Abstract
Background
Recent evidence suggests that opening a grocery store in a food desert does not translate to better diet quality among community residents.
Purpose
This study evaluated the influence of proximity to a healthy food store on the effect of a dietary behavioral intervention on diet among overweight/obese adults randomized to either a high fiber or American Heart Association diet intervention.
Methods
Participants were recruited from Worcester County, Massachusetts between May 2009 and January 2012. Dietary data were collected via 24-hour recalls at baseline and 3, 6 and 12 months post-intervention. Based on in-store inspection data, a store was considered as having adequate availability of healthy foods if it had at least one item available in each of 20 healthy food categories. Linear models evaluated maximum change in dietary outcomes in relation to road distance from residence to the nearest healthy food store. The analysis was conducted in January to June 2014.
Results
On average, participants (N=204) were aged 52 years, BMI=34.9 kg/m2, and included 72% women and 89% non-Hispanic whites. Shorter distance to a healthy food store was associated with greater improvements in consumption of fiber (b= −1.07 grams/day per mile, p<0.01) and fruit and vegetables (b= −0.19 servings/day per mile, p=0.03) with and without covariate adjustment.
Conclusions
The effectiveness of dietary interventions is significantly influenced by the presence of a supportive community nutrition environment. Considering the nationwide efforts on promotion of healthy eating, the value of improving community access to healthy foods should not be underestimated.
Introduction
To curb the rising prevalence of obesity and associated chronic diseases, nationwide efforts are being made to improve accessibility of healthy foods in communities. These efforts are well justified because a calorically balanced diet that is low in saturated fat and sodium, and high in fruits and vegetables, is essential for maintaining health and has been associated with lower risk for obesity and related chronic diseases.1 However, nutrient-rich, calorie-light foods are predominantly only available in well-stocked grocery stores.
Many studies, mostly cross-sectional, have shown associations of greater access to healthy foods with better dietary quality and lower prevalence of chronic conditions.2–9 A study of 60,775 postmenopausal women in the U.S. found that greater availability of grocery stores within a 1.5-mile radius of the participant’s home was associated with lower BMI and diastolic blood pressure.10 In the Framingham Heart Study,11 however, living closer to a grocery store was associated with a higher BMI. In the Multi-Ethnic Study of Atherosclerosis (MESA),5 a population-based prospective study of adults aged 45 and older, better access to healthy foods was associated with a 38% lower incidence in type 2 diabetes. Among younger adults, greater availability of grocery stores was not associated with better diet quality.3 To date, the evidence for greater healthy food availability translating into better health in communities remains equivocal.
Two critical issues regarding physical access to healthy foods remain to be answered. The first is whether improving a community’s retail food infrastructure alone will induce desired changes in dietary behaviors. A recent study by Cummins et al.12 reported that the opening of a new supermarket in a low-income Philadelphia community considered a “food desert” did not lead to improvements in fruit and vegetable intake or BMI. These results highlight the importance of concurrent community-based behavioral interventions such as raising awareness and motivating residents for positive behavioral changes, because improved access alone failed to induce desired outcomes. The second issue is to what extent an individual living in a community with limited access to healthy foods can improve their diet. This paper addresses this issue by examining whether access to healthy food stores influences the success of a dietary intervention among community-dwelling obese adults with metabolic syndrome. The analysis used prospectively collected 24-hour dietary recall data on participants of a randomized dietary intervention trial funded by the National Heart, Lung and Blood Institute (NCT00911885), and prospectively collected information on availability and quality of food items in food stores located in close proximity to participants’ residence during the same period.
Methods
Study Population and Setting
Methods for recruiting participants and collection of participant sociodemographic, anthropometric, behavioral, clinical, and dietary data have been described elsewhere.13 Briefly, 240 participants were recruited from Worcester County, Massachusetts and surrounding municipalities between May 2009 and January 2012. The randomized trial was designed to compare the efficacy of two interventional approaches to dietary change among community-dwelling obese adults with metabolic syndrome. The two approaches were: (1) the American Heart Association (AHA) Dietary Guidelines,14 which are the current recommendation for patients with the metabolic syndrome15, 16; and (2) a dietary change condition that focused exclusively on increasing dietary fiber consumption. Participants were randomized to one of the two interventions (n=120 per arm). The dietary intervention for both conditions consisted of 14 sessions (two individual and 12 group) described in detail elsewhere.13 The study protocol was approved by the University of Massachusetts Medical School (UMMS) IRB and all participants gave written informed consent.
The present analysis included 204 (85% of total) participants after excluding 19 without dietary recall data at a post-baseline visit, and an additional 17 whose residential neighborhoods were outside Worcester County, Massachusetts, where no food store data were collected.
