Abstract
Objective
To examine outcomes associated with dual eligibility (Medicare and Medicaid) of patients who are admitted to skilled nursing facility (SNF) care and whether differences in outcomes are related to states' Medicaid long-term care policies.
Data Sources/Collection
We used national Medicare enrollment data and claims, and the Minimum Data Set for 890,922 community-residing Medicare fee-for-service beneficiaries who were discharged to an SNF from a general hospital between July 2008 and June 2009.
Study Design
We estimated the effect of dual eligibility on the likelihood of 30-day rehospitalization, becoming a long-stay nursing home resident, and 180-day survival while controlling for clinical, demographic, socio-economic, residential neighborhood characteristics, and SNF-fixed effects. We estimated the differences in outcomes by dual eligibility status separately for each state and showed their relationship with state policies: the average Medicaid payment rate; presence of nursing home certificate-of-need (CON) laws; and Medicaid home and community-based services (HCBS) spending.
Principal Findings
Dual-eligible patients are equally likely to experience 30-day rehospitalization, 12 percentage points more likely to become long-stay residents, and 2 percentage points more likely to survive 180 days compared to Medicare-only patients. This longer survival can be attributed to longer nursing home length of stay. While higher HCBS spending reduces the length-of-stay gap without affecting the survival gap, presence of CON laws reduces both the length-of-stay and survival gaps.
Conclusions
Dual eligibles utilize more SNF care and experience higher survival rates than comparable Medicare-only patients. Higher HCBS spending may reduce the longer SNF length of stay of dual eligibles without increasing mortality and may save money for both Medicare and Medicaid.
Keywords: Health economics, long-term care, Medicaid
Utilization and cost of Medicare paid skilled nursing facility (SNF) care provided in a nursing home following an acute care hospitalization have been a major health policy concern. Per capita Medicare fee-for-service spending on SNF care almost doubled over the last decade (Medpac 2012). More important, while only 5 percent of all Medicare expenditures are spent on SNF care (Medpac 2012), about 15 percent of the variation in these expenditures is explained by variation in SNF care services (Institute-of-Medicine 2013). This paper underscores the higher SNF care utilization by patients who are enrolled in both Medicare and Medicaid and referred to herein as “dual eligible.” Compared to other services, dual eligibles disproportionately use SNFs. In 2008, average Medicare spending was about 1.8 times higher and Medicare-supported SNF care was about 2.6 times higher for dual eligibles than for those who were Medicare-only (Medpac 2012). While it is well known that dual eligibles use SNF at a higher rate than their counterparts, there has been little empirical work that examines the causes and implications of longer SNF length of stay for dual-eligible beneficiaries.
The central hypothesis of this paper is that dual-eligible patients have greater incentive to remain at nursing homes for longer periods of time than Medicare-only patients because of the absence of cost sharing and poorer living conditions at home. Nursing home stays beyond 100 days following SNF admission are not covered by Medicare and are typically paid out of pocket by Medicare-only patients until they spend-down their wealth (Liu, Doty, and Manton 1990; Mor, Intrator, and Laliberte 1993; Intrator et al. 1996) and become eligible for Medicaid when Medicaid pays for nursing home care. Additionally, because dual-eligible patients may have poorer living conditions in the community than their counterparts, it is plausible they are more likely to become long-stay nursing home residents. We hypothesize that state Medicaid policies play an important role in reducing the length of nursing home stays of dual-eligible patients primarily because Medicaid is responsible for financing the nursing home care of these patients once they become long-stay residents. We investigate whether three state policies are related to length of stay among dual-eligible beneficiaries: presence of certificate-of-need (CON) legislation, home and community-based services (HCBS) spending, and the average Medicaid payment rate for custodial nursing home care. These policies may also affect patients' long-term health outcomes like survival through the change in nursing home length of stay. These ideas can be summarized by two testable hypotheses:
Dual eligibles are more likely to become long-stay nursing home residents than Medicare-only patients with comparable clinical conditions.
State Medicaid policies aiming to reduce the costs of nursing home care affect the likelihood of becoming a long-stay nursing home resident, 30-day rehospitalization and survival of dual-eligible patients at a higher rate than those of Medicare-only patients.
We tested these hypotheses using a set of community-residing Medicare beneficiaries from the 48 contiguous states who were admitted to a nursing home for Medicare paid SNF care following an acute hospital stay.
Conceptual Framework
We examined three outcomes following SNF admission: 30-day rehospitalization, becoming a long-stay nursing home resident, and 180-day survival. There are several differences between dual-eligible and Medicare-only patients that may affect relative differences between these two groups in terms of both length of stay in a nursing home following SNF care and health outcomes.
First, current coverage policies for nursing home care do not provide dual-eligible beneficiaries any incentive to reduce SNF length of stay. Medicare pays a predetermined price for 100 days following SNF admission. Any stay beyond 20 days involves copayment (of $139 per day in 2010), which is typically covered by supplemental insurance (Medigap) for Medicare-only patients and by Medicaid for dual-eligible patients. However, for any stay beyond 100 days, Medicare-only patients pay out-of-pocket and Medicaid pays for dual-eligible patients. Thus, Medicare-only patients have a strong economic incentive to go back to community in timely manner.
