Abstract
Obesity and its health sequelae affect a significant portion of children in the United States. Yet, the current gold-standard family-based behavioral weight-loss treatments are only effective for one-third of children long-term. Therefore, we developed iROC (Intervention for Regulation of Cues) to specifically target a method to decrease overeating in overweight children, based on learning theory, to inform and enhance interventions targeting diet and obesity in youth. This study will rigorously test extinction processes as a method of decreasing physiological and psychological responses to food cues in overweight and obese children. Through exposing children to their highly craved foods, and ‘training the brain and body’ to decrease overeating, we are hoping to produce longer-lasting weight loss or weight-gain prevention over time.
Keywords: obesity, eating in the absence of hunger, cue exposure, overeating, child
1. Introduction
Childhood obesity is prevalent1 and eating past nutritional needs is the proximal cause of rising obesity rates over the past three decades.2 Food intake in humans is a complex process that originates and is maintained by basic learning and conditioning processes.3–5 Obese individuals, compared to lean, have been shown to differentially respond to external food cues, with increases in both subjective ratings (increased desire to eat) and physiological responses (increased cephalic phase responses-biological preparations to eat).6,7 Evidence from neuroimaging shows that obese adults and adolescents, compared to lean, exhibit a greater increase in fronto-striatal circuitry activation during anticipation of high-caloric foods.8,9 Additionally, obese children compared to lean children have higher activation in neural circuitry involved in reward, motivation, and cognitive control when shown pictures of food10,11 and activation in areas associated with learning, memory, and reward when given a taste of food.12 This project focuses on Pavlovian conditioning because it is the most basic principle of learning and there are extinction processes that can be used to weaken the relationships that lead to overeating. To date, it is unknown whether physiological reflexes to food cues and subjective experiences of food craving can be altered via extinction learning.
Basic science research in extinction has highlighted challenges in the long-term retention of extinction learning. It is now understood that extinction involves new learning and the original learning remains available under the right circumstances.13,14 The context (cues in the environment) in which extinction takes place also influences subsequent long-term retention of extinction learning.13,15 There are two general strategies that can be employed to optimize extinction.16 The first is to strengthen the extinction learning. The second is to bridge two or more contexts to promote extinction in the new context. Research suggests that extinction can be optimized/strengthened by manipulating trial spacing and frequency of extinction trials16–19 by the inclusion of a partial reinforcement schedule, which slows the rate of reacquisition of old learning.13,20,21 Furthermore, extinction may be bridged across two or more contexts by increasing the number of contexts in which extinction occurs16 and the use of extinction cues.22,23
Cue Exposure Treatments (CET-Food) utilize extinction processes by providing repeated non-reinforced exposures to food associated with overeating to extinguish the individual’s conditioned response (i.e. cravings or physiological responses) in addition to training the individual to habituate to (tolerate) the cravings associated with the cue. We have tested CET-Food in two published projects to date.24,25 In our studies, CET-Food was delivered once a week utilizing exposures to a different single food each week based on the individual’s hierarchy of highly craved foods. However, the evaluation of the above variables from basic extinction learning may enhance the effects of CET-Food. At this point, the optimal frequency, format, partial reinforcement schedule, and context of the CET-Food intervention has not been identified.
Understanding the processes of extinction as it relates to food cues has the potential to significantly enhance and target interventions for overeating. This study, entitled Intervention for Regulation of Cues (iROC), will advance scientific knowledge by employing principles of extinction in CET-Food to impact cephalic phase responses (CPRs) and self-reported cravings, to ultimately decrease overeating.
2. Objectives for iROC study
The iROC study is funded by a grant from NIDDK (R01). This study builds upon our pilot studies that were funded by a University of Minnesota Faculty Development Grant and which demonstrated the feasibility and acceptability of CET-Food for overweight and obese children and their families.24,25 The primary aim of the current project is to evaluate the most salient factors from basic learning literature that could potentially improve CET-Food for children. There are numerous studies within this project, and each will build on the previous study. We will present our plan of research here, however, we recognize that it may change during the course of the study. During the first two studies in iROC, we will test four concepts related to extinction focusing on strengthening extinction learning and bridging extinction to multiple contexts. Finally, we will combine the most effective factors in a proof of concept study. At the conclusion of this project, we will have a well-defined protocol and a procedures manual for CET-Food, estimates of variability and levels of response in overweight children, and preliminary information about the efficacy of this intervention in overweight children in preparation for future studies. The secondary aim of the current project is to explore changes in aspects of food cue reactivity (subjective and physiological responses to the food cues) that could be associated with the effectiveness of CET-Food in the reduction of overeating.
3. Study Design
3.1 Overview
The extinction concepts that will be tested in the iROC study will be evaluated in two 2 × 2 studies, and then we will test the most effective methods in a proof of concept study. During Study 1 and Study 2, we will test 4 concepts related to Pavlovian extinction literature that are salient to human food intake: 1) number of extinction trials, 2) single vs. multiple foods in exposures, 3) extinction training in multiple contexts and 4) the use of an enhanced partial reinforcement schedule. (See Figure 1 ) All of the trials will incorporate extinction cues22,23 (bracelets) to remind the children of their new learning and thus help to bridge extinction between contexts. Following an exposure learning session, the children will verbalize what they have learned as a result of the session to enhance inhibitory processes.26 Study 3 will be a proof of concept study, which develops the intervention based on the results of Studies 1 and 2 and evaluates initial efficacy and acceptability.
Figure 1.
