Abstract
A gap exists in the literature regarding aggression in autism spectrum disorders (ASD) and how this behavior compares to other groups. In this multisite study, the Children’s Scale for Hostility and Aggression: Reactive/Proactive (C-SHARP) and the Aggression subscale of the Child Behavior Checklist (CBCL) were rated for 414 children with ASD (Autistic Disorder, 69%; PDD-NOS, 24%; Asperger’s Disorder, 7%) and 243 clinic-referred children without ASD, aged 1-21 years (mean age about 7). Participants were not selected for aggressive behavior. Relative to the comparison group, children with ASD were reported to have less aggression and were more likely to be rated as reactive rather than proactive. Among all subjects, sex was not associated with aggression; higher IQ/adaptive behavior and older age were associated with more sophisticated types of aggression while lower scores on IQ, adaptive behavior, and communication measures were associated with more physical aggression. The interaction between demographic variables and diagnosis was significant only for age: younger but not older children with ASD showed less aggression than clinic-referred controls.
Keywords: Autism spectrum disorders, aggression, C-SHARP, CBCL, reactive aggression, proactive aggression
In the general population, an early history of aggression may be associated with later substance abuse, mental health issues, victimization, and criminal behavior {Tremblay, 2004 #1817}. For individuals with developmental disabilities, including those with autism spectrum disorders (ASD), aggression is a leading cause of residential placement and results in fewer opportunities for independent functioning and interpersonal relationships {McIntyre, 2002 #1818;Benson, 1999 #2089}. Aggression is also associated with classroom removal, exclusion from services, use of psychotropic medication, and institutionalization {Tsakanikos, 2007 #1819}. Additionally, aggression is a major source of stress and strain for parents, caregivers, and teachers {Lecavalier, 2006 #1825;Rubin, 2002 #2091;Hodgetts, 2013 #2154}. Thus, the study of the structure, prevalence, and risk factors associated with aggression is important.
Aggressive behavior has been well-characterized in the general population, and data consistently show that aggression is more common among children and adults with intellectual disability (ID) than their typical peers {Benson, 2008 #2155}. Some studies in ID have included ASD; these data generally show that co-occurring ASD is a risk factor for aggression {McClintock, 2003 #1857;Holden, 2006 #1858}. One population-based study found that ASD conferred additional risk of behavioral and emotional problems, including conduct problems, even in the presence of ID {Totsika, 2011 #2586}. Efforts to quantify aggressive behaviors in ASD at the group level (versus single-subject) have been rare {Lecavalier, 2006 #1848;Farmer, 2010 #1856}. Available data suggest that aggression is relatively common in ASD. The Totsika et al. {, 2011 #2586} study found clinical levels of parent-reported conduct problems in about 65% of children with ASD, with or without ID. In a series of studies using large databases of children and adolescents with ASD, rates of physical aggression were estimated at more than 50% for current behavior and nearly 70% for aggression towards caregivers in the past {Kanne, 2011 #43;Mazurek, 2013 #2147}. One study of young clinic-referred children with ASD found that 23% of the children in the sample had Child Behavior Checklist {CBCL`; Achenbach, 2001 #2093} Aggression syndrome scale scores in the clinically significant range {Hartley, 2008 #1878}. In a cluster analysis, Lecavalier {, 2006 #1848} found that 23% of a large sample of individuals with ASD were characterized by high scores on the Nisonger Child Behavior Rating Form Conduct Problem subscale, which includes aggression. Although these studies are consistent in finding physical aggression and related syndromes to be significant problems for children with ASD, they shed little light on the many forms that aggression might take. The assessment of validated subtypes of aggression has implications for our ability to assess correlates, response to treatment, and prognosis {Connor, 1998 #2583}.
From the field of developmental psychopathology, studies show that several risk factors are reliably associated with physically aggressive behavior, including younger age, male sex, low IQ, lower verbal abilities, and family characteristics such as low socioeconomic status and harsh parenting practices {Lahey, 1999 #1883;Network, 2004 #1914;Nagin, 2001 #1917;Tremblay, 2000 #1922}. Less is known about risk and protective factors for non-physical aggression, or for aggression in children with ASD. Much of the research on aggression in ASD has been in the applied behavior analysis literature, focusing on function and maintenance factors for individuals. While single-subject designs are useful and important, these data do not allow researchers to identify risk or protective factors for aggression. Some group-level data suggest that adaptive behavior, cognitive functioning, and language ability are inversely related to aggression in ASD {Lecavalier, 2006 #1848;Hartley, 2008 #1878;Estes, 2007 #1927;Dominick, 2007 #1928}. These data also suggest that more severe core symptoms of ASD may be associated with increased aggression {Kanne, 2011 #43;Dominick, 2007 #1928;Mazurek, 2013 #2147}. In several ASD studies, age did not correlate with levels of aggression {Lecavalier, 2006 #1848;Farmer, 2011 #1875;Dominick, 2007 #1928}, though one study found that younger children engaged in slightly more physical aggression than older children {Mazurek, 2013 #2147}.
Current Study
Given the lack of data on the prevalence and risk factors for subtypes of aggression in youth with ASD, the primary goal of this study was to characterize empirically derived classes of aggressive behavior in a large multi-site sample. We hypothesized that the amount of aggressive behavior engaged in by children with ASD would vary by subtype of aggression (e.g., higher scores on physical aggression, lower on verbal behaviors). We also sought to contextualize the results of this characterization by comparing them to behaviors observed in children from the same clinic-referral stream (i.e., children referred to the developmental clinic for ASD or other behavioral/psychological evaluation, but who did not receive an ASD diagnosis). Thus, the comparison group was selected to reflect the clinical context in which children with ASD are embedded, in order to evaluate the differences that might be observed in the community. Given the lack of available data, we made no prediction about the amount of aggressive behavior in children with ASD compared to a clinic-referred comparison group. The secondary goal of this study was to assess potential correlates (age, sex, cognitive ability, adaptive behavior, and language) of subtypes of aggressive behavior. The few data available in ASD suggest that some of these variables are associated with aggressive behavior. Consistent with these studies, we hypothesized that adaptive behavior, language, and cognitive ability would be inversely related with physical manifestations of aggression and positively related with verbal aggression. Male sex and younger age is known to correlate with physical aggression in samples with both typical development and intellectual disability, but these relationships have not yet been supported in ASD. Thus, we predicted that age and sex would be unrelated to all types of aggression.
