Abstract
We conducted a meta-analysis of randomized controlled trials to examine the association of mobile phone intervention with net change in weight-related measures among overweight and obese adults. We searched electronic databases and conducted a bibliography review to identify articles published between the inception date of each database and March 27, 2014. Fourteen trials (including 1,337 participants in total) that met the eligibility criteria were included. Two investigators independently abstracted information on study characteristics and study outcomes. Net change estimates comparing the intervention group with the control group were pooled across trials using random-effects models. Compared with the control group, mobile phone intervention was associated with significant changes in body weight and body mass index (weight (kg)/height (m)2) of −1.44 kg (95% confidence interval (CI): −2.12, −0.76) and −0.24 units (95% CI: −0.40, −0.08), respectively. Subgroup analyses revealed that the associations were consistent across study-duration and intervention-type subgroups. For example, net body weight changes were −0.92 kg (95% CI: −1.58, −0.25) and −1.85 kg (95% CI: −2.99, −0.71) in trials of shorter (<6 months) and longer (≥6 months) duration, respectively. These findings provide evidence that mobile phone intervention may be a useful tool for promoting weight loss among overweight and obese adults.
Keywords: behavioral intervention, mobile phones, obesity, overweight, weight loss
Overweight/obesity is a major global health challenge due to its high prevalence and associated increases in chronic disease morbidity and mortality (1–3). In 2005, an estimated 1.3 billion adults were either overweight or obese globally, with estimates projected to increase to 3.3 billion by 2025 (2). As one of the leading risk factors for mortality and morbidity worldwide, high body mass index (BMI) was responsible for approximately 3.4 million deaths and 3.8% of global disability-adjusted life-years in 2010 (4). Furthermore, overweight/obesity exerts a substantial economic toll, accounting for approximately 7% of total health-care costs worldwide (5).
Studies have shown that even modest levels of sustained weight loss could yield substantial reductions in weight-related morbidity, mortality, and health-care costs (6–9). For example, 1 kg of weight loss has been associated with a 13% reduction in the risk of incident diabetes (10). Behavioral changes, including increased physical activity, improved diet quality, and restriction of caloric intake, are important components of weight management. However, randomized controlled trials (RCTs) of these types of interventions have shown limited success in sustaining weight loss due to a lack of long-term compliance (11–13). Intervention by mobile telephone, including contact by short message service (SMS) (text messages) and multimedia message service (MMS) (pictures or other multimedia materials), that delivers frequent reminders of nutritional and physical activity goals or recommendations may be a convenient and potentially cost-effective method of encouraging people to maintain healthy behavior and lose weight. Studies of mobile phone interventions have shown promise in reducing diabetes risk (14), increasing physical activity (15), and promoting smoking cessation (16). However, the associations of mobile phone intervention with weight loss are still controversial. Some RCTs have found text messaging to be a useful method of promoting weight loss in overweight adults (17, 18), while others have not shown benefits (19, 20). In addition, many of these trials have had limited statistical power to detect moderate but meaningful body weight reductions associated with mobile phone intervention (18, 21). Given the conflicting results and limitations of previous trials, we determined that a meta-analysis of RCTs would allow for more precise estimation of the association of mobile phone interventions with weight loss.
The purpose of the current meta-analysis of RCTs was to estimate the association of mobile phone intervention with weight-related health measures, including body weight, BMI, waist circumference (WC), waist:hip ratio, and body fat percentage, among overweight and obese adults. In addition, we explored whether the relationship between weight-related measures and mobile phone intervention varied by trial duration (shorter (<6 months) vs. longer (≥6 months)) or by type of intervention (SMS alone vs. SMS combined with MMS).
METHODS
We utilized a standardized written protocol for conducting the literature search, selecting studies, extracting data, and synthesizing results, following the outlines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (22). The PRISMA checklist and flow diagram were used for reporting the results of this analysis (22).
Search strategy and study selection
We conducted a systematic literature search of Medline (via PubMed; National Library of Medicine, Bethesda, Maryland) (1966–March 27, 2014), the Excerpta Medica Database (Embase; Elsevier B.V., Amsterdam, the Netherlands) (1947–March 27, 2014), the Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Collaboration, Oxford, United Kingdom) (March 2014 issue), and Web of Science (Thomson Reuters, New York, New York) (1976–March 27, 2014) to identify trials examining the association of mobile phone intervention with weight-related measures. Details on the search strategy are presented in the Web Appendix (available at http://aje.oxfordjournals.org/). Briefly, our literature search strategy combined all synonyms for the intervention “cellular phone” with all synonyms for the outcomes “weight loss,” “body mass index,” “waist circumference,” “waist-to-hip ratio,” or “body fat.” The search was limited to adults aged ≥18 years, with no language restrictions. A manual search of all references from eligible articles, reviews, systematic reviews, and meta-analyses was performed.
To determine eligibility for the meta-analysis, 2 investigators independently reviewed each of the articles generated by the literature search after removal of duplicates. BMI was calculated as kilograms of weight per square meter of height. To be included in the meta-analysis, a study had to meet the following criteria: 1) participants were at least 18 years of age; 2) at least 80% of the study participants were overweight or obese (the BMI cutpoint for overweight/obesity was ≥25 units (23)); 3) the application of mobile phone messaging was part of the intervention; 4) the only difference between intervention and control groups was the mobile phone intervention; 5) mobile phone intervention included delivery of information on healthy eating, physical activity, or weight loss; 6) changes in body weight, BMI, WC, waist:hip ratio, or body fat percentage or data with which to calculate the changes in these measures were provided, along with a measure of variance or confidence interval; and 7) allocation to the intervention or control group was random. If the results of a study had been published more than once, only the article with the most complete and up-to-date information was included in the analysis. Any between-reviewer discrepancies regarding study eligibility were resolved by reviewer discussion and consensus.
Data extraction
A standardized data abstraction form was used to obtain information from selected articles (see Web Appendix). Two investigators independently abstracted the following items from eligible articles: general study information (including title, authors, name of the trial, and year of publication), study characteristics (including study design, primary outcome of the study, randomization, blinding, outcome measurement, and statistical analysis methods), participant characteristics (including age, sex, race/ethnicity, and comorbid conditions), information about the intervention (including intervention type, duration, frequency, and feedback requirements), and study outcome measures (including body weight, BMI, WC, waist:hip ratio, or body fat percentage). Abstraction results were compared, and discrepancies were resolved by discussion and consensus. If any data were missing or incomplete, the original study authors were contacted (20).
