Abstract
Chronic obstructive pulmonary disease (COPD) is a lifestyle-related chronic inflammatory pulmonary disease associated with significant morbidity and mortality worldwide. COPD is associated with various comorbidities found in all stages of COPD. The comorbidities have significant impact in terms of morbidity, mortality, and economic burden in COPD. Management of comorbidities should be incorporated into the comprehensive management of COPD as this will also have an effect on the outcome in COPD patients. Various comorbidities reported in COPD include cardiovascular disease, skeletal muscle dysfunction, anemia, metabolic syndrome, and osteoporosis. Osteoporosis is a significant comorbidity in COPD patients. Various risk factors, such as tobacco smoking, systemic inflammation, vitamin D deficiency, and the use of oral or inhaled corticosteroids (ICSs) are responsible for its occurrence in patients with COPD. This review will focus on the prevalence, pathogenesis, risk factors, diagnosis, and treatment of osteoporosis in COPD patients.
Keywords: COPD, osteoporosis, RANK, osteoprotegerin
Introduction
Chronic obstructive pulmonary disease (COPD) is a lifestyle-related chronic inflammatory pulmonary disease and a major cause of morbidity and mortality globally. The projection is that by the year 2020, COPD would become the third leading cause of death globally.1 The Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014 update defined COPD as a “common preventable and treatable disease, characterized by persistent airflow limitation that is progressive and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases. Exacerbations and comorbidities contribute to the overall severity in individual patients.”2 The importance of comorbidities has been reflected in the recent GOLD guideline. Comprehensive management of COPD should include routinely the assessment for comorbidities as comorbidities are associated with an increase risk of hospitalization, mortality, and worsening health status.3–6 Various comorbidities reported in COPD patients include cardiovascular disease, lung cancer, osteoporosis, diabetes, anxiety/depression, and obstructive sleep apnea.7 Osteoporosis is the most common metabolic bone disorder worldwide and is a significant comorbidity in COPD patients.8,9 The World Health Organization (WHO) defined osteoporosis as “a disease characterized by low bone mass and micro-architectural deterioration of bone tissue, leading to enhanced bone fragility and a consequent increase in fracture risk.”10 The strength of the bone depends on bone mineral density (BMD) and bone quality. The BMD is measured by the dual-energy X-ray absorptiometry (DEXA) scan, whereas the bone quality is measured by the microarchitecture analysis, markers of bone turnover, accumulation of microfractures, and mineralization.11 Various risk factors explaining the prevalence of osteoporosis in COPD patients include aging, smoking, physical inactivity, systemic inflammation, malnutrition, low body-mass index (BMI), hypogonadism, vitamin D deficiency, and the frequent use of corticosteroids.12 Patients with other chronic lung disease also show increased prevalence of osteoporosis. In patients with advanced pulmonary diseases (COPD, cystic fibrosis, idiopathic pulmonary fibrosis, and other lung diseases) awaiting lung transplantation, a high prevalence of osteoporosis and osteopenia has been reported.13
Impact of Osteoporosis on COPD Patients
Osteoporosis is a silent disease unless it is complicated by fractures. Patients with osteoporosis are at an increased risk of fracture, particularly fragility fractures. Fragility fractures are caused by injury that would be insufficient to break a normal bone.14 The impact of osteoporosis- and osteoporosis-induced fractures in COPD patients is enormous.
The most common type of osteoporosis-induced fracture is the vertebral compression fractures (VCFs).15 VCFs are associated with back pain and kyphosis. Kyphosis can cause loss of height, resulting in impaired lung function.16 Every single VCF decreases the vital capacity by 9%, and the lung function impairment is most notable when kyphotic angle is more than 55°.17 The impact of reduced lung function would be more pronounced in COPD patients with already poor lung reserve.18 Patients with rib fractures may develop exacerbations of COPD because of chest pain-induced hypoventilation and decreased ability to expectorate.13 Moreover, osteoporotic fractures in COPD may further decrease the mobility of the patients, thereby, predisposing them to the risk of deep venous thrombosis (DVT) and pulmonary embolism. Therefore, diagnosis and prevention of osteoporosis should be an important goal in the management of patients with COPD. This review will focus on epidemiology, pathogenesis, diagnosis, and management of osteoporosis in patients with COPD.
Low BMD in COPD Patients
The National Health and Nutrition Examination Survey (NHANES), which included 14,828 subjects aged 45 years or older, noted a 16.9% prevalence of osteoporosis in COPD patients compared with 8.5% in subjects without coexisting COPD.19 Graat-Verboom et al.9 in a systematic review of 13 studies involving 775 COPD patients reported an overall prevalence of osteoporosis of 35.1% (range 9–69%) and osteopenia of 38.4% (range 27–67%). There were more male patients (67% vs. 33%). Predictors of osteoporosis or a low BMD in COPD patients include low BMI, low fat-free mass index (FFMI), severity of COPD, and treatment with corticosteroids.9 In a cross-sectional study, Silva et al.20 evaluated the BMD of clinically stable COPD patients by DEXA scan and reported osteoporosis and osteopenia each in 42% of patients. There was a significant correlation between BMD and BMI, level of physical activity, and BODE index (Body-mass index, airflow Obstruction, Dyspnea, and Exercise). They also reported significantly impaired pulmonary function tests in patients with low BMD than in patients with normal BMD. However, no correlation was found between BMD and sun exposure, corticosteroid treatment, or smoking. There are very few studies related to the prevalence of osteoporosis in COPD patients in India. Hattiholi and Gaude21 measured the BMD in COPD patients by DEXA scan. They reported osteoporosis in 68 patients (66.6%) and osteopenia in 20 patients (19.6%). Independent predictors of low BMD in COPD patients are severity of COPD, number of exacerbations, and steroid cumulative dose of >1,000 mg. Bhattacharyya et al.22 studied BMD by ultrasound bone densitometer in a small number of advanced COPD patients and reported osteopenia/osteoporosis in 27 (73%) patients. There was male predominance in both the studies. There were certain limitations of Bhattacharyya et al study. First, they included only advanced COPD patients. Second, BMD was measured by ultrasound bone densitometer and not by DEXA scan. Lastly; a single heel measurement was used in their study. The multicentric TORCH (TOwards a Revolution in COPD Health) study, which included 658 COPD patients, had reported osteoporosis in 23% and osteopenia in 43% patients at the hip or the lumbar spine on DEXA scan.23
Osteoporosis tends to progress in COPD patients also. In a three-year follow-up study, osteoporosis prevalence increased from 47% to 61% in stable COPD patients. Clinically, stable patients of COPD, defined as not treated for an acute COPD exacerbation in the previous six months, were included in the study. The increased prevalence is mainly because of vertebral fractures. The predictors of progression of osteoporosis are lower baseline T-score at the trochanter level and vitamin D deficiency.24 Osteoporosis is an undertreated entity in COPD patients as 82% of osteoporotic COPD patients were not prescribed any specific treatment in a study.25
Vertebral Fractures in COPD
The most common locations of VCFs are the thoracic-lumbar junction (T12–L1) and mid-thoracic area (T7–T8).26 Presence of VCFs is a strong risk for the development of future vertebral fractures. About 60–70% of VCFs are asymptomatic and are not diagnosed, allowing the relentless progression of underlying osteoporosis.27 Furthermore, the kyphotic deformity causes paraspinal muscle contraction to maintain posture that increases the load across the vertebral bodies and explains the subsequent VCFs development.28 Patients with osteoporosis-related VCFs are associated with a 2.8-fold increased risk of hip fracture and a 5-fold increased risk of subsequent vertebral fracture within three years.29,30 VCFs, in general, increase the rate and duration of hospitalization and worsen the health-related quality of life.15,31
Since most cases of VCFs remain asymptomatic, underdiagnosis of VCFs is a common occurrence, and the IMPACT study reported the phenomenon of underdiagnosis as a global problem with the frequency being 34%.32 This leads to the undertreatment of osteoporosis, resulting in its progression. VCFs are common in patients with COPD, with a prevalence ranging from 49% to 63% depending on systemic glucocorticoid therapy.33
Chest radiographs are an important tool in the diagnosis of VCFs, as they can visualize the mid-thoracic (T7–T8) spine and the thoracic-lumbar junction (T12–L1) adequately and can potentially identify about 80–90% of VCFs.34 A common aspect in the management of acute exacerbation of COPD (AE-COPD) is to recommend a chest radiograph, so it can be a valuable tool in the diagnosis of vertebral fractures also.
Majumdar et al.16 prospectively studied the prevalence of VCFs in COPD patients with acute exacerbation, and reported a prevalence of 9% of VCFs diagnosed by posteroanterior and lateral chest radiographs. Patients with VCFs were generally older, sicker, had more severe and longer duration of COPD, and had a low BMI. However, after adjustment for age, sex, and duration of COPD, the only independent correlation was BMI. Nuti et al.18 detected vertebral fractures by lateral chest radiograph in 40% of 2,981 COPD patients. The risk of vertebral fractures is related to COPD severity and glucocorticoid treatment, both inhaled and oral. Additional risk factor is low values of quantitative ultrasound (QUS) at calcaneus. Long-term corticosteroid administration is, therefore, a major risk factor for osteoporosis.