Methods
This study was approved by the Institutional Review Boards at the following institutions: Ohio State University, Nationwide Children’s Hospital of Columbus, University of Missouri, University of Illinois at Chicago, University of Utah, Seattle Children’s Hospital, and the Children’s Medical Center of Dayton.
Participants
The sample comprised two groups: ASD (n=414; 69% Autistic Disorder, 24% PDD-NOS, and 7% Asperger’s Disorder) and a comparison group of children seen at a behavioral clinic, for whom ASD had been ruled out (n=243) (Table 1). Comorbid diagnoses in the ASD group included ADHD (n=36, 9%) and speech disorders (n=51, 12%), among others. While 12% of the comparison group received no diagnosis (n=28), the remaining participants had a non-ASD diagnosis, most commonly ADHD (n=85, 35%). The groups did not differ on age, ranging from 1 year to 21 years.
Table 1.
Sample Characteristics
| ASD | Non-ASD Clinic- Referred |
p | |
|---|---|---|---|
| n | 414 | 243 | |
| Age, M ± SD | 7.67±4.51 n(%) |
7.1±3.68 n(%) |
.10 |
| Sex (% Male) | 347(84) | 167(69) | < .001 |
| No Data | 6(1) | 4(2) | |
| IQ, > 70 | 196(47) | 145(60) | .001 |
| No Data | 83(20) | 47(19) | |
| Adaptive Behavior, > 70 | 164(40) | 116(48) | .05 |
| No Data | 105(25) | 23(56) | |
| Vineland-II Communication, > 70 | 123(30) | 119(49) | < .001 |
| No Data | 168(41) | 70(29) | |
| ASD Diagnosis | - | ||
| Autistic Disorder | 284(69) | - | |
| PDD-NOS | 100(24) | - | |
| Asperger's Disorder | 30(7) | - | |
| Other Diagnoses | - | ||
| No diagnoses | - | 28(12) | |
| Non-ASD Developmental Delay | 30(7) | 29(12) | |
| ADHD | 36(9) | 85(35) | |
| ODD or CD | 9(2) | 40(16) | |
| Anxiety Disorder | 20(5) | 46(19) | |
| Mood Disorder | 13(3) | 9(4) | |
| Learning Disorder | 2(0) | 7(3) | |
| Speech Disorder | 51(12) | 65(27) | |
| Tourette's or Tic Disorder | 3(1) | 3(1) | |
| No Data | 5(1) | 0(0) | |
| Medications | - | ||
| Any Behavioral (excl. melatonin) | 65(16) | 53(22) | |
| ADHD | 39(9) | 40(16) | |
| Mood | 22(5) | 9(4) | |
| Antipsychotic | 15(4) | 13(5) | |
| Anxiolytic | 1(0) | 1(0) | |
| Anticonvulsant | 9(2) | 5(2) | |
| Antihypertensive | 6(1) | 5(2) | |
| Melatonin | 28(7) | 26(11) | |
| No Data | 87(21) | 0(0) |
Note: IQ and Adaptive Behavior are composite variables reflecting results from several standardized measures. Of the ASD group, the following n(%) were obtained from each of the sites: NCH, 201(49); Thompson Center, 82(20); Seattle Children’s, 47(11); University of Utah, 42(10); University of Illinois Chicago, 37(9), Dayton Children’s, 5(1). Non-ASD group, n(%): Columbus, 216(89); Seattle, 19(8), Chicago, 8(3).
Instruments
The parent-rated Children’s Scale for Hostility and Aggression: Reactive/Proactive {C-SHARP`; Farmer, 2009 #293;Farmer, 2010 #1856} is an empirically derived instrument with five subscales: Verbal Aggression (12 items), Bullying (12 items), Covert Aggression (10 items), Hostility (9 items), and Physical Aggression (8 items). Each item receives two ratings: the Problem Scale (0-3) reflects the frequency and severity of the behavior. Preliminary data suggested that the Problem Scale has good reliability and validity {Farmer, 2010 #1856}, and in the current study, Cronbach’s alpha (a measure of internal consistency) ranged from .77 (Physical Aggression) to .91 (Verbal Aggression). The Provocation Scale asks the rater to indicate whether the behavior is always provoked/reactive (−2) through neutral (0) to always unprovoked/proactive (+2). Zero scores are also assigned when the Problem Scale is rated as zero. In the current study, Provocation scores were summed by subscale and categorized into Reactive (sum less than zero), Neutral (sum of zero; either no aggression, or similar rates of reactive and proactive behavior), or Proactive (sum greater than zero). The initial psychometric data on the Provocation Scale were inconclusive (see Farmer & Aman, 2010), but the internal consistency in the current study was acceptable (Verbal: α=.81, Bullying: α=.81, Covert: α=.72, Hostile: α=.83, Physical: α=.68). Thus, in the current study, Provocation data are presented in an exploratory fashion. Two versions of the CBCL were used, depending on the child’s age: School-age (6-18 years) or Preschool (1.5-5 years). This study used only the standardized scores for Aggressive Behavior subscale of the Syndrome Scale, which queries primarily physical-type behaviors. By convention, scores above 70 are considered clinically significant.