Quality assessment of individual trials
A standardized 5-point Jadad scale was used to examine the quality of selected studies, which included assessment of the following items: randomization, blinding, description of dropout and withdrawal, and evaluation of randomization and blinding (24). Two investigators assessed the articles independently, and discrepancies were resolved by discussion and consensus. Quality assessment details and the score for each trial are given in Web Table 1.
Data synthesis and statistical analysis
For each RCT, if the net effect size was not provided, the net effect size was calculated as the change in body weight–related measures resulting from treatment (T) (from baseline (B) to the end of intervention) in the intervention group minus the change in body weight–related measures in the control (C) group: (XTT − XTB) – (XCT – XCB). For studies without variance data, we calculated the variance from confidence intervals or test statistics. If the variance for change between baseline and the end of the intervention (σΔ) was not reported, it was calculated from the following equation (25):
where σpre corresponds to the variance at baseline, σpost corresponds to the variance at the end of intervention, and ρ is the correlation coefficient for correlations between measurements taken at baseline and the end of intervention (ρ estimates of 0.925 for the intervention group and 0.959 for the control group were imputed based on reported data (26)). Since a ρ value of 0.5 is frequently imputed, we also conducted a sensitivity analysis using this ρ value (13).
Random-effects models were used to pool net change estimates across trials. The heterogeneity of net changes was assessed across studies using the Cochrane Q and I2 statistics (27). We also conducted analyses using 2 a priori-defined subgroups to examine the associations of mobile phone intervention with weight loss on the basis of study duration (<6 months or ≥6 months) and type of intervention (SMS only or both SMS and MMS). We also performed a meta-regression analysis examining study duration as a continuous measure. To further assess the robustness of our findings, we performed several sensitivity analyses by restricting the data on the basis of quality parameters—for example, restricting the analyses to high-quality trials (Jadad score ≥3 (24)), trials with weight control as the primary outcome, trials using intention-to-treat (ITT) analysis, trials with an intervention frequency of ≥1 message/day, trials with outcome measurement by a physician, trials requiring feedback, or trials with a sample size of ≥40—or excluding trials with normal-weight participants or clustered RCTs. We also removed each trial sequentially to determine the magnitude of its influence on the overall pooled estimates.
Publication bias was evaluated using visual inspection of funnel plots which plotted the standard errors against the net change for each study and also using Egger's test to assess the asymmetry of the funnel plot (28). The Duval and Tweedie nonparametric “trim-and-fill” method (29) was used to examine any influence of publication bias on meta-analysis findings. All of the analyses were conducted using Stata software, version 12.0 (StataCorp LP, College Station, Texas). A 2-sided P value less than 0.05 was considered statistically significant.
RESULTS
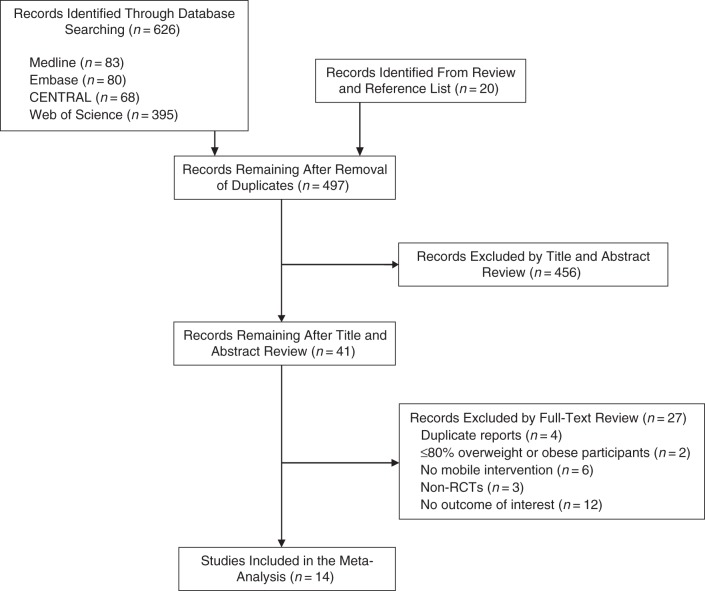
Of the 497 relevant citations retrieved, 14 trials of 1,337 randomized participants were included in the current meta-analysis (Figure 1). Characteristics of the 14 trials in the current meta-analysis are shown in Table 1, and detailed information on types of mobile phone intervention is presented in Web Table 2. The trials, published between 2004 and 2013, varied in size from 30 participants to 250 participants. Study durations ranged from 8 weeks to 12 months. Most of the studies had been conducted in the United States or European countries, while 1 study was conducted in South Korea (19). Participants in intervention groups received mobile phone interventions, including SMS or MMS. Intervention frequency, feedback requirements (requiring participant response to the delivery service), and outcome measurements varied across trials. Of the 14 trials, 8 were conducted to assess the primary outcome of weight loss, 7 applied ITT analysis, and 13 were categorized as high-quality (Jadad score ≥3).
Figure 1.
Selection of eligible randomized controlled trials (RCTs) examining the association of mobile phone intervention with weight-related measures, 2004–2013. CENTRAL, Cochrane Central Register of Controlled Trials.
Table 1.
