Abstract
The intestine comprises an exceptional venue for a dynamic and complex interplay of numerous chemical and biological processes. Here, multiple chemical and biological systems, including the intestinal tissue itself, its associated immune system, the gut microbiota, xenobiotics, and metabolites meet and interact to form a sophisticated and tightly regulated state of tissue homoeostasis. Disturbance of this homeostasis can cause inflammatory bowel disease (IBD) – a chronic disease of multifactorial etiology that is strongly associated with increased risk for cancer development. This review addresses recent developments in research into chemical and biological mechanisms underlying the etiology of inflammation-induced colon cancer. Beginning with a general overview of reactive chemical species generated during colonic inflammation, the mechanistic interplay between chemical and biological mediators of inflammation, the role of genetic toxicology and microbial pathogenesis in disease development are discussed. When possible, we systematically compare evidence from studies utilizing human IBD patients with experimental investigations in mice. The comparison reveals that many strong pathological and mechanistic correlates exist between mouse models of colitis-associated cancer, and the clinically relevant situation in humans. We also summarize several emerging issues in the field, such as the carcinogenic potential of novel inflammation-related DNA adducts and genotoxic microbial factors, the systemic dimension of inflammation-induced genotoxicity, and the complex role of genome maintenance mechanisms during these processes. Taken together, current evidence points to the induction of genetic and epigenetic alterations by chemical and biological inflammatory stimuli ultimately leading to cancer formation.
Keywords: Inflammation, cancer, inflammatory bowel disease, innate immunity, nitric oxide, peroxynitrite, hypochlorous acid, iNOS, myeloperoxidase, DNA damage, DNA repair, biomarkers
1. Introduction: inflammatory bowel disease and colon cancer
With respect to a functional interplay between chemistry and biology, the intestinal tract is one of the most complex organs in the body. In the intestine, local epithelial cells closely interact with the body’s immune system and meet with a complex bacterial microflora and a plethora of endogenous metabolites and xenobiotic substances. All of these factors need to be tightly balanced to ensure intestinal homeostasis and to guarantee efficient uptake of nutrients and excretion of metabolites. If this balance is disturbed, pathological states can appear, such as inflammatory bowel disease (IBD). As a major risk factor for colon cancer, IBD entails chronic, relapsing inflammation of the gastrointestinal tract that affects millions of people worldwide, with >1 million new patients each year in the US alone [1]. The paucity of safe and effective therapies for IBD amplifies its public health impact and motivates the hunt for the molecular etiology of the disease and the mechanisms linking colitis with colon carcinogenesis. This review addresses recent developments in chemical and biological mechanisms underlying inflammation-induced colon cancer, starting with a general overview of the reactive chemical species generated during colonic inflammation followed by a discussion of the mechanistic interplay between chemical and biological mediators of inflammation and the role of microbial pathogenesis and genetic toxicology in the etiology of inflammation-induced colon cancer. The reader is referred to several recent reviews of molecular aspects of IBD and cancer development not covered here, in particular immunological and genetic studies [1–7].
1.1 Inflammatory bowel disease: Crohn’s disease and ulcerative colitis
Inflammatory bowel disease comes in two distinct forms: Crohn’s disease and ulcerative colitis. In Crohn’s disease, inflammation often affects the entire thickness of the bowel wall and affects mainly the ileum and colon, but can discontinuously spread throughout any part of the intestine. In contrast, the inflammation in ulcerative colitis is usually confined to the mucosal surface of the intestines and limited to colon and rectum, spreading in a continuous fashion (reviewed in [1]). The pathophysiology of IBD is multifactorial, with contributions from genetic, epigenetic, environmental, and endogenous microbial factors (reviewed in [3,8]). Genetic background is an important determinant for IBD, evidenced by the fact that family history is a risk factor for disease development with a concordance rate in monozygotic twins of 10–15% in ulcerative colitis and 30–35% in Crohn’s disease. At present, more than 150 genetic loci have been associated with disease development [9]. IBD-associated genes are involved in several disease-relevant pathways crucial for intestinal homeostasis, including epithelial barrier function, microbial defense mechanisms, regulation of immunity, autophagy, generation of reactive oxygen and nitrogen species (ROS, RNS) and signaling functions. About 30% of these loci are shared between ulcerative colitis and Crohn’s disease, so the two pathological states share some similar molecular mechanisms, but also exhibit many disease-specific features [3,9]. The contribution of environmental factors is not well understood, but evidence indicates that they play a significant role, as suggested by the high prevalence of IBD in industrialized countries. This pattern of high prevalence appears not to be related to genetic factors, since migrant studies have demonstrated that individuals relocating from a region with low prevalence to one of high prevalence are at increased risk of developing IBD [10]. Environmental influences include life-style factors such as smoking and dietary composition among others, but may also be related to improved sanitation and hygiene. The latter is based on the hypothesis that lack of childhood exposure to enteric pathogens may lead to inappropriate immune responses to new antigens in adulthood and an imbalance in host-microbe interaction, which play an important role in the maintenance of mucosal homeostasis [10]. An imbalance of host-microbe homeostasis is of paramount importance in the etiology of IBD, supported by the fact that some IBD patients benefit from antibiotic treatment and most mouse models of IBD require the presence of intestinal bacteria to develop colitis [1]. Furthermore, an altered immune response to the intestinal flora plays a pivotal role in the etiology of IBD [8]. Notably, the intestine and its associated tissues represent the largest immunological organ of the body. In particular, the intestinal lamina propria contains a complex mixture of immune cells that maintain immune tolerance and pathogen defense in a tightly controlled balance (reviewed in [1]). Active IBD is characterized by a massive infiltration of innate immune cells, including neutrophils, macrophages, dendritic cells, and natural killer cells, which fulfill complex roles under physiological as well as pathophysiological conditions. Importantly in the context of this review, activated neutrophils and macrophages are major sources of ROS and RNS that are among the main factors against invading pathogens, but can also cause collateral damage to the host tissue, thereby potentially initiating and promoting carcinogenesis (see below). Apart from innate immune cells, those of the adaptive immune system (e.g., B and T cells), also control intestinal homeostasis. Perturbation of the balance of Th17 cells, which produce the pro-inflammatory signature cytokines IL-17, IL-21, and IL-23, and regulatory T-cells, which produce the anti-inflammatory cytokines IL-10 and TGF-β appear to be of particular importance. An imbalance in these systems seems to play a crucial role in the etiology of IBD (reviewed in [2]). For an in-depth discussion on the intestinal immunology in the pathology of IBD, the reader is referred to several recent reviews [2,4,6,11–17]. In summary, IBD is a multifactorial disease that is thought to result from a perturbation in host-microbe interactions leading to an immunological imbalance and chronic inflammation in genetically susceptible individuals [3].
Strong epidemiological evidence indicates that inflammation existing in Crohn’s disease and ulcerative colitis is associated with increased risk of colon cancer, but the responsible molecular mechanisms remain largely undefined. More than 20% of patients with IBD develop colitis-associated cancers within 30 years of disease onset, and >50% of these patients die from them [7]. Notably, patients who develop IBD at a young age (< 30 yrs) have a much greater risk of cancer development [18]. In general, the risk for colon cancer increases with duration and severity of disease, whereas it decreases when patients are treated with anti-inflammatory drugs such as mesalamine and corticosteroids, consistent with a causative role for inflammation in colon carcinogenesis (reviewed in [19]).
Spontaneous colorectal cancer shares many common pathophysiological mechanisms with colitis-associated cancer, but differs in some distinct ways (reviewed in [7]). For example, both types of cancer progress through a sequence of aberrant crypt foci, polyps, adenomas, and carcinomas. However, dysplasia in spontaneous colorectal cancer is often focal, whereas colitis-associated cancers often develop through a sequence of chronic inflammation, tissue injury, and multifocal dysplasia leading to the formation of poorly-defined carcinomas. The genetic alterations such as chromosomal instability, microsatellite instability, and DNA hypermethylation found in spontaneous colon cancers also occur in colitis-associated cancers; these characteristics arise in inflamed tissue before the appearance of histological evidence of dysplasia or cancer [19]. Common tumor-related signaling pathways, including factors such as Wnt, β-catenin, K-ras, p53, TGF-β, and DNA repair, are affected in development of spontaneous as well as colitis-associated cancers, but at different stages of tumor formation [7]. It is very likely that crypt stem cells represent the cells-of-origin for cancer development, in both spontaneous colorectal and colitis-associated cancers [20]. However, recent studies demonstrate that NF-κB signaling can lead to dedifferentiation of intestinal epithelial cells into tumor-initiating cells with stem cell-like properties [21]. This is consistent with the fact that colitis-associated carcinogenesis (CAC) is characterized by production of NF-κB and Stat3-dependent pro-inflammatory cytokines, and activation or inactivation of oncogenes and tumor suppressors, respectively. Reactive chemical species are likely to play an important role in these processes and there is increasing experimental evidence supporting the hypothesis that during inflammation, cells of the innate immune system generate large amounts of ROS and RNS inducing genetic and epigenetic changes, which may lead to mutations and tumor initiation and promotion [22].
1.2 Mouse models of colitis-associated carcinogenesis
Several mouse models of colitis have been developed to study molecular disease mechanisms and to define targets for translational approaches. Colitis is induced by chemical agents, by genetic intervention, by infection or by combinations of these factors (Table 1). In light of the recent criticism of mouse models of human disease [23,24], which in our opinion has been overstated and inaccurate, we demonstrate that many compelling pathological and mechanistic correlates exist between mouse models of colitis-associated cancer and the clinically relevant disease in humans. Indeed, as we review here, a plethora of studies in mouse models of colitis have revealed that many chemical and biological mechanisms of pathology share strong similarities across species boundaries (Table 2), which is most evident by the fact that human IBD and various forms of colitis in mice lead to an increased risk of colon carcinogenesis. Only through the combination of animal models and studies utilizing human IBD patients can a deeper understanding be obtained of the molecular mechanisms in CAC, through the use of multidisciplinary approaches from genetics to microbiology, chemistry, systems biology and mathematical modeling, combined with thoughtful data interpretation.
Table 1.
Common mouse models of colitis-associated carcinogenesis. For more detailed reviews on mouse models of IBD see [261–263].
| Model | Specification | Mechanism | Reference |
|---|---|---|---|
| DSS | Chemical-induced (Supplementation of drinking water) |
Disruption of the epithelial barrier. DSS polymers are not genotoxic, but directly toxic to colonic epithelial cells of the basal crypts. Protocols exist for acute and chronic colitis. Colitis induced within 2 (acute) to 8 (chronic) weeks. Development of dysplasia and colon cancers requires several months. In the acute phase inflammation is mainly driven by innate immunity. | [264] |
| DSS + AOM | Chemical-induced (Supplementation of drinking water) |
Carcinogen-induced. Initial dose of AOM in combination with DSS. Bioactivation of AOM to mutagenic methyldiazonium ion. Tumor formation within 10 weeks. Useful to study the role of inflammation after carcinogen-induced tumor-initiation. | [265] |
| TNBS in ethanol | Chemical-induced (intrarectal administration) |
Hapten-induced hypersensitivity. Activation of a T-cell-mediated response against hapten-modified autologous proteins/luminal antigens. Protocols for acute and chronic colitis. Colitis induced within 2 weeks. Inflammation dependent on innate and adaptive immunity (Th1- and Th17-type). | [264] |
| Il-10−/− mice | Genetic | Disruption of anti-inflammatory signaling. Mild disease progression. Development of a spontaneous CD4+ Th1-driven enterocolitis. Dependent on IFN-γ in the initial phase and Il12 for disease progression. Development of adenocarcinoma after ~6 months. | [266,267] |
| Gpx1/2−/− mice | Genetic | Interference with antioxidant response. GPx1/2 detoxify H2O2 by glutathione oxidation. Development of ileocolitis between 2–7 weeks of age. Dysplasia and adenocarcinoma after ~4 months. | [120] |
| H.h.-infected Rag2−/−mice | Genetic + infection | Lack of adaptive immunity causes disturbed pathogen response. Induction of chronic typhlocolitis 10 weeks p.i. with first occurrence of colon carcinomas 20 weeks p.i. Since Rag2−/− mice lack adaptive immunity, inflammation is driven by innate immunity. | [25–28] |
AOM, azoxymethane; DSS, dextran sodium sulfate; TNBS, 2,4,6-trinitro benzene sulfonic acid; GPx, glutathione peroxidase; H.h., Helicobacter hepaticus; p.i., post infection.
Table 2.
Comparison of mouse and human studies on parameters of immunological chemistry and genotoxicology.
| Parameter | Mouse (model system) | Human |
|---|---|---|
| Infiltration of neutrophils and macrophages | ↑ [37] (acetic acid), [39] (TNBS) [38] (Il10−/), [26,27] (H.h. Rag2−/−), [104] (C.r) |
↑ [1] |
| Induction of NADPH ox expression | ↑ [27] (H.h. Rag2−/−) |
↑ [46,47] |
| Induction of XOR expression | ↑ [27] (H.h. Rag2−/−) |
n.c. [53] |
| Induction of iNOS expression | ↑ [37] (acetic acid), [39,77,97] (TNBS), [78,86] (DSS), [38] (Il10−/−), [26,27] (H.h. Rag2−/−) |
↑ [53,73,74,93,94,96,98,99,268–270] |
| Induction of MPO expression | ↑ [79] (DSS), [39,97] (TNBS), [26,27] (H.h. Rag2−/−), [104] (C.r.) |
↑ [53,110] |
| GSH content | ↓ (transient) [111] (TNBS) |
↓ [113,114] |
| Induction of GPx2 expression | ↑ [117] (DSS), [117] (TNBS), [27] (H.h. Rag2−/−) |
↑ [114,117] |
| Nitrotyrosine | ↑ [86] (DSS), [39,97] (TNBS) [29] (H.h. Rag2−/−), [104] (C.r.) |
↑ [53,73,74,95,96] ↑ (in serum) [29] |
| Chlorotyrosine | ↑ [29] (H.h. Rag2−/−), [104] (C.r.) |
↑ (in serum) [29] |
| Nitrosative DNA deamination | dI ↑ [27] (H.h. Rag2−/−) |
n.a. |
| Oxidative DNA damage | ↑ [61,168,175] (DSS), [168] (Il10−/−); [167] (CD45RBhigh CD4+ T cell→SCID transfer model), [32] (Ikkβ(EE)IEC/Apc+/ΔIEC) ↓ (transient) [27] (H.h. Rag2−/−) |
↑ [114,170] |
| Lipid-peroxidation-induced damage | ↑ [175] (DSS) ↓ (transient) [27] (H.h. Rag2−/−) |
↑ [173,176–178] ↓ (in PBMC from CRC patients) [181] |
| Halogenation DNA damage | ↑ [27] (H.h. Rag2−/−) |
Detected [29] |
| DSB and chromosomal rearrangements | ↑ [168,207] (DSS), [168,207] (Il10−/−), [57] (TNBS), [27] (H.h. Rag2−/−) |
↑ [208–212] |
n.c., no change; n.a., data not available, CRC, colorectal cancer; C.r., Citrobacter rodentium; H.h., Helicobacter hepaticus
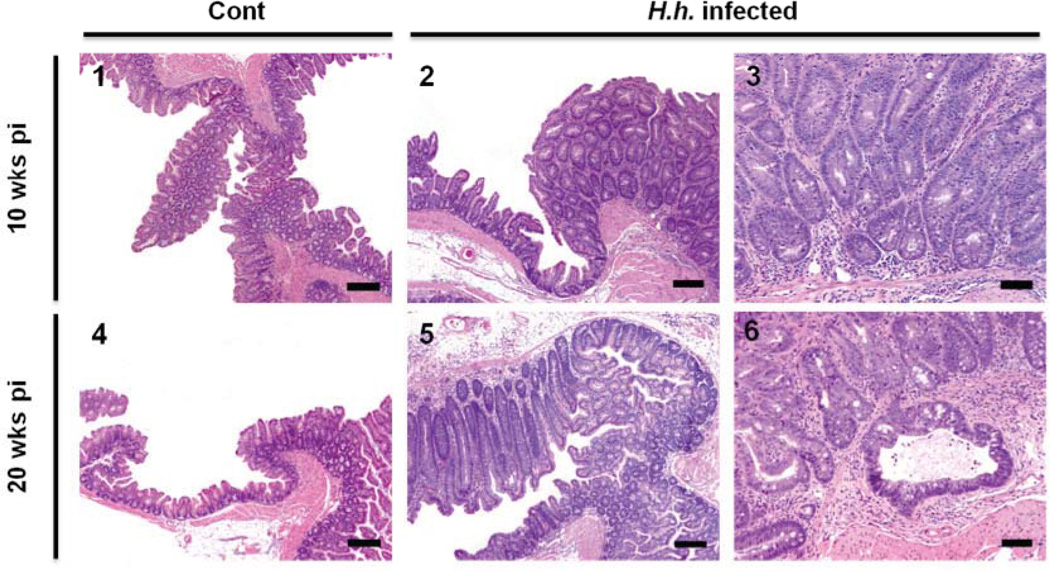
We recently conducted a systematic analysis of mechanisms and biomarkers of Helicobacter hepaticus (H. hepaticus)-induced colitis in immunodeficient 129 Rag2−/− mice with respect to various aspects of disease development [25–29]. The gram-negative spiral bacterium H. hepaticus colonizes the liver and intestinal crypts of the cecum and the colon, establishing a life-long infection [25,26,30,31]. H. hepaticus does not typically cause disease in immunocompetent mice, but infection in susceptible mouse strains or in immunodeficient mice, such as those lacking the recombinase-activating gene-2 (Rag2), results in chronic colitis and colon cancer [25] (Figure 1). H. hepaticus infection in Rag2−/− mice emulates many aspects of human IBD and as discussed here, this mouse model has proved to be a valuable tool specifically to study features of innate immunity during CAC.
Figure 1. Colon histopathology in H. hepaticus infected Rag2−/− mice.
Photomicrographs of H&E-stained sections of ileocecocolic junction. Representative sections from control (1 and 4) and H. hepaticus-infected (2–3 and 5–6) mice at 10 and 20 weeks post infection (wks pi). Images 2 and 5 show marked mucosal hyperplasia in infected mice at both time-points. Images 3 and 6 represent higher magnification photomicrographs to demonstrate the associated dysplasia and carcinoma development. Reprinted from [27]; with permission of the PNAS.
2 Immunological chemistry of inflammatory bowel disease
Colonic inflammation results in a local release of cytokines and other chemotactic factors that cause infiltration and activation of innate immune cells to produce large quantities of other cytokines and chemokines resulting in the activation of various enzymes that generate a wide spectrum of reactive chemical species as summarized in Figure 2 and discussed in the following sections in detail. In particular, we summarize evidence that these chemical mediators of inflammation can react with all types of macromolecules, including proteins, RNA, and DNA, to cause mutagenic and cytotoxic damage, thereby contributing to colon carcinogenesis.
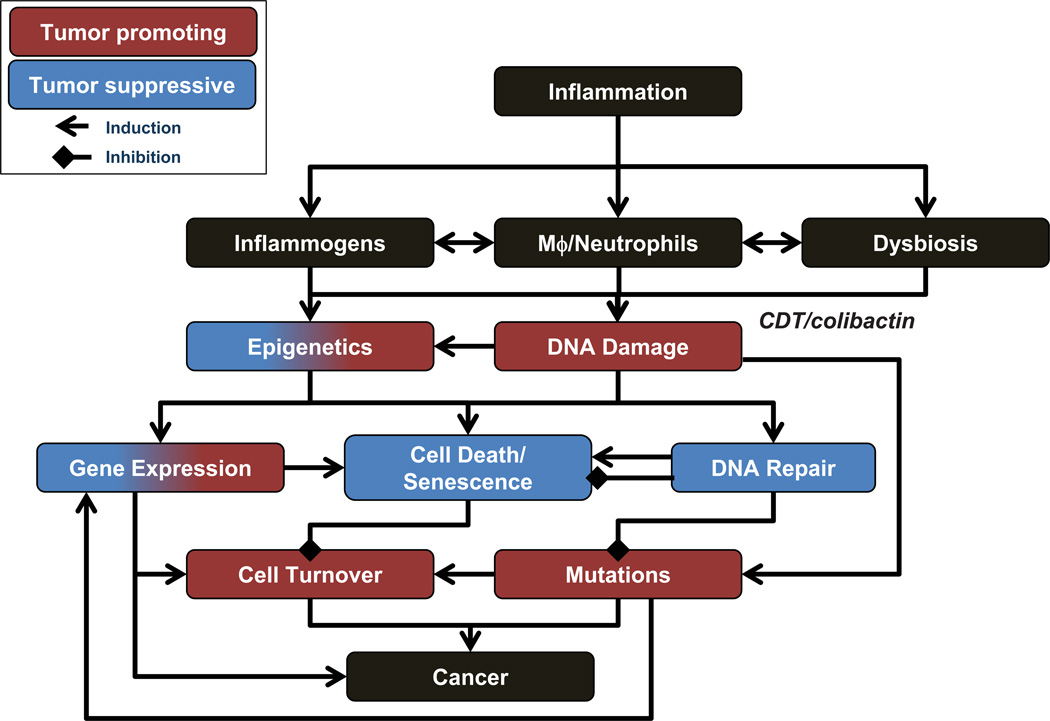
Figure 2. Chemical and biological mechanisms of inflammation [Illustration by Jeff Dixon].
For details see text. iNOS, inducible nitric oxide synthase; MPO, myeloperoxidase; NOX, NADPH oxidase; XO, xanthine oxidase.
2.1 Cell types involved in the generation of reactive chemical species during IBD
In addition to the endogenous production of NO by colonic epithelial cells [32–35], macrophages and neutrophils are thought to be responsible for the bulk of ROS and RNS generation during acute and chronic inflammation (Figure 2). Both cell types are closely related and cooperate during the onset, progression and resolution of inflammation. Usually, tissue-resident macrophages and dendritic cells sense inflammatory stimuli, which causes chemokine-dependent recruitment of neutrophils followed by infiltration of blood monocytes, both of which then differentiate and become activated (reviewed in [14]).
Initial support of the hypothesis that innate immune cells can act as carcinogens was obtained by Weitzman and colleagues, who exposed mouse fibroblasts to activated human neutrophils or a cell-free ROS-producing system. Following injection of the fibroblasts into nude mice, tumors developed, but only in mice injected with exposed cells. Mice injected with control cells remained tumor-free, which indicated that activated neutrophils and ROS are able to mediate malignant cell transformation [36]. It is well established that neutrophils and macrophages play a pivotal role in the induction and maintenance of inflammation during colitis in mice and humans [26,37–39]. In addition, several studies support the functional relevance of these cell types during colon carcinogenesis. For example, in a rat model of dextran sodium sulfate (DSS)-induced acute colitis, selective depletion of neutrophils by intraperitoneal injection of a neutrophil-specific monoclonal antibody significantly reduced pathology [40]. A similar antibody-based approach was used to selectively deplete mature neutrophils in H. hepaticus-infected Rag2−/− mice, a model in which there is massive infiltration of macrophages and neutrophils during disease development [26,27,29]. Interestingly, depletion of neutrophils in these mice significantly decreased the severity of colon pathology, including cancer rates, and led to lower expression of pro-inflammatory cytokines and ROS/RNS-generating enzymes (see below) [26]. Macrophages can also contribute to disease progression and severity, as shown in a mouse model of H. bilis-induced typhlocolitis, in which macrophages were selectively depleted by treatment with clodronate-containing liposomes. Clodronate-treated mice exhibited significantly lower histopathology scores and suppressed expression of macrophage-related factors, such as TNF-α, Il-1β, and iNOS, suggesting that macrophages are important mediators of H. bilis-induced colitis. However, the finding that clodronate treatment concomitantly reduced the number of MPO-positive neutrophils suggests that both macrophages and neutrophils closely interact in disease development on a functional level [41]. This view is supported by the H. hepaticus Rag2−/− mouse model that revealed cytokine signatures suggestive of both neutrophil and macrophage activity [29]. Interestingly, this finding correlated well with results from patients with Crohn’s disease. In contrast, cytokine signatures of patients with ulcerative colitis were more suggestive of neutrophil activity only, indicating specific differences between the two types of IBD on a molecular level [29].
