowley Trauma Center.
Female internal medicine residents face the dilemma of “role incongruity,” as effective leadership attributes tend to correlate with stereotypic male qualities.12,13 Residents of both sexes concluded that male residents were viewed as more authoritative, confident, and assertive—a finding consistent with research on gender behavioral norms, leadership, and power differentials in other contexts.
An anthropological pilot study documented gender behavior differences among male and female trauma team members.14 Female leaders performed menial tasks rather than asking team members to assist, whereas males did not. Males were unapologetic about aggressiveness during emergent and nonemergent resuscitations, while females were infrequently aggressive, even if it hindered their ability to view exam results or participate. Females said “please” and “thank you” more often than males. Nonverbal female behavior included body language that established interpersonal dynamics, which acknowledged individual team members, while males addressed the entirety of the space and team as a cohesive unit. The authors of this study did not assess if the behaviors affected team dynamics or patient care during trauma resuscitations.14
In summary, significant gender-based differences have been identified in trauma triage and the delivery of early acute care. More research is needed to delineate gender-related factors that contribute to disparities in the care of traumatically injured patients.
SEX-BASED DIFFERENCES IN TRAUMA OUTCOMES
Recommendation 2
Include gender, race, and sex hormone status as patient-specific variables in trauma outcome studies to determine whether outcome differences are related to gender-based differences in health care delivery or alterations in sex hormones.
Discussion
Studies of the effect of gender on morbidity and mortality after trauma continue to yield conflicting results. Increased mortality has been associated with male gender,15–17 but conflicting results have been reported as well.18–20 Most of these studies are retrospective analyses of trauma registries using multivariate logistic regression to control for variables that can influence trauma outcomes. Relatively small sample sizes might have contributed to the heterogeneity of results in early studies; larger studies confirmed increased mortality rates for men, particularly those more than 50 years of age.15,21–26 The largest prospective cohort study, involving more than 1,400 trauma patients with 5-year follow-up, confirmed female sex as protective for all-cause mortality (OR = 0.57). This study also documented that male trauma patients expressed a more robust proinflammatory cytokine profile, suggesting that a sex-based cytokine response to injury could, in part, be responsible for the mortality differences.27 In contrast to studies investigating sex-based outcomes in blunt trauma, female gender has been associated with increased mortality after burn injury.28–30
In clinical conditions (in contrast to experimental conditions), variations in the genetic background and comorbidities of critically ill trauma patients affect outcome. Many studies do not capture data regarding chronic health conditions and potentially relevant comorbidities or specific treatments and their timing. For instance, for trauma patients with diabetes, the extent of glycemic control could have an effect on ultimate outcome, but is infrequently included as a covariate in the outcome analysis.31
Most studies have confirmed a female survival advantage in trauma, but two confounding factors make definitive conclusions in this area problematic. First, acute sex hormonal changes that occur after injury in both males and females might affect trauma outcomes (high estrogen levels are associated with increased mortality rates). Second, racial disparities that contribute to sex-based outcome differences in trauma have been identified (inordinately worse outcomes for Asian males).32 Future studies must delineate how these three factors (sex, hormone status, and race) interact.
In experimental preclinical studies, sex hormones have been shown to affect sex-specific immune responses. Male sex hormones are deleterious, whereas female hormones are protective. But hormonal status is not evaluated in most clinical studies. Studies that have followed sex hormone levels during trauma patients’ clinical course have shown a correlation between estrogen/progesterone and tumor necrosis factor-α (TNF-α), an immune regulator with a myriad of activities during inflammation.33 Estradiol alone has shown a negative correlation with TNF-α immediately after injury. Conflicting data have emerged with respect to other immune modulators and sex hormone levels.34
High estradiol levels after injury have been associated with an increased mortality rate.35 Serum estradiol is a marker of injury severity and a predictor of death in critically injured patients, regardless of sex.36 Whether or not estradiol plays a causal role in outcomes is unclear, since additional trials have not confirmed these results.
The use of exogenous hormone replacement therapy is also an important consideration when analyzing sex-specific trauma outcomes, especially in older women. An estimated 21% of women in the United States take hormone replacement medication. Failure to measure sex hormone plasma levels significantly limits most clinical studies investigating gender differences.
