Abstract
There is much to be learned from falls-related research outside the field of multiple sclerosis (MS), as well as from work within the MS field but not specific to falls or falls prevention. This article describes three examples of such bodies of work that have potential to broaden approaches to falls-prevention research: 1) sensory components of postural control among older adults, 2) lessons learned from physical activity promotion among people with spinal cord injury (SCI), and 3) aging among people with MS. Age-related deterioration in visual, vestibular, and somatosensory systems or in sensory integration can adversely affect postural control and can contribute to falls in older people. Sensory-specific interventions designed for improving balance in older people could be adapted for preventing falls in individuals with MS. Spinal Cord Injury (SCI) Action Canada's strategy for disseminating physical activity promotion interventions for adults with SCI has been successful and widely accepted by community partners. Many of the peer-based interventions developed by SCI Action Canada are potentially relevant and could be adapted to the MS population for both physical activity promotion and falls prevention. Considering that older people with MS constitute a growing proportion of the MS population and over 70% of older people with MS report moderate to extreme balance problems, falls prevention should be one of the key components, particularly for MS management in older or more disabled groups. Overall, given people's different ages, symptoms, strengths, and barriers, a tailored MS falls-prevention intervention that includes peer/caregiver support is critical.
Accidental and injurious falls are not unique to people with multiple sclerosis (MS), nor are the efforts to understand and reduce them. It is well accepted that falls are multifactorial1,2 as well as preventable.2,3 Preventing falls requires knowledge of modifiable risks and the ability to apply theory-driven strategies to change them. In 2012, Gillespie and colleagues4 included 159 randomized controlled trials in a Cochrane review focused on examining the effects of interventions to reduce the incidence of falls among community-dwelling older adults. Interventions included in the review attempted to compensate for or remediate physical impairments (eg, weakness, visual problems), environmental barriers, and psychosocial factors. The volume of evidence is less for populations with chronic conditions (eg, stroke,5 Parkinson's disease6). Consequently, there is much to be learned from falls-related research done outside of MS as well as from work within the MS field but not specific to falls or falls prevention. Therefore, the initial session of the inaugural meeting of the International MS Falls Prevention Research Network, which took place on March 3, 2014, at Queen's University, Kingston, Ontario, Canada, sought to highlight research from other areas of investigation that could be brought to bear in the development of an MS falls-prevention intervention protocol.
While research from a number of fields could be drawn on to inform the development of an MS falls-prevention protocol, three specific topics are addressed in this article: 1) sensory components of postural control among older adults, 2) exercise interventions for people with spinal cord injury, and 3) aging among people with MS. Balance was highlighted because one of the most commonly identified risk factors for falls in older adults is impaired balance.7 Balance is subserved by efficient postural control mechanisms. The topic of postural control among older adults was identified by the meeting planners as important and relevant to the Network's discussions because people with MS have well-documented challenges with postural control.8 While understanding of postural control among people with MS is growing, awareness of the current state of knowledge about older adults has the potential to drive new insights into falls among people with MS.
The topic of physical activity was highlighted because activity-based approaches are a common component of falls-prevention interventions for people with MS. Physical activity can help people with MS improve their balance and strength, impairments of which are associated with accidental falls. Research establishing the benefits of physical activity for people with MS is burgeoning.9,10 However, there are still gaps in research aiming to identify effective methods for broadly disseminating evidence-based physical activity interventions. Strategies to address these gaps are also relevant to falls prevention. To extend knowledge and generate new ideas specific to preventing falls among people with MS, the topic of physical activity interventions for people with disabilities, specifically the systematic approach to physical activity promotion established by Spinal Cord Injury (SCI) Action Canada,11 was identified by the meeting planners as important and relevant to the Network's discussions.
Finally, aging was considered an important topic for discussion because the broader literature on falls and falls prevention is dominated by studies of older adults. This is not the case in the MS literature, in which study participants have ranged in age from their 20s to over 90. Nevertheless, the meeting planners recognized that aging and age-related concerns are important factors to consider when developing an MS falls-prevention intervention and protocol. Therefore, research on aging with MS was included in the discussions.
Understanding the Underlying Sensory Components of Postural Control Among Older Adults
Three systems—namely, the visual, vestibular, and somatosensory systems—collectively contribute sensory information required for precise and accurate postural control.
