Abstract
Non-pharmaceutical interventions (NPIs) are an important public health tool for responding to infectious disease outbreaks, including pandemics. However, little is known about the individual characteristics associated with support for NPIs, or whether they are consistent across regions. This study draws on survey data from four regions—Hong Kong, Singapore, Taiwan, and the United States—collected following the Severe Acute Respiratory Syndrome (SARS) outbreak of 2002–03, and employs regression techniques to estimate predictors of NPI support. It finds that characteristics associated with NPI support vary widely by region, possibly because of cultural variation and prior experience, and that minority groups tend to be less supportive of NPIs when arrest is the consequence of noncompliance. Prior experience of face-mask usage also results in increased support for future usage, as well as other NPIs. Policymakers should be attentive to local preferences and to the application of compulsory interventions. It is speculated here that some public health interventions may serve as ‘gateway’ exposures to future public health interventions.
Keywords: compulsory, epidemic, non-pharmaceutical interventions, pandemic, survey
Introduction
Public concerns about infectious disease threats have risen owing to severe acute respiratory syndrome (SARS) outbreaks, anthrax attacks, the evolution of the H5N1 influenza strain, and the H1N1 influenza pandemic of 2009 (Cooper et al., 2006; Germann et al., 2006; Katz, Staiti, and McKenzie, 2006; Department of Health, 2007). Experts and policymakers continue to confront the potential emergence of novel infectious diseases with unknown characteristics (Morens and Fauci, 2007). Although pharmaceutical interventions, including anti-viral medications and antibiotics, are a major component of the response to infectious disease threats, they may not be readily available or affordable, especially in lower income regions of the world. Moreover, antibiotics, antivirals, and vaccines alone may not prevent adequately morbidity, mortality, transmission, and the spread of disease, and they may have other limitations, such as with regard to resistance (Gani et al., 2005; Longini et al., 2005; Germann et al., 2006; Morse, Garwin, and Olsiewski, 2006; CDC, 2007; Nuno, Chowell, and Gumel, 2007; Davey and Glass, 2008; Kerneis et al., 2008). According to the World Health Organization (WHO), NPIs undertaken outside of the healthcare system are interventions that:
limit international spread of the virus (such as travel screening and restrictions);
reduce the spread of the virus within national and local populations (such as isolation and treatment of ill persons, monitoring and possible quarantine of exposed persons, and social distancing measures, including cancellation of mass gatherings and the closure of schools);
reduce an individual person’s risk of infection (such as hand hygiene); and
communicate risk to the public (World Health Organization Writing Group, 2006).
NPIs are socially and economically disruptive, and usually require compliance by a significant proportion of the population to be effective (Haber et al., 2007; Hatchett, Mecher, and Lipsitch, 2007; Markel et al., 2007; Halloran et al., 2008; McLeod et al., 2008). Compliance depends on public support, and the public may not comply with unpopular or unclear measures. Trust in public health officials and health professionals is critical for NPI compliance (Blendon and Benson, 2001; Quah and Hin-Peng, 2004, Taylor-Clark et al., 2005, Inglesby et al., 2006). In addition, it is important for public health agencies to know which policies are likely to be supported under a given set of conditions or by certain subgroups of the population (Leung et al., 2003; Eisenman et al., 2007). Infectious disease models often rely on assumptions about public behaviour and compliance with public health recommendations; data to support these assumptions, though, are limited. Better understanding of the predictors of NPI support may help public health officials, scientists, and policymakers to design preparedness plans, to construct models to predict the outcomes of different interventions, and to interpret experiences of public health emergencies.
This study investigates the predictors of NPI support in four locations: Hong Kong, Singapore, Taiwan, and the United States. Most previous research employs simple descriptive and bivariate analyses to illustrate relationships between individual characteristics and public support. By contrast, this study uses multivariate methods and illuminates relationships between various demographic and experiential characteristics and public support. Consequently, it is possible to compare results across multiple countries and to address differences in support for voluntary versus mandatory interventions. The data were collected in the year following the SARS outbreak of 2002–03, permitting the measurement of public opinion subsequent to a real event, during which NPIs actually were used. This study is a follow-up to the paper entitled ‘Attitudes toward the use of quarantine in a public health emergency in four countries’ (Blendon et al., 2006).
Methods
Data sources
The data for this study come from a survey by the Harvard School of Public Health and the Centers for Disease Control and Prevention in response to the SARS outbreak of 2002–03. The survey was conducted by telephone in Hong Kong, Singapore, Taiwan, and the US between 18 November and 16 December 2004. Interviewees were selected through a combination of random-digit dialling (RDD) and telephone directory sampling, as was available in each region. Approximately 500 interviews were held in each region, and this information was weighted using a common weighting scheme, including age, income, number of people in the household, number of telephone lines in the household, and sex. The study sought and received Institutional Review Board approval, through the Harvard School of Public Health.
Research questions
Four major hypotheses regarding NPI prediction were developed:
Trust, particularly in public sources of information, will lead to increased support for the use of NPIs as well as punishment for non-compliance.
Concerns about infectious disease threats will lead to an increase in support for NPI utilisation and non-compliance punishment, while concerns about interventions will lead to a decrease in support.
Positive perceptions about the effectiveness of NPIs and prior experience of NPIs will lead to greater NPI support.
While levels of NPI support vary globally, the expectation is that this variation will be explained by demographic and experiential differences. Thus, the predictors of NPI support will be similar across regions.
Data analysis
Data were analysed using Stata 9 with survey analysis capabilities. Linear and logistic regression models were employed to establish the relationship between demographic and experiential factors and support for NPIs. The dependent variables (support for NPIs) were created from eight survey items. These eight items were grouped into three categories that were confirmed using factor analysis (see Appendix 1). The three categories were: support for basic NPIs; support for non-compliance punishment by arrest (that is, making an NPI mandatory); and quarantine location preferences (see Table 1). Ultimately, three main models were run for each of the four regions (see below). In addition, the same models were run for all four regions together, controlling for region, as well as for the three regions of Asia together, controlling for region. Also included are some results for identical models evaluating support for individual NPIs, instead of the support indices. These models use identical independent variables.