Preclinical and clinical studies have suggested that women are more tolerant to shock.37 In contrast, a recent study identified that use of high plasma:red blood cell (RBC) or platelet:RBC ratios in massive transfusion for trauma patients in hemorrhagic shock was associated with reduced mortality in males, but not females. This could be due to sex-related differences in coagulation or different host responses to transfusion.38
When considering the prediction of trauma outcomes, there is no universally accepted trauma scoring system, but most scoring methods incorporate anatomic injury severity and physiological parameters. Although sex is confirmed as an independent predictor for trauma outcomes, none of the current trauma scoring systems includes sex and gender as a risk factor, and this should be reconsidered.
Research Questions
Do differences in time to critical care interventions, the decision to admit to an ICU, life-support care initiation, and guideline-based treatments contribute to sex-based differences in the acute care of trauma patients?
What is the effect of acute changes in sex hormone status after injury on differences in trauma patient outcomes according to race and gender?
What information regarding exogenous hormonal replacement therapy in trauma patients is most helpful in clarifying reasons for sex-based differences in the acute care of trauma patients?
Would the addition of sex and gender, race, and sex hormone levels improve the injury severity scoring systems used to predict trauma patients’ outcome?
Evidence Summary
Gender dichotomy in clinical outcomes after injury exists, but it is difficult to determine whether it is related to endogenous patient factors, treatment differences, patients’ responses to treatment, or acute changes in sex hormone levels. Most of the studies reported to date are limited by their retrospective designs, their lack of information on hormonal status, and the difficulty in controlling for other variables that can influence trauma.39
Some authors have suggested that females receive less intensive care treatment.40 A retrospective cohort study (n = 466,792) documented that women over the age of 50 were less likely to receive life-supporting treatments, which increased their mortality rate.41 Sex differences in the provision of critical care do exist, but the specific underlying reasons (e.g., risk factors, patient or surrogate decision-making, or health care practitioner decision-making) are unclear.
It was recently documented that major deviations from evidence-based clinical management guidelines in the treatment of critically injured trauma patients are associated with increased mortality rates. The strict use of guidelines is associated with better outcomes, and sex differences may have a role in this aspect of trauma care.42,43
A present conundrum is that most studies confirm that female gender is associated with a decreased mortality rate after trauma, but high estrogen levels are associated with an increased mortality rate. The goal of prospective research studies should be to determine if the sex hormone environment after injury (in addition to racial and sex differences) affects the intensity of the immune response, modifies resuscitation requirements, and thus influences important clinical outcomes. Sex hormone modulation represents a potential means of improving outcomes in critically ill trauma patients. Fundamental research in this area will provide the foundation for future treatment studies in resuscitative endocrinology.
INFLUENCE OF GENDER/SEX HORMONES ON IMMUNITY, INFLAMMATION, AND COAGULATION IN TRAUMA
Recommendation 3
Investigate the influence of sex hormones and gender on immunity, inflammation, and coagulation in the body’s response to trauma and consider resuscitative endocrinology as treatment.
Discussion
Over the past two decades, sex hormones have received considerable attention in the preclinical setting. These hormones have been shown to influence inflammatory cell lines, endothelial cells, and the inflammatory cascade.44 Research into hormonal differences following injury could lead to therapeutic breakthroughs. Male gender has been identified as a risk factor for hypofibrinogenemia in trauma.45
Prospective studies specifically designed to consider sex hormone levels in men and women in the immediate postinjury period are required. Continued research into potential sex hormone–based differences may close the gap between bench and bedside and ultimately promote therapeutic interventions to improve trauma patient outcomes. In this respect, individualized estrogen or progesterone treatment should be based on actual hormonal status immediately after injury.
Additional translational research studies are warranted to examine this important issue in gender-based trauma research, particularly since “resuscitative endocrinology” studies are already under way in the prehospital and ED settings.46 Clinical studies using progesterone as a neuroprotective drug after traumatic brain injury (TBI) have demonstrated safety.47
Research Questions
Can the expansion of “resuscitative endocrinology” research in trauma allow the rigorous design of studies of sex hormones as therapeutic agents?
What additional knowledge can be gained by including gender and sex hormone status in all prospective trauma trials investigating immune, inflammation, and coagulation changes following injury?
Can the development of point-of-care laboratory testing to identify hormonal status influence hormonal treatment strategies in early trauma care in a meaningful way?
Evidence Summary
Hormones have been studied as modifiers in inflammation, immunity, and coagulation. Long-term medications, including hormone replacement therapy, as well as in-hospital medications (e.g., heparin, cyclooxygenase inhibitors, steroids, and immunosuppressants) may alter immune responses and should be considered potential confounders in all studies examining gender-related issues in trauma.