Characteristics of 14 Randomized Controlled Trials That Examined the Association of Mobile Phone Intervention With Net Change in Weight-Related Measures Among Overweight and Obese Adults, 2004–2013
| First Author, Year (Reference No.) | No. of Participants | Country | Study Design | Study Population | Duration of Study | Blinding | Weight Loss as Primary Outcome | Type of Intervention | Control Group Treatment | Intervention Frequency | Feedback Requirement | Outcome | Anthropometric Measurement | Intention-to-Treat Analysisa | Jadad Scoreb |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Márquez Contreras, 2004 (30) | 67 | Spain | Clustered RCT | Persons with HT | 6 months | No | Noc | SMS + usual care | Usual care | 2 times/week | No | BW | PM | No | 3 |
| Hurling, 2007 (15) |
77 | United Kingdom | RCT | GP | 9 weeks | No | Nod | SMS + PA monitoring | PA monitoring | As appropriate | Yes | BMIe, body fat % | PM | Yes | 3 |
| Faridi, 2008 (31) |
30 | United States | Clustered RCT | Persons with DM | 3 months | No | Nof | SMS | Standard self-management | Once per day | Yes | BW, BMI | PM | Yes | 3 |
| Helsel, 2009 (32) |
30 | United States | RCT | GP | 16 weeks | NR | Yes | IPWP + SMS | IPWP | 3 times/day | NR | BW | NR | Yes | 2 |
| Haapala, 2009 (17) | 125 | Finland | RCT | GP | 12 months | No | Yes | SMS | No intervention | As appropriate | Yes | BW, WC | PM | Yes | 3 |
| Patrick, 2009 (18) |
65 | United States | RCT | GP | 16 weeks | No | Yes | SMS + MMS + paper materials | Paper materials | 2–5 times/day | Yes | BW | PM | Yes | 3 |
| Yoo, 2009 (19) |
111 | South Korea | RCT | Persons with HT and DM | 12 weeks | No | Nog | SMS | Usual outpatient treatment | 3 times/day | Yes | BW, BMI, WC | Self-measurement | No | 3 |
| Zuercher, 2009 (33) |
177 | United States | RCT | GP | 1 month | No | Yes | SMS + standard care | Standard care | Once per day | Yes | BW, BMI | Self-report | No | 3 |
| Lombard, 2010 (34) | 250 | Australia | Clustered RCT | GP | 12 months | Single | Yes | SMS + pedometer + group sessions | Group sessions + pedometer | Once per month | No | BW, WC | PM | No | 5 |
| Turner-McGrievy, 2011 (20) | 102 | United States | RCT | GP | 6 months | Single | Yes | SMS + podcast | No support | ≥2 times/day | No | BW | PM | Yes | 3 |
| Shapiro, 2012 (35) |
170 | United States | RCT | GP | 12 months | No | Yes | SMS + MMS + monthly e-newsletters | Monthly e-newsletters | 4 times/day | Yes | BW | PM | Yes | 3 |
| Orsama, 2013 (21) | 48 | Canada | RCT | Persons with HT and DM | 10 months | No | Noc,f | SMS + education | Education | As appropriate | Yes | BW | Self-report | No | 3 |
| Napolitano, 2013 (36) | 35 | United States | RCT | GP | 8 weeks | No | Yes | SMS + Facebookh | Once per day | Yes | BW | PM | No | 3 | |
| Steinberg, 2013 (37) | 50 | United States | RCT | GP | 6 months | No | Yes | SMS + usual care | Usual care | ≥1 time per day | Yes | BW, BMI | PM | Yes | 3 |
Abbreviations: BMI, body mass index; BW, body weight; DM, diabetes mellitus; GP, general population; HT, hypertension; IPWP, in-person weight-loss program; MMS, multimedia message service; NR, not reported; PA, physical activity; PM, physician measurement; RCT, randomized controlled trial; SMS, short message service; WC, waist circumference; WHR, waist:hip ratio.
a Identified by the extracted data.
b Based on the 5-item Jadad scale (24).
c The primary outcome was lowering blood pressure.
d The primary outcome was increasing PA.
e Weight (kg)/height (m)2.
f The primary outcome was lowering blood glucose level.
g The primary outcome was chronic disease self-management.
h Facebook, Inc. (Menlo Park, California).
Table 2 shows characteristics of participants at baseline in the intervention and control groups, respectively. The average age ranged from 20.5 years to 57.0 years. The percentage of males ranged from 0% to 54% in the intervention groups and from 0% to 65% in the control groups. Average BMI ranged from 25.6 to 35.8 in intervention groups and from 25.5 to 36.9 in control groups. Five trials included participants with hypertension or type 2 diabetes.
Table 2.
Characteristics of Participants in 14 Randomized Controlled Trials That Examined the Association of Mobile Phone Intervention With Net Change in Weight-Related Measures Among Overweight and Obese Adults, 2004–2013
| First Author, Year (Reference No.) | Intervention Group |
Control Group |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Persons | Mean Age, years (SD) |
Male Sex |
Mean BMIa (SD) |
Mean Body Weight, kg (SD) | Mean WC, cm (SD) |
No. of Persons | Mean Age, years (SD) |
Male Sex |
Mean BMI (SD) |
Mean Body Weight, kg (SD) |
Mean WC, cm (SD) |
|||
| No. | % | No. | % | |||||||||||
| Márquez Contreras, 2004 (30) |
34 | 52.3 (10.2) | 18 | 52.9 | 82.0 (10.9) | 33 | 59.4 (10.9) | 16 | 47.6 | 79.8 (13.6) | ||||
| Hurling, 2007 (15) |
47 | 40.5 (7.1) | 17 | 36.2 | 26.2 (2.8) | 75.1 (11.7) | 30 | 40.1 (7.7) | 9 | 30.0 | 26.5 (4.1) | 73.9 (10.2) | ||
| Faridi, 2008 (31) |
15 | 55.3 (8.7) | 6 | 40.0 | 34.3 (7.4) | 93.7 (24.1) | 15 | 56.7 (10.6) | 5 | 33.3 | 36.9 (12.5) | 100.5 (28.8) | ||
| Helsel, 2009 (32)b,c |
15 | 44.2 (3.9) | 31.2 (2.4) | 15 | ||||||||||
| Haapala, 2009 (17) |
62 | 38.1 (4.7) | 13 | 21.0 | 30.6 (2.7) | 87.5 (12.6) | 98.5 (10.3) | 63 | 38.0 (4.7) | 15 | 24.0 | 30.4 (2.8) | 86.4 (12.5) | 96.6 (10.4) |
| Patrick, 2009 (18) |
33 | 47.4 (7.1) | 8 | 24.2 | 32.8 (4.3) | 89.8 (17.2)d | 32 | 42.4 (7.5) | 5 | 15.6 | 33.5 (4.5) | 88.0 (13.1)d | ||
| Yoo, 2009 (19) |
57 | 57.0 (9.1) | 30 | 52.6 | 25.6 (3.5) | 66.4 (12.5) | 89.5 (9.7) | 54 | 59.4 (8.4) | 35 | 64.8 | 25.5 (3.3) | 67.7 (10.8) | 91.3 (7.5) |
| Zuercher, 2009 (33) |
88 | 23.6 (3.5) | 0 | 0 | 26.1 (5.2) | 72.5 (15.6) | 89 | 24.0 (3.4) | 0 | 0 | 27.1 (7.5) | 73.8 (21.1) | ||
| Lombard, 2010 (34) |
127 | 40.6 (4.8) | 0 | 0 | 27.5 (5.1) | 73.2 (13.8) | 94.8 (12.6) | 123 | 40.3 (4.8) | 0 | 0 | 28.1 (5.8) | 74.6 (16.1) | 96.8 (14.6) |
| Turner-McGrievy, 2011 (20) | 47 | 42.6 (10.7) | 11 | 23.0 | 32.9 (4.8) | 49 | 43.2 (11.7) | 13 | 27.0 | 32.2 (4.5) | ||||
| Shapiro, 2012 (35) |
81 | 43.1 (11.1) | 27 | 33 | 32.4 (4.2) | 91.6 (17.2) | 89 | 40.9 (12.1) | 32 | 64 | 32.0 (4.0) | 92.9 (17.9) | ||
| Orsama, 2013 (21) |
27 | 62.3 (6.5) | 13 | 54.0 | 30.7 (4.5) | 26 | 61.5 (9.1) | 13 | 54.0 | 33.5 (8.0) | ||||
| Napolitano, 2013 (36)c |
18 | 20.5 (2.2) | 5 | 13.5 | 31.4 (5.3) | 86.5 (17.1) | 17 | |||||||
| Steinberg, 2013 (37) |
26 | 37.6 (7.4) | 0 | 0 | 35.8 (6.1) | 102.0 (16.6) | 24 | 39.0 (9.0) | 0 | 0 | 34.6 (5.8) | 96.0 (23.1) | ||
Abbreviations: BMI, body mass index; SD, standard deviation; WC, waist circumference.
