Abstract
Context:
Takayasu arteritis (TA) is a chronic inflammatory disease involving large vessels like aorta and its major branches. It presents to clinician with features of arm claudication, stroke, asymmetrical pulse, or asymmetrical blood pressure in both limbs. Digital gangrene may be occurred secondary to various systemic diseases like diabetes, thrombophilic states, vascular embolism, and medium and small vessel vasculitis or infections. Through evaluation to diagnose the exact etiology and timely intervention is needed to prevent progression of the gangrene which at the time can be life-threatening. Digital gangrene as an initial presentation in TA is very rare. In medical literature, there are only few case reports have been reported.
Case Report:
We are reporting a case of a 26-year-old female patient presented with right little finger and index finger gangrene, ultimately diagnosed as TA and responded dramatically to treatment.
Conclusion:
Though rare, TA should be taken in the differential diagnosis for work up in a case of digital gangrene and it necessitates more studies in this field to uncover the exact pathophysiology for such presentation.
Keywords: Digital gangrene, Takayasu arteritis, Initial prasentation, Differential diagnosis
Introduction
Takayasu arteritis (TA) is inflammatory vasculitis of unknown origin involving large vessels and its major branches, most frequently in young women.[1,2] It occurs more commonly in Japan, China, India, and Southeast Asia; the disease is also prevalent in Mexico.[1] Vascular insufficiency from stenosis, occlusion, or aneurysm is the common mode of presentation. These are arm claudication, absent pulse, carotid bruit, hypertension, asymmetric arm blood pressure, carotidynia, lightheadedness, stroke, and aortic regurgitation.[1] Constitutional symptoms like fever, malaise, weight loss, and night sweats are also commonly present.[1,3] Cutaneous manifestations develop less than 10% of patients of TA.[1] Erythema nodosum is most common. Livedo reticularis, ulceration, and purpura are very rare. Digital gangrene is also very rare, only one case reported worldwide till date.[4] Our patient who is suffering from Takayasu's arteritis according to American College of Rheumatology Criteria has digital gangrene of both hands, a rare manifestation of TA.
Case Presentation
A 26-year-old female patient came to our hospital with history of pain and black discoloration of index and little fingers of right hand for last 1 month with history of intermittent claudication of right arm for which she had difficulty in doing her household work. Patient was not a known diabetic or hypertensive. There was no history of fever, joint pain, oral ulcer, photosensitive rashes, Raynaud's phenomenon, chest pain, palpitation, trauma, pain abdomen, pedal swelling, headache, visual abnormalities, chronic drug intake, or addiction. Past and family history was noncontributory. Patient was unmarried.
On examination, pulse rate was 88 beats/min, regular with brachial and radial pulse on right side found to be feeble compared to left side. Lower limb peripheral pulses were normal and equally palpable both side. Blood pressure was 94/68 mmHg in the right arm, 124/78 mmHg on left arm, and 138/84 and 144/80 mmHg in right and left leg, respectively. There was a bruit audible over infraclavicular region on the right side without any renal or abdominal bruit. Local examination of left hand showed, there was a dry gangrene with a clear cut line of demarcation between normal and gangrenous tissue [Figure 1]. Other systemic examination was absolutely normal.
Figure 1.

Dry gangrene of left little and ring finger of left hand
Further investigational workup revealed patient's hemoglobin was 10.4 g/dL, total leukocyte count of 8,600/mm3 with normal differential count and platelet count. Erythrocyte sedimentation rate (ESR) was 104 mm/h withhigh sensitive C-reactive protein (hsCRP) was 8 mg/L. Patient had fasting and postprandial blood glucose of 98 and 116 mg/dL, respectively. Liver, renal function, and coagulation profile were normal with lipid profile study showed total cholesterol of 98 mg/dL, triglyceride of 123 mg/dL, and low density lipoprotein (LDL) of 45 mg/dL. Antinuclear antibody (ANA), perinuclear antineutrophil cytoplasmic antibody (p-ANCA), cytoplasmic antineutrophil cytoplasmic antibody (c-ANCA), anti-β2 GP1antibody, anticardiolipin antibody, lupus anticoagulant, hepatitis B surface antigen, hepatitis C virus, and human immunodeficiency virus (HIV) status were negative. Cardiac evaluation with electrocardiogram and two-dimesnional (2D) echocardiography was absolutely normal. Carotid Doppler study showed narrowing of lumen of bilateral internal carotid artery with normal carotid intima-media thickness (CIMT) without any evidence of plaque.
Invasive peripheral conventional angiography revealed stenosis in the left subclavian artery proximal to the origin of the vertebral artery and right common carotid artery [Figure 2c–e]. According to angiographic classification, patient had type I TA. Bilateral renal, common iliac artery showed normal pattern [Figure 2a and b].
Figure 2.