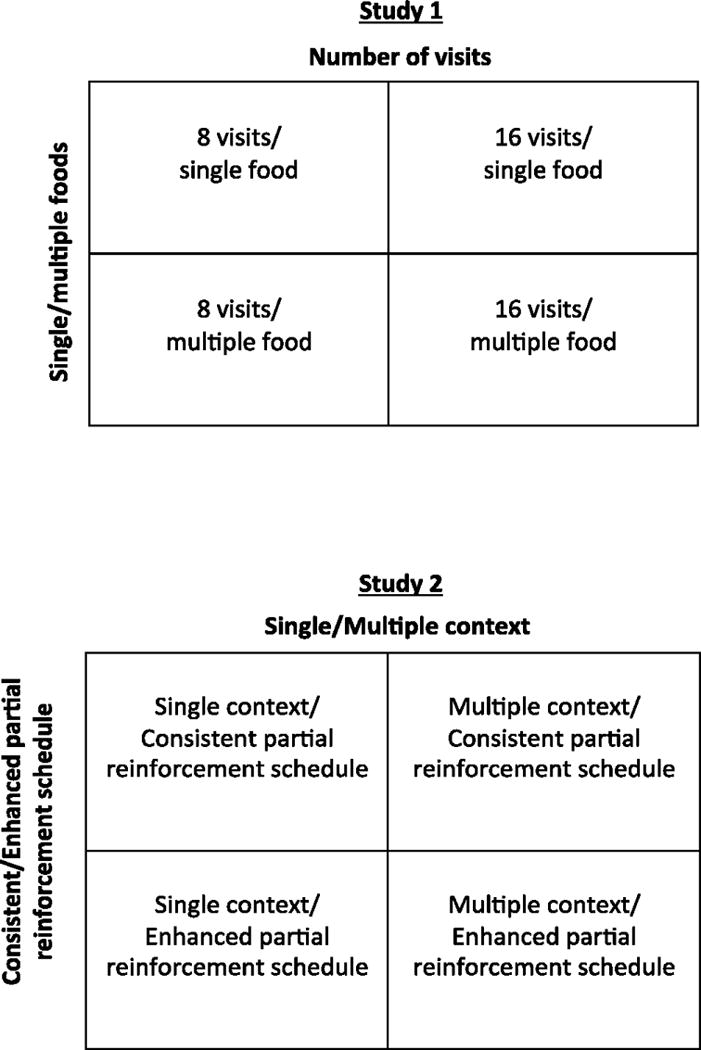
Study design for Study 1 and Study 2.
3.2 Participants
Participants in all studies will be overweight and obese 8–13 year old children, and their parent. We chose the 8–13 year-old age period for theoretical, biological and developmental reasons. From a learning theory perspective, children have shorter and less ingrained learning histories than adults and interventions targeting extinction have a potentially greater influence with children. There is considerable evidence suggesting that the preteen age range is a risk period for weight gain.27–29,30 Additionally, working with children just prior to their adolescent years has added benefit as the children have developed some abstract thinking but have not yet entered in the process of differentiating and separating themselves from their families and therefore may be more likely to participate in the process with their parent.
3.3. Inclusion/Exclusion criteria
The inclusion criteria for all the studies in this project include: 1) An overweight or obese child (BMI ≥ 85th percentile for age and gender) in the family who is between the ages of 8 and 13 years; 2) Child who can read at a minimum of a 2nd grade level in English; 3) Parent who can read at a minimum of a 5th grade level in English; 4) Parent and child willing to commit to attendance and assessments; 5) Child overeating (as demonstrated in laboratory paradigm (see measures section) and parent report).
The exclusion criteria for all the studies in this project include: 1) Major child or parent psychiatric disorder, including eating disorder (as diagnosed by interview); 2) An obese child with a BMI > 99.9th percentile; 3) Child or parent diagnosis of serious medical condition which could significantly decrease their ability to participate in the intervention, requires supervision or limitations of their diet; 4) Child taking a medication that can affect mental status, eating or weight; 5) Family with restrictions on types of food that can be eaten, such as food allergies, or religious or ethnic practices that limit the foods available in the home.
3.4 Recruitment and retention
Families in the San Diego Metropolitan area with an overweight child will be recruited through online advertisements, flyers, pediatricians and other health care providers, and direct mailings or emails to families. All families who call and are interested will be contacted by the research staff to describe the study and screened over the phone for eligibility. If participants meet initial criteria, they will be scheduled to attend a study orientation that describes the purpose of the study. If families are still interested after the orientation, they will be scheduled to complete initial baseline assessments.
After families have enrolled in the study, their attendance will be tracked weekly and efforts will be made by staff and interventionists to reasonably accommodate families’ schedules and barriers to participation that may arise, such as illness and scheduling conflicts with after-school activities. Participants will be informed that they can not miss more than 2 out of 16 sessions in the 16-session condition or 1 out of 8 sessions in the 8-session condition. Staff and interventionists will emphasize building rapport with the families to increase treatment adherence. In addition, families will receive incentives for attending treatment sessions and assessment visits. Families will be compensated with a $10 gift card for each treatment session they attend. Families will also receive a $10 gift card for completing both the second and third baseline assessment visits, and a $50 gift card for completing both the post-treatment and 3-months post-treatment assessment visits. Additionally, as part of this study, we will offer all families who complete the iROC study a free 8-week traditional family-based pediatric obesity group following the experimental treatment as an added incentive.
3.5 Assessment and outcome measures
Measurements along with the time points that they will be administered are listed in Table 1. At the beginning of the assessments, children will create and rank order an individualized list of highly craved foods with the assessment staff. Children will then be asked to rank order two pre-set lists of foods – eight foods used in the Eating in the Absence of Hunger paradigm (described below), as well as a list of eight standardized foods chosen by the experimenters (includes cinnamon rolls, Kraft® Macaroni and Cheese, brownies, Pringles®, vanilla cupcake, cheese pizza, McDonald’s® French fries, and glazed donut). The selection and rank ordering of these foods will be used to determine which foods will be presented to the child during the exposure visits.
Table 1.
Table of self-report measures in the iROC study
| Domain | Instrument | Child or Parent |
|---|---|---|
| Demographics | Age, gender, ethnicity, grade in school (for child) | C, P |
| Barratt Simplified Measure of Social Status (Hollingshead Modified)59 | P | |
| Medical History | Medical history | P |
| Parental Feeding | Child Feeding Questionnaire60 | C, P |
| Disinhibited Eating | Binge Eating Scale61 | P |
| Eating in the Absence of Hunger- Adult, Parent62 | P | |
| Eating in the Absence of Hunger- Child63 | C | |
| Child Eating Behavior Questionnaire64 | C,P | |
| Eating Disorder Examination Questionnaire65 | P | |
| Craving | Food Cravings Questionnaire-trait (adapted for children)66 | C,P |
| Power of Food Scale (adapted for children)67 | C, P | |
| Psychopathology | Center for Epidemiologic Studies Depression Scale for Children68 | C |
| Multidimensional Anxiety Scale for Children69 | C | |
| State Trait Anxiety Inventory – child version70 | C | |
| State Trait Anxiety Inventory71 | P | |
| Child Behavior Checklist72 | P | |
| Physical Activity | GODIN Leisure-time exercise questionnaire73 | P |
| Social Desirability | Social Desirability Questionnaire74 | C |
| Treatment Acceptability | Treatment Acceptability and Preference | P |
Screening for inclusion/exclusion criteria
The child inclusion/exclusion criteria will be assessed at the first assessment visit, and is determined by self-report by the parent, anthropometry, EAH paradigm (see description below) and interview (Mini International Neuropsychiatric Interview for Children and Adolescents31 and Eating Disorders Examination, Child Version).32 Additionally, we will evaluate parent reading level (Wide-Range Achievement Test – Fourth Edition, Word Reading Subtest)33 and parent psychopathology (Mini International Neuropsychiatric Interview)31 at baseline only as exclusion criteria. Anthropometry and EAH will also be measured at each time point as outcome variables.