Individual-Level Measurements
Dietary intake data were collected via 24-hour recalls at baseline and 3, 6, and 12 months post-intervention. Dietary intake was assessed with a 24-hour recall interview conducted by phone on two randomly selected weekdays and one weekend day, which is the gold standard for collecting dietary intake data among community-living adults. The dietary analysis was conducted using the current version of the multiple-pass, interactive Nutrition Data System for Research (NDS-R, Nutrition Coordinating Center, University of Minnesota, Minneapolis MN). Many measures have been developed to provide a single dietary score for U.S. populations with evidence that the whole-diet eating pattern is important in disease risk.17–19 Dietary quality was measured using the alternate healthy eating index (AHEI),20, 21 which evaluates selected criteria of a healthy cardiovascular diet including: (1) fruit; (2) vegetables; (3) nuts and legumes; (4) ratio of white to red meat; (5) cereal fiber; (6) trans fat; (7) ratio of polyunsaturated fat to saturated fat; and (8) alcohol. Meal locations were identified by participants as where they consumed their food, which were chosen from locations in NDS-R and grouped according to meals eaten “at/away from home.” Percentage of total kilocalories by meal location were then determined.
Anthropometric, sociodemographic, and clinical characteristics were evaluated at the baseline visit including age, race/ethnicity, income, employment status, blood pressure, lipids, and overall physical and mental health. In addition, the investigators assessed several psychosocial variables related to healthy eating, including dietary attitudes, self efficacy, social support, and perceived barriers.
Geographic coordinates of participants’ homes were obtained by geocoding their residential addresses using ArcGIS Desktop, version 10.1 (ESRI, Redlands CA). Participants’ town-level demographic and socioeconomic indicators were obtained from the U.S. Census 2010 and the American Community Surveys. Participants’ neighborhood characteristics of interest included measures of income, educational attainment, housing characteristics, community stability, and urbanicity.
Neighborhood Healthy Food Availability Measurement
There were 106 grocery stores, defined as those selling at least one item of fresh produce year-round, in Worcester County. They were identified annually through on-site surveying and InfoUSA (Infogroup©, Papillion NE) databases using Standard Industrial Classification (SIC) code 5411 and related subsidiary codes, including 541100 (grocery stores), 541101 (supermarkets), 541199 (grocery stores by type and ownership), and 5431 (fruit and vegetable markets) and its subsidiary codes. The stores were surveyed annually between 2007 and 2010.
Healthy food availability was assessed using the validated Community Nutrition Environment Evaluation Data System (C-NEEDS), which is modified from the Nutrition Environment Measures Survey.22 Briefly, the C-NEEDS captures detailed information on availability, quality, and nutrient content of healthy and unhealthy foods sold in food stores in the Northeast region. Key modifications were: (1) inclusion of regionally available and popular foods with improved cultural relevance to the Northeast; (2) addition of canned and frozen foods important to low-income and rural populations; (3) inclusion of foods common to Latino/Hispanic populations; (4) finer assessment of foods containing nutrients deemed beneficial or detrimental to cardiovascular health and weight control (e.g., saturated versus monounsaturated fats, and the inclusion of fiber and other micronutrients); and (5) the addition of a survey form specific for farmer’s markets, wholesale, discount, and superstores that are major food suppliers in the study areas. The C-NEEDS collects data corresponding to the key components of the U.S. Department of Agriculture dietary guidelines,23 which encourage the consumption of a higher-nutrient/lower-calorie diet rich in vegetables and fruits; whole-grains, high-fiber bread and cereal products; and a selection of processed foods low in saturated fat (such as snack foods, bakery items, animal and vegetable proteins, and dairy).
Healthy food availability index (HFAI) was derived for each store following procedures developed by Glanz and colleagues22 and Franco et al.24 Minor modifications were made to the HFAI to suit the C-NEEDS data. The HFAI ranged from 0 to 33 points, with a higher score indicating a greater availability of healthy foods. The HFAI scores had inter-rater reliability of 0.99 and intra-rater reliability of 0.98. Adequate availability of healthy foods is defined herein as at or above the median HFAI (≥20) in surveyed food stores or having at least one item available in each of the 20 healthy food categories (Appendix Table 1, available online).
The road network distance in miles and motor vehicle travel time in minutes from the participant residence to the closest food store with adequate healthy food availability were calculated using ArcGIS, version 10.1. Other density measures included any and number of stores with HFAI ≥20 within 0.5, 1, 2, 3 miles or 5, 15, or 30 minutes of drive time from residence. Data analysis was conducted between January and June 2014.