Vision
Dependence on visual information for postural control increases with increasing age.12 However, age-related changes in the visual system result in a decline of visual acuity, contrast sensitivity, depth perception, visual field, and adaptation.13 Visual impairment, measured as well as self-reported, is strongly associated with the risk of falling among older persons,14 and this relationship is stronger for falls in outdoor environments.15 Although reduced visual acuity has been associated with falls, reduced contrast sensitivity and depth perception are more important vision-related risk factors for falls, recurrent falls, and fall-related hip fractures in older individuals.13
Vestibular System
Decline in vestibular function correlates well with decline in balance in older people.16 The incidence of falls is almost double in older adults with bilateral vestibular hypofunction compared with age-matched controls.17 Further, almost three-quarters of the older idiopathic fallers referred for fall risk assessment have quantitative evidence of either peripheral or central vestibular system hypofunction.18 Significantly diminished vestibulo-ocular reflex has been recorded in older fallers with hip fracture.19 It is possible that age-related degradation of central and peripheral vestibular pathways plays a role in age-related decline in balance and contributes to falls.
Somatosensory System
Age-related deficits have been demonstrated in various aspects of lower-limb somatosensation, including cutaneous (touch, vibration)20,21 and proprioceptive (joint position and motion) sensitivity.22,23 Older people with poor overall somatosensory function are more likely to report multiple (two or more) falls.24 Several studies have used a peripheral neuropathy model to demonstrate a relationship between lower-limb somatosensory function and falls in older people. However, impaired lower-limb tactile acuity,25 vibrotactile sensitivity, and proprioception in older adults are associated with increased falls26 independent of overt peripheral neuropathy.
Sensory Integration
The visual, vestibular, and somatosensory systems provide complementary information and thus help to eliminate ambiguity arising from individual sensory inputs.27 The central nervous system (CNS) processes multiple sensory inputs concurrently and modulates (up- or down-regulates) the central gain of the sensory systems depending on the relevance and reliability of the sensory information, the task, and the environment.28 Therefore, the accuracy of the information received from the three sensory systems as well as the ability of the CNS to appropriately weigh and integrate these inputs depending on the task and the environment is key for adequate postural control.29 The ability to reweight sensory information is particularly important when the sensory context for postural control changes owing to changes in the environment (eg, walking from a well-lit corridor to a dimly lit carpeted room) and/or changes in the availability of sensory information to the individual (eg, normal vs. cataract-related visual impairment vs. peripheral neuropathy–related somatosensory impairment).28
Although older adults can prevent a loss of balance with manipulation of two of the three sensory systems, those with a history of falls have difficulty even when one sensory input is manipulated.30 Those with a history of multiple falls have particular difficulty compensating for conflicting visual information.31 In addition, the proportion of participants who lose balance in the most challenging balance conditions (ie, inaccurate visual and lower-limb somatosensory information) decreases significantly with repeated trials in nonfallers and single fallers but not in multiple fallers.32 These results indicate that multiple fallers fail to learn even when repeatedly exposed to conflicting sensory conditions.
With increasing age, the ability to reintegrate sensory information, once it becomes available, also deteriorates (eg, longer time delays, higher attentional demands)33 and creates imbalance in the weight assignment of the CNS.34 However, it is not known if these differences are more pronounced in older fallers compared with nonfallers.
Sensory-specific exercise interventions have long been designed and implemented to improve sensory integration for postural control in the general older population.35 Such interventions can decrease unnecessary high gains of visual and somatosensory systems under challenging sensory conditions36 and reduce delay in reintegration of sensory information.23 These have proven effective for improving measured as well as self-reported balance in older individuals and may also reduce falls.37
Relevance to MS
Research has shown that people with MS often have problems with postural control, which likely contributes to their heightened risk of falls.8 Studies of standing posture have shown that compared with healthy controls, people with MS evoke delayed automatic postural responses in response to perturbations.38 Deficits in postural control in people with MS can have multifactorial etiology (eg, motor or cognitive deficits, fatigue, depression) and may differ from one person to the next. However, recent studies highlight the slowed somatosensory conduction and impaired central integration as primary causes.38,39 The adverse effects of MS on people's visual and vestibular systems40 may reduce the redundancy available in sensory information and further accentuate the impact of impaired central integration. Encouraging results from a recent study41 indicate that sensory integration training may improve postural control in people with MS. Future studies are warranted to rigorously examine the utility of sensory-specific interventions for reducing falls and fall risk in patients with MS.
Developing and Disseminating Physical Activity Interventions for People with Disability
Learning from Example: Promoting Physical Activity Among Adults with Spinal Cord Injury
Similar to adults with MS, most adults with SCI are inactive. Recognizing the need for comprehensive intervention, SCI Action Canada was founded (a full description is available in Ginis et al.42). SCI Action Canada is a partnership of 15 international researchers and 16 provincial and national community-based organizations. Its mission is to develop and mobilize strategies that will inform, teach, and enable people living with SCI to initiate and maintain a physically active lifestyle. The organization's activities were guided by five established principles for translating evidence-based interventions into practice43: 1) what research evidence should be transferred, 2) who is the target audience, 3) who are the key messengers, 4) what are the preferred methods for dissemination, and 5) what are the effects of dissemination. Some of the seminal activities of the partnership are summarized below (detailed information is available in the cited articles).