Primary measures
Primary outcome measures in this study are eating in the absence of hunger and BMI change. Data obtained from these measures will help determine the most optimal format for CET-Food.
Eating in the Absence of Hunger (Child only)
Eating in the absence of hunger (EAH) is a lab-based measurement of how much children eat when physiologically satiated. The assessment measure of EAH has been described by Birch and colleagues34,35 and has been used in our pilot studies.24,25 To measure EAH, each child will be provided with a standard ad libitum pizza dinner plus apples or carrots and fruit punch during the baseline assessment. Children are instructed to eat as much of the dinner as they like. After the meal, children will then complete a self-report post-meal satiety-rating questionnaire using a cartoon representation of three levels of fullness.36 If children do not mark half full or full, they will be encouraged to eat until they are full.
Ten minutes following the completion of the pizza dinner, children will be provided with eight bowls of pre-weighed snack foods (gummy bears, chocolate chip cookies, Oreo® cookies, M & M’s®, Skittles®, Doritos®, popcorn, and Cheetos®) and toys. Children will taste and rate their liking of each of the foods with the research assistant. After the liking ratings, the children will be told that the research assistant has to set up for the next activity, and that they are welcome to eat the food or play with games. After 10 minutes of free access to the snack foods and toys, the remaining food items are weighed, and total calories consumed by each child is calculated by food and in total and translated to percent of calorie needs consumed using age and gender-specific formulas for calculating energy requirements.37
Anthropometry
Child and parent height will be measured in triplicate. Height will be recorded on a Tanita HR-200 stadiometer to the nearest 0.1 cm, and the average of the three values will be used for analysis. Body weight will be measured twice using a Tanita BWB-800 series scale. Weight will be recorded in kilograms to the nearest 0.1 kg and the average of the 2 values will be used for analysis. Height and weight will be converted to body mass index (BMI=[kg/m2]). Since children are growing, BMI will be translated to BMI for age percentile score using the CDC growth charts38 and to standardized BMI (BMI-Z ).39
Secondary measures
The following measures explore the impact of CET-Food on cognitive and physiological measures of food cue reactivity, including attentional bias to food cues, memory for food cues, motor impulsivity to food cues, food reward, food cue interference and physiological responses to food cues.
Attentional bias to food cues
Attentional bias will be measured by a task developed by our group.40,41 The purpose of this task is to examine attentional biases for food cues as compared to non-food cues. Participants will be presented with 48 trials comprised from six food/neutral word pairs matched for length and readability. The assessment consisted of equal number of trials for probe type (“E” or “F”), location of probe (top or bottom), and location of food word (top or bottom). Different word sets will be used for assessments before and after CET-Food. Response latencies will be recorded from the onset of the probe (“E” or “F”) to the button press. A food bias score will be computed by subtracting the response latency for probes following food words from the response latency for probes that followed neutral words. Larger positive bias scores will indicate an attentional bias toward food related words, while larger negative bias scores will indicate an attentional bias away from food related words.
Memory for food
Children’s memory for food words will be measured using the VLTF-C (Verbal Learning Test for Children – Food version), an adaptation of the CVLT-C (California Verbal Learning Test – Children’s version).42 The purpose of this modified test is to examine whether there are attention, learning, and memory differences in calorically-dense food words versus low-calorie foods and non-food words. The examiner will read a list of 15 words containing 3 categories of words (fruits, toys, and calorically-dense foods) to the child. After the list is read, the child will be asked to recall as many of the words on the list as they can. The child will be given five trials of hearing and recalling this list. After this initial free recall, a different list of interference (distraction words) will be read to the child, followed by short-delay free recall and cued recall trials. Free recall, cued recall (child given prompts to recall semantic categories of words), and a word recognition trial will also be administered after a 20-minute delay. Children who are more food cue sensitive, will store food cues in their memory longer, and are expected to exhibit a greater recall of food relative to non-food words.
Food motor impulsivity
Food-specific motor impulsivity will be measured using an adapted version of the Food Stop Task.43 The original stop task44,45 assesses global and motor impulsivity, above and beyond the contribution of reaction time. Participants will complete both the go task and the stop task. Participants will be presented with pictures of eight highly palatable foods and eight attractive toy pictures (neutral condition). In the go task trials (75% of the trials), participants will first discriminate between food and a toy on a computer screen, and will be instructed to press the correct corresponding letter on the keyboard as quickly as they can. However, in the stop task trials (25% of the trials), a thick border around the food or toy will be presented, which signals to the participant to inhibit their go response and not push a letter on the keyboard. The speed at which the stimuli are presented will be adjusted dynamically depending on the participants’ response time. Children who are more impulsive around foods are expected to have more errors when responding to food cues when they should be inhibiting responses, as compared to non-food cues.
Food reinforcement
The food reinforcement task is a behavioral choice computer task to measure the reinforcing/rewarding value of food.46 The food reinforcement task is an operant task with a fixed ratio schedule of reinforcement. The children will be told that they will be playing a computer game to earn points toward a reward (their first most highly craved food from the initial food selection). Children will be rewarded with 50 calories of their most highly craved food after 50 mouse clicks in response to the prompts in the game until they state that they are finished. Children who value food more are expected to continue working towards food for a longer time period (for more total calories).
Food attentional control and interference
Food-specific attentional control and interference will be measured using a computerized Stroop task using food cues similar to that used by Braet and colleagues.47,48 Words will be shown, one at a time, on a computer screen in either blue, red, green, or yellow colored text. The child will be asked to respond to the stimulus by pressing the corresponding color key on the keyboard, as quickly and accurately as they can. Children will be first asked to complete a practice trial consisting of 20 non-food (neutral) words as the stimuli. After the practice trial, the child will be presented with 20 highly palatable food words, followed by 20 neutral words. This trial will be repeated once. Longer latencies to respond will represent increased attentional interference of food cues compared to non-food cues.
Psychophysiological Reactivity to food cues
Responsivity to food cues is developed through Pavlovian and operant conditioning processes and can be demonstrated by changes in physiology in response to food cues that are normally invoked in response to the food itself (e.g. cephalic phase responses, CPRs). All of the psychophysiological measures in iROC were chosen as measures of cephalic phase responses (biological preparatory responses to food) and have shown sensitivity to conditioning paradigms with food.49,50 Electrophysiological recordings will all be sampled at 250 Hz and recordings of 6-minute blocks will be made. Psychophysiological measures, including heart rate variability (ECG), skin conductance (GSR), and swallowing (EMG) will be taken during a food exposure session using a BIOPAC MP150 model (BIOPAC Systems, Inc.).