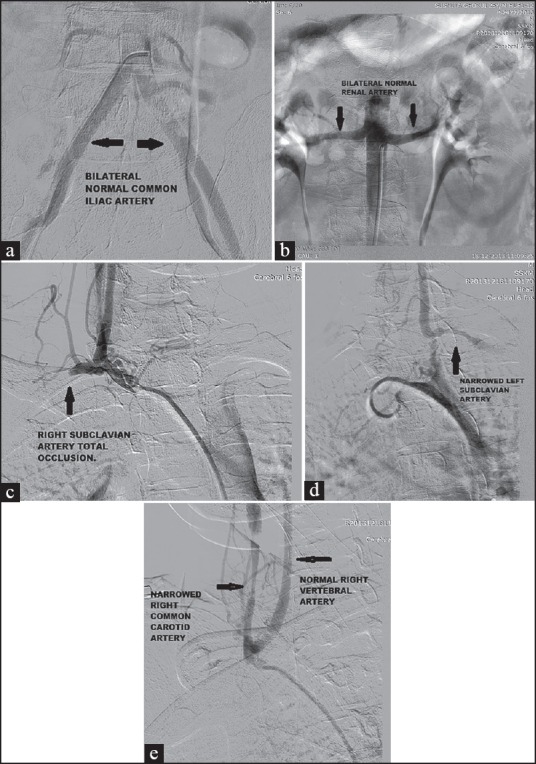
(a) Digital subtraction peripheral angiography showing normal bilateral common iliac artery. (b) Digital subtraction peripheral angiography showing normal bilateral renal artery. (c) Digital subtraction peripheral angiography showing total occlusion of right subclavian artery.(d) Digital subtraction peripheral angiography showing narrowing of left subclavian artery. (e) Digital subtraction peripheral angiography showing narrowing of right common carotid artery and normal vertebral artery
Patient was put on prednisolone 1mg/kg body weight and wound debridement done under surgical department. Patient discharged thereafter, and put on follow-up in outpatient door. Patient showed dramatic improvement in symptoms in late visit.
Discussion
The common causes of digital gangrene are atherosclerosis; connective tissue diseases like systemic lupus erythematosus and scleroderma; antiphospholipid antibody syndrome; small to medium vessel vasculitis like polyarteritis nodosa (28-58%), microscopic angitis (15-20%), granulomatosis with polyangitis (30-40%), and Buerger's disease.[5,6] Dislodgement of vegetations in case of infective endocarditis and mural thrombus during episodes of atrial fibrillation or otherarrhythmiasare also responsible.[7]
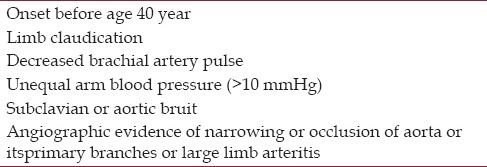
For diagnosis of TA, a criterion was formed by American College of Rheumatology [Table 1]. The diagnosis is made when three out of six points are present. The sensitivity and specificity for diagnosis TA are 91 and 98%, respectively.[8] Our patient met all points of the criteria.
Table 1.
American College of Rheumatology criteria for diagnosing Takayasu's arteritis
The patient had gangrene involving digits of the left hand. Digital gangrene in a patient of TA is very rare manifestation. Till now, few cases of digital gangrene involving lower limbs and only one case of digital gangrene involving hand were reported worldwide in TA.[4]
Patient is nonsmoker and nondiabetic. There was no history of Raynaud's phenomenon, rash, arthritis, oral ulceration, and hemoptysis. There was no evidence of sepsis. Serum ANA, p-ANCA, and c-ANCA were negative. Lipid profile and CIMT were normal. Prothrombin time and partial thromboplastin time were normal. Antiphospholipids antibody syndrome was excluded as anticardiolipin antibody, lupus anticoagulant, and beta-2 glycoprotein-I antibody assay were negative. Echocardiography did not show any vegetation or left atrial clot.
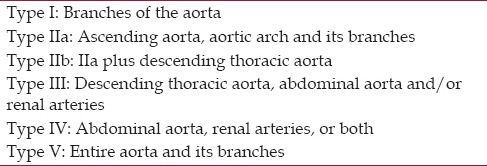
The diagnosis was confirmed by angiography. It could notdifferentiate between active and inactive lesion. There are six types according to angiographic classification [Table 2].[9] Our patient had type I TA.
Table 2.
Angiographic classification of Takayasu's arteritis
Digital gangrene in upper limb is very uncommon as there is abundance of collaterals and rarity of atherosclerosis. So, this patient who was suffering from TA with digital gangrene is a very rare manifestation. One should always consider TA as a differential diagnosis of digital gangrene.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takyasu arteritis. Ann Intern Med. 1994;120:919–29. doi: 10.7326/0003-4819-120-11-199406010-00004. [DOI] [PubMed] [Google Scholar]
- 2.Takayasu M. A case of a peculiar change in the central retinal vessels. Acta Soc Ophthalmol Jpn. 1908;12:55. [Google Scholar]
- 3.Park MC, Lee SW, Park YB, Chung NS, Lee SK. Clinical characteristics and outcomes of Takayasu's arteritis: Analysis of 108 patients using standardized criteria for diagnosis, activity assessment, and angiographic classification. Scand J Rheumatol. 2005;34:284–92. doi: 10.1080/03009740510026526. [DOI] [PubMed] [Google Scholar]
- 4.Verma S, Saraf S, Himanshu D, Singh S. Takayasu's arteritis presenting as digital gangrene of right hand. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2012-007854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dieter RS, Dieter RA Jr, Dieter RA III, editors. 1st ed. New York: McGraw-Hill Professional; 2009. Peripheral arterial disease; pp. 197–233. [Google Scholar]
- 6.Balls GV, Bridges SL. 2nd ed. Oxford: Oxford University Press; 2008. Vasculitis; pp. 439–61. [Google Scholar]
- 7.Abbott WM, Maloney RD, McCabe CC, Lee CE, Wirthlin LS. Arterial embolism: A 44 year perspective. Am J Surg. 1982;143:460–4. doi: 10.1016/0002-9610(82)90196-9. [DOI] [PubMed] [Google Scholar]
- 8.Imboden JB, Hellmann DB, Stone JH, editors. Current Rheumatology Diagnosis and Treatment. New York: Large Medical Books/McGrow Hill; American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 33:1129. From Hellmann DB: Takayasu arteritis. [Google Scholar]
- 9.Hata A, Noda M, Moriwaki R, Numano F. Angiographic findings of Takayasu's arteritis: New classification. Int J Cardiol. 1996;54:S155–63. doi: 10.1016/s0167-5273(96)02813-6. [DOI] [PubMed] [Google Scholar]