Table 1.
Dependent variables
| Dependent variable index | Index description | Variables included in the index |
|---|---|---|
| Basic NPIs | Average support across three variables. (Reported as 0–100%) |
Binary variables that describe support for the use of: (i) quarantine, (ii) face masks in public places, and (iii) temperature screening in public places. |
| Punishment | Average support across three variables. (Reported as 0–100%) |
Binary variables that describe support for making basic NPI non-compliance punishable by arrest, conditional on having supported the basic NPI. |
| Quarantine location preferences | Binary index, reflecting overall preference for home or facility preference (mixed results were omitted, amounting to 13.65 per cent of the overall sample population). | Preference for home or facility quarantine for 1) the respondent, and 2) a member of the respondent’s family. |
Source: authors.
Survey items were used to create the independent variables, comprising four major types of variables: trust; concern; experiential; and demographic characteristics (see Table 2). For trust, the study included a measurement of trust in public sources of information as well as a measurement of trust in private sources of information—trust in sources of information is composed of many of the key characteristics of overall trust (Frewer et al., 1996; Hunt and Frewer, 1999). To create the information trust variables, a factor analysis was used that divided the five survey trust items into two groups, which are described here as public and private sources. Public sources of information include the media, physicians, and public health officials, whereas private sources of information include employers and family/friends. Based on the results of the factor analysis, public sources of information may also be construed as more official sources of information, while private sources of information may be interpreted as more social sources of information. Each trust variable was developed by generating an average across the related survey items for each respondent, which was then modified into a binary variable (that is, those with higher levels of trust, as compared to those with lower levels of trust).
Table 2.
Independent variables
| Variable type | Name | Description |
|---|---|---|
| Trust | Public (PubTrust) | Respondent’s trust in public sources of information relating to public health. Binary variable divided along the distribution of the sample population. |
| Private (PrivateTrust) | Respondent’s average trust in private sources of information relating to public health. | |
| Concern | Disease (DsConcern) | Respondent’s concern about the 12-month risk of three infectious diseases (Avian Influenza, SARS, Smallpox). Binary variable divided along the distribution of the sample population. |
| Quarantine (QuarConcern) | Respondent’s average concern about five potential consequences of quarantine. | |
| Experiential | Personal experience (PersExp) | Respondent had heard of the use of quarantine in his/her region in the past two years. |
| Personal experience of face-mask usage (PersExpMask) | Respondent has used a face mask in the past two years, for public health purposes. | |
| Perceived efficacy of quarantine (PercEffic) | Respondent’s perception about whether quarantine was effective (among those who had heard of quarantine use in the past two years). | |
| Demographic | Gender (sex) | Gender. |
| Marital status (married) | Marital status. | |
| Education (Educ) | Education level (primary, secondary, or higher). | |
| Dependent child status (child) | Presence of a dependent child in the household. |
Source: authors.
For concern, a measurement of concern about infectious disease and a measurement of concern about the use of quarantine were included.
Experiential characteristics included: (i) the perceived effectiveness of quarantine; (ii) personal experience of quarantine; and (iii) personal experience of face-mask usage.
Finally, demographic characteristics included educational, gender, marital status, and dependent child status.
In some regional models, some of the experiential variables were dropped from the analysis because of an insufficient sample with the relevant experience. Furthermore, ethnicity variables were added for the Singapore and US analyses. Ethnicity in Singapore was specified as Chinese, Indian, Malaysian, or other, whereas ethnicity in the US was specified as white or non-white.
Ultimately, the independent variables described above were used to predict the three types of dependent variables. To test which variables were predictive of basic NPI support, a linear regression model for the basic NPI index was developed, utilising all of the independent variables above. To test support for non-compliance punishment, an identical model was used, substituting the punishment index as the dependent variable. To assess quarantine location preference, a logistic model was used, where ‘1’ represented a preference for facility-based quarantine and ‘0’ represented a preference for in-home quarantine. A set of logistic regression models was employed to predict support for the individual (non-indexed) NPIs as warranted for additional investigation. For these models, ‘1’ represented individual support and ‘0’ represented no support. These logistic models used the same set of independent variables as the linear regression models. The following are the general specifications for the three types of models for each dependent variable:
Basic NPIs = trust variables + concern variables + experiential variables + demographic variables (+/− regional controls): multivariate regression.
Non-compliance punishment = trust variables + concern variables + experiential variables + demographic variables (+/− regional controls): multivariate regression.
Quarantine location preference = trust variables + concern variables + experiential variables + demographic variables (+/− regional controls): logistic regression.
Results
Trust and NPI support
Consistent with the literature, trust in public sources of information led to significant increases in basic NPI support in Singapore and the US, as well as in the combined four region and the three Asian region samples. Individuals with higher levels of public information trust demonstrated a 7.5 percentage point increase in NPI support in the US relative to those with lower levels of public information trust (see Table 3). On analysing the subcomponents of the trust index, trust in information from physicians (as opposed to public health officials or the media) was found to be the critical determinant of whether respondents supported NPI utilisation (10 percentage point increase for those with more trust). The difference in NPI support based on trust in public sources of information in Singapore was 11.8 percentage points. In the case of Singapore, this result was driven largely by a single variable in the index: support for quarantine. Individuals with higher levels of public information trust in Singapore were significantly more likely to support quarantine than those without public information trust (odds ratio (OR): 6.83). There were no other significant predictors of quarantine support in that region. None of the study’s demographic characteristics showed statistically significant variation with respect to public trust in Singapore. Interestingly, trust in private sources of information was not a statistically significant predictor of NPI support in any sample.
Table 3.
Trust, concern, and basic NPI support (select significant results)
| Four region sample |
Hong Kong | Singapore | Taiwan | United States | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean initial support |
Coefficient | Mean initial support |
Coefficient | Mean initial support |
Coefficient | Mean initial support |
Coefficient | Mean initial support |
Coefficient | |
| 84% | 86% | 86% | 98% | 64% | ||||||
| Public trust | 0.029 (0.017)+ | 0.118 (0.033)** | 0.075 (0.037)* | |||||||
| Disease concern | 0.052 (0.028)+ | 0.052 (0.025)* | 0.085 (0.045)+ | |||||||
| Concern about quarantine | −0.067 (0.040) + | |||||||||
Notes:
Standard errors in parentheses.