Second, studies have also documented differences in living conditions between dual-eligible and Medicare-only patients. Dual-eligible beneficiaries are more likely to live alone (Howell et al. 2007; Cai, Salmon, and Rodgers 2009; Martikainen et al. 2009; Kelly et al. 2010) and have lower socio-economic status (Martikainen et al. 2009), lower household's net worth (Kelly et al. 2010), higher dissatisfaction with living conditions at home (Howell et al. 2007), and lower rates of home ownership (Cai, Salmon, and Rodgers 2009).
Third, dual eligibles are more likely to have poorer health status (Howell et al. 2007; Cai, Salmon, and Rodgers 2009; Martikainen et al. 2009; Kelly et al. 2010). Such difference in health status is likely to contribute to the difference in nursing home length of stay.
Fourth, there is a substantial difference in nursing homes treating dual-eligible and Medicare-only patients (Rahman et al. 2014), which is likely to have important effects on outcomes. Dual eligibles are treated in relatively poor-quality SNFs for two reasons: residential neighborhood and insurance status. SNFs near high-poverty neighborhoods typically provide lower quality care (Feng et al. 2011). As distance plays an important role in one's choice of SNF (Zwanziger, Mukamel, and Indridason 2002; Shugarman and Brown 2006; Grabowski et al. 2013; Rahman et al. 2013), dual eligibles are more likely to be treated in low-quality SNFs. In addition, dual eligibles are admitted to nursing homes with fewer nursing staff and greater proportions of Medicaid paid residents compared to Medicare-only patients from the same neighborhood and treating hospital (Rahman et al. 2014).
We estimated the difference in outcomes between dual-eligible and Medicare-only patients after controlling for a rich set of clinical conditions based on qualifying hospitalization claims and SNF admission assessments; demographic attributes like age, race, and marital status; socio-economic characteristics like education, poverty rate, and per capita income of the patient's residential neighborhood; and SNF-fixed effects. We argue that the estimated differences are attributable to nonhealth factors, which include cost sharing and the living situation of the person. As 30-day rehospitalization should not be affected by cost sharing and living arrangements at home, significant estimated differences in this outcome imply unobserved gaps in health status and thus serves as a falsification test. On the other hand, 180-day survival is likely to be affected by living arrangements at home and length of the SNF stay.
In terms of state policies, CON legislation was one of the earliest efforts to address the escalating cost of health care services and requires that to enter the market or to expand an existing facility, nursing homes must obtain permission from a government health service planning agency. A series of studies in the 1980s and 1990s showed that the presence of CON laws reduced the growth in the number of nursing home beds (Swan and Harrington 1990; Zinn 1994; Harrington et al. 1997) and resulted in excess demand (Nyman 1988, 1989, 1994). However, the nursing home occupancy rate has dropped progressively since the late 1980s, and all the studies during the 1990s and 2000s concluded that CON policies may no longer be as important in constraining the growth of nursing home market (Nyman 1993; Grabowski 2001a; Grabowski, Ohsfeldt, and Morrisey 2003). However, using nursing home level data, the occupancy rate in CON states is about 2 percentage points higher than in non-CON states (84 percent vs 82 percent in 2008) (see Figure2a). Similarly, as can be verified from county level Area Resource File data, nursing home bed supply per 65+ age population is about 5 percent lower in CON states (see Figure2b). Given that the nursing home bed supply in a CON state is restricted, we hypothesize that nursing homes are not as likely to keep dual eligibles for as long time as they would if more beds were available.
Figure 2.
Plot of Estimated Dual-Eligible-Medicare-Only Differences in 180-Day Survival in Different States onto Estimated Dual-Eligible-Medicare-Only Differences in Rate of Becoming Long-Stay Nursing Home Resident
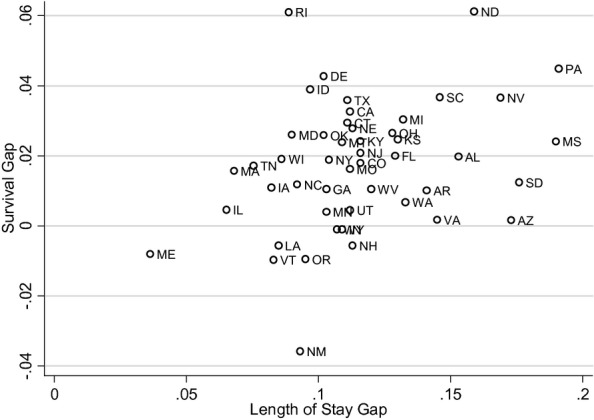
Note. Estimated equation of survival gap onto length-of-stay gap and rehospitalization gap is: Survival group= –0.002[0.25]+0.191[3.13] *; length-of-stay gap –0.034[0.20] *;rehospitalizationgap.
States vary greatly in their support for HCBS, which are intended to help disabled seniors live in the community. Differences in the proportion of Medicaid spending on HCBS have been shown to be related to differences in patients' behavior. Specifically, higher HCBS spending is related to a decreased likelihood of nursing home admission (Burr, Mutchler, and Pilcher-Warren 2002; Muramatsu et al. 2007), the proportion of residents in nursing homes with low-care needs (Hahn et al. 2011; Thomas and Mor 2013), and the proportion of people who are able to die at home and avoid institutionalization (Muramatsu et al. 2008). As dual eligibles typically have worse living arrangements at home than Medicare-only patients, we hypothesize that states that spend more on their HCBS will have a smaller length of nursing home stay gap between dual-eligible and Medicare-only patients.