a Weight (kg)/height (m)2.
b This conference poster stated only that the total sample size was 30; we assumed there were 15 participants in each group.
c Only average age, number of males, and average body weight for all participants were reported.
d For participants analyzed in terms of body weight change.
Among the 14 trials, 13 reported comparisons of body weight (17–21, 30–37), 5 reported comparisons of BMI (15, 19, 31, 33, 37), 3 reported comparisons of WC (17, 19, 34), and 1 reported a comparison of body fat percentage (15) (Table 3). Body weight change ranged from −5.16 kg to −0.05 kg in intervention groups and from −2.60 kg to 1.41 kg in control groups; BMI change ranged from −0.50 units to 0 units in intervention groups and from −0.50 units to 1.00 unit in control groups; and WC change ranged from −4.50 cm to −1.30 cm in intervention groups and from −2.20 cm to −0.12 cm in control groups.
Table 3.
Average Change in Body Weight–Related Measures Among Participants From 14 Randomized Controlled Trials, 2004–2013
| First Author, Year (Reference No.) |
Intervention Group |
Control Group |
||||
|---|---|---|---|---|---|---|
| Mean Weight Change, kg (SD) | Mean BMIa Change (SD) | Mean WC Change, cm (SD) | Mean Weight Change, kg (SD) | Mean BMI Change (SD) | Mean WC Change, cm (SD) | |
| Márquez Contreras, 2004 (30) | −5.16 (4.30) | −0.20 (3.86) | ||||
| Hurling, 2007 (15) | −0.24 (0.75) | 0.10 (0.77) | ||||
| Faridi, 2008 (31) | −0.05 (2.45) | 0 (0.41) | 1.41 (3.40) | 1.00 (3.49) | ||
| Helsel, 2009 (32) | −4.9 (5.4) | −2.6 (3.4) | ||||
| Haapala, 2009 (17) | −3.1 (4.9) | −4.5 (5.3) | −0.7 (4.7) | −1.6 (4.5) | ||
| Patrick, 2009 (18) | −2.10 (2.99) | −0.40 (3.00) | ||||
| Yoo, 2009 (19) | −1.10 (4.88) | −0.50 (1.36) | −2.70 (3.78) | −1.30 (3.06) | −0.50 (0.94) | −2.20 (2.16) |
| Zuercher, 2009 (33) | −0.5 (2.5) | −0.2 (0.9) | 0 (2.2) | 0 (0.8) | ||
| Lombard, 2010 (34) | −0.20 (3.70) | −1.30 (5.99) | 0.83 (3.76) | −0.12 (5.73) | ||
| Turner-McGrievy, 2011 (20) | −2.57 (2.60) | −2.45 (4.39) | ||||
| Shapiro, 2012 (35) | −1.65 (5.45) | −1.03 (4.26) | ||||
| Orsama, 2013 (21) | −2.10 (3.75) | 0.40 (3.75) | ||||
| Napolitano, 2013 (36) | −2.4 (2.5) | −0.63 (2.40) | ||||
| Steinberg, 2013 (37) | −1.27 (6.51) | −0.47 (2.42) | 1.14 (2.53) | 0.42 (0.90) | ||
Abbreviations: BMI, body mass index; SD, standard deviation; WC, waist circumference.
a Weight (kg)/height (m)2.