Each session will involve six minutes of baseline data collection, followed by seven minutes of exposure (six minutes for the food, one minute for the toy), six minutes of recovery immediately following the exposure, and then six additional minutes of data collection post recovery. After a thirty-minute delay, a long-delay post recovery data collection period will commence for a final six-minute interval. The child’s second most highly craved food (see food selection) will be presented in front of the child during the food exposure period. The examiner will ask the child to look at the food for 30 seconds and rate their craving level to the food on a scale of 1–5. Then the child will be asked to smell the food for 30 seconds and rate their craving to the food. The child will be prompted to either look at or smell the food and rate their craving levels every thirty seconds during the five minutes of food exposure. The child will also be presented with a standardized toy (used as the control object) during the session for one minute either before or after the food exposure. The order of the presentation of food and toy will be counterbalanced among participants.
Heart rate and heart rate variability will be measured using two Ag±AgCl electrodes, one attached on the left side of the subject, the other attached under the right collarbone.51 R-waves will be detected off-line with a template matching procedure, and inter-beat intervals will be calculated. Skin conductance will be measured with two Ag±AgCl electrodes, placed on the thenar and hypothenar eminences of the palm of the non-dominant hand. Salivation will be measured using swallows recorded by electromyography. The EMG signal will be recorded with three Ag±AgCl electrodes, two electrodes will be attached under the left jaw, in the length of the anterior part of the musculus digastricus and a reference electrode will be placed on the left mastoid process. The definition of a swallowing response will be determined as a response of the integrated signal above a five mV threshold.52
Self-report questionnaires (Parent and child)
A battery of psychometrically reliable and valid measures of eating, craving levels, psychological issues, physical activity, and social desirability will also be administered to parents and children as part of the assessment for the study. Parents will complete demographics, motivation, and medical history questionnaires. Please see Table 1 for a detailed list of the self-report measures and their references.
Treatment acceptability
At the post-treatment assessment, parents will be asked to complete a treatment acceptability and preference questionnaire designed by the study team to better understand the families’ perceptions of the various treatment aspects, including time commitment, treatment feasibility, and estimation of benefits and progress.
3.6. Details on Specific Studies in iROC
3.61 Overall design issues related to Studies 1 and 2
The aim of Study 1 and Study 2 is to evaluate four factors from learning theory that can inform the content, structure and frequency of CET-Food for overweight and obese children. There are a number of similarities in Studies 1 and 2; Similar components are described first and then specifics regarding each study follow.
Study design
Both Study 1 and Study 2 utilize 2 between-subjects factors, each with two levels (2 × 2 design), and a repeated measures factor with three timepoints (pre-treatment, post-treatment, and 3-month follow-up).
Assessments
Assessments will be completed pre-exposure treatment, post-exposure treatment and 3-month follow-up.
Outcomes
The primary outcomes include EAH and BMI change. Secondary outcomes include cognitive and psychophysiological variables related to food cue reactivity, as well as questionnaires on eating behaviors and cravings. All outcomes are described in the measurement section.
3.62 Specific design of Study 1
Design
The purpose of this study is to evaluate the impact of the number of foods and the number of CET-Food exposure trials. This study utilizes two between-subjects factors ((number of foods (single vs. multiple) and number of extinction trials (8 vs. 16)), each with two levels, and a repeated measures factor with three levels (pre, post, follow-up; see Figure 1). In the single food sessions, the child and parent will be exposed to the same set of four foods in weekly sessions. Two of the four foods will come from the child-generated list of highly craved foods. These foods will be generated during a food selection process in which the child identifies his/her most highly craved foods, with the examiner and child’s parent’s assistance if needed, and rank orders them from most highly craved to least craved. The other two foods will be the child’s most highly rated craved foods from the list of standardized foods and EAH foods. In other words, the four foods in the single food condition will consist of two child-generated foods, one standardized food, and one EAH food. In the multiple food exposure sessions, a different set of four foods will be presented in each weekly session, including two foods that the participant chooses, one standardized food, and one EAH food. In the multiple food eight-week condition, participants will be exposed to 32 of their top craved foods (16 they selected, 8 from the standardized food list and 8 from the EAH food list). In the multiple food sixteen-week condition, participants will be exposed to the same make-up of 32 foods, but will repeat the foods halfway through treatment (in a different order and combination), thus being exposed to each food twice over the sixteen weeks.
Participants and randomization
Forty-eight overweight and obese children and their parent will be randomized to one of four possible treatment arms: 8 sessions/single food, 8 sessions/multiple food, 16 sessions/single food, 16 sessions/multiple foods.
3.63 Specific design of Study 2
Design
The purpose of this study is to evaluate the provision of CET-Food in different contexts and the use of an enhanced partial reinforcement schedule. This study utilizes two between-subjects factors, context (single context vs. multiple context) and partial reinforcement schedule (standard vs. enhanced), each with two levels, and a repeated measures factor with three levels (pre, post, follow-up; see Figure 1). The context condition will consist of two levels – single context, in which participants will be randomized to complete treatment in only one of three settings (laboratory, home, or food court), or multiple contexts, in which participants attend treatment sessions in all three of the contexts. In the standard partial reinforcement group, participants take a “small taste” of the food during each CET-Food visit. In the enhanced partial reinforcement group, during 25% of the sessions, the child will eat ¾ of the food, and in the other 75% of the sessions, the child will have a “small taste” as in the standard group.
Participants and randomization
Forty-eight overweight and obese children and their parents will be randomized to one of four possible treatment arms: Single context/standard partial reinforcement, multiple context/standard partial reinforcement, single context/enhanced partial reinforcement, and multiple context/enhanced partial reinforcement.
3.64 Specific design of Study 3
Design
The purpose of this study is to manualize and test CET-Food based on the findings from Studies 1 and 2 and to evaluate the efficacy and acceptability of CET-Food with overweight and obese children and their parents, using a quasi-experimental one-group treatment design, as a proof of concept study. Studies 1 and 2 will be used to inform treatment design, such as number of extinction trials, number of foods presented, context (location) of treatment, and the use of an enhanced partial reinforcement. For instance, if the findings from Study 1 and Study 2 indicate that 8 weekly sessions using multiple foods in a single context without enhanced partial reinforcement produces the best outcomes for participants, then Study 3 will be conceptualized utilizing those conditions. We will collect data pre-treatment, post-treatment and three months post-treatment.
Participants
Twenty 8–13 year old overweight and obese children and their parents.
Outcomes
In addition to pertinent assessments determined in Study 1 and 2, we will also collect acceptability, liking (from both parents and children) and adherence and retention data.