Significant at 10%;
Significant at 5%;
Significant at 1%.
Source: authors.
Respondents who supported a given NPI were asked if they would continue to support it if non-compliance was punishable by arrest. While trust in public sources of information was significant in the formation of basic NPI support, it was not associated with support for punishment for non-compliance in most regions (see Table 4). The exception to this was Taiwan, where individuals with higher levels of trust in public sources demonstrated a 7.5 percentage point increase in support for punishment (significant at p<0.1).
Table 4.
Trust, concern, and punishment support (select significant results)
| Four region sample |
Hong Kong | Singapore | Taiwan | United States | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean initial support |
Coefficient | Mean initial support |
Coefficient | Mean initial support |
Coefficient | Mean initial support |
Coefficient | Mean initial support |
Coefficient | |
| 72% | 58% | 72% | 82% | 72% | ||||||
| PubTrust | 0.117 (0.069)+ | 0.075 (0.041)+ | ||||||||
| DsConcern | 0.078 (0.029)** | 0.128 (0.059)* | 0.119 (0.054)* | |||||||
Notes:
Standard errors in parentheses.
Significant at 10%;
Significant at 5%;
Significant at 1%.
Source: authors.
Minorities and non-compliance punishment
The effects of ethnicity were perhaps the most striking in terms of support for non-compliance punishment. In the US, non-whites were significantly less likely to support arrest for non-compliance than their white counterparts (see Figure 1). Being non-white was associated with a 26.6 percentage point decrease in support for punishment. This result was significant across all three individual variables in the index, with non-whites less likely to support punishment for quarantine non-compliance (OR: 0.37), less likely to support punishment for face-mask usage non-compliance (OR: 0.27), and less likely to support punishment for temperature-screening non-compliance (OR: 0.32). In Singapore, respondents who reported their ethnicity as Malaysian, as opposed to Chinese, were ~20 percentage points less likely to support the punishment index. This was driven entirely by decreased support for punishment for quarantine non-compliance; Malaysians were less likely to support arrest (OR: 0.36).
Figure 1.
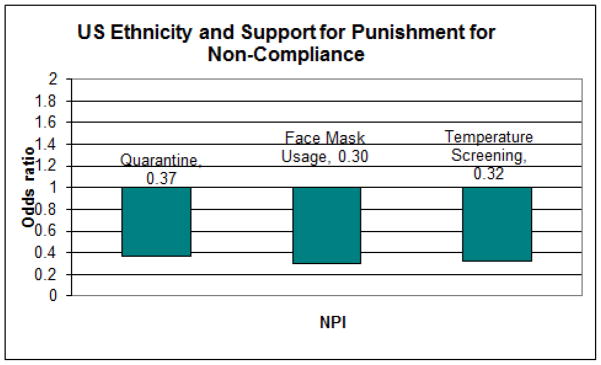
US ethnicity and support for punishment of non-compliance
Note: support for NPI compliance is lower among non-white US citizens than white US citizens (OR<1).
Source: authors.
Concern about disease
Those with higher levels of concern about disease demonstrated significant increases in basic NPI support in Singapore and marginally significant increases in NPI support in Hong Kong and the US (see Table 3). High levels of concern about disease, relative to low levels, led to more support for punishment in the Hong Kong, Singapore, and combined four region samples (see Table 4).
The study speculated that specific diseases may be more predictive of NPI support than others. To test this, the models were run again, substituting a specific disease (Avian Influenza, SARS, Seasonal Influenza, or Smallpox) for the disease concern index (results not shown). In Hong Kong, statistically significant or marginally significant increases in support for the basic index for all four types of disease concern were found. When broken down into individual NPIs, disease concerns generally led to increased support for temperature screening only. In the US, concern about Smallpox and Seasonal Influenza led to increased support for the basic index. Quarantine, face-mask usage, and temperature screening all produced marginally significant results related to Smallpox (OR: 6.42, 2.52, 2.40), whereas quarantine and temperature screening produced significant results related to Seasonal Influenza (OR: 4.25, 2.20). In Singapore, it was found that concerns about Smallpox resulted in increased support for the punishment index, which could be attributed to support for punishment for non-compliance with face-mask usage (OR: 3.23). A factor analysis showed that all four diseases loaded onto a single factor for the full sample, as well as by region.
Perceived effectiveness and personal experience
Higher perceived efficacy of quarantine correlated with an increase in support for the basic NPI index in the Hong Kong (25.1 percentage points) and combined region samples (12–13 percentage points) (results not shown). With regard to punishment for non-compliance, perceptions about quarantine efficacy led to decreases in support of ~25 percentage points in Hong Kong and Singapore. Personal experience of quarantine generally failed to predict support for either NPI utilisation or non-compliance punishment. The only exception was Taiwan, where prior experience led to an increase in support for punishment (10.4 percentage points). A surprising result of the study was the significance of prior experience of face-mask usage, which was significantly and positively associated with support for the basic NPI index in all individual regions and in the combined sample (see Figure 2). At the individual variable level, prior experience positively predicted support for face-mask usage in all regions, with individuals more likely to support it if they had had prior experience. Prior experience of face-mask usage also led to support for the use of quarantine in Taiwan, with experienced respondents significantly more likely to support quarantine than inexperienced ones (OR: 48.13). Furthermore, no other variable significantly predicted support for the use of quarantine in Taiwan.
Figure 2.
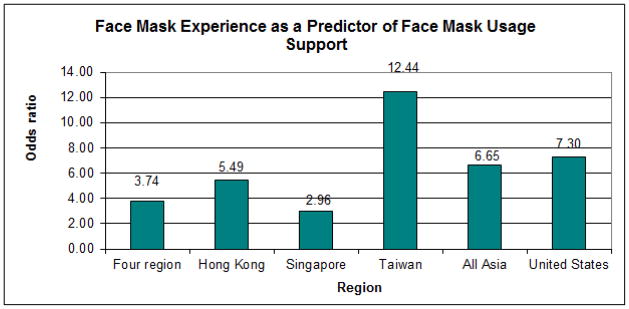
Prior experience as a predictor of support for face-mask usage
Note: respondents who had used a face mask in the past demonstrated increased support for the use of face masks in public health emergencies, relative to those with no experience (OR>1). This effect can be seen in all regions and samples investigated.