Differences in Medicaid payment rates across states affect how attractive to a nursing home a Medicaid paid patient is relative to a Medicare or a private pay patient. Previous studies indicate that higher Medicaid payment rates are associated with lower rates of hospitalization (Intrator and Mor 2004; Intrator et al. 2007), higher staffing ratios (Harrington, Swan, and Carrillo 2007), and better quality of care (Grabowski 2001b; Grabowski, Angelelli, and Mor 2004). We hypothesize that higher Medicaid payment rates will increase the likelihood of dual-eligible patients becoming long-stay residents at a higher rate than Medicare-only patients.
Methods
Data
Data for these analyses come from three individual-level datasets: the nursing home Resident Assessment Instrument Minimum Data Set (MDS), Medicare Part A claims (for hospital and SNF care), and Medicare enrollment data. Applying the Residential History File (RHF) methodology (Intrator et al. 2011), we concatenate MDS assessments and Medicare claims into individual beneficiary histories that allow us to track individuals' daily medical service utilization. Additionally, we matched these data to zip-code-level census aggregates for the year 2000.
Sample
Using the RHF, we identified all Medicare fee-for-service beneficiaries who were discharged from a general inpatient hospital and admitted to an SNF between July 1, 2008 and June 30, 2009. We excluded individuals who had a nursing home stay during the 12 months prior to their qualifying SNF admission. These patients are not only more likely to be dual eligible because of their long-term care use but also have a high probability of returning to nursing homes to become long-stay residents. We also excluded patients who were under age 65 at the time of SNF admission. Finally, we used the residential zip code obtained from the Medicare enrollment data to merge with census-based aggregates. Our final sample consisted of 890,922 Medicare fee-for-service beneficiaries with complete data residing in the contiguous 48 states.
Outcome Variables
Our three binary outcome variables include (1) within 30-day rehospitalization; (2) becoming a long-stay nursing home resident; and (3) 180-day survival. Using the RHF, we followed each patient for 180 days from the day of SNF admission to calculate these outcome variables. The 30-day rehospitalization indicates whether the patient had at least one acute hospitalization within 30 days of SNF admission. Rehospitalization is a sign of dysfunction in the continuity of care and is widely used as a health outcome in the public health literature (Jencks, Williams, and Coleman 2009; Mor et al. 2010; Rahman, Zinn, and Mor 2013; Rahman et al. 2013). Becoming a long-stay nursing home resident is defined as whether the patient remained at the nursing home for more than 100 days. We identified whether a patient was at the nursing home or not on each day during the 180 days following SNF admission using the RHF and calculated nursing home length of stay. Previous research has utilized 90 cut-off to indicate that an SNF patient has become a long-stay nursing home resident (Lau et al. 2005), whereas others have identified long-stay residents by the presence of a quarterly MDS assessment for that patient (Intrator, Zinn, and Mor 2004). We used a 100-day length of stay to identify long-stay residents because this is the number of days Medicare will cover for a SNF stay. A 180-day survival indicates whether a patient survived for at least 180 days following SNF admission.
Explanatory Variables
The main variable of interest is a patient's dual eligibility status. We followed (Rahman et al. 2014) to define a patient as dually eligible if s/he was Medicaid-eligible for at least one of the 6 months before SNF admission. Those who spent down (i.e., became Medicaid eligible) following the SNF admission were not considered dual eligible for the purpose of this study because such change in dual eligibility affected SNF stay.
We obtained age, gender, race, and residential zip code from the Medicare enrollment file. We used four zip-code-level variables obtained from the 2000 U.S. Census, including per capita income, poverty rate among the 65 and older population, percent black, and percent of the population living in rural areas. Clinical variables obtained from the claims data included Elixhauser (Elixhauser et al. 1998) and Deyo (Deyo, Cherkin, and Ciol 1992) comorbidity indices, hospital and intensive care unit (ICU) length of stay, and an indicator of home health care use prior to the qualifying hospital admission. Clinical variables from the MDS included several diagnosis indicators, the number of medications taken in the last 7 days, activity of daily living scale (Morris, Sherwood, and Mor 1984), cognitive performance scale (Morris et al. 1994), and resource utilization group (5.12). We included marital status and educational attainment from MDS assessments as well. Some 17 percent of the individuals in our cohort had missing education on the MDS assessments, so we used a dummy variable to indicate missing education data.
Our three main independent state policy variables were (1) presence of CON legislation; (2) long-term care spending on Home and Community Based Services (HCBS-a sum of total expenditures on home health, personal care services, Aged and Disabled Waivers, 1915c Waivers, 1115 Waivers and 1915J Waivers) per capita (Thomas and Mor 2013); and (3) the average Medicaid per-diem payment rate. We also included indicators of a case mix-based payment system, Medicaid bed-hold policy, and the fraction of the dual-eligible patients calculated from our sample to control for correlation across state policies and difference in poverty rates across the states.
Analysis
To estimate the difference in outcomes between dual-eligible and Medicare-only patients, we estimated the statistical model described by equation (1).
| 1 |
Here, Yins is the outcome of patient i treated in nursing home n located in state s. DEi indicated dual eligibility of patient i. Xi represents the vector of control variables. θn represents nursing home-fixed effects. β captures the difference in outcome by dual eligibility status. As we were interested in the difference in the likelihood of a certain outcome between dual-eligible and Medicare-only patients, we estimated the above equations using a linear probability model that yields the marginal effects directly. A nonlinear model like logit does not allow us to calculate the marginal effects in the presence of fixed effects.