Hip Fractures
Hip fractures are the most serious among osteoporosis-induced fractures because of their high morbidity and mortality. Mortality related to surgery itself is 4%,35 and the one-year mortality rate varies from 14% to 36%.36,37 Other consequences of hip fractures are loss of independence, increased health care utilization, depression, cognitive impairment, high cost, and increased risk of future fracture.38 The exact prevalence of hip fractures in patients with COPD is not known, but the presence of COPD in patients with hip fractures carries a poor prognosis. de Luise et al.39 in the Danish cohort study reported a 60–70% higher risk of death following hip fracture in patients with COPD than those without COPD. The risk of death attributable to COPD remained elevated even at the end of one year, and it was 14%. Also Regan et al.40 showed poor outcome in COPD patients who had hip fractures. COPD was diagnosed in 47% of the 12,646 patients with hip fracture. The mortality rate increased in severe COPD. Severe COPD patients had one-year mortality of 40.2% compared to 31.0% in mild COPD and 28.8% in non-COPD patients. Modifiable risk factors identified in adjusted models are current smokers, use of general anesthesia, and delays to surgery. In a retrospective cohort study, risk of hip fractures was evaluated in patients receiving oral corticosteroids in the United Kingdom general practice. The most common reason for oral corticosteroid use was respiratory disease (40%). The relative risk of hip fracture and vertebral fracture was 1.61 and 2.60, respectively. A dose-dependence relationship was reported. The relative risk of hip fracture was 1.77 in patients receiving a relatively low daily dose of prednisone (2.5–7.5 mg/day), and it was increased to 2.27-fold for those patients receiving prednisone dose of ≥7.5 mg/day.41
Skeletal Microstructural Abnormalities
Microarchitectural distortion also occurs in osteoporosis, but very few studies had focused on demonstration of the micro-architectural abnormalities of bone tissue. It is important to know the bone architecture first for better understanding of microarchitectural changes. There are two major kinds of bone, trabecular (spongy) and cortical. Trabecular bone gives supporting strength to the ends of the weight-bearing bone and is the major site of bone remodeling, whereas the cortical bone forms the shafts of the long bone.42,43 Osteoporosis affects both the trabecular and cortical bones. Osteoporosis decreases the number and size of trabecular bone. The trabeculae also become thinner and rodlike, replacing the stronger platelike shape.44 It also causes loss of the cortical bone. Kulak et al.45 evaluated the bone microstructure and remodeling in postmenopausal woman with COPD. Kulak et al.45 performed microcomputed tomography (μCT) and bone histomorpho metry analysis of the transiliac bone biopsy sample in postmenopausal women with COPD. They demonstrated significant lower mean cancellous bone volume, trabecular number, and trabecular thickness in patients with COPD compared to controls. Trabecular separation and cortical porosity were significantly higher in COPD patients compared to control. Patients with GOLD stages III and IV showed a lower bone formation rate than those with GOLD stages I and II. These microarchitectural changes are responsible for reduced bone strength and increased risk of fractures. The evaluation of bone microstructure is important as COPD patients with a normal BMD can have vertebral fractures.46
Pathogenesis of Osteoporosis in COPD
Bone is a dynamic tissue and in a continuous process of wear and tear. Modeling and remodeling has an important role to play in maintaining a healthy skeleton. Remodeling is the physiological process of new bone formation by the osteoblasts preceded by the osteoclasts-mediated bone resorption.47 Bone modeling, on the other hand, is characterized by the process of bone formation but not preceded by prior bone resorption. It is estimated that about 25% of trabecular bone and about 3% of cortical bone are replaced in adults every year.12 Parathyroid hormone (PTH), vitamin D, and gonadal hormones are the key regulators of bone formation and resorption. Osteoporosis develops because of an imbalance between bone formation and bone resorption, either excessive resorption or decreased formation. Osteoblasts, osteoclasts, and osteocytes interactions are important for the process of bone remodeling. Osteoclasts are multinucleate giant cells derived from blood monocytes/macrophage lineage. Osteoclastogenesis is stimulated by the monocytes/macrophage colony-stimulating factor (M-CSF) and the receptor activator of nuclear factor-κB (RANK)-ligand (RANKL).48 Osteoclasts function as bone eaters by secreting a mixture of hydrogen and chloride ions and proteolytic enzymes. By secreting hydrogen ions, they make an acidic microenvironment, which is necessary for the activation of proteolytic enzymes that subsequently dissolve the bone collagen. Bone resorption helps in the clearance of microdamaged bone tissue and makes the foundation for the laying of new bones (Fig. 1).
Figure 1.

Pathogenesis of osteoporosis in COPD.
Osteoblasts are derived from the mesenchymal stem cells (MSCs) and form new bones.49 Osteocytes are the cells that initiate bone remodeling as these cells detect microdamages within the bone. Osteocytes after detecting the microdamages communicate with the osteoblasts and osteoclasts, which in turn initiate bone remodeling.50
Osteoprotegerin (OPG)/RANK/RANKL Axis
OPG, RANK, and RANKL systems, also known as the OPG/RANK/RANKL axis, play a critical role in the pathogenesis of osteoporosis. RANKL expressed on the surface of osteoblasts, bone stromal cells, and activated T cells plays a key role in the process of bone resorption.51 RANKL binds specifically to the receptor, RANK, is expressed in osteoclast progenitors/mature osteoclasts. The RANKL–RANK interaction results in the activation of osteoclastogenesis by promoting maturation of osteoclast progenitors into mature osteoclasts. It also inhibits apoptosis of osteoclasts.52,53 RANKL is therefore linked to the resorption of bones. OPG, an anti-inflammatory protein, derived from the osteoblasts and bone stromal cells inhibits osteoclastogenesis. It acts as a soluble decoy receptor specific for RANKL.54 Binding of OPG with RANKL inhibits the RANKL–RANK interaction on the osteoclast cell membranes, thereby inhibiting osteoclastogenesis and subsequent bone loss. Impairment of the fine balance between RANKL and OPG is responsible for the development of osteoporosis – either through an increase in RANKL or a decrease in OPG (Fig. 2).
Figure 2.

Relationship between RANK, RANKL, and OPG.
Bucay et al.55 studied the role of OPG deficiency in OPG-knockout mice generated by the targeted deletion of the OPG gene. They demonstrated development of an osteoporotic skeletal phenotype, including a high bone-remodeling rate, decreased BMD, and increased incidence of fragility fractures and bone deformities in OPG-knockout mice. These effects stem from the unopposed RANKL activity because of the absence of a decoy receptor. OPG-knockout mice are the first animal model for studying osteoporosis. Therefore, OPG is an important negative regulator of osteoclastogenesis. Another molecule that stimulates osteoclastogenesis is M-CSF. M-CSF increases the number of osteoclast progenitors, and RANKL then binds to its receptor RANK expressed on the surface of osteoclast progenitors.56 Various hormones, growth factors, and cytokines regulate the OPG/RANK/RANKL axis.57 Proresorptive cytokines are IL-1, IL-7, IL-17, and tumor necrosis factor-alpha (TNF-α) as they upregulate RANKL, whereas IL-4, IL-13, and interferon-γ are antiresorptive cytokines as they suppress osteoclastogenesis.57,58
COPD and OPG/RANK/RANKL Axis
Bai et al.59 studied the level of inflammatory cytokines and OPG/RANK/RANKL protein levels in 80 stable male COPD patients. They found a significant correlation between radiographic emphysema measured by low-attenuation area (LAA%) and low BMD in COPD patients who are current or former smokers. Compared to COPD patients with normal BMD, patients with low BMD had significantly higher levels of RANKL and a higher RANKL/OPG ratio. The serum levels of IL-6 and TNF-α were also found to be significantly higher in the COPD patients with low BMD, but the level of IL-1β, although higher in the low BMD group than in the normal BMD group, did not reach statistical significance. Cytokines such as IL-6, TNF-α, and IL-1β are secreted by bone stromal cells and monocytes and increase the production of both RANKL and OPG, but their dominant effect is on the RANKL. Eagan et al.60 also noted significantly lower levels of OPG in COPD patients compared to the control. The characteristics of COPD is the development of systemic inflammation with resulting rise in the serum levels of inflammatory cytokines eg, IL-6, TNF-α, and IL-1β.61,62 These cytokines tilt the balance of the OPG/RANK/RANKL axis toward RANKL, which results in the development of osteoporosis in COPD patients. Interestingly, the elevated RANKL can also upregulate the expression of IL-6 and TNF-α, which may augment inflammatory milieu of COPD patients.63
Wnt/β-catenin Signaling System
Another signaling pathway of importance in osteoporosis is Wnt/β-catenin signaling system. Wnt/β-catenin signaling system is one of the main mechanisms controlling osteoblastogenesis.64 First, Wnt/β-catenin pathway promotes osteoblastogenesis by stimulating differentiation of pluripotent MSCs toward the osteoblast lineage and decreasing differentiation of MSCs toward adipogenic lineage.65 Second, Wnt signaling promotes osteoblast survival by inhibiting its apoptosis.66 Wnt/β-catenin signaling system also inhibits the osteoclastogenesis process by stimulating production and secretion of OPG.67 Therefore, activation of Wnt/β-catenin signaling promotes bone formation, whereas inhibition of Wnt signaling promotes bone resorption and contributes to osteoporosis.68
Kneidinger et al analyzed the Wnt/β-catenin signals in the lung tissues obtained from COPD patients undergoing lung transplantation and reported decreased activity of Wnt/β-catenin signals in COPD patients. The impaired activity of Wnt/β-catenin signals may explain the occurrence of both emphysema and osteoporosis.69
Role of Matrix Metalloproteinases (MMPs)
MMPs are a large family of calcium-activated endopeptidases responsible for the degradation of extracellular connective tissue matrix.70 Regulation of MMP activity is important to prevent untoward consequences, and tissue inhibitors of metalloproteinases (TIMPs) play an important role in regulating the local activities of MMPs in tissues.71 Balance between MMPs and TIMPs is essential in order to maintain homeostasis in the body, and tilting the balance in favor of MMPs results in the development of various disease processes.