Source: authors.
There were few statistically significant differences between population groupings, in terms of their experience with face masks. In the four region sample, education was associated with lower experience of face-mask usage. Those with primary and secondary education had more experience (71 and 56 per cent, respectively). Only 39 per cent of those with higher education had experience of face-mask usage. Moreover, married respondents were more likely to have used a face mask (57 per cent). In Singapore, the proportion of Chinese respondents who had used a mask was lower than the proportion who had no such experience. Only six per cent of separated or divorced individuals had experience of face masks, as compared to 30 per cent of married respondents. Gender was the only characteristic that showed any difference in Taiwan, with men (85 per cent) having less experience than women (94 per cent).
Quarantine location preference
The survey asked respondents about their preferences for home versus institutional quarantine for themselves and their families. In general, it was discovered that the study’s models explained very little of the variation in this area and that few variables were significantly associated with preferences. There were a few exceptions to this. First, perceptions about the effectiveness of quarantine led to increases in the likelihood of institutional quarantine preference in Singapore (OR: 3.97). In the US, rising levels of education were associated with increased preferences for institutional quarantine, with those with secondary and higher education more likely to support institutional quarantine over in-home quarantine (OR: ~10–14). Ethnicity was again significant in the US, with non-whites more likely to support in-home quarantine (OR: 0.35). Finally, concern about infectious diseases led to an increase in support for in-home quarantine in the four region sample (OR: 0.66).
Discussion
It is unlikely that pharmaceutical options will be available immediately and will be unlimited, which is why NPIs are an important consideration for the response to any future infectious disease threat. However, there is no single strategy for NPI implementation. There is a growing body of evidence that suggests that NPIs are most effective when instituted in a timely, sustained, and layered fashion (Longini et al., 2005; Ferguson et al., 2005, 2006; Germann et al., 2006; Glass et al., 2006; Bootsma and Ferguson, 2007; Hatchett, Mecher, and Lipsitch, 2007; Halloran et al., 2008; Lee, Lye, and Wilder-Smith, 2009; Stern, Cetron, and Markel, 2009). The more disruptive an intervention, the more challenging it is for the public to comply (Finkelstein et al., 2009). Understanding how the public is likely to respond to a public health intervention is crucial, therefore, to pandemic planning.
No single response
Contrary to the expectations of the authors, the results suggest that there are significant differences in the predictors of NPI policy support between regions. This was true for both the indices of support as well as for the models for individual NPIs (only select data shown). While international planning organisations, such as WHO, do recommend that nation states accommodate their own population needs, policy recommendations often are uniform (World Health Organization Writing Group, 2006). Even accounting for variations in the population characteristics themselves, this research indicates that public support will likely vary widely between regions. Immeasurable variables, such as culture, may provide the only explanation for this variation.
Importantly, NPI use remains a particularly valuable option for underdeveloped regions of the world, where a pharmaceutical response may be totally absent or extremely delayed (World Health Organization Writing Group, 2006). The study’s finding suggests that policy planning should account for some degree of local flexibility or decentralisation. Research from other pandemic/epidemic events also should be evaluated in context. That is, local experiences may not be directly translatable and careful attention should be paid to the willingness of a population to adopt specific public health interventions.
A related concept is the evaluation of characteristics for their static and dynamic properties. While the data in this study are cross-sectional and cannot describe changes over time, it is reasonable to expect that some of these variables will not remain constant, especially in the case of a progressing pandemic. Demographic variables are likely to be static, at least in the short run, while variables such as concern, trust, and personal experience are more likely to be dynamic. Understanding the dominance of a characteristic as well as its stability over time may help decision-makers to develop the most readily accepted and supported policies.
Infectious disease concerns
The literature, including recent studies of the H1N1 response, has demonstrated a relationship between concern (risk perception) and behavioural change, including responses to infectious disease threats (Leung et al., 2003; Cava et al., 2005; Abbate et al., 2006; Brewer et al., 2007; Jones and Salathe, 2009; Rubin et al., 2009; Eastwood et al., 2010; Manuell and Cukor, 2011). The study’s results did not reflect such a strong association. However, unlike the short-term perspective of many studies, the results of this research reflect perceptions about 12-month risk to self and family. While short-term risk perception should be captured by a long-term perspective, it is possible that perceptions of long-term risk have less variation across individuals than short-term risk (that is, risk perceptions converge). If this is the case, then the results would seem to suggest that it is acute risk perceptions, not overall concerns about disease, that translate into behavioural change. Furthermore, where significant results were not apparent, they were disease-specific and did not translate across all of the infectious disease threats (with the exception of Hong Kong and support for temperature screening). Jones and Salathe (2009), in their analysis of the H1N1 response, suggest that certain risk perceptions (public health and otherwise) clustered together. The results of the current study do not show a similar clustering, but, again, this may be due to the long-term nature of the survey items.
Trust
Consistent with the existing literature, the research did find linkages between trust in sources of public information and NPI support. This was particularly true in the case of the individual’s own physician or healthcare provider. This does yield a strong policy lever, in that healthcare providers can be seen as instrumental in NPI education and promotion and thus targeted. Likewise, it is essential to make sure that the providers themselves are well-educated in the requirements and the benefits of the NPI needed. Sources of private information were not as influential for support, but this survey was conducted before significant changes in the social media landscape, which may have a bearing on this finding.