We estimated the (β) for all three outcomes separately for all 48 states using the above model. We plot the gaps in likelihood of becoming long-stay resident using maps to show the regional variation. We also plotted survival gap against length-of-stay gap to examine whether the survival gap is partially attributable to longer nursing home stay. Finally, we examined the relationship between estimated gaps (β) in different outcomes and state policy variables. We estimated these state-level equations using number of patients in our sample in corresponding states as weights.
Sensitivity Analysis
Given that dual-eligible and Medicare-only patients are observably quite different, we also performed our statistical analysis using a subset of patients who are observably similar (i.e., have similar propensity score of being dual eligible). We estimated the propensity score of being dual eligible using all the clinical, demographic, and residential neighborhood characteristics and SNF-fixed effects using a logit model. We used the nearest neighbor matching method to identify the Medicare-only patients who are comparable to dual-eligible patients. We also plotted the outcomes with respect to the propensity score separately for dual-eligible and Medicare-only patients.
While examining the role of state policies, we estimated differences in outcomes for each state and examined how these differences are related to state policies. Here, we allowed control variables in equation (1) to have different estimated parameters in different states. However, if we assume that the effect of control variables is the same in all the states, we can estimate the effect of state policies on differences in outcomes between dual-eligible and Medicare-only patients adding interactions of state policy variables with dual eligibility dummy in equation (1). We estimated these models using both the entire sample and propensity score-matched sample (results are presented in the Appendix).
Results
Table1 shows the demographic and clinical characteristics separately for dual-eligible and Medicare-only beneficiaries in our sample. About 19 percent of the patients in our sample were Medicaid eligible before their qualifying SNF admission. On average, dual-eligible beneficiaries were younger but had higher acuity. They are more likely to belong to a minority group and to reside in low-income and rural neighborhoods. Dual-eligible beneficiaries have much lower educational attainment as well. Medicare-only beneficiaries are two times more likely to be married than dual eligibles. Diabetes and mental illnesses are noticeably more prevalent among the dual eligibles. The only two diagnoses that are less prevalent among duals are hip fracture and cancer.
Table 1.
Descriptive Statistics of the Patients
| Nondual | Dual | |
|---|---|---|
| N = 720,551 (80.88%) | N = 170,371 (19.12%) | |
| Mean (SD) or % | Mean (SD) or % | |
| Demographic characteristics | ||
| Age | 81.75 (7.63) | 79.84 (8.33) |
| Female | 64.2 | 72.5 |
| Black | 5.0 | 16.3 |
| Other races than black or white | 1.5 | 10.0 |
| Married | 38.4 | 18.2 |
| Education missing | 17.7 | 15.2 |
| High school graduate | 38.7 | 33.9 |
| More than high school education | 29.0 | 13.3 |
| Neighborhood zip code characteristics | ||
| Percentage of age 65+ population black | 6.08 (13.50) | 11.01 (19.91) |
| Per capita income | 23,484 (9,581) | 19,533 (7,658) |
| Percentage of age 65+ population poor | 8.50 (5.51) | 12.27 (7.81) |
| Percentage of population in rural area | 21.95 (31.84) | 26.02 (34.98) |
| Clinical characteristics from claims | ||
| Days of ICU use in last hospital stay | 1.68 (3.63) | 1.86 (4.15) |
| Length of stay of last hospital stay | 8.86 (7.05) | 9.72 (7.48) |
| Any home health use before last hospital stay | 14.4 | 21.3 |
| Deyo index >1 | 40.8 | 48.6 |
| Elix-hauser >2 | 49.7 | 53.3 |
| Clinical characteristics from MDS | ||
| Diabetes mellitus | 27.8 | 38.2 |
| Congestive heart failure | 19.9 | 23.4 |
| Hip fracture | 9.3 | 7.8 |
| Alzheimer | 3.7 | 4.4 |
| Cerebrovascular accident (stroke) | 11.5 | 15.0 |
| Dementia other than Alzheimer | 11.5 | 13.7 |
| Bipolar disease | 0.8 | 1.5 |
| Schizophrenia | 0.3 | 1.7 |
| Emphysema/COPD | 18.5 | 24.5 |
| Cancer | 7.5 | 6.5 |
| Number of meds in last 7 days at admission | 12.06 (4.76) | 12.12 (4.92) |
| Morris additive ADL scale (0–28) at admission | 16.30 (5.36) | 16.99 (5.76) |
| CPS scale, Fries/Morris 92 at admission | 1.26 (1.51) | 1.60 (1.62) |
| RUG-III grouped into 7 categories | 6.09 (1.81) | 5.98 (1.87) |
Table2 presents the difference between dual-eligible and Medicare-only patients in terms of three outcomes. Based on the unadjusted rates, a dual-eligible patient is about 16 percentage points more likely to stay in SNF for more than 100 days, 2 percentage points more likely to be rehospitalized within 30 days, and 0.4 percentage points less likely to survive 180 days following SNF admission. After controlling for observed characteristics, dual-eligible patients have the same likelihood of 30-day rehospitalization as their Medicare-only counterparts, are 12 percentage points more likely to become a long-stay resident, and 2 percentage points more likely to survive 180 days. These differences are the same when estimated from a subsample of patients matched by propensity score.
Table 2.