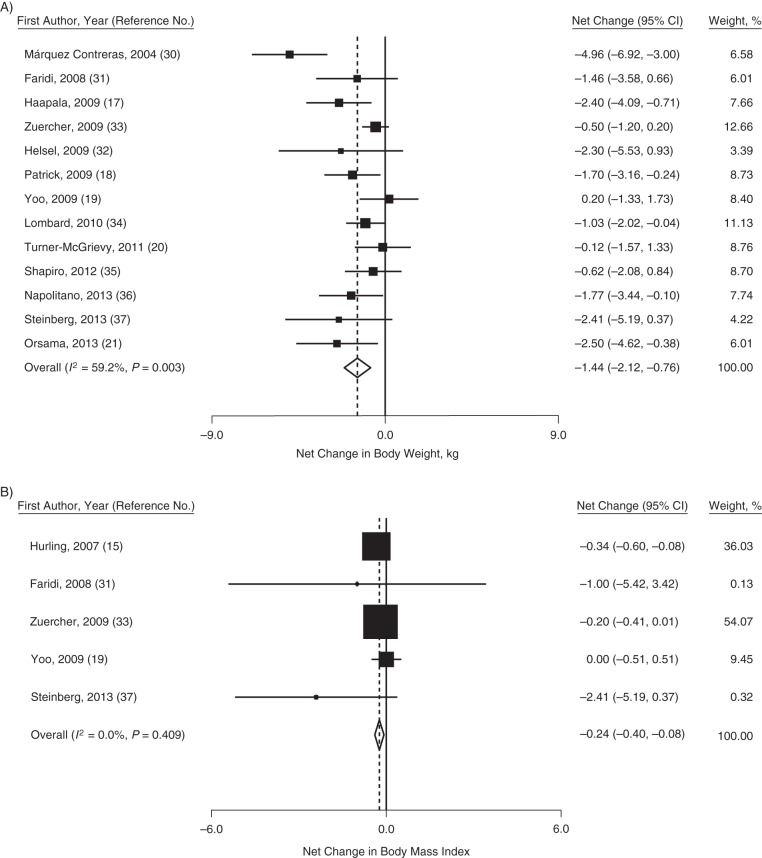
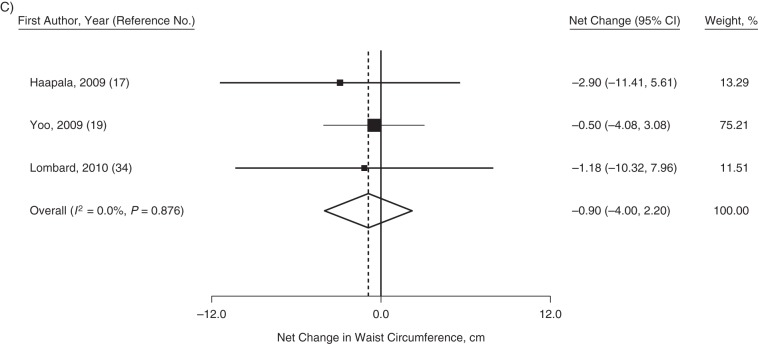
Pooled estimates of the net changes in body weight, BMI, and WC are presented in parts A–C of Figure 2, respectively. On average, compared with the control group, mobile phone intervention resulted in significant decreases in body weight, with a net body weight change of −1.44 kg (95% confidence interval (CI): −2.12, −0.76; P < 0.001, I2 = 59.2%). Similarly, BMI was also significantly decreased in response to the mobile phone intervention, with a net BMI change of −0.24 units (95% CI: −0.40, −0.08; P = 0.41, I2 = 0). In comparison with the control group, no statistically significant difference in WC was associated with mobile phone intervention, with a pooled net change estimate of −0.90 cm (95% CI: −4.00, 2.20; P = 0.88, I2 = 0), but this result was based on only 3 trials.
Figure 2.
Average net change in body weight (kg) (A), body mass index (weight (kg)/height (m)2) (B), and waist circumference (cm) (C) in randomized controlled trials comparing persons receiving weight-related mobile phone intervention with a control group, 2004–2013. The size of each square is proportional to the percent weight that each study contributed in the pooled estimate. The pooled effect size is indicated by the diamond. Bars, 95% confidence intervals (CI).
Subgroup analyses for body weight, BMI, and WC were generally consistent with overall findings (Table 4), showing no significant differences in weight-related measures between trials of shorter and longer duration (P for difference = 0.33) or trials employing only SMS versus those employing SMS plus MMS (P for difference = 0.71). Furthermore, meta-regression analysis revealed no association between trial duration as a continuous variable and net change estimates (data not shown; P = 0.62). In order to examine the robustness of our findings, we also conducted sensitivity analyses restricting the data on the basis of quality parameters. The pooled net change estimates were not substantially different from the overall estimates (Table 4). In addition, the net changes were similar to the overall estimates when we imputed a ρ value of 0.5 to estimate variance in the 2 studies that did not present variance estimates for the change measures. Results of the influence analysis did not identify any trials whose removal would have significantly altered the findings (Web Figure 1).
Table 4.
Results From Subgroup Analyses and Sensitivity Analyses of Net Change in Body Weight, Body Mass Index, and Waist Circumference in a Meta-Analysis of 14 Randomized Controlled Trials, 2004–2013
| Analysis | Body Weight |
Body Mass Indexa |
Waist Circumference |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Net Change, kg | 95% CI | Heterogeneity |
No. of Studies | Net Change | 95% CI | Heterogeneity |
No. of Studies | Net Change, cm | 95% CI | Heterogeneity |
||||
| I2, % | P Value | I2, % | P Value | I2, % | P Value | ||||||||||
| All studies | 13 | −1.44 | −2.12, −0.76 | 59.2 | 0.003 | 5 | −0.24 | −0.40, −0.08 | 0 | 0.409 | 3 | −0.90 | −0.40, 2.20 | 0 | 0.876 |
| Subgroup analysis | |||||||||||||||
| Study duration | |||||||||||||||
| <6 months | 6 | −0.92 | −1.58, −0.25 | 20.9 | 0.276 | 3 | −0.27 | −0.51, −0.04 | 0 | 0.487 | |||||
| ≥6 months | 7 | −1.85 | −2.99, −0.71 | 70.1 | 0.003 | 2 | −0.85 | −2.83, 1.12 | 58.5 | 0.121 | 2 | −2.10 | −8.33, 4.13 | 0 | 0.787 |
| Type of intervention | |||||||||||||||
| SMS only | 11 | −1.53 | −2.34, −0.73 | 64.8 | 0.002 | ||||||||||
| SMS + MMS | 2 | −1.16 | −2.22, −0.10 | 4.9 | 0.305 | ||||||||||
| Sensitivity analysis | |||||||||||||||
| High-quality trialsb | 12 | −1.41 | −2.11, −0.71 | 62.0 | 0.002 | 5 | −0.24 | −0.40, −0.08 | 0 | 0.409 | 3 | −0.90 | −0.40, 2.21 | 0 | 0.876 |
| Exclusion of studies with normal-weight participants | 10 | −1.27 | −1.91, −0.63 | 21.5 | 0.245 | 2 | −0.85 | −2.83, 1.12 | 58.5 | 0.121 | 2 | −0.86 | −4.16, 2.44 | 0 | 0.610 |
| Weight control was the primary outcome | 9 | −1.05 | −1.55, −0.54 | 16.4 | 0.296 | 2 | −0.54 | −1.65, 0.57 | 21.0 | 0.282 | 2 | −2.10 | −8.33, 4.13 | 0 | 0.787 |
| Use of ITT analysis | 7 | −1.30 | −1.99, −0.60 | 4.6 | 0.392 | 3 | −0.49 | −1.23, −0.24 | 8.6 | 0.335 | |||||
| Frequency of contact ≥1 time/day | 9 | −0.79 | −1.28, −0.29 | 5.7 | 0.388 | 3 | −0.58 | −2.03, 0.87 | 32.3 | 0.228 | |||||
| Physician measurement | 9 | −1.68 | −2.53, −0.84 | 58.7 | 0.013 | 4 | −0.24 | −0.44, −0.04 | 22.4 | 0.276 | 2 | −2.10 | −8.33, 4.13 | 0 | 0.787 |
| Feedback requirement | 9 | −1.20 | −1.83, −0.57 | 33.5 | 0.150 | 5 | −0.24 | −0.40, −0.08 | 0 | 0.409 | 2 | −0.86 | −4.16, 2.44 | 0 | 0.610 |
| Sample size ≥40 | 10 | −1.40 | −2.20, −0.60 | 68.0 | 0.001 | 4 | −0.27 | −0.40, −0.10 | 1.8 | 0.383 | 3 | −0.90 | −0.40, 2.20 | 0 | 0.876 |
| Exclusion of clustered RCTs | 10 | −1.10 | −1.71, −0.49 | 34.6 | 0.131 | 4 | −0.24 | −0.44, −0.08 | 22.4 | 0.276 | 2 | −0.86 | −4.16, 2.44 | 0 | 0.610 |
| Exclusion of non-peer-reviewed studies | 11 | −1.56 | −0.78, −2.34 | 59.6 | 0.006 | 4 | −0.29 | −0.52, −0.05 | 18.8 | 0.297 | 3 | −0.90 | −0.40, 2.20 | 0 | 0.876 |
Abbreviations: CI, confidence interval; ITT, intention-to-treat; MMS, multimedia message service; RCT, randomized controlled trial; SMS, short message service.