A variety of standardized cognitive and adaptive behavior measures were used to characterize the children in the sample. The full scale IQ (or equivalent) was used from the Stanford Binet Intelligence Scales-Fifth Edition {Roid, 2003 #2094}, the Wechsler Intelligence Scales for Children {Wechsler, 2003 #2299}, the Mullen Scales of Early Learning {Mullen, 1995 #1983}, the Bayley Scales of Infant Development {Bayley, 1993 #2300}, and the Differential Ability Scales, Second Edition {Elliott, 2007 #1984}. To measure adaptive behavior, we used composite scores from the Vineland-II Adaptive Behavior Scales {Adaptive Behavior Composite`; Sparrow, 2005 #2095} and the Adaptive Behavior Assessment System {General Adaptive Composite`; Harrison, 2003 #2301}. The Communication standard score on the Vineland-II was used to estimate language level. Standard scores on all cognitive, adaptive behavior, and language scales were dichotomized at 70.
Procedure
Data were collected from six sites across the United States. For three sites [Nationwide Children’s Hospital (NCH) Child Development Center (Columbus, Ohio), Seattle (Washington) Children’s Hospital Autism Center, and The Children’s Medical Center of Dayton (Ohio)], data were collected prospectively through clinic intake packets. The remaining sites contributed participants who were previously or currently involved in research [Thompson Center for Autism and Neurodevelopmental Disorders (Columbia, MO), University of Utah (Salt Lake City), and the Institute for Juvenile Research at the University of Illinois (Chicago)]. Importantly, these research-based sites were selected for participation because the studies did not recruit subjects for any particular feature beyond ASD symptoms. Therefore, there were no expected systematic differences on relevant phenotypic characteristics, and both clinic- and research-based sites were expected to be representative of a broader ASD population.
For the ASD group, a clinical diagnosis of ASD was made using the Autism Diagnostic Interview-Revised {ADI-R`; Lord, 1994 #862}, the Autism Diagnostic Observation Schedule {Lord, 2000 #850}, and/or clinical judgment using DSM-IV-TR {APA, 2000 #1363} in some combination. Non-ASD diagnoses were made using child interview and assessment, parent and/or teacher report, and clinical judgment (DSM-IV-TR). For all sites, ASD group inclusion criteria were (a) a parent or caregiver completed C-SHARP and (b) a completed diagnostic workup yielding a diagnosis of ASD. Other data were obtained through chart review when available.
The clinic-referred comparison group was obtained contemporaneously from three sites, primarily from NCH (89%). The Child Development Center at NCH provides assessment and diagnostic services to children suspected of having ASD and/or other developmental disabilities. In addition to ASD, intellectual disability, attention-deficit hyperactivity disorder, specific learning disabilities, or other neurodevelopmental conditions are other common referral concerns for these children. Children who met criterion (a) above, but for whom a diagnosis of ASD was ruled out by the clinician, were included in the comparison group. Thus, the comparison group represented the non-ASD population presenting to child psychological clinics.
Statistical Analyses
For all C-SHARP subscales and the CBCL, the data were not normally distributed and the variances were not homogenous, so the data were square-root transformed. After testing for between-group differences on the subscales, each potential correlate (sex, age, IQ, and adaptive behavior) was entered into a distinct factorial model along with group (ASD versus non-ASD) and the interaction predicting the five C-SHARP subscales and CBCL Aggressive Behavior. This allowed for the simultaneous evaluation of main effects of group and correlates, controlling for one another, as well as moderation. Moderation was defined as a significant interaction, which would suggest that the relationship between the correlate and aggression differs between groups {Farmer, 2012 #1941}.
The Statistical Package for the Social Sciences-Version 19 was used for all calculations, and alpha was set to p<.01 to acknowledge multiplicity. The GLM Univariate procedure was used to assess the factorial models described above. Chi-squared tests were used for categorical comparisons. Effect sizes are Cohen’s d {Cohen, 1988 #2146} with pooled standard deviation, using non-transformed data for ease of interpretation.
Results
Between-group differences
On all C-SHARP problem subscales, the comparison group received significantly higher (worse) scores than the ASD group (Table 2; F values in Table 3): Verbal Aggression [d=0.25, 95% CI=(0.09, 0.41)]; Bullying [d=0.42, 95% CI=(0.26, 0.58)]; Covert Aggression [d=0.40, 95% CI=(0.24, 0.56)]; Hostility [d=0.25, 95% CI=(0.09, 0.41)]; and Physical Aggression [d=0.35, 95% CI=(0.19, 0.51)]. CBCL data were available for approximately 70% of the total sample. The comparison group was rated significantly higher (worse) than the ASD group on the CBCL Aggressive Behavior subscale [d=0.51, 95% CI=(0.32, 0.70)]. Using a cutoff of T=70, children in the comparison group were significantly more likely to receive a score in the clinical range on CBCL Aggressive Behavior (36% versus 19%, χ2=17.29, p<.001).
Table 2.
C-SHARP and CBCL scores.
| ASD (n=414) |
Non-ASD Clinic-Referred (n=243) |
|||||
|---|---|---|---|---|---|---|
| Zero Score, n(%) |
M±SD | Range | Zero Score, n(%) |
M±SD | Range | |
| C-SHARP | ||||||
| Verbal Aggression | 73(18) | 3.75±6.14 | (0,32) | 30(12) | 5.4±7.05 | (0,30) |
| Bullying | 67(16) | 6.29±6.42 | (0,34) | 27(11) | 9.33±8.42 | (0,31) |
| Covert Aggression | 67(16) | 6.04±6.08 | (0,30) | 27(11) | 8.6±7.05 | (0,27) |
| Hostility | 51(12) | 8.71±6.98 | (0,27) | 23(10) | 10.51±7.5 | (0,27) |
| Physical Aggression | 193(47) | 1.84±2.7 | (0,19) | 94(39) | 2.98±4.02 | (0,17) |
| CBCL Aggressive Behavior | 209(51) | 61.52±10.67 | (50,100) | 77(32) | 67.34±12.38 | (50,100) |
Note: See Table 3 for test statistics. Site differences (p<.01) were observed on several subscales (Verbal, Bullying, Covert, and Hostile). All omnibus site differences were accounted for by one research-based site (Missouri) having higher scores than one of the clinic-based sites. Cohen’s d effect sizes for these differences were moderate. Data available upon request.