Estimated Difference in Outcomes by Dual Eligibility
| Any Rehospitalization within 30 Days of SNF Admission | Stayed at Nursing Home for More Than 100 Days | Survived at Least 180 Days Since SNF Admission | |
|---|---|---|---|
| Unadjusted rates | |||
| Medicare only | 0.174 | 0.146 | 0.784 |
| Dual eligible | 0.193 | 0.303 | 0.780 |
| Difference | 0.019 | 0.157 | −0.004 |
| Adjusted difference after controlling for | |||
| Individual and neighborhood variables | 0.004 [3.52]*** | 0.121 [75.85]*** | 0.0158 [12.93]*** |
| Individual and neighborhood variables and SNF-fixed effects | 0.002 [1.75]* | 0.112 [75.27]*** | 0.0195 [15.93]*** |
Note. Robust t-statistics, which are obtained clustering errors by nursing homes, have been reported in square brackets.
p < .01
p < 0.1.
We estimated the same model separately for each state and presented the adjusted difference in likelihood of becoming a long-stay resident (i.e., the length-of-stay gap) in Figure1. In all states, duals have a higher likelihood of becoming a long-stay resident. However, the sizes of the estimated difference vary widely; the lowest difference is in Maine (4.1 percentage points), while the highest is in Mississippi (19.5 percentage points). Estimated length-of-stay gaps are lower in New England and North Central states compared to the rest of the county.
Figure 1.
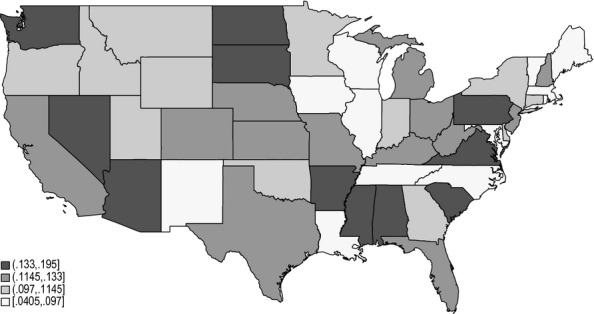
Adjusted Difference between Dual Eligibles and Other Medicare Beneficiaries in Likelihood of Becoming Long-Stay Nursing Home Resident Note. To obtain the adjusted difference, for each state, we estimated linear probability model with all the characteristics listed in Table1 and nursing facility-fixed effects.
Figure2 plots estimated the survival gap with respect to the estimated length-of-stay gap by state. It shows whether dual-eligible beneficiaries enjoyed additional survival relative to Medicare-only patients in the states where dual beneficiaries stayed at a nursing home for relatively longer periods of time. We indeed see positive correlation between the length-of-stay gap and the survival gap. We did not find any correlation between the rehospitalization gap and the survival gap.
Table3 presents the effect of state policies on differences in outcomes between dual-eligible and Medicare-only patients. The results show that state policies do not affect rehospitalization among the two types of patients differently. However, all the policies affect the likelihood of dual eligibles becoming long-stay nursing home residents differently compared to the Medicare-only patients. The difference in likelihood of becoming a long-stay resident between dual-eligible and Medicare-only patients is about 2 percentage points lower in states with CON legislation, increases about 0.4 percentage points with a $10 (1.1 percentage points with a one standard deviation) increase in the Medicaid payment rate, and decreases about 0.2 percentage points with a $10 (one percentage points with a one standard deviation) increase in HCBS spending per enrollee. This table also shows that the survival gap between Medicare-only and dual-eligible patients was slightly smaller in states with CON laws. These patterns are roughly the same when we use estimated them directly using state policy and dual eligibility interaction terms in equation (1) or with subsample of patients matched by propensity score of being dual eligible (Table S1).
Table 3.
Effects of State Policies on within State Gap in Outcomes between Dual-Eligible and Medicare-Only Patients
| (1) 30-Day Rehospitalization Gap | (2) Gap in Likelihood of Becoming Long-Stay Resident | (3) 180-Day Survival Gap | |
|---|---|---|---|
| Certificate of need | 0.00148 [0.436] | −0.0247 [−2.714]*** | −0.0106 [−2.373]** |
| Medicaid payment rate (change by $10) | −0.000964 [−1.468] | 0.00380 [2.166]** | 0.00102 [1.178] |
| HCBS spending per enrollee (change by $10) | 0.000629 [1.807]* | −0.00196 [−2.107]** | −0.000242 [−0.528] |
| Case mix payment policy | 2.73e-05 [0.00830] | −0.00655 [−0.746] | −0.00460 [−1.065] |
| Fraction of patients dual eligible | 0.0421 [1.630] | −0.0957 [−1.386] | −0.00502 [−0.148] |
| Medicaid bed-hold policy | 0.00294 [0.693] | −0.00809 [−0.713] | 0.000552 [0.0987] |
| Constant | −0.000813 [−0.0687] | 0.117 [3.682]*** | 0.0172 [1.103] |
| Observations | 48 | 48 | 48 |
| R-squared | 0.219 | 0.325 | 0.166 |
Note. t-statistics in brackets.
p < 0.01
p < 0.05
p < 0.1.