a Weight (kg)/height (m)2.
b Jadad score ≥3 (24).
The funnel plot demonstrated that the distribution of net body weight change estimates for individual studies was somewhat asymmetrical (Figure 3A), and Egger's test indicated significant publication bias (P = 0.04). Application of the nonparametric trim-and-fill method to assess the potential influence of publication bias on our findings resulted in virtually unchanged net body weight change. In addition, there was little evidence of publication bias for BMI change (Figure 3B) and WC change (Figure 3C) (P = 0.42 and P = 0.40, respectively).
Figure 3.
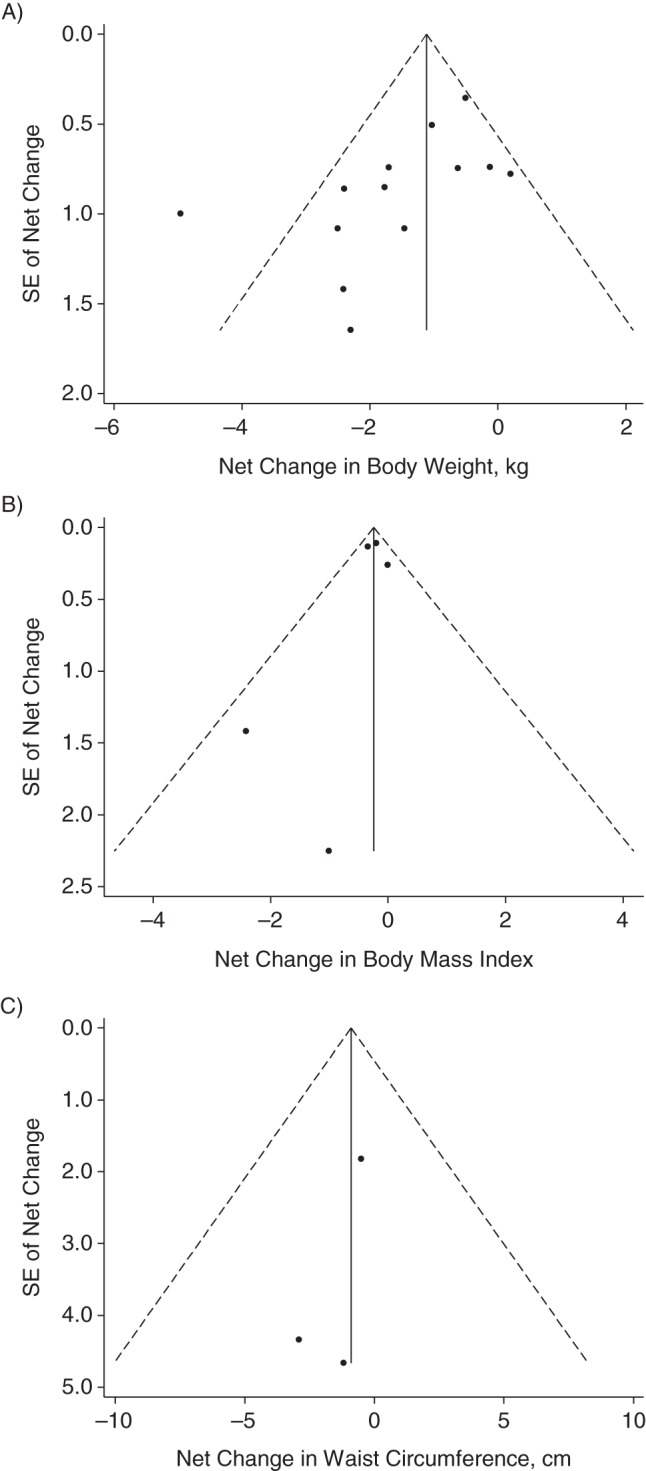
Funnel plots from a meta-analysis of the association of mobile phone intervention with body weight change (kg) (A), body mass index change (weight (kg)/height (m)2) (B), and waist circumference change (cm) (C), 2004–2013. SE, standard error.
DISCUSSION
The current meta-analysis, incorporating data from 14 published and unpublished RCTs on more than 1,300 participants, documented significant decreases of approximately 1.44 kg in body weight and 0.24 units in BMI associated with mobile phone intervention. Body weight decreases were not significantly different between shorter- and longer-duration trials, although statistical power for confirming possibly larger net changes with longer-duration trials was limited. Furthermore, the association of mobile phone intervention with weight loss did not differ by type of mobile phone intervention (SMS or SMS and MMS combined), and findings were robust across sensitivity analyses. Although there was no association between mobile phone intervention and waist circumference, this negative finding may be explained by the very limited number of trials assessing this body weight–related measure. In aggregate, our findings indicated that mobile phone intervention could be an important strategy for promoting weight loss.
