Abstract
Background:
Central venous catheterization (CVC) is an important procedure in emergency departments (EDs). Despite existence of ultrasonography (US) devices in every ED, CVC is done using anatomical landmarks in many EDs in Iran.
Objectives:
This study aimed to compare the traditional landmark method vs. US-guided method of CVC placement in terms of complications and success rate.
Patients and Methods:
In this randomized controlled trial, patients who were candidate for internal jugular vein catheterization, and referred to Baqiyatallah Hospital ED were randomly allocated into US-guided CVC and anatomical landmarks guided CVC groups. Central vein access time, number of attempts, success rate, and complications in each group were evaluated. Mann-Whitney U, chi-square and Fisher exact tests along with Pearson and Spearman correlation coefficients were used to analyze the data.
Results:
Out of 100 patients, 56 were male and 44 were female. No significant differences were found between the US-guided and traditional landmark methods of CVC insertion in terms of age, gender, BMI, and site of catheter insertion. The mean access time was significantly lower in the US-guided group (37.12 ± 17.33 s vs. 63.42 ± 35.19 s, P < 0.001). The mean number of attempts was also significantly lower in the US-guided group (1.12 ± 0.3 vs. 1.58 ± 0.64 times, P < 0.001). Eighty-eight percent of patients in the US-guided group were catheterized in the first attempt, while 50% of patients in the traditional landmark group were catheterized in the second or more attempts (P < 0.001). The success rate was 100% in the US-guided group, while it was 88% in the landmark group (P = 0.013). Moreover, the rate of complications was significantly lower in the US-guided group (4% vs. 24%, P = 0.004).
Conclusions:
The US-guided method for CVC placement was superior to the traditional landmark method in terms of access time, number of attempts, success rate, and fewer complications.
Keywords: Central Venous Catheterization, Jugular Vein, Ultrasonography
1. Background
Central venous catheterization (CVC) is commonly used as a diagnostic-therapeutic procedure in emergency medicine by administration of fluids, blood products, vasoactive drugs, and heart pacemaker placement. Over the last decade, the use of CVC has increased worldwide so that in the UK, more than 200000 CVCs are placed annually (1, 2). The increased use of CVCs has been accompanied with increased rates of complications. The fourth rank of nosocomial infections outbreak is related to the catheter site infection, with a prevalence rate of 3% to 60%. These complications impose high costs on healthcare systems (2-6). The increase in number of cannulations, unsuccessful attempts, and improper catheter placement could increase the risk of bacterial colonization (5). Moreover, in cases where the location of the catheter insertion is determined incorrectly by landmarks, the possibility of complications such as pneumothorax, hemothorax, hematoma, and brachial plexus injury would be increased. To a large extent, the occurrence of these complications depends on physician’s experience, patient’s age, and his or her underlying medical condition such as coagulopathy, cancer, and hemodynamic conditions (7, 8).
Because of the high rates of the CVC’s complications over the past 10 years, several studies have focused on the use of ultrasound guided (US-guided) CVC insertion and considered it as a method for reducing the rate of complications and the time of catheter insertion (1, 9). The significant increase in the success of this method, has led to the use of ultrasound in CVC placement guidelines by Scandinavian Society of Anesthesiology (10). Unfortunately, despite the existing evidence on the advantages of US-guided CVC placement and existence of ultrasound devices in most of emergency departments in Iran, ultrasound (US) is not routinely used for catheterization, because of the lack of education and the time needed for preparing the apparatus. Therefore, most professionals are still using the traditional landmark method.
2. Objectives
This study aimed to compare the traditional landmark method vs. US-guided method of CVC in terms of complications and success rate.