2.2 NADPH oxidases, xanthine oxidoreductase, and the generation of ROS
Superoxide (O2•−), is the primary source of ROS in humans. Under physiological conditions, mitochondrial respiration is the major source, whereas NADPH oxidase (official gene symbol: Nox, not to be confused with NOx which refers to NO oxidation products) and xanthine oxidoreductase (XOR) significantly contribute to the generation of O2•− under pathophysiological conditions (reviewed in [42–44]) (Figure 2).
NADPH oxidases represent a widely distributed family of enzymes, with each species consisting of a flavoprotein, cytochrome b and several regulatory subunits. When activated, the enzymes assemble in the cell membrane and reduce oxygen to O2•−. Phagocytic cells express NADPH oxidase 2 in the phagosomal membrane, where it generates high fluxes of O2•− (reviewed in [42,43,45]). In addition to ‘phagocyte NADPH oxidases 2’, NADPH oxidases 1 is highly expressed in the gastrointestinal tract. Levels of the mRNA of NADPH oxidase 1, also known as the ‘colon NADPH oxidase’, increase from proximal to distal colon [45]. Even under physiological conditions, NADPH oxidase 1 is highly expressed in colon epithelial cells, both within the crypts and on the luminal surface [46,47]. Maturation-dependent factors seem to regulate the expression of NADPH oxidase 1 in colonic epithelial cells, which leads to the highest expression levels in surface mucous cells where NADPH oxidases are thought to contribute to host defense. However, under pathophysiological conditions, they may mediate tissue damage by generating ROS. This view is consistent with results from H. hepaticus-induced colitis in Rag2−/− mice, in which gene expression of NADPH oxidases 1 and 2 (Nox 1, Nox2) was significantly up-regulated in inflamed tissue. This was accompanied by higher expression levels of several regulatory subunits of the NADPH oxidase system, such as Ncf1 (p47phox) and Ncf2 (p67phox) [27], presumably a result of tissue infiltration of innate immune cells. In addition, studies in mice and human cells have shown that pro-inflammatory cytokines induced during colitis activate expression of NADPH oxidases [48,49]. The role of NADPH oxidase in human IBD and colon carcinogenesis is not well characterized. Some evidence comes from patients with chronic granulomatous disease, many of whom have genetic defects in the NADPH oxidase system that results in an immunodeficiency phenotype characterized by an inability of phagocytes to kill invading pathogens. These patients exhibit an increased risk for IBD, suggesting that NADPH oxidases have a direct role in controlling intestinal homeostasis [45,50,51]. Szanto et al. reported strong expression of NADPH oxidase 1 in active lesions from patients with Crohn’s disease and ulcerative colitis [46] and Fukuyama et al. reported significant up-regulation of NADPH oxidase 1 in colonic tumor tissue [47], suggesting a functional role of NADPH oxidases in disease progression. Despite these findings, comprehensive understanding of the functional role of NADPH oxidases in CAC is incomplete, and conclusions rely mainly on correlative studies, while mechanistic studies in mice and humans are limited. Genetic studies analyzing mechanisms of CAC in mice carrying mutations or deletions in the NADPH oxidase system would be of interest with respect to pharmacological interventions, since NADPH oxidases are already being considered as potential drug targets for treatment of other inflammatory disorders, such as vascular disease [43].
Xanthine oxidoreductase (XOR) is a multifunctional enzyme that is expressed and secreted by many epithelial cells including those in the colonic mucosa (reviewed in [44]) (Figure 2). The enzyme possesses two activities, as both a reductase and an oxidase. The reductase catalyzes the oxidative hydroxylation of hypoxanthine to xanthine and subsequently of xanthine to uric acid. In this functional state, xanthine reductase acts as a housekeeping enzyme with a role in purine catabolism, detoxification and the regulation of the cellular redox potential. Various stimuli induce the conversion into an oxidase, either reversibly by thiol oxidation or irreversibly by limited proteolysis. In contrast to the reductase, xanthine oxidase is associated with production of large amounts of ROS including O2•− [44]. The enzyme has also been directly implicated in the activation of macrophages through effects on chemokine expression and other factors, thereby participating in macrophage-mediated neutrophil recruitment [52].
In the human colon, XOR immunostaining follows a gradient along the villus-crypt axis in a pattern similar to that observed for NOX1, with luminal epithelial cells showing the strongest staining. XOR staining was also observed in cells at the base of the crypt, as well as in neutrophils and endothelial cells in the lamina propria [53]. Data on the role of XOR in colitis and associated cancer development is limited and controversial. H. hepaticus-infected Rag2−/− mice showed higher expression levels of XOR mRNA in inflamed tissue, but the origin of this increase is currently unknown [27]. Up-regulation of XOR is consistent with the finding that XOR is stimulated by IFN-γ, TNF-α, and IL-1, and some of these factors also trigger the reductase-oxidase conversion [44]. Furthermore, Siems et al. reported that the XOR inhibitor oxypurinol protects mice from morphological and molecular changes occurring in TNBS-induced colitis. However, as is it the case with every pharmacological inhibitor, specificity of the compound is an issue. Although these results indicate a role of XOR in murine colitis and XOR has been associated with other inflammatory diseases [44], its role in human IBD awaits further clarification. Kruidenier et al. reported that epithelial apoptosis in patients with Crohn’s disease was strongly associated with XOR expression, suggesting a role for XOR in the regulation of epithelial homeostasis. However, in this study, overall levels of XOR were unaffected during intestinal inflammation, indicating that XOR contributes to disease development more through local and functional changes in its activity [53]. Mouse genetics could shed some light on the role of XOR in colitis, which could be instrumental to test potential treatment options by targeting this enzyme. In this respect, generation of colon-specific knock-out mice or mice that specifically lack the enzymes’s oxidase function may represent one possible line of investigation, since Xor−/− mice die within the first six weeks after birth due to renal failure [54,55].
Superoxide can be transformed by superoxide dismutases (SOD) into hydrogen peroxide (H2O2), which can be either detoxified by catalases and peroxidases into H2O and O2, or it can be reduced by divalent metal ions in Fenton chemistry that gives rise to highly reactive hydroxyl radicals (•OH) [42] (Figure 2). Since H2O2 reacts poorly with most biological molecules and is highly diffusible, it acts as an important signal transducer (reviewed in [42,56]). For example, H2O2 activates phosphorylation cascades resulting in downstream effects such as enhanced stress resistance, cell proliferation, cytokine release, cell adhesion, growth arrest and apoptosis. Its damaging effects are mainly caused by its reaction with seleno-, thiol or heme peroxidases to produce radical and non-radical species as well as through •OH formed by Fenton chemistry [42]. In mice with TNBS-induced colitis, H2O2 levels immediately increased in the muscularis externa within the first week after treatment, with peak levels achieved after the first day [57]. That the generation of H2O2 acts as a detoxifying pathway is suggested by studies of SOD, the major source of H2O2. For example, in DSS-induced colitis, Cu/Zn-SOD-overexpressing transgenic mice showed a survival benefit that was accompanied by an enhanced clearance of neutrophils [58]. Moreover, studies in which SOD and SOD mimetics were administered during TNBS and DSS-induced colitis revealed beneficial effects of SOD with regards to disease severity and molecular damage [59–62]. In studies of human colitis, MnSOD was strongly up-regulated in inflamed epithelium, whereas the Cu/ZnSOD content decreased with inflammation. On a cellular level, Cu/Zn and MnSOD were prominently present in neutrophils and macrophages, while extracellular (EC)-SOD was mainly localized in small vessels, stromal cells, and neutrophils. This differential regulation of the SOD isoforms indicates that ROS generation and its detoxification are important factors in the etiology of IBD, whose specific role needs to be clarified in future studies [63].
2.3 Nitric oxide synthases and the generation of reactive nitrogen species (RNS)
Nitric oxide (NO) is the key molecule during the generation of RNS (Figure 2). Since NO has a low molecular weight, is uncharged, and is soluble in both aqueous and hydrophobic environments, it is highly diffusible across cell membranes and through tissues. The diffusion coefficient for NO is 3300 µm2s−1, which is comparable to that for O2 (2800 µm2s−1) and implies that NO is able to diffuse as far as 5–10 cell diameters in 1 sec [56]. NO production in cell culture studies coincides with the appearance of NO2− and NO3−, which are formed at approximately equal and constant rates [64]. These metabolites arise from NO auto-oxidation by reacting with O2 to form nitrogen dioxide radical (NO2•) that can react further with NO2• or NO to form N2O4 or N2O3, respectively. These higher N-oxides can subsequently form NO2−, NO3− and nitroso products, which are closely related with enzymatic as well as non-enzymatic conversions with complex (patho-)physiological consequences [65–67]. Furthermore, NO reacts with O2•− at diffusion controlled rates to form peroxynitrite (ONOO−) [68] (Figure 2). ONOO− represents an important source of a complex spectrum of highly reactive secondary radicals [42]. Its protonated form, ONOOH, undergoes rapid (t1/2 ~ 1 sec) homolysis to form the strongly oxidizing •OH and the weaker oxidant NO2•. In addition, ONOO− reacts with CO2, which is present in millimolar concentrations in tissues, to form nitrosoperoxycarbonate (ONOOCO2−), which decomposes with a half life of ~50 msec into NO2• and highly reactive carbonate radical anions (CO3•−) [69]. When the concentration of NO• exceeds that of O2•−, which predominantly occurs within cellular membranes, autoxidation leads to the formation of NO2• and N2O3. N2O3 itself is an S- and N-nitrosating species, but readily decomposes with a half-life of 0.2 msec [56,69].
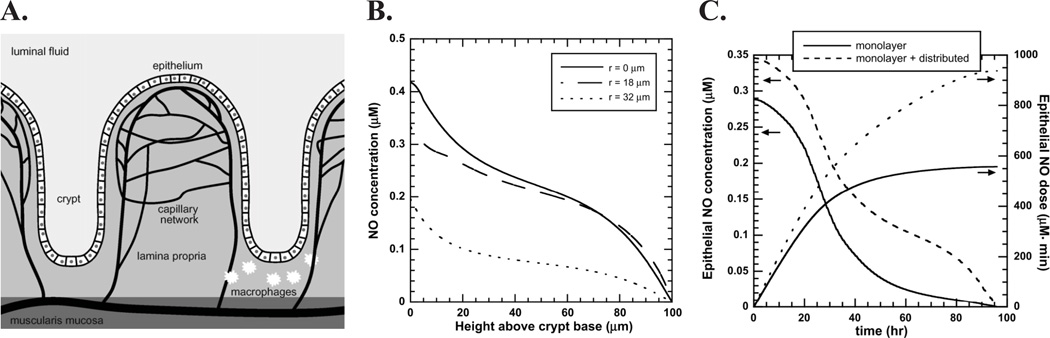
Three isoforms of NO synthases exist that can generate NO over a wide range of concentrations in an NADPH and O2-dependent process by converting L-arginine to citrulline and NO [70]. Neuronal and endothelial NOS produce NO at low levels in nerve and endothelial cells, respectively, while activation of inducible NOS (iNOS) leads to high NO concentrations in macrophages during inflamation (reviewed in [71]). In general, the biology of NO can be divided into two categories: (i) direct effects of NO mediated by chemical reactions that occur fast enough to allow NO to react directly with biological target molecules, and (ii) indirect effects that require that NO reacts with other ROS to generate RNS, which then react with biological targets [56]. Biological functions of NO are highly concentration dependent, with relevant concentrations varying over three orders-of-magnitude. One of the major challenges in the study of colitis has been to define the concentrations of NO arising in the inflamed colon and the biological consequences of the different concentrations of NO and its derivatives in the inflamed tissue. In this regard, significant insights have been obtained from computational modeling. By describing rates of reaction and diffusion in realistic geometries, mathematical modeling has estimated that maximal NO concentrations reached at the base of a crypt are in the sub-micromolar range (~0.3 µM) and the cumulative NO dose an epithelial cell is experiencing during migration from the base to the top of the crypt is ~560 µM min [72] (Figure 3). Taking into account findings that epithelial cells contribute to the NO production in the colon [32,73,74] and that macrophages are able to infiltrate into the lamina propria, these models predict maximal NO concentrations of ~ 0.4 µM and maximal cumulative doses of ~1 µM min [72] (Figure 3). These calculations are in accordance with cell culture studies demonstrating that upon stimulation macrophages produce levels of NO up to 1 µM [64]. As a rule of thumb, at low (nM) concentrations NO promotes cell survival and proliferation and acts as an important signaling molecule in the cardiovascular, nervous and immune systems, while, at higher concentrations (≤ 1 µM), such as may occur at sites of inflammation, it can be cytotoxic and cytostatic, inducing cell cycle arrest, apoptosis and senescence [56,69,75,76].
Figure 3. Computational modeling of colonic NO concentration.
A. Schematic representation of colonic crypt anatomy. The inner lining of the colonic mucosa consists of three distinct layers: the muscularis mucosa, the lamina propria, and the epithelium. B. NO concentration as a function of height above crypt base taking into account NO synthesis by macrophages and epithelial cells. The NO synthesis rate per unit volume in epithelial cells was assumed here to be 5.6 µM/s, the same as the baseline rate for macrophages. This is a conservative value; it is conceivable that rates in vivo are much higher. Axial concentration variations are shown for radial positions r = 0, 18, 32 µm, which corresponds to the center of the luminal fluid, middle of the epithelium, and middle of the lamina propria region, respectively. C. Time-dependent NO concentration and cumulative NO dose experienced by an epithelial cell as it migrates from the crypt base to the mucosal surface. The total time for migration was assumed to be 96 h. The ‘monolayer model’ assumes that the main source of NO is a confluent monolayer of macrophages localized in the region below the crypt base (see A.), whereas the ‘monolayer + distributed model’ assumes that macrophages are also distributed throughout the lamina propria. Reprinted from [72] (with permission of Elsevier).
During colitis, iNOS is considered the main source of NO. In healthy mice, iNOS mRNA is expressed in the ileum, but not in the jejunum or colon. iNOS protein is also detected in normal ileal epithelial cells, suggesting that it may also fulfill a role in maintaining intestinal homeostasis [33]. In the inflamed gut, iNOS is present throughout the intestinal tract, including the jejunum and colon [26,27,33,37,77,78]. Induction of iNOS is regulated by neutrophils and macrophages in combination with cytokine stimuli, as suggested by the fact that depletion of Gr-1+ neutrophils, clodronate-induced depletion of macrophages, and blocking of TNF-α in the colon, respectively, prevented iNOS induction [26,41]. Various mouse studies demonstrated that colitis-induced activation of iNOS is accompanied by increased levels of NO-derived species in plasma and urine [26,38,39,79]. Saijo et al. studied the dynamics of biomarkers of NO production, such as NO2−, NO3−, and nitroso and nitrosyl species during DSS-induced chronic and acute colitis [80], and showed that blood levels of nitroso products correlated well with disease development. This correlation was also true for plasma levels of NO2− and NO3−, but only in acute colitis during the onset of the inflammatory response. A more complex response of these ions was observed in tissues as well as in the chronic colitis model. Interestingly, for all markers analyzed, similar changes were observed in organs other than colon, such as liver, brain, aorta, and heart, highlighting the systemic effects of this disease. In general, the study by Saijo et al. suggests that NO2− serves as a suitable indicator of colitis per se, although the rise of plasma NO2− may not correlate well with the progression and resolution of inflammation [80].
Supporting the notion that NO generation during colitis can be attributed to the activation of iNOS, no increase in NO-derived species was observed during colitis in Il-10−/− mice in an iNos−/− background [38]. Similarly, in H. hepaticus-infected Rag2−/− mice concurrent administration of an iNOS inhibitor prevented NO3− production and reduced epithelial pathology and cancer incidence [26]. Similarly, an iNOS inhibitor significantly reduced colonic adenocarcinoma formation in a dose-dependent manner in a CAC model using DSS-treated ApcMin/+ mice [81]. These effects can be directly attributed to iNOS inhibition, since during H. hepaticus-induced colitis, iNOS inhibitor treatment had no influence on the numbers of neutrophils and macrophages [26]. Interestingly, administration of iNOS inhibitors also decreased the levels of pro-inflammatory cytokines such as TNF-α and IL-1β in DSS-induced colitis, indicating a positive-feedback regulation of these components under inflammatory conditions [79,81]. The notion that ONOO− can not only act as a downstream effector molecule, but also as an active driving force of disease development is supported by the finding that intrarectal administration of ONOO− itself was sufficient to induce the generation of NO-derived species, iNOS expression, and colitis in rats [82].
Ambiguous results were obtained from genetic studies of colitis in iNos−/− mice. Several groups reported a protective effect of iNOS depletion on tissue inflammation, damage, and cancer rates [39,78,83–85], whereas others found no effect [38,86] or even more severe tissue damage and pathology in iNos−/− mice [37,87]. Krieglstein et al. performed bone marrow transplantation experiments using iNOS-proficient or -deficient cells transplanted into wild-type or iNos−/− mice. In mice deficient in either tissue or blood cell iNOS, or both, DSS-induced colitis was attenuated. Interestingly, MPO activity was also lower in iNos−/− mice and occurred at the lowest levels in iNos−/− mice transplanted with blood cells carrying functional iNOS. These results suggest that both blood-cell and tissue-derived iNOS plays a role in DSS-induced colitis, with tissue-associated iNOS making a larger contribution to the recruitment of MPO-positive inflammatory cells [84]. Similarly, Beck et al. showed that chimeric mouse lines with iNOS-deficient blood cells were more resistant to DSS and TNBS-induced colitis; in the DSS model neutrophils were the main source of iNOS [88]. This is in agreement with our finding that depletion of Gr-1+ neutrophils of H. hepaticus-infected mice prevented iNOS induction in the colon [26]. Another study analyzed mouse lines deficient in iNOS, nNOS, eNOS or e/nNOS and revealed that loss of iNOS or eNOS was protective on DSS-induced colitis, whereas loss of nNOS resulted in more severe disease and higher mortality rates. These results indicate that NO produced by individual isoforms plays different roles in the modulation of intestinal inflammation [85]. In terms of signature biomarkers of iNOS activity, H. hepaticus-induced colitis in Rag2−/− mice led to significantly higher levels of nitrotyrosine in colon tissue as well as in serum [29]. Similarly, TNBS-induced colitis led to increased levels of nitrotyrosine [39]. In this model, ablation of iNOS resulted in reduced levels of nitrotyrosine indicating that iNOS is required for the generation of nitrosative damage [39]. On the other hand, in iNos+/+ and iNos−/− mice with chronic DSS-induced colitis showed no differences in nitrotyrosine levels, pointing to a role of MPO activity (see below) [86]. These apparently contradictory results may be reconciled by a mechanism in which depletion of iNOS has a protective effect mostly in models of acute, severe colitis, whereas, in models of chronic colitis, depletion of iNOS has either no effect or results in more severe pathology [37,38,86,87]. The different effects of iNOS depletion in different colitis models may therefore be dependent upon the severity of disease at the time point analyzed and may represent the double-edged role of NO as a signaling molecule on the one hand and a tissue-damaging factor on the other. Moreover, there is evidence for endogenous production of NO by iNOS in epithelial cells [87,88[73,74]. Recently, Shaked et al. demonstrated that mice with a deletion in one allele of the Apc gene specifically in intestinal epithelial cells (IEC) in combination with constitutively active NF-κB signaling in these cells (Ikkβ(EE)IEC/Apc+/ΔIEC mice) show increased levels of iNOS expression, DNA damage induction and elevated colon carcinogenesis [32]. Interestingly, these mice developed intestinal tumors despite the absence of signs of pathology and hyperplasia typical of colonic inflammation. Treatment of these mice with an iNOS inhibitor reduced cancer rates and molecular damage markers highlighting the iNOS-dependency of the observed effects (see below for further discussion of this mouse model) [32].
Although there is a controversy about the factors that trigger human macrophages to produce NO and the quantity of NO generated [89–92], the results obtained with rodent models of IBD have largely been confirmed in humans. Thus, increased iNOS expression and activity were also identified in patients with Crohn’s disease and ulcerative colitis [73,74,93,94]. Interestingly, as observed in mouse models, iNOS and nitrotyrosine were not only detected in mononuclear cells, but also in neutrophils, which suggests a significant role for this cell type in NO production during human disease [74]. Several studies have found a correlation between increased iNOS expression during IBD and nitrotyrosine levels and NO production itself [73,74,94–97], but correlation of NOS activity with severity of disease was not always evident, and profound differences in molecular fingerprints existing between Crohn’s disease and ulcerative colitis [93,98,99]. In terms of biomarker development, a recent study of 38 patients with ulcerative colitis and 42 patients with Crohn’s disease revealed only slightly elevated plasma levels of nitrotyrosine in active compared to inactive IBD, and no significant differences were found compared to non-IBD control subjects. These results suggest that NO-derived damage is less pronounced in humans compared to rodent colitis models and that nitrotyrosine may not be the most suitable biomarker of human disease [29].
2.4 MPO and the generation of HOCl
Hypochlorous acid (HOCl,) is one of the most potent antimicrobial compounds released by activated immune cells as a first-line defense mechanism against invading pathogens. During inflammation, HOCl could lead to injurious reactions in surrounding host tissue. HOCl is generated from Cl− and H2O2 by heme peroxidases, such as neutrophil MPO or eosinophil peroxidase (EPO) (Figure 2). Analogous reactions generate hypobromous acid (HOBr) and hypothiocyanous acids (HOSCN). All of these molecules are particularly reactive with thiols, methionine, and tyrosine, and are also capable of damaging nucleobases (see below, reviewed in [42,100,101]). For a more in-depth discussion of the various and complex reactions mediated by MPO, the reader is referred to recent reviews [102,103].
Although there are reports that MPO is expressed in specific monocytes and macrophages, its major site of expression is the neutrophil, and MPO immunostaining is often used as a marker for the in situ detection of neutrophils. Within neutrophils, MPO is stored mainly in azurophilic granules, which are released into the extracellular space during neutrophil activation [103]. It is therefore not surprising that MPO protein levels and activity are elevated during colitis, since neutrophils are recruited to sites of inflammation [27,79,104]. In mouse models of C. rodentium-induced acute colitis and H. hepaticus-induced chronic colitis, infiltration of MPO-positive cells was associated with increased tissue and serum levels of protein damage markers of HOCl (e.g., chlorotyrosine) [27,29,104]. Interestingly, in both mouse models, increases in chlorotyrosine were much more pronounced than increases in nitrotyrosine, indicating that MPO-mediated halogenation chemistry is of central importance during infection-induced colitis in mice. Increases in nitrotyrosine in these mouse models may be also attributable to MPO activity, since it was shown that MPO (and EPO) can use H2O2 to convert NO2− to NO2• via a nitryl chloride (NO2Cl) intermediate [105]. During inflammation this process may also contribute to cytotoxicity mediated by tyrosine nitration and chlorination, and other macromolecular damage. Using MPO- and EPO-deficient mice, Brennan et al. demonstrated that MPO and EPO participate in nitrotyrosine formation in vivo, possibly by generation of NO2• and, to a lesser extent, ONOO−; in some instances, MPO and EPO accounted for the majority of the nitrotyrosine formed [106]. Similar results were obtained in a model in which peritonitis was induced either by cecal ligation and puncture or by infection with K. pneumoniae; only the latter led to an increase of total NO2− and NO3− levels of about 20-fold and to increased levels of nitrotyrosine [107]. In contrast, nitrotyrosine levels remained unchanged in K. pneumoniae-infected mice deficient in MPO, supporting the view that MPO is capable of generating RNS in vivo [107]. Also noteworthy was the finding in a human study that increases in nitrotyrosine in ulcerative colitis correlated only with MPO expression and not with that of iNOS [53].
In contrast to reports of studies in iNos−/− mice, none have been reported in Mpo−/− -deficient mice to assess the role of MPO during colitis and CAC. However, some information is available from other pathological states. While Mpo−/− mice were more susceptible to several types of infections, such as infections with Candida albicans and Klebsiella pneumoniae, they paradoxically showed more severe atherosclerosis [108]. Additionally, deficiency in MPO was associated with increased infarct volumes and nitrotyrosine formation in a mouse model of ischemic brain injury [109]. These studies thus suggest a protective, anti-inflammatory role of MPO, in at least select inflammation-related pathologies [103,108,109]. Thus, the possibility cannot be excluded that MPO expression and activity during colitis might serve as in part a mechanism of tissue protection rather than tissue destruction. Studies in Mpo−/− mice with respect to colitis and colon cancer development would help to clarify this interesting question.