We identified significant reductions in body weight and BMI of 1.44 kg and 0.24 units, respectively, due to mobile phone intervention in comparison with the control group. In a previous systematic review, Stephens and Allen (38) suggested that mobile phone intervention is effective for increasing physical activity and/or reducing overweight/obesity. The current meta-analysis provides important quantitative evidence of the benefits of mobile phone intervention in body weight and BMI reduction from the accumulation of RCT results in this area.
Of particular importance was our finding of nonsignificant differences between the weight reductions observed in trials of shorter duration and those of longer duration. While some previous studies have found that lifestyle intervention can result in meaningful, sustained weight loss (39), several others have observed body weight regain after 6 months' intervention (13, 26, 40, 41). Such results may be due to reduced intervention compliance. Mobile phone intervention is convenient for study participants, and the widespread use of and accessibility of mobile phones facilitates high compliance. Findings from the current meta-analysis indicate that methods such as mobile phone intervention, which delivers frequent reminders about healthy eating and physical activity and other information related to weight loss, may be a potentially useful tool for achieving successful long-term weight management (42–44).
To our knowledge, the current study is the first meta-analysis of RCTs to have assessed the association of mobile phone intervention with weight loss. One strength of this study was the inclusion of only RCTs, reducing the likelihood that the observed association between mobile phone intervention and overweight/obesity-related traits can be explained entirely by bias and confounding. In addition, only 6 of the 14 trials of body weight and only 1 of the 5 trials of BMI had individually statistically significant results, highlighting the benefits of meta-analysis for identifying important effect sizes with increased statistical power.
Still, some limitations of this study should be addressed. Although we searched for and included “gray literature” in the current meta-analysis, there was some indication of possible publication bias for the body weight trait. However, the results were virtually unchanged upon application of the trim-and-fill method for assessment of the potential influence of publication bias. Furthermore, restricting the meta-analysis to only larger trials had no influence on the findings. In addition, there was considerable heterogeneity in the pooled estimates of net change in body weight (59%). Heterogeneity was substantially reduced when we restricted the meta-analysis to trials using ITT analysis and trials with an intervention frequency of ≥1 message/day, suggesting that these factors could contribute to inconsistency between studies. While we found evidence that weight loss could be sustained in trials of longer duration, there were no trials of over 1 year's duration. Therefore, more research is needed to determine whether mobile phone intervention can maintain its benefits over longer periods of time. In addition, investigators in 6 of the 14 trials did not apply ITT analysis. However, sensitivity analyses restricted to only studies using ITT analysis produced findings similar to the overall pooled estimate. Moreover, nearly all trials included in the current meta-analysis were conducted in high-income countries in North America and Europe. The paucity of data from low- and middle-income nations limits the generalizability of meta-analysis findings to these areas.
While numerous studies examined the association of mobile phone intervention with body weight, fewer studies examined the associations with BMI and WC. Subgroup and sensitivity analyses were probably underpowered and, under some circumstances, could not be conducted for BMI and WC traits. It is also likely that the main WC analysis was substantially underpowered to detect the seemingly modest benefits of mobile phone intervention. In addition, no studies examined the associations of mobile phone intervention with waist:hip ratio, and only 1 study examined its benefit in reducing body fat percentage. Therefore, these traits could not be examined in the meta-analysis. Future studies are needed to assess the impact of mobile phone intervention on these important overweight/obesity-related measures.
In conclusion, this meta-analysis provides evidence that mobile phone intervention is an effective strategy for promoting weight loss. While these findings are encouraging, additional trials are required to examine the long-term (>1 year) association of mobile phone intervention with weight loss. Furthermore, studies designed to better understand the associations of mobile phone intervention with WC, waist:hip ratio, and body fat percentage are warranted. Research will also be needed to assess the cost-effectiveness of mobile phone intervention (45–47). In aggregate, the results of the current meta-analysis are promising, suggesting that mobile phone intervention could contribute to meaningful reductions in body weight and BMI at the population level. While the current meta-analysis focused on the individual benefits of mobile phone intervention, combining this approach with other behavioral and lifestyle modifications could prove especially beneficial for achieving weight loss success and helping to curb the worldwide overweight/obesity epidemic.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, Department of Epidemiology, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China (Fangchao Liu, Jie Cao, Shufeng Chen, Jianfeng Huang, Dongfeng Gu); Department of Epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, Louisiana (Fangchao Liu, Xiaomu Kong, Jie Cao, Shufeng Chen, Changwei Li, Tanika N. Kelly); and Department of Endocrinology, China-Japan Friendship Hospital, Beijing, China (Xiaomu Kong).
This research was not funded by any specific grant. F.L., X.K., J.C., and S.C. were supported by the Fogarty International Center of the US National Institutes of Health (award D43TW009107).
We thank Dr. Bonnie Spring and H. Gene McFadden for their help in calculating ρ values using their own data (26). We also thank Dr. Gabrielle Turner-McGrievy for providing more information on the study by Turner-McGrievy and Tate (20).
Conflict of interest: none declared.