Table 3.
Diagnosis and other correlates of aggressive behavior.
| Square-Root Transformed Subscale |
Effect | Study Group |
Correlate |
||||
|---|---|---|---|---|---|---|---|
| Sex |
IQ |
Adaptive Behavior |
Vineland-II Communication |
Age (Years) |
|||
| F(1,655) | F(1,643) | F(1,523) | F(1,492) | F(1,415) | F(1,653) | ||
| Verbal Aggression | Group | 16.69* | 18.56* | 7.66* | 14.02* | 12.51* | 21.96* |
| Predictor | 0.53 | 17.26*, a | 0.31 | 1.09 | 37.55*, a | ||
| Group x Predictor | 2.45 | 2.61 | 5.49 | 8.18* | 7.39* | ||
| R2 | .03 | .03 | .07 | .03 | .05 | .12 | |
| Bullying | Group | 21.66* | 28.08* | 15.35* | 14.11* | 8.05* | 27.99* |
| Predictor | 0.59 | 0.22 | 11.83*, b | 2.67 | 22.11*, b | ||
| Group x Predictor | 6.35 | 0.19 | 0.14 | 1.16 | 12.81* | ||
| R2 | .03 | .04 | .04 | .05 | .01 | .07 | |
| Covert Aggression | Group | 23.00* | 24.85* | 13.83* | 20.76* | 15.60* | 15.91* |
| Predictor | 0.29 | 16.71*, a | 3.44 | 0.03 | 21.37*, a | ||
| Group x Predictor | 3.93 | 0.00 | 0.84 | 4.16 | 2.77 | ||
| R2 | .03 | .04 | .07 | .04 | .05 | .09 | |
| Hostility | Group | 7.84* | 9.94* | 3.88 | 8.23* | 5.01 | 14.38* |
| Predictor | 0.01 | 5.50 | 4.87 | 0.10 | 2.55 | ||
| Group x Predictor | 2.61 | 0.43 | 0.09 | 1.17 | 7.15* | ||
| R2 | .01 | .02 | .03 | .02 | .01 | .04 | |
| Physical Aggression | Group | 13.48* | 20.15* | 11.96* | 8.69* | 9.25* | 21.84* |
| Predictor | 0.01 | 3.20 | 13.39*, b | 12.46*, b | 26.11*, b | ||
| Group x Predictor | 6.47 | 0.63 | 1.20 | 1.46 | 11.78* | ||
| R2 | .02 | .03 | .04 | .04 | .04 | .06 | |
| CBCL Aggressionc | Group | 29.25* | 20.86* | 18.77* | 22.14* | 14.94* | 21.49* |
| Predictor | 0.05 | 0.37 | 15.87*, b | 10.36*, b | 9.28*, b | ||
| Group x Predictor | 0.19 | 3.60 | 0.38 | 0.23 | 5.73 | ||
| R2 | .06 | .06 | .08 | .09 | .07 | .08 | |
p < 0.01
Low values on predictor associated with lower aggression scores.
Low values on predictor associated with higher aggression scores.
df for CBCL Aggression were as follows (by column): Study Group (1,466), Sex (1,455), IQ (1,396), Adaptive Behavior (1,356), Vineland-II Communication, (1,326), Age (1,465).
Note: All significant main effects of Study Group were in the direction of lower scores for ASD than for non-ASD comparison group.
The profile of C-SHARP scores were explored in the subgroup of children with CBCL Aggressive Behavior scores in the clinical range (ASD, n=55; non-ASD, n=64). In both study groups of these more aggressive children, Bullying was the only subscale for which the group comparison remained significant [non-ASD>ASD; d=0.60, 95% CI=(0.23, 0.97)]. However, within-group, the rank order of scores was the same: Hostility received the highest score, followed by Covert Aggression, Bullying, Verbal Aggression, and Physical Aggression.
A significant proportion of the non-ASD sample had a diagnosis of oppositional defiant disorder or conduct disorder, which are both associated with aggression. To determine if this difference accounted for the group effect on subscale scores, participants from both groups with these diagnoses (ASD: n=9, 2%, non-ASD: n=40, 16%) were excluded. Though smaller in magnitude, the following comparisons remained statistically significant: Verbal Aggression [d=0.16, 95% CI=(0.00, 0.33)]; Bullying [d=0.29, 95% CI=(0.12, 0.46)]; Covert Aggression [d=0.33, 95% CI=(0.16, 0.50)]; and CBCL Aggressive Behavior [d=0.36, 95% CI=(0.16, 0.56)]. Between-group differences on C-SHARP Hostility and Physical Aggression were no longer significant, suggesting that the children with disruptive behavior disorders were responsible for those effects. The exclusion of these children did not affect any of the remaining analyses.
Exploratory analyses were done with the Provocation Scale. The groups differed significantly on three subscales: Verbal Aggression, Bullying, and Hostility (Table 4). On Verbal Aggression, children in the ASD group were more likely to be rated as neutral, while the comparison group was more likely to be rated as proactive. This was likely a function of the higher proportion of zero scores on the Verbal Aggression Problem Scale, which automatically resulted in a neutral score on the Provocation Scale. For both Bullying and Hostility, children with ASD were more often rated as reactive while the comparison group was more frequently reported to be proactive.
Table 4.