Acute or chronic alcohol consumption may affect men and women differently with respect to coagulation. A recent study confirmed that consumption of commonly ingested quantities of alcohol correlated with the development of a hypocoagulable state in male trauma patients, but had no effect on coagulation status in injured women. Although the study had several limitations, it did bring to attention the important question of how alcohol consumption (a common cofactor in trauma) and gender interplay to produce coagulation differences.48
Sex hormones have gained significant interest as therapeutic agents. The Resuscitation Outcomes Consortium (https://roc.uwctc.org/tiki/current-studies) recently launched the “Resuscitative Endocrinology: Single-Dose Clinical Uses for Estrogen-Traumatic Hemorrhagic Shock (RESCUE-SHOCK)” study (ClinicalTrials.gov NCT00973674). The goal of this study was to determine if a single dose of conjugated estrogens improved 28-day survival in patients with traumatic hemorrhagic shock. The first phase of the study is currently under way. A parallel investigation is studying the same drug in patients with TBI (RESCUE-TBI; ClinicalTrials.gov NCT00973674).
INTERMEDIATE AND LONG-TERM CARE
Recommendation 4
Study hormonal and other preexisting factors that contribute to sex-related differences in posttraumatic outcomes. Investigate societal and cultural factors associated with posttrauma outcomes.
Discussion
The proposed differences between the sexes in ability to survive traumatic injury and the development of postinjury complications might reveal important tools that can be developed to improve patient outcomes. There is evidence of sex-related differences in postinjury complications and outcome. Females have a lower rate of most complications but a higher rate of acute respiratory distress syndrome (ARDS). No gender-related differences in pneumonia-associated mortality have been identified. The differences in metabolic and endocrine changes following trauma have not been studied adequately. There are gender-based differences in quality of life and cognitive functioning after injury (without strong evidence of why they exist). We need to understand the reasons for these differences and then apply that knowledge toward improving patient outcomes in both male and female trauma patients.
Women are at risk for markedly worse functional and psychological outcomes after major trauma than men, independent of injury severity and mechanism.49,50 Female sex has been shown to be an independent predictor of worse quality of life, psychological morbidity, and rates of posttraumatic stress disorder.51,52
Research Questions
Does the sex or hormonal status of a trauma patient at the time of injury influence long-term trauma outcomes, including postinjury complications?
Is the metabolic, endocrine, and inflammatory environment of the trauma patient a marker of severity or an influence on outcome and are there differential effects according to sex?
Can manipulation of the metabolic and endocrine environment improve outcomes and help close sex-based disparity gaps?
Are there social or societal factors that influence the quality of life and cognitive outcome of trauma patients according to sex and gender?
Evidence Summary
Multiple studies support the theory of female advantage in survival following traumatic injury as well as in postinjury complications24 of infection, sepsis,53–55 and multiple organ failure.56 However, prospective data show a higher rate of ARDS in females, despite similarities in ARDS-associated mortality rates between the sexes. Development of ARDS may have more to do with a proinflammatory sex hormone profile (low testosterone and high estradiol) than gender.57
Trauma mechanism, chest injury severity, and male sex are independent risk factors for ventilator-associated pneumonia, but sex is not an independent predictor of pneumonia-associated mortality.58 A large multicenter prospective study detected no sex-specific differences in postinjury pneumonia mortality rates when trauma patients were stratified by age, injury severity, and physiological measures.54
Both hyperglycemia and blood glucose variability have been documented as predicting poor outcome after injury. Sex differences in this physiological response to trauma have not yet been critically examined. A recent retrospective observational study (n = 1,915) documented that endocrine dysfunction in the form of blood glucose variability predicted higher mortality in male, but not female, trauma patients.59 Failed glucose homeostasis is an important marker of endocrine dysfunction after severe injury, and increased blood glucose variability in males (but not females) is associated with a higher mortality rate. These data have significant implications for sex-related differences in postinjury management.
Similarly, the acute metabolic response to trauma is affected by age, sex, and severity of injury. Prospective randomized trials confirmed sex-based differences in the trauma response. Women responded to increasing severity of injury with increased serum insulin-like growth factor-1 and little change in transthyretin concentrations early after injury. In men, both insulin-like growth factor-1 and transthyretin concentrations decreased with increasing injury severity.60,61
Women with spinal cord injury participate less in physical activity, which has implications for functional long-term outcome. It is not clearly understood why, but men are more likely to use vocational rehabilitation services and follow through on affiliated services. This may be related to women’s roles in society and their support systems. Females perform significantly better than males on tests of attention/working memory and language 1 year after TBI, while males outperform females in visual analytic skills.62
Neimeier and associates63 reported that violent mechanisms of injury and gender are the strongest predictors of executive function after trauma. They suggested that females might have better ability to respond to changes in the environment after TBI. Even when men and women are compared by symptoms following TBI, discreet differences are evident, such as women having more difficulty with headaches, dizziness, and loss of confidence, while men struggle with goal setting and restlessness.64 More information about these long-term consequences from traumatic injury will be important in the design of effective rehabilitation programs.