Minority populations
Research has shown that minorities and vulnerable populations are likely to fare worse than the general public during public health emergencies (Fothergill, Maestas, and Darlington, 1999; Cutter et al., 2006). Recently (in 2009), US minorities were shown to have experienced worse outcomes than non-minorities during the H1N1 pandemic (Quinn et al., 2011), with disparities also extending to infection rates and intervention uptake. The reasons for this include social vulnerabilities (Cutter and Finch, 2008; Schoch-Spana et al., 2010; Quinn et al., 2011) and baseline-level co-morbidities (Hutchins et al., 2009). Minority and vulnerable populations also may belong to distinct social networks, and may utilise separate communication lines and sources of information, which are not always congruous with public health messaging (Plough et al., 2011). Thus, targeting interventions appropriately for these populations is an important part of public health policy setting (Hutchins et al., 2009).
The study’s results show that non-white US citizens in particular had concerns about the legal enforcement of authoritative public health measures and that these concerns were consistent across different measures. Historical experience as well as perceived social and economic disenfranchisement may account for such a striking difference in support for the use of arrest for non-compliance. However, this is probably not limited to the issue of race in the US, since other types of minority populations are likely to express distinct needs and preferences and other regions may face similar heterogeneity. It is not news that public health policymakers and practitioners will need to make efforts to increase trust and to educate subgroups before events to secure more willingness to comply. The study’s results go further, though, suggesting that the specific consequences associated with public health policies will need to be vetted carefully for minority support. This is particularly true for law enforcement, but may also apply to the compulsory or voluntary nature of an intervention.
Face-mask usage and gateway interventions
Significant positive associations were found between prior face-mask usage and basic NPI support, both in the aggregated and the individual analyses. There are several potential explanations for the results. Notably, the people who have been willing to use a face mask in response to prior disease threats may be those who were already most concerned about disease or most accepting of public health suggestions. Alternatively, the wearing of a face mask may accustom users to participation in public health measures and condition them to expect positive outcomes from such initiatives, and hence make them more willing to use face masks again or to comply with other public health recommendations.
The latter explanations suggest that face-mask usage could serve as a ‘gateway’ to acceptance of, and participation in, other public health interventions. If NPI support can be influenced through introduction to certain measures, then it may be possible to expose populations to NPIs in advance of an emergency. The exposure of populations to face masks prior to an outbreak is a particularly intriguing option, since they are inexpensive and easy to distribute. While the effectiveness of face-mask usage is currently under debate (MacIntyre et al., 2009; Cowling et al., 2010; Tracht, Del Valle, and Hyman, 2010), their usefulness may go beyond their direct role in disease prevention and instead be a way to increase population compliance with other NPIs, such as quarantine. The effectiveness discussion is largely scientific; however, an individual may perceive an experience of face-mask usage as ‘positive’ with a much more simple perspective. This could happen when he/she does not become ill or does not make the family ill when wearing the mask, or simply when he/she finds the wearing of the mask to be non-burdensome. If face masks were shown to be completely ineffective or harmful in the future, though, this could lead to a negative gateway experience, potentially reducing future compliance. In much the same way as hand sanitizers came to be widely accepted before H1N1, the correct usage of pre-pandemic exposures to public health interventions may create a more public health aware and savvy population.
Limitations
This study provides some valuable lessons for policymakers in understanding the variation in policy support prediction. However, it does have some limitations and caveats. The sample was limited to roughly 500 individuals per region and only four regions were included in the study. In addition, the analysis was restricted to items from the survey, and does not give insight into details about personal experiences, such as those concerning quarantine or face-mask usage. More research is needed to validate the findings on face-mask utilisation, particularly into how these findings may be useful in serving public health aims. The study was also conducted in four regions as a follow-up to the SARS epidemic, with which these regions had varying levels of exposure and NPI experience. Yet, while levels of public opinion (concern, trust, for example) and policy support may vary over time, there is no reason to believe that the relationships between individual characteristics and policy support are as variable.
Conclusion
Culture appears to play a major role in the relationships between individual characteristics and NPI support, suggesting that a single global strategy for NPI implementation is unlikely to be successful. Public health policymakers also should be aware of the relationships between minorities and the consequences for non-compliance, which may extend to the compulsory or voluntary nature of an NPI. Finally, the research suggests that some public health interventions may be ‘gateway’ interventions and could lead to increased acceptance of and compliance with future public health interventions.
Acknowledgments
The authors would like to acknowledge the Agency for Healthcare Research and Quality and the National Institutes of Health for their funding support: AHRQ: T32 HS000055 (J. Newhouse); NIH: 5 T32 AI07433 – 14 (K. Freedberg); and AHRQ: T32 HS017587 (K. Kraemer).
Appendix 1. Supplemental materials
Demographic characteristics
| Demographic characteristics | Four region sample | All Asia sample | United States | Hong Kong | Taiwan | Singapore | |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | 46.17% | 47.69% | 41.60% | 46.11% | 50.00% | 46.97% | |
| Female | 53.83% | 52.31% | 58.40% | 53.89% | 50.00% | 53.03% | |
| Marital status | |||||||
| Married | 62.65% | 64.62% | 56.49% | 61.90% | 68.50% | 63.53% | |
| Divorced/separated | 6.22% | 2.47% | 17.99% | 3.43% | 2.03% | 1.96% | |
| Widow(er) | 4.00% | 2.54% | 8.58% | 5.04% | .41% | 2.16% | |
| Single | 27.13% | 30.37% | 16.95% | 29.64% | 29.07% | 32.35% | |
| Education | |||||||
| Primary | 15.28% | 17.94% | 7.05% | 22.02% | 20.82% | 11.20% | |
| Secondary | 37.20% | 40.29% | 27.59% | 49.09% | 33.06% | 38.70% | |
| Post-secondary | 47.52% | 41.77% | 65.35% | 28.89% | 46.12% | 50.10% | |
| Dependent child | |||||||
| Yes | 55.46% | 53.11% | 62.71% | 60.94% | 49.48% | 49.02% | |
| No | 44.54% | 46.89% | 37.29% | 39.06% | 50.52% | 50.98% | |
| US ethnicity | |||||||
| White | 76.04% | ||||||
| Non-white | 23.96% | ||||||
| Singapore ethnicity | |||||||
| Chinese | 73.78% | ||||||
| Malaysian | 17.42% | ||||||
| Indian | 5.28% | ||||||
| Other | 3.52% | ||||||
Factor analysis results
Trust variables
The survey was composed of five items relating to sources of public health information in which the respondent could express trust: public health authorities; media sources; friends and family; doctors/healthcare professionals; and employers. A similar factor analysis (principal component analysis (PCA) with promax rotation) was conducted, which resulted in two factors: public trust, including public health authorities, doctors, and the media; and private trust, including friends/family and employers. Rotated factor loadings are presented below.