Statistical Analysis
Means/SDs and frequency distributions were calculated to describe the study population at baseline according to proximity to a store with adequate availability of healthy foods. The main outcomes under analysis were the maximum (or peak) and time-specific changes over the study duration in total dietary fiber (grams/day), servings of fruit and vegetable consumption, whole grains (servings/day), and overall dietary quality as measured by the AHEI. Changes from baseline in dietary outcomes were regressed on distance to a healthy food store using an ANCOVA model adjusting for baseline dietary value. A full range of town- and individual-level variables was initially considered for analysis and final selection of variables based on stepwise backwards elimination approach. The final models adjusted for social support for healthy eating, and indicator variables for diet intervention group (fiber versus AHA), age (≥50 years versus <50 years), and annual gross household income (≥$40,000 versus <$40,000). Participants living within the same town/city were treated as a cluster in the models to obtain robust variances. Model assumptions were carefully examined and met. All analyses were conducted using Stata, version 12.1 (StataCorp LP, College Station TX).
Results
The mean age of participants was 52 years (range, 20–72 years), 72% were women, and 89% white. Almost half of the participants had at least a bachelor’s degree and one third reported a gross household income exceeding $75,000 per year.
In total, 106 food stores were evaluated during the study period. Approximately 57% had an HFAI ≥20 points. The mean (SD) of HFAI was 20.9 (11.5). The median distance from home to the nearest grocery store was 1.58 miles (range, 0.07–8.50), and distance to the nearest store with an HFAI ≥20 was 1.85 miles (range, 0.18–8.85).
Table 1 presents participant baseline characteristics according to the median cutpoint of road network distance to a food store with adequate healthy food options. Participants living farther from a food store with adequate healthy options were more likely to be white, have an annual household income of at least $40,000, and consume a better quality diet with more dietary fiber. There were no significant differences between other baseline characteristics and distance to food stores with adequate healthy food.
Table 1.
Participants’ characteristics by road distance to the nearest healthy food store
| Characteristic | Distance (Median=1.84 miles) | p-value | |||
|---|---|---|---|---|---|
| <1.84 (n=102) | >=1.84 (n=102) | ||||
| Sociodemographic | Mean | SD | Mean | SD | |
| Age (years) | 52.3 | 10.1 | 53.7 | 9.1 | 0.28 |
| Female [n (%)] | 76 | 74.5 | 72 | 70.6 | 0.53 |
| White [n (%)] | 83 | 81.4 | 100 | 98.0 | <0.01 |
| Work full/part-time [n (%)] | 59 | 59.0 | 71 | 69.6 | 0.12 |
| Gross household income | |||||
| 0–$40,000 [n (%)] | 24 | 23.5 | 11 | 10.8 | |
| $40,000+ [n (%)] | 57 | 55.9 | 69 | 67.6 | 0.05 |
| Treatment group | |||||
| AHA | 51 | 50.0 | 53 | 52.0 | |
| High fiber | 51 | 50.0 | 49 | 48.0 | 0.78 |
| Anthropometric and clinical | |||||
| Body mass index (kg/m2) | 34.8 | 3.1 | 34.9 | 2.8 | 0.85 |
| Sedentary activity (min/week) | 17.6 | 23.6 | 22.5 | 28.7 | 0.18 |
| Systolic blood pressure (mmHg) | 137.0 | 9.8 | 135.0 | 9.5 | 0.13 |
| Diastolic blood pressure (mmHg) | 81.0 | 8.9 | 79.9 | 8.7 | 0.36 |
| HDL (mg/dL) | 47.3 | 9.4 | 48.9 | 10.6 | 0.26 |
| Triglycerides (mg/dL) | 151.0 | 76.0 | 153.2 | 82.4 | 0.84 |
| Glucose (mg/dL) | 99.8 | 14.3 | 99.5 | 10.4 | 0.83 |
| HbA1c (%) | 5.7 | 0.4 | 5.7 | 0.4 | 0.98 |
| Insulin (uIU/mL) | 14.8 | 13.7 | 15.1 | 12.9 | 0.90 |
| HOMA-IR | 3.7 | 3.7 | 3.8 | 3.7 | 0.90 |
| CES-Depression score | 7.1 | 5.8 | 6.4 | 5.4 | 0.41 |
| Physical health scale | 46.0 | 8.8 | 47.1 | 8.4 | 0.38 |
| Mental health scale | 51.5 | 8.0 | 51.5 | 8.0 | 0.99 |
| Dietary variables | |||||
| Alternate healthy eating index (0–80) | 31.5 | 9.0 | 34.3 | 9.2 | 0.03 |
| Total energy intake (kilocalories/day) | 1896.1 | 637.5 | 1909.9 | 625.5 | 0.88 |
| Fat (% of total kilocalories) | 33.3 | 6.1 | 32.5 | 5.5 | 0.34 |
| Saturated fat (% of total kilocalories) | 11.8 | 2.8 | 11.1 | 2.5 | 0.06 |
| Carbohydrate (% of total kilocalories) | 48.1 | 7.7 | 47.1 | 6.8 | 0.33 |
| Protein (% of total kilocalories) | 17.0 | 4.2 | 17.3 | 3.5 | 0.61 |
| Total dietary cholesterol (mg/day) | 262.6 | 132.4 | 260.5 | 130.7 | 0.91 |
| Total dietary fiber (g/day) | 18.5 | 6.3 | 20.5 | 7.5 | 0.04 |
| Fruit and vegetables (servings/day) | 3.5 | 1.9 | 4.0 | 2.2 | 0.08 |
| Whole grains (servings/day) | 1.2 | 1.1 | 1.3 | 1.2 | 0.41 |
| % kilocalories eaten at home | 64.5 | 28.9 | 67.0 | 28.1 | 0.53 |
| Psychosocial factors for healthy eating | |||||
| Self efficacy (0–26) | 21.1 | 4.0 | 20.9 | 4.6 | 0.70 |
| Dietary attitudes (0–48) | 39.8 | 8.4 | 40.5 | 6.8 | 0.53 |
| Social support (0–18) | 2.5 | 2.6 | 2.5 | 2.3 | 0.99 |
| Perceived barriers (0–28) | 7.6 | 5.9 | 6.5 | 4.9 | 0.14 |
Notes: Data are means (standard deviation) unless otherwise noted.