Principle 1: Select the Evidence. A series of cross-sectional and prospective cohort studies were conducted to identify key behavioral determinants.44 Task and barrier self-efficacy (ie, confidence to perform physical activity and overcome barriers), goal-setting, and planning emerged as key theoretical determinants. A series of interventions to target these determinants were pilot tested.45
1) Active Homes45: A certified personal trainer and a peer visited the home of participants with paraplegia to conduct an introductory strength training session. During the session, peers demonstrated a series of strength training exercises using an elastic resistance band. This pre-post pilot intervention resulted in significant increases in the amount of strength training participants engaged in 1 month after the visit.
2) Brief Action Planning46: Peer mentors with SCI from a community partner organization attended a 4-hour training session introducing principles of brief action planning as a strategy to promote physical activity to their mentees. Brief action planning is a client-centered counseling style that aims to encourage clients to set a clear plan for attaining a goal behavior. Follow-up evaluations 2 to 4 weeks after the intervention revealed that the peer mentors had acquired many of the critical skills necessary to counsel mentees.
Principle 2: Identify the Target Audience. The target audience for each intervention aligned with the priority of our community partners. Two key audiences were targeted: adults with SCI and health professionals.47
Principle 3: Identify Key Messengers. A scoping review48 and a series of focus groups49 were conducted. Health professionals, community-based service organizations, and particularly peers emerged as preferred sources of physical activity information.
Principle 4: Identify Preferred Methods. Preferred methods of dissemination were identified in the scoping review48 and focus groups.49 Direct interpersonal communication (ie, a conversation), online resources, and print media were identified as preferred channels of dissemination. Because the interventions were disseminated in collaboration with community partners, the method of dissemination used for each intervention was determined largely by community partners' ongoing programming and resource availability.
Principle 5: Evaluate the Effects of Dissemination. All SCI Action Canada activities were monitored using metrics from the RE-AIM framework (Reach, Efficacy, Adoption, Implementation, and Maintenance)—a tool for evaluating the impact of putting evidence-based interventions into practice.50
As a result of this systematic approach, SCI Action Canada has been successful in broadly disseminating its evidence-based programs, initiatives, and resources across Canada. Moreover, owing to the collaborative nature of the partnership, the resulting interventions have been widely accepted and implemented by community partners.50
Promoting Physical Activity for Adults with MS: What We Know So Far
Using SCI Action Canada's approach as a model, researchers have begun to apply the principles for promoting physical activity for adults with MS. Key theory-based determinants of behavior have been identified, including task and barrier self-efficacy, goal-setting, and planning.51 Through a series of qualitative interviews, health-care professionals, community-based organizations (ie, the MS Society of Canada), and peers have been identified as key messengers.52 Interestingly, these theoretical determinants and key messengers are the same as those for adults with SCI. Although there is overlap, conducting these preliminary investigations within the MS population was important in acknowledging the unique (or not so unique) characteristics and needs of the MS population and creating acceptance of the findings by end users (eg, people with MS and community partners). With the key determinants and messengers identified, researchers and practitioners should now move forward to develop, test, and disseminate interventions that target these key determinants and that can be delivered by preferred messengers. Many of the peer-based interventions developed by SCI Action Canada are potentially relevant and could easily be adapted to the MS population for both physical activity promotion and falls prevention. Stakeholders (eg, people living with MS) should be engaged in the process of adapting this model and the intervention approaches described to optimize acceptability to the population.
Research on Aging and Older Adults with Multiple Sclerosis
Older people with MS constitute a growing proportion of the MS population53; however, little is known about aging with MS or factors that affect successful aging with MS. In order to describe healthy aging from the perspective of the older person with MS, researchers interviewed 18 people who were 55 years of age and older with symptoms for 20 or more years.54,55 Analysis of key themes emerging from the data showed that older people with MS highly valued four major factors that they felt contributed to health and life satisfaction as they aged54: work and social engagement, effective and accessible health care, healthy lifestyle habits, and maintaining independence at home.
Work and Social Engagement. Participants strived to maintain their societal roles in which they felt they were making a contribution to others. For example, one participant was extremely distressed when he had to retire prematurely owing to his mobility problems.
Effective and Accessible Health Care. Access to trusted health-care providers with expertise in MS care was highly valued among participants. Conversational communication in which the health-care provider listened attentively rather than “informing” or “telling” was believed to be critical in obtaining effective health care.
Healthy Lifestyle Habits. Many participants described deliberate strategies to maintain a healthy body, including low-fat diets, supplements, and physical activity practices.