Rotated factor loadings (pattern matrix) and unique variances
| Variable | | Factor 1 | Factor2 | | Uniqueness |
|---|---|---|---|
| q20_1 | | 0.8785 | −0.1820 | | 0.2867 |
| q20_2 | | 0.7228 | 0.0758 | | 0.4405 |
| q20_3 | | −0.1895 | 0.8963 | | 0.2581 |
| q20_4 | | 0.5339 | 0.1773 | | 0.6293 |
| q20_5 | | 0.1484 | 0.7347 | | 0.3757 |
Variable descriptions:
q20_1 = government public health authorities
q20_2 = newspapers, magazines, television, or radio that you usually watch, read or listen to
q20_3 = a family member or a friend
q20_4 = your doctor or other healthcare professional
q20_5 = your employer
Non-pharmaceutical interventions
The last two factor analyses related to the dependent variables, the NPIs. The survey included a lengthy list of potential NPIs in which respondents could express support, including NPI usage (such as quarantine, face-mask usage. and temperature screening), quarantine monitoring (such as call monitoring, video monitoring, daily visitation, electronic bracelet usage, and posting guards), and a preference for home/institutional quarantine (for respondent and family). The factor analysis confirmed the presence of three factors that follow the groupings listed above: ‘basic NPI support’; ‘quarantine monitoring support’; and ‘quarantine location preference’. Quarantine monitoring support variables subsequently were omitted from the study. The rotated factor loadings are presented below.
Rotated factor loadings (pattern matrix) and unique variances
| Variable | | Factor 1 | Factor 2 | Factor 3 | | Uniqueness |
|---|---|---|---|---|
| SuppQuar | | 0.6130 | 0.0796 | 0.1040 | | 0.5879 |
| SuppMask | | 0.8080 | −0.1768 | −0.0843 | | 0.4122 |
| SuppTemp | | 0.7144 | −0.0354 | −0.0793 | | 0.4866 |
| SuppCallMon | | 0.0408 | 0.5698 | 0.3116 | | 0.6066 |
| SuppVidMon | | −0.1968 | 0.7748 | −0.1182 | | 0.4599 |
| SuppDailyVis | | 0.3653 | 0.1966 | 0.0913 | | 0.7738 |
| SuppElecBr~e | | 0.0079 | 0.6501 | −0.1342 | | 0.5322 |
| SuppGuards | | 0.1616 | 0.4017 | −0.1386 | | 0.7170 |
| FamQuarPref | | −0.0053 | −0.0667 | 0.8782 | | 0.2075 |
| SelfQuarPref | | −0.0728 | −0.0217 | 0.8677 | | 0.2154 |
Variable descriptions:
SuppQuar: support for the use of quarantine.
SuppMask: support for the use of face masks.
SuppTemp: support for the use of temperature screening.
SuppCallMon: support for the use of call monitoring.
SuppVidMon: support for the use of video monitoring.
SuppDailyVis: support for the use of daily visitation for monitoring.
SuppElecBrace: support for the use of electronic bracelets for monitoring.
SuppGuards: support for the use of guards for monitoring.
FamQuarPref: home or institutional preference for quarantine for respondent’s family.
SelfQuarPref: home or institutional preference for quarantine for respondent.
The survey also contained three items that enquired into whether respondents would continue to support the basic NPIs if non-compliance was punishable by arrest. These items could not be factored into the earlier analysis, because they were asked conditionally in relation to support for the NPI itself. Hence, these items were factored separately, yielding a single factor called ‘support for NPI punishment’. The rotated factor loadings are presented below.
Rotated factor loadings (pattern matrix) and unique variances
| Variable | | Factor 1 | | Uniqueness |
|---|---|---|
| SuppQuarPun | | 0.7777 | | 0.3952 |
| SuppMaskPun | | 0.8624 | | 0.2562 |
| SuppTempPun | | 0.8772 | | 0.2305 |
Variable descriptions:
SuppQuarPun: support for quarantine, when non-compliance is punishable by arrest.
SuppMaskPun: support for face-mask usage, when non-compliance is punishable by arrest.
SuppTempPun: support for temperature screening, when non-compliance is punishable by arrest.
Selected survey items
Basic NPI support items
‘If there were a major outbreak of a serious contagious disease such as SARS, smallpox, or avian flu, the government could take a number of steps to control its spread. Would you favor or oppose…?’
(Favor/Oppose)
requiring people suspected of having been exposed to the disease to be quarantined.
requiring everyone to wear a mask in public.
requiring everyone to have their temperature taken to screen for illness before entering public places.
Punishment for non-compliance items
‘Would you still favor that even if people who refuse could be arrested or would you oppose that?’
(Favor/Oppose)
requiring people suspected of having been exposed to the disease to be quarantined.
requiring everyone to wear a mask in public.
requiring everyone to have their temperature taken to screen for illness before entering public places.
Personal experience of face-mask use
‘Thinking about other outbreaks of contagious disease in your community in the past two years, have you worn a mask in public to protect yourself against becoming ill, or haven’t you done this?’
(Have/Have not)
Quarantine location preference
‘If one of your family members had to be quarantined because they may have been exposed to a contagious disease, would you prefer to have them quarantined at home with you or in a separate facility?’
(Home/Facility)
‘If YOU had to be quarantined because you may have been exposed to a contagious disease, would you prefer to be quarantined at home or in a separate facility?’
(Home/Facility)
Trust in information sources
‘If there were an outbreak of a contagious disease such as SARS, smallpox, or avian flu in your community how much would you trust the following sources to give you useful and accurate information about the outbreak?’
The first is [INSERT]. Would you trust them a lot, a little, or not at all?
Government public health authorities.
Newspapers, magazines, television, or radio that you usually watch, read or listen to.
A family member or a friend.
Your doctor or other healthcare professional.
Your employer.