MMPs are produced by osteoclasts and osteoclast progenitors, as well as by monocytes/macrophages. MMPs stimulate osteoclastic bone resorption and promote osteoporosis. In contrast, TIMPs prevent bone loss.72 Bolton et al.73 measured MMP level in 70 clinically stable COPD patients and reported increased circulating levels of MMP-9 in patients with COPD compared with the healthy controls. The rise in MMPs was not associated with a similar change in circulating TIMP-1 and -2 levels. Among COPD patients with reduced BMD, the MMP-9 rise was greater in those with osteoporosis than in those with osteopenia, COPD patients with no bone disease, and control subjects. An increase in MMP level is therefore a marker of osteoporosis. Zhang et al.74 studied MMP-9, TNF-α, and OPG/RANK/RANKL systems in 90 male patients with clinically stable COPD and reported higher MMP-9 level in patients with osteoporosis than in patients with normal BMD. As in the work of Bolton et al.73, no difference in TIMP-1 serum level was detected among the three groups. An increase in MMP level may therefore explain the occurrence of osteoporosis in patients with COPD and may also explain the correlation between radiological emphysema and osteoporosis.
Risk Factors for Osteoporosis in COPD
Vitamin D deficiency
Vitamin D along with PTHs plays a key role in regulating calcium and bone homeostasis. First, the 25(OH)D3 is the form measured in the blood as the half-life of 25(OH)D3 is 10.4 days,75 whereas the 1,25(OH)2D3 is not measured as the circulating half-life is only 4 hours. Second, serum 1,25(OH)2D3 level can be normal or even elevated despite the presence of vitamin D deficiency. Low 25(OH)D3 level increases PTH secretion, which augments the conversion of 25(OH)D3 to 1,25(OH)2D3.76 The Endocrine Society’s clinical guidelines defined vitamin D deficiency as a 25(OH)D3 level below 20 ng/mL (50 nmol/L) and vitamin D insufficiency as a 25(OH)D3 level between 21 and 29 ng/mL (52.5–72.5 nmol/L).77
Studies of vitamin D deficiency in COPD
Vitamin D deficiency is common in COPD patients. Førli et al.78 quantified vitamin D level in 71 patients with advanced respiratory diseases waiting for lung transplantation, and 46 of them had COPD. The majority of this cohort (both normal weight and underweight patients) suffered from vitamin D deficiency (25(OH) D3 <20 ng/mL). Vitamin D deficiency was associated with reduced femoral neck T-scores in underweight patients. Romme et al.79 similarly reported vitamin D deficiency in 58% of 151 patients with moderate-to-very severe COPD entering the pulmonary rehabilitation program. They reported positive correlation between plasma vitamin D level and BMD. The prevalence of vitamin D deficiency was also related to severity of COPD as deficiency increased significantly from GOLD stage II to stage IV. Vitamin D deficiency was 43% in GOLD stage II patients, 50% in GOLD stage III patients, and 76% in GOLD stage IV patients.79 However, both of the aforementioned studies did not have control. Janssens et al.80 analyzed the 25(OH)D3 levels and the variants of vitamin D binding gene in patients with COPD. The prevalence of vitamin D deficiency was 31% in healthy smokers, 39% in GOLD grade I patients, 47% in GOLD grade II patients, 60% in GOLD grade III patients, and 77% in GOLD grade IV patients. Therefore, a high prevalence of vitamin D deficiency was demonstrated in patients with COPD compared to age-, sex-, and smoking-matched controls. They also reported higher risk of COPD in homozygous carriers of the rs7041 T allele of vitamin D-binding gene. This study suggests a strong relationship between GOLD stages of COPD and vitamin D deficiency.
Various factors that have been implicated for the deficiency of vitamin D in COPD patients include poor diet, less exposure to sunlight because of decreased physical activity, accelerated skin ageing, renal dysfunction, depression, and treatment with corticosteroids. Depression may be associated with lower levels of vitamin D because of several reasons. Depressed patients perform less physical activity and spend more time indoors than outdoors.81 Smoking decreases vitamin D level by accelerating skin aging, thereby, decreases the skin production of vitamin D. Smoking can also decrease circulating levels of 25(OH)D3 and 1,25(OH)2D3 by 10% and PTH level by 20%. It decreases serum PTH levels either by decrease in secretion or an increased smoking-augmented hepatic metabolism.82
Mechanisms of osteoporosis development in Vitamin D deficiency
Vitamin D deficiency is characterized by low serum 25(OH)D level that results in reduced serum calcium level and compensatory increase in serum PTH level.83 PTH enhances the production of calcitriol by stimulating 1-α-hydroxylase enzyme in the proximal convoluted tubules.84 Calcitriol increases intestinal calcium and phosphate absorption. Calcitriol increases the expression of RANKL on the surface of osteoblasts leading to augmented RANK/RANKL interaction. RANK/RANKL interaction causes bone resorption and subsequent decrease in BMD. Bone resorption leads to increase in serum calcium level. However, there is a check on this system. Increased serum calcium level decreases PTH secretion. Calcitriol also checks bone resorption by increasing the OPG expression in mature osteoblasts.85 However, this inhibition of bone resorption is less active in cancellous bone, effectively making this region susceptible for resorption. Vitamin D deficiency, therefore, increases the susceptibility to osteoporotic fractures because of low BMD. It also increases the fracture risk by causing swaying of the body and falls because of muscle weakness.86
Corticosteroids use
Oral and inhaled corticosteroids (ICSs) are frequently prescribed in COPD patients. ICSs are used in moderate-to-severe COPD, reducing the frequency of exacerbation and improving quality of life.87 Oral steroids are used on hospitalized patients with exacerbation of COPD, and they cause shortening of the hospitalization period and early improvement of lung functions. Glucocorticoid use is the most common cause of iatrogenic and secondary osteoporosis. In a meta-analysis of seven cohort studies of 42,000 subjects, current and prior use of glucorticosteroids (GCSs) was found to be a predictor of the increased risk of fractures, independent of previous history of fractures and BMD.88 The greatest risk of fractures is noted during the first three to six months after beginning of steroids therapy, and the risk persists for one year after the cessation of corticosteroid use, indicating reversibility of the process.89 A meta-analysis of randomized controlled trials (16 trials) and observational studies (7 trials) revealed that in patients with COPD, ICS use was associated with a modest but statistically significant increase (>20%) in the risk of fractures.90 Similarly, in a nested case–control study, including 1708 COPD patients with non-vertebral fractures and 6817 matched control subjects, current use of high-dose ICS (more than 700 μg/day) was associated with an increased risk of non-vertebral fractures compared with patients with no ICS exposure (adjusted odds ratio = 1.68; 95% confidence interval, 1.10–2.57).91 The impact of ICS on BMD is dose dependent. In a randomized controlled trial, Mathioudakis et al.92 had shown that long-term use of low-dose ICS protects the COPD patients from developing osteoporosis. This is secondary to the decrease in lungs inflammation, which further decreases the systemic spillover. However, at higher doses, ICS may gain access to the systemic circulation and can produce systemic side effects.93 The impact of other drugs, for example, antileukotrienes and phosphodiesterase-4 inhibitors, on the systemic inflammation and BMD requires investigation in future.