P-value from t-test for continuous variables and chi-squared test for categorical variables.
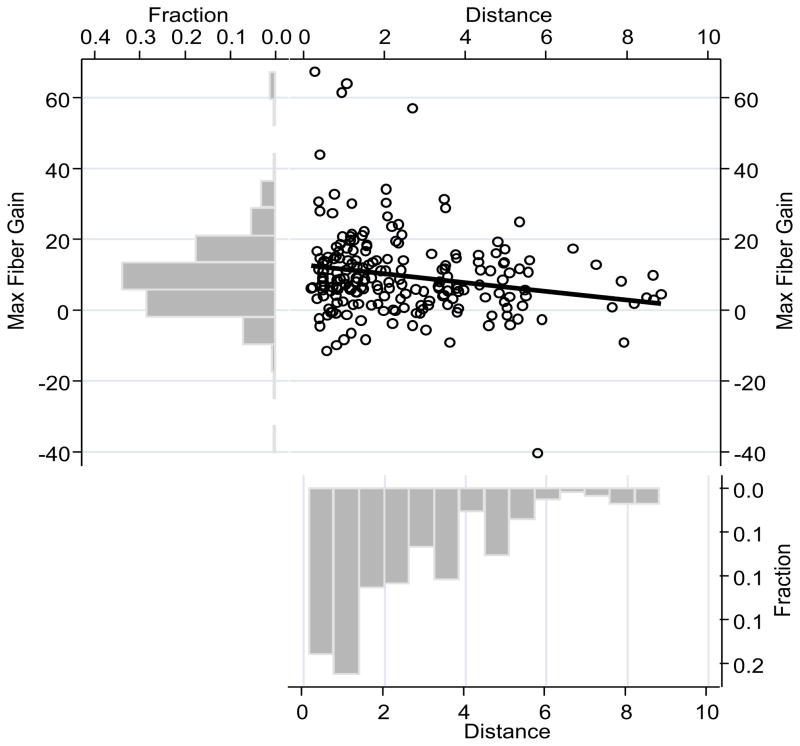
Figure 1 illustrates that participants living farther away from the nearest food store with HFAI ≥20 reported lower maximum dietary fiber gain. Means and 95% CIs of changes in each outcome at peak and 3, 6, and 12 months post-intervention are summarized in Table 2. All post-intervention changes were statistically significant (p<0.01). The table also shows regression coefficients and associated 95% CIs of each dietary outcome in relation to distance to the nearest food store with HFAI ≥20, adjusting for baseline value of the dietary variable, treatment group, age, income, employment, and social support for healthy eating. Living closer to a healthy food store was associated with greater improvements in consumption of dietary fiber and total fruit and vegetables. Significant associations were not found for servings of whole grains or AHEI, a composite score indicating dietary quality. Other participant characteristics associated with maximum improvement in total dietary fiber were being in the fiber intervention group, aged 50 years and older, having an income ≥$40,000, and having social support for eating healthy. Other assessed psychosocial variables were not associated with dietary improvements, including self-reported perceived barriers to healthy eating or depression. Examining potential interactions between distance and other covariates including income, age, and diet intervention group, confirmed that the relation between dietary improvements and distance to a healthy food store did not differ by these variables.
Figure 1.
Effect of the dietary intervention on total dietary fiber intake is modified by participant distance to food stores with adequate healthy food availability
Note: Maximum fiber gain (grams/day) regressed on network distance (miles) to nearest food store with adequate healthy food availability.