4. Intervention
4.1 Interventionists
All interventionists will be clinical psychologists, advanced graduate students or postdoctoral fellows in clinical psychology. All interventionists will follow a treatment manual and protocol and participate in trainings with the study director. All interventionists will conduct mock treatment cases that will be videotaped and scored for adherence to the protocol by the study director before treating study cases. Treatment sessions will be videotaped to allow the investigator to assess each interventionist’s performance and protocol adherence. Investigators will rate 10% of the recorded sessions for treatment fidelity. Interventionists will attend weekly supervision sessions with the investigator and study director to review each parent and child’s progress and make necessary adjustments to the protocol.
4.2 CET-Food intervention
All families will attend a one-hour initial psychoeducation session describing the background, purpose, and expectations of the treatment before beginning the exposure sessions. All parents/adults who may attend treatments with the child will be required to attend the psychoeducation session. The psychoeducation session includes information about how the obesogenic environment, food cue sensitivity, and learning mechanisms conditioning contribute to overeating and being overweight. The interventionist describes learning theory, the rationale for cue exposure treatment as a potential treatment for managing cravings to food in the presence of food, and the importance of learning behavioral skills to reduce overeating. Parent and child are also provided specific details about the treatment process and upcoming exposure sessions. Between the psychoeducation session and the first exposure session, parent and child will be asked to complete hunger and craving logs, with the purpose of introducing appetite awareness, learning the differences between hunger and cravings, and triggers and patterns for cravings, and the types of foods they crave.
In each treatment visit, parent and child will meet with the interventionist together, will discuss psychoeducational material, review homework and craving logs, participate in a CET-Food session, and participate in post-processing to consolidate learnings from the exposure experience. Each session will include a review of skills that will enhance treatment (e.g. self-monitoring of cravings, parenting skills). Parents will participate alongside their child, even if they are not struggling with overeating and will be asked to model appropriate responding to food cues and cravings. The child (with parent’s assistance as needed) will be asked to track their cravings in between exposure sessions. All treatment sessions will be approximately one hour in duration.
Each treatment visit will begin by a review of the craving self-monitoring journals. Families are also asked whether they have had any of the previous exposure session’s food since their last session. This is done to track whether there were opportunities for re-pairing of previous foods used in exposures with consumption.
The treatment sessions will use the metaphor of a craving volcano as a way of discussing and assessing cravings. Parent and child will track their cravings on a 1–5 scale. During the CET-Food sessions, the interventionist will place the exposure food on plates in front of the parent and child. Children and parents will be told to hold, smell, or taste the food and notice and track their self-reported cravings on a craving sheet every thirty seconds. After three minutes, the interventionist will prompt the parent and child to again hold, smell, or taste the food, with thirty seconds elapsing between each prompt. In addition to these action prompts, children and parents are also directed to notice and/or describe their physiological responding to the food (e.g., salivation), sensory perceptions of the food, and cognitions about the food. After five minutes, children and parents will be asked to throw away the food. The next food is brought into the room and the above procedures are followed until exposures to all four foods are complete.
Treatment sessions also include psychoeducation on various topics and skills related to CET-Food. Each child and parent will be given handouts each week that focus on each of the topics in Table 2. Psychoeducational content and materials will be titrated to the number of sessions. Parenting skills (modeling, teamwork, praise, stimulus control, daily check-ins about progress) are provided to reinforce the learning of skills learned in treatment sessions and increase generalizability of skills outside of treatment sessions. Participants will not be prescribed a diet as part of the iROC program; however, handouts denoting foods that are likely to decrease hunger/increase satiety and reduce cravings will be provided. Moreover, the parent will be encouraged to use stimulus control around the child’s highly craved foods, and recommendations will be made to limit the access to these foods until they feel that the child can manage their cravings successfully. Additionally, a motivation system will be implemented to increase session attendance. Children will receive points that can be exchanged for toy incentives in the lab.
Table 2.
List of psychoeducational handouts for the iROC treatment.
| Session # | Topic |
|---|---|
| 1 | Food exposures and cravings, self-monitoring, daily meetings |
| 2 | What causes cravings? |
| 3 | The environment and cravings |
| 4 | Stimulus and portion control |
| 5 | Parenting skills |
| 6 | Child coping skills |
| 7 | Hunger, satiety, and cravings |
| 8 | Diet/nutrition related to hunger, satiety and cravings |
| 9 | Pavlovian conditioning review |
| 10 | Exposures review |
| 11 | Cravings review |
| 12 | Self-monitoring review |
| 13 | Stimulus and portion control review |
| 14 | Parenting, child coping skills review |
| 15 | Diet/nutrition related to hunger, satiety and cravings review |
| 16 | Congratulations, reflect on successes |
Note: The schedule of topics above is for the 16-week condition. The 8-week condition will include two topics at each session.
During the post-exposure verbal processing section, positive reinforcement will be used to reinforce the child’s ability to resist the foods and recognize their craving levels throughout the exposure. The interventionist will process challenges during the exposure with the child and will discuss how the child overcame them. The child’s self-competency in managing their cravings to food outside of the treatment sessions will also be discussed. If the child’s cravings are still high at the end of the session, the interventionist will help the child understand that cravings are normal and that an important skill the child is demonstrating is that he or she can experience a craving, but still not eat the food.
5. Data
5.1 Data collection and management
All data will be collected at the UCSD Center for Healthy Eating and Activity Research (CHEAR) by trained and certified assessment staff. Children and parents will directly enter de-identified data using a participant number in a secure, web-based survey system. All assessment staff will be supervised on a weekly basis. All data will be checked following participant assessments. All non-web-based data will be scored and double entered, and checked for missing data and outliers. Necessary firewall and password protections are implemented, and nightly backups will be conducted by the IT division in the Pediatrics Department at UCSD. The Data Manager, under the supervision of the PI and the statistician, will be responsible for developing and maintaining the database.
5.2 Statistical analyses
Analyses will be based on generalized linear mixed models54–56 implemented in SAS® version 9.2.57 Continuous outcomes will be modeled with a normal distribution and identity link function and count outcomes with a Poisson distribution and a log link function. For the experimental studies (Studies 1 and 2), fixed effects will include coefficients for time, factor (i.e., between-subjects treatment), and time by factor interactions. For each outcome, selection of a covariance structure for the residuals will be based on fitting four structures (compound symmetry, first order autoregressive, Toeplitz, and an unstructured covariance matrix) and selecting the one with the lowest sample size adjusted Akaike’s Information Criterion.53 Standard errors for fixed effects will be based on empirical standard errors estimated with the root sandwich estimator, which make the standard errors less sensitive to misspecification of the covariance structure and has less bias than the classical sandwich estimator when used with small samples.54 For count outcomes, an additional overdispersion parameter will be incorporated into the model. Significance tests will focus on the treatment by time interactions. Follow-up contrasts will be used to test comparisons of interest. For contrasts a correction to the p-value will be applied based on a simulated Holm’s procedure.55 All significance tests will use a nominal alpha of .05.