C-SHARP Provocation subscale scores by study group.
| Provocation Score Category |
ASD | Non-ASD Clinic-Referred |
χ2 (p) | |
|---|---|---|---|---|
| Verbal Aggression, n(%) | Reactive | 125(30) | 76(31) | 18.92(<.001) |
| Neutral | 239(58) | 108(44) | ||
| Proactive | 50(12) | 59(24) | ||
| Bullying, n(%) | Reactive | 143(35) | 57(23) | 17.97(<.001) |
| Neutral | 146(35) | 74(30) | ||
| Proactive | 125(30) | 112(46) | ||
| Covert Aggression, n(%) | Reactive | 127(31) | 60(25) | 7.04(.03) |
| Neutral | 136(33) | 69(28) | ||
| Proactive | 151(36) | 114(47) | ||
| Hostility, n(%) | Reactive | 181(44) | 77(32) | 15.54(<.001) |
| Neutral | 119(29) | 64(26) | ||
| Proactive | 113(27) | 101(42) | ||
| Physical Aggression, n(%) | Reactive | 93(22) | 50(21) | 3.43(.18) |
| Neutral | 247(60) | 135(56) | ||
| Proactive | 74(18) | 58(24) |
Correlates of C-SHARP and CBCL scores
Relationships between possible correlates were assessed using point-biserial correlations (age only) or chi-square (dichotomized IQ, adaptive behavior, Vineland-II Communication, and sex). Sex was unrelated to all other variables. Age was unrelated to adaptive behavior, and Vineland-II Communication, but was positively and moderately related to IQ (r=.20, p<.001). As expected, IQ, adaptive behavior, and Vineland-II Communication were interrelated (IQ versus adaptive behavior, φ=.39; IQ versus language, φ=.46; adaptive behavior versus language, φ=.74; all p<.001). Possible correlates of aggressive behavior in the full sample were entered into separate models as a correlate (age) or fixed factor (sex, IQ, adaptive behavior, Vineland-II Communication) (Table 3). No effects of sex were observed. Participants with younger age and lower IQ had significantly lower scores on Verbal Aggression and Covert Aggression. However, higher scores were observed on the Bullying, Physical Aggression, and CBCL Aggressive Behavior subscales in participants with lower adaptive behavior scores, younger age, and lower Vineland Communication scores (Physical and CBCL only).
The main effect of group (ASD versus comparison) remained statistically significant for most subscales when sex, IQ, adaptive behavior, Vineland-II Communication, and age were added into the model. The exception was C-SHARP Hostility; when IQ or Vineland-II Communication was added to the model, the main effect of group was rendered non-significant.
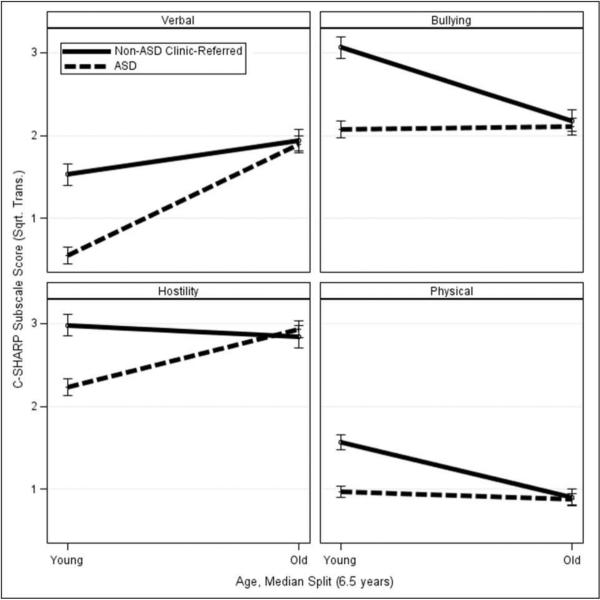
Study group was explored as a moderator of these correlates of reported aggression. Significant interactions were observed between group (ASD versus comparison) and age in predicting scores on most C-SHARP subscales. Age was dichotomized at the median (6.5 years) for visual inspection. For Bullying and Physical Aggression, the interaction was a result of a steeper negative relationship within the comparison group; for Verbal Aggression and Hostility, a steeper positive relationship was observed within the ASD group (Figure 1). The interaction between diagnosis and Vineland-II Communication score was also significant in predicting Verbal Aggression. Little relationship between the Communication score and Verbal Aggression was observed in the comparison group (which had higher Communication scores), while Communication scores were positively related with Verbal Aggression in children with ASD.
Figure 1.
Diagnosis and age interact in predicting C-SHARP subscale scores. Age was dichotomized 6.5 years for visual representation.
Discussion
This study of a large sample of children aged 1-21 years showed that while a wide variety of aggressive behaviors was generally common, aggression was reported to occur with less severity in children with ASD than in a comparison sample of clinic-referred children without ASD. The scores observed in this ASD sample are similar to those found in the C-SHARP development sample; however, in that study, children with ASD were rated slightly higher on all subscales than a general developmental delay group {Farmer, 2011 #1875}. Approximately 50% of the current ASD group engaged in at least one behavior on C-SHARP Physical Aggression, nearly identical to the findings in two studies of large, well-characterized samples of children with ASD {Kanne, 2011 #43;Mazurek, 2013 #2147}. Thus, this study is consistent with existing literature and confirms that aggressive behavior is a consistent concern among parents of children with ASD, while adding data about the frequency of several types of aggressive behavior.
It is important to note that prior to the current study, little was known about how various types of parent-reported aggression in ASD compared to other clinical or typical populations. The few existing studies found no differences compared to groups with ID {Brereton, 2006 #1949}, non-ASD genetic conditions {e.g.`, Williams syndrome and Prader-Willi syndrome`; Dimitropoulos, 2009 #1955}, language impairment {Dominick, 2007 #1928}, or typically developing controls {Guttmann-Steinmetz, 2009 #1959}. In this study, the ASD group received significantly lower ratings than the comparison group on all C-SHARP and CBCL subscales, representing several types of aggression, and most differences remained even when participants with oppositional defiant disorder and conduct disorder were excluded. Still, nearly 20% of the ASD sample received a score on CBCL Aggressive Behavior in the clinical range, which occurred for only 3% of the CBCL normative sample. These data suggest that while children with ASD may not be differentiated by aggression from the remainder of the referral stream, children with ASD do engage in more aggressive behavior than would have been expected of typically developing children.