Discussion
This study explored differences in discharge outcomes between dual-eligible and Medicare-only beneficiaries. Although dual-eligible patients were found to be about 12 percentage points (i.e., about 1.8 times) more likely to become long-stay residents and 2 percentage points less likely to die within 180 days of SNF admission, we found no discernible difference in health outcomes, such as hospital readmission, between these two groups. Our analyses showed that health conditions, residential neighborhood characteristics, and the treating nursing facility explained most of the observed difference in rehospitalization between dual-eligible and Medicare-only patients, but only a very small fraction of such observed difference in the likelihood of becoming a long-stay nursing home resident. Our findings are among the first to provide evidence that dual-eligible patients are remaining in nursing homes following postacute care at higher rates and have lower mortality than Medicare-only patients.
The lack of differences in rehospitalization between the two groups, particularly in light of their substantial case mix acuity differences, suggests that the dual-eligible patients' greater likelihood of getting “stuck” in a nursing home is primarily due to nonclinical factors. We would suggest that the absence of cost-sharing and income-related factors, including perhaps less favorable environments at home, acts as the key forces behind the increased use of long-term nursing home care among dual eligibles. However, we also conclude that lower mortality among dual-eligible patients is attributable to longer nursing home length of stay.
This article clearly demonstrates that Medicaid policies can be used to reduce the longer nursing home length of stay among dual-eligible individuals. Although previous studies concluded that CON laws are not effective because of the falling occupancy rates in nursing facilities (Grabowski, Ohsfeldt, and Morrisey 2003), we found that CON laws reduced the length-of-stay gap between dual-eligible and Medicare-only patients. However, the survival gap between dual-eligible and Medicare-only patients was smaller in states with CON laws. We think that the smaller length-of-stay gap in CON states is due to constrained nursing home bed supply. We also noted that the likelihood of becoming a long-stay nursing home resident is smaller in CON states for both dual-eligible and Medicare-only patients. Unlike CON laws, increased HCBS by states reduced the length-of-stay gap without affecting the mortality. This result suggests that nursing home care can be substituted by home-based care to some extent and that the expansion of home and community-based care programs could save money for both Medicare and Medicaid. Our results imply that higher Medicaid payment rate increases the length of stay of dual eligibles compared to Medicare-only patients. This is the first paper, to the best of our knowledge, that shows an unintended consequence of higher payment rate, which may actually encourage nursing homes to keep patients for a relatively longer time.
A key limitation of this study is that we cannot identify the effect of dual eligibility and rather estimate the difference between two groups of patients. Because we do not have detailed data on income or living arrangements in the community, estimation of the effect of dual eligibility on patient outcomes requires a random assignment of dual eligibility or a quasi-experimental setup, which is beyond the scope of this paper. Another key limitation is that we focused on individuals who were discharged to SNFs, thereby ignoring the role of other types of postacute care settings such as inpatient rehabilitation facilities, long-term care hospitals, and support from home health agencies. Given that dual-eligible patients are not randomly distributed across different postacute care settings (Kane et al. 1996) and different postacute care settings have different lengths of stay (Kane et al. 2000), our results are not generalizable to the population who receive postacute care in a setting other than an SNF. The final limitation is that our study considers only SNF patients who were dual eligible before SNF admission. A nondual in our sample could have become dual eligible after paying SNF copayments. This phenomenon is called spend-down (Liu and Manton 1989; Liu, Doty, and Manton 1990; Adams, Meiners, and Burwell 1993) and has been treated as an outcome of nursing home use. Our findings suggest that such spend-down may have its own effect on further use of nursing home care. Further research is needed to address this issue.
This study explores the role of state Medicaid policies on nursing home length of stay and health outcomes of dual-eligible Medicare beneficiaries. Compared to Medicare-only counterparts, dual eligibles are equally likely to be rehospitalized but are more likely to remain in the nursing home for long-term care after their SNF coverage has ended and less likely to die within 6 months of SNF admission. However, the differences in likelihood of becoming long-stay were reduced in states with CON laws and more spending on home and community-based services. In addition, in states with greater spending on HCBS, shorter nursing homes stays were not accompanied by increased mortality. Therefore, spending on HCBS has the potential to reduce spending in the Medicare and Medicaid programs without negatively affecting patient survival. Future research should further explore this finding.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the National Institute of Aging grants P01AG027296 (PI: Vincent Mor).
Disclosures: None.
Disclaimers: None.
Supporting Information
Appendix SA1: Author Matrix.
Figure S1: Polynomial Regression of Outcomes onto Propensity Score of Being Dual Eligible Separately for Dual-Eligible and Medicare-Only Population.
Figure S2: Box Plot of Occupancy Rates in Nursing Homes by States' Certificate-of-Need (CON) Legislation.
Table S1: Effects of State Policies on Differential Outcomes between Dual-Eligible and Medicare-Only Patients.