3. Patients and Methods
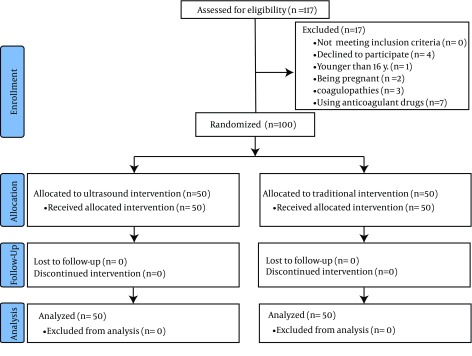
This is a randomized controlled trial conducted on 100 patients referred to emergency department (ED) of Baqiyatallah Hospital, Tehran, Iran, who needed internal jugular vein (IJV) catheterization. Sample size was calculated using the results of a previous study (11) in which S1, S2, 1μ, and 2μ were equal to 0.6, 2.9, 1.1 and 2.6, respectively. Accordingly, with a type I error of 0.05 and a power of 0.80, the sample size was determined to be 50 patients in each group. The study flow chart is shown in Figure 1. All patients who had an order of IJV catheterization (with any reason such as hypovolemia, hypotension, shock, or fluid resuscitation) in the ED were enrolled. Indications of IJV catheterization were defined by the ED physicians. Patients younger than 16 years old, pregnant women, patients with uncontrolled coagulopathies and those who received anticoagulant drugs were excluded from the study.
Figure 1. Study Flow Chart.
Patients were assigned blindly into two groups by a nurse using a balanced block randomization method with a block size of four patients. Catheterization was accomplished using ultrasound guidance after viewing the IJV in one group, and anatomical landmarks (AL) in the second group. All catheterizations in the two groups were performed by a unique specialist and with the aid of a nurse. In US-guided method the neck area was draped sterilely while patients were in supine position. The skin at the top of the triangle between the sternum and the head of sternocleidomastoid muscle disinfected using povidone-iodine solution. Local anesthesia was performed with subcutaneous injection of 0.4 mL/kg of 1% Xylocaine (maximum 30 mL) using a 22-gauge needle. Return of blood into syringe confirmed the entrance of the catheter into the vessel. Sonographies were performed using an M-Tube ultrasound system from SonositeTM company and with a non-needle probe and a HFL38X transducer for vascular view. In the AL group, the patients were also placed supine. The physician determined the location of the IJV by a needle connected to a 2-mL syringe as the needle was advanced through the skin at an angle of 45° in the direction of the same side nipple. A 19-gauge, 10-cm arrow Jet™ needle was used in all patients. Demographic data, including age, gender, as well as body mass index (BMI), side of catheterization (left or right), existing of risk factors (such as hypertension, diabetes mellitus, coagulopathies, ischemic heart disease, cigarette smoking, edema and local masses at cannulation cite, shock, cardiac arrest, chronic lung diseases, loss of consciousness, sepsis, malignancy, renal disease, trauma, hepatic failure, hematologic disorders, electrolyte imbalance, and respiratory distress) were evaluated and recorded in a checklist. Moreover, venous access time (from needle contacting skin to accessing jugular blood flow), number of attempts (skin cannulations), success rate, and catheter related complications (i.e. hematoma, carotid puncture, hemothorax, and pneumothorax) were also documented in the checklist to be compared between the two groups. The BMI was calculated using weight (kg) divided by the height squared (m2). A PA chest X-ray was performed for all patients (immediately after the cannulation) to evaluate the success of the procedure and to assess possible complications. A visible catheter tip in the superior vena cava parallel to its wall in chest X-ray was considered as successful attempt and any other tip placements were considered as unsuccessful attempt. The corresponding author of this manuscript gathered all data. He observed the process of all cannulations and monitored all the patients in ED (in the post cannulation phase till they were discharged from ED and filled out each patients’ checklist).
3.1. Ethical Considerations
The study protocol was approved by Ethics Committee of Baqiyatallah University of Medical Sciences (No. 28-2 dated 14 Jun, 2013). All patients were signed a written informed consent after they were briefed about the study. They were informed that participation in the study is voluntary and their refusal to take part in the study would not disturb their treatment process. All participants were also assured about the confidentially of their personal information. Researchers were committed to consider the participants' rights in accordance to the principles explained in the Declaration of Helsinki.