In order to assess the extent to which cue exposure training generalizes to other foods we will compare calories eaten of the target food to the average of calories eaten of all other foods in a particular food category. Repeated measures t-tests will be used to evaluate these hypotheses. To assess whether time to extinction decreases over exposure sessions, we will use generalized linear mixed models, in which we will fit a non-normal error distributions (e.g., gamma), given the likelihood of a positively skewed distribution. In these analyses neither censored observations nor missing data are anticipated.
6. Discussion
The iROC study evaluates four factors from the extinction and learning literature to strengthen CET-Food and to translate the learnings to multiple contexts, and then uses the data from these studies to conduct a proof of concept study. To date, there are very few studies on translating basic behavioral concepts, including extinction, to interventions for overeating. The studies in iROC draw upon Bouton’s conceptualization of conditioning and appetite56 and expands these concepts by adding the translation to human studies using cue exposure treatments. This study will provide data to support the design of a CET-Food intervention to decrease overeating in overweight and obese children. Furthermore, this study extends the basic science literature on conditioning and extinction, and will provide in depth knowledge regarding how these concepts translate to humans, and how they can be most effectively utilized.
Our approach is novel in that we assess overeating in the laboratory using a well-established paradigm (eating in the absence of hunger)34,35 as well as a multi-modal assessment battery testing multiple components of food cravings, from physiological assessments to subjective perception. The knowledge gained by the psychophysiological markers could greatly enhance our knowledge of physiological responding, and decreasing responding to food. It will contribute to the knowledge base regarding extinction of food cue reactivity in humans. The psychophysiological markers could be useful in laboratory studies, as outcomes in larger clinical trials, as well as targets in future treatments. Furthermore, our assessment battery includes measures f cognitive and physiological measures of food cue reactivity, including attentional bias to food cues, memory for food cues, motor impulsivity to food cues, food reward, food cue interference and physiological responses to food cues. Some of these measures were created by the authors, and once validated, will add substantially to the field in understanding the behavioral and brain processes in relation to food intake behaviors and weight. Combined with self-report questionnaires and interviews, the addition of several behavioral laboratory experimental paradigms will provide a more comprehensive picture of a child’s relationship with food, and may provide insight into weight-loss treatment modalities best suited for individuals with high levels of eating in the absence of hunger.
Current models of family-based treatment for childhood obesity57,58 include “stimulus control techniques,” or methods to avoid being exposed to tempting food cues. It is impossible in today’s environment to attempt to avoid all potential cues for overeating, especially for children who have less control over their own environments than adults. Rather than elimination, teaching mastery of psychological and physiological food cue responsivity may have profound implications for overweight children in managing the omnipresent food cues in their environment. However, embarking down a substantially different path is not without its challenges, and we may need to make refinements throughout this trial as we gain more experience with these methods. Additionally, although we utilize a laboratory based measure of overeating, we recognize the biases inherent in these methods and attempt to identify behavioral tasks and measures that can serve as intermediary assessments in developing treatments that target cue reactivity.
There are potential important challenges that may arise during the iROC study. It is possible, but not probable, that conducting CET-Food with one food each week for eight weeks will have the largest effect on outcome measures, similar to our previous studies. We will analyze data in between studies to understand the impact of CET-Food on outcome measures, and will adjust the next studies accordingly. Additionally, it is possible, that our measures may not show consistent results in each treatment arm. In this case, it will be important to consider the basic research, and the conceptual reasons behind the outcome measures, in order to determine which line of outcomes to follow. Finally, it is possible that we will have challenges with recruiting overweight and obese children and their parents for such a study. However, at the time of the writing of this manuscript, we have completed Study 1 with very little attrition (7%).
By the end of this series of studies, we will have a method for providing CET-Food to obese children and their parents, as well as proof of concept data on CET-Food, in preparation for randomized clinical trials that may utilize CET-Food as an enhancement or potentially as a stand-alone treatment. We will also have information on the translation of extinction processes to food cue reactivity. These studies have the opportunity to introduce a new paradigm for the treatment of childhood obesity, targeting reduction of food cue reactivity and tolerance.
7. Conclusions
Very little research in obesity utilizes knowledge from basic behavioral sciences to develop interventions in a methodical manner. The iROC study will use a hierarchical approach to utilize information from conditioning and extinction literature to improve CET-Food. Although in its infancy, these studies have the opportunity to introduce a new paradigm for the treatment of childhood obesity. It is possible that this treatment could be delivered to a specific behavioral phenotype of overweight children who are most responsive to this treatment, or more broadly, tailoring interventions to subtypes of children that will respond best to particular treatment modes. The psychophysiological data could also launch a series of other studies evaluating different types of interventions (e.g. medications) to decrease physiological responding to food.