References
- Adams EK, Meiners MR. Burwell BO. Asset Spend-Down in Nursing Homes. Methods and Insights. Medical Care. 1993;31(1):1–23. doi: 10.1097/00005650-199301000-00001. [DOI] [PubMed] [Google Scholar]
- Cai Q, Salmon JW. Rodgers ME. Factors Associated with Long-Stay Nursing Home Admissions among the U.S. Elderly Population: Comparison of Logistic Regression and the Cox Proportional Hazards Model with Policy Implications for Social Work. Social Work in Health Care. 2009;48(2):154–68. doi: 10.1080/00981380802580588. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Cherkin DC. Ciol MA. Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases. Journal of Clinical Epidemiology. 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR. Coffey RM. Comorbidity Measures for Use with Administrative Data. Medical Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Feng Z, Lepore M, Clark MA, Tyler D, Smith DB, Mor V. Fennell ML. Geographic Concentration and Correlates of Nursing Home Closures: 1999-2008. Archives of Internal Medicine. 2011;171(9):806–13. doi: 10.1001/archinternmed.2010.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC. Does an Increase in the Medicaid Reimbursement Rate Improve Nursing Home Quality? Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2001a;56(2):S84–93. doi: 10.1093/geronb/56.2.s84. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. Medicaid Reimbursement and the Quality of Nursing Home Care. Journal of Health Economics. 2001b;20(4):549–69. doi: 10.1016/s0167-6296(01)00083-2. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Angelelli JJ. Mor V. Medicaid Payment and Risk-Adjusted Nursing Home Quality Measures. Health Affairs (Millwood) 2004;23(5):243–52. doi: 10.1377/hlthaff.23.5.243. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Ohsfeldt RL. Morrisey MA. The Effects of CON Repeal on Medicaid Nursing Home and Long-Term Care Expenditures. Inquiry. 2003;40(2):146–57. doi: 10.5034/inquiryjrnl_40.2.146. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Feng Z, Hirth R, Rahman M. Mor V. Effect of Nursing Home Ownership on the Quality of Post-Acute Care: An Instrumental Variables Approach. Journal of Health Economics. 2013;32(1):12–21. doi: 10.1016/j.jhealeco.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn EA, Thomas KS, Hyer K, Andel R. Meng H. Predictors of Low-Care Prevalence in Florida Nursing Homes: The Role of Medicaid Waiver Programs. Gerontologist. 2011;51(4):495–503. doi: 10.1093/geront/gnr020. [DOI] [PubMed] [Google Scholar]
- Harrington C, Swan JH. Carrillo H. Nurse Staffing Levels and Medicaid Reimbursement Rates in Nursing Facilities. Health Services Research. 2007;42(3 Pt 1):1105–29. doi: 10.1111/j.1475-6773.2006.00641.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C, Swan JH, Nyman JA. Carrillo H. The Effect of Certificate of Need and Moratoria Policy on Change in Nursing Home Beds in the United States. Medical Care. 1997;35(6):574–88. doi: 10.1097/00005650-199706000-00004. [DOI] [PubMed] [Google Scholar]
- Howell S, Silberberg M, Quinn WV. Lucas JA. Determinants of Remaining in the Community after Discharge: Results from New Jersey's Nursing Home Transition Program. Gerontologist. 2007;47(4):535–47. doi: 10.1093/geront/47.4.535. [DOI] [PubMed] [Google Scholar]
- Institute-of-Medicine. Interim Report of the Committee on Geographic Variation in Health Care Spending and Promotion of High-Value Care: Preliminary Committee Observations. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- Intrator O. Mor V. Effect of State Medicaid Reimbursement Rates on Hospitalizations from Nursing Homes. Journal of the American Geriatrics Society. 2004;52(3):393–8. doi: 10.1111/j.1532-5415.2004.52111.x. [DOI] [PubMed] [Google Scholar]
- Intrator O, Zinn J. Mor V. Nursing Home Characteristics and Potentially Preventable Hospitalizations of Long-Stay Residents. Journal of the American Geriatrics Society. 2004;52(10):1730–6. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- Intrator O, Mor V, Hines MA, Lancaster T, Laliberte LL. Freiberger W. Effect of the Medicare Catastrophic Coverage Act on Payer Source Changes among Nursing Home Residents. Inquiry. 1996;33(1):42–52. [PubMed] [Google Scholar]
- Intrator O, Grabowski DC, Zinn J, Schleinitz M, Feng Z, Miller S. Mor V. Hospitalization of Nursing Home Residents: The Effects of States' Medicaid Payment and Bed-Hold Policies. Health Services Research. 2007;42(4):1651–71. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O, Hiris J, Berg K, Miller SC. Mor V. The Residential History File: Studying Nursing Home Residents' Long-Term Care Histories. Health Services Research. 2011;46(1):120–37. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks SF, Williams MV. Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. New England Journal of Medicine. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Kane RL, Finch M, Blewett L, Chen Q, Burns R. Moskowitz M. Use of Post-Hospital Care by Medicare Patients. Journal of the American Geriatrics Society. 1996;44(3):242–50. doi: 10.1111/j.1532-5415.1996.tb00909.x. [DOI] [PubMed] [Google Scholar]
- Kane RL, Chen Q, Finch M, Blewett L, Burns R. Moskowitz M. The Optimal Outcomes of Post-Hospital Care under Medicare. Health Services Research. 2000;35(3):615–61. [PMC free article] [PubMed] [Google Scholar]