Personal experience of quarantine
‘Have you heard or read about anyone being quarantined in [INSERT RESPONDENT’S COUNTRY/REGION] during the past two years?’
(Yes/No)
Perceived efficacy of quarantine
‘When quarantine was last used in [INSERT RESPONDENT’S COUNTRY/REGION], do you think it was effective or not effective in keeping the disease from spreading?’
(Was effective/Was not effective)
Infectious disease concerns
‘Are you worried that you or someone in your immediate family may get sick from [INSERT ITEM] DURING THE NEXT 12 MONTHS, or aren’t you concerned about that?’
(Worried/Not worried)
SARS.
Smallpox.
The regular or seasonal flu.
The avian or bird flu.
‘[If worried] How worried are you that you or someone in your immediate family may get sick from [INSERT ITEM FROM Q1] during the next 12 months? Are you very worried, somewhat worried, or not very worried?’
SARS.
Smallpox.
The regular or seasonal flu.
The avian or bird flu.
Contributor Information
Francesca Matthews Pillemer, Policy Researcher at the RAND Corporation, United States.
Robert J. Blendon, Senior Associate Dean for Policy Translation and Leadership Development and Professor of Health Policy and Political Analysis at Harvard School of Public Health, United States.
Alan M. Zaslavsky, Professor of Health Care Policy at the Department of Health Care Policy, Harvard Medical School, United States.
Bruce Y. Lee, Director of Operations Research at the International Vaccine Access Center, Johns Hopkins Bloomberg School of Public Health, United States.
References
- Abbate R, Di Giuseppe G, Marinelli P, Angelillo IF. Knowledge, attitudes, and practices of avian influenza, poultry workers, Italy. Emerging Infectious Diseases. 2006;12(11):1762–1765. doi: 10.3201/eid1211.060671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blendon RJ, Benson JM. Americans’ views on health policy: a fifty-year historical perspective. Health Affairs. 2001;20(2):33–46. doi: 10.1377/hlthaff.20.2.33. [DOI] [PubMed] [Google Scholar]
- Blendon RJ, et al. Attitudes toward the use of quarantine in a public health emergency in four countries. Health Affairs. 2006;25(2):w15–w25. doi: 10.1377/hlthaff.25.w15. [DOI] [PubMed] [Google Scholar]
- Bootsma MC, Ferguson NM. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(18):7588–7593. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychology. 2007;26(2):136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- Cava MA, Fay KE, Beanlands HJ, McCay EA, Wignall R. Risk perception and compliance with quarantine during the SARS outbreak. Journal of Nursing Scholarship. 2005;37(4):343–347. doi: 10.1111/j.1547-5069.2005.00059.x. [DOI] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention) Interim Pre-pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States. CDC; Atlanta: 2007. [Google Scholar]
- Cooper B, Pitman R, Edmunds W, Gay N. Delaying the international spread of pandemic influenza. PLoS Medicine. 2006;3(6):e212. doi: 10.1371/journal.pmed.0030212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling BJ, Zhou Y, Ip DK, Leung GM, Aiello AE. Face masks to prevent transmission of influenza virus: a systematic review. Epidemiology and Infection. 2010;138(4):449–456. doi: 10.1017/S0950268809991658. [DOI] [PubMed] [Google Scholar]
- Cutter S, et al. The long road home: race, class, and recovery from Hurricane Katrina. Environment: Science and Policy for Sustainable Development. 2006;48(2):8–20. [Google Scholar]
- Cutter SL, Finch C. Temporal and spatial changes in social vulnerability to natural hazards. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(7):2301–2306. doi: 10.1073/pnas.0710375105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey VJ, Glass RJ. Rescinding community mitigation strategies in an influenza pandemic. Emerging Infectious Diseases. 2008;14(3):365–372. doi: 10.3201/eid1403.070673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health. Risk of a Human Influenza Pandemic Emerging from Avian H5N1 Viruses: Scientific Evidence Base. Department of Health; London: 2007. [Google Scholar]
- Eastwood K, Durrheim DN, Butler M, Jon A. Responses to pandemic (H1N1) 2009, Australia. Emerging Infectious Diseases. 2010;16(8):1211–1216. doi: 10.3201/eid1608.100132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenman DP, Cordasco KM, Asch S, Golden JF, Glik D. Disaster planning and risk communication with vulnerable communities: lessons from Hurricane Katrina. American Journal of Public Health. 2007;97(Supplement 1):S109–S115. doi: 10.2105/AJPH.2005.084335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson NM, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437(7056):209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- Ferguson NM, et al. Strategies for mitigating an influenza pandemic. Nature. 2006;442(27 July 2006):448–452. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein S, Prakash S, Nigmatulina K, Klaiman T, Larson R. Pandemic influenza: non-pharmaceutical interventions and behavioral changes that may save lives. International Journal of Health Management and Information. 2009;1(1):1–18. [Google Scholar]
- Fothergill A, Maestas EG, Darlington JD. Race, ethnicity and disasters in the United States: a review of the literature. Disasters. 1999;23(2):156–173. doi: 10.1111/1467-7717.00111. [DOI] [PubMed] [Google Scholar]
- Frewer LJ, Howard C, Hedderley D, Shepherd R. What determines trust in information about food-related risks? Underlying psychological constructs. Risk Analysis. 1996;16(4):473–486. doi: 10.1111/j.1539-6924.1996.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Gani R, et al. Potential impact of antiviral drug use during influenza pandemic. Emerging Infectious Diseases. 2005;11(9):1355–1362. doi: 10.3201/eid1109.041344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germann TC, Kadau K, Longini IM, Jr, Macken CA. Mitigation strategies for pandemic influenza in the United States. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(15):5935–5940. doi: 10.1073/pnas.0601266103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass RJ, Glass LM, Beyeler WE, Min HJ. Targeted social distancing design for pandemic influenza. Emerging Infectious Diseases. 2006;12(11):1671–1681. doi: 10.3201/eid1211.060255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haber MJ, et al. Effectiveness of interventions to reduce contact rates during a simulated influenza pandemic. Emerging Infectious Diseases. 2007;13(4):581–589. doi: 10.3201/eid1304.060828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halloran ME, et al. Modeling targeted layered containment of an influenza pandemic in the United States. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(12):4639–4644. doi: 10.1073/pnas.0706849105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(18):7582–7587. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt S, Frewer LJ. Public trust in sources of information about radiation risks in the UK. Journal of Risk Research. 1999;2(2):167–180. [Google Scholar]