A unique aspect of the C-SHARP is that the rater is asked to indicate if aggressive behaviors are generally provoked or unprovoked, corresponding roughly to reactive or proactive aggression {Farmer, 2009 #293}. In general, the comparison children were likelier to be rated as proactive, while the ASD sample was more likely to be rated as neutral or reactive. The few existing data corroborate that children with ASD may be likely to engage in reactive behavior. In one study, researchers found that during a blood draw, children with low IQ and ASD were more likely than typical controls to lash out, which was characterized as reactive aggression {Bronsard, 2010 #1946}. Using a computer-based task, another study found that boys with ASD were more likely to differ from typical controls on measures of reactive physical aggression than were girls with ASD {Kaartinen, 2012 #2406}. The C-SHARP conceptualizes reactive and proactive aggression as a continuum, passing through a neutral category. Although this is convenient for scoring purposes, it is possible that these constructs are separate and not mutually exclusive. To this point, existing data suggest a moderate correlation between the two (meta-analysis median r=.68) {Card, 2006 #2295}. Further elucidation of these function-based subtypes in ASD is warranted.
The second goal of this study was to evaluate potential correlates of aggression. Although male sex is associated with increased aggression in both typical and ID samples {McClintock, 2003 #1857}, this relationship was not confirmed in the current study. This may be due to the relatively young age of the sample; the studies in ID samples have been frequently in older adolescents and adults. Overall, the cross-sectional finding in the current study that older age was associated with more complex aggressive behaviors (Verbal and Covert Aggression) was consistent with studies in the general population {NICHD`, , 2004 #1914}, though some studies in ASD have failed to find a relationship between age and aggression {Lecavalier, 2006 #1848;Farmer, 2011 #1875;Dominick, 2007 #1928}. Importantly, these studies did not differentiate between less sophisticated aggressive behaviors (e.g., physical aggression, which predominates in younger children) and the higher-level behaviors which occur at older ages. In fact, the physical-type subscales in the current study showed little effect of age within the ASD sample, supporting the null findings of other studies. This result highlights the utility of assessing subtypes of aggression.
Adaptive behavior was inversely related with physical aggression in this study, consistent with previous reports that found this relationship for both adaptive behavior and IQ {Lecavalier, 2006 #1848;Hartley, 2008 #1878;Estes, 2007 #1927;Dominick, 2007 #1928}. This study expands upon those findings by showing that IQ was positively related to the more complex expressions of aggression. Although a standardized direct measure of language ability was not available in this study, results with Vineland-II Communication scores indicated that children with better communication engaged in less physical-type behaviors, regardless of diagnosis. Thus, it is possible that language level explains much of the relationship between these types of aggression and IQ. These results highlight the utility of assessing subtypes of aggression; scales that do not survey the more complex behaviors may overlook other types of aggression in higher-functioning or more verbal children.
ASD diagnosis did not moderate most correlates, with the exception of age and Vineland-II Communication. While no relationship was observed between Communication and Verbal Aggression in the non-ASD group, better communication ability did appear to be a risk factor for children in the ASD group. Two general patterns emerged for age: age was not related to the less sophisticated types of aggression in the ASD group, but in the comparison group, older children engaged in less physical-type aggression than younger children (consistent with data from population-based studies such as Tremblay et al., 2004). Conversely, age was unrelated to more complex behaviors in the comparison group, but within the ASD group, older children received higher scores than younger children. In all cases, the larger between-group difference was observed in younger children. These results may represent different trajectories that require study in longitudinal samples; alternatively, they may be artifacts of delayed development in the ASD group, or of more complicated interactions between age and factors such as ASD core symptom severity and language ability.
The composition of the comparison group selected for this study did pose some limitations. It was heterogeneous, but the uniting aspect was that all children were referred to specialty clinics for behavioral or psychological evaluation, on suspicion of some developmental disability (including ASD). Thus, this comparison group was included with the intent of determining whether aggressive behavior distinguished children with ASD from other children in the same “referral stream.” Behavioral issues are a common reason for initial referral (even for children eventually diagnosed with ASD), so it is possible that the children not diagnosed with ASD may have had inflated levels of aggression. Few published reports of the CBCL in developmental clinics are available, though one study in preschoolers referred to such clinics found average Aggression scores of 51.7±4.2 (18-23 months age group), 54.2±6.7 (24-29 month age group), and 57.4±10.4 (30-35 month age group) {Rescorla, 2007 #2407}. These scores are lower than that observed for the comparison sample in this study (67.34±12.38), but this may be attributed to the difference in age between groups. Other more homogenous comparison groups, such as those with typical development or ID, may have allowed for more clear-cut conclusions. However, this comparison sample does reflect the population that many clinicians in the ASD field encounter, and is therefore readily applicable to practice.
The goal of a large, representative, and well-characterized sample of children with ASD required a multiple-site approach. Several attendant limitations were incurred, including the lack of consistent instrumentation and missing data. These data were likely not missing-at-random; children who do not receive an IQ test in a clinical setting are often too impaired to receive a standard score on an age-appropriate standardized measure. Site differences in some C-SHARP scores were also observed, where one research-based site received higher average scores than the major clinical site on several subscales. This may have reflected natural variation in the broader ASD sample, or it may have been a methodological artifact. Parent report has limitations, including the possibility that parents of children with disabilities may mute their report of problem behaviors by attributing the child’s behavior to the disability {Pearson, 1994 #1945;Pearson, 1994 #1945;Pearson, 1994 #1945;Pearson, 1994 #1945}. Other fields have successfully used teacher and caregiver report in the study of aggression, which will be an important future step. Finally, despite the large size, the study sample may not be representative of the broader ASD population. For example, the psychiatric comorbidity in this ASD sample was low compared to other studies. Simonoff and colleagues {, 2008 #2587} reported the point prevalence of several disorders in an epidemiological sample of children aged 10-14 years with ASD: 42% of that sample met criteria for an anxiety/phobic disorder, 30% met criteria for ODD/CD, and 28% met criteria for ADHD. The younger age of the current sample may explain this difference, however, the possibility remains that these children may be less psychiatrically and behaviorally impaired than the general ASD population. Totsika et al. {, 2011 #2586} provide a thorough review of the limitations of non-population-based methods, which is a consistent limitation of ASD research and may result in biased samples. For this reason, as well as the limitations inherent with the selection of any one control group, future population-based study of subtypes of aggression is warranted.