Table 2.
Mean and predictors of improvement in dietary outcomes over 1-year after a dietary behavioral intervention
| Outcomes and predictors | Mean and Regression coefficient (95% CI)
|
|||
|---|---|---|---|---|
| Dietary fiber (g/day) | Vegetables and fruits (servings/day) | Whole grains (servings/day) | Dietary quality (AHEI score) | |
|
| ||||
| Peak dietary change | ||||
| Mean | 9.67 (7.98, 11.36) | 2.10 (1.74, 2.46) | 1.69 (1.39, 1.99) | 12.94 (11.47, 14.40) |
| Regression coefficient | ||||
| Distance to food store with HFAI ≥ 20 (miles) | −1.07 (−1.89, −0.26) | −0.19 (−0.37, −0.02) | −0.08 (−0.22, 0.06) | −0.57 (−1.22, 0.09) |
| Baseline dietary value | −0.25 (−0.48, −0.02) | −0.43 (−0.59, −0.27) | −0.73 (−0.98, −0.48) | −0.55 (−0.69, −0.41) |
| Fiber vs. AHA treatment | 5.54 (2.37, 8.70) | −0.15 (−0.83, 0.53) | 0.21 (−0.35, 0.77) | −0.23 (−2.81, 2.35) |
| Age 50+ yr vs. <50yr | 3.75 (0.23, 7.26) | 0.82 (0.06, 1.58) | 0.26 (−0.37, 0.88) | 3.58 (0.71, 6.45) |
| Household income $40,000+ vs. Less | 4.74 (0.37, 9.10) | 0.17 (−0.78, 1.11) | 0.49 (−0.28, 1.27) | 4.59 (1.03, 8.15) |
| Social support for healthy eating (score) | 0.76 (0.11, 1.41) | 0.05 (−0.09, 0.19) | 0.05 (−0.06, 0.17) | 0.15 (−0.38, 0.69) |
|
| ||||
| Average dietary change over 3 time points # | 3.75 (2.61, 4.88) | 0.65 (0.35, 0.95) | 0.66 (0.45, 0.87) | 6.62 (5.67, 7.58) |
| Regression coefficient | ||||
| Distance to food store with HFAI ≥ 20 (miles) | −0.57 (−0.74, −0.40) | −0.08 (−0.14, −0.03) | −0.01 (−0.05, 0.04) | −0.41 (−0.68, −0.13) |
| Baseline dietary value | −0.36 (−0.42, −0.29 | −0.55 (−0.61, −0.49) | −0.82 (−0.90, −0.75) | −0.53 (−0.59, −0.47) |
| Fiber vs. AHA treatment | 4.22 (3.50, 4.95) | −0.19 (−0.40, 0.02) | 0.15 (0.01, 0.30) | −0.17 (−1.14, 0.80) |
| Age 50+ yr vs. <50yr | 1.16 (0.55, 1.78) | 0.21 (−0.01, 0.43) | 0.30 (0.11, 0.49) | 1.42 (0.37, 2.47) |
| Household income $40,000+ vs. Less | 1.99 (1.07, 2.90) | 0.04 (−0.22, 0.30) | 0.02 (−0.21, 0.24) | 2.98 (1.47, 4.50) |
| Social support for healthy eating (score) | 0.35 (0.19, 0.51) | 0.02 (−0.03, 0.06) | 0.00 (−0.03, 0.03) | 0.23 (0.02, 0.44) |
|
| ||||
| Change from baseline to 3-month follow-up | ||||
| Mean | 4.63 (2.79, 6.47) | 0.59 (0.18, 1.00) | 0.84 (0.51, 1.17) | 7.53 (5.65, 9.41) |
| Regression coefficient | ||||
| Distance to food store with HFAI ≥ 20 (miles) | −0.86 (−1.76, 0.03) | −0.22 (−0.41, −0.04) | 0.02 (−0.15, 0.18) | −0.28 (−1.17, 0.60) |
| Baseline dietary value | −0.44 (−0.69, −0.18) | −0.65 (−0.83, −0.47) | −0.75 (−1.03, −0.47) | −0.59 (−0.79, −0.39) |
| Fiber vs. AHA treatment | 3.24 (−0.27, 6.74) | −0.49 (−1.23, 0.25) | 0.02 (−0.61, 0.66) | −0.03 (−3.54, 3.48) |
| Age 50+ yr vs. <50yr | 2.44 (−1.48, 6.36) | 0.46 (−0.37, 1.29) | −0.09 (−0.80, 0.62) | 2.30 (−1.64, 6.24) |
| Household income $40,000+ vs. Less | 3.76 (−1.14, 8.66) | 0.48 (−0.56, 1.52) | 0.28 (−0.61, 1.17) | 5.82 (0.91, 10.74) |
| Social support for healthy eating (score) | 1.03 (0.31, 1.75) | 0.00 (−0.15, 0.15) | 0.03 (−0.10, 0.16) | 0.23 (−0.50, 0.95) |
|
| ||||
| Change from baseline to 6-month follow-up | ||||
| Mean | 3.25 (1.91, 4.59) | 0.62 (0.28, 0.95) | 0.67 (0.45, 0.89) | 6.53 (5.07, 7.99) |
| Regression coefficient | ||||
| Distance to food store with HFAI ≥ 20 (miles) | −0.64 (−1.29, 0.01) | −0.08 (−0.24, 0.08) | −0.03 (−0.13, 0.06) | −0.37 (−1.07, 0.33) |
| Baseline dietary value | −0.38 (−0.56, −0.20) | −0.49 (−0.64, −0.35) | −0.76 (−0.93, −0.58) | −0.49 (−0.64, −0.34) |