Maintaining Independence at Home. Participants felt distressed when they had to rely on others to provide personal care. The ability to complete activities of daily living (eg, bathing, toileting) independently was a critical ingredient to perception of health and satisfaction with life.
Researchers observed that people who viewed their aging as successful also had some common characteristics or beliefs that appeared fundamental to achieving their goals of healthy aging. These included resilience, mental health, financial flexibility, and social support.
Resilience. Participants described instances that suggested they were able to adapt successfully to change. They overcame challenges or obstacles using strategies such as activity modification but rarely activity avoidance.
Mental Health. Absence of depression or cognitive impairment seemed important to the participant's views on health and successful aging. People experiencing depression viewed their situation and their quality of life as poor whether they were physically disabled or not.
Financial Flexibility. Older people with MS who described themselves as financially challenged were more concerned with basic living needs such as housing, food, and transportation. Those who were more financially flexible focused more on health and social outlets that provided enjoyment.
Social Support. Those participants who seemed to be more successful in meeting their healthy aging goals described a strong social support network.
Fall Circumstances Vary Depending on Disability
Based on clinical experience throughout the continuum of care and findings from qualitative research,54–56 we know that fall circumstances change as one ages with MS and depend on mobility level55 (Figure 1). During interviews with older people with MS, participants did not identify themselves as “fallers” or “at risk,” and they often viewed falls as both “routine” (“I fall all the time”) and yet “unexpected.” Using a qualitative research approach, researchers found that study participants, despite reporting problems with balance and falls, did not wish to use walking aids or wheelchairs.55 They explained that using these devices had two drawbacks from their points of view: first, canes, walkers, and wheelchairs were perceived as clear signs of disability that attracted sometimes unwanted attention from others; second, they considered the use of devices to be a sign of “giving up” or accommodating to MS. Participants felt that by using mobility aids, they would sacrifice potentially beneficial exercise effects of unaided (but often unsteady) walking on their balance and leg strength. Many participants described switching to a new gait aid reluctantly after a fall, sometimes at the insistence of concerned family members.
Figure 1.
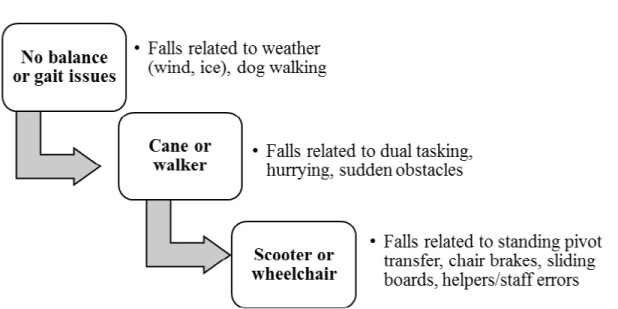
Reasons for falls in multiple sclerosis change over time
The Impact of Balance Problems Among Older People with MS
It is intuitive to think that safety in balance and mobility and lack of falls are integral to healthy aging with MS. However, there is little research examining the relationship between falls, balance, and health among older people with MS or people with higher degrees of MS-related disability. Grounded by qualitative findings, Ploughman and colleagues56 conducted the largest survey of health, lifestyle, and aging with MS in Canada. They recruited older people with MS (≥55 years of age) with symptoms for at least 20 years. Through Canadian MS clinics, MS Society chapters, and newspapers, 921 people were contacted and 743 surveys were returned.56 Participants ranged in age from 55 to 88 years, with a mean (±SD) age of 64.6 (±6.2) years and a mean duration of MS symptoms of 32.9 (±9.5) years. Although the researchers did not specifically ask participants about falls, survey respondents were asked about the extent of their balance problems (29-item Multiple Sclerosis Impact Scale, Question 22),57 their independence in activities of daily living (Barthel Index),58 and health-related quality of life (visual analogue scale). Over 70% of the sample reported moderate to extreme problems with balance (Figure 2). Severity of balance problems was inversely correlated with Barthel Index score (Pearson correlation −0.46, P < .0001; Figure 3) and with perceived health-related quality of life (using a 100-mm visual analogue scale; Pearson correlation −0.33, P < .0001; Figure 4).
Figure 2.
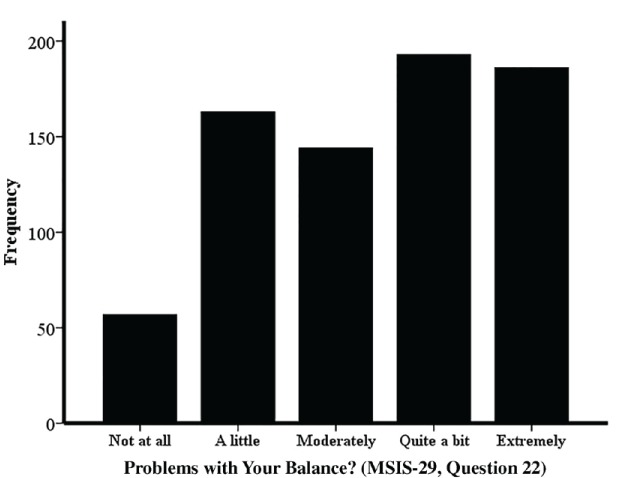
Balance problems among older people with multiple sclerosis
MSIS-29, 29-item Multiple Sclerosis Impact Scale.