Mechanisms of corticosteroids-induced osteoporosis
There are some unique characteristics of GCSs-induced fractures. First, fractures because of GCSs occur even with normal BMD, unlike fractures occurring in patients with postmenopausal osteoporosis.94 Second, with long-term GCSs therapy, the number of osteoclasts is usually maintained in the normal range, whereas the number of osteoblasts falls and bone formation is substantially reduced. This is in contrast to postmenopausal osteoporosis or hyperparathyroidism; both of them are characterized by increased bone formation and resorption.95 Third, loss of bone strength occurs even before the loss of BMD.96 GCSs-induced osteoporosis occurs in two phases; a rapid phase of bone loss via osteoclasts mediated bone resorption, followed by the later phase of bone loss caused by decreased bone formation.97 GCSs exert their effects on both osteoblasts and osteoclasts in osteoporosis, but the most important effect is inhibition of osteoblasts functions.98 GCSs impair osteoblast recruitment and activity, and promote apoptosis of osteoblasts and osteocytes.99 They affect both the trabecular and cortical bone formation, but the trabecular bone is initially more affected than the cortical bone.100
GCSs inhibit osteoblast differentiation and function at pharmacological doses by inhibiting Wnt/β-catenin and bone morphogenetic protein 2 (BMP-2) signaling system necessary for osteoblastogenesis. Decreased osteoblastogenesis diverts the MSCs toward the adipocyte lineages.99 In cultured cell lines, steroids increased the expression of Dickkopf-1 (Dkk-1), an antagonist of Wnt signaling system. Increased level of Dkk-1 inhibits the Wnt signal in osteoblasts, which may explain the mechanisms of glucocorticoid-induced osteoporosis.101
Apoptosis of osteocytes is also a significant event as it is responsible for the hardening of bones and consequent increased fracture risk compared with soft bones. Osteocytes also perform an important function of repairing microdamage that is also jeopardized by GCSs. Osteocytes via hypoxia-inducible factor-α (HIF-α) enhance VEGF level, and therefore, promote angiogenesis within the skeleton.102 GCSs decrease angiogenesis by promoting apoptosis of osteocytes, therefore decreasing the level of VEGF.103 Decreased level of VEGF reduces bone hydration, resulting in reduced strength of the bone. GCSs are also osteoclastogenic as they increase the expression of M-CSF, IL-6, and RANKL and decrease the expression of OPG in stromal and osteoblastic cells.104–106 They also inhibit apoptosis of osteoclasts.107
In addition, there are some indirect effects also. GCSs reduce intestinal calcium absorption and enhance renal calcium loss. High-dose GCSs can cause hypogonadism in men and premenopausal women by suppressing testosterone and/or estrogen levels, which can result in further bone loss. Steroid-induced proximal myopathy results in muscle weakness and higher frequency of falls and fractures.108
Risk factors for GCS-induced osteoporosis include advanced age, glucocorticoid receptor genotype, female sex, increased expression of 11β-hydroxysteroid dehydrogenase (11β-HSD1), low bodyweight (body-mass index <24 kg/m2), low BMD, and cumulative steroid dose. Cumulative dose depends on both high dose and duration of treatment of greater than three months. Even alternate day therapy is not safe.109
Different steroids have variable effects on the bone. Deflazacort causes less bone loss compared to other steroids. Prednisone and deflazacort produced a rate of bone loss of −3.0%/year and −1.1%/year, respectively.110 This variable effect can be explained by the variable effects of steroids on the OPG/RANK/RANKL axis. Deflazacort was a poor stimulator of RANKL gene expression, unlike prednisolone. Deflazacort stimulates the RANKL gene by one-to-three-fold compared to seven-fold by prednisolone. Therefore, deflazacort has less potential to cause bone loss than prednisolone.111
Low body-mass index/low fat-free mass (FFM)/sarcopenia
Low BMI has been recognized as a key risk factor for low BMD and future risk of fragility fracture, whereas a high BMI is protective against osteoporosis.112,113 De Laet et al.114, in a large meta-analysis of 12 prospective population-based cohorts of 60,000 men and women, described an inverse and non-linear relationship between BMI and total fractures, osteoporotic fractures, and hip fractures. There was an increasing fracture risk with BMI <25 kg/m2. For every standard deviation (SD) decrease in BMI, the age-adjusted risk for fractures increased by approximately 18%.115 Low BMI is not uncommon in COPD patients as a large population-based study from China detected BMI of less than 18.5 kg/m2 in 21% patients.116 The risk of low BMI is even higher in advanced COPD.117
Changes in the body composition are important physiological derangements in COPD patients. Our body composition broadly consists of two components: fat mass and FFM. FFM contains the metabolically active organs, and skeletal muscle is the largest of these organs.118 BMI is less sensitive to changes in the body composition as BMI can be normal or even high despite the presence of low FFM.119 Normal FFMI is ≥16 (men) or ≥15 (women).120 Based on BMI and FFMI, Schols et al.120 proposed the following definitions: cachexia (low BMI and depleted FFMI), muscle atrophy (normal BMI and depleted FFMI), semi-starvation (low BMI and normal FFMI), normal (normal BMI and normal FFMI), overweight (overweight BMI and normal FFMI), and obese (obese BMI and normal FFMI). Among outpatients with moderate-to-severe COPD, FFM was depleted in 26% of patients,121 and in patients eligible for pulmonary rehabilitation, the loss was 35%.122 Apart from low FFM, COPD patients are also associated with reduced muscle strength and sarcopenia. The European Working Group on Sarcopenia in Older People (EWGSOP)122 defined sarcopenia by the reduced muscle mass and at least one of either low muscle strength or physical performance. The Korea National Health and Nutrition Examination Survey (KNHANES) detected sarcopenia in 32.8% of male patients and 12.2% of female patients with COPD.123 Several studies have reported significant correlation between sarcopenia and osteoporosis and/or BMD. Coin et al.124 detected a significant higher prevalence of osteoporosis in sarcopenic groups compared with non-sarcopenic groups (46% vs. 0%; P <0.05). Bolton et al similarly reported a very high prevalence of osteoporosis (50%) and osteopenia (50%) in cachectic COPD patients.125 Various factors linking low FFM with osteoporosis include reduced physical activity, vitamin D deficiency, inflammatory mediators, genetic factors, and the use of corticosteroids.126 Systemic inflammation causes loss of both FFM and BMD as inflammation can cause skeletal muscle atrophy and protein breakdown.125 Low mechanical loads on the bones because of low BMI and FFM loss can reduce the bone formation.
The relationship between fat and bone has become an important topic nowadays. Adipose tissue might affect the bone by various mechanisms. Adipose tissue produces several bone-active substances, together called adipokines, which include TNF-α, leptin, adiponectin, and resistin.127 Leptin modulates bone cells either directly or indirectly via the central nervous system. Leptin promotes proliferation and differentiation of osteoblasts via its receptors present on the osteoblasts.128,129 Leptin inhibits the osteoclast function by reducing the production of RANK and RANKL and increasing OPG production.130 Leptin promotes skeletal mass formation via these mechanisms. Leptin deficiency results in reduced bone formation and increased bone resorption. Vondracek et al.131 reported significantly lower body-mass and serum leptin concentrations in men with COPD and osteoporosis compared with men with COPD but without osteoporosis. However, the central action of leptin is opposite to peripheral action. Experimental infusion of leptin into the third ventricle results in bone loss and weight loss.132,133 It causes bone loss via inhibition of bone formation and stimulation of bone resorption. Peripheral effect of leptin normally predominates.134 Pobeha et al.135 specifically studied the relation between expressions of leptin and OPG in the adipose tissue, and development of osteoporosis in patients with COPD. COPD patients with osteoporosis had significantly lower serum levels and adipose tissue expressions of leptin, OPG, in association with increased serum β-crosslaps (marker of bone turnover).
Anemia and osteoporosis
Anemia is a common entity in COPD patients, and its prevalence varies from 7.5% to 34%, depending upon the selected populations and the diagnostic tools to determine the hemoglobin level.136 Several studies reported a connection between anemia and BMD. Cesari et al.137 in the InCHIANTI study conducted among the elderly Italian population documented anemia and low hemoglobin levels negatively and independently associated with bone mass and density. Low hemoglobin levels are associated with higher bone loss in the cortical bone in women, independent of systemic inflammation. Similarly, Korkmaz et al.138 demonstrated significantly higher prevalence of anemia in patients with low BMD of the femur and spine. They also documented that the presence of anemia among Turkish postmenopausal women was an independent predictor of low BMD of the spine, after adjusting for BMI and other confounders. Anemia is also associated with higher fracture risk among healthy multiethnic elderly women.139 Rutten et al.140 reported 20% prevalence of anemia among 321 COPD patients admitted for pulmonary rehabilitation, and anemia was also found to be an independent predictor of low BMD. The pathophysiological nexus between anemia and osteoporosis is not clear; however, human and animal experiments suggest the role of anemia-associated hypoxia as the potential mechanisms for the development of osteoporosis.141
Reduced physical activity
Physical inactivity is an important modifiable risk factor for osteoporosis, and several studies have suggested that exercise can prevent bone loss. Gustavsson et al.142 in a six-year longitudinal study found that their subject, a young ice hockey player, lost BMD of the femoral neck rapidly after decreased physical activity. A systematic review had suggested that exercise can reduce falls, fall-related fractures, and several risk factors for falls in individuals with low BMD.143 Physical activity does this by increasing the BMD. Exercise reduces the age-related decrease in BMD by approximately 1% per year in postmenopausal women.144 The Cochrane database demonstrated that aerobics, weight- bearing, and resistance exercises are effective for improving the BMD of the spine in postmenopausal women, and walking improves the BMD of the hip.145
Polidoulis et al.146 further analyzed the impact of exercise on bone structure and strength by peripheral quantitative CT (pQCT) scan analysis and showed that by maintaining cortical and trabecular volumetric BMD, exercise may decrease the bone loss in postmenopausal women. Physical inactivity decreases BMD by reducing osteoblast recruitment and differentiation and inducing its apoptosis.147 It also causes osteoprogenitor cell differentiation toward adipocyte lineages. Osteoblastogenesis is influenced by insulin-like growth factor (IGF), BMPs, PTH, and sclerostin.147 Lin et al demonstrated via animal experimentation that mechanical unloading increased sclerostin level in wild mice and sclerostin inhibits bone formation by inhibiting the Wnt signaling pathway.148 Physical inactivity, therefore, reduces the Wnt signaling pathway. Patients with COPD have significantly reduced levels of physical activity compared with healthy control subjects.149 In transgenic mice experiments, Robinson et al.150 showed that mechanical loading activates the Wnt/β-catenin pathway and enhances the sensitivity of osteoblasts/osteocytes to mechanical loading. This may explain another aspect of development of osteoporosis in COPD patients because of physical inactivity. Therefore, regular physical activity can be an important goal in the prevention of osteoporosis. Improved physical activity also resulted in improved BMD: COPD patients who underwent lung volume reduction surgery showed an improvement in BMD because of an increase in physical activity.151
COPD exacerbations
Exacerbation of COPD can also be a risk factor for reduced BMD. Kiyokawa et al.152 in a longitudinal study measured BMD of thoracic vertebra by CT scan. They noted that COPD exacerbation was independently associated with progression of osteoporosis. Stanojkovic et al.153 provided the mechanistic link between COPD exacerbations and osteoporosis. Exacerbations of COPD are associated with augmentation of inflammation, hypoxia, protease/antiprotease imbalance, and oxidative stress, all of these may contribute to increased bone resorption as evidenced by the elevated type I collagen fragments level, which is a predictor of bone loss. Other factors are use of steroids during exacerbations and physical inactivity. The systemic inflammation is augmented in patients with reduced lung function, and systemic inflammation is a recognized risk factor for osteoporosis, cachexia, and weight loss.154 Osteoporosis progression should be evaluated in COPD patients, especially in those with a history of frequent exacerbations.