EMERGING RESEARCH
To date, the majority of clinical studies have confirmed that female sex is protective in trauma. However, a persistent conundrum is the finding that a high estrogen blood level in males and females early after injury is associated with adverse outcomes. Recent studies have made significant progress in addressing the potential contribution of sex chromosome differences to sex-based inflammation changes.
Interleukin-1 receptor-associated kinase-1 (IRAK-1), a constituent member of the Toll-like receptor (TLR) signaling cascade, resides on the X-chromosome. TLRs detect nucleic acids from invading pathogens and trigger cytokine release during inflammation and infection.65 IRAK-1 plays a central role in TLR2- and TLR4-induced activation of nuclear factor (NF)-κB, a critical event in the transcriptional regulation of many proinflammatory mediators. The IRAK-1 protein has multiple haplotype forms, with a less common variant associated with worse outcome in septic patients.66,67 The first clinical trial to characterize IRAK-1 polymorphism as an alternative mechanism responsible for sex-based outcome differences following injury confirmed that the IRAK-1 variant (present in 12.5% of the study cohort) was associated with poor clinical outcome.68 The IRAK-1 variant was independently associated with over a sixfold (OR = 6.4; 95% CI = 1.8 to 23) greater risk of multiple organ failure and five-fold (OR = 5.8; 95% CI = 1.4 to 24) greater risk of mortality. These differences were most prominent in males, while females heterozygous for the IRAK-1 variant demonstrated worse outcomes in a dose-dependent fashion.68 Other X-linked immunomodulatory genetic variants might contribute to or confound sex-related changes that occur after injury through increased representation of X-linked risk alleles in men.
CONCLUSIONS
Rigorous, high-quality, sex- and gender-specific research in the area of trauma and resuscitation is required to advance our understanding of differences in gender-related outcomes after injury. To advance the many layers of this important field forward, variables related to sex need to be considered in all trauma outcomes studies. Investigators are poised to make substantial contributions in this important area of research, but this will be accomplished only by employing sound research methodology using prospective translational studies to investigate both sex and gender and individual patients’ sex hormone status at the time of injury. Advances in gender-specific and sex hormone trauma outcomes research will provide the foundation for “resuscitative endocrinology” research for the future. This field is moving forward quickly. Recent studies on X-linked genetic polymorphisms added a new dimension to the basic science of trauma resuscitation research.66,67 There is increasing evidence that patients’ gender influences trauma outcomes, but emerging studies also confirm that stratification by gender alone is not sufficient to unravel this complex relationship.
Acknowledgments
The consensus conference was supported by grant 1R13NS087861-01 from the National Institute of Neurological Disorders and Stroke and the Office of Research on Women’s Health at the National Institutes of Health. Additional funding was provided by several organizational, institutional, and individual donors. Non-CME events were supported by Janssen Pharmaceuticals and Besins Critical Care/BH Pharma. See the executive summary elsewhere in this issue for full funding information.
Footnotes
Breakout group participants (alphabetical order): Stephanie Abbuhl, Fuad Abujarad, Jordan Barnhart, Helen Barr (FDA), Robert Barraco, John Beddla, Rebecca Brafran, Jeremy Brown (NIH), David Cone, Cassidy Dahn, Tamara Espinoza, Christal Esposito, Rosemarie Filart (NIH), Marna Greenberg, Richelle Jessey, Colleen Kalynych, Bryan Kane, Kathleen Kane, Gloria Kuhn, Evie Marcolini, Jasmine Matthews, Lisa Merck, Angela Mills, Alice Mitchell, Elizabeth Moore, Lena Napolitano, Elizabeth Nestor, Michael Nguyen, Roma Patel, Neha Raukar, Aaron Reilly, Rocky Sayegh, Kinjal Sethuraman, Wesley Stonely, Vicken Totten, Federico Vaca, Jody Vogel, Jessica Weiland, and David Wright.
The authors have no relevant financial information or potential conflicts to disclose.