Figure 3.
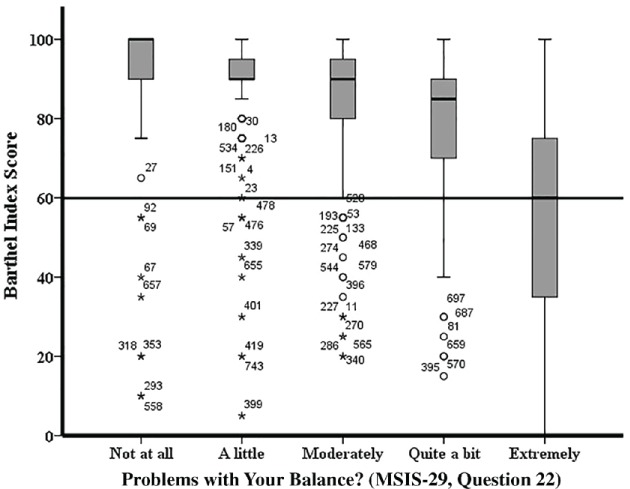
Relationship between balance difficulties and degree of disability measured with the Barthel Index
The reference line indicates the Barthel Index score cutoff; scores below 60 indicate severe dependence in activities of daily living. Note that participants with Barthel Index scores below 60 (indicating severe dependence) reported the full range of balance problem severity from “not at all” to “extremely.” MSIS-29, 29-item Multiple Sclerosis Impact Scale.
Figure 4.
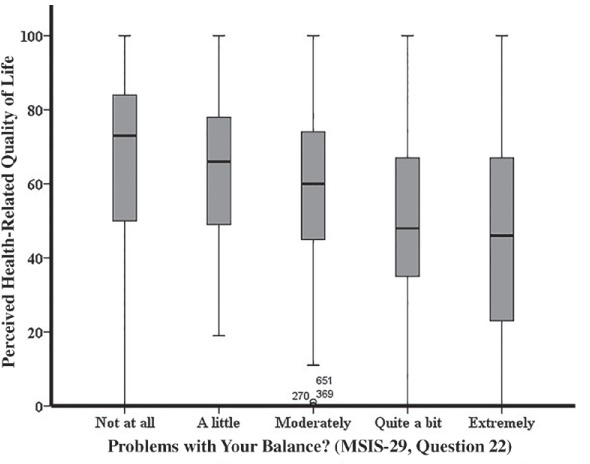
Relationship between reported balance problems and perceived health status
MSIS-29, 29-item Multiple Sclerosis Impact Scale.
Discussion
Upon the conclusion of the related knowledge presentations, the meeting participants were asked to consider the following question: “What is the most important message from these presentations for our MS falls-prevention intervention?” The key points that were raised during the discussion period were as follows:
Any MS falls-prevention intervention will need to help people understand their bodies better and enhance their ability to use compensatory strategies.
Falls-prevention interventions may need to look different for middle-aged and older adults with MS compared with younger groups.
People with MS can attend clinical services only for limited time periods, so falls-prevention interventions that include peer mentoring or caregiver support are worth considering. Promoting long-term changes in behavior that facilitate a more active lifestyle is also an important factor.
Finding ways to tailor an MS falls-prevention intervention will be important given people's different symptoms, strengths (eg, resilience, mental health, social support), and barriers.
Ensuring that the intervention has lasting effects will require careful consideration of a guiding theoretical framework.
Conclusion
This article has presented research and perspectives on three discrete topics that each contribute to the understanding of preventing falls in people with MS. The information gleaned will inform the content and delivery of a falls-prevention intervention designed by the International MS Falls Prevention Research Network.
PracticePoints.
The central nervous system simultaneously integrates visual, vestibular, and sensorimotor information to precisely control balance. Age-related changes in these systems are associated with increased risk of falls.
People with MS are less active than their peers without MS. Research suggests that behavioral determinants of physical activity among people with MS are similar to those among people with other types of disability such as spinal cord injury; self-efficacy to overcome barriers, goal-setting, and planning are key determinants of physical activity.
Most older adults with MS report moderate to severe balance problems, which are associated with higher levels of disability and poorer quality of life.