Smoking
Smoking is an important risk factor for COPD. Smoking may also cause osteoporosis. A meta-analysis by Ward and Klesges155 demonstrated that tobacco smoking had a cumulative, dose-dependent independent effect on bone mass. Smokers had significantly reduced bone mass compared with nonsmokers at several major sites of osteoporosis-related fractures, including the hip, lumbar spine, and forearm, but the effect is most pronounced at the hip. Overall, the greatest effect was seen in men and elderly. Smoking induces osteoporosis by several potential mechanisms: altered metabolism of calciotropic hormone; dysregulation in the production, metabolism, and binding of estradiol; altered metabolism of adrenal cortical hormone; effects on the RANK–RANKL–OPG system; and effects on collagen metabolism and bone angiogenesis.156
Hypoxia and hypercapnia
Dimai et al.157 evaluated the impact of hypercapnia on the BMD and noted a lower BMD, arterial pH, and a higher serum cross-linked telopeptide of type I collagen (ICTP), a bone resorption marker in COPD patients with hypercapnia than COPD patients with eucapnia. The BMD and serum ICTP level were not different between compensatory respiratory acidosis and uncompensated respiratory acidosis, clearly indicating the role of hypercapnia rather than uncompensated respiratory acidosis as the cause of bone resorption. Carbon dioxide directly stimulates the osteoclasts as, first, they have receptor for CO2158 and second, CO2 stimulates the carbonic anhydrase II within the osteoclasts, leading to activation of osteoclastic-mediated bone resorption.159 Hypoxia has also got a role in the development of osteoporosis. Hypoxia blocks the growth and differentiation of osteoblasts, whereas it strongly stimulates osteoclast-mediated bone resorption.160 Hypoxia inhibits osteoblast formation by reducing the expression of RUNX2, a key transcription factor required for stem cell selection toward osteoblastic lineage and osteoblast differentiation.161
Hypogonadism
Sex steroids play a crucial role in maintaining skeletal integrity via stimulating bone formation and inhibiting bone resorption.162 The reported prevalence of hypogonadism in men with COPD varies from 22% to 69% and has been associated with osteoporosis, depression, and muscle weakness.163 Although, hypogonadism is an independent risk factor for the development of osteoporosis both in men and women, the role of testosterone deficiency in osteoporosis development is modest in nature. On the other hand, levels of estradiol are more closely linked to skeletal health than the levels of testosterone even in men.164
Diagnostic Imaging of Osteoporosis
Osteoporosis is a disease that affects the bone mass and bone microarchitecture. Bone mass can be assessed by measuring the BMD, whereas bone microarchitecture can be assessed only by bone biopsy, which is not routinely done in developing countries. Measurement of BMD by DEXA scan is the gold standard for the diagnosis of osteoporosis.165 It is also used to monitor the response to treatment and to measure the body composition.166 BMD is reported as the SD of means, the T- and Z-scores. The T-score is the difference in the number of SDs between the mean BMD value of the patient and the mean BMD of a young sex-matched adult control population. The Z-score is the difference in the number of SDs between the mean BMD value of the patient and the mean BMD of a race-, sex-, and age-matched reference population.166 Reduction of 1 SD in the BMD value increases fracture risk by 1.5- to 3-fold.167 In postmenopausal women and in men aged 50 years and above, T-score is used to stratify patients into one of the following categories: normal, osteopenia (low bone mass), and osteoporosis. Normal DEXA-scan report is shown in Figure 3. The WHO definition is shown in Table 1.168
Figure 3.

Normal DEXA scan of a patient.
Table 1.
WHO definition of osteoporosis and osteopenia.
| Normal | T-score 0 to –0.99 |
| Osteopenia | T-score between –1 to –2.499 |
| Osteoporosis | T-score of ≤–2.5 |
| Severe osteoporosis | T-score of ≤–2.5 along with fracture |
The Z-score is used in premenopausal women, younger men (<50 years), and children. Based on the BMD, patients can be classified as those with normal BMD for age defined as Z-score higher than −2.0 and low BMD for age defined as Z-score of −2.0 or lower.169 Hip and spine are the common sites of osteoporotic fracture, so these are the preferred sites for scan.170 The International Society for Clinical Densitometry advocates BMD measurement of the lumbar spine and the hip and to diagnose osteoporosis based on the lowest T-score of the measured locations.171 Lumbar spine is preferred as it is enriched with high proportion of trabecular bone, allowing for early detection; however, in patients with degenerative changes in the spine, spine BMD measurement has limited use.171 The BMD of the forearm should be measured in very obese patients or in patients where BMD of spine or hip is either not measurable or not interpretable because of severe degenerative disease or extensive surgical instrumentation.172 Although, DEXA scan is an easy-to-use technique coupled with high precision and low-radiation dose (1–6 μSv),173 it has some disadvantages also. DEXA scan is a two-dimensional (2D) measurement, and it only measures density/area (in grams per square centimeter), not the volumetric density; therefore, the measured BMD is called the areal BMD. Areal BMD is susceptible to bone size and will overestimate the fracture risk in individuals with a small body frame, who will have lower areal BMD than normal-sized individuals. Another pitfall of areal BMD is that it is sensitive to degenerative changes of the spine and may report increased BMD and falsely low fracture risk.174 Suitability of DEXA for follow-up study is questionable as it requires ≥2 years to detect statistically significant changes in areal BMD.175 DEXA scan does not detect bone microarchitecture changes. The BMD measurement alone does not reliably predict osteoporotic fractures. WHO had developed a web-based fracture risk algorithm (FRAX), based on use of up to 10 variables, including the current age, gender, low body-mass index (kg/m2), a prior osteoporotic fracture (including morphometric vertebral fracture), parental history of hip fracture, oral glucocorticoids ≥5 mg/day of prednisone for ≥3 months (ever), current smoking, alcohol intake (three or more drinks per day), rheumatoid arthritis, secondary osteoporosis, and femoral neck BMD. FRAX estimates an individual’s 10-year probability of fracture.175 COPD patients are at high risk of developing VCFs, and early recognition of VCFs is important since their presence is an important risk of future fractures. Both the DEXA scan and the vertebral fracture assessment using X-ray should be used together to diagnose osteoporosis in patients with COPD as vertebral fractures can occur in COPD patients with a normal BMD on DEXA-scan result.46
The diagnostic modality of choice for vertebral fractures is the visual semiquantitative assessment method described by Genant et al.176 The reduction in vertebral height and morphologic changes are noted visually. Vertebral deformities are classified morphologically into wedge, biconcave, or crush and are graded as normal (grade 0), grade 1(reduction of 20–25% of height and 10–20% of projected vertebral area), grade 2 (reduction of 26–40% of height and 21–40% of projected vertebral area), and grade 3 (reduction of >40% of height and projected vertebral area). The FRAX algorithm does not reliably predict the development of osteoporotic vertebral fractures in patients presenting with more than moderately severe COPD. Two additional risk factors identified in advanced COPD are low FEV1 and the presence of chronic respiratory failure, indicating the requirement for the development of a COPD-specific FRAX algorithm.177
Measurement of Bone Quality
Recently, various techniques have been developed to assess the bone quality, though most are in use for research purposes. These are quantitative ultrasonography (US), magnetic resonance (MR) imaging and MR spectroscopy, multidetector CT, quantitative CT (QCT) and high-resolution peripheral quantitative CT (HR-pQCT).174
Quantitative CT
Unlike DEXA, which is a 2D method, QCT is 3D imaging modality. It is useful in young children because it measures a volumetric BMD and is not affected by bone size. It measures BMD of both cortical and trabecular area separately. Trabecular bones being more active metabolically are more sensitive to changes.
QCT is generally applied to the lumbar spine on whole-body CT scanners. The standard QCT scans the lumbar vertebrae with a mineral reference phantom in the same field. It measures the attenuation of the lumbar vertebrae in Hounsfield unit (HU) and transforms it into a bone mineral equivalent (mg/cm3) using standardized software.178 High-resolution peripheral QCT (HR-pQCT) is a low-radiation method for assessing bone microarchitecture and volumetric BMD in cortical and trabecular compartments of the distal radius, tibia, and metacarpals. The radiation dose to the patient from a HR-pQCT single-scan is estimated to be 3 μSv.179 HR-pQCT measures structural parameters such as total, cortical, and cancellous BMD; trabecular thickness; trabecular separation; and trabecular number and mechanical parameters such as bone stiffness and failure load.180,181 Disadvantages of HR-pQCT include its limitation to peripheral skeletal sites and providing no direct insight into bone quality in the lumbar spine or proximal femur, common sites for osteoporotic fragility fractures.182
The T-score thresholds defined by the WHO for diagnosis of osteoporosis are not applicable to either peripheral or central QCT scan. In the lumbar spine, a trabecular BMD of 80–120 mg/cm3 is defined as osteopenic and a BMD <80 mg/cm3 as osteoporotic on QCT.183 Romme et al.184 studied the role of routine chest CT in osteoporosis assessment. The authors measured the average attenuation of thoracic vertebrae 4, 7, and 10 on chest CT and compared these measurements with the lowest BMD of the hip and lumbar spine (L1–L4) on DEXA scan in COPD patients. A strong correlation was found between the average attenuation of the three thoracic vertebrae and the lowest BMD of the hip and lumbar spine with an attenuation threshold value of 147 HU. However, more studies are required to establish its role in osteoporosis detection.
Detection of Microstructural Changes
The bone microarchitectural changes can be assessed either by the histomorphometric analysis or the μCT analysis of bone biopsy samples.47 Detection of microarchitectural changes is difficult in routine clinical practice because of its invasiveness. The 3D micro-CT images and morphometric calculations on human trabecular bone (lumbar vertebra) are shown in Figure 4A and B.
Figure 4.