3.2. Data Analysis
Data were analyzed using statistical package for social sciences (SPSS) version 13 (SPSS Inc. Chicago, IL) for Windows. The Kolmogorov–Smirnov test was used to assess the normal distribution of the variables. The BMI had normal distribution, whereas age, access time, and number of attempts had non-normal distribution. Then, quantitative variables were compared using independent sample t test and its equivalent nonparametric test (Mann-Whitney U test) between the groups. Pearson and its nonparametric equivalent (Spearman) tests were also used for evaluation of correlation between quantitative variables. Chi-square and Fisher exact tests were also used to compare categorical variables between the two groups.
4. Results
One hundred patients with a mean age of 50.60 ± 11.49 y were evaluated. Fifty-six patients were male and 44 were female. No significant differences were found between the two groups in terms of age, gender, BMI, and site of catheter insertion (Table 1). The mean access time was significantly lower in the US-guided group (37.12 ± 17.33 s vs. 63.42 ± 35.19 s, P < 0.001) (Table 2). The mean number of attempts was also significantly lower in the US-guided group (1.12 ± 0.328 vs. 1.58 ± 0.641 times, P < 0.001) (Table 2). Eighty-eight percent of the patients in the US-guided group were catheterized in the first attempt while 50% of patients in the AL group were catheterized in the second or more attempts (P < 0.001) (Table 2). As table 2 shows, the overall success rate was 100% in the US-guided group, whereas it was 88% in the AL group (P = 0.013). Moreover, the rate of complications was significantly lower in the US-guided group (4% vs. 24%, P = 0.004) (Table 2). No significant differences were found between the mean access time (53.46 ± 32.3 s vs. 46.2 ± 28.13 s, P = 0.681) and the success rate (96.4% vs. 90.9%, P = 0.232), in male and female patients. However, the mean number of attempts was lower in males than females (1.21 ± 0.494 vs. 1.52 ± 0.59 times, P = 0.007). Moreover, the mean age was significantly higher in patients with complications (58.86 ± 14.66 y) than those without complications (50.29 ± 11.81 y) (P = 0.014). In addition, the mean BMI was significantly higher in patients with complications (24.26 ± 2.33 kg/m²) than those without complications (21.48 ± 2.84 kg/m²) (P = 0.001). No significant correlation was observed between the patients’ age and vein access time (r = 0.024, P = 0.398). Also, no significant correlation was observed between the patients’ BMI and vein access time (r = 0.092, P = 0.363). There was a significant correlation between BMI and number of attempts (r = 0.213, P = 0.033), and significant correlation between access time and number of attempts (r = 0.150, P = 0.047).
Table 1. Comparison of the Patients’ Characteristics in the Two Groups (n = 50) a.
| Variables | The Study Groups | P Value | |
|---|---|---|---|
| Ultrasound Guided | Anatomic Landmarks | ||
| Age, y | 49.93 ± 10.98 | 51.16 ± 11.94 | 0.617 |
| Gender | 0.687 | ||
| Male | 27 (54) | 29 (58) | |
| Female | 23 (46) | 21 (42) | |
| BMI, kg/m 2 | 21.91 ± 3.2 | 21.82 ± 2.67 | 0.877 |
| Location of catheter | 0.349 | ||
| Right side | 40 (80) | 36 (72) | |
| Left side | 10 (20) | 14 (28) | |
aData are presented as No. (%) or Mean ± SD.
Table 2. Comparison of the Catheterization Outcomes in the Two Groups (n = 50) a.
| Variables | The Study Groups | P Value | |
|---|---|---|---|
| Ultrasound Guided | Anatomic Landmarks | ||
| Access Time, Second | 37.12 ± 17.33 | 63.42 ± 35.19 | < 0.001 |
| Numbers of attempts | 1.12 ± 0.328 | 1.58 ± 0.641 | < 0.001 |
| One attempt | 44 (88) | 25 (50) | < 0.001 |
| Two attempts | 6 (12) | 21 (42) | |
| More than two attempts | 0 (0) | 4 (8) | |
| Success rate | < 0.013 | ||
| Successful | 50 (100) | 44 (88) | |
| Unsuccessful | 0 (0) | 6 (12) | |
| Complications | < 0.004 | ||
| No complications occurred | 48 (96) | 38 (76) | |
| Complication occurred | 2 (4) | 12 (24) | |
| Types of complications | |||
| Hematoma | 1 (2) | 4 (8) | 0.181 |
| Carotid Puncture | 1 (2) | 5 (10) | 0.102 |
| Hemothorax | 0 (0) | 2 (4) | 0.247 |
| Pneumothorax | 0 (0) | 1 (2) | 0.501 |
aData are presented as No. (%) or Mean ± SD.