Acknowledgments
The authors thank Chelsea Harris for assistance with references for this article.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose. Dr. Finlayson is a member of the editorial board of the IJMSC.
Funding/Support: This work was supported, in part, by a Canadian Institutes of Health Research Planning Grant (Funding Reference Number 129594).
References
- 1.Finlayson ML, Peterson EW. Falls, aging, and disability. Phys Med Rehabil Clin N Am. 2010;21:357–373. doi: 10.1016/j.pmr.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Lord SR. Falls in Older People: Risk Factors and Strategies for Prevention. 2nd ed. New York, NY: Cambridge University Press; 2007. [Google Scholar]
- 3.Nutt JG, Horak FB, Bloem BR. Milestones in gait, balance, and falling. Mov Disord. 2011;26:1166–1174. doi: 10.1002/mds.23588. [DOI] [PubMed] [Google Scholar]
- 4.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verheyden GS, Weerdesteyn V, Pickering RM et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev. 2013;5:CD008728. doi: 10.1002/14651858.CD008728.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allen NE, Sherrington C, Paul SS, Canning CG. Balance and falls in Parkinson's disease: a meta-analysis of the effect of exercise and motor training. Mov Disord. 2011;26:1605–1615. doi: 10.1002/mds.23790. [DOI] [PubMed] [Google Scholar]
- 7.Muir SW, Berg K, Chesworth B, Klar N, Speechley M. Quantifying the magnitude of risk for balance impairment on falls in community-dwelling older adults: a systematic review and meta-analysis. J Clin Epidemiol. 2010;63:389–406. doi: 10.1016/j.jclinepi.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Cameron MH, Lord S. Postural control in multiple sclerosis: implications for fall prevention. Curr Neurol Neurosci Rep. 2010;10:407–412. doi: 10.1007/s11910-010-0128-0. [DOI] [PubMed] [Google Scholar]
- 9.Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Nat Rev Neurol. 2012;8:487–497. doi: 10.1038/nrneurol.2012.136. [DOI] [PubMed] [Google Scholar]
- 10.Latimer-Cheung AE, Pilutti LA, Hicks AL et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94:1800–1828.e3. doi: 10.1016/j.apmr.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 11.SCI Action Canada. SCI Action Canada Web site. www.sciactioncanada.ca. Accessed July 23, 2014.
- 12.Anand V, Buckley JG, Scally A, Elliott DB. Postural stability changes in the elderly with cataract simulation and refractive blur. Invest Ophthalmol Vis Sci. 2003;44:4670–4675. doi: 10.1167/iovs.03-0455. [DOI] [PubMed] [Google Scholar]
- 13.Lord SR. Visual risk factors for falls in older people. Age Ageing. 2006;35(suppl 2):ii42–ii45. doi: 10.1093/ageing/afl085. [DOI] [PubMed] [Google Scholar]
- 14.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297:77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 15.Bergland A, Jarnlo GB, Laake K. Predictors of falls in the elderly by location. Aging Clin Exp Res. 2003;15:43–50. doi: 10.1007/BF03324479. [DOI] [PubMed] [Google Scholar]
- 16.Kerber KA, Ishiyama GP, Baloh RW. A longitudinal study of oculomotor function in normal older people. Neurobiol Aging. 2006;27:1346–1353. doi: 10.1016/j.neurobiolaging.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 17.Herdman SJ, Blatt P, Schubert MC, Tusa RJ. Falls in patients with vestibular deficits. Am J Otol. 2000;21:847–851. [PubMed] [Google Scholar]
- 18.Jacobson GP, McCaslin DL, Grantham SL, Piker EG. Significant vestibular system impairment is common in a cohort of elderly patients referred for assessment of falls risk. J Am Acad Audiol. 2008;19:799–807. doi: 10.3766/jaaa.19.10.7. [DOI] [PubMed] [Google Scholar]
- 19.Zur O, Carmeli E, Himellfarb M, Berner YN. [Vestibular function, falls and hip fracture in elderly—a relationship study] Harefuah. 2004;143:197–202. 246. [PubMed] [Google Scholar]
- 20.van Vliet D, Novak CB, Mackinnon SE. Duration of contact time alters cutaneous pressure threshold measurements. Ann Plast Surg. 1993;31:335–339. doi: 10.1097/00000637-199310000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Deshpande N, Metter EJ, Ling S, Conwit R, Ferrucci L. Physiological correlates of age-related decline in vibrotactile sensitivity. Neurobiol Aging. 2008;29:765–773. doi: 10.1016/j.neurobiolaging.2006.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deshpande N, Connelly DM, Culham EG, Costigan PA. Reliability and validity of ankle proprioceptive measures. Arch Phys Med Rehabil. 2003;84:883–889. doi: 10.1016/s0003-9993(03)00016-9. [DOI] [PubMed] [Google Scholar]