The results of this study contribute to a modest-but-growing literature confirming the existence of aggression in ASD, and the study is among the first to characterize the behavior as reactive or proactive. While the results of this study were largely consistent with existing literature, the comparison group data give context. Future studies expanding on this work by using scales that assess subtypes of aggression, homogenous control groups, and direct observation or teacher report may show that aggressive behavior is not a result of ASD, per se, but rather of the increased incidence of risk factors relative to the general population.
Acknowledgements
The following individuals assisted in data collection and entry: Christopher Cope, Meghan Ellingsworth, Caroline Sansbury, Aaron Kaat, Annahir Cariello, Alyson Froehlich, Denise Ward, and Kristina Butler. This work was prepared from the doctoral dissertation of C. Farmer, Ohio State University.
Funding: This work was supported by an Alumni Grant from the Graduate School of the Ohio State University (Farmer), a Graduate Student Grant from the Organization for Autism Research (Farmer), and the National Institute for Child Health and Development (P50 HD055751, Cook).
References
- Achenbach T, Rescorla L. Manual for ASEBA School-Age Forms and Profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington, VT: 2001. [Google Scholar]
- APA . Diagnostic and statistical manual of mental disorders : DSM-IV-TR. 4th American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Bayley N. Bayley Scales of Infant Development. 2nd Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Benson B, Aman M. Disruptive Behavior Disorders in Children with Mental Retardation. In: Quay H, Hogan A, editors. Handbook of Disruptive Behavior Disorders. Kluwer Academic/Plenum Publishers; New York: 1999. pp. 559–578. [Google Scholar]
- Benson BA, Brooks WT. Aggressive challenging behaviour and intellectual disability. Current Opinion in Psychiatry. 2008;21(5):454–458. doi: 10.1097/YCO.0b013e328306a090. 410.1097/YCO.1090b1013e328306a328090. [DOI] [PubMed] [Google Scholar]
- Brereton AV, Tonge BJ, Einfeld SL. Psychopathology in children and adolescents with autism compared to young people with intellectual disability. Journal of Autism and Developmental Disorders. 2006;36(7):863–870. doi: 10.1007/s10803-006-0125-y. doi: DOI 10.1007/s10803-006-0125-y. [DOI] [PubMed] [Google Scholar]
- Bronsard G, Botbol M, Tordjman S. Aggression in Low Functioning Children and Adolescents with Autistic Disorder. Plos One. 2010;5(12) doi: 10.1371/journal.pone.0014358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card NA, Little TD. Proactive and reactive aggression in childhood and adolescence: A meta-analysis of differential relations with psychosocial adjustment. International Journal of Behavioral Development. 2006;30(5):466–480. doi: Doi 10.1177/0165025406071904. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Lawrence Erlbaum; 1988. [Google Scholar]
- Connor DF, Melloni RH, Jr., Harrison RJ. Overt categorical aggression in referred children and adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37(1):66–73. doi: 10.1097/00004583-199801000-00019. [DOI] [PubMed] [Google Scholar]
- Dimitropoulos A, Ho AY, Klaiman C, Koenig K, Schultz RT. A comparison of behavioral and emotional characteristics in children with autism, Prader-Willi Syndrome, and Williams Syndrome. Journal of Mental Health Research in Intellectual Disabilities. 2009;2(3):220–243. [Google Scholar]
- Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S. Atypical behaviors in children with autism and children with a history of language impairment. Research in Developmental Disabilities. 2007;28(2):145–162. doi: 10.1016/j.ridd.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Elliott CD, editor. Manual for the Differential Ability Scales. Second Harcourt Assessment; San Antonio, TX: 2007. [Google Scholar]
- Estes AM, Dawson G, Sterling L, Munson J. Level of intellectual functioning predicts patterns of associated symptoms in school-age children with autism spectrum disorder. Am J Ment Retard. 2007;112(6):439–449. doi: 10.1352/0895-8017(2007)112[439:LOIFPP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Farmer C. Demystifying moderators and mediators in intellectual and developmental disabilities research: a primer and review of the literature. Journal of intellectual disability research : JIDR. 2012;56(12):1148–1160. doi: 10.1111/j.1365-2788.2011.01508.x. [DOI] [PubMed] [Google Scholar]
- Farmer CA, Aman MG. Development of the Children's Scale of Hostility and Aggression: Reactive/Proactive (C-SHARP) Research in Developmental Disabilities. 2009;30(6):1155–1167. doi: 10.1016/j.ridd.2009.03.001. doi: 10.1016/j.ridd.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Farmer CA, Aman MG. Psychometric properties of the Children's Scale of Hostility and Aggression: Reactive/Proactive (C-SHARP) Research in Developmental Disabilities. 2010;31(1):270–280. doi: 10.1016/j.ridd.2009.09.014. [DOI] [PubMed] [Google Scholar]
- Farmer CA, Aman MG. Aggressive behavior in a sample of children with autism spectrum disorders. Research in Autism Spectrum Disorders. 2011;5(1):317–323. doi: DOI 10.1016/j.rasd.2010.04.014. [Google Scholar]
- Guttmann-Steinmetz S, Gadow KD, Devincent CJ. Oppositional defiant and conduct disorder behaviors in boys with autism spectrum disorder with and without attention-deficit hyperactivity disorder versus several comparison samples. J Autism Dev Disord. 2009;39(7):976–985. doi: 10.1007/s10803-009-0706-7. doi: 10.1007/s10803-009-0706-7. [DOI] [PubMed] [Google Scholar]
- Harrison PL, Oakland T. Adaptive Behavior Assessment System–Second Edition. Wiley Online Library; 2003. [Google Scholar]