In the context of the fact that MPO expression is well correlated with human IBD, a recent study revealed that MPO immunostaining may serve as marker to assess disease activity in patients with ulcerative colitis [110]. This is consistent with our own study in patients with ulcerative colitis and Crohn’s disease where MPO-derived chlorotyrosine was significantly elevated in serum from patients with ulcerative colitis and Crohn’s disease, potentially contributing to a set of biomarkers for IBD activity in human serum [29].
2.5 Antioxidant defense
Efficient antioxidant defense systems exist to keep the cellular redox state in balance. The most prominent ones include the glutathione/glutathione disulfide (GSH/GSSG), cysteine/cystine (Cys/CySS), and thioredoxin/thioredoxin disulfide (TRx/TRxSS) redox couples. These systems maintain mucosal integrity and intestinal homeostasis, which is evident by the fact that, e.g., GSH is present in millimolar concentrations in the intestinal epithelium and its de novo synthesis can be efficiently induced upon pathological stimuli. Nevertheless, conditions of oxidative and nitrosatative stress can occur if ROS and RNS levels exceed the cellular antioxidative capacity.
Evidence supporting an active role of antioxidant defense mechanisms in the control of intestinal homeostasis comes from both mouse and human studies. Ardite et al. suggested that TNBS-induced colitis is triggered by ROS generation followed by GSH depletion. Following treatment with TNBS, GSH pools in colon mucosa were found to be depleted, an effect that was inhibited by administration of the GSH precursor and antioxidant N-acetylcysteine (NAC), which resulted in significantly less histological injury. Underpining the dynamic and tightly regulated control of antioxidant systems, GSH levels recovered after ~1 week of TNBS treatment due to induction of γ-glutamylcysteine synthase gene expression [111]. NAC-protective effects were also observed in a long-term DSS-induced colitis model, in which NAC treatment reduced histopathology accompanied by reduced numbers of nitrotyrosine and iNOS-containing cells in the mucosa. Mechanistically, the finding that NAC administration reduced tumor incidence may be attributed to sensitization of epithelial cells to apoptosis [112]. Redox regulation also plays an important role in human IBD, which is evident by findings that intestinal subepithelial myofibroblasts in patients with Crohn’s disease exhibited an increased oxidative state due to a decrease in the GSH/GSSG ratio [113] and GSH content in tissue from colorectal tumors was much lower than in non-malignant tissue [114].
Several enzymes are involved in the intra-intestinal antioxidant defense. For example, glutaredoxins (GRx) and glutathione reductase (GSR) catalyze the reduction of GSSG through thiol-disulfide exchanges. Similarly, thioredoxin reductases (TxnRD) are involved in the regeneration of thioredoxin. Gluthathione peroxidases (GPx) are the major H2O2-reducing intestinal selenoproteins and GSH S-transferases catalyze GSH-detoxification reactions of luminal electrophiles and carcinogens (reviewed in [115]). These antioxidant defense systems are dynamically regulated in the course of colitis development as recently revealed by sensitive qPCR-array-based gene expression profiling in H. hepaticus-infected Rag2−/− mice [27]. Unexpectedly, several antioxidant enzymes, such as MnSOD and catalase, showed modestly decreased levels in inflamed tissue, whereas others, including glutathione and thioredoxin reductases (Gsr and Txnrd1) as well as Gpx2, displayed higher expression levels, which points to complex regulatory networks that counteract oxidative stress during colitis.
In particular, GPx2 is an interesting factor in the etiology of colitis. GPx2 is a gastrointestinal-specific form of GPx that is highly expressed at crypt bases. Similar to other glutathione peroxidases, GPx2 reduces hydroperoxides using GSH. However, GPx2 seems to play a double-edged role during the etiology of IBD [116]. GPx2 is up regulated during colitis, and possibly could protect colon tissue by reducing concentrations of inflammation-derived hydroperoxides, which may otherwise give rise to highly reactive •OH [117]. In accordance with this view, Gpx2−/− mice were susceptible to DSS-induced colitis and Gpx2−/− mice treated with a combination of DSS and azoxymethane (AOM) tended to develop higher incidence of tumors than wild-type animals [118]. Of note, tumor incidence in this model showed a strong positive correlation with inflammation scores [116]. Some defects caused by GPx2 deficiency are thought to be compensated by up-regulation of GPx1 [119]. This becomes more evident by the finding that in GPx1/2 double deficiency spontaneous development of colitis was accompanied by elevated levels of MPO activity, increased mutation frequencies, and spontaneous cancer development [120]. In spite of the evidence for a protective role, tumor sizes were smaller in Gpx2−/− mice. This has been associated with anti-apoptotic and pro-proliferative properties of GPx2 and highlights the double-edged role of this enzyme in CAC [116,118,119]. This view is consistent with human data showing that expression levels of GPx1 and GPx3 were significantly decreased in colorectal tumor samples, whereas those of GPx2 were increased [114].
Gpx2 expression is regulated by the transcription factor NRF2, which acts as a cellular master switch in controlling expression of a plethora of oxidative stress response genes. Its activity is controlled by KEAP1, which binds to NRF2 and retains it in the cytosol, inducing its degradation via ubiquitylation. Upon oxidation or nitrosylation of specific thiol residues, KEAP1 releases NRF2 to the nucleus, where it induces expression of antioxidant and detoxifying genes, such as heme oxygenase, GSTs, and GPx2 [121]. It is important to note that in addition to their direct role in redox regulation, GSH and TRx serve as trans-nitrosylation agents with functional consequences on several important biochemical signaling pathways [122]. Because GSH is the predominant pool of thiol groups in cells, it can serve as the initial pool of nitrosothiols (RSNO), which are then available for transnitrosylation to many other proteins and peptides [123]. For example, it was shown that GSNO is able to site-specifically transnitrosate TRx in a redox-controlled manner which is then able to catalyze caspase-3 nitrosation leading to inhibition of cell death [124–126]. With regard to NRF2 regulation, studies in the human colon cancer cell line HCT116 revealed that S-nitrosylation can have direct functional consequences to cellular mechanisms in response to oxidative stress by regulating NRF2 activity [34]. Thus, direct S-nitrosylation of KEAP1 may trigger nuclear translocation of NRF2, where it induces protective responses to counteract NO-induced damage to prevent CAC. (N.B.: As discussed below, this may contribute to the relative resistance of HCT116 cells to NO-induced cytotoxicity [34]). Support for such a hypothesis comes from several animal studies demonstrating that Nrf2−/− mice have an increased susceptibility to DSS-induced colitis and associated colon cancer. Specifically, increases in the severity of colitis and cancer incidence in Nrf2−/− mice were associated with repression of antioxidant/detoxifying genes and increased expression of mediators of inflammation such as iNOS, MPO, IL-1β, and TNFα as well as increased levels of nitrotyrosine staining [127–129]. Interestingly, Choi et al. showed that Nrf2 expression is modestly suppressed by oxidative stress during TNBS-induced colitis. NRF2 stimulation by sulforaphane significantly reduced DNA instability during inflammation, indicating that suppression of NRF2 by unknown mechanisms has functional consequences in CAC [57]. The finding that Nrf2 is suppressed during colitis may also account for the down-regulation of some antioxidant and detoxifying genes in H. hepaticus-induced murine colitis [27]. Significantly, an epidemiological study suggested that a promoter polymorphism in the human Nrf2 gene is associated with ulcerative colitis in a Japanese population [130].
In summary, these results provide a potential foundation for development of pharmacological intervention to treat IBD. Several mouse studies with antioxidant compounds have shown promising results, while clinical trials with these compounds largely proved to be negative because of adverse effects, non-specific drug distribution, and low retention in the colon [131–133]. A recent report addressed the pharmacokinetic and pharmacodynamic problems encountered in previous studies by using NO-containing nanoparticles that exhibit antioxidant properties. These particles showed improved accumulation and retention in the colonic mucosa and less up-take into the blood circulation compared to the low-molecular weight analogue TEMPOL. Subsequently, therapeutic effects were significantly improved in a mouse model of DSS-induced colitis, suggesting that this type of treatment could offer a useful perspective for human therapy [134].
3 Genotoxicology of ROS and RNS during inflammatory bowel disease
Many of the chemical mediators of inflammation are thought to act as anti-microbial factors or signaling molecules, depending on their source and local concentration. In particular oxidative and nitrative modification of proteins and changes in the cellular oxidative state are thought to fulfill various signaling functions that lead to diverse biological outcomes, such as cell proliferation, cell cycle regulation, and induction of senescence and apoptosis. On the other hand, these reactive chemical species can damage all classes of cellular biomolecules, including DNA, by both direct and indirect mechanisms, which elicit mutagenic and cytotoxic effects. In the following section, we provide an overview of the genetic toxicology of inflammation-related chemical species during colitis. We begin with an overview on RNS-related cytotoxicity studies, and then examine more closely genotoxicological mechanisms involved in murine colitis and human IBD. Finally, we discuss the regulation of DNA repair mechanisms during colitis and summarize work providing evidence that non-repaired, persistent damage products contribute to genomic mutations that initiate and promote CAC.
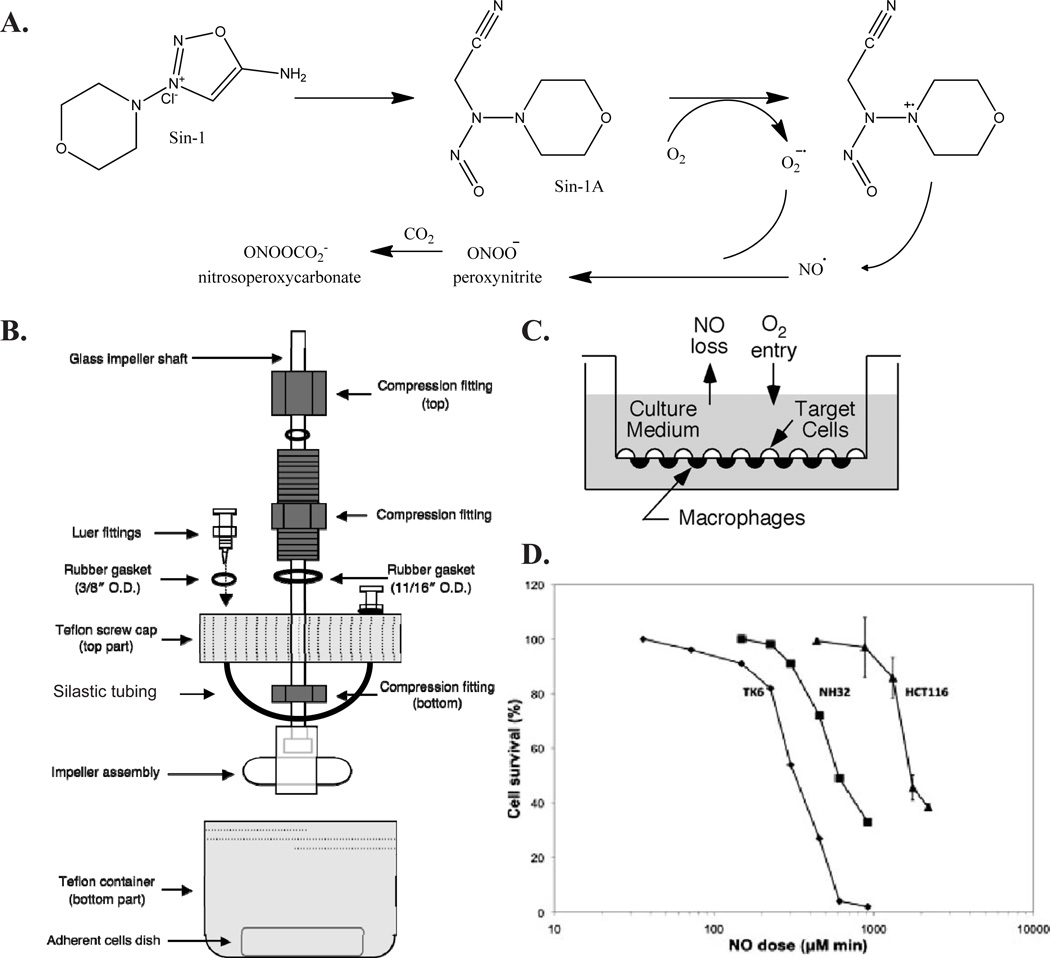
CytotoxicityApplication of precise and biologically relevant concentrations of NO and its derivatives is essential to mimic the biological environment and to study the physiological and cytotoxic functions of these chemical species. In general, NO can be delivered to cells via three approaches: NO donor compounds, such as NONOates, NO gas, or NO produced by activated macrophages [135] (Figure 4 A–C). The most rigorous conditions are achieved by using of NO and O2-permeable polydimethylsiloxande (Silastic) tubing to deliver gases at constant and predictable rates. These delivery systems are specifically designed and optimized to provide controlled, steady state concentrations of NO, O2, and NO2, thereby mimicking the chemical environment thought to exist in inflamed tissues [136–140].The range of estimated concentrations of NO in inflamed tissue, as obtained by mathematical modeling (Figure 3), are in reasonable agreement with those found to be cytotoxic in studies applying NO and O2 via Silastic tubing to cell culture media (Figure 4 D). For example, the minimum NO dose that was associated with cytotoxicity in TK6 human lymphoblastoid cells was ~150 µM min [141]. Interestingly, TK6-isogenic cells that lack p53 (NH32 cells) [141] and cells derived from colonic origin (HCT116 cells) [34,139] were more resistant, displaying threshold doses of 300 µM min and 1000–1600 µM min, respectively (Figure 4 D). These findings may be related to the importance of p53-dependent apoptosis in cytotoxic mechanisms (see below) and to the activation of the NRF2-KEAP1 signaling pathway to mitigate NO-mediated damage (see above), respectively. NO production in macrophages stimulated by LPS and IFN-γ resulting in growth inhibition and impaired cell viability, which could be attenuated by addition of the NOS inhibitor, NMA [142]. Moreover, co-culture of TK6 cells with stimulated macrophages also resulted in a substantial decrease in cell viability, both in the macrophages and the TK6 cells. Again, application of NMA reduced cytotoxicity in both cell types, which verifies the role of NO in the induction of these responses [143].
Figure 4. Examples of NO delivery systems for cell culture studies and cytotoxic profiles of different cell lines.
A. Sin-1 is used as a chemical donor of NO and ONOO−. B. Delivery via NO and O2-permeable polydimethylsiloxande (Silastic) tubing enables controlled exposure of an adherent target cell line to NO/O2. Shown is a schematic of a typical delivery apparatus. C. Co-cultivation of a target cell line with activated macrophages. D. Cell viability in TK6 and NH32 cells at 48 h and HCT116 cells at 24 h after exposure to NO and O2 or argon. Reprinted from [139] and [241] (with permissions of Elsevier and ACS).
These results provide strong evidence that local NO concentrations, as they exist in the vicinity of activated immune cells, can reach pathophysiological and cytotoxic levels in vivo. Mechanistic studies revealed that NO-mediated cytotoxicity is an extremely complex process involving several cell death pathways, including apoptosis and necrosis, depending on the cell type studied. Potential mechanisms include energy depletion upon acotinase inhibition, lipid peroxidation and protein modification through nitrotyrosine formation [144]. However, the earliest cellular effects observed include the inhibition of DNA synthesis, most likely as a result of DNA damage, leading to cell cycle arrest and apoptosis induction [145]. Most of the cells, however, will experience sub-toxic doses of ROS and RNS, causing macromolecular damage. As discussed in the following sections if such damage occurs in DNA, this may lead to mutational events driving tumor initiation and progression.
3.1 DNA damage during inflammatory bowel disease
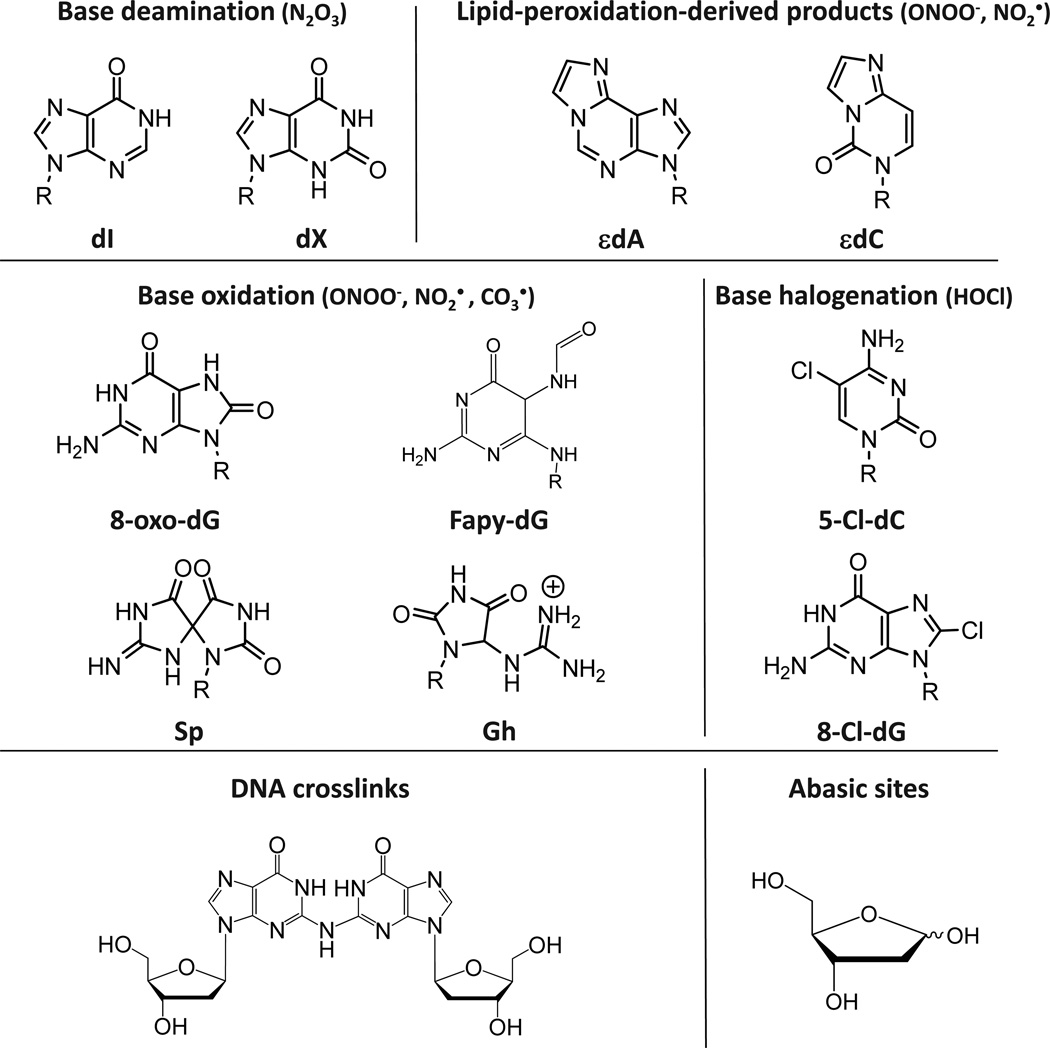
ROS and RNS-mediated DNA damage products span a wide range of reactions, including nitrosation, nitration, oxidation, and halogenation reactions (Figure 5), which are discussed in the following with a special emphasis on studies analyzing murine and human colitis. For a more general overview of the chemical biology of oxidative and nitrosative DNA damage the reader is referred to more specific reviews on this topic [146,147].
Figure 5. Overview of DNA damage products that are related to colitis-associated carcinogenesis.
For details see text.
3.1.1 Nitrosative deamination
N2O3 which is thought to be the primary agent causing nitrosative deamination of DNA. Other mechanisms include spontaneous hydrolysis and enzymatic processes by deaminases. DNA damage products formed by nitrosative deamination include 2’-deoxy-uridine (dU) derived from cytosine, 2’-deoxy-inosine (dI) derived from adenine, 2’-deoxy-xanthosine (dX) or 2’-deoxyoxanosine (dO) derived from guanine, and 2’-deoxythymidine (dT) derived from methylcytosine [69,148] (Figure 5). Due to their mutagenic potential, formation of these damage products is of high functional relevance. For example, during replication formation of deamination products mainly cause single-base transition mutations such as A:T to G:C (dI), C:G to T:A (dU), and G:C to A:T transitions (dX). In addition to deamination of exocyclic amines, nitrosation of heterocyclic nitrogens such as N7 or N3 in dA and N7 in dG can induce depurination creating abasic sites [149]. In an attempt to define the spectrum of nitrosative DNA lesions induced by RNS, purified DNA was exposed to NO (1.3 µM) and O2 (190 µM) [149]. Subsequent quantification of several DNA adducts by stable isotope-dilution mass spectrometry revealed that dX, dI and dU were formed at nearly identical rates to the extent of ~80 lesions per 106 nt after 12 h exposure to NO. Furthermore, abasic sites were generated at a rate of ~10 per 106 nt after 12 h of exposure to NO. In combination with other studies, which demonstrated that nitrosative guanine deamination can lead to the formation of interstrand cross-links (see below) [150], it can be estimated that under these conditions the following spectrum of nitrosative DNA damage occurs: 25–35% each of dX, dI, and dU, 4–6% abasic sites and ~2% dG-dG cross-links [149]. In cell culture, a ~4-fold protective effect by the cellular environment was observed against the formation of dX, dI and dU. Notably, significant elevations of these products of ~4-fold were only observed when cells were exposed to cytotoxic doses of NO and N2O3 (i.e., 1.75 µM NO and 186 µM O2 for >12 h) [135,151]. An earlier study detected a similar increase in dX levels of about ~6-fold using stimulated macrophages [152]. The slightly higher values obtained in the latter study may be related to the possibility that intracellular NO levels in stimulated macrophages as used in the study by Dong and Dedon may exceed local concentrations of 1–2 µM [135,152]. In vivo, recent results obtained from H. hepaticus-infected Rag2−/− mice revealed a small increase in levels of dI in inflamed colon tissue by 26%, whereas similar levels of dX were observed in colitis-affected and control tissue [27].
Taken together, these results indicate that nitrosative deamination products arise in cells and tissues under conditions of inflammation, but the relatively small increases suggest either limited nitrosative chemistry in nuclear DNA or effective protection and repair mechanisms, both in cell culture models and in the mouse [27,135]. That this holds true for the human situation awaits further study.
3.1.2 DNA oxidation
DNA can also be directly damaged by nucleobase oxidation by ONOO− and ONOOCO2−derived oxidants such as OH•, NO2•, and CO3•− [148]. While ONOO− itself, mainly causes 2-deoxyribose oxidation (i.e., strand breaks) and some base oxidation, ONOOCO2− causes mainly base oxidation [153]. Due to its low reduction potential, guanine represents the most vulnerable nucleobase, which shows DNA sequence- and agent-specific variations in damage chemistry [147,154–156]. Consequently, in vitro experiments demonstrated significant reactivity of ONOO− only with dG, leading to the formation of two major oxidation products, i.e., 8-oxo-7,8-dihydro-2’-deoxy-guanosine (8-oxo-dG) and 8-nitro-dG [147,157] (Figure 5). Apart from iNOS- and NADPH oxidase-dependent generation of ROS and RNS, which is thought to occur mainly in macrophages, nitration and oxidation of dG can be also be induced by neutrophils via MPO-dependent reactions that generate NO2• [158,159]. 8-oxo-dG and 8-nitro-dG are significantly more reactive with ONOO− than dG itself, however 8-nitro-dG is not stable and depurinates to 8-nitro-G generating an abasic site in the DNA backbone (t1/2 ~ 1 h at 37°C), which can cause base substitutions such as G → T transversions [147,157]. In contrast, 8-oxo-dG is more stable than 8-nitro-dG, but exhibits a ~1,000-fold higher reactivity than dG and gives rise to more than 10 different secondary oxidation products [153]. It is important nonetheless to keep in mind that even a 1000-fold difference in the reactivity of dG and 8-oxo-dG means that dG is still the major target in cellular DNA when 8-oxo-dG is present at steady state levels of 1–10 per 106 nucleotides [151,154]. Secondary dG oxidation products include spiroiminodiydantoin (Sp), guanidinohydantoin (Gh), and oxazalone (Ox), all of which have been extensively described in vitro [154,160–163]. In contrast to nitrosative DNA damage that mainly causes transition mutations, oxidative lesions tend to cause transversion mutations. While 8-oxo-dG itself can lead to C:G to A:T transversion mutations [164], secondary oxidation products such as Sp cause G:C to T:A and G:C to C:G transversions and can act as a strong inhibitor of DNA polymerase extension leading to replicative stress. Similarly, Gh lesions are also highly mutagenic causing G:C to C:G transversions, though they can be bypassed nearly as efficiently as 8-oxo-dG. For both secondary damage products, mutation frequencies are at least an order of magnitude higher than for 8-oxo-dG [165].