- 23.Westlake KP, Culham EG. Sensory-specific balance training in older adults: effect on proprioceptive reintegration and cognitive demands. Phys Ther. 2007;87:1274–1283. doi: 10.2522/ptj.20060263. [DOI] [PubMed] [Google Scholar]
- 24.Deshpande N, Metter EJ, Ferrucci L. Validity of clinically derived cumulative somatosensory impairment index. Arch Phys Med Rehabil. 2010;91:226–232. doi: 10.1016/j.apmr.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Melzer I, Benjuya N, Kaplanski J. Postural stability in the elderly: a comparison between fallers and non-fallers. Age Ageing. 2004;33:602–607. doi: 10.1093/ageing/afh218. [DOI] [PubMed] [Google Scholar]
- 26.Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42:1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 27.Shumway-Cook A, Woollacott MH. Motor Control—Translating Research into Clinical Practice. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 28.Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(suppl 2):ii7–ii11. doi: 10.1093/ageing/afl077. [DOI] [PubMed] [Google Scholar]
- 29.Woollacott JMaM. Posture and Equilibrium. 2nd ed. London, UK: Arnold Publishers; 2004. [Google Scholar]
- 30.Shumway-Cook A, Woollacott M. Attentional demands and postural control: the effect of sensory context. J Gerontol A Biol Sci Med Sci. 2000;55:M10–16. doi: 10.1093/gerona/55.1.m10. [DOI] [PubMed] [Google Scholar]
- 31.Mujdeci B, Aksoy S, Atas A. Evaluation of balance in fallers and non-fallers elderly. Braz J Otorhinolaryngol. 2012;78:104–109. doi: 10.5935/1808-8694.20120016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buatois S, Gueguen R, Gauchard GC, Benetos A, Perrin PP. Posturography and risk of recurrent falls in healthy non-institutionalized persons aged over 65. Gerontology. 2006;52:345–352. doi: 10.1159/000094983. [DOI] [PubMed] [Google Scholar]
- 33.Teasdale N, Simoneau M. Attentional demands for postural control: the effects of aging and sensory reintegration. Gait Posture. 2001;14:203–210. doi: 10.1016/s0966-6362(01)00134-5. [DOI] [PubMed] [Google Scholar]
- 34.Peterka RJ, Loughlin PJ. Dynamic regulation of sensorimotor integration in human postural control. J Neurophysiol. 2004;91:410–423. doi: 10.1152/jn.00516.2003. [DOI] [PubMed] [Google Scholar]
- 35.Hu MH, Woollacott MH. Multisensory training of standing balance in older adults: I. Postural stability and one-leg stance balance. J Gerontol. 1994;49:M52–61. doi: 10.1093/geronj/49.2.m52. [DOI] [PubMed] [Google Scholar]
- 36.Allison LK, Kiemel T, Jeka JJ. Multisensory reweighting of vision and touch is intact in healthy and fall-prone older adults. Exp Brain Res. 2006;175:342–352. doi: 10.1007/s00221-006-0559-7. [DOI] [PubMed] [Google Scholar]
- 37.Kristinsdottir EK, Baldursdottir B. Effect of multi-sensory balance training for unsteady elderly people: pilot study of the “Reykjavik model.”. Disabil Rehabil. 2014;36:1211–1218. doi: 10.3109/09638288.2013.835452. [DOI] [PubMed] [Google Scholar]
- 38.Cameron MH, Horak FB, Herndon RR, Bourdette D. Imbalance in multiple sclerosis: a result of slowed spinal somatosensory conduction. Somatosens Mot Res. 2008;25:113–122. doi: 10.1080/08990220802131127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nelson SR, Di Fabio RP, Anderson JH. Vestibular and sensory interaction deficits assessed by dynamic platform posturography in patients with multiple sclerosis. Ann Otol Rhinol Laryngol. 1995;104:62–68. doi: 10.1177/000348949510400110. [DOI] [PubMed] [Google Scholar]
- 40.Bermel RA, Balcer LJ. Optic neuritis and the evaluation of visual impairment in multiple sclerosis. Continuum (Minneap Minn) 2013;19(4 Multiple Sclerosis):1074–1086. doi: 10.1212/01.CON.0000433282.00221.7e. [DOI] [PubMed] [Google Scholar]