| Fiber vs. AHA treatment | 4.91 (2.45, 7.38) | −0.01 (−0.63, 0.60) | 0.45 (0.08, 0.82) | 0.75 (−1.92, 3.42) |
| Age 50+ yr vs. <50yr | 2.09 (−0.67, 4.85) | 0.67 (−0.02, 1.36) | 0.56 (0.14, 0.97) | 4.45 (1.45, 7.45) |
| Household income $40,000+ vs. Less | 2.64 (−0.81, 6.08) | 0.07 (−0.79, 0.93) | 0.03 (−0.49, 0.54) | 0.96 (−2.78, 4.69) |
| Social support for healthy eating (score) | 0.06 (−0.45, 0.58) | −0.05 (−0.18, 0.08) | −0.01 (−0.09, 0.06) | 0.02 (−0.54, 0.59) |
|
| ||||
| Change from baseline to 12-month follow-up | ||||
| Mean | 3.23 (1.88, 4.59) | 0.76 (0.37, 1.15) | 0.44 (0.17, 0.71) | 5.65 (4.10, 7.19) |
| Regression coefficient | ||||
| Distance to food store with HFAI ≥ 20 (miles) | −0.60 (−1.30, 0.10) | −0.02 (−0.20, 0.17) | −0.07 (−0.19, 0.04) | −0.37 (−1.10, 0.36) |
| Baseline dietary value | −0.28 (−0.49, −0.08) | −0.57 (−0.74, −0.41) | −0.98 (−1.19, −0.76) | −0.57 (−0.72, −0.41) |
| Fiber vs. AHA treatment | 3.26 (0.63, 5.89) | 0.05 (−0.66, 0.76) | 0.02 (−0.43, 0.47) | −0.51 (−3.25, 2.23) |
| Age 50+ yr vs. <50yr | −0.51 (−3.64, 2.61) | 0.07 (−0.77, 0.91) | 0.09 (−0.45, 0.63) | −0.76 (−4.02, 2.51) |
| Household income $40,000+ vs. Less | 1.30 (−2.37, 4.97) | −0.37 (−1.36, 0.62) | 0.38 (−0.24, 1.01) | 1.82 (−1.99, 5.64) |
| Social support for healthy eating (score) | 0.18 (−0.36, 0.72) | 0.12 (−0.02, 0.27) | 0.00 (−0.09, 0.09) | 0.11 (−0.46, 0.68) |
Notes: Boldface indicates statistical significance (p<0.05).
Estimated using linear mixed models which accounted for autocorrelations within repeated measures on dietary outcomes of the same patient.
AHEI, Alternate Healthy Eating Index; HFAI, Healthy Food Availability Index; AHA, American Heart Association.
Discussion
Findings from this study suggest that shorter distance from home to the nearest food store with adequate healthy food accessibility predicts greater improvements in consumption of dietary fiber and total fruit and vegetable servings after a dietary intervention among community-dwelling obese adults with metabolic syndrome. These results were robust to adjustment of a number of participant sociodemographic and behavioral factors that are known to modify the effects of dietary interventions, such as age, sex, educational attainment, and income. Therefore, the results support the claim that geographic or physical access to healthy foods is an independent predictor of a person’s likely response to dietary interventions. To our knowledge, this is a new addition to the literature.
Many previous studies have shown association of lower obesity prevalence with larger number and higher density of grocery stores in communities. However, a surprisingly small subset has evaluated these correlations in longitudinal studies. In a review of 131 papers (1985–2009) examining the relationships between geographic life environments and cardiometabolic risk factors, only 14 studies were longitudinal by design.9 Of these, only a handful of studies evaluated aspects of the food environment,4, 6, 7, 25, 26 and there were no results reported for the influence of the food environment on individuals’ dietary intake. The current study reports novel findings on the effect modification of physical access to food stores with adequate healthy food supplies on responses to dietary interventions among highly motivated individuals with or without minor economic barriers.