5. Discussion
This study aimed to compare the AL method with US-guided method of CVC with regard to their complications and success rate. Our study results showed that US-guided CVC was remarkably superior in almost every aspect (access time, success rate, number of attempts, and catheter related complication) compared to the AL method. In the present study, the success rate of US-guided methods of CVC was 100%, while the traditional AL method had a failure of 12%. As in previous studies, results of this research showed the relatively high success rate with the use of US-guided method (7, 11-13). In a study conducted by Verghese et al. the success rate was 100% in the catheterization using US-guided method while this rate was 77% in patients that traditional AL method was used (14). Although the success rates are significantly higher in US-guided method, the success rate of both methods are largely depends on the physicians’ skills and experiences (15, 16). In the present study, the success rate of AL method was higher and its complication rates were less than some previous investigations (15-18). This finding may be attributed to the greater use of this method in Iran and the physicians’ experiences. Hence, training the traditional AL method should always be considered along with promoting the use of US-guided method in EDs (19, 20).
In the present study, the IJV access time was significantly shorter in the US-guided method compared to the traditional AL method. This finding is in line with previous studies. This issue is especially important in the EDs, where the patients’ conditions are usually critical and the time saving would be vital for the patients (18, 21). Another important point is the number of attempts to place the catheter in the IJV, which was considerably lower in US-guided method. This finding is consistent with other studies focusing on the number of catheter placement efforts. The importance of this issue lies in the direct relationship of shorter access time with the fewer number of attempts. Then, the risk of complications, catheter-related infections and bacterial proliferation would be reduced (1, 8, 9, 18, 22, 23).
BMI is an important factor influencing the number of attempts in catheter insertion. In our study, the number of attempts and complications of catheterization also increased in patients with higher BMI. In a study by Schummer et al. more attempts were needed for catheter insertion in people with BMI over 30 kg/m² (24). This finding may be attributed to the peripheral obesity of these people that makes it harder to find the vein (21). In our study, despite the absence of significant difference between the two groups in terms of complications, the frequency of total side effects was significantly higher in catheterization using AL method. In a study by Karakitsos et al.hematoma and pneumothorax were not observed in US-guided method while 8 patients catheterized using AL method experienced such complications (25). Similar findings were also reported in a study by Rando et al. (26). Lower rates of complications are responsible for the cost-effectiveness of using US-guided method of CVC placement, as reported by Calvert et al. in a systematic review and economic evaluation of the US-guided CVC (27). The advantages and effectiveness of the US-guided CVC were also confirmed in a study by Merrer et al. who investigated the complications of femoral and subclavian venous catheterization in critically ill patients (28). Therefore, while it is essential for physicians to be skilled in CVC through traditional AL method, Feller et al. emphasized that it is necessary for physicians and nurses in EDs to be trained in CVC using US-guided method as an easy, applicable and cost-effectiveness method (29).
We studied a small sample of patients and this may affect the results. Thus, further studies with larger sample size are suggested. Moreover, we excluded the high risk patients such as patients with coagulopathies, malignancies, multiple trauma, and morbidly obese. Therefore, further studies are suggested to be performed in these high risk patients with evaluating further confounders. Moreover, studies could also be suggested to evaluate bacterial colonization and catheter-related infections in US-guided and traditional AL methods. Lack of blindness from the side of patients was also a limitation of the present study and may confound our results. Therefore, studies with blinded designs are suggested. In this study, we did not evaluate the correctness of the indications for CVC and this may affect the results as a confounder. We also assessed the complications only for a short period while the patients were in the ED. Thus; studies with longer periods of evaluation for complications are suggested.