- 41.Gandolfi M, Geroin C, Picelli A et al. Robot-assisted vs. sensory integration training in treating gait and balance dysfunctions in patients with multiple sclerosis: a randomized controlled trial. Front Hum Neurosci. 2014;8:318. doi: 10.3389/fnhum.2014.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ginis KA, Latimer-Cheung A, Corkum S et al. A case study of a community-university multidisciplinary partnership approach to increasing physical activity participation among people with spinal cord injury. Transl Behav Med. 2012;2:516–522. doi: 10.1007/s13142-012-0157-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lavis JN, Robertson D, Woodside JM, McLeod CB, Abelson J. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q. 2003;81:221–248. 171–172. doi: 10.1111/1468-0009.t01-1-00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ginis KA, Tomasone JR, Latimer-Cheung AE, Arbour-Nicitopoulos KP, Bassett-Gunter RL, Wolfe DL. Developing physical activity interventions for adults with spinal cord injury. Part 1: a comparison of social cognitions across actors, intenders, and nonintenders. Rehabil Psychol. 2013;58:299–306. doi: 10.1037/a0032815. [DOI] [PubMed] [Google Scholar]
- 45.Latimer-Cheung AE, Arbour-Nicitopoulos KP, Brawley LR et al. Developing physical activity interventions for adults with spinal cord injury. Part 2: motivational counseling and peer-mediated interventions for people intending to be active. Rehabil Psychol. 2013;58:307–315. doi: 10.1037/a0032816. [DOI] [PubMed] [Google Scholar]
- 46.Gainforth HL, Latimer-Cheung AE, Davis C, Casemore S, Martin Ginis KA. Testing the feasibility of training peers with a spinal cord injury to learn and implement brief action planning to promote physical activity to people with spinal cord injury. J Spinal Cord Injury Med. doi: 10.1179/2045772314Y.0000000239. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tomasone JR, Martin Ginis KA, Estabrooks PA, Domenicucci L. ‘Changing minds’: determining the effectiveness and key ingredients of an educational intervention to enhance healthcare professionals' intentions to prescribe physical activity to patients with physical disabilities. Implement Sci. 2014;9:30. doi: 10.1186/1748-5908-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Faulkner G, Gorczynski P, Arbour KP, Letts L, Wolfe D, Martin Ginis KA. Messengers and methods of disseminating health information among individuals with spinal cord injury: a scoping review. In: Berkovsky TC, editor. Handbook of Spinal Cord Injuries. Hauppauge, NY: Nova Science Publishers, Inc; 2010. pp. 349–374. [Google Scholar]
- 49.Letts L, Martin Ginis KA, Faulkner G, Colquhoun H, Levac D, Gorczynski P. Preferred methods and messengers for delivering physical activity information to people with spinal cord injury: a focus group study. Rehabil Psychol. 2011;56:128–137. doi: 10.1037/a0023624. [DOI] [PubMed] [Google Scholar]
- 50.Sweet SN, Latimer-Cheung AE, Bourne C, Ginis KA. Assessing the research use and needs of organizations promoting healthy living for adults with disabilities. Transl Behav Med. 2014;4:86–94. doi: 10.1007/s13142-013-0231-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shirazipour CH, Motl RW, Martin Ginis KA, Latimer-Cheung AE. A systematic review of qualitative studies examining psychosocial constructs associated with physical activity participation. Ann Behav Med. doi: 10.1016/j.apmr.2017.01.027. (in press) [DOI] [PubMed] [Google Scholar]
- 52.Sweet SN, Perrier MJ, Podzyhun C, Latimer-Cheung AE. Identifying physical activity information needs and preferred methods of delivery of people with multiple sclerosis. Disabil Rehabil. 2013;35:2056–2063. doi: 10.3109/09638288.2013.800915. [DOI] [PubMed] [Google Scholar]
- 53.Marrie RA, Yu N, Blanchard J, Leung S, Elliott L. The rising prevalence and changing age distribution of multiple sclerosis in Manitoba. Neurology. 2010;74:465–471. doi: 10.1212/WNL.0b013e3181cf6ec0. [DOI] [PubMed] [Google Scholar]
- 54.Ploughman M, Austin MW, Murdoch M et al. Factors influencing healthy aging with multiple sclerosis: a qualitative study. Disabil Rehabil. 2012;34:26–33. doi: 10.3109/09638288.2011.585212. [DOI] [PubMed] [Google Scholar]
- 55.Ploughman M, Austin MW, Murdoch M, Kearney A, Godwin M, Stefanelli M. The path to self-management: a qualitative study involving older people with multiple sclerosis. Physiother Can. 2012;64:6–17. doi: 10.3138/ptc.2010-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ploughman M, Beaulieu S, Harris C et al. The Canadian survey of health, lifestyle and ageing with multiple sclerosis: methodology and initial results. BMJ Open. 2014;4:e005718. doi: 10.1136/bmjopen-2014-005718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hobart J, Lamping D, Fitzpatrick R, Riazi A, Thompson A. The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain. 2001;124(pt 5):962–973. doi: 10.1093/brain/124.5.962. [DOI] [PubMed] [Google Scholar]
- 58.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]