The current study population tended to be well educated and have modest to high income. The majority of the participants had annual household incomes well exceeding $40,000 per year. The limited variation in income level may have affected the results in two aspects. First, economic access to healthy foods in this study area is likely to be less of a problem than for individuals living in more socioeconomically disadvantaged neighborhoods. In the study area of central Massachusetts, suburban and some parts of the rural communities tend to be wealthier than urban communities. Therefore, the observed effect modification of dietary intervention by physical access to healthy foods is unlikely to be a confounding effect of limited economic access. The regression adjustments for individual and community-level income factors also support this point.
Second, the limited variation in income level might have impaired the study’s ability to detect the potential effect modification of income on the relationship between distance to a healthy food store and dietary outcomes. Recent findings from a study conducted among adults living in Houston, Texas found that income modified the association between distance to fast food restaurants and BMI, with stronger associations among those having an annual income of less than $40,000.27 Thus, lower-income households may be more sensitive to travel costs associated with food purchasing, but this study was unable to contest this hypothesis.
Both cross-sectional and longitudinal associations with distance from healthy food stores were observed in this study. Cross-sectionally, participants living at a greater distance from a healthy food store were more likely to be white, have higher income, and at baseline eat more fiber and have better dietary quality. By separating the cross-sectional and longitudinal associations between healthy food availability and diet, this analysis uncovered important longitudinal relationships that were missed in broader cross-sectional surveys. This study discovered that intervention-induced improvements in fiber and vegetable fruit intake were greater among participants within closer proximity to a grocery store with adequate healthy food availability. This new finding on the effect modification by neighborhood food environment is informative to the design of future community-based dietary interventions.
Strengths of this study include well-measured food environment data based on in-store inspections of all food stores in the study area, in addition to detailed participant measures, including three 24-hour dietary recalls, collected at multiple time points during the course of a 1-year intervention study. However, 15% of the trial participants were excluded from analysis owing to attrition or living outside of the Worcester County area where food stores were surveyed. Comparisons of the characteristics of excluded versus included participants found no appreciable differences, with the exception of excluded participants having a slightly younger mean age. Although it unlikely caused selection bias, the exclusion of these participants, however, somewhat limited the statistical power to detect modest to weak associations. The lack of a non-intervention control group limited the ability to estimate the effects solely attributable to the interventions. The generalizability of the outcomes from this research may be considered limited, as all participants were from central Massachusetts communities, a relatively small geographic region. The current population is located in the northeastern part of the country, predominantly white, has higher education and income levels, and thus may not be representative of the general U.S. population. To confirm the results, similar analyses need to be conducted using data from other geographic areas.
As recently reported by Cummins and colleagues,12 opening a new supermarket in a low-income, food desert community may improve awareness and perception of accessibility to healthy foods, but may not be sufficient to result in desired changes in healthy eating among the residents. Results from the current analysis show that effectiveness of dietary interventions is likely minimal among patients living in communities without supporting nutrition environment, even though they were highly motivated to make dietary changes to manage their metabolic syndrome as referred by their physicians. Considering the nationwide efforts on promotion of healthy eating, the value of improving community access to healthy foods should not be underestimated. To be effective, future interventions should take into account both aspects.
In summary, findings from the current analysis suggest that dietary improvements may be supported by a closer proximity to a food store with adequate healthy food. This is the first study to our knowledge to report likely effect modifications of dietary interventions by physical access to a healthy food store. Future dietary interventions should consider the potential influence of a participant’s neighborhood food environment, both perceived and actual, on their ability to adhere to dietary intervention regimens.
Supplementary Material
Acknowledgments
Data on participants were obtained from a study funded by the National Heart, Lung and Blood Institute (grant No. 5R01HL094575-04). Socioeconomic and demographic data on communities were obtained from a study funded by the National Institute on Aging (grant No. AG028738). Grocery store data collection and geographic analysis were funded by a development fund from the University of Massachusetts Medical School.