Because of their promutagenic potential, significant biological consequences are expected if such primary and secondary oxidation products are formed in mammalian DNA in vivo. While 8-oxo-dG is one of the most widely studied DNA damage lesions in vivo [166], data on the existence of guanine secondary oxidation products is not as abundant. Our recent LC-MS/MS-based study on a comprehensive set of inflammation-related DNA damage products in H. hepaticus-infected Rag2−/− mice aimed to detect guanine secondary oxidation products in mammalian tissues. In fact, Sp and Gh were detected in mouse liver and colon at absolute levels of ~1–5 lesions per 108 nucleotides, which are ~100 times lower than those of 8-oxo-dG. Interestingly, levels of Sp and Gh displayed tissue-specific differences and correlated strongly with their parent molecule 8-oxo-dG, indicating that these molecules indeed arise from 8-oxo-dG in vivo. In this study, no strong influence of colitis induction on whole tissue levels of 8-oxo-dG and its secondary oxidation products was observed. Thus, while 8-oxo-dG levels showed a slight and transient decrease during colitis development, levels of Sp tended to correlate positively with corresponding colonic histopathology indices, suggesting that these lesions may have biological significance during inflammation [27]. Similarly, Shaked et al. found modestly elevated levels of oxidative DNA damage lesions, such as 8,5′-cyclo-2′-deoxyadenosine (cdA) and 8,5′-cyclo-2′-deoxyguanosine (cdG), in intestinal epithelium in a mouse model with constitutive induction of iNOS expression measured by LC-MS/MS analysis (see above) [32]. It is important to stress that these studies analyzed lesion frequencies in tissue samples. Therefore, even small changes as detected in these studies may be related to more drastic effects on a single cell level. Although immuno-chemical methods of DNA damage detection based on DNA-damage-specific antibody binding have their limitations such as lack of chemical specificity and high background signals, these methods allow assessment of DNA damage on a single cell level. In this respect an analysis of an immunological colitis model detected elevated immuno-reactivity towards 8-oxo-dG and 8-nitro-G in nuclei of epithelial cells. These levels correlated with iNOS expression, suggesting a functional interplay between those factors [167]. Furthermore, stronger 8-oxo-dG immuno-reactivity was also detected in colonic epithelia of DSS-treated mice - an effect that could be almost completely suppressed by ectopic expression of extracellular SOD, which also considerably improved disease severity [61]. Interestingly, systemic effects of oxidative DNA damage were identified in mouse models of DSS-induced and immune mediated colitis using Il-10−/− mice: circulating blood leukocytes isolated from diseased mice showed significantly increased 8-oxo-dG immuno-reactivity, which correlated to oxidative damage detected in inflamed tissue [168]. Such systemic effecs may be related to activation of circulating innate immune cells and other factors or through the effect of circulating cytokines and acute phase proteins that autonomously induce oxidative stress in circulating peripheral cells [168].
There is also considerable evidence for the formation of oxidative damage during human IBD. For example, using the reduced-thiol-specific probe 14C-iodoacetamide (IAM), McKenzie et al. examined the thiol redox status as an indicator of oxidative protein damage and detected increased levels of oxidated thiol groups in colon epithelial crypt cells from IBD patients [169]. Furthermore, higher levels of 8-oxo-dG were detected in colorectal tumor tissue [114] and in inflamed tissues and tumors from patients with ulcerative colitis [170]. However, results from the latter study must be interpreted with caution, since it reported absolute values of >1 lesion/104 bp, which is at least two orders of magnitude higher than widely established basal levels and raises the possibility of adventitious oxidation during sample manipulation [170]. Interestingly, genomic hot-spots of oxidative DNA damage seem to exist, which is evident by the findings that p53 and TGF-β genes in H. pylori-infected individuals showed higher levels of oxidative damage than BAX and β-ACTIN, as analyzed by an OGG1-based PCR method [171]. The basis for this observation awaits further clarification, but may include sequence-specific events, the transcriptional or replicative state of the gene locus, the nature of the damaging agent, or the type of DNA lesion [171].
In summary, a large body of evidence demonstrates that oxidative damage to DNA plays an important role during CAC, but so far the exact mechanisms are poorly understood. Another level of complexity is added by the recent finding that oxidatively-induced DNA damage may also interfere with epigenetic mechanisms that contribute to CAC. In this respect, O’Hagan et al. reported that, in cells treated with H2O2 and in a mouse model of acute colitis, oxidative stress causes enrichment of members of the silencing complex including DNMT1 at promoter CpG islands, which may be related to a role of DNMT1 in DNA repair. This may result in epigenetic alterations in affected cells [172].
3.1.3 Lipid peroxidation-induced damage
Apart from direct oxidative damage, DNA nucleobases can be damaged by oxidation products arising from lipid peroxidation of polyunsaturated fatty acids. For example, peroxidation of linoleic acid gives rise to several α,β-unsaturated aldehydes, such as trans-4-hydroxy-2-nonenal (4-HNE), acrolein, and malondialdehyde (MDA), which can react with nucleobases to form exocyclic etheno adducts, such as 1-N6-2’-deoxy-ethenoadenosine (εdA) and 3-N4-2’-deoxy-ethenocytidine (3-N4-εdC), glyoxal adducts, and a series of other adducts [69,135] (Figure 5). Several repair mechanisms exist that act on lipid peroxidation products, including base excision repair, direct reversal by AlkB family proteins, nucleotide excision repair and homologous recombination (see below) [173]. If persistent, lipid peroxidation adducts exhibit strong promutagenic potential causing transversion and transition mutations, depending on the nature of the adduct. Additonally, lipid peroxidation adducts can interfere with DNA replication and gene transcription, thereby contributing to cytotoxicity.
Elevated levels of these adducts were identified in several inflammatory conditions. Strong evidence for sustained formation of lipid peroxidation adducts comes from the SJL mouse model of NO overproduction, in which RcsX-tumor bearing SJL mice develop severe inflammation in the spleen and liver. Increased levels of DNA etheno adducts were not only observed in liver and spleen, but also in kidney, which again points to systemic effects, since the kidney is not considered a primary target of inflammation in this model [174]. Increases in etheno adducts were also observed in DSS-induced colitis in mice [175] and in tissues from patients with Crohn’s disease and ulcerative colitis [173,176–178]. Increased levels of 4-HNE and MDA have been detected in biopsies from colorectal cancers, and were associated with dysregulation of antioxidant factors such as GPx1–3, SOD1, and GSH. This illustrates the pleiotropic cellular consequences of conditions of oxidative stress [114]. In addition to iNOS-dependent initiation of lipid peroxidation, this process may be also driven by MPO, as evident from the finding that Mpo−/− mice generated less lipid peroxidation intermediates compared to wild-type mice in a peritonitis model [179]. H2O2 may also play a significant role in the initiation of the lipid peroxidation cascade during colitis, since DSS-treated mice with ectopic expression of EC-SOD displayed lower levels of MDA compared to untreated controls as evaluated by immunohistochemical staining of mucosal epithelial cells [61].
Paradoxically, several studies reported decreased levels of lipid peroxidation products in the course of inflammatory diseases. For example, Godschalk et al. detected decreased levels of lipid peroxidation-induced DNA damage in the onset of atherogenesis in apolipoprotein E deficient mice [180]. These results are similar to those in H. hepaticus-induced colitis, which revealed transiently reduced levels of DNA-etheno adducts in the course of the disease. The finding that levels in RNA remained unaffected suggests that either DNA repair or protective effects of the nuclear environment underlie the transient decrease in etheno adducts, rather than changes in the cellular radical load. Inconsistent results were also obtained in human studies, in which lower levels of etheno adducts were detected in peripheral blood lymphocytes from patients with colorectal cancer. In this study, mRNA levels of some repair enzymes (i.e., glycosylases and APE1) were higher in peripheral blood lymphocytes of colon cancer patients than those of controls, but did not lead to higher excision rates of etheno adducts. In contrast, in target colon tissues, excision rates of etheno-adducts were higher compared to control tissue, while levels of DNA etheno adducts were lower in tumors than in non-tumorigenic tissue, pointing to complex local and time-dependent changes in adduct levels during disease development [181].
In summary, alterations in lipid peroxidation adducts have been reported in several mouse models of colitis as well as in human disease, however these changes exhibit a dynamic nature and are highly dependent on the model and condition analyzed. The molecular bases for these inconsistencies remain unclear, but may be related to dynamic regulation of the repair efficiencies of these adducts.
3.1.4 Halogenation-induced damage
The reaction of nucleobases with MPO-derived HOCl leads to the formation of products such as 5-chloro-2’-deoxy-cytidine (5-Cl-dC), 5-chloro-2’-deoxy-uridine (5-Cl-dU), as a deamination product of 5-Cl-dC, 8-chloro-2’-deoxy-guanine (8-Cl-dG), as well as dihalogenated nucleobases (Figure 5). All of these molecules have been detected in cellular RNA as well as in murine and human DNA under inflammatory conditions, such as sepsis and atherosclerosis, and were therefore proposed as potential biomarkers of inflammatory diseases [182–189]. Of note, following LPS treatment, 8-Cl-dG was only observed in the liver of wild-type but not of Mpo−/− mice, which indicates that in vivo formation of halogenation damage predominantly depends on this enzyme [182]. Repair mechanisms for these adducts are poorly characterized, but potentially rely on base excision repair (BER), since free base adducts, such as 8-Cl-dG, were detected in urine of LPS-treated rats [182]. In particular, 5-Cl-dC appears to be of biological relevance, since it mimics 5-methylcytosine and thereby enhances binding of the binding domain of methyl-CpG-binding protein 2 (MeCP2) and serves as a substrate for DNMT1 [190,191]. It is plausible that, within a CpG sequence context, this results in heritable, reversible gene silencing, with altered cytosine methylation patterns providing a potential link between inflammation, epigenetic changes, and tumor initiation [192]. CpG hypermethylation has been associated with CAC revealing high methylation frequencies in several genes, including the tumor suppressor p16 (see below) [193]. Hypermethylation was also present in non-dysplastic, normal-appearing epithelium from patients with ulcerative colitis, but not from control individuals, indicating that methylation precedes dysplasia [193]. In this context, it is interesting to note that a polymorphism in the MPO gene (G463A) associated with reduced MPO mRNA expression reduces the risk for lung cancer development [194–196]. Regarding formation of chlorination adducts during murine colitis, our recent studies in H. hepaticus-infected Rag2−/− mice demonstrated significantly elevated levels of adducts in DNA (5-Cl-dC) and RNA (5-Cl-rC) in colitis-affected mice [27]. While increases in DNA and RNA were modest (~25%), more drastic changes were observed on the protein level, with 3-Cl-Tyr levels below the limit of detection in control mice, but clearly detectable in all H. hepaticus-infected mice at 20 weeks post infection [29]. These results indicate that either proteins are more accessible to damage induction and/or damaged nucleic acids are less stable (RNA) or efficiently repaired (DNA). Nevertheless, it is important to note that mild increases in damage levels in whole colonic DNA may correspond to drastic changes on a single cell level, potentially contributing to cellular transformation and colon cancer development in H. hepaticus-infected Rag2−/− mice. In this context, it would be interesting to determine whether changes in methylation patterns are generated in colitis induced in Mpo−/− mice. We recently detected 5-Cl-dC in colon biopsies from IBD patients, levels of which were in the same range of those found in Rag2−/− mice [29], but have not yet analyzed in non-inflamed tissues from unaffected individuals for comparison.
3.1.5 Crosslinks, double strand breaks and chromosomal aberrations
Apart from small base lesions, inflammation-induced reactive chemical species can also cause more complex DNA adducts, such as crosslinks, and genomic aberrations, such as strand breaks and chromosomal rearrangements (Figure 5). Crosslinks can arise as by-products of lipid-peroxidation, such as acrolein and crotonaldehyde R, β-unsaturated aldehydes [197–199], but were also observed in an in vitro system using an oligonucleotide treated with NO. In the latter system, the proportion of crosslinks reached levels up to 6% of the amount of deamination products [200]. Such levels may be of pathophysiological significance, since DNA crosslinks are potently toxic lesions; this is the mode of action of many highly toxic cancer chemotherapeutic agents. Special interstrand crosslink repair mechanisms exist that function at the interface of nucleotide excision repair and homologous recombination and are promoted by Fanconi anemia-related genes [199]. If not repaired, DNA crosslinks may interfere with the transcriptional and replication machinery as well as with chromosomal segregation, thereby potentially supporting genetic instability and tumor development. Not only DNA intra- and interstrand crosslinks may be of toxicological relevance, but also DNA-protein crosslinks are expected to have a major impact on genetic stability and gene transcription [199]. Other types of damage that affect the integrity of DNA include strand breaks potentially causing chromosomal rearrangements and aberrations. Double strand breaks (DSB) were detected upon NO delivery to cells in culture, even at sublethal doses when other types of damage products, such as deamination products, were not yet obvious, suggesting that those may be also useful markers in vivo. Substantial evidence has demonstrated that NO-induced DSB arise mainly through enzymatic processes during the repair of primary DNA lesions, since neither N2O3 nor ONOO− are able to cause DSB by direct reaction with DNA. Thus, a likely scenario includes that primary base lesions or abasic sites are repaired by BER during which single strand breaks (SSB) are introduced that may convert to DSB when occurring in close proximity to each other or when the replication fork approaches the SSB during DNA replication [136,201]. Li et al. reported that the formation of DSB was accompanied by increased frequencies of sister chromatid exchanges (SCE), which represent major chromosomal aberrations associated with cell transformation [136]. SCE are caused by chromosomal rearrangements occurring during homologous recombination in an attempt to repair DSB. It was found that ONOO−, but not N2O3, acts as a potent inducer of HR [202]. This is in line with the fact that N2O3 is a potent DNA deaminating agent, whereas ONOO− is a potent DNA oxidizing agent that acts mainly on DNA bases and sugar moieties. Consequently, it was shown that oxidatively-induced DNA damage exhibit a higher recombinogenic potential than nitrosative deamination damage [202]. This was interpreted to be due to the fact that DNA oxidation produces recombinogenic strand breaks by both direct attack on the sugar-phosphate backbone and indirectly during BER repair of oxidized bases, while nitrosative damage does not involve strand breaks [202]. As a consequence, such recombinogenic processes can lead to sequence rearrangements that can drive carcinogenesis during inflammation.
Support for a potential role of strand breaks during CAC in vivo comes from a study analyzing TNBS-induced colitis in rats [57]. Using a PCR approach, Choi et al. demonstrated that strand breaks were introduced in specific sequences of gene promoter regions. This was accompanied by increased phosphorylation of the histone variant H2A.X, which is considered a marker for the DSB response, in colonic smooth muscle cells [57]. These findings are consistent with gene expression studies in H. hepaticus-infected Rag2−/− mice, which revealed a robust up-regulation of the DNA-damage-signaling and senescence marker Cdkna2 (p16) pointing to the induction of DSB in inflamed tissue of infection-induced murine colitis [27]. Usually p16 is up-regulated in premalignant lesions as a mechanism to suppress tumor development and expression is subsequently lost in invasive colon carcinomas by Cdkn2a hypermethylation both in spontaneous colorectal cancer and in CAC (see below) [203–206]. As observed for other damage products, DNA strand breaks and gross chromosomal aberrations were also observed in peripheral blood cells as well as in other extra-intestinal tissues, such as lymphoid organs and liver, in chemical and immune-mediated mouse models of colitis with damage levels correlating with disease severity [168,207]. This is in line with results from H. hepaticus-infected Rag2−/− mice showing strong p16 induction, not only in the colon, but also in liver tissue [27]. Whether this is of any significance with regard to cancer development in tissues other than intestine needs to be evaluated, but results from H. hepaticus-infected Rag2−/− mice point to a transient induction of hepatitis presumably as a consequence of colitis development.
Systemic effects of colitis on genetic instability were also observed in human patients. Significantly higher SCE levels were reported in peripheral blood lymphocytes from patients with Crohn’s disease compared to control subjects, and a significant positive correlation exists between SCE levels and disease severity [208]. Human studies also revealed multiple lines of evidence for a casual relationship between genetic instability and colon cancer development. Rabinovitch et al. showed that chromosomal instability is present throughout the colon of patients with ulcerative colitis and high grade dysplasia or cancer [209]. More importantly, chromosomal abnormalities affected the entire colon and were even present in non-dysplastic biopsies. Analysis of chromosomal instability was sufficient to fully differentiate these ulcerative colitis biopsies from control biopsies. However, further studies are needed to assess whether these markers of genomic instability will serve as prospective indicators of cancer risk in IBD [210]. Follow-up studies revealed that chromosomal abnormalities are at least in part related to telomere shortening [210–212]. This result is consistent with the findings that oxidative stress leads to greatly accelerated telomere attrition [213]. In particular, it was shown that telomeres shorten with age almost twice as rapidly in patients with ulcerative colitis as in normal controls with extensive telomere shortening occurring within the first 8 years of disease duration [212]. In addition, epithelial cells from colon biopsies from patients with active ulcerative colitis revealed increased phosphorylation of H2A.X and higher frequencies of anaphase bridges, which are associated with non-resolved chromosomes during mitosis [210,212]. Anaphase bridges are a hallmark of telomere dysfunction and can lead to gross chromosomal rearrangements, including chromosome losses and gains. Since genetic instability precedes cancer formation, this may contribute to a mutator and genetic instability phenotype, as it is characteristic for neoplastic progression in general. The finding that genomic instability affected the entire colon of patients with ulcerative colitis is consistent with the multifocal occurrence of tumor development under these conditions. A recent study in patients with ulcerative colitis correlated factors of inflammation, genetic instability and cellular senescence, revealing that high levels of infiltrating leukocytes were associated with increased telomere shortening, DNA damage (γ-H2A.X), and cellular senescence. This provides important evidence that senescence acts as a tumor suppressor mechanism that is abrogated during the transition from low grade to high grade dysplastic tissue [211].
Thus, these studies suggest that colitis-associated colon cancer arises in a preneoplastic environment of inflammation-driven genetic instability, apoptosis, and cellular senescence.
3.2 DNA repair and DNA damage response
To assess the functional relevance of DNA damage during colitis with respect to disease and cancer development, a useful approach is to interfere with mechanisms that repair such lesions. Several studies have addressed this issue and impressively demonstrated the functional role of multiple repair mechanisms, including mismatch repair, base excision repair, dealkylation repair, and general DNA damage response in the maintenance of colonic homeostasis and prevention of CAC.
DNA mismatch repair (MMR) is a repair mechanism active when replication errors occur, but also when damaged bases mispair with their counterparts. One of the most important proteins in MMR is MSH2, which participates in damage recognition as part of the MutSα and MutSβ complex. When Msh2−/− mice were subjected to chronic DSS-induced colitis, they developed a ~4-fold higher frequency of high-grade dysplasia and a 2-fold higher susceptibility to the development of colon tumors than controls [214]. In contrast to wild-type mice, the majority of Msh2−/− mice developed tumors with a microsatellite instability phenotype, indicative of MMR defects. Of note, this instability appeared also in non-neoplastic tissue, presumably due to increased inflammation-induced cell proliferation [214]. Microsatellite instability was also found in patients with ulcerative colitis, in both tumor and in premalignant tissue that had no histological evidence of neoplastic change. Thus, in this setting microsatellite instability may reflect the inability of MMR to compensate for damage resulting from chronic inflammation, and may contribute to malignant cellular transformation and increased cancer risk in patients with ulcerative colitis [215]. However, as Kohonen-Corish et al. point out, although MMR predisposes to inflammation-induced tumor formation in mice, it is obviously not the only factor involved, since not only Msh2−/− but also ~30% of wild-type mice developed tumors [214]. Liao et al. showed that in Ogg1−/− mice, which lack the DNA glycosylase responsible for the excision of 8-oxo-dG as an initial step during BER, DSS-induced colitis leads to twice as many colorectal adenocarcinomas than observed in wild-type mice. This outcome was partially independent of potential differences in disease severity, since Ogg1−/− and wild-type mice exhibited similar numbers of infiltrating macrophages. Importantly, quantities of 8-oxo-dG were considerably increased in inflammatory and epithelial cells in Ogg1−/− mice [216].
Another DNA glycosylase involved in the removal of small base adducts, such as methylated bases, hypoxanthine and base ethenoadducts is alkyladenine DNA glycosylase (AAG, also known as MPG). Exposure of Aag−/− mice to DSS-induced colitis led to a higher accumulation of etheno adducts and oxidative base lesions in colonic DNA. This was accompanied by more pronounced colonic epithelial damage and higher cancer rates, indicating that AAG-mediated DNA repair contributes to tumor-protective mechanisms in DSS-induced colitis [175]. Impressively, when combined with genetic deletions of Alkbh2 and Alkbh3, which are also involved in the repair of DNA etheno adducts, the triple knock-out mice were unable to survive a single DSS application (administered alone or in combination with AOM), indicating that AAG, ALKBH2 and ALKBH3 are crucial to maintain colon homeostasis and whole-animal survival during acute inflammatory conditions. Triple knock-out mice also exhibited decreased histopathology scores, indicating that a functional DNA damage response is important to trigger full tissue inflammation. It is important to note that DSS itself does not induced DNA damage and that the observed effects can be attributed to tissue response mechanisms. This is evidenced by the finding that when triple knockout mice were exposed to alkylating agents such as AOM and MMS alone, this did not affect their ability to survive the stimulus, highlighting the importance of inflammatory mechanisms in the observed response. The observed sensitivity of the triple knock-out mice seems to be dependent on the nature of the inflammatory trigger and the organ affected, since they were also sensitive to LPS-induced sepsis, but showed similar responses as wild-type mice to cerulein, which induces pancreatitis. This may be related to the fact that DSS colitis and LPS-induced inflammation act through TLR-signaling, while cerulein induces pancreatitis via cholecystokinin receptor signaling [217]. Changes in BER were also observed in non-cancerous tissues from patients with ulcerative colitis. Hofseth et al reported that levels of AAG and APE1 were elevated in inflamed tissue and that this was positively correlated with microsatellite instability indicating that proper balance of repair enzyme activities is essential to maintain genomic stability [218]. Similarly, Mutamba et al. showed that overexpression of AAG rendered XRCC1-deficient cells sensitive to NO-induced DNA damage [219]. ROS and RNS dependent mechanisms may also lead to inactivation of DNA repair mechanisms, since our recent study in H. hepaticus- infected Rag2−/− mice revealed that inflamed colons showed globally lower expression levels of DNA repair factors [27]. Several other studies have also reported impairments in DNA repair mechanisms during inflammatory conditions [220–222]. Such changes may be caused by epigenetic silencing [221,222] or by direct inhibition via ROS and RNS-induced chemical modifications [223–227]. Furthermore, ROS and RNS-independent mechanisms may also contribute to changes in the expression levels of DNA repair factors. Kim et al. demonstrated that exposure of gastric cancer cell lines to co-culture with extracts of H. pylori led to decreased levels of MutS and MutL DNA MMR proteins in a dose-dependent manner. Reduction in MMR protein levels was caused by heat-sensitive H. pylori products, but the nature of these products is not known [228].