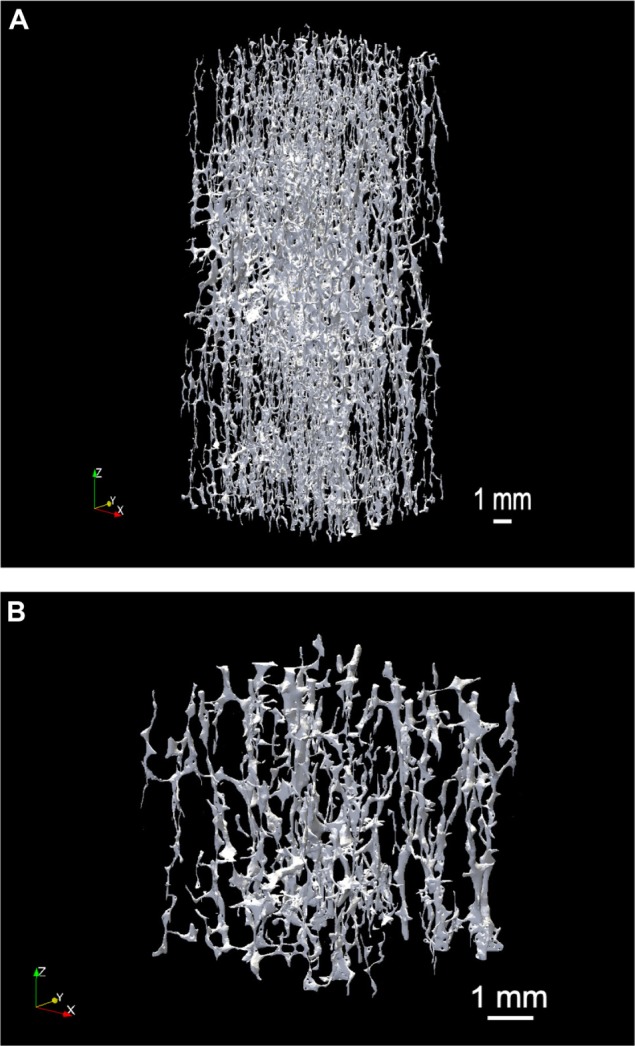
(A) 3D micro-CT image (17 μm/pixel) of human trabecular bone (lumbar vertebra), size of the volume of interest: 10 × 10 × 19 mm. (B) 3D micro-CT image (17 μm/pixel) of human trabecular bone (lumbar vertebra). This bone has very low bone volume fraction, with a mainly rod-like appearance. Image courtesy: Dr Egon Perilli, Flinders University, Adelaide, SA, Australia.
Relationship between CT Quantification of Emphysema and BMD
Few studies evaluated the relationship between radiological extents of emphysema with BMD. Bon et al demonstrated that radiographic emphysema is a strong predictor of low BMD, and it was independent of airflow obstruction and other osteoporotic risk factors.185 The most plausible mechanistic link between the two could be systemic inflammation as the authors revealed a positive correlation between the osteoclastogenic cytokine IL-6 and the percentage of low- attenuation lung units measured by QCT.186 Ohara et al.187 found a significant correlation between CT extent of emphysema and CT measured BMD of the thoracic and lumbar vertebrae (T4, T7, T10, and L1) in 65 male patients with COPD. Multiple regression analysis showed that only LAA% and BMI were predictive of BMD among age, BMI, smoking index, FEV1, arterial blood gas, and LAA%, indicating COPD as an independent risk factor for low BMD.
Prevention and Treatment of Osteoporosis in COPD Patients
The general principal governing the treatment of osteoporosis is preventing fractures, and can be divided into pharmacological and non-pharmacological interventions.
Non-pharmacological management
COPD is a lifestyle-related disease, and several lifestyle-related factors such as smoking, physical inactivity, and poor diet have been linked to osteoporosis development. A systematic review by Howe et al.188 revealed that exercise had a relatively small, but, statistically significant positive effect on BMD in postmenopausal females. Cigarette smoking is a reversible risk factor for osteoporosis, and smoking cessation results in the improvement in BMD.152 Active smoking cessation should be instituted at the earliest. Patients should be counseled on fall prevention. Weight-bearing and strengthening exercise should be encouraged. Overuse of ICS in COPD must be avoided. ICS use should be restricted to COPD patients with forced expiratory volume (FEV1) <50% of predicted. Unnecessary prolonged use of oral steroids during COPD exacerbations should be avoided.
Leuppi et al.189 in a randomized, non-inferiority multicenter trial had shown that a five-day course of oral prednisone (at 40 mg daily) was similar to conventional 14-day course of prednisone with regard to re-exacerbation within six months of follow-up. Therefore, most patients with AEs-COPD can be treated with a five-day course of prednisone or equivalent (40 mg daily).
Pharmacological management
Pharmacological interventions consist of calcium and vitamin D supplementation and anti-resorptive therapy. Vitamin D and calcium supplementation is an integral part in the prevention and treatment of osteoporosis. Tang et al.190 evaluated the effects of calcium alone or in combination with Vitamin D on osteoporotic fractures and BMD in adults aged 50 years or older in a systematic review of 29 randomized controlled trials. In all, 17 trials reported fracture as an outcome, and treatment was associated with a 12% risk reduction in fractures of all types, whereas in the 24 trials that reported BMD as an outcome, treatment resulted in reduced bone loss of 0.54% at the hip and 1.19% at the spine. The treatment effects was found better with good adherence to therapy and with calcium dosages of 1200 mg or more or vitamin D dosages of 800 IU or more. The populations that gained maximum benefit from calcium supplementation in terms of reduction in fracture risk were older, institutionalized, low baseline calcium intake (<700 mg/day), and low serum 25(OH)D <25 nmol/L levels. Vitamin D also influences the fracture risk by decreasing falls and increasing the BMD, and these benefits are dose dependent.191 Vitamin D doses below 700 IU a day has no effect on the prevention of falls. Vitamin D deficiency causes falls because of the development of muscle weakness.192 Vitamin D binds to its nuclear receptor in muscle tissue and increases de novo protein synthesis in the muscles.192 This effect precedes the effect of vitamin D on bone.193 In a pooled analysis of several randomized controlled trials, reduction in the risk of fractures was noted only with 800 IU daily doses, with a 30% reduction in the risk of hip fracture and a 14% reduction in the risk of any non-vertebral fractures.194 Combination therapy is the best for fracture prevention. Vitamin D without calcium supplementation is ineffective in preventing fractures.195
Bisphosphonates
Bisphosphonates are the most commonly prescribed drugs for the prevention and treatment of osteoporosis. Bisphosphonates are chemically stable derivatives of inorganic pyrophosphate (PPi), but contain a carbon in the backbone of the molecule (P-C-P), instead of oxygen (P-O-P in pyrophosphate).196 The P-C-P configuration makes the molecules chemically stable by conferring resistance to chemical and enzymatic hydrolysis.197
Bisphosphonates have a very high skeletal retention because of their avidity to hydroxyapatite crystals. They are internalized by endocytosis and inhibit bone resorption by reducing the recruitment and activity of osteoclasts and increasing their apoptosis.196 Bisphosphonates also inhibit osteoblasts and osteocytes apoptosis, but the importance of this function is currently unclear. Bisphosphonates inhibit the osteoclast functions by inhibiting farnesyl pyrophosphate synthase (FPPS), an essential enzyme of mevalonate pathway within osteoclasts, resulting in reduced formation of prenylated GTP-binding proteins.197 The prenylated GTP-binding protein is an important signal in osteoclasts, and lack of these proteins produce altered membrane trafficking, lack of cellular morphology control, disruption of integrin signaling, loss of membrane ruffling, and ultimately apoptosis.198,199 The ranking of bisphosphonates from the highest to lowest hydroxyapatite affinity is as follows: zoledronate > pamidronate > alendronate > ibandronate > risedronate > etidronate > clodronate.200 Bisphosphonates tend to bind more avidly to trabecular bone, as trabecular bone is more accessible and metabolically active than cortical bone. It explains the greater reduction of the vertebral fracture risk compared to reduction in non-vertebral fracture risk, as the vertebrae are enriched with trabecular bone.200 Bisphosphonates are classified into two major groups: nitrogen-containing (NC) and non–nitrogen-containing (NNC) bisphosphonates. The NC group contains zoledronic acid, pamidronate, alendronate, and risedronate.201 A protective effect of bisphosphonates has been reported in postmenopausal and glucocorticoid-induced osteoporosis in many large randomized controlled trials.202 Smith et al.203 evaluated the role of daily alendronate on BMD in patients with airways disease with low BMD. They reported a significant improvement in the lumbar spine, but not hip, BMD with daily alendronate for 12 months. Zoledronic acid has the best overall fracture protection among the available bisphosphonates for osteoporosis.204 Maximum effect of bisphosphonates becomes obvious in three to six months, and with continued treatment, it is maintained in a new steady state for 10 years.205 Toxicities reported with bisphosphonates therapy are low. Patients may develop mild gastrointestinal complaints. Orally administered drugs may irritate the esophagus and should be avoided in the following groups: inability to stand or sit upright for at least 30 minutes, active upper gastrointestinal symptoms, or have delayed esophageal emptying (eg, strictures, achalasia, or severe dysmotility).206 Other side effects are acute phase reaction in patients treated with intravenous bisphosphonates, nephrotoxicity, osteonecrosis of the jaw, and atrial fibrillation.