REFERENCES
- 1.Abelson P, Kennedy D. The obesity epidemic. Science. 2004;304(5676):1413. doi: 10.1126/science.304.5676.1413. [editorial] [DOI] [PubMed] [Google Scholar]
- 2.Kelly T, Yang W, Chen CS, et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008;32(9):1431–1437. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- 3.Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 4.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12(2):131–141. doi: 10.1111/j.1467-789X.2009.00712.x. [DOI] [PubMed] [Google Scholar]
- 6.Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2004;110(18):2952–2967. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 7.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaukua J, Pekkarinen T, Sane T, et al. Health-related quality of life in obese outpatients losing weight with very-low-energy diet and behaviour modification—a 2-y follow-up study. Int J Obes Relat Metab Disord. 2003;27(10):1233–1241. doi: 10.1038/sj.ijo.0802379. [DOI] [PubMed] [Google Scholar]
- 9.Ryan DH, Kushner R. The state of obesity and obesity research. JAMA. 2010;304(16):1835–1836. doi: 10.1001/jama.2010.1531. [editorial] [DOI] [PubMed] [Google Scholar]
- 10.Kriska AM, Delahanty LM, Pettee KK. Lifestyle intervention for the prevention of type 2 diabetes: translation and future recommendations. Curr Diab Rep. 2004;4(2):113–118. doi: 10.1007/s11892-004-0066-9. [DOI] [PubMed] [Google Scholar]
- 11.Shaw K, O'Rourke P, Del Mar C, et al. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005;(2):CD003818. doi: 10.1002/14651858.CD003818.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Wadden TA, Butryn ML. Behavioral treatment of obesity. Endocrinol Metab Clin North Am. 2003;32(4):981–1003. doi: 10.1016/s0889-8529(03)00072-0. x. [DOI] [PubMed] [Google Scholar]
- 13.Dansinger ML, Tatsioni A, Wong JB, et al. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med. 2007;147(1):41–50. doi: 10.7326/0003-4819-147-1-200707030-00007. [DOI] [PubMed] [Google Scholar]
- 14.Franklin VL, Waller A, Pagliari C, et al. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 15.Hurling R, Catt M, Boni MD, et al. Using Internet and mobile phone technology to deliver an automated physical activity program: randomized controlled trial. J Med Internet Res. 2007;9(2):e7. doi: 10.2196/jmir.9.2.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14(4):255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haapala I, Barengo NC, Biggs S, et al. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutr. 2009;12(12):2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- 18.Patrick K, Raab F, Adams MA, et al. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res. 2009;11(1):e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoo HJ, Park MS, Kim TN, et al. A ubiquitous chronic disease care system using cellular phones and the Internet. Diabet Med. 2009;26(6):628–635. doi: 10.1111/j.1464-5491.2009.02732.x. [DOI] [PubMed] [Google Scholar]
- 20.Turner-McGrievy G, Tate D. Tweets, apps, and pods: results of the 6-month Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. J Med Internet Res. 2011;13(4):e120. doi: 10.2196/jmir.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orsama AL, Lähteenmäki J, Harno K, et al. Active assistance technology reduces glycosylated hemoglobin and weight in individuals with type 2 diabetes: results of a theory-based randomized trial. Diabetes Technol Ther. 2013;15(8):662–669. doi: 10.1089/dia.2013.0056. [DOI] [PubMed] [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 23.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 24.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 25.Thiessen Philbrook H, Barrowman N, Garg AX. Imputing variance estimates do not alter the conclusions of a meta-analysis with continuous outcomes: a case study of changes in renal function after living kidney donation. J Clin Epidemiol. 2007;60(3):228–240. doi: 10.1016/j.jclinepi.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 26.Spring B, Duncan JM, Janke EA, et al. Integrating technology into standard weight loss treatment: a randomized controlled trial. JAMA Intern Med. 2013;173(2):105–111. doi: 10.1001/jamainternmed.2013.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 28.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 30.Márquez Contreras E, de la Figuera von Wichmann M, Gil Guillén V, et al. Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phones (HTA-Alert) Aten Primaria. 2004;34(8):399–405. doi: 10.1016/S0212-6567(04)78922-2. [in Spanish] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Faridi Z, Liberti L, Shuval K, et al. Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self-management: the NICHE pilot study. J Eval Clin Pract. 2008;14(3):465–469. doi: 10.1111/j.1365-2753.2007.00881.x. [DOI] [PubMed] [Google Scholar]
- 32.Helsel DL, Jakicic JM. Effect of adding telephone text message prompts to in-person weight loss program [abstract 788-P] Obesity. 2009;17(suppl 2):S263. [Google Scholar]
- 33.Zuercher JL. Developing Strategies for Helping Women Improve Weight-Related Health Behaviors. Chapel Hill, NC: University of North Carolina at Chapel Hill; 2009. [doctoral dissertation] [Google Scholar]
- 34.Lombard C, Deeks A, Jolley D, et al. A low intensity, community based lifestyle programme to prevent weight gain in women with young children: cluster randomised controlled trial. BMJ. 2010;341:c3215. doi: 10.1136/bmj.c3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shapiro JR, Koro T, Doran N, et al. Text4Diet: a randomized controlled study using text messaging for weight loss behaviors. Prev Med. 2012;55(5):412–417. doi: 10.1016/j.ypmed.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 36.Napolitano MA, Hayes S, Bennett GG, et al. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity (Silver Spring) 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 37.Steinberg DM, Tate DF, Bennett GG, et al. The efficacy of a daily self-weighing weight loss intervention using smart scales and e-mail. Obesity (Silver Spring) 2013;21(9):1789–1797. doi: 10.1002/oby.20396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28(4):320–329. doi: 10.1097/JCN.0b013e318250a3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wadden TA, Neiberg RH, Wing RR, et al. Four-year weight losses in the Look AHEAD Study: factors associated with long-term success. Obesity (Silver Spring) 2011;19(10):1987–1998. doi: 10.1038/oby.2011.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Wier MF, Dekkers JC, Hendriksen IJ, et al. Effectiveness of phone and e-mail lifestyle counseling for long term weight control among overweight employees. J Occup Environ Med. 2011;53(6):680–686. doi: 10.1097/JOM.0b013e31821f2bbb. [DOI] [PubMed] [Google Scholar]
- 41.Champagne CM, Broyles ST, Moran LD, et al. Dietary intakes associated with successful weight loss and maintenance during the Weight Loss Maintenance Trial. J Am Diet Assoc. 2011;111(12):1826–1835. doi: 10.1016/j.jada.2011.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Milsom VA, Middleton KM, Perri MG. Successful long-term weight loss maintenance in a rural population. Clin Interv Aging. 2011;6:303–309. doi: 10.2147/CIA.S25389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shuger SL, Barry VW, Sui X, et al. Electronic feedback in a diet- and physical activity-based lifestyle intervention for weight loss: a randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8:41. doi: 10.1186/1479-5868-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003;289(14):1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 45.Hebden L, Balestracci K, McGeechan K, et al. ‘TXT2BFiT’ a mobile phone-based healthy lifestyle program for preventing unhealthy weight gain in young adults: study protocol for a randomized controlled trial. Trials. 2013;14:75. doi: 10.1186/1745-6215-14-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Batch BC, Tyson C, Bagwell J, et al. Weight loss intervention for young adults using mobile technology: design and rationale of a randomized controlled trial—Cell Phone Intervention for You (CITY) Contemp Clin Trials. 2014;37(2):333–341. doi: 10.1016/j.cct.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Duncan MJ, Vandelanotte C, Rosenkranz RR, et al. Effectiveness of a website and mobile phone based physical activity and nutrition intervention for middle-aged males: trial protocol and baseline findings of the ManUp Study. BMC Public Health. 2012;12:656. doi: 10.1186/1471-2458-12-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.