References
- 1.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control [Accessed Sep 23, 2014];Web-based Injury Statistics Query and Reporting System (WISQARS) Available at: http://www.cdc.gov/injury/wisqars/
- 2.McGregor AJ, Greenberg M, Safdar B, et al. Focusing a gender lens on emergency medicine research: 2012 update. Acad Emerg Med. 2013;20:313–20. doi: 10.1111/acem.12085. [DOI] [PubMed] [Google Scholar]
- 3.Farace E, Alves WM. Do women fare worse: a metaanalysis of gender differences in traumatic brain injury outcome. J Neurosurg. 2000;93:539–45. doi: 10.3171/jns.2000.93.4.0539. [DOI] [PubMed] [Google Scholar]
- 4.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 5.Haas B, Stukel TA, Gomez D, et al. The mortality benefit of direct trauma center transport in a regional trauma system: a population-based analysis. J Trauma Acute Care Surg. 2012;72:1510–7. doi: 10.1097/TA.0b013e318252510a. [DOI] [PubMed] [Google Scholar]
- 6.Garwe T, Cowan LD, Neas B, Cathey T, Danford BC, Greenawalt P. Survival benefit of transfer to tertiary trauma centers for major trauma patients initially presenting to nontertiary trauma centers. Acad Emerg Med. 2010;17:1223–32. doi: 10.1111/j.1553-2712.2010.00918.x. [DOI] [PubMed] [Google Scholar]
- 7.Gomez D, Haas B, de Mestral C, et al. Gender-associated differences in access to trauma center care: a population-based analysis. Surgery. 2012;152:179–85. doi: 10.1016/j.surg.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Knaus W, Draper E, Wagner D, Zimmerman S. An evaluation of outcome from intensive care in major medical centers. Ann Intern Med. 1986;104:410–8. doi: 10.7326/0003-4819-104-3-410. [DOI] [PubMed] [Google Scholar]
- 9.Shortell SM, Zimmerman JE, Rousseau DM, et al. The performance of intensive care units: does good management make a difference? Med Care. 1994;32:508–25. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Sexton J, Thomas E, Helmreich RL. Error, stress and teamwork in medicine and aviation: cross sectional surveys. BMJ. 2000;320:745–9. doi: 10.1136/bmj.320.7237.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCunn M, Paciotti B, Narayan M, Ziegert J, Barg FK. Leadership and Gender During Acute Trauma Resuscitation. Annual Scientific Meeting, Eastern Association for the Surgery of Trauma; Naples, Florida. January 2014. [Google Scholar]
- 12.Eagly AH, Karau SJ. Role incongruity theory of prejudice toward female leaders. Psychol Rev. 2002;109:573–98. doi: 10.1037/0033-295x.109.3.573. [DOI] [PubMed] [Google Scholar]
- 13.Bartels C, Goetz S, Ward E, Carnes M. Internal medicine resident’s perceived ability to direct patient care: impact of gender and experience. J Womens Health (Larchmnt) 2008;17:1615–21. doi: 10.1089/jwh.2008.0798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCunn M, Burchill C, Speck RM, Pascual J, Bohm E, Barg FP. Collaboration and Satisfaction of Trauma Team Members: Physicians and Males Are More Satisfied. Mid-Atlantic Regional Meeting; Philadelphia. March 2014; Society for Academic Emergency Medicine; [Google Scholar]
- 15.Yang KC, Zhou MJ, Sperry JL, et al. Significant sex-based outcome differences in severely injured Chinese trauma patients. Shock. 2014;42:11–5. doi: 10.1097/SHK.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 16.Wohltmann CD, Franklin GA, Boaz PW, et al. A multicenter evaluation of whether gender dimorphism affects survival after trauma. Am J Surg. 2001;181:297–300. doi: 10.1016/s0002-9610(01)00582-7. [DOI] [PubMed] [Google Scholar]
- 17.Magnotti LJ, Fischer PE, Zarzaur BL, Fabian TC, Croce MA. Impact of gender on outcomes after blunt injury: a definitive analysis of more than 36,000 trauma patients. J Am Coll Surg. 2008;206:984–92. doi: 10.1016/j.jamcollsurg.2007.12.038. [DOI] [PubMed] [Google Scholar]
- 18.Rappold JF, Coimbra R, Hoyt DB, et al. Female gender does not protect blunt trauma patients from complications and mortality. J Trauma. 2002;53:436–41. doi: 10.1097/00005373-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Bowles BJ, Roth B, Demetriades D. Sexual dimorphism in trauma? A retrospective evaluation of outcome. Injury. 2003;34:27–31. doi: 10.1016/s0020-1383(02)00018-9. [DOI] [PubMed] [Google Scholar]