- Kelly A, Conell-Price J, Covinsky K, Cenzer IS, Chang A, Boscardin WJ. Smith AK. Length of Stay for Older Adults Residing in Nursing Homes at the End of Life. Journal of the American Geriatrics Society. 2010;58(9):1701–6. doi: 10.1111/j.1532-5415.2010.03005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau DT, Kasper JD, Potter DE, Lyles A. Bennett RG. Hospitalization and Death Associated with Potentially Inappropriate Medication Prescriptions among Elderly Nursing Home Residents. Archives of Internal Medicine. 2005;165(1):68–74. doi: 10.1001/archinte.165.1.68. [DOI] [PubMed] [Google Scholar]
- Liu K, Doty P. Manton K. Medicaid Spenddown in Nursing Homes. Gerontologist. 1990;30(1):7–15. doi: 10.1093/geront/30.1.7. [DOI] [PubMed] [Google Scholar]
- Liu K. Manton KG. The Effect of Nursing Home Use on Medicaid Eligibility. Gerontologist. 1989;29(1):59–66. doi: 10.1093/geront/29.1.59. [DOI] [PubMed] [Google Scholar]
- Martikainen P, Moustgaard H, Murphy M, Einio EK, Koskinen S, Martelin T. Noro A. Gender, Living Arrangements, and Social Circumstances as Determinants of Entry Into and Exit from Long-Term Institutional Care at Older Ages: A 6-Year Follow-Up Study of Older Finns. Gerontologist. 2009;49(1):34–45. doi: 10.1093/geront/gnp013. [DOI] [PubMed] [Google Scholar]
- Medpac. A Data Book: Health Care Spending and the Medicare Program. Washington, DC: Medicare Payment Advisory Committee; 2012. [Google Scholar]
- Mor V, Intrator O. Laliberte L. Factors Affecting Conversion Rates to Medicaid among New Admissions to Nursing Homes. Health Services Research. 1993;28(1):1–25. [PMC free article] [PubMed] [Google Scholar]
- Mor V, Intrator O, Feng Z. Grabowski DC. The Revolving Door of Rehospitalization from Skilled Nursing Facilities. Health Affairs (Millwood) 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Sherwood S. Mor V. An Assessment Tool for Use in Identifying Functionally Vulnerable Persons in the Community. Gerontologist. 1984;24(4):373–9. doi: 10.1093/geront/24.4.373. [DOI] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V. Lipsitz LA. MDS Cognitive Performance Scale. Journal of Gerontology. 1994;49(4):M174–82. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- Muramatsu N, Yin H, Campbell RT, Hoyem RL, Jacob MA. Ross CO. Risk of Nursing Home Admission among Older Americans: Does States' Spending on Home- and Community-Based Services Matter? Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2007;62(3):S169–78. doi: 10.1093/geronb/62.3.s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muramatsu N, Hoyem RL, Yin HJ. Campbell RT. Place of Death among Older Americans — Does State Spending on Home- and Community-Based Services Promote Home Death? Medical Care. 2008;46(8):829–38. doi: 10.1097/MLR.0b013e3181791a79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyman JA. Excess-Demand, the Percentage of Medicaid Patients, and the Quality of Nursing-Home Care. Journal of Human Resources. 1988;23(1):76–92. [Google Scholar]
- Nyman JA. Analysis of Nursing-Home Use and Bed Supply — Wisconsin, 1983. Health Services Research. 1989;24(4):511–37. [PMC free article] [PubMed] [Google Scholar]
- Nyman JA. Testing for Excess Demand in Nursing Home Care Markets. Medical Care. 1993;31(8):680–93. doi: 10.1097/00005650-199308000-00002. [DOI] [PubMed] [Google Scholar]
- Nyman JA. The Effects of Market Concentration and Excess-Demand on the Price of Nursing-Home Care. Journal of Industrial Economics. 1994;42(2):193–204. [Google Scholar]
- Rahman M, Zinn JS. Mor V. The Impact of Hospital-Based Skilled Nursing Facility Closures on Rehospitalizations. Health Services Research. 2013;28:499–518. doi: 10.1111/1475-6773.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M, Foster AD, Grabowski DC, Zinn JS. Mor V. Effect of Hospital-SNF Referral Linkages on Rehospitalization. Health Services Research. 2013;48:1898–1919. doi: 10.1111/1475-6773.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M, Grabowski DC, Gozalo PL, Thomas KS. Mor V. Are Dual Eligibles Admitted to Poorer Quality Skilled Nursing Facilities? Health Services Research. 2014;29:798–817. doi: 10.1111/1475-6773.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shugarman LR. Brown JA. Nursing Home Selection: How Do Consumers Choose? Volume I: Findings from Focus Groups of Consumers and Information Intermediaries. Washington, DC: Prepared for Office of Disability, Aging and Long-Term Care Policy, Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2006. Contract #HHS-100-03-0023. [Google Scholar]
- Swan J. Harrington C. Certificate of Need and Nursing Home Bed Capacity in States. Journal of Health and Social Policy. 1990;2(2):87–105. doi: 10.1300/j045v02n02_06. [DOI] [PubMed] [Google Scholar]
- Thomas KS. Mor V. The Relationship between Older Americans Act Title III State Expenditures and Prevalence of Low-Care Nursing Home Residents. Health Services Research. 2013;48(3):1215–26. doi: 10.1111/1475-6773.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinn JS. Market Competition and the Quality of Nursing-Home Care. Journal of Health Politics Policy and Law. 1994;19(3):555–82. doi: 10.1215/03616878-19-3-555. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Mukamel DB. Indridason I. Use of Resident-Origin Data to Define Nursing Home Market Boundaries. Inquiry. 2002;39(1):56–66. doi: 10.5034/inquiryjrnl_39.1.56. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Figure S1: Polynomial Regression of Outcomes onto Propensity Score of Being Dual Eligible Separately for Dual-Eligible and Medicare-Only Population.
Figure S2: Box Plot of Occupancy Rates in Nursing Homes by States' Certificate-of-Need (CON) Legislation.
Table S1: Effects of State Policies on Differential Outcomes between Dual-Eligible and Medicare-Only Patients.