Footnotes
Clinical Trial Registration Number: NCT00911885
All authors have read and approved the submission of this original article.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U. S Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 2.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18(5):1172–87. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, Shikany JM, Lewis CE, Popkin BM. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med. 2011;171(13):1162–70. doi: 10.1001/archinternmed.2011.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auchincloss AH, Diez Roux AV, Mujahid MS, Shen M, Bertoni AG, Carnethon MR. Neighborhood resources for physical activity and healthy foods and incidence of type 2 diabetes mellitus: the Multi-Ethnic study of Atherosclerosis. Arch Intern Med. 2009;169(18):1698–704. doi: 10.1001/archinternmed.2009.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Auchincloss AH, Mujahid MS, Shen M, Michos ED, Whitt-Glover MC, Diez Roux AV. Neighborhood health-promoting resources and obesity risk (the multi-ethnic study of atherosclerosis) Obesity (Silver Spring) 2013;21(3):621–8. doi: 10.1038/oby.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li F, Harmer P, Cardinal BJ, Vongjaturapat N. Built environment and changes in blood pressure in middle aged and older adults. Prev Med. 2009;48(3):237–41. doi: 10.1016/j.ypmed.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li F, Harmer P, Cardinal BJ, Bosworth M, Johnson-Shelton D, Moore JM, et al. Built environment and 1-year change in weight and waist circumference in middle-aged and older adults: Portland Neighborhood Environment and Health Study. Am J Epidemiol. 2009;169(4):401–8. doi: 10.1093/aje/kwn398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zenk SN, Schulz AJ, Izumi BT, Mentz G, Israel BA, Lockett M. Neighborhood food environment role in modifying psychosocial stress-diet relationships. Appetite. 2013;65:170–7. doi: 10.1016/j.appet.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12(3):217–30. doi: 10.1111/j.1467-789X.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- 10.Dubowitz T, Ghosh-Dastidar M, Eibner C, Slaughter ME, Fernandes M, Whitsel EA, et al. The Women’s Health Initiative: The food environment, neighborhood socioeconomic status, BMI, and blood pressure. Obesity (Silver Spring) 2012;20(4):862–71. doi: 10.1038/oby.2011.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Block JP, Christakis NA, O’Malley AJ, Subramanian SV. Proximity to food establishments and body mass index in the Framingham Heart Study offspring cohort over 30 years. Am J Epidemiol. 2011;174(10):1108–14. doi: 10.1093/aje/kwr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health affairs. 2014;33(2):283–91. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merriam PA, Ma Y, Olendzki BC, Schneider KL, Li W, Ockene IS, et al. Design and methods for testing a simple dietary message to improve weight loss and dietary quality. BMC Med Res Methodol. 2009;9:87. doi: 10.1186/1471-2288-9-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 15.Zivkovic AM, German JB, Sanyal AJ. Comparative review of diets for the metabolic syndrome: implications for nonalcoholic fatty liver disease. Am J Clin Nutr. 2007;86(2):285–300. doi: 10.1093/ajcn/86.2.285. [DOI] [PubMed] [Google Scholar]
- 16.Feldeisen SE, Tucker KL. Nutritional strategies in the prevention and treatment of metabolic syndrome. Appl Physiol Nutr Metab. 2007;32(1):46–60. doi: 10.1139/h06-101. [DOI] [PubMed] [Google Scholar]
- 17.Kant AK, Schatzkin A, Graubard BI, Schairer C. A prospective study of diet quality and mortality in women. JAMA. 2000;283(16):2109–15. doi: 10.1001/jama.283.16.2109. [DOI] [PubMed] [Google Scholar]
- 18.Fung TT, Rimm EB, Spiegelman D, Rifai N, Tofler GH, Willett WC, et al. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am J Clin Nutr. 2001;73(1):61–7. doi: 10.1093/ajcn/73.1.61. [DOI] [PubMed] [Google Scholar]
- 19.Michels KB, Wolk A. A prospective study of variety of healthy foods and mortality in women. Int J Epidemiol. 2002;31(4):847–54. doi: 10.1093/ije/31.4.847. [DOI] [PubMed] [Google Scholar]
- 20.McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–71. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- 21.McCullough ML, Willett WC. Evaluating adherence to recommended diets in adults: the Alternate Healthy Eating Index. Public Health Nutr. 2006;9(1A):152–7. doi: 10.1079/phn2005938. [DOI] [PubMed] [Google Scholar]
- 22.Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in stores (NEMS-S): development and evaluation. Am J Prev Med. 2007;32(4):282–9. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- 23.Nydahl M, Gustafsson I, Ohrvall M, Vessby B. Similar Serum Lipoprotein Cholesterol Concentrations in Healthy Subjects on Diets Enriched with Rapeseed and Sunflower Oil. Eur J Clin Nutri. 1994;48(2):128–137. [PubMed] [Google Scholar]
- 24.Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. American Journal of Preventive Medicine. 2008;35(6):561–7. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li F, Harmer P, Cardinal BJ, Bosworth M, Johnson-Shelton D. Obesity and the built environment: does the density of neighborhood fast-food outlets matter? Am J Health Promot. 2009;23(3):203–9. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059–68. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Reitzel LR, Regan SD, Nguyen N, Cromley EK, Strong LL, Wetter DW, et al. Density and proximity of fast food restaurants and body mass index among African Americans. Am J Public Health. 2014;104(1):110–6. doi: 10.2105/AJPH.2012.301140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.