Apart from DNA repair, DNA damage signaling also contributes to the stress response during colitis. For example, Atm−/− mice exhibit an increased sensitivity to DSS-induced colitis that was associated with elevated DNA damage levels and persistent immune activation [229]. Further, these mice displayed higher levels of tissue damage, up-regulation of pro-inflammatory cytokines, and increased levels of 8-oxo-dG, again indicating a positive feedback mechanism of DNA damage, signaling and inflammatory response [229]. Cell culture experiments demonstrated that NO activates ATM (and ATR) signaling which triggered the activation of downstream targets such as p53. This can lead to p53 stabilization and its nuclear accumulation, where it regulates DNA repair, cell cycle progression and cell survival/death [230]. Such DNA damage response signaling was also identified in non-cancerous tissue from patients with ulcerative colitis, showing that iNOS gene expression positively correlates with p53 serine 15 phosphorylation levels and activation of p53-dependent downstream targets such as p21 [230]. Consistent with its general role as a master switch in tumor suppressive mechanisms, p53−/− mice are prone to tumor development in a model of DSS-induced colitis [231], indicating that inactivation of p53 acts as a common mechanism of malignant transformation in CAC [232–237]. Such an inactivation of p53 and other tumor suppressors as well as activation of oncogenes can arise through DNA damage-dependent base mispairing and generation of loss-of-function as well as gain-of-function mutations leading to cellular transformation.
In the next section we will summarize initial attempts to link the formation of DNA damage products to the occurrence of genetic mutations that initiate and drive carcinogenesis.
3.3 Mutagenicity
Several studies focused on the conversion of ROS and RNS-mediated DNA damage into gene mutations thought to be a prerequisite for malignant transformation of cells [136,141,238–240]. A recent study demonstrated that when cells were exposed to NO delivered by Silastic tubing into the medium, this resulted in about 5-fold higher mutation frequencies in several cell types (TK6, AS52) at different genetic loci (HPRT, TK1) [241]. When Chinese hamster ovary (CHO) AS52 cells that carry a single genomic copy of the E. coli xanthine-guanine phosphoribosyltransferase (gpt) as a reporter gene were exposed to activated macrophages, the mutation frequency in the genetic target cell was enhanced by more than 9-fold compared to background levels. Application of the NOS inhibitor NMA and the O2•− scavenger Tiron, completely prevented this response, indicating the importance of NO• in the induction of these mutations. In an attempt to identify mutational fingerprints indicative of the spectrum of reactive chemical species, sequencing studies revealed that base substitutions dominate the mutation spectra, with transversion mutations (30–40%) being more prevalent than transition mutations (10–20%). Deletion mutations occurred at a lower frequency in mutants exposed to activated macrophages (20%) than in spontaneous mutants (~50%). These results suggest that small base-damage adducts, as induced by oxidation and nitrosative deamination, rather than erroneous repaired DSB cause increased mutation frequencies under these conditions. Almost all mutations occurred at guanine sites leading to G:C to T:A transversions (~30%) and G:C to A:T transitions (10–20%). Notably, this led to functional consequences as the frequency of gene inactivation doubled in cells exposed to gaseous NO• or to activated macrophages affecting 40% of induced mutants vs 20% of spontaneous mutants.
These results are consistent with those obtained from in vivo studies analyzing gastric tissue of gpt δ mice infected with H. pylori [242]. These mice harbor tandem arrays of 80 copies of the gpt reporter gene at a single genetic locus on chromosome 17. Mutation frequencies were significantly higher in H. pylori-infected female mice, which displayed a mutation spectrum consistent with the expected spectrum induced by ROS and RNS: ~4 times more A:T to G:C transitions and ~2 times more G:C to T:A transversions than in uninfected controls. Similarly to the in vitro model, no increase in the frequency of deletions was observed. A notable difference, however, was the higher frequency of A:T to G:C transitions in the H. pylori in vivo model, which may arise from deamination of adenine, mediated by N2O3 leading to hypoxanthine which mispairs with cytosine; or, alternatively through ROS and RNS-induced lipid peroxidation products leading to highly mutagenic ethenoadenine [241,242]. Similar results were obtained in a colitis model using Il-10−/− mice in combination with a transgenic gpt gene [243], in which the total mutation frequency in the colon of gpt+/Il-10−/− mice was ~5-times higher than in gpt+/Il-10+/+ control mice. Similarly to the H. pylori model, transition and transversion mutations dominated the mutation spectrum and were around ~4-fold higher in gpt+/Il-10−/− mice compared to controls. However, in contrast to the H. pylori model, the frequency of small deletions and insertions was also increased in inflamed tissue by ~10-fold, indicating organ- and disease-specific induction of mutation spectra which point to differences in the nature of reactive chemical species formed during inflammation [243]. Consistent with these results, similar mutation spectra were identified in APC and p53 tumor suppressor genes, and K-ras oncogenes dysplastic tissue of patients with ulcerative colitis [237,244,245]. These studies revealed a positive correlation between iNOS activity and increased frequencies in p53 transition mutations in colitis and colon cancer, suggesting that ROS and RNS are able to induce DNA damage products that can cause mutation in genes relevant for tumor development [237,245]. Concerning the cell-types which are at the highest risk to accumulate such mutations, computational models predict that stem cells near the base of the crypt are exposed to the highest concentrations of NO. In contrast to migrating epithelial cells, any oncogenic mutation in stem cells could accumulate over time, eventually leading to cellular transformation [72]. This is in accordance with experimental studies showing that crypt stem cells represent the cells-of-origin for colon cancer development [20].
Further studies will be required to define the exact spectrum of reactive chemical species that induce the observed mutational profiles. Mouse models with constitutive or tissue-specific deficiencies in genes that are responsible for the generation of reactive chemical species (e.g., iNos, Mpo, NADPH oxidases, etc.) represent a possible tool to answer this question.
3.4 Microbial-induced genotoxicity
In considering causative parameters of genotoxicity, the potential contribution of the gut microbiota, which harbor up to 100 trillion bacteria, needs to be taken into account [246]. While it is beyond the scope of this review to discuss the various contributions of gut bacteria during colonic inflammation (reviewed in [247]), some studies elucidating the role of the gut microbiota on genomic stability of host cells deserve mention. Many mouse models of colitis and inflammation-induced carcinogenesis rely on the presence of an active gut microbiome, since germ-free mice do not develop colitis nor do they show significantly increased tumor frequencies in several colon carcinogenesis models [247]. Further, imbalance of the gut microbiota, termed dysbiosis, is sufficient to induce colitis in specific mouse strains, as noted for the H. hepaticus-infection model. To date two mechanisms have been identified regarding microbiotic factors directly contributing to genotoxicity in host cells. Huycke et al. showed that the commensal microorganism, Enterococcus faecalis, produces substantial levels of extracellular O2-• and other ROS derivatives, through autooxidation of membrane-associated demethylmenaquinone and subsequent activation of host macrophages [248,249]. When mammalian cells and rats were colonized with O2-•-producing E. faecalis, significantly higher levels of DNA strand breaks were found than in control rats colonized with a mutant form, resulting in increased levels of chromosomal instability [250,251]. Some bacteria, including Helicobacter and pks+ E. coli produce genotoxins such as cytolethal distending toxin (CDT) and colibactin, respectively. These toxins cause DNA SSB that accumulate as DSB, enhance cellular mutation frequencies and genomic instability that may promote malignant transformation of host cells [252–255]. Two recent studies suggest that colonic inflammation leads to a shift of the microbial composition towards facultative anaerobic bacteria such as Enterobacteriaceae, including colibactin-generating E. coli [246,256,257]. Specifically, Winter et al. showed that iNOS-derived nitrate generated during inflammation conferred a growth advantage to E. coli by anaerobic nitrate respiration– an effect that was not observed in iNos−/− mice [246,257].
4 Conclusions
The studies discussed in this review demonstrate the critical role played by chemical mediators of inflammation in linking inflammation to colon cancer (Figure 2 and 6). Damage products covering the full spectrum of inflammation-related chemistries have been detected during colonic inflammation, notably in many cases at stages that clearly precede cancer formation (Figure 5). Consequently, some of these damage products may be included in a yet to be defined set of disease biomarkers to assess the individual status and cancer risk of IBD patients. Furthermore, mutational analyses and studies from DNA repair-deficient mice indicate that DNA damage products are of functional relevance in the etiology of CAC. Taken together, it is very likely that inflammation-related chemical species induce genetic and epigenetic alterations that affect molecular mechanisms involved in tumor initiation and progression during CAC (Figure 6).
Figure 6. Overview of mechanisms that may contribute to tumor initiation and promotion during colitis-associated carcinogenesis.
Modified from [27]; with permission of PNAS.
Despite the large body of evidence linking colonic inflammation to DNA damage and carcinogenesis, many of the studies rely on correlative data, with few mechanistic studies that evaluate the functional relevance of inflammation-induced DNA damage. In this respect, the question of the role of DNA modifications as cytotoxic products that drive replication-dependent mutagenesis or as directly mutagenic species in their own right remains to be answered. Moreover, the dynamics of genetic and epigenetic alterations and the role of repair pathways need to be defined in greater detail. In many respects, the holes in our knowledge result from limitations of current methods to map and quantify DNA lesions. That is, methods effective on a single cell level (e.g., antibodies) often lack chemical specificity, while methods of high chemical specificity (e.g., LC-MS/MS) are currently not sensitive enough to be used in single cell analyses. This motivates the development of methods capable of mapping sites of DNA damage genome-wide, ideally in a real-time, dynamic manner. Such methods could be employed to define the whole adductome of DNA lesions in a genome-wide manner and to determine the contribution of the individual types of damage to induce gene mutations in different types and stages of IBD. A first step in this direction has been taken recently in a proof-of-principle study by employing nanopore sequencing technology to detect guanine oxidation products in a DNA sequence context [258,259]. In addition, further progress in defining the mechanistic link between IBD and cancer will be made by large-scale sequencing analysis of genetic and epigenetic changes occurring during inflammation-induced carcinogenesis and by developing mouse models of constitutive or conditional deletions of enzymes involved in the generation of ROS and RNS, such as iNOS, NADPH oxidases, MPO, and XOR. With respect to the latter point, it is worth mentioning that, despite the finding that gene regulatory mechanisms during some inflammatory diseases show weak conservation between a specific mouse strain and humans [23], the data reviewed here demonstrate that this may not be the case for expression and activation of enzymes generating reactive chemical species, and in particular, not for the damage products that arise from these species. Indeed, many classes of macromolecular damage products arise during both murine colitis and human IBD (Table 2). Therefore, in addition to efforts to modulate immunological mechanisms to treat IBD [260], it is worth considering other factors as potential therapeutic targets, such bacterial genotoxins and enzymes producing or scavenging reactive chemical species. The fact that it usually takes decades from the onset of IBD to the first occurrence of neoplastic lesions opens a significant time window for therapeutic intervention to prevent tumor development. A detailed understanding of the chemical and biological mechanisms underlying the etiology of colitis associated carcinogenesis lays the foundation for the development of such strategies.
Acknowledgments
Declaration of interest
Our experimental work was supported by grants from the NIH (CA26731) and the MIT Center for Environmental Health Sciences (ES002109).
ABBREVIATIONS
- AOM
azoxymethane
- CAC
colitis-associated carcinogenesis
- GPx
gluthathione peroxidases
- GRx
glutaredoxins
- GSR
glutathione reductase
- IBD
inflammatory bowel disease
- iNOS
inducible nitric oxide synthase
- MPO
myeloperoxidase
- NOX
NADPH oxidase
- NOx
NO oxidation products
- RNS
reactive nitrogen species
- ROS
reactive oxygen species
- TNBS
2,4,6-trinitro benzene sulfonic acid
- TxnRD
thioredoxin reductases
- XOR
xanthine oxidoreductase
References
- 1.Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361(21):2066–2078. doi: 10.1056/NEJMra0804647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abraham C, Medzhitov R. Interactions between the host innate immune system and microbes in inflammatory bowel disease. Gastroenterology. 2011;140(6):1729–1737. doi: 10.1053/j.gastro.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474(7351):307–317. doi: 10.1038/nature10209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varol C, Zigmond E, Jung S. Securing the immune tightrope: mononuclear phagocytes in the intestinal lamina propria. Nat Rev Immunol. 2010;10(6):415–426. doi: 10.1038/nri2778. [DOI] [PubMed] [Google Scholar]
- 5.Garrett WS, Gordon JI, Glimcher LH. Homeostasis and inflammation in the intestine. Cell. 2010;140(6):859–870. doi: 10.1016/j.cell.2010.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maloy KJ, Powrie F. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature. 2011;474(7351):298–306. doi: 10.1038/nature10208. [DOI] [PubMed] [Google Scholar]
- 7.Terzic J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010;138(6):2101–2114. e5. doi: 10.1053/j.gastro.2010.01.058. [DOI] [PubMed] [Google Scholar]
- 8.Rubin DC, Shaker A, Levin MS. Chronic intestinal inflammation: inflammatory bowel disease and colitis-associated colon cancer. Front Immunol. 2012;3:107. doi: 10.3389/fimmu.2012.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jostins L, Ripke S, Weersma RK, Duerr RH, McGovern DP, Hui KY, Lee JC, Schumm LP, Sharma Y, Anderson CA, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491(7422):119–124. doi: 10.1038/nature11582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molodecky NA, Kaplan GG. Environmental risk factors for inflammatory bowel disease. Gastroenterol Hepatol (N Y) 2010;6(5):339–346. [PMC free article] [PubMed] [Google Scholar]
- 11.Dale DC, Boxer L, Liles WC. The phagocytes: neutrophils and monocytes. Blood. 2008;112(4):935–945. doi: 10.1182/blood-2007-12-077917. [DOI] [PubMed] [Google Scholar]
- 12.Nathan C. Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol. 2006;6(3):173–182. doi: 10.1038/nri1785. [DOI] [PubMed] [Google Scholar]
- 13.Weber B, Saurer L, Mueller C. Intestinal macrophages: differentiation and involvement in intestinal immunopathologies. Semin Immunopathol. 2009;31(2):171–184. doi: 10.1007/s00281-009-0156-5. [DOI] [PubMed] [Google Scholar]
- 14.Soehnlein O, Lindbom L. Phagocyte partnership during the onset and resolution of inflammation. Nat Rev Immunol. 2010;10(6):427–439. doi: 10.1038/nri2779. [DOI] [PubMed] [Google Scholar]
- 15.Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol. 2011;11(8):519–531. doi: 10.1038/nri3024. [DOI] [PubMed] [Google Scholar]
- 16.Cua DJ, Tato CM. Innate IL-17-producing cells: the sentinels of the immune system. Nat Rev Immunol. 2010;10(7):479–489. doi: 10.1038/nri2800. [DOI] [PubMed] [Google Scholar]
- 17.Strober W, Fuss IJ. Proinflammatory cytokines in the pathogenesis of inflammatory bowel diseases. Gastroenterology. 2011;140(6):1756–1767. doi: 10.1053/j.gastro.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ekbom A, Helmick C, Zack M, Adami HO. Increased risk of large-bowel cancer in Crohn's disease with colonic involvement. Lancet. 1990;336(8711):357–359. doi: 10.1016/0140-6736(90)91889-i. [DOI] [PubMed] [Google Scholar]
- 19.Ullman TA, Itzkowitz SH. Intestinal inflammation and cancer. Gastroenterology. 2011;140(6):1807–1816. doi: 10.1053/j.gastro.2011.01.057. [DOI] [PubMed] [Google Scholar]
- 20.Barker N, Ridgway RA, van Es JH, van de Wetering M, Begthel H, van den Born M, Danenberg E, Clarke AR, Sansom OJ, Clevers H. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457(7229):608–611. doi: 10.1038/nature07602. [DOI] [PubMed] [Google Scholar]
- 21.Schwitalla S, Fingerle AA, Cammareri P, Nebelsiek T, Goktuna SI, Ziegler PK, Canli O, Heijmans J, Huels DJ, Moreaux G, et al. Intestinal Tumorigenesis Initiated by Dedifferentiation and Acquisition of Stem-Cell-like Properties. Cell. 2012 doi: 10.1016/j.cell.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 22.Hussain SP, Hofseth LJ, Harris CC. Radical causes of cancer. Nat Rev Cancer. 2003;3(4):276–285. doi: 10.1038/nrc1046. [DOI] [PubMed] [Google Scholar]
- 23.Seok J, Warren HS, Cuenca AG, Mindrinos MN, Baker HV, Xu W, Richards DR, McDonald-Smith GP, Gao H, Hennessy L, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci U S A. 2013;110(9):3507–3512. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kolata G. Mice Fall Short as Test Subjects for Deadly Illnesses. The New York Times. 2013 [Google Scholar]
- 25.Erdman SE, Poutahidis T, Tomczak M, Rogers AB, Cormier K, Plank B, Horwitz BH, Fox JG. CD4+ CD25+ regulatory T lymphocytes inhibit microbially induced colon cancer in Rag2-deficient mice. Am J Pathol. 2003;162(2):691–702. doi: 10.1016/S0002-9440(10)63863-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Erdman SE, Rao VP, Poutahidis T, Rogers AB, Taylor CL, Jackson EA, Ge Z, Lee CW, Schauer DB, Wogan GN, et al. Nitric oxide and TNF-alpha trigger colonic inflammation and carcinogenesis in Helicobacter hepaticus-infected, Rag2-deficient mice. Proc Natl Acad Sci U S A. 2009;106(4):1027–1032. doi: 10.1073/pnas.0812347106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mangerich A, Knutson CG, Parry NM, Muthupalani S, Ye W, Prestwich E, Cui L, McFaline JL, Mobley M, Ge Z, et al. Infection-induced colitis in mice causes dynamic and tissue-specific changes in stress response and DNA damage leading to colon cancer. Proc Natl Acad Sci U S A. 2012;109(27):E1820–E1829. doi: 10.1073/pnas.1207829109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lu K, Knutson CG, Wishnok JS, Fox JG, Tannenbaum SR. Serum Metabolomics in a Helicobacter hepaticus Mouse Model of Inflammatory Bowel Disease Reveal Important Changes in the Microbiome, Serum Peptides, and Intermediary Metabolism. J Proteome Res. 2012;11(10):4916–4926. doi: 10.1021/pr300429x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knutson CG, Mangerich A, Zeng Y, Raczynski AR, Liberman RG, Kang P, Ye W, Prestwich E, Lu K, Wishnok JS, et al. Chemical and cytokine features of innate immunity characterize serum and tissue profiles in inflammatory bowel disease. Proc Natl Acad Sci U S A. 2013 doi: 10.1073/pnas.1222669110. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fox JG, Dewhirst FE, Tully JG, Paster BJ, Yan L, Taylor NS, Collins MJ, Jr, Gorelick PL, Ward JM. Helicobacter hepaticus sp. nov., a microaerophilic bacterium isolated from livers and intestinal mucosal scrapings from mice. J Clin Microbiol. 1994;32(5):1238–1245. doi: 10.1128/jcm.32.5.1238-1245.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fox JG, Ge Z, Whary MT, Erdman SE, Horwitz BH. Helicobacter hepaticus infection in mice: models for understanding lower bowel inflammation and cancer. Mucosal Immunol. 2011;4(1):22–30. doi: 10.1038/mi.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shaked H, Hofseth LJ, Chumanevich A, Chumanevich AA, Wang J, Wang Y, Taniguchi K, Guma M, Shenouda S, Clevers H, et al. Chronic epithelial NF-kappaB activation accelerates APC loss and intestinal tumor initiation through iNOS up-regulation. Proc Natl Acad Sci U S A. 2012;109(35):14007–14012. doi: 10.1073/pnas.1211509109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoffman RA, Zhang G, Nussler NC, Gleixner SL, Ford HR, Simmons RL, Watkins SC. Constitutive expression of inducible nitric oxide synthase in the mouse ileal mucosa. Am J Physiol. 1997;272(2 Pt 1):G383–G392. doi: 10.1152/ajpgi.1997.272.2.G383. [DOI] [PubMed] [Google Scholar]