- 20.Coimbra R, Hoyt DB, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Does sexual dimorphism influence outcome of traumatic brain injury patients? The answer is no! J Trauma. 2003;54:689–700. doi: 10.1097/01.TA.0000058314.31655.5F. [DOI] [PubMed] [Google Scholar]
- 21.Gannon CJ, Napolitano LM, Pasquale M, Tracy JK, McCarter RJ. A statewide population-based study of gender differences in trauma: validation of a prior single-institution study. J Am Coll Surg. 2002;195:11–8. doi: 10.1016/s1072-7515(02)01187-0. [DOI] [PubMed] [Google Scholar]
- 22.George RL, McGwin G, Jr, Metzger J, Chaudry IH, Rue LW., 3rd The association between gender and mortality among trauma patients as modified by age. J Trauma. 2003;54:464–71. doi: 10.1097/01.TA.0000051939.95039.E6. [DOI] [PubMed] [Google Scholar]
- 23.Napolitano LM, Greco ME, Rodriguez A, Kufera JA, West RS, Scalea TM. Gender differences in adverse outcomes after blunt trauma. J Trauma. 2001;50:274–80. doi: 10.1097/00005373-200102000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Haider AH, Crompton JG, Oyetunji T, et al. Females have fewer complications and lower mortality following trauma than similarly injured males: a risk adjusted analysis of adults in the National Trauma Data Bank. Surgery. 2009;146:308–15. doi: 10.1016/j.surg.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 25.Sperry JL, Nathens AB, Frankel HL, et al. Characterization of the gender dimorphism after injury and hemorrhagic shock: are hormonal differences responsible? Crit Care Med. 2008;36:1838–45. doi: 10.1097/CCM.0b013e3181760c14. [DOI] [PubMed] [Google Scholar]
- 26.Haider AH, Crompton JG, Chang DC, et al. Evidence of hormonal basis for improved survival among females with trauma-associated shock: an analysis of the National Trauma Data Bank. J Trauma. 2010;69:537–40. doi: 10.1097/TA.0b013e3181efc67b. [DOI] [PubMed] [Google Scholar]
- 27.Guidry CA, Swenson BR, Davies SW, et al. Sex- and diagnosis-dependent differences in mortality and admission cytokine levels among patients admitted for intensive care. Crit Care Med. 2014;42:1110–20. doi: 10.1097/CCM.0000000000000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kerby JD, McGwin G, Jr, George RL, Cross JA, Chaudry IH, Rue LW., 3rd Sex differences in mortality after burn injury: results of analysis of the National Burn Repository of the American Burn Association. J Burn Care Res. 2006;27:452–6. doi: 10.1097/01.BCR.0000225957.01854.EE. [DOI] [PubMed] [Google Scholar]
- 29.George RL, McGwin G, Jr, Schwacha MG, et al. The association between sex and mortality among burn patients as modified by age. J Burn Care Rehabil. 2005;26:416–21. doi: 10.1097/01.bcr.0000176888.44949.87. [DOI] [PubMed] [Google Scholar]
- 30.Summers JI, Ziembicki JA, Corcos AC, Peitzman AB, Billiar TR, Sperry JL. Characterization of the sex dimorphism following severe thermal injury. J Burn Care Res. 2014 doi: 10.1097/BCR.0000000000000018. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gale SC, Sicoutris C, Reilly PM, Schwab CW, Gracias VH. Poor glycemic control is associated with increased mortality in critically ill trauma patients. Am Surg. 2007;73:454–60. doi: 10.1177/000313480707300507. [DOI] [PubMed] [Google Scholar]
- 32.Sperry JL, Vodovotz Y, Ferrell RE, et al. Racial disparities and sex-based outcomes differences after severe injury. J Am Coll Surg. 2012;214:973–80. doi: 10.1016/j.jamcollsurg.2012.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gee AC, Sawai RS, Differding J, Muller P, Underwood S, Schreiber MA. The influence of sex hormones on coagulation and inflammation in the trauma patient. Shock. 2008;29:334–41. doi: 10.1097/shk.0b013e3181506ee5. [DOI] [PubMed] [Google Scholar]
- 34.Angele MK, Faist E. Gender-specific immune response following shock: clinical and experimental data. Eur J Trauma. 2000;26:267–77. [Google Scholar]