Our study showed that the use of US-guided method for CVC was superior to the traditional AL method. Unfortunately, despite the existence of ultrasound devices in most of our EDs, using the US-guided CVC placement is not common and most experts still use traditional AL method. Undoubtedly, the existence of ultrasound devices in EDs and having skilled staff are necessary, if this method is used. It should be noted that although US-guided method can reduce complications, and increase the success rate, all physicians working in EDs should also be skilled in the traditional AL method too.
Acknowledgments
Researchers would like to thank all staff of Baqiyatallah Hospital Emergency Department. This study was registered in Iranian Registry of Clinical Trials and the registry number is IRCT2014062117413N6.
Footnotes
Authors’ Contributions:All of the authors have equally participated in the process of preparing the manuscript.
Funding/ Support:This study was supported by the Deputy of Research of Baqiyatallah University of Medical Sciences with reference number 28-2.
References
- 1.Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327(7411):361. doi: 10.1136/bmj.327.7411.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salwender HJ, Egerer G, Bach A, Hahn U, Goldschmidt H, Ho AD. Central venous catheter-related complications. Antibiot Chemother (1971). 2000;50:133–43. doi: 10.1159/000059322. [DOI] [PubMed] [Google Scholar]
- 3.Mahieu LM, Buitenweg N, Beutels P, De Dooy JJ. Additional hospital stay and charges due to hospital-acquired infections in a neonatal intensive care unit. J Hosp Infect. 2001;47(3):223–9. doi: 10.1053/jhin.2000.0852. [DOI] [PubMed] [Google Scholar]
- 4.Dimick JB, Pelz RK, Consunji R, Swoboda SM, Hendrix CW, Lipsett PA. Increased resource use associated with catheter-related bloodstream infection in the surgical intensive care unit. Arch Surg. 2001;136(2):229–34. doi: 10.1001/archsurg.136.2.229. [DOI] [PubMed] [Google Scholar]
- 5.Lorente L, Henry C, Martin MM, Jimenez A, Mora ML. Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care. 2005;9(6):R631–5. doi: 10.1186/cc3824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Templeton A, Schlegel M, Fleisch F, Rettenmund G, Schobi B, Henz S, et al. Multilumen central venous catheters increase risk for catheter-related bloodstream infection: prospective surveillance study. Infection. 2008;36(4):322–7. doi: 10.1007/s15010-008-7314-x. [DOI] [PubMed] [Google Scholar]
- 7.Hayashi H, Amano M. Does ultrasound imaging before puncture facilitate internal jugular vein cannulation? Prospective randomized comparison with landmark-guided puncture in ventilated patients. J Cardiothorac Vasc Anesth. 2002;16(5):572–5. doi: 10.1053/jcan.2002.126950. [DOI] [PubMed] [Google Scholar]
- 8.Leung J, Duffy M, Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;48(5):540–7. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Miller AH, Roth BA, Mills TJ, Woody JR, Longmoor CE, Foster B. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the emergency department. Acad Emerg Med. 2002;9(8):800–5. doi: 10.1111/j.1553-2712.2002.tb02168.x. [DOI] [PubMed] [Google Scholar]
- 10.Frykholm P, Pikwer A, Hammarskjold F, Larsson AT, Lindgren S, Lindwall R, et al. Clinical guidelines on central venous catheterisation. Acta Anaesthesiol Scand. 2014;58(5):508–24. doi: 10.1111/aas.12295. [DOI] [PubMed] [Google Scholar]
- 11.Shiloh AL, Savel RH, Paulin LM, Eisen LA. Ultrasound-guided catheterization of the radial artery: a systematic review and meta-analysis of randomized controlled trials. Chest. 2011;139(3):524–9. doi: 10.1378/chest.10-0919. [DOI] [PubMed] [Google Scholar]
- 12.Airapetian N, Maizel J, Langelle F, Modeliar SS, Karakitsos D, Dupont H, et al. Ultrasound-guided central venous cannulation is superior to quick-look ultrasound and landmark methods among inexperienced operators: a prospective randomized study. Intensive Care Med. 2013;39(11):1938–44. doi: 10.1007/s00134-013-3072-z. [DOI] [PubMed] [Google Scholar]