- 34.Li CQ, Kim MY, Godoy LC, Thiantanawat A, Trudel LJ, Wogan GN. Nitric oxide activation of Keap1/Nrf2 signaling in human colon carcinoma cells. Proc Natl Acad Sci U S A. 2009;106(34):14547–14551. doi: 10.1073/pnas.0907539106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chin MP, Schauer DB, Deen WM. Nitric oxide, oxygen, and superoxide formation and consumption in macrophages and colonic epithelial cells. Chem Res Toxicol. 2010;23(4):778–787. doi: 10.1021/tx900415k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weitzman SA, Weitberg AB, Clark EP, Stossel TP. Phagocytes as carcinogens: malignant transformation produced by human neutrophils. Science. 1985;227(4691):1231–1233. doi: 10.1126/science.3975611. [DOI] [PubMed] [Google Scholar]
- 37.McCafferty DM, Mudgett JS, Swain MG, Kubes P. Inducible nitric oxide synthase plays a critical role in resolving intestinal inflammation. Gastroenterology. 1997;112(3):1022–1027. doi: 10.1053/gast.1997.v112.pm9041266. [DOI] [PubMed] [Google Scholar]
- 38.McCafferty DM, Sihota E, Muscara M, Wallace JL, Sharkey KA, Kubes P. Spontaneously developing chronic colitis in IL-10/iNOS double-deficient mice. Am J Physiol Gastrointest Liver Physiol. 2000;279(1):G90–G99. doi: 10.1152/ajpgi.2000.279.1.G90. [DOI] [PubMed] [Google Scholar]
- 39.Zingarelli B, Szabo C, Salzman AL. Reduced oxidative and nitrosative damage in murine experimental colitis in the absence of inducible nitric oxide synthase. Gut. 1999;45(2):199–209. doi: 10.1136/gut.45.2.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Natsui M, Kawasaki K, Takizawa H, Hayashi SI, Matsuda Y, Sugimura K, Seki K, Narisawa R, Sendo F, Asakura H. Selective depletion of neutrophils by a monoclonal antibody, RP-3, suppresses dextran sulphate sodium-induced colitis in rats. J Gastroenterol Hepatol. 1997;12(12):801–808. doi: 10.1111/j.1440-1746.1997.tb00375.x. [DOI] [PubMed] [Google Scholar]
- 41.Muthupalani S, Ge Z, Feng Y, Rickman B, Mobley M, McCabe A, Van Rooijen N, Fox JG. Systemic macrophage depletion inhibits Helicobacter bilis-induced proinflammatory cytokine-mediated typhlocolitis and impairs bacterial colonization dynamics in a BALB/c Rag2−/− mouse model of inflammatory bowel disease. Infect Immun. 2012;80(12):4388–4397. doi: 10.1128/IAI.00530-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Winterbourn CC. Reconciling the chemistry and biology of reactive oxygen species. Nat Chem Biol. 2008;4(5):278–286. doi: 10.1038/nchembio.85. [DOI] [PubMed] [Google Scholar]
- 43.Drummond GR, Selemidis S, Griendling KK, Sobey CG. Combating oxidative stress in vascular disease: NADPH oxidases as therapeutic targets. Nat Rev Drug Discov. 2011;10(6):453–471. doi: 10.1038/nrd3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vorbach C, Harrison R, Capecchi MR. Xanthine oxidoreductase is central to the evolution and function of the innate immune system. Trends Immunol. 2003;24(9):512–517. doi: 10.1016/s1471-4906(03)00237-0. [DOI] [PubMed] [Google Scholar]
- 45.Rokutan K, Kawahara T, Kuwano Y, Tominaga K, Nishida K, Teshima-Kondo S. Nox enzymes and oxidative stress in the immunopathology of the gastrointestinal tract. Semin Immunopathol. 2008;30(3):315–327. doi: 10.1007/s00281-008-0124-5. [DOI] [PubMed] [Google Scholar]
- 46.Szanto I, Rubbia-Brandt L, Kiss P, Steger K, Banfi B, Kovari E, Herrmann F, Hadengue A, Krause KH. Expression of NOX1, a superoxide-generating NADPH oxidase, in colon cancer and inflammatory bowel disease. J Pathol. 2005;207(2):164–176. doi: 10.1002/path.1824. [DOI] [PubMed] [Google Scholar]
- 47.Fukuyama M, Rokutan K, Sano T, Miyake H, Shimada M, Tashiro S. Overexpression of a novel superoxide-producing enzyme, NADPH oxidase 1, in adenoma and well differentiated adenocarcinoma of the human colon. Cancer Lett. 2005;221(1):97–104. doi: 10.1016/j.canlet.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 48.Kamizato M, Nishida K, Masuda K, Takeo K, Yamamoto Y, Kawai T, Teshima-Kondo S, Tanahashi T, Rokutan K. Interleukin 10 inhibits interferon gamma- and tumor necrosis factor alpha-stimulated activation of NADPH oxidase 1 in human colonic epithelial cells and the mouse colon. J Gastroenterol. 2009;44(12):1172–1184. doi: 10.1007/s00535-009-0119-6. [DOI] [PubMed] [Google Scholar]
- 49.Kuwano Y, Tominaga K, Kawahara T, Sasaki H, Takeo K, Nishida K, Masuda K, Kawai T, Teshima-Kondo S, Rokutan K. Tumor necrosis factor alpha activates transcription of the NADPH oxidase organizer 1 (NOXO1) gene and upregulates superoxide production in colon epithelial cells. Free Radic Biol Med. 2008;45(12):1642–1652. doi: 10.1016/j.freeradbiomed.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 50.Huang JS, Noack D, Rae J, Ellis BA, Newbury R, Pong AL, Lavine JE, Curnutte JT, Bastian J. Chronic granulomatous disease caused by a deficiency in p47(phox) mimicking Crohn's disease. Clin Gastroenterol Hepatol. 2004;2(8):690–695. doi: 10.1016/s1542-3565(04)00292-7. [DOI] [PubMed] [Google Scholar]
- 51.Marciano BE, Rosenzweig SD, Kleiner DE, Anderson VL, Darnell DN, Anaya-O'Brien S, Hilligoss DM, Malech HL, Gallin JI, Holland SM. Gastrointestinal involvement in chronic granulomatous disease. Pediatrics. 2004;114(2):462–468. doi: 10.1542/peds.114.2.462. [DOI] [PubMed] [Google Scholar]
- 52.Gibbings S, Elkins ND, Fitzgerald H, Tiao J, Weyman ME, Shibao G, Fini MA, Wright RM. Xanthine oxidoreductase promotes the inflammatory state of mononuclear phagocytes through effects on chemokine expression, peroxisome proliferator-activated receptor-{gamma} sumoylation, and HIF-1{alpha} J Biol Chem. 2011;286(2):961–975. doi: 10.1074/jbc.M110.150847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kruidenier L, Kuiper I, Lamers CB, Verspaget HW. Intestinal oxidative damage in inflammatory bowel disease: semi-quantification, localization, and association with mucosal antioxidants. J Pathol. 2003;201(1):28–36. doi: 10.1002/path.1409. [DOI] [PubMed] [Google Scholar]
- 54.Vorbach C, Scriven A, Capecchi MR. The housekeeping gene xanthine oxidoreductase is necessary for milk fat droplet enveloping and secretion: gene sharing in the lactating mammary gland. Genes Dev. 2002;16(24):3223–3235. doi: 10.1101/gad.1032702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ohtsubo T, Matsumura K, Sakagami K, Fujii K, Tsuruya K, Noguchi H, Rovira II, Finkel T, Iida M. Xanthine oxidoreductase depletion induces renal interstitial fibrosis through aberrant lipid and purine accumulation in renal tubules. Hypertension. 2009;54(4):868–876. doi: 10.1161/HYPERTENSIONAHA.109.135152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thomas DD, Ridnour LA, Isenberg JS, Flores-Santana W, Switzer CH, Donzelli S, Hussain P, Vecoli C, Paolocci N, Ambs S, et al. The chemical biology of nitric oxide: implications in cellular signaling. Free Radic Biol Med. 2008;45(1):18–31. doi: 10.1016/j.freeradbiomed.2008.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Choi K, Chen J, Mitra S, Sarna SK. Impaired integrity of DNA after recovery from inflammation causes persistent dysfunction of colonic smooth muscle. Gastroenterology. 2011;141(4):1293–1301. doi: 10.1053/j.gastro.2011.06.074. 1301 e1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kruidenier L, van Meeteren ME, Kuiper I, Jaarsma D, Lamers CB, Zijlstra FJ, Verspaget HW. Attenuated mild colonic inflammation and improved survival from severe DSS-colitis of transgenic Cu/Zn-SOD mice. Free Radic Biol Med. 2003;34(6):753–765. doi: 10.1016/s0891-5849(02)01426-0. [DOI] [PubMed] [Google Scholar]
- 59.Weiss RH, Fretland DJ, Baron DA, Ryan US, Riley DP. Manganese-based superoxide dismutase mimetics inhibit neutrophil infiltration in vivo. J Biol Chem. 1996;271(42):26149–26156. doi: 10.1074/jbc.271.42.26149. [DOI] [PubMed] [Google Scholar]
- 60.Segui J, Gironella M, Sans M, Granell S, Gil F, Gimeno M, Coronel P, Pique JM, Panes J. Superoxide dismutase ameliorates TNBS-induced colitis by reducing oxidative stress, adhesion molecule expression, and leukocyte recruitment into the inflamed intestine. J Leukoc Biol. 2004;76(3):537–544. doi: 10.1189/jlb.0304196. [DOI] [PubMed] [Google Scholar]
- 61.Oku T, Iyama S, Sato T, Sato Y, Tanaka M, Sagawa T, Kuribayashi K, Sumiyosi T, Murase K, Machida T, et al. Amelioration of murine dextran sulfate sodium-induced colitis by ex vivo extracellular superoxide dismutase gene transfer. Inflamm Bowel Dis. 2006;12(7):630–640. doi: 10.1097/01.MIB.0000225335.68614.73. [DOI] [PubMed] [Google Scholar]
- 62.Ishihara T, Tanaka K, Tasaka Y, Namba T, Suzuki J, Okamoto S, Hibi T, Takenaga M, Igarashi R, Sato K, et al. Therapeutic effect of lecithinized superoxide dismutase against colitis. J Pharmacol Exp Ther. 2009;328(1):152–164. doi: 10.1124/jpet.108.144451. [DOI] [PubMed] [Google Scholar]
- 63.Kruidenier L, Kuiper I, van Duijn W, Marklund SL, van Hogezand RA, Lamers CB, Verspaget HW. Differential mucosal expression of three superoxide dismutase isoforms in inflammatory bowel disease. J Pathol. 2003;201(1):7–16. doi: 10.1002/path.1407. [DOI] [PubMed] [Google Scholar]
- 64.Lewis RS, Tamir S, Tannenbaum SR, Deen WM. Kinetic analysis of the fate of nitric oxide synthesized by macrophages in vitro. J Biol Chem. 1995;270(49):29350–29355. doi: 10.1074/jbc.270.49.29350. [DOI] [PubMed] [Google Scholar]
- 65.Tannenbaum SR, Fett D, Young VR, Land PD, Bruce WR. Nitrite and nitrate are formed by endogenous synthesis in the human intestine. Science. 1978;200(4349):1487–1489. doi: 10.1126/science.663630. [DOI] [PubMed] [Google Scholar]
- 66.Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov. 2008;7(2):156–167. doi: 10.1038/nrd2466. [DOI] [PubMed] [Google Scholar]
- 67.Bryan NS, Fernandez BO, Bauer SM, Garcia-Saura MF, Milsom AB, Rassaf T, Maloney RE, Bharti A, Rodriguez J, Feelisch M. Nitrite is a signaling molecule and regulator of gene expression in mammalian tissues. Nat Chem Biol. 2005;1(5):290–297. doi: 10.1038/nchembio734. [DOI] [PubMed] [Google Scholar]
- 68.Ferrer-Sueta G, Radi R. Chemical biology of peroxynitrite: kinetics, diffusion, and radicals. ACS Chem Biol. 2009;4(3):161–177. doi: 10.1021/cb800279q. [DOI] [PubMed] [Google Scholar]
- 69.Lonkar P, Dedon PC. Reactive species and DNA damage in chronic inflammation: Reconciling chemical mechanisms and biological fates. Int J Cancer. 2010 doi: 10.1002/ijc.25815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marletta MA, Yoon PS, Iyengar R, Leaf CD, Wishnok JS. Macrophage oxidation of L-arginine to nitrite and nitrate: nitric oxide is an intermediate. Biochemistry. 1988;27(24):8706–8711. doi: 10.1021/bi00424a003. [DOI] [PubMed] [Google Scholar]
- 71.Stuehr DJ, Santolini J, Wang ZQ, Wei CC, Adak S. Update on mechanism and catalytic regulation in the NO synthases. J Biol Chem. 2004;279(35):36167–36170. doi: 10.1074/jbc.R400017200. [DOI] [PubMed] [Google Scholar]
- 72.Chin MP, Schauer DB, Deen WM. Prediction of nitric oxide concentrations in colonic crypts during inflammation. Nitric Oxide. 2008;19(3):266–275. doi: 10.1016/j.niox.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 73.Kimura H, Hokari R, Miura S, Shigematsu T, Hirokawa M, Akiba Y, Kurose I, Higuchi H, Fujimori H, Tsuzuki Y, et al. Increased expression of an inducible isoform of nitric oxide synthase and the formation of peroxynitrite in colonic mucosa of patients with active ulcerative colitis. Gut. 1998;42(2):180–187. doi: 10.1136/gut.42.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Singer II, Kawka DW, Scott S, Weidner JR, Mumford RA, Riehl TE, Stenson WF. Expression of inducible nitric oxide synthase and nitrotyrosine in colonic epithelium in inflammatory bowel disease. Gastroenterology. 1996;111(4):871–885. doi: 10.1016/s0016-5085(96)70055-0. [DOI] [PubMed] [Google Scholar]
- 75.Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci U S A. 1987;84(24):9265–9269. doi: 10.1073/pnas.84.24.9265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Palmer RM, Ferrige AG, Moncada S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature. 1987;327(6122):524–526. doi: 10.1038/327524a0. [DOI] [PubMed] [Google Scholar]
- 77.MacNaughton WK, Lowe SS, Cushing K. Role of nitric oxide in inflammation-induced suppression of secretion in a mouse model of acute colitis. Am J Physiol. 1998;275(6 Pt 1):G1353–G1360. doi: 10.1152/ajpgi.1998.275.6.G1353. [DOI] [PubMed] [Google Scholar]
- 78.Hokari R, Kato S, Matsuzaki K, Kuroki M, Iwai A, Kawaguchi A, Nagao S, Miyahara T, Itoh K, Sekizuka E, et al. Reduced sensitivity of inducible nitric oxide synthase-deficient mice to chronic colitis. Free Radic Biol Med. 2001;31(2):153–163. doi: 10.1016/s0891-5849(01)00565-2. [DOI] [PubMed] [Google Scholar]
- 79.Yasukawa K, Tokuda H, Tun X, Utsumi H, Yamada KI. The detrimental effect of nitric oxide on tissue is associated with inflammatory events in the vascular endothelium and neutrophils in mice with dextran sodium sulfate-induced colitis. Free Radic Res. 2012 doi: 10.3109/10715762.2012.732698. [DOI] [PubMed] [Google Scholar]
- 80.Saijo F, Milsom AB, Bryan NS, Bauer SM, Vowinkel T, Ivanovic M, Andry C, Granger DN, Rodriguez J, Feelisch M. On the dynamics of nitrite, nitrate and other biomarkers of nitric oxide production in inflammatory bowel disease. Nitric Oxide. 2010;22(2):155–167. doi: 10.1016/j.niox.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 81.Kohno H, Takahashi M, Yasui Y, Suzuki R, Miyamoto S, Kamanaka Y, Naka M, Maruyama T, Wakabayashi K, Tanaka T. A specific inducible nitric oxide synthase inhibitor, ONO-1714 attenuates inflammation-related large bowel carcinogenesis in male Apc(Min/+) mice. Int J Cancer. 2007;121(3):506–513. doi: 10.1002/ijc.22736. [DOI] [PubMed] [Google Scholar]
- 82.Rachmilewitz D, Stamler JS, Karmeli F, Mullins ME, Singel DJ, Loscalzo J, Xavier RJ, Podolsky DK. Peroxynitrite-induced rat colitis--a new model of colonic inflammation. Gastroenterology. 1993;105(6):1681–1688. doi: 10.1016/0016-5085(93)91063-n. [DOI] [PubMed] [Google Scholar]
- 83.Ahn B, Ohshima H. Suppression of intestinal polyposis in Apc(Min/+) mice by inhibiting nitric oxide production. Cancer Res. 2001;61(23):8357–8360. [PubMed] [Google Scholar]
- 84.Krieglstein CF, Anthoni C, Cerwinka WH, Stokes KY, Russell J, Grisham MB, Granger DN. Role of blood- and tissue-associated inducible nitric-oxide synthase in colonic inflammation. Am J Pathol. 2007;170(2):490–496. doi: 10.2353/ajpath.2007.060594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Beck PL, Xavier R, Wong J, Ezedi I, Mashimo H, Mizoguchi A, Mizoguchi E, Bhan AK, Podolsky DK. Paradoxical roles of different nitric oxide synthase isoforms in colonic injury. Am J Physiol Gastrointest Liver Physiol. 2004;286(1):G137–G147. doi: 10.1152/ajpgi.00309.2003. [DOI] [PubMed] [Google Scholar]
- 86.Seril DN, Liao J, Yang GY. Colorectal carcinoma development in inducible nitric oxide synthase-deficient mice with dextran sulfate sodium-induced ulcerative colitis. Mol Carcinog. 2007;46(5):341–353. doi: 10.1002/mc.20282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang R, Ma A, Urbanski SJ, McCafferty DM. Induction of inducible nitric oxide synthase: a protective mechanism in colitis-induced adenocarcinoma. Carcinogenesis. 2007;28(5):1122–1130. doi: 10.1093/carcin/bgl224. [DOI] [PubMed] [Google Scholar]
- 88.Beck PL, Li Y, Wong J, Chen CW, Keenan CM, Sharkey KA, McCafferty DM. Inducible nitric oxide synthase from bone marrow-derived cells plays a critical role in regulating colonic inflammation. Gastroenterology. 2007;132(5):1778–1790. doi: 10.1053/j.gastro.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 89.Schneemann M, Schoedon G. Species differences in macrophage NO production are important. Nat Immunol. 2002;3(2):102. doi: 10.1038/ni0202-102a. [DOI] [PubMed] [Google Scholar]
- 90.Mestas J, Hughes CC. Of mice and not men: differences between mouse and human immunology. J Immunol. 2004;172(5):2731–2738. doi: 10.4049/jimmunol.172.5.2731. [DOI] [PubMed] [Google Scholar]
- 91.Fang FC, Nathan CF. Man is not a mouse: reply. J Leukoc Biol. 2007;81(3):580. doi: 10.1189/jlb.1206715. [DOI] [PubMed] [Google Scholar]
- 92.Schneemann M, Schoeden G. Macrophage biology and immunology: man is not a mouse. J Leukoc Biol. 2007;81(3):579. doi: 10.1189/jlb.1106702. discussion 580. [DOI] [PubMed] [Google Scholar]
- 93.Boughton-Smith NK, Evans SM, Hawkey CJ, Cole AT, Balsitis M, Whittle BJ, Moncada S. Nitric oxide synthase activity in ulcerative colitis and Crohn's disease. Lancet. 1993;342(8867):338–340. doi: 10.1016/0140-6736(93)91476-3. [DOI] [PubMed] [Google Scholar]
- 94.Rachmilewitz D, Stamler JS, Bachwich D, Karmeli F, Ackerman Z, Podolsky DK. Enhanced colonic nitric oxide generation and nitric oxide synthase activity in ulcerative colitis and Crohn's disease. Gut. 1995;36(5):718–723. doi: 10.1136/gut.36.5.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Keshavarzian A, Banan A, Farhadi A, Komanduri S, Mutlu E, Zhang Y, Fields JZ. Increases in free radicals and cytoskeletal protein oxidation and nitration in the colon of patients with inflammatory bowel disease. Gut. 2003;52(5):720–728. doi: 10.1136/gut.52.5.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gochman E, Mahajna J, Shenzer P, Dahan A, Blatt A, Elyakim R, Reznick AZ. The expression of iNOS and nitrotyrosine in colitis and colon cancer in humans. Acta Histochem. 2012;114(8):827–835. doi: 10.1016/j.acthis.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 97.Yue G, Lai PS, Yin K, Sun FF, Nagele RG, Liu X, Linask KK, Wang C, Lin KT, Wong PY. Colon epithelial cell death in 2,4,6-trinitrobenzenesulfonic acid-induced colitis is associated with increased inducible nitric-oxide synthase expression and peroxynitrite production. J Pharmacol Exp Ther. 2001;297(3):915–925. [PubMed] [Google Scholar]
- 98.Guihot G, Guimbaud R, Bertrand V, Narcy-Lambare B, Couturier D, Duee PH, Chaussade S, Blachier F. Inducible nitric oxide synthase activity in colon biopsies from inflammatory areas: correlation with inflammation intensity in patients with ulcerative colitis but not with Crohn's disease. Amino Acids. 2000;18(3):229–237. doi: 10.1007/s007260050020. [DOI] [PubMed] [Google Scholar]
- 99.Kimura H, Miura S, Shigematsu T, Ohkubo N, Tsuzuki Y, Kurose I, Higuchi H, Akiba Y, Hokari R, Hirokawa M, et al. Increased nitric oxide production and inducible nitric oxide synthase activity in colonic mucosa of patients with active ulcerative colitis and Crohn's disease. Dig Dis Sci. 1997;42(5):1047–1054. doi: 10.1023/a:1018849405922. [DOI] [PubMed] [Google Scholar]
- 100.van der Veen BS, de Winther MP, Heeringa P. Myeloperoxidase: molecular mechanisms of action and their relevance to human health and disease. Antioxid Redox Signal. 2009;11(11):2899–2937. doi: 10.1089/ars.2009.2538. [DOI] [PubMed] [Google Scholar]
- 101.Klebanoff SJ. Myeloperoxidase: friend and foe. J Leukoc Biol. 2005;77(5):598–625. doi: 10.1189/jlb.1204697. [DOI] [PubMed] [Google Scholar]
- 102.Pattison DI, Davies MJ, Hawkins CL. Reactions and reactivity of myeloperoxidase-derived oxidants: differential biological effects of hypochlorous and hypothiocyanous acids. Free Radic Res. 2012;46(8):975–995. doi: 10.3109/10715762.2012.667566. [DOI] [PubMed] [Google Scholar]
- 103.Arnhold J, Flemmig J. Human myeloperoxidase in innate and acquired immunity. Arch Biochem Biophys. 2010;500(1):92–106. doi: 10.1016/j.abb.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 104.McBee ME, Zeng Y, Parry N, Nagler CR, Tannenbaum SR, Schauer DB. Multivariate modeling identifies neutrophil- and Th17-related factors as differential serum biomarkers of chronic murine colitis. PLoS ONE. 2010;5(10):e13277. doi: 10.1371/journal.pone.0013277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Eiserich JP, Hristova M, Cross CE, Jones AD, Freeman BA, Halliwell B, van der Vliet A. Formation of nitric oxide-derived inflammatory oxidants by myeloperoxidase in neutrophils. Nature. 1998;391(6665):393–397. doi: 10.1038/34923. [DOI] [PubMed] [Google Scholar]
- 106.Brennan ML, Wu W, Fu X, Shen Z, Song W, Frost H, Vadseth C, Narine L, Lenkiewicz E, Borchers MT, et al. A tale of two controversies: defining both the role of peroxidases in nitrotyrosine formation in vivo using eosinophil peroxidase and myeloperoxidase-deficient mice, and the nature of peroxidase-generated reactive nitrogen species. J Biol Chem. 2002;277(20):17415–17427. doi: 10.1074/jbc.M112400200. [DOI] [PubMed] [Google Scholar]
- 107.Gaut JP, Byun J, Tran HD, Lauber WM, Carroll JA, Hotchkiss RS, Belaaouaj A, Heinecke JW. Myeloperoxidase produces nitrating oxidants in vivo. J Clin Invest. 2002;109(10):1311–1319. doi: 10.1172/JCI15021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Brennan ML, Anderson MM, Shih DM, Qu XD, Wang X, Mehta AC, Lim LL, Shi W, Hazen SL, Jacob JS, et al. Increased atherosclerosis in myeloperoxidase-deficient mice. J Clin Invest. 2001;107(4):419–430. doi: 10.1172/JCI8797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Takizawa S, Aratani Y, Fukuyama N, Maeda N, Hirabayashi H, Koyama H, Shinohara Y, Nakazawa H. Deficiency of myeloperoxidase increases infarct volume and nitrotyrosine formation in mouse brain. J Cereb Blood Flow Metab. 2002;22(1):50–54. doi: 10.1097/00004647-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 110.Garrity-Park M, Loftus EV, Jr, Sandborn WJ, Smyrk TC. Myeloperoxidase immunohistochemistry as a measure of disease activity in ulcerative colitis: association with ulcerative colitis-colorectal cancer, tumor necrosis factor polymorphism and RUNX3 methylation. Inflamm Bowel Dis. 2012;18(2):275–283. doi: 10.1002/ibd.21681. [DOI] [PubMed] [Google Scholar]
- 111.Ardite E, Sans M, Panes J, Romero FJ, Pique JM, Fernandez-Checa JC. Replenishment of glutathione levels improves mucosal function in experimental acute colitis. Lab Invest. 2000;80(5):735–744. doi: 10.1038/labinvest.3780077. [DOI] [PubMed] [Google Scholar]