- 35.Dossett LA, Swenson BR, Heffernan D, et al. High levels of endogenous estrogens are associated with death in the critically injured adult. J Trauma. 2008;64:580–5. doi: 10.1097/TA.0b013e31816543dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.May AK, Dossett LA, Norris PR, et al. Estradiol is associated with mortality in critically ill trauma and surgical patients. Crit Care Med. 2008;36:62–8. doi: 10.1097/01.CCM.0000292015.16171.6D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deitch EA, Livingston DH, Lavery RF, Monaghan SF, Bongu A, Machiedo GW. Hormonally active women tolerate shock-trauma better than do men: a prospective study of over 4000 trauma patients. Ann Surg. 2007;246:447–55. doi: 10.1097/SLA.0b013e318148566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rowell SE, Barbosa RR, Allison CE, et al. Gender-based differences in mortality in response to high product ratio massive transfusion. J Trauma. 2011;71(2 suppl 3):S375–9. doi: 10.1097/TA.0b013e318227f1aa. [DOI] [PubMed] [Google Scholar]
- 39.Alspach JG. Is there gender bias in critical care? Crit Care Nurse. 2012;32:8–14. doi: 10.4037/ccn2012727. [DOI] [PubMed] [Google Scholar]
- 40.Fowler RA, Filate W, Hartleib M, Frost DW, Lazongas C, Hladunewich M. Sex and critical illness. Curr Opin Crit Care. 2009;15:442–9. doi: 10.1097/MCC.0b013e3283307a12. [DOI] [PubMed] [Google Scholar]
- 41.Fowler RA, Sabur N, Li P, et al. Sex-and age-based differences in the delivery and outcomes of critical care. CMAJ. 2007;177:1513–9. doi: 10.1503/cmaj.071112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rice TW, Morris S, Tortella BJ, Wheeler AP, Christensen MC. Deviations from evidence-based clinical management guidelines increase mortality in critically injured trauma patients. Crit Care Med. 2012;40:778–86. doi: 10.1097/CCM.0b013e318236f168. [DOI] [PubMed] [Google Scholar]
- 43.Napolitano LM. Guideline compliance in trauma: evidence-based protocols to improve trauma outcomes? Crit Care Med. 2012;40:990–2. doi: 10.1097/CCM.0b013e3182411154. [DOI] [PubMed] [Google Scholar]
- 44.Gilliver SC. Sex steroids as inflammatory regulators. J Steroid Biochem Mol Biol. 2010;120:105–15. doi: 10.1016/j.jsbmb.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 45.Hagemo JS, Stanworth S, Juffermans NP, et al. Prevalence, predictors and outcome of hypofibrinogenaemia in trauma: a multicentre observational study. Crit Care. 2014;18:R52. doi: 10.1186/cc13798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wright DW, Espinoza TR, Merck LH, Ratcliff JJ, Backster A, Stein DG. Gender differences in neurological emergencies part II: a consensus summary and research agenda on traumatic brain injury. Acad Emerg Med. 2014;21 doi: 10.1111/acem.12532. 000–00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wright DW, Kellermann AL, Hertzberg VS, et al. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49:391–402. doi: 10.1016/j.annemergmed.2006.07.932. [DOI] [PubMed] [Google Scholar]
- 48.Spoerke N, Underwood S, Differding J, et al. Effects of ethanol intoxication and gender on blood coagulation. J Trauma. 2010;68:1106–11. doi: 10.1097/TA.0b013e3181d86860. [DOI] [PubMed] [Google Scholar]
- 49.Holbrook TL, Hoyt DB, Anderson JP. The importance of gender on outcome after major trauma: functional and psychologic outcomes in women versus men. J Trauma. 2001;50:270–3. doi: 10.1097/00005373-200102000-00012. [DOI] [PubMed] [Google Scholar]
- 50.Holbrook TL, Hoyt DB, Stein MB, Sieber WJ. Gender differences in long-term posttraumatic stress disorder outcomes after major trauma: women are at higher risk of adverse outcomes than men. J Trauma. 2002;53:882–8. doi: 10.1097/00005373-200211000-00012. [DOI] [PubMed] [Google Scholar]
- 51.Holbrook TL, Hoyt DB. The impact of major trauma: quality-of-life outcomes are worse in women than in men, independent of mechanism and injury severity. J Trauma. 2004;56:284–90. doi: 10.1097/01.TA.0000109758.75406.F8. [DOI] [PubMed] [Google Scholar]