Teriparatide is the 1–34 N-terminal active fragment of endogenous PTH and is effective in women with postmenopausal osteoporosis, men with idiopathic or hypogonadal osteoporosis, and patients with glucocorticoid-induced osteoporosis.207 The skeletal effect of PTH depends on the nature of exposure. Continuous exposure results in an increased differentiation of osteoclasts, and intermittent exposure preferentially stimulates osteoblasts, resulting in new bone formation.208 In corticosteroid-induced osteoporosis, teriparatide was found to be more effective than alendronate. Saag et al.209,210 in a randomized controlled trial compared the effects of teriparatide (20 μg/day) and alendronate on BMD in patients with corticosteroid-induced osteoporosis. BMD of the lumbar spine increased significantly after 18 months follow-up in the teriparatide group than in the alendronate group (7.2 vs. 3.4%; P < 0.001). They also had fewer new vertebral fractures. BMD of the total hip increased from baseline by 3.8% and 5.2%, respectively, at 18 and 36 months follow-up in the teriparatide group.
Denosumab is a promising new anti-resorptive drug. It is a fully humanized recombinant monoclonal antibody that binds to the RANKL. Denosumab decreases bone resorption by binding to the RANKL and inhibiting the RANKL/RANK interaction on the surface of osteoclasts and osteoclast precursors. It results in inhibition of osteoclast differentiation, activity, and survival.196,211 Denosumab is administered at a dosage of 60 mg as a single subcutaneous injection into the thigh, abdomen, or upper arm once every six months for up to three years. Patients must be given calcium and vitamin D supplements as denosumab is contraindicated in patients with hypocalcemia. In several international phase III trials involving more than 12,000 women with postmenopausal osteoporosis or low BMD, denosumab reduces the incidence of vertebral, non-vertebral, and hip fractures relative to placebo. It also increases BMD at all skeletal sites evaluated, including the lumbar spine and total hip, and increases the BMD significantly compared to that by oral alendronate, ibandronate, or risedronate.212 Combined effect of teriparatide and denosumab on the spine and hip BMD is significantly more than either drug alone. In the Denosumab and Teriparatide Administration (DATA) study, Tsai et al.213 demonstrated that 12 months of combined denosumab and teriparatide therapy increase areal BMD at the spine and hip more than either treatment alone and more than what has been reported with any currently recommended treatment. The same authors also studied the effect of this combination on bone microarchitecture by HR-pQCT study.214 The combination therapy improved the bone microstructure more as compared to either drug alone. These superior effects of combination therapy may result in greater resistance to fracture and their potential role in patients with severe osteoporosis. Denosumab by reducing the osteoclast function also reduces osteoblastic bone formation. Therefore, it may further reduce bone formation in patients with corticosteroid-induced osteoporosis.
All symptomatic COPD patients should be evaluated for the presence of following minor criteria: BMI <21 kg/m2, current smoking, use of ethanol >3 units/day, age >65 years, parent hip fracture, rib fracture, menopause, inactivity, FEV1 <50% predicted, and major criteria: systemic corticosteroids (three months/year) and major fragility fracture (spine/hip).
BMD of the hip and lumbar spine should be measured by DEXA scan along with serum 25-OH D if at least three minor or one major criterion is present. Pharmacologic therapy is indicated in the following conditions:215
COPD with documented fragility hip or vertebral fractures,
T-score below −2.5SD, and
−2.5, T-score <−1 and one major criterion.
However, there is a practical problem with this approach as it will impose a huge economic burden, particularly in developing countries with high burden of COPD. We need more research in this field to develop a COPD-centric evidence-based guideline suitable for mass implication.
Fracture risk in corticosteroid-associated osteoporosis is mostly independent of BMD; therefore, the American College of Rheumatology (ACR) guideline recommends estimation of patient’s overall clinical risk by FRAX score instead of T-scores alone for pharmacologic intervention.216 Anti-resorptive therapy should be started early during corticosteroid treatment as the bone loss starts quite early and fracture risk is independent of BMD. Alendronate, risedronate, and zoledronic acid are normally used; however, in severe osteoporosis, teriparatide is recommended.217
Monitoring
In otherwise healthy individuals treated for osteoporosis, repeat DEXA scan is usually recommended after a minimum of two years of anti-resorptive treatment, as it takes minimal two years to have a least significant change in BMD.218 COPD patients treated with oral corticosteroids develop osteoporosis at an accelerated pace and is recommended to have annual repeat DEXA scans, and corticosteroids-treated COPD patients should be monitored in the same fashion.219
Conclusion
Comorbidities are common in COPD patients, and their assessment should be done routinely. Osteoporosis is a common comorbidity in COPD patients and is associated with significant morbidity. Various factors implicated in the pathogenesis of osteoporosis are systemic inflammatory, physical inactivity, body composition changes, tobacco exposure, corticosteroids use, hypogonadism, anemia, COPD exacerbation, and hypoxia. DEXA scan is the gold standard for the diagnosis of osteoporosis. Early diagnosis and treatment prevents future fracture risk. However, in developing countries with insufficient resources, there is a practical problem of applying screening procedure to all COPD patients. We definitely need a COPD-specific guideline for osteoporosis in the future.
Glossary
Abbreviations
- COPD
Chronic obstructive pulmonary disease
- GOLD
Global Initiative for Chronic Obstructive Lung Disease
- WHO
World Health Organization
- BMD
Bone mineral density
- DEXA
Dual-energy X-ray absorptiometry
- FFMI
Fat-free mass index
- OPG
Osteoprotegerin
- RANK
Receptor activator of nuclear factor-kB
- RANKL
RANK-ligand
Footnotes
ACADEMIC EDITOR: Hussein D. Foda, Editor in Chief
FUNDING: Authors disclose no funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review by minimum of two reviewers. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: MS. Analyzed the data: MS, JK. Wrote the first draft of the manuscript: MS, RB. Contributed to the writing of the manuscript: MS, IM, JK. Agree with manuscript results and conclusions: MS, IM. Jointly developed the structure and arguments for the paper: MS, RB. Made critical revisions and approved final version: MS. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020 Global Burden of Disease study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2014. [Accessed July 30, 2014]. Available at: http://www.goldcopd.org.
- 3.Chatila WM, Thomashow BM, Minai OA, Criner GJ, Make BJ. Comorbidities in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(4):549–55. doi: 10.1513/pats.200709-148ET. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terzano C, Conti V, Di Stefano F, et al. Comorbidity, hospitalization, and mortality in COPD: results from a longitudinal study. Lung. 2010;188(4):321–9. doi: 10.1007/s00408-009-9222-y. [DOI] [PubMed] [Google Scholar]
- 5.Frei A, Muggensturm P, Putcha N, et al. Five comorbidities reflected the health status in patients with chronic obstructive pulmonary disease: the newly developed COMCOLD index. J Clin Epidemiol. 2014;67(8):904–11. doi: 10.1016/j.jclinepi.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Burgel PR, Escamilla R, Perez T, et al. INITIATIVES BPCO Scientific Committee Impact of comorbidities on COPD-specific health-related quality of life. Respir Med. 2013;107(2):233–41. doi: 10.1016/j.rmed.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Choudhury G, Rabinovich R, MacNee W. Comorbidities and systemic effects of chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(1):101–30. doi: 10.1016/j.ccm.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Guglielmi G, Muscarella S, Bazzocchi A. Integrated imaging approach to osteoporosis: state-of-the-art review and update. Radiographics. 2011;31(5):1343–64. doi: 10.1148/rg.315105712. [DOI] [PubMed] [Google Scholar]
- 9.Graat-Verboom L, Wouters EF, Smeenk FW, van den Borne BE, Lunde R, Spruit MA. Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J. 2009;34(1):209–18. doi: 10.1183/09031936.50130408. [DOI] [PubMed] [Google Scholar]
- 10.WHO . Assessment of Fracture Risk and its Application to Screening for Postmenopausal Osteoporosis. Geneva: WHO; 1994. (Technical report series 843). [PubMed] [Google Scholar]
- 11.NIH Consensus Development Panel on Osteoporosis Prevention, diagnosis, and therapy. osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285(6):785–95. doi: 10.1001/jama.285.6.785. [DOI] [PubMed] [Google Scholar]
- 12.Lehouck A, Boonen S, Decramer M, Janssens W. COPD, bone metabolism, and osteoporosis. Chest. 2011;139(3):648–57. doi: 10.1378/chest.10-1427. [DOI] [PubMed] [Google Scholar]
- 13.Shane E, Silverberg SJ, Donovan D, et al. Osteoporosis in lung transplantation candidates with end-stage pulmonary disease. Am J Med. 1996;101(3):262–9. doi: 10.1016/S0002-9343(96)00155-6. [DOI] [PubMed] [Google Scholar]
- 14.Gosch M, Kammerlander C, Roth T, Doshi HK, Gasser RW, Blauth M. Surgeons save bones: an algorithm for orthopedic surgeons managing secondary fracture prevention. Arch Orthop Trauma Surg. 2013;133:1101–8. doi: 10.1007/s00402-013-1774-x. [DOI] [PubMed] [Google Scholar]