Acknowledgments
Supported by grants to KB (R01DK094475; K02HL112042)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimer statement: Authors have no conflicts to declare
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swinburn BA, Sacks G, Lo SK, Westerterp KR, Rush EC, Rosenbaum M, et al. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr. 2009;89(6):1723–8. doi: 10.3945/ajcn.2008.27061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woods SC. The eating paradox: How we tolerate food. Psychol Rev. 1991;98(4):488–505. doi: 10.1037/0033-295x.98.4.488. [DOI] [PubMed] [Google Scholar]
- 4.Woods SC, Strubbe JH. The psychobiology of meals. Psychonomic Bulletin & Review. 1994;1:141–55. doi: 10.3758/BF03200770. [DOI] [PubMed] [Google Scholar]
- 5.Holland PC, Petrovich GD. A neural systems analysis of the potentiation of feeding by conditioned stimuli. Physiol Behav. 2005;86(5):747–61. doi: 10.1016/j.physbeh.2005.08.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferriday D, Brunstrom JM. ‘I just can’t help myself’: Effects of food-cue exposure in overweight and lean individuals. Int J Obes. 2011;35(1):142–9. doi: 10.1038/ijo.2010.117. [DOI] [PubMed] [Google Scholar]
- 7.Tetley A, Brunstrom J, Griffiths P. Individual differences in food-cue reactivity. The role of BMI and everyday portion-size selections Appetite. 2009;52(3):614–20. doi: 10.1016/j.appet.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Stice E, Spoor S, Bohon C, Small DM. Relation between obesity and blunted striatal response to food is moderated by TaqIA A1 allele. Science. 2008;322(5900):449–52. doi: 10.1126/science.1161550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stoeckel LE, Weller RE, Cook EW, 3rd, Twieg DB, Knowlton RC, Cox JE. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. Neuroimage. 2008;41(2):636–47. doi: 10.1016/j.neuroimage.2008.02.031. [DOI] [PubMed] [Google Scholar]
- 10.Bruce AS, Holsen LM, Chambers RJ, Martin LE, Brooks WM, Zarcone JR, et al. Obese children show hyperactivation to food pictures in brain networks linked to motivation, reward and cognitive control. Int J Obes. 2010;34(10):1494–500. doi: 10.1038/ijo.2010.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davids S, Lauffer H, Thoms K, Jagdhuhn M, Hirschfeld H, Domin M, et al. Increased dorsolateral prefrontal cortex activation in obese children during observation of food stimuli. Int J Obes. 2010;34(1):94–104. doi: 10.1038/ijo.2009.193. [DOI] [PubMed] [Google Scholar]
- 12.Boutelle KN, Wierenga CE, Bischoff-Grethe A, Melrose AJ, Grenesko-Stevens E, Paulus MP, Kaye WH. Increased brain response to appetitive tastes in the insula and amygdala in obese compared to healthy weight children when sated. International Journal of Obesity. 2014 doi: 10.1038/ijo.2014.206. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bouton ME. Context and behavioral processes in extinction. Learn Mem. 2004;11(5):485–94. doi: 10.1101/lm.78804. [DOI] [PubMed] [Google Scholar]
- 14.Myers KM, Davis M. Behavioral and neural analysis of extinction. Neuron. 2002;36(4):567–84. doi: 10.1016/s0896-6273(02)01064-4. [DOI] [PubMed] [Google Scholar]
- 15.Bouton ME. Context, ambiguity, and unlearning: sources of relapse after behavioral extinction. Biol Psychiatry. 2002;52(10):976–86. doi: 10.1016/s0006-3223(02)01546-9. [DOI] [PubMed] [Google Scholar]
- 16.Bouton ME, Woods AM, Moody EW, Sunsay C, Garcia-Gutierrez A. Counteracting the context-dependence of extinction: Relapse and tests of some relapse prevention methods. In: Craske MG, Hermans D, Vansteenwegen, editors. Fear and learning; From basic processes to clinical implications. Washington, D.C.: American Psychological Association; 2006. [Google Scholar]
- 17.Moody EW, Sunsay C, Bouton ME. Priming and trial spacing in extinction: effects on extinction performance, spontaneous recovery, and reinstatement in appetitive conditioning. Q J Exp Psychol (Colchester) 2006;59(5):809–29. doi: 10.1080/17470210500299045. [DOI] [PubMed] [Google Scholar]
- 18.Sunsay C, Bouton ME. Analysis of a trial-spacing effect with relatively long intertrial intervals. Learn Behav. 2008;36(2):104–15. doi: 10.3758/lb.36.2.104. [DOI] [PubMed] [Google Scholar]
- 19.Sunsay C, Stetson L, Bouton ME. Memory priming and trial spacing effects in Pavlovian learning. Learn Behav. 2004;32(2):220–9. doi: 10.3758/bf03196023. [DOI] [PubMed] [Google Scholar]
- 20.Bouton ME, Sunsay C. Contextual control of appetitive conditioning: influence of a contextual stimulus generated by a partial reinforcement procedure. Q J Exp Psychol B. 2001;54(2):109–25. doi: 10.1080/713932752. [DOI] [PubMed] [Google Scholar]
- 21.Bouton ME, Sunsay C. Importance of trials versus accumulating time across trials in partially reinforced appetitive conditioning. J Exp Psychol Anim Behav Process. 2003;29(1):62–77. [PubMed] [Google Scholar]
- 22.Collins BN, Brandon TH. Effects of extinction context and retrieval cues on alcohol cue reactivity among nonalcoholic drinkers. J Consult Clin Psychol. 2002;70(2):390–7. [PubMed] [Google Scholar]
- 23.Stasiewicz PR, Brandon TH, Bradizza CM. Effects of extinction context and retrieval cues on renewal of alcohol-cue reactivity among alcohol-dependent outpatients. Psychol Addict Behav. 2007;21(2):244–8. doi: 10.1037/0893-164X.21.2.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boutelle KN, Zucker NL, Peterson CB, Rydell SA, Cafri G, Harnack L. Two novel treatments to reduce overeating in overweight children: a randomized controlled trial. J Consult Clin Psychol. 2011;79(6):759–71. doi: 10.1037/a0025713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boutelle KN, Zucker N, Peterson CB, Rydell S, Carlson J, Harnack LJ. An Intervention Based on Schachter’s Externality Theory for Overweight Children: The Regulation of Cues Pilot. J Pediatr Psychol. 2014 doi: 10.1093/jpepsy/jst142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behaviour Research and Therapy. 2014;58:10–23. doi: 10.1016/j.brat.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dietz WH. Periods of risk in childhood for the development of adult obesity–what do we need to learn? J Nutr. 1997;127(9):1884S–86S. doi: 10.1093/jn/127.9.1884S. [DOI] [PubMed] [Google Scholar]
- 28.Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr. 1994;59(5):955–9. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- 29.Magarey AM, Daniels LA, Boulton TJ, Cockington RA. Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes Relat Metab Disord. 2003;27(4):505–13. doi: 10.1038/sj.ijo.0802251. [DOI] [PubMed] [Google Scholar]
- 30.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 31.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- 32.Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the eating disorder examination with children: a pilot study. Int J Eat Disord. 1996;19(4):391–7. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 33.Wilkinson GS, Robertson GJ. Wide Range Achievement Test 4 professional manual. Lutz, FL: Psychological Assessment Resources; 2006. [Google Scholar]
- 34.Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. Am J Clin Nutr. 2002;76(1):226–31. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Birch LL, Fisher JO. Mothers’ child-feeding practices influence daughters’ eating and weight. Am J Clin Nutr. 2000;71(5):1054–61. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Eating in the absence of hunger: a genetic marker for childhood obesity in prepubertal boys? Obesity. 2006;14(1):131–8. doi: 10.1038/oby.2006.16. [DOI] [PubMed] [Google Scholar]
- 37.National Academy of Sciences. Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) 2005 Retrieved from http://fnic.nal.usda.gov/nal_dispaly/index.php?