- 52.Axinn WG, Ghimire DJ, Williams NE, Scott KM. Gender, traumatic events, and mental health disorders in a rural Asian setting. J Health Soc Behavior. 2013;54:444–61. doi: 10.1177/0022146513501518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Osborn TM, Tracy JK, Dunne JR, Pasquale M, Napolitano LM. Epidemiology of sepsis in patients with traumatic injury. Crit Care Med. 2004;32:2234–40. doi: 10.1097/01.ccm.0000145586.23276.0f. [DOI] [PubMed] [Google Scholar]
- 54.Gannon CJ, Pasquale M, Tracy JK, McCarter RJ, Napolitano LM. Male gender is associated with increased risk for postinjury pneumonia. Shock. 2004;21:410–4. doi: 10.1097/00024382-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 55.Schoeneberg C, Kauther MD, Hussmann B, Keitel J, Schmitz D, Lendemans S. Gender-specific differences in severely injured patients between 2002 and 2011: data analysis with matched-pair analysis. Crit Care. 2013;17:R277. doi: 10.1186/cc13132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Frink M, Pape HC, van Griensven M, Krettek C, Chaudry IH, Hildebrand F. Influence of sex and age on MODS and cytokines after multiple injuries. Shock. 2007;27:151–6. doi: 10.1097/01.shk.0000239767.64786.de. [DOI] [PubMed] [Google Scholar]
- 57.Heffernan DS, Dossett LA, Lightfoot MA, et al. Gender and acute respiratory distress syndrome in critically injured adults: a prospective study. J Trauma. 2011;71:878–85. doi: 10.1097/TA.0b013e31822c0d31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Croce MA, Brasel KJ, Coimbra R, et al. National Trauma Institute prospective evaluation of the ventilator bundle in trauma patients: does it really work? J Trauma Acute Care Surg. 2013;74:354–62. doi: 10.1097/TA.0b013e31827a0c65. [DOI] [PubMed] [Google Scholar]
- 59.Mohr AM, Lavery RF, Sifri ZC, et al. Gender differences in glucose variability after severe trauma. Am Surg. 2010;76:896–902. [PubMed] [Google Scholar]
- 60.Houston-Bolze MS, Downing MT, Sayed AM, Meserve LA. Gender differences in the responses of serum insulin-like growth factor-1 and transthyretin (prealbumin) to trauma. Crit Care Med. 1996;24:1982–7. doi: 10.1097/00003246-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 61.Houston-Bolze MS, Downing MT, Sayed AM, Williford JH. Serum insulin-like growth factor binding protein-3 responds differently to trauma in men and women. Crit Care Med. 1996;24:1988–92. doi: 10.1097/00003246-199612000-00010. [DOI] [PubMed] [Google Scholar]
- 62.Ratcliff JJ, Greenspan AI, Goldstein FC, et al. Gender and traumatic brain injury: do the sexes fare differently? Brain Inj. 2007;21:1023–30. doi: 10.1080/02699050701633072. [DOI] [PubMed] [Google Scholar]
- 63.Neimeier JP, Marwitz JH, Lesher K, Walker WC, Bushnik T. Gender differences in executive functions following traumatic brain injury. Neuropsychol Rehab. 2007;17:293–313. doi: 10.1080/09602010600814729. [DOI] [PubMed] [Google Scholar]
- 64.Colantonio A, Harris JE, Ratcliff G, Chase S, Ellis K. Gender differences in self reported long term outcomes following moderate to severer traumatic brain injury. BMC Neurol. 2010;10:102. doi: 10.1186/1471-2377-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Blasius AL, Beutler B. Intracellular Toll-like receptors. Immunity. 2010;32:305–15. doi: 10.1016/j.immuni.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 66.Toubiana J, Courtine E, Pène F, et al. IRAK1 functional genetic variant affects severity of septic shock. Crit Care Med. 2010;38:2287–94. doi: 10.1097/CCM.0b013e3181f9f9c7. [DOI] [PubMed] [Google Scholar]
- 67.Arcaroli J, Silva E, Maloney JP, et al. Variant IRAK-1 haplotype is associated with increased nuclear factor-kappaB activation and worse outcomes in sepsis. Am J Respir Crit Care Med. 2006;173:1335–41. doi: 10.1164/rccm.200603-341OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sperry J, Zuckerbraun B, Zolin S, et al. X-Chromosome Linked IRAK1 Polymorphism Is Strong Predictor of Multiple Organ Failure and Mortality Post-injury. Presented at the 134th Annual Meeting of the American Surgical Association; Boston. April 10—12, 2014. [Google Scholar]