- 112.Seril DN, Liao J, Ho KL, Yang CS, Yang GY. Inhibition of chronic ulcerative colitis-associated colorectal adenocarcinoma development in a murine model by N-acetylcysteine. Carcinogenesis. 2002;23(6):993–1001. doi: 10.1093/carcin/23.6.993. [DOI] [PubMed] [Google Scholar]
- 113.Catarzi S, Favilli F, Romagnoli C, Marcucci T, Picariello L, Tonelli F, Vincenzini MT, Iantomasi T. Oxidative state and IL-6 production in intestinal myofibroblasts of Crohn's disease patients. Inflamm Bowel Dis. 2011;17(8):1674–1684. doi: 10.1002/ibd.21552. [DOI] [PubMed] [Google Scholar]
- 114.Murawaki Y, Tsuchiya H, Kanbe T, Harada K, Yashima K, Nozaka K, Tanida O, Kohno M, Mukoyama T, Nishimuki E, et al. Aberrant expression of selenoproteins in the progression of colorectal cancer. Cancer Lett. 2008;259(2):218–230. doi: 10.1016/j.canlet.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 115.Circu ML, Aw TY. Intestinal redox biology and oxidative stress. Semin Cell Dev Biol. 2012;23(7):729–737. doi: 10.1016/j.semcdb.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Brigelius-Flohe R, Kipp AP. Physiological functions of GPx2 and its role in inflammation-triggered carcinogenesis. Ann N Y Acad Sci. 2012;1259:19–25. doi: 10.1111/j.1749-6632.2012.06574.x. [DOI] [PubMed] [Google Scholar]
- 117.Te Velde AA, Pronk I, de Kort F, Stokkers PC. Glutathione peroxidase 2 and aquaporin 8 as new markers for colonic inflammation in experimental colitis and inflammatory bowel diseases: an important role for H2O2? Eur J Gastroenterol Hepatol. 2008;20(6):555–560. doi: 10.1097/MEG.0b013e3282f45751. [DOI] [PubMed] [Google Scholar]
- 118.Krehl S, Loewinger M, Florian S, Kipp AP, Banning A, Wessjohann LA, Brauer MN, Iori R, Esworthy RS, Chu FF, et al. Glutathione peroxidase-2 and selenium decreased inflammation and tumors in a mouse model of inflammation-associated carcinogenesis whereas sulforaphane effects differed with selenium supply. Carcinogenesis. 2012;33(3):620–628. doi: 10.1093/carcin/bgr288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Florian S, Krehl S, Loewinger M, Kipp A, Banning A, Esworthy S, Chu FF, Brigelius-Flohe R. Loss of GPx2 increases apoptosis, mitosis, and GPx1 expression in the intestine of mice. Free Radic Biol Med. 2010;49(11):1694–1702. doi: 10.1016/j.freeradbiomed.2010.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Esworthy RS, Aranda R, Martin MG, Doroshow JH, Binder SW, Chu FF. Mice with combined disruption of Gpx1 and Gpx2 genes have colitis. Am J Physiol Gastrointest Liver Physiol. 2001;281(3):G848–G855. doi: 10.1152/ajpgi.2001.281.3.G848. [DOI] [PubMed] [Google Scholar]
- 121.Nguyen T, Nioi P, Pickett CB. The Nrf2-antioxidant response element signaling pathway and its activation by oxidative stress. J Biol Chem. 2009;284(20):13291–13295. doi: 10.1074/jbc.R900010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hess DT, Matsumoto A, Kim SO, Marshall HE, Stamler JS. Protein S-nitrosylation: purview and parameters. Nat Rev Mol Cell Biol. 2005;6(2):150–166. doi: 10.1038/nrm1569. [DOI] [PubMed] [Google Scholar]
- 123.Tannenbaum SR, Kim JE. Controlled S-nitrosation. Nat Chem Biol. 2005;1(3):126–127. doi: 10.1038/nchembio0805-126. [DOI] [PubMed] [Google Scholar]
- 124.Barglow KT, Knutson CG, Wishnok JS, Tannenbaum SR, Marletta MA. Site-specific and redox-controlled S-nitrosation of thioredoxin. Proc Natl Acad Sci U S A. 2011;108(35):E600–E606. doi: 10.1073/pnas.1110736108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mitchell DA, Morton SU, Fernhoff NB, Marletta MA. Thioredoxin is required for S-nitrosation of procaspase-3 and the inhibition of apoptosis in Jurkat cells. Proc Natl Acad Sci U S A. 2007;104(28):11609–11614. doi: 10.1073/pnas.0704898104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mitchell DA, Marletta MA. Thioredoxin catalyzes the S-nitrosation of the caspase-3 active site cysteine. Nat Chem Biol. 2005;1(3):154–158. doi: 10.1038/nchembio720. [DOI] [PubMed] [Google Scholar]
- 127.Khor TO, Huang MT, Prawan A, Liu Y, Hao X, Yu S, Cheung WK, Chan JY, Reddy BS, Yang CS, et al. Increased susceptibility of Nrf2 knockout mice to colitis-associated colorectal cancer. Cancer Prev Res (Phila) 2008;1(3):187–191. doi: 10.1158/1940-6207.CAPR-08-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Khor TO, Huang MT, Kwon KH, Chan JY, Reddy BS, Kong AN. Nrf2-deficient mice have an increased susceptibility to dextran sulfate sodium-induced colitis. Cancer Res. 2006;66(24):11580–11584. doi: 10.1158/0008-5472.CAN-06-3562. [DOI] [PubMed] [Google Scholar]
- 129.Osburn WO, Karim B, Dolan PM, Liu G, Yamamoto M, Huso DL, Kensler TW. Increased colonic inflammatory injury and formation of aberrant crypt foci in Nrf2-deficient mice upon dextran sulfate treatment. Int J Cancer. 2007;121(9):1883–1891. doi: 10.1002/ijc.22943. [DOI] [PubMed] [Google Scholar]
- 130.Arisawa T, Tahara T, Shibata T, Nagasaka M, Nakamura M, Kamiya Y, Fujita H, Yoshioka D, Okubo M, Sakata M, et al. Nrf2 gene promoter polymorphism is associated with ulcerative colitis in a Japanese population. Hepatogastroenterology. 2008;55(82–83):394–397. [PubMed] [Google Scholar]
- 131.Jin Y, Kotakadi VS, Ying L, Hofseth AB, Cui X, Wood PA, Windust A, Matesic LE, Pena EA, Chiuzan C, et al. American ginseng suppresses inflammation and DNA damage associated with mouse colitis. Carcinogenesis. 2008;29(12):2351–2359. doi: 10.1093/carcin/bgn211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ju J, Hao X, Lee MJ, Lambert JD, Lu G, Xiao H, Newmark HL, Yang CS. A gamma-tocopherol-rich mixture of tocopherols inhibits colon inflammation and carcinogenesis in azoxymethane and dextran sulfate sodium-treated mice. Cancer Prev Res (Phila) 2009;2(2):143–152. doi: 10.1158/1940-6207.CAPR-08-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hao X, Sun Y, Yang CS, Bose M, Lambert JD, Ju J, Lu G, Lee MJ, Park S, Husain A, et al. Inhibition of intestinal tumorigenesis in Apc(min/+) mice by green tea polyphenols (polyphenon E) and individual catechins. Nutr Cancer. 2007;59(1):62–69. doi: 10.1080/01635580701365050. [DOI] [PubMed] [Google Scholar]
- 134.Vong LB, Tomita T, Yoshitomi T, Matsui H, Nagasaki Y. An orally administered redox nanoparticle that accumulates in the colonic mucosa and reduces colitis in mice. Gastroenterology. 2012;143(4):1027–1036. e3. doi: 10.1053/j.gastro.2012.06.043. [DOI] [PubMed] [Google Scholar]
- 135.Dong M, Dedon PC. Relatively small increases in the steady-state levels of nucleobase deamination products in DNA from human TK6 cells exposed to toxic levels of nitric oxide. Chem Res Toxicol. 2006;19(1):50–57. doi: 10.1021/tx050252j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Li CQ, Pang B, Kiziltepe T, Trudel LJ, Engelward BP, Dedon PC, Wogan GN. Threshold effects of nitric oxide-induced toxicity and cellular responses in wild-type and p53-null human lymphoblastoid cells. Chem Res Toxicol. 2006;19(3):399–406. doi: 10.1021/tx050283e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Skinn BT, Lim CH, Deen WM. Nitric oxide delivery system for biological media. Free Radic Biol Med. 2011;50(2):381–388. doi: 10.1016/j.freeradbiomed.2010.10.713. [DOI] [PubMed] [Google Scholar]
- 138.Wang C, Deen WM. Peroxynitrite delivery methods for toxicity studies. Chem Res Toxicol. 2004;17(1):32–44. doi: 10.1021/tx0341557. [DOI] [PubMed] [Google Scholar]
- 139.Dendroulakis V, Russell BS, Elmquist CE, Trudel LJ, Wogan GN, Deen WM, Dedon PC. A system for exposing molecules and cells to biologically relevant and accurately controlled steady-state concentrations of nitric oxide and oxygen. Nitric Oxide. 2012;27(3):161–168. doi: 10.1016/j.niox.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Skinn BT, Deen WM. Nitrogen Dioxide Delivery System for Biological Media. Free Radic Biol Med. 2012 doi: 10.1016/j.freeradbiomed.2012.10.534. [DOI] [PubMed] [Google Scholar]
- 141.Wang C, Trudel LJ, Wogan GN, Deen WM. Thresholds of nitric oxide-mediated toxicity in human lymphoblastoid cells. Chem Res Toxicol. 2003;16(8):1004–1013. doi: 10.1021/tx0340448. [DOI] [PubMed] [Google Scholar]
- 142.Zhuang JC, Wogan GN. Growth and viability of macrophages continuously stimulated to produce nitric oxide. Proc Natl Acad Sci U S A. 1997;94(22):11875–11880. doi: 10.1073/pnas.94.22.11875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zhuang JC, Lin D, Lin C, Jethwaney D, Wogan GN. Genotoxicity associated with NO production in macrophages and co-cultured target cells. Free Radic Biol Med. 2002;33(1):94–102. doi: 10.1016/s0891-5849(02)00866-3. [DOI] [PubMed] [Google Scholar]
- 144.Li CQ, Wogan GN. Nitric oxide as a modulator of apoptosis. Cancer Lett. 2005;226(1):1–15. doi: 10.1016/j.canlet.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 145.Burney S, Tamir S, Gal A, Tannenbaum SR. A mechanistic analysis of nitric oxide-induced cellular toxicity. Nitric Oxide. 1997;1(2):130–144. doi: 10.1006/niox.1996.0114. [DOI] [PubMed] [Google Scholar]
- 146.Niles JC, Wishnok JS, Tannenbaum SR. Peroxynitrite-induced oxidation and nitration products of guanine and 8-oxoguanine: structures and mechanisms of product formation. Nitric Oxide. 2006;14(2):109–121. doi: 10.1016/j.niox.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 147.Neeley WL, Essigmann JM. Mechanisms of formation, genotoxicity, and mutation of guanine oxidation products. Chem Res Toxicol. 2006;19(4):491–505. doi: 10.1021/tx0600043. [DOI] [PubMed] [Google Scholar]
- 148.Dedon PC, Tannenbaum SR. Reactive nitrogen species in the chemical biology of inflammation. Arch Biochem Biophys. 2004;423(1):12–22. doi: 10.1016/j.abb.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 149.Dong M, Wang C, Deen WM, Dedon PC. Absence of 2'-deoxyoxanosine and presence of abasic sites in DNA exposed to nitric oxide at controlled physiological concentrations. Chem Res Toxicol. 2003;16(9):1044–1055. doi: 10.1021/tx034046s. [DOI] [PubMed] [Google Scholar]
- 150.Glaser R, Wu H, Lewis M. Cytosine catalysis of nitrosative guanine deamination and interstrand cross-link formation. J Am Chem Soc. 2005;127(20):7346–7358. doi: 10.1021/ja0501159. [DOI] [PubMed] [Google Scholar]
- 151.Son J, Pang B, McFaline JL, Taghizadeh K, Dedon PC. Surveying the damage: the challenges of developing nucleic acid biomarkers of inflammation. Mol Biosyst. 2008;4(9):902–908. doi: 10.1039/b719411k. [DOI] [PubMed] [Google Scholar]
- 152.deRojas-Walker T, Tamir S, Ji H, Wishnok JS, Tannenbaum SR. Nitric oxide induces oxidative damage in addition to deamination in macrophage DNA. Chem Res Toxicol. 1995;8(3):473–477. doi: 10.1021/tx00045a020. [DOI] [PubMed] [Google Scholar]
- 153.Tretyakova NY, Burney S, Pamir B, Wishnok JS, Dedon PC, Wogan GN, Tannenbaum SR. Peroxynitrite-induced DNA damage in the supF gene: correlation with the mutational spectrum. Mutat Res. 2000;447(2):287–303. doi: 10.1016/s0027-5107(99)00221-3. [DOI] [PubMed] [Google Scholar]
- 154.Cui L, Ye W, Prestwich EG, Wishnok JS, Taghizadeh K, Dedon PC, Tannenbaum SR. Comparative analysis of four oxidized guanine lesions from reactions of DNA with peroxynitrite, singlet oxygen, and gamma-radiation. Chem Res Toxicol. 2013;26(2):195–202. doi: 10.1021/tx300294d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Margolin Y, Shafirovich V, Geacintov NE, DeMott MS, Dedon PC. DNA sequence context as a determinant of the quantity and chemistry of guanine oxidation produced by hydroxyl radicals and one-electron oxidants. J Biol Chem. 2008;283(51):35569–35578. doi: 10.1074/jbc.M806809200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Margolin Y, Cloutier JF, Shafirovich V, Geacintov NE, Dedon PC. Paradoxical hotspots for guanine oxidation by a chemical mediator of inflammation. Nat Chem Biol. 2006;2(7):365–366. doi: 10.1038/nchembio796. [DOI] [PubMed] [Google Scholar]
- 157.Burney S, Niles JC, Dedon PC, Tannenbaum SR. DNA damage in deoxynucleosides and oligonucleotides treated with peroxynitrite. Chem Res Toxicol. 1999;12(6):513–520. doi: 10.1021/tx980254m. [DOI] [PubMed] [Google Scholar]
- 158.Shen Z, Wu W, Hazen SL. Activated leukocytes oxidatively damage DNA, RNA, and the nucleotide pool through halide-dependent formation of hydroxyl radical. Biochemistry. 2000;39(18):5474–5482. doi: 10.1021/bi992809y. [DOI] [PubMed] [Google Scholar]
- 159.Byun J, Henderson JP, Mueller DM, Heinecke JW. 8-Nitro-2'-deoxyguanosine, a specific marker of oxidation by reactive nitrogen species, is generated by the myeloperoxidase-hydrogen peroxide-nitrite system of activated human phagocytes. Biochemistry. 1999;38(8):2590–2600. doi: 10.1021/bi9822980. [DOI] [PubMed] [Google Scholar]
- 160.Luo W, Muller JG, Rachlin EM, Burrows CJ. Characterization of hydantoin products from one-electron oxidation of 8-oxo-7,8-dihydroguanosine in a nucleoside model. Chem Res Toxicol. 2001;14(7):927–938. doi: 10.1021/tx010072j. [DOI] [PubMed] [Google Scholar]
- 161.Luo W, Muller JG, Rachlin EM, Burrows CJ. Characterization of Spiroiminodihydantoin as a Product of One-Electron Oxidation of 8-Oxo-7,8-dihydroguanosine. Organic Letters. 2000;2(5):613–616. doi: 10.1021/ol9913643. [DOI] [PubMed] [Google Scholar]
- 162.Yu H, Venkatarangan L, Wishnok JS, Tannenbaum SR. Quantitation of four guanine oxidation products from reaction of DNA with varying doses of peroxynitrite. Chem Res Toxicol. 2005;18(12):1849–1857. doi: 10.1021/tx050146h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Niles JC, Wishnok JS, Tannenbaum SR. Spiroiminodihydantoin and guanidinohydantoin are the dominant products of 8-oxoguanosine oxidation at low fluxes of peroxynitrite: mechanistic studies with 18O. Chem Res Toxicol. 2004;17(11):1510–1519. doi: 10.1021/tx0400048. [DOI] [PubMed] [Google Scholar]
- 164.Nakabeppu Y, Sakumi K, Sakamoto K, Tsuchimoto D, Tsuzuki T, Nakatsu Y. Mutagenesis and carcinogenesis caused by the oxidation of nucleic acids. Biol Chem. 2006;387(4):373–379. doi: 10.1515/BC.2006.050. [DOI] [PubMed] [Google Scholar]
- 165.Henderson PT, Delaney JC, Muller JG, Neeley WL, Tannenbaum SR, Burrows CJ, Essigmann JM. The hydantoin lesions formed from oxidation of 7,8-dihydro-8-oxoguanine are potent sources of replication errors in vivo. Biochemistry. 2003;42(31):9257–9262. doi: 10.1021/bi0347252. [DOI] [PubMed] [Google Scholar]
- 166.van Loon B, Markkanen E, Hübscher U. Oxygen as a friend and enemy: How to combat the mutational potential of 8-oxo-guanine. DNA Repair. 2010;9(6):604–616. doi: 10.1016/j.dnarep.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 167.Ding X, Hiraku Y, Ma N, Kato T, Saito K, Nagahama M, Semba R, Kuribayashi K, Kawanishi S. Inducible nitric oxide synthase-dependent DNA damage in mouse model of inflammatory bowel disease. Cancer Sci. 2005;96(3):157–163. doi: 10.1111/j.1349-7006.2005.00024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Westbrook AM, Wei B, Braun J, Schiestl RH. Intestinal mucosal inflammation leads to systemic genotoxicity in mice. Cancer Res. 2009;69(11):4827–4834. doi: 10.1158/0008-5472.CAN-08-4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.McKenzie SJ, Baker MS, Buffinton GD, Doe WF. Evidence of oxidant-induced injury to epithelial cells during inflammatory bowel disease. J Clin Invest. 1996;98(1):136–141. doi: 10.1172/JCI118757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.D'Inca R, Cardin R, Benazzato L, Angriman I, Martines D, Sturniolo GC. Oxidative DNA damage in the mucosa of ulcerative colitis increases with disease duration and dysplasia. Inflamm Bowel Dis. 2004;10(1):23–27. doi: 10.1097/00054725-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 171.Choi J, Yoon SH, Kim JE, Rhee KH, Youn HS, Chung MH. Gene-specific oxidative DNA damage in Helicobacter pylori-infected human gastric mucosa. Int J Cancer. 2002;99(4):485–490. doi: 10.1002/ijc.10366. [DOI] [PubMed] [Google Scholar]
- 172.O'Hagan HM, Wang W, Sen S, Destefano Shields C, Lee SS, Zhang YW, Clements EG, Cai Y, Van Neste L, Easwaran H, et al. Oxidative damage targets complexes containing DNA methyltransferases, SIRT1, and polycomb members to promoter CpG Islands. Cancer Cell. 2011;20(5):606–619. doi: 10.1016/j.ccr.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Winczura A, Zdzalik D, Tudek B. Damage of DNA and proteins by major lipid peroxidation products in genome stability. Free Radic Res. 2012;46(4):442–459. doi: 10.3109/10715762.2012.658516. [DOI] [PubMed] [Google Scholar]
- 174.Pang B, Zhou X, Yu H, Dong M, Taghizadeh K, Wishnok JS, Tannenbaum SR, Dedon PC. Lipid peroxidation dominates the chemistry of DNA adduct formation in a mouse model of inflammation. Carcinogenesis. 2007;28(8):1807–1813. doi: 10.1093/carcin/bgm037. [DOI] [PubMed] [Google Scholar]
- 175.Meira LB, Bugni JM, Green SL, Lee CW, Pang B, Borenshtein D, Rickman BH, Rogers AB, Moroski-Erkul CA, McFaline JL, et al. DNA damage induced by chronic inflammation contributes to colon carcinogenesis in mice. J Clin Invest. 2008;118(7):2516–2525. doi: 10.1172/JCI35073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Nair J, Gansauge F, Beger H, Dolara P, Winde G, Bartsch H. Increased etheno-DNA adducts in affected tissues of patients suffering from Crohn's disease, ulcerative colitis, and chronic pancreatitis. Antioxid Redox Signal. 2006;8(5–6):1003–1010. doi: 10.1089/ars.2006.8.1003. [DOI] [PubMed] [Google Scholar]
- 177.Bartsch H, Nair J. Potential role of lipid peroxidation derived DNA damage in human colon carcinogenesis: studies on exocyclic base adducts as stable oxidative stress markers. Cancer Detect Prev. 2002;26(4):308–312. doi: 10.1016/s0361-090x(02)00093-4. [DOI] [PubMed] [Google Scholar]
- 178.Nair U, Bartsch H, Nair J. Lipid peroxidation-induced DNA damage in cancer-prone inflammatory diseases: a review of published adduct types and levels in humans. Free Radic Biol Med. 2007;43(8):1109–1120. doi: 10.1016/j.freeradbiomed.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 179.Zhang R, Brennan ML, Shen Z, MacPherson JC, Schmitt D, Molenda CE, Hazen SL. Myeloperoxidase functions as a major enzymatic catalyst for initiation of lipid peroxidation at sites of inflammation. J Biol Chem. 2002;277(48):46116–46122. doi: 10.1074/jbc.M209124200. [DOI] [PubMed] [Google Scholar]
- 180.Godschalk RW, Albrecht C, Curfs DM, Schins RP, Bartsch H, van Schooten FJ, Nair J. Decreased levels of lipid peroxidation-induced DNA damage in the onset of atherogenesis in apolipoprotein E deficient mice. Mutat Res. 2007;621(1–2):87–94. doi: 10.1016/j.mrfmmm.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 181.Obtulowicz T, Winczura A, Speina E, Swoboda M, Janik J, Janowska B, Ciesla JM, Kowalczyk P, Jawien A, Gackowski D, et al. Aberrant repair of etheno-DNA adducts in leukocytes and colon tissue of colon cancer patients. Free Radic Biol Med. 2010;49(6):1064–1071. doi: 10.1016/j.freeradbiomed.2010.06.027. [DOI] [PubMed] [Google Scholar]
- 182.Asahi T, Kondo H, Masuda M, Nishino H, Aratani Y, Naito Y, Yoshikawa T, Hisaka S, Kato Y, Osawa T. Chemical and immunochemical detection of 8-halogenated deoxyguanosines at early stage inflammation. J Biol Chem. 2010;285(12):9282–9291. doi: 10.1074/jbc.M109.054213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Kawai Y, Morinaga H, Kondo H, Miyoshi N, Nakamura Y, Uchida K, Osawa T. Endogenous formation of novel halogenated 2'-deoxycytidine. Hypohalous acid-mediated DNA modification at the site of inflammation. J Biol Chem. 2004;279(49):51241–51249. doi: 10.1074/jbc.M408210200. [DOI] [PubMed] [Google Scholar]
- 184.Henderson JP, Byun J, Takeshita J, Heinecke JW. Phagocytes produce 5-chlorouracil and 5-bromouracil, two mutagenic products of myeloperoxidase, in human inflammatory tissue. J Biol Chem. 2003;278(26):23522–23528. doi: 10.1074/jbc.M303928200. [DOI] [PubMed] [Google Scholar]
- 185.Masuda M, Suzuki T, Friesen MD, Ravanat JL, Cadet J, Pignatelli B, Nishino H, Ohshima H. Chlorination of guanosine and other nucleosides by hypochlorous acid and myeloperoxidase of activated human neutrophils. Catalysis by nicotine and trimethylamine. J Biol Chem. 2001;276(44):40486–40496. doi: 10.1074/jbc.M102700200. [DOI] [PubMed] [Google Scholar]
- 186.Henderson JP, Byun J, Heinecke JW. Molecular chlorine generated by the myeloperoxidase-hydrogen peroxide-chloride system of phagocytes produces 5-chlorocytosine in bacterial RNA. J Biol Chem. 1999;274(47):33440–33448. doi: 10.1074/jbc.274.47.33440. [DOI] [PubMed] [Google Scholar]
- 187.Badouard C, Masuda M, Nishino H, Cadet J, Favier A, Ravanat JL. Detection of chlorinated DNA and RNA nucleosides by HPLC coupled to tandem mass spectrometry as potential biomarkers of inflammation. J Chromatogr B Analyt Technol Biomed Life Sci. 2005;827(1):26–31. doi: 10.1016/j.jchromb.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 188.Jiang Q, Blount BC, Ames BN. 5-Chlorouracil, a marker of DNA damage from hypochlorous acid during inflammation. A gas chromatography-mass spectrometry assay. J Biol Chem. 2003;278(35):32834–32840. doi: 10.1074/jbc.M304021200. [DOI] [PubMed] [Google Scholar]
- 189.Takeshita J, Byun J, Nhan TQ, Pritchard DK, Pennathur S, Schwartz SM, Chait A, Heinecke JW. Myeloperoxidase generates 5-chlorouracil in human atherosclerotic tissue: a potential pathway for somatic mutagenesis by macrophages. J Biol Chem. 2006;281(6):3096–3104. doi: 10.1074/jbc.M509236200. [DOI] [PubMed] [Google Scholar]
- 190.Valinluck V, Liu P, Kang JI, Jr, Burdzy A, Sowers LC. 5-halogenated pyrimidine lesions within a CpG sequence context mimic 5-methylcytosine by enhancing the binding of the methyl-CpG-binding domain of methyl-CpG-binding protein 2 (MeCP2) Nucleic Acids Res. 2005;33(9):3057–3064. doi: 10.1093/nar/gki612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Valinluck V, Sowers LC. Endogenous cytosine damage products alter the site selectivity of human DNA maintenance methyltransferase DNMT1. Cancer Res. 2007;67(3):946–950. doi: 10.1158/0008-5472.CAN-06-3123. [DOI] [PubMed] [Google Scholar]