- 38.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 39.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;(314):1–27. [PubMed] [Google Scholar]
- 40.Amir N, Beard C, Burns M, Bomyea J. Attention modification program in individuals with generalized anxiety disorder. J Abnorm Psychol. 2009;118(1):28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boutelle KN, Kuckertz JM, Carlson J, Amir N. A pilot study evaluating a one-session attention modification training to decrease overeating in obese children. Appetite. 2014;76:180–5. doi: 10.1016/j.appet.2014.01.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Delis DCKJ, Kaplan E, Ober BA. The California Verbal Learning Test-Children’s Version. New York: Psychological Corporation; 1994. [Google Scholar]
- 43.Nederkoorn C, Coelho JS, Guerrieri R, Houben K, Jansen A. Specificity of the failure to inhibit responses in overweight children. Appetite. 2012;59(2):409–13. doi: 10.1016/j.appet.2012.05.028. [DOI] [PubMed] [Google Scholar]
- 44.Logan GD, Cowan WB, Davis KA. On the ability to inhibit simple and choice reaction time responses: a model and a method. J Exp Psychol Hum Percept Perform. 1984;10(2):276–91. doi: 10.1037//0096-1523.10.2.276. [DOI] [PubMed] [Google Scholar]
- 45.Verbruggen F, Logan GD, Stevens MA. STOP-IT: Windows executable software for the stop-signal paradigm. Behav Res Methods. 2008;40(2):479–83. doi: 10.3758/brm.40.2.479. [DOI] [PubMed] [Google Scholar]
- 46.Epstein LH. Behavioral Choice Task for Measuring Absolute and Relative Reinforcing Value and Habituation of Operant Behavior. 2007. [Google Scholar]
- 47.Braet C, Crombez G. Cognitive interference due to food cues in childhood obesity. J Clin Child Adolesc Psychol. 2003;32(1):32–9. doi: 10.1207/S15374424JCCP3201_04. [DOI] [PubMed] [Google Scholar]
- 48.Soetens B, Braet C. Information processing of food cues in overweight and normal weight adolescents. Br J Health Psychol. 2007;12(Pt 2):285–304. doi: 10.1348/135910706X107604. [DOI] [PubMed] [Google Scholar]
- 49.Nederkoorn C, Smulders FT, Jansen A. Cephalic phase responses, craving and food intake in normal subjects. Appetite. 2000;35(1):45–55. doi: 10.1006/appe.2000.0328. [DOI] [PubMed] [Google Scholar]
- 50.Nederkoorn C, Jansen A. Cue reactivity and regulation of food intake. Eat Behav. 2002;3(1):61–72. doi: 10.1016/s1471-0153(01)00045-9. [DOI] [PubMed] [Google Scholar]
- 51.Carney RM, Freedland KE. Depression and heart rate variability in patients with coronary heart disease. Cleve Clin J Med. 2009;76(Suppl 2):S13–7. doi: 10.3949/ccjm.76.s2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nederkoorn C, Smulders FT, Jansen A. Recording of swallowing events using electromyography as a non-invasive measurement of salivation. Appetite. 1999;33(3):361–9. doi: 10.1006/appe.1999.0268. [DOI] [PubMed] [Google Scholar]
- 53.Burnham KP, Anderson DR. Model Selection and Multimodel Inference: A Practical Information-Theoretic Approach. 2. Springer-Verlag; 2002. [Google Scholar]
- 54.Kauermann G, Carroll RJ. A Note on the Efficiency of Sandwich Covariance Estimation. Journal of the American Statistical Association. 2001;(96):1387–96. [Google Scholar]
- 55.Westfall PH. Multiple Testing of General Contrasts Using Logical Constraints and Correlations. Journal of the American Statistical Association. 1997;92:299–306. [Google Scholar]
- 56.Bouton ME. Learning and the persistence of appetite: extinction and the motivation to eat and overeat. Physiology & behavior. 2011;103(1):51–8. doi: 10.1016/j.physbeh.2010.11.025. [DOI] [PubMed] [Google Scholar]
- 57.Epstein LH. Family-based behavioural intervention for obese children. Int J Obes Relat Metab Disord. 1996;20(Suppl 1):S14–21. [PubMed] [Google Scholar]
- 58.Epstein LH, Roemmich JN, Raynor HA. Behavioral therapy in the treatment of pediatric obesity. Pediatr Clin North Am. 2001;48(4):981–93. doi: 10.1016/s0031-3955(05)70352-7. [DOI] [PubMed] [Google Scholar]
- 59.Barratt W. The Barratt Simplified Measure of Social Status (BSMSS) measuring SES. Indiana State University; 2006. [Google Scholar]
- 60.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36(3):201–10. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 61.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addictive behaviors. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 62.Shomaker LB, Tanofsky-Kraff M, Elliott C, Wolkoff LE, Columbo KM, Ranzenhofer LM, et al. Salience of loss of control for pediatric binge episodes: Does size really matter? The International journal of eating disorders. 2009 doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tanofsky-Kraff M, Ranzenhofer LM, Yanovski SZ, Schvey NA, Faith M, Gustafson J, et al. Psychometric properties of a new questionnaire to assess eating in the absence of hunger in children and adolescents. Appetite. 2008;51(1):148–55. doi: 10.1016/j.appet.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the Children’s Eating Behaviour Questionnaire. Journal of child psychology and psychiatry, and allied disciplines. 2001;42(7):963–70. doi: 10.1111/1469-7610.00792. [DOI] [PubMed] [Google Scholar]
- 65.Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–70. [PubMed] [Google Scholar]
- 66.Cepeda-Benito A, Gleaves DH, Williams TL, Erath SA. The development and validation of the state and trait food-cravings questionnaires. Behavior therapy. 2000;31(1):151–73. doi: 10.1016/s0005-7967(99)00141-2. [DOI] [PubMed] [Google Scholar]
- 67.Lowe MR, Butryn ML, Didie ER, Annunziato RA, Thomas JG, Crerand CE, et al. The Power of Food Scale. A new measure of the psychological influence of the food environment Appetite. 2009;53(1):114–8. doi: 10.1016/j.appet.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 68.Radloff LA. The use of the Center for Epidemiological Studies Depression Scale in adolescent and young adults. Journal of Youth and Adolescence. 1991;20:149–66. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 69.March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(4):554–65. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 70.Spielberger CD. Manual for the State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- 71.Spielberger C, Gorsuch R, Lushene R. Manual for the State-Trait Anxiety Inventory. 1970. [Google Scholar]
- 72.Achenbach TM, Edelbroch D. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont, Department of Psychology; 1991. [Google Scholar]
- 73.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–6. [PubMed] [Google Scholar]
- 74.Crandall VC, Crandall VJ, Katkovsky W. A Children’s Social Desirability Questionnaire. Journal of consulting psychology. 1965;29:27–36. doi: 10.1037/h0020966. [DOI] [PubMed] [Google Scholar]