- Hutchins SS, Fiscella K, Levine RS, Ompad DC, McDonald M. Protection of racial/ethnic minority populations during an influenza pandemic. American Journal of Public Health. 2009;99(Supplement 2):S261–S270. doi: 10.2105/AJPH.2009.161505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglesby TV, Nuzzo JB, O’Toole T, Henderson DA. Disease mitigation measures in the control of pandemic influenza. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2006;4(4):366–375. doi: 10.1089/bsp.2006.4.366. [DOI] [PubMed] [Google Scholar]
- Jones JH, Salathe M. Early assessment of anxiety and behavioral response to novel swine-origin influenza A(H1N1) PLoS One. 2009;4(12):e8032. doi: 10.1371/journal.pone.0008032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz A, Staiti AB, McKenzie KL. Preparing for the unknown, responding to the known: communities and public health preparedness. Health Affairs. 2006;25(4):946–957. doi: 10.1377/hlthaff.25.4.946. [DOI] [PubMed] [Google Scholar]
- Kerneis S, Grais RF, Boelle PY, Flahault A, Vergu E. Does the effectiveness of control measures depend on the influenza pandemic profile? PLoS ONE. 2008;3(1):e1478. doi: 10.1371/journal.pone.0001478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee V, Lye D, Wilder-Smith A. Combination strategies for pandemic influenza response—a systematic review of mathematical modeling studies. BMC Medicine. 2009;7(1) doi: 10.1186/1741-7015-7-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung GM, et al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. Journal of Epidemiology and Community Health. 2003;57(1):857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longini IM, Jr, et al. Containing pandemic influenza at the source. Science. 2005;309(5737):1083–1087. doi: 10.1126/science.1115717. [DOI] [PubMed] [Google Scholar]
- MacIntyre CR, et al. Face mask use and control of respiratory virus transmission in households. Emerging Infectious Diseases. 2009;15(2):233–241. doi: 10.3201/eid1502.081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manuell M-E, Cukor J. Mother Nature versus human nature: public compliance with evacuation and quarantine. Disasters. 2011;35(2):417–442. doi: 10.1111/j.1467-7717.2010.01219.x. [DOI] [PubMed] [Google Scholar]
- Markel H, et al. Nonpharmaceutical interventions implemented by US cities during the 1918–1919 influenza pandemic. Journal of the American Medical Association. 2007;298(6):644–654. doi: 10.1001/jama.298.6.644. [DOI] [PubMed] [Google Scholar]
- McLeod MA, et al. Protective effect of maritime quarantine in South Pacific jurisdictions, 1918–19 influenza pandemic. Emerging Infectious Diseases. 2008;14(3):468–470. doi: 10.3201/eid1403.07-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morens DM, Fauci AS. The 1918 influenza pandemic: insights for the 21st Century. Journal of Infectious Diseases. 2007;195(7):1018–1028. doi: 10.1086/511989. [DOI] [PubMed] [Google Scholar]
- Morse SS, Garwin RL, Olsiewski PJ. Public health. Next flu pandemic: what to do until the vaccine arrives? Science. 2006;314(5801):929. doi: 10.1126/science.1135823. [DOI] [PubMed] [Google Scholar]
- Nuno M, Chowell G, Gumel AB. Assessing the role of basic control measures, antivirals and vaccine in curtailing pandemic influenza: scenarios for the US, UK and the Netherlands. Journal of the Royal Society, Interface. 2007;4(14):505–5021. doi: 10.1098/rsif.2006.0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plough A, Bristow B, Fielding J, Caldwell S, Khan S. Pandemics and health equity: lessons learned from the H1N1 response in Los Angeles County. Journal of Public Health Management and Practice. 2011;17(1):20–27. doi: 10.1097/PHH.0b013e3181ff2ad7. [DOI] [PubMed] [Google Scholar]
- Quah SR, Hin-Peng L. Crisis prevention and management during SARS outbreak, Singapore. Emerging Infectious Diseases. 2004;10(2):364–368. doi: 10.3201/eid1002.030418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn SC, et al. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. American Journal of Public Health. 2011;101(2):285–293. doi: 10.2105/AJPH.2009.188029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin GJ, Amlot R, Page L, Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. British Medical Journal. 2009;339:b2651. doi: 10.1136/bmj.b2651. http://dx.doi.org/10.1136/bmj.b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoch-Spana M, Bouri N, Rambhia KJ, Norwood A. Stigma, health disparities, and the 2009 H1N1 influenza pandemic: how to protect Latino farmworkers in future health emergencies. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2010;8(3):243–254. doi: 10.1089/bsp.2010.0021. [DOI] [PubMed] [Google Scholar]
- Stern AM, Cetron MS, Markel H. Closing the schools: lessons from the 1918–19 U.S. influenza pandemic. Health Affairs. 2009;28(6):w1066–w1078. doi: 10.1377/hlthaff.28.6.w1066. [DOI] [PubMed] [Google Scholar]
- Taylor-Clark K, Blendon RJ, Zaslavsky A, Benson J. Confidence in crisis? Understanding trust in government and public attitudes toward mandatory state health powers. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2005;3(2):138–147. doi: 10.1089/bsp.2005.3.138. [DOI] [PubMed] [Google Scholar]
- Tracht SM, Del Valle SY, Hyman JM. Mathematical modeling of the effectiveness of facemasks in reducing the spread of novel influenza A (H1N1)’. PloS ONE. 2010;5(2):e9018. doi: 10.1371/journal.pone.0009018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Writing Group . Nonpharmaceutical interventions for pandemic influenza, international measures. Emerging Infectious Diseases. 2006;12(1):81–87. doi: 10.3201/eid1201.051370. [DOI] [PMC free article] [PubMed] [Google Scholar]