- 192.Lao VV, Herring JL, Kim CH, Darwanto A, Soto U, Sowers LC. Incorporation of 5-chlorocytosine into mammalian DNA results in heritable gene silencing and altered cytosine methylation patterns. Carcinogenesis. 2009;30(5):886–893. doi: 10.1093/carcin/bgp060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Issa JP, Ahuja N, Toyota M, Bronner MP, Brentnall TA. Accelerated age-related CpG island methylation in ulcerative colitis. Cancer Res. 2001;61(9):3573–3577. [PubMed] [Google Scholar]
- 194.London SJ, Lehman TA, Taylor JA. Myeloperoxidase genetic polymorphism and lung cancer risk. Cancer Res. 1997;57(22):5001–5003. [PubMed] [Google Scholar]
- 195.Cascorbi I, Henning S, Brockmoller J, Gephart J, Meisel C, Muller JM, Loddenkemper R, Roots I. Substantially reduced risk of cancer of the aerodigestive tract in subjects with variant--463A of the myeloperoxidase gene. Cancer Res. 2000;60(3):644–649. [PubMed] [Google Scholar]
- 196.Le Marchand L, Seifried A, Lum A, Wilkens LR. Association of the myeloperoxidase -463G--> a polymorphism with lung cancer risk. Cancer Epidemiol Biomarkers Prev. 2000;9(2):181–184. [PubMed] [Google Scholar]
- 197.Kozekov ID, Nechev LV, Moseley MS, Harris CM, Rizzo CJ, Stone MP, Harris TM. DNA interchain cross-links formed by acrolein and crotonaldehyde. J Am Chem Soc. 2003;125(1):50–61. doi: 10.1021/ja020778f. [DOI] [PubMed] [Google Scholar]
- 198.Stone MP, Cho YJ, Huang H, Kim HY, Kozekov ID, Kozekova A, Wang H, Minko IG, Lloyd RS, Harris TM, et al. Interstrand DNA cross-links induced by alpha,beta-unsaturated aldehydes derived from lipid peroxidation and environmental sources. Acc Chem Res. 2008;41(7):793–804. doi: 10.1021/ar700246x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Deans AJ, West SC. DNA interstrand crosslink repair and cancer. Nat Rev Cancer. 2011;11(7):467–480. doi: 10.1038/nrc3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Caulfield JL, Wishnok JS, Tannenbaum SR. Nitric oxide-induced interstrand cross-links in DNA. Chem Res Toxicol. 2003;16(5):571–574. doi: 10.1021/tx020117w. [DOI] [PubMed] [Google Scholar]
- 201.Burney S, Caulfield JL, Niles JC, Wishnok JS, Tannenbaum SR. The chemistry of DNA damage from nitric oxide and peroxynitrite. Mutat Res. 1999;424(1–2):37–49. doi: 10.1016/s0027-5107(99)00006-8. [DOI] [PubMed] [Google Scholar]
- 202.Kiziltepe T, Yan A, Dong M, Jonnalagadda VS, Dedon PC, Engelward BP. Delineation of the chemical pathways underlying nitric oxide-induced homologous recombination in mammalian cells. Chem Biol. 2005;12(3):357–369. doi: 10.1016/j.chembiol.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 203.Yang Q, Dong Y, Wu W, Zhu C, Chong H, Lu J, Yu D, Liu L, Lv F, Wang S. Detection and differential diagnosis of colon cancer by a cumulative analysis of promoter methylation. Nat Commun. 2012;3:1206. doi: 10.1038/ncomms2209. [DOI] [PubMed] [Google Scholar]
- 204.Kriegl L, Neumann J, Vieth M, Greten FR, Reu S, Jung A, Kirchner T. Up and downregulation of p16(Ink4a) expression in BRAF-mutated polyps/adenomas indicates a senescence barrier in the serrated route to colon cancer. Mod Pathol. 2011;24(7):1015–1022. doi: 10.1038/modpathol.2011.43. [DOI] [PubMed] [Google Scholar]
- 205.Wang FY, Arisawa T, Tahara T, Takahama K, Watanabe M, Hirata I, Nakano H. Aberrant DNA methylation in ulcerative colitis without neoplasia. Hepatogastroenterology. 2008;55(81):62–65. [PubMed] [Google Scholar]
- 206.Hsieh CJ, Klump B, Holzmann K, Borchard F, Gregor M, Porschen R. Hypermethylation of the p16INK4a promoter in colectomy specimens of patients with long-standing and extensive ulcerative colitis. Cancer Res. 1998;58(17):3942–3945. [PubMed] [Google Scholar]
- 207.Westbrook AM, Wei B, Braun J, Schiestl RH. Intestinal inflammation induces genotoxicity to extraintestinal tissues and cell types in mice. Int J Cancer. 2011 doi: 10.1002/ijc.26146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Kang MH, Genser D, Elmadfa I. Increased sister chromatid exchanges in peripheral lymphocytes of patients with Crohn's disease. Mutat Res. 1997;381(1):141–148. doi: 10.1016/s0027-5107(97)00161-9. [DOI] [PubMed] [Google Scholar]
- 209.Rabinovitch PS, Dziadon S, Brentnall TA, Emond MJ, Crispin DA, Haggitt RC, Bronner MP. Pancolonic chromosomal instability precedes dysplasia and cancer in ulcerative colitis. Cancer Res. 1999;59(20):5148–5153. [PubMed] [Google Scholar]
- 210.O'Sullivan JN, Bronner MP, Brentnall TA, Finley JC, Shen WT, Emerson S, Emond MJ, Gollahon KA, Moskovitz AH, Crispin DA, et al. Chromosomal instability in ulcerative colitis is related to telomere shortening. Nat Genet. 2002;32(2):280–284. doi: 10.1038/ng989. [DOI] [PubMed] [Google Scholar]
- 211.Risques RA, Lai LA, Himmetoglu C, Ebaee A, Li L, Feng Z, Bronner MP, Al-Lahham B, Kowdley KV, Lindor KD, et al. Ulcerative colitis-associated colorectal cancer arises in a field of short telomeres, senescence, and inflammation. Cancer Res. 2011;71(5):1669–1679. doi: 10.1158/0008-5472.CAN-10-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Risques RA, Lai LA, Brentnall TA, Li L, Feng Z, Gallaher J, Mandelson MT, Potter JD, Bronner MP, Rabinovitch PS. Ulcerative colitis is a disease of accelerated colon aging: evidence from telomere attrition and DNA damage. Gastroenterology. 2008;135(2):410–418. doi: 10.1053/j.gastro.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.von Zglinicki T, Saretzki G, Docke W, Lotze C. Mild hyperoxia shortens telomeres and inhibits proliferation of fibroblasts: a model for senescence? Exp Cell Res. 1995;220(1):186–193. doi: 10.1006/excr.1995.1305. [DOI] [PubMed] [Google Scholar]
- 214.Kohonen-Corish MR, Daniel JJ, te Riele H, Buffinton GD, Dahlstrom JE. Susceptibility of Msh2-deficient mice to inflammation-associated colorectal tumors. Cancer Res. 2002;62(7):2092–2097. [PubMed] [Google Scholar]
- 215.Brentnall TA, Crispin DA, Bronner MP, Cherian SP, Hueffed M, Rabinovitch PS, Rubin CE, Haggitt RC, Boland CR. Microsatellite instability in nonneoplastic mucosa from patients with chronic ulcerative colitis. Cancer Res. 1996;56(6):1237–1240. [PubMed] [Google Scholar]
- 216.Liao J, Seril DN, Lu GG, Zhang M, Toyokuni S, Yang AL, Yang GY. Increased susceptibility of chronic ulcerative colitis-induced carcinoma development in DNA repair enzyme Ogg1 deficient mice. Mol Carcinog. 2008;47(8):638–646. doi: 10.1002/mc.20427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Calvo JA, Meira LB, Lee CY, Moroski-Erkul CA, Abolhassani N, Taghizadeh K, Eichinger LW, Muthupalani S, Nordstrand LM, Klungland A, et al. DNA repair is indispensable for survival after acute inflammation. J Clin Invest. 2012 doi: 10.1172/JCI63338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Hofseth LJ, Khan MA, Ambrose M, Nikolayeva O, Xu-Welliver M, Kartalou M, Hussain SP, Roth RB, Zhou X, Mechanic LE, et al. The adaptive imbalance in base excision-repair enzymes generates microsatellite instability in chronic inflammation. J Clin Invest. 2003;112(12):1887–1894. doi: 10.1172/JCI19757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Mutamba JT, Svilar D, Prasongtanakij S, Wang XH, Lin YC, Dedon PC, Sobol RW, Engelward BP. XRCC1 and base excision repair balance in response to nitric oxide. DNA Repair (Amst) 2011;10(12):1282–1293. doi: 10.1016/j.dnarep.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Machado AM, Figueiredo C, Touati E, Maximo V, Sousa S, Michel V, Carneiro F, Nielsen FC, Seruca R, Rasmussen LJ. Helicobacter pylori infection induces genetic instability of nuclear and mitochondrial DNA in gastric cells. Clin Cancer Res. 2009;15(9):2995–3002. doi: 10.1158/1078-0432.CCR-08-2686. [DOI] [PubMed] [Google Scholar]
- 221.Fleisher AS, Esteller M, Harpaz N, Leytin A, Rashid A, Xu Y, Liang J, Stine OC, Yin J, Zou TT, et al. Microsatellite instability in inflammatory bowel disease-associated neoplastic lesions is associated with hypermethylation and diminished expression of the DNA mismatch repair gene, hMLH1. Cancer Res. 2000;60(17):4864–4868. [PubMed] [Google Scholar]
- 222.Edwards RA, Witherspoon M, Wang K, Afrasiabi K, Pham T, Birnbaumer L, Lipkin SM. Epigenetic repression of DNA mismatch repair by inflammation and hypoxia in inflammatory bowel disease-associated colorectal cancer. Cancer Res. 2009;69(16):6423–6429. doi: 10.1158/0008-5472.CAN-09-1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Graziewicz M, Wink DA, Laval F. Nitric oxide inhibits DNA ligase activity: potential mechanisms for NO-mediated DNA damage. Carcinogenesis. 1996;17(11):2501–2505. doi: 10.1093/carcin/17.11.2501. [DOI] [PubMed] [Google Scholar]
- 224.Laval F, Wink DA. Inhibition by nitric oxide of the repair protein, O6-methylguanine-DNA-methyltransferase. Carcinogenesis. 1994;15(3):443–447. doi: 10.1093/carcin/15.3.443. [DOI] [PubMed] [Google Scholar]
- 225.Sidorkina O, Espey MG, Miranda KM, Wink DA, Laval J. Inhibition of poly(ADP-RIBOSE) polymerase (PARP) by nitric oxide and reactive nitrogen oxide species. Free Radic Biol Med. 2003;35(11):1431–1438. doi: 10.1016/j.freeradbiomed.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 226.Wu X, Takenaka K, Sonoda E, Hochegger H, Kawanishi S, Kawamoto T, Takeda S, Yamazoe M. Critical roles for polymerase zeta in cellular tolerance to nitric oxide-induced DNA damage. Cancer Res. 2006;66(2):748–754. doi: 10.1158/0008-5472.CAN-05-2884. [DOI] [PubMed] [Google Scholar]
- 227.Chang CL, Marra G, Chauhan DP, Ha HT, Chang DK, Ricciardiello L, Randolph A, Carethers JM, Boland CR. Oxidative stress inactivates the human DNA mismatch repair system. Am J Physiol Cell Physiol. 2002;283(1):C148–C154. doi: 10.1152/ajpcell.00422.2001. [DOI] [PubMed] [Google Scholar]
- 228.Kim JJ, Tao H, Carloni E, Leung WK, Graham DY, Sepulveda AR. Helicobacter pylori impairs DNA mismatch repair in gastric epithelial cells. Gastroenterology. 2002;123(2):542–553. doi: 10.1053/gast.2002.34751. [DOI] [PubMed] [Google Scholar]
- 229.Westbrook AM, Schiestl RH. Atm-deficient mice exhibit increased sensitivity to dextran sulfate sodium-induced colitis characterized by elevated DNA damage and persistent immune activation. Cancer Res. 2010;70(5):1875–1884. doi: 10.1158/0008-5472.CAN-09-2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Hofseth LJ, Saito S, Hussain SP, Espey MG, Miranda KM, Araki Y, Jhappan C, Higashimoto Y, He P, Linke SP, et al. Nitric oxide-induced cellular stress and p53 activation in chronic inflammation. Proc Natl Acad Sci U S A. 2003;100(1):143–148. doi: 10.1073/pnas.0237083100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Fujii S, Fujimori T, Kawamata H, Takeda J, Kitajima K, Omotehara F, Kaihara T, Kusaka T, Ichikawa K, Ohkura Y, et al. Development of colonic neoplasia in p53 deficient mice with experimental colitis induced by dextran sulphate sodium. Gut. 2004;53(5):710–716. doi: 10.1136/gut.2003.028779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Yin J, Harpaz N, Tong Y, Huang Y, Laurin J, Greenwald BD, Hontanosas M, Newkirk C, Meltzer SJ. p53 point mutations in dysplastic and cancerous ulcerative colitis lesions. Gastroenterology. 1993;104(6):1633–1639. doi: 10.1016/0016-5085(93)90639-t. [DOI] [PubMed] [Google Scholar]
- 233.Burmer GC, Rabinovitch PS, Haggitt RC, Crispin DA, Brentnall TA, Kolli VR, Stevens AC, Rubin CE. Neoplastic progression in ulcerative colitis: histology, DNA content, and loss of a p53 allele. Gastroenterology. 1992;103(5):1602–1610. doi: 10.1016/0016-5085(92)91184-6. [DOI] [PubMed] [Google Scholar]
- 234.Greenwald BD, Harpaz N, Yin J, Huang Y, Tong Y, Brown VL, McDaniel T, Newkirk C, Resau JH, Meltzer SJ. Loss of heterozygosity affecting the p53, Rb, mcc/apc tumor suppressor gene loci in dysplastic and cancerous ulcerative colitis. Cancer Res. 1992;52(3):741–745. [PubMed] [Google Scholar]
- 235.Brentnall TA, Crispin DA, Rabinovitch PS, Haggitt RC, Rubin CE, Stevens AC, Burmer GC. Mutations in the p53 gene: an early marker of neoplastic progression in ulcerative colitis. Gastroenterology. 1994;107(2):369–378. doi: 10.1016/0016-5085(94)90161-9. [DOI] [PubMed] [Google Scholar]
- 236.Harpaz N, Peck AL, Yin J, Fiel I, Hontanosas M, Tong TR, Laurin JN, Abraham JM, Greenwald BD, Meltzer SJ. p53 protein expression in ulcerative colitis-associated colorectal dysplasia and carcinoma. Hum Pathol. 1994;25(10):1069–1074. doi: 10.1016/0046-8177(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 237.Hussain SP, Amstad P, Raja K, Ambs S, Nagashima M, Bennett WP, Shields PG, Ham AJ, Swenberg JA, Marrogi AJ, et al. Increased p53 mutation load in noncancerous colon tissue from ulcerative colitis: a cancer-prone chronic inflammatory disease. Cancer Res. 2000;60(13):3333–3337. [PubMed] [Google Scholar]
- 238.Zhuang JC, Wright TL, deRojas-Walker T, Tannenbaum SR, Wogan GN. Nitric oxide-induced mutations in the HPRT gene of human lymphoblastoid TK6 cells and in Salmonella typhimurium. Environ Mol Mutagen. 2000;35(1):39–47. doi: 10.1002/(sici)1098-2280(2000)35:1<39::aid-em6>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 239.Li CQ, Trudel LJ, Wogan GN. Nitric oxide-induced genotoxicity, mitochondrial damage, and apoptosis in human lymphoblastoid cells expressing wild-type and mutant p53. Proc Natl Acad Sci U S A. 2002;99(16):10364–10369. doi: 10.1073/pnas.162356399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Nguyen T, Brunson D, Crespi CL, Penman BW, Wishnok JS, Tannenbaum SR. DNA damage and mutation in human cells exposed to nitric oxide in vitro. Proc Natl Acad Sci U S A. 1992;89(7):3030–3034. doi: 10.1073/pnas.89.7.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Kim MY, Lim CH, Trudel LJ, Deen WM, Wogan GN. Delivery method, target gene structure, and growth properties of target cells impact mutagenic responses to reactive nitrogen and oxygen species. Chem Res Toxicol. 2012;25(4):873–883. doi: 10.1021/tx2004882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Sheh A, Lee CW, Masumura K, Rickman BH, Nohmi T, Wogan GN, Fox JG, Schauer DB. Mutagenic potency of Helicobacter pylori in the gastric mucosa of mice is determined by sex and duration of infection. Proc Natl Acad Sci U S A. 2010;107(34):15217–15222. doi: 10.1073/pnas.1009017107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Sato Y, Takahashi S, Kinouchi Y, Shiraki M, Endo K, Matsumura Y, Kakuta Y, Tosa M, Motida A, Abe H, et al. IL-10 deficiency leads to somatic mutations in a model of IBD. Carcinogenesis. 2006;27(5):1068–1073. doi: 10.1093/carcin/bgi327. [DOI] [PubMed] [Google Scholar]
- 244.Redston MS, Papadopoulos N, Caldas C, Kinzler KW, Kern SE. Common occurrence of APC and K-ras gene mutations in the spectrum of colitis-associated neoplasias. Gastroenterology. 1995;108(2):383–392. doi: 10.1016/0016-5085(95)90064-0. [DOI] [PubMed] [Google Scholar]
- 245.Goodman JE, Hofseth LJ, Hussain SP, Harris CC. Nitric oxide and p53 in cancer-prone chronic inflammation and oxyradical overload disease. Environ Mol Mutagen. 2004;44(1):3–9. doi: 10.1002/em.20024. [DOI] [PubMed] [Google Scholar]
- 246.Schwabe RF, Wang TC. Cancer. Bacteria deliver a genotoxic hit. Science. 2012;338(6103):52–53. doi: 10.1126/science.1229905. [DOI] [PubMed] [Google Scholar]
- 247.Grivennikov SI. Inflammation and colorectal cancer: colitis-associated neoplasia. Semin Immunopathol. 2013;35(2):229–244. doi: 10.1007/s00281-012-0352-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Wang X, Yang Y, Moore DR, Nimmo SL, Lightfoot SA, Huycke MM. 4-hydroxy-2-nonenal mediates genotoxicity and bystander effects caused by Enterococcus faecalis-infected macrophages. Gastroenterology. 2012;142(3):543–551. e7. doi: 10.1053/j.gastro.2011.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Huycke MM, Moore D, Joyce W, Wise P, Shepard L, Kotake Y, Gilmore MS. Extracellular superoxide production by Enterococcus faecalis requires demethylmenaquinone and is attenuated by functional terminal quinol oxidases. Mol Microbiol. 2001;42(3):729–740. doi: 10.1046/j.1365-2958.2001.02638.x. [DOI] [PubMed] [Google Scholar]
- 250.Wang X, Huycke MM. Extracellular superoxide production by Enterococcus faecalis promotes chromosomal instability in mammalian cells. Gastroenterology. 2007;132(2):551–561. doi: 10.1053/j.gastro.2006.11.040. [DOI] [PubMed] [Google Scholar]
- 251.Huycke MM, Moore DR. In vivo production of hydroxyl radical by Enterococcus faecalis colonizing the intestinal tract using aromatic hydroxylation. Free Radic Biol Med. 2002;33(6):818–826. doi: 10.1016/s0891-5849(02)00977-2. [DOI] [PubMed] [Google Scholar]
- 252.Cuevas-Ramos G, Petit CR, Marcq I, Boury M, Oswald E, Nougayrede JP. Escherichia coli induces DNA damage in vivo and triggers genomic instability in mammalian cells. Proc Natl Acad Sci U S A. 2010;107(25):11537–11542. doi: 10.1073/pnas.1001261107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Nougayrede JP, Homburg S, Taieb F, Boury M, Brzuszkiewicz E, Gottschalk G, Buchrieser C, Hacker J, Dobrindt U, Oswald E. Escherichia coli induces DNA double-strand breaks in eukaryotic cells. Science. 2006;313(5788):848–851. doi: 10.1126/science.1127059. [DOI] [PubMed] [Google Scholar]
- 254.Ge Z, Rogers AB, Feng Y, Lee A, Xu S, Taylor NS, Fox JG. Bacterial cytolethal distending toxin promotes the development of dysplasia in a model of microbially induced hepatocarcinogenesis. Cell Microbiol. 2007;9(8):2070–2080. doi: 10.1111/j.1462-5822.2007.00939.x. [DOI] [PubMed] [Google Scholar]
- 255.Guidi R, Guerra L, Levi L, Stenerlow B, Fox JG, Josenhans C, Masucci MG, Frisan T. Chronic exposure to the cytolethal distending toxins of Gram-negative bacteria promotes genomic instability and altered DNA damage response. Cell Microbiol. 2013;15(1):98–113. doi: 10.1111/cmi.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Arthur JC, Perez-Chanona E, Muhlbauer M, Tomkovich S, Uronis JM, Fan TJ, Campbell BJ, Abujamel T, Dogan B, Rogers AB, et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science. 2012;338(6103):120–123. doi: 10.1126/science.1224820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Winter SE, Winter MG, Xavier MN, Thiennimitr P, Poon V, Keestra AM, Laughlin RC, Gomez G, Wu J, Lawhon SD, et al. Host-Derived Nitrate Boosts Growth of E. coli in the Inflamed Gut. Science. 2013;339(6120):708–711. doi: 10.1126/science.1232467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Venkatesan BM, Bashir R. Nanopore sensors for nucleic acid analysis. Nat Nanotechnol. 2011;6(10):615–624. doi: 10.1038/nnano.2011.129. [DOI] [PubMed] [Google Scholar]
- 259.Schibel AE, An N, Jin Q, Fleming AM, Burrows CJ, White HS. Nanopore detection of 8-oxo-7,8-dihydro-2'-deoxyguanosine in immobilized single-stranded DNA via adduct formation to the DNA damage site. J Am Chem Soc. 2010;132(51):17992–17995. doi: 10.1021/ja109501x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Korzenik JR, Podolsky DK. Evolving knowledge and therapy of inflammatory bowel disease. Nat Rev Drug Discov. 2006;5(3):197–209. doi: 10.1038/nrd1986. [DOI] [PubMed] [Google Scholar]
- 261.Elson CO, Cong Y, McCracken VJ, Dimmitt RA, Lorenz RG, Weaver CT. Experimental models of inflammatory bowel disease reveal innate, adaptive, and regulatory mechanisms of host dialogue with the microbiota. Immunol Rev. 2005;206:260–276. doi: 10.1111/j.0105-2896.2005.00291.x. [DOI] [PubMed] [Google Scholar]
- 262.Wirtz S, Neurath MF. Mouse models of inflammatory bowel disease. Adv Drug Deliv Rev. 2007;59(11):1073–1083. doi: 10.1016/j.addr.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 263.Westbrook AM, Szakmary A, Schiestl RH. Mechanisms of intestinal inflammation and development of associated cancers: lessons learned from mouse models. Mutat Res. 2010;705(1):40–59. doi: 10.1016/j.mrrev.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Wirtz S, Neufert C, Weigmann B, Neurath MF. Chemically induced mouse models of intestinal inflammation. Nat Protoc. 2007;2(3):541–546. doi: 10.1038/nprot.2007.41. [DOI] [PubMed] [Google Scholar]
- 265.Neufert C, Becker C, Neurath MF. An inducible mouse model of colon carcinogenesis for the analysis of sporadic and inflammation-driven tumor progression. Nat Protoc. 2007;2(8):1998–2004. doi: 10.1038/nprot.2007.279. [DOI] [PubMed] [Google Scholar]
- 266.Kuhn R, Lohler J, Rennick D, Rajewsky K, Muller W. Interleukin-10-deficient mice develop chronic enterocolitis. Cell. 1993;75(2):263–274. doi: 10.1016/0092-8674(93)80068-p. [DOI] [PubMed] [Google Scholar]
- 267.Rennick DM, Fort MM. Lessons from genetically engineered animal models. XII. IL-10-deficient (IL-10(−/−) mice and intestinal inflammation. Am J Physiol Gastrointest Liver Physiol. 2000;278(6):G829–G833. doi: 10.1152/ajpgi.2000.278.6.G829. [DOI] [PubMed] [Google Scholar]
- 268.Dijkstra G, Moshage H, van Dullemen HM, de Jager-Krikken A, Tiebosch AT, Kleibeuker JH, Jansen PL, van Goor H. Expression of nitric oxide synthases and formation of nitrotyrosine and reactive oxygen species in inflammatory bowel disease. J Pathol. 1998;186(4):416–421. doi: 10.1002/(SICI)1096-9896(199812)186:4<416::AID-PATH201>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 269.Godkin AJ, De Belder AJ, Villa L, Wong A, Beesley JE, Kane SP, Martin JF. Expression of nitric oxide synthase in ulcerative colitis. Eur J Clin Invest. 1996;26(10):867–872. doi: 10.1111/j.1365-2362.1996.tb02131.x. [DOI] [PubMed] [Google Scholar]
- 270.Ikeda I, Kasajima T, Ishiyama S, Shimojo T, Takeo Y, Nishikawa T, Kameoka S, Hiroe M, Mitsunaga A. Distribution of inducible nitric oxide synthase in ulcerative colitis. Am J Gastroenterol. 1997;92(8):1339–1341. [PubMed] [Google Scholar]