- Hartley SL, Sikora DM, Mccoy R. Prevalence and risk factors of maladaptive behaviour in young children with Autistic Disorder. Journal of Intellectual Disability Research. 2008;52:819–829. doi: 10.1111/j.1365-2788.2008.01065.x. doi: DOI 10.1111/j.1365-2788.2008.01065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgetts S, Nicholas D, Zwaigenbaum L. Home Sweet Home? Families’ Experiences With Aggression in Children With Autism Spectrum Disorders. Focus on Autism and Other Developmental Disabilities. 2013 [Google Scholar]
- Holden B, Gitlesen JP. A total population study of challenging behaviour in the county of Hedmark, Norway: prevalence, and risk markers. Research in Developmental Disabilities. 2006;27(4):456–465. doi: 10.1016/j.ridd.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Kaartinen M, Puura K, Helminen M, Salmelin R, Pelkonen E, Juujarvi P. Reactive aggression among children with and without autism spectrum disorder. J Autism Dev Disord. 2012 doi: 10.1007/s10803-012-1743-1. [DOI] [PubMed] [Google Scholar]
- Kanne SM, Mazurek MO. Aggression in Children and Adolescents with ASD: Prevalence and Risk Factors. Journal of Autism and Developmental Disorders. 2011;41(7):926–937. doi: 10.1007/s10803-010-1118-4. doi: 10.1007/s10803-010-1118-4. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID, McBurnett K. Annotation: The development of antisocial behavior: An integrative causal model. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40(5):669–682. doi: Doi 10.1017/S0021963099004047. [PubMed] [Google Scholar]
- Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: relative prevalence, effects of subject characteristics, and empirical classification. Journal of Autism and Developmental Disorders. 2006;36(8):1101–1114. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of intellectual disability research : JIDR. 2006;50:172–183. doi: 10.1111/j.1365-2788.2005.00732.x. Pt 3. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr., Leventhal BL, DiLavore PC, Rutter M. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Mazurek MO, Kanne SM, Wodka EL. Physical aggression in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders. 2013;7(3):455–465. doi: http://dx.doi.org/10.1016/j.rasd.2012.11.004. [Google Scholar]
- McClintock K, Hall S, Oliver C. Risk markers associated with challenging behaviours in people with intellectual disabilities: a meta-analytic study. Journal of intellectual disability research : JIDR. 2003;47:405–416. doi: 10.1046/j.1365-2788.2003.00517.x. Pt 6. [DOI] [PubMed] [Google Scholar]
- McIntyre LL, Blacher J, Baker BL. Behaviour/mental health problems in young adults with intellectual disability: the impact on families. Journal of Intellectual Disability Research. 2002;46:239–249. doi: 10.1046/j.1365-2788.2002.00371.x. [DOI] [PubMed] [Google Scholar]
- Mullen EM, editor. Mullen Scales of Early Learning. American Guidance Service; Circle Pines, MN: 1995. [Google Scholar]
- Nagin DS, Tremblay RE. Parental and early childhood predictors of persistent physical aggression in boys from kindergarten to high school. Archives of General Psychiatry. 2001;58(4):389–394. doi: 10.1001/archpsyc.58.4.389. [DOI] [PubMed] [Google Scholar]
- Network NECCR. Trajectories of physical aggression from toddlerhood to middle childhood: predictors, correlates, and outcomes. Monographs of the Society for Research in Child Development. 2004;69(4):1–129. doi: 10.1111/j.0037-976x.2004.00312.x. vii. [DOI] [PubMed] [Google Scholar]
- Pearson DA, Aman MG. Ratings of hyperactivity and developmental indices: should clinicians correct for developmental level? Journal of Autism and Developmental Disorders. 1994;24(4):395–411. doi: 10.1007/BF02172125. [DOI] [PubMed] [Google Scholar]
- Rescorla L, Ross GS, McClure S. Language delay and behavioral/emotional problems in toddlers: findings from two developmental clinics. J Speech Lang Hear Res. 2007;50(4):1063–1078. doi: 10.1044/1092-4388(2007/074). [DOI] [PubMed] [Google Scholar]
- Roid G. Stanford-Binet Intelligence Scales, Fifth Edition, Examiner's Manual. Riverside Publishing; Itasca, IL: 2003. [Google Scholar]
- Rubin KH, Burgess KB, Hastings PD. Stability and social-behavioral consequences of toddlers' inhibited temperament and parenting behaviors. Child Development. 2002;73(2):483–495. doi: 10.1111/1467-8624.00419. doi: Doi 10.1111/1467-8624.00419. [DOI] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Sparrow S, Cicchetti D, Baila D. Vineland-II: Vineland Adaptive Behavior Scales: Survey Forms Manual. (2nd) 2005 [Google Scholar]
- Totsika V, Hastings RP, Emerson E, Lancaster GA, Berridge DM. A population-based investigation of behavioural and emotional problems and maternal mental health: associations with autism spectrum disorder and intellectual disability. J Child Psychol Psychiatry. 2011;52(1):91–99. doi: 10.1111/j.1469-7610.2010.02295.x. [DOI] [PubMed] [Google Scholar]
- Tremblay RE. The development of aggressive behaviour during childhood: What have we learned in the past century? International Journal of Behavioral Development. 2000;24(2):129–141. [Google Scholar]
- Tremblay RE, Nagin DS, Seguin JR, Zoccolillo M, Zelazo PD, Boivin M, Japel C. Physical aggression during early childhood: trajectories and predictors. Pediatrics. 2004;114(1):e43–50. doi: 10.1542/peds.114.1.e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsakanikos E, Costello H, Holt G, Sturmey P, Bouras N. Behaviour management problems as predictors of psychotropic medication and use of psychiatric services in adults with autism. Journal of Autism and Developmental Disorders. 2007;37(6):1080–1085. doi: 10.1007/s10803-006-0248-1. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children. 4th Psychological Corporation; San Antonio, TX: 2003. [Google Scholar]