- 13.Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med. 2006;21(1):40–6. doi: 10.1177/0885066605280884. [DOI] [PubMed] [Google Scholar]
- 14.Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE. Ultrasound-guided internal jugular venous cannulation in infants: a prospective comparison with the traditional palpation method. Anesthesiology. 1999;91(1):71–7. doi: 10.1097/00000542-199907000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Mey U, Glasmacher A, Hahn C, Gorschluter M, Ziske C, Mergelsberg M, et al. Evaluation of an ultrasound-guided technique for central venous access via the internal jugular vein in 493 patients. Support Care Cancer. 2003;11(3):148–55. doi: 10.1007/s00520-002-0399-3. [DOI] [PubMed] [Google Scholar]
- 16.Mitre CI, Golea A, Acalovschi I, Mocan T, Caea AM, Ruta C, et al. Ultrasound-guided external jugular vein cannulation for central venous access by inexperienced trainees. Eur J Anaesthesiol. 2010;27(3):300–3. doi: 10.1097/EJA.0b013e328333c2d6. [DOI] [PubMed] [Google Scholar]
- 17.Fragou M, Gravvanis A, Dimitriou V, Papalois A, Kouraklis G, Karabinis A, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011;39(7):1607–12. doi: 10.1097/CCM.0b013e318218a1ae. [DOI] [PubMed] [Google Scholar]
- 18.National Nosocomial Infections Surveillance S. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32(8):470–85. doi: 10.1016/S0196655304005425. [DOI] [PubMed] [Google Scholar]
- 19.O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Guidelines for the Prevention of Intravascular Catheter-related Infections. Clin Infect Dis. 2011;52(9):e162–93. doi: 10.1093/cid/cir257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbert RE, Harden M. Effectiveness of impregnated central venous catheters for catheter related blood stream infection: a systematic review. Curr Opin Infect Dis. 2008;21(3):235–45. doi: 10.1097/QCO.0b013e3282ffd6e0. [DOI] [PubMed] [Google Scholar]
- 21.Fragou M, Kouraklis G, Dimitriou V, Karakitsos D. Risk factors for acute adverse events during ultrasound-guided central venous cannulation in the emergency department. Acad Emerg Med. 2011;18(4):443–4. doi: 10.1111/j.1553-2712.2011.01021.x. author reply 445-6. [DOI] [PubMed] [Google Scholar]
- 22.Khare MD, Bukhari SS, Swann A, Spiers P, McLaren I, Myers J. Reduction of catheter-related colonisation by the use of a silver zeolite-impregnated central vascular catheter in adult critical care. J Infect. 2007;54(2):146–50. doi: 10.1016/j.jinf.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 23.Goede MR, Coopersmith CM. Catheter-related bloodstream infection. Surg Clin North Am. 2009;89(2):463–74. doi: 10.1016/j.suc.2008.09.003. ix. [DOI] [PubMed] [Google Scholar]
- 24.Schummer W, Schummer C, Tuppatsch H, Fuchs J, Bloos F, Huttemann E. Ultrasound-guided central venous cannulation: is there a difference between Doppler and B-mode ultrasound? J Clin Anesth. 2006;18(3):167–72. doi: 10.1016/j.jclinane.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 25.Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J, et al. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10(6):R162. doi: 10.1186/cc5101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rando K, Castelli J, Pratt JP, Scavino M, Rey G, Rocca ME, et al. Ultrasound-guided internal jugular vein catheterization: a randomized controlled trial. Heart Lung Vessel. 2014;6(1):13–23. [PMC free article] [PubMed] [Google Scholar]
- 27.Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A. The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation. Health Technol Assess. 2003;7(12):1–84. doi: 10.3310/hta7120. [DOI] [PubMed] [Google Scholar]
- 28.Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001;286(6):700–7. doi: 10.1001/jama.286.6.700. [DOI] [PubMed] [Google Scholar]
- 29.Feller-Kopman D. Ultrasound-guided internal jugular access: a proposed standardized approach and implications for training and practice. Chest. 2007;132(1):302–9. doi: 10.1378/chest.06-2711. [DOI] [PubMed] [Google Scholar]