- 15.Papaioannou A, Watts NB, Kendler DL, Yuen CK, Adachi JD, Ferko N. Diagnosis and management of vertebral fractures in elderly adults. Am J Med. 2002;113(3):220–8. doi: 10.1016/s0002-9343(02)01190-7. [DOI] [PubMed] [Google Scholar]
- 16.Majumdar SR, Villa-Roel C, Lyons KJ, Rowe BH. Prevalence and predictors of vertebral fracture in patients with chronic obstructive pulmonary disease. Respir Med. 2010;104(2):260–6. doi: 10.1016/j.rmed.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Harrison RA, Siminoski K, Vethanayagam D, Majumdar SR. Osteoporosis-related kyphosis and impairments in pulmonary function: a systematic review. J Bone Miner Res. 2007;22:447–57. doi: 10.1359/jbmr.061202. [DOI] [PubMed] [Google Scholar]
- 18.Nuti R, Siviero P, Maggi S, et al. Vertebral fractures in patients with chronic obstructive pulmonary disease: the EOLO study. Osteoporos Int. 2009;20(6):989–98. doi: 10.1007/s00198-008-0770-4. [DOI] [PubMed] [Google Scholar]
- 19.Schnell K, Weiss CO, Lee T, et al. The prevalence of clinically-relevant comorbid conditions in patients with physician-diagnosed COPD: a cross-sectional study using data from NHANES 1999–2008. BMC Pulm Med. 2012;12:26. doi: 10.1186/1471-2466-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silva DR, Coelho AC, Dumke A, et al. Osteoporosis prevalence and associated factors in patients with COPD: a cross-sectional study. Respir Care. 2011;56(7):961–8. doi: 10.4187/respcare.01056. [DOI] [PubMed] [Google Scholar]
- 21.Hattiholi J, Gaude GS. Prevalence and correlates of osteoporosis in chronic obstructive pulmonary disease patients in India. Lung India. 2014;31(3):221–7. doi: 10.4103/0970-2113.135759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhattacharyya P, Paul R, Ghosh M, et al. Prevalence of osteoporosis and osteopenia in advanced chronic obstructive pulmonary disease patients. Lung India. 2011;28(3):184–6. doi: 10.4103/0970-2113.83974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferguson GT, Calverley PM, Anderson JA, et al. Prevalence and progression of osteoporosis in patients with COPD: results from the TOwards a Revolution in COPD Health study. Chest. 2009;136:1456–65. doi: 10.1378/chest.08-3016. [DOI] [PubMed] [Google Scholar]
- 24.Graat-Verboom L, Smeenk FW, van den Borne BE, et al. Progression of osteoporosis in patients with COPD: a 3 year follow-up study. Respir Med. 2012;106(6):861–70. doi: 10.1016/j.rmed.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 25.Graat-Verboom L, Spruit MA, van den Borne BE, et al. CIRO Network Correlates of osteoporosis in chronic obstructive pulmonary disease: an underestimated systemic component. Respir Med. 2009;103:1143–51. doi: 10.1016/j.rmed.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ., III Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–9. J Bone Miner Res. 1992;7:221–7. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 27.Cooper C, Melton LJ., III Vertebral fractures: how large is the silent epidemic? BMJ. 1992;304:793–4. doi: 10.1136/bmj.304.6830.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alexandru D, So W. Evaluation and management of vertebral compression fractures. Perm J. 2012;16:46–51. doi: 10.7812/tpp/12-037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, III, Berger M. Patients with prior fracture have an increased risk of future fracture: summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–7. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 30.Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14:821–8. doi: 10.1359/jbmr.1999.14.5.821. [DOI] [PubMed] [Google Scholar]
- 31.Silverman SL, Minshall ME, Shen W, Harper KD, Xie S. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation study. Arthritis Rheum. 2001;44:2611–9. doi: 10.1002/1529-0131(200111)44:11<2611::aid-art441>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 32.Delmas PD, van de Langerijt L, Watts NB, et al. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20:557–63. doi: 10.1359/JBMR.041214. [DOI] [PubMed] [Google Scholar]
- 33.McEvoy CE, Ensrud KE, Bender E, et al. Association between corticosteroid use and vertebral fractures in older men with chronic obstructive lung disease. Am J Respir Crit Care Med. 1998;157:704–9. doi: 10.1164/ajrccm.157.3.9703080. [DOI] [PubMed] [Google Scholar]
- 34.Kim N, Rowe BH, Raymond G, et al. Underreporting of vertebral fractures on routine chest radiography. AJR Am J Roentgenol. 2004;182:297–300. doi: 10.2214/ajr.182.2.1820297. [DOI] [PubMed] [Google Scholar]
- 35.Morris AH, Zuckerman JD. National consensus conference on improving the continuum of care for patients with hip fracture. J Bone Joint Surg Am. 2002;84(4):670–4. doi: 10.2106/00004623-200204000-00027. [DOI] [PubMed] [Google Scholar]
- 36.Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg. 2008;16:596–607. doi: 10.5435/00124635-200810000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Dell R, Green D. Is osteoporosis disease management cost effective? Curr Osteoporos Rep. 2010;8:49–55. doi: 10.1007/s11914-010-0009-0. [DOI] [PubMed] [Google Scholar]
- 38.Friedman SM, Mendelson DA. Epidemiology of fragility fractures. Clin Geriatr Med. 2014;30:175–81. doi: 10.1016/j.cger.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 39.de Luise C, Brimacombe M, Pedersen L, Sørensen HT. Chronic obstructive pulmonary disease and mortality following hip fracture: a population-based cohort study. Eur J Epidemiol. 2008;23(2):115–22. doi: 10.1007/s10654-007-9211-5. [DOI] [PubMed] [Google Scholar]
- 40.Regan EA, Radcliff TA, Henderson WG, et al. Improving hip fractures outcomes for COPD patients. COPD. 2013;10(1):11–9. doi: 10.3109/15412555.2012.723072. [DOI] [PubMed] [Google Scholar]
- 41.Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2000;15:993–1000. doi: 10.1359/jbmr.2000.15.6.993. [DOI] [PubMed] [Google Scholar]
- 42.Dempster DW. Anatomy and functions of the adult skeleton. In: Favus MJ, et al., editors. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism. 6th ed. Washington, DC: American Society for Bone and Mineral Research; 2006. pp. 7–11. [Google Scholar]
- 43.Feng X, McDonald JM. Disorders of bone remodeling. Annu Rev Pathol. 2011;6:121–45. doi: 10.1146/annurev-pathol-011110-130203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Akhter MP, Lappe JM, Davies KM, Recker RR. Transmenopausal changes in the trabecular bone structure. Bone. 2007;41(1):111–6. doi: 10.1016/j.bone.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 45.Kulak CA, Borba VC, Jorgetti V, et al. Skeletal microstructural abnormalities in postmenopausal women with chronic obstructive pulmonary disease. J Bone Miner Res. 2010;25(9):1931–40. doi: 10.1002/jbmr.88. [DOI] [PubMed] [Google Scholar]
- 46.Graat-Verboom L, van den Borne BE, Smeenk FW, Spruit MA, Wouters EF. Osteoporosis in COPD outpatients based on bone mineral density and vertebral fractures. J Bone Miner Res. 2011;26(3):561–8. doi: 10.1002/jbmr.257. [DOI] [PubMed] [Google Scholar]
- 47.Brandi ML. Microarchitecture, the key to bone quality. Rheumatology (Oxford) 2009;48(suppl 4):iv3–8. doi: 10.1093/rheumatology/kep273. [DOI] [PubMed] [Google Scholar]
- 48.Steiner NK, Milhorn D, Hammett-Stabler C. Osteoporosis in men. Clin Biochem. 2014;47:950–9. doi: 10.1016/j.clinbiochem.2014.03.026. [DOI] [PubMed] [Google Scholar]
- 49.Sims NA, Gooi JH. Bone remodeling: multiple cellular interactions required for coupling of bone formation and resorption. Semin Cell Dev Biol. 2008;19:444–51. doi: 10.1016/j.semcdb.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 50.Zuo C, Huang Y, Bajis R, et al. Osteoblastogenesis regulation signals in bone remodeling. Osteoporos Int. 2012;23:1653–63. doi: 10.1007/s00198-012-1909-x. [DOI] [PubMed] [Google Scholar]
- 51.Baud’huin M, Duplomb L, Teletchea S, et al. Osteoprotegerin: multiple partners for multiple functions. Cytokine Growth Factor Rev. 2013;24(5):401–9. doi: 10.1016/j.cytogfr.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 52.Dougall WC. RANKL signaling in bone physiology and cancer. Curr Opin Support Palliat Care. 2007;1(4):317–22. doi: 10.1097/SPC.0b013e3282f335be. [DOI] [PubMed] [Google Scholar]
- 53.Roodman GD. Biology of osteoclast activation in cancer. J Clin Oncol. 2001;19:3562–71. doi: 10.1200/JCO.2001.19.15.3562. [DOI] [PubMed] [Google Scholar]
- 54.Yasuda H, Shima N, Nakagawa N, et al. Identity of osteoclastogenesis inhibitory factor (OCIF) and osteoprotegerin (OPG): a mechanism by which OPG/OCIF inhibits osteoclastogenesis in vitro. Endocrinology. 1998;139:1329–37. doi: 10.1210/endo.139.3.5837. [DOI] [PubMed] [Google Scholar]
- 55.Bucay N, Sarosi I, Dunstan CR, et al. Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev. 1998;12:1260–8. doi: 10.1101/gad.12.9.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lacey DL, Timms E, Tan HL, et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;93(2):165–76. doi: 10.1016/s0092-8674(00)81569-x. [DOI] [PubMed] [Google Scholar]
- 57.Trouvin P, Goëb V. Receptor activator of nuclear factor-κB ligand and osteoprotegerin: maintaining the balance to prevent bone loss. Clin Interv Aging. 2010;5:345–54. doi: 10.2147/CIA.S10153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Theill LE, Boyle WJ, Penninger JM. RANK-L and RANK: T cells, bone loss, and mammalian evolution. Annu Rev Immunol. 2002;20:795–823. doi: 10.1146/annurev.immunol.20.100301.064753. [DOI] [PubMed] [Google Scholar]
- 59.Bai P, Sun Y, Jin J, et al. Disturbance of the OPG/RANK/RANKL pathway and systemic inflammation in COPD patients with emphysema and osteoporosis. Respir Res. 2011;12:157. doi: 10.1186/1465-9921-12-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eagan TM, Ueland T, Wagner PD, et al. Systemic inflammatory markers in COPD: results from the Bergen COPD Cohort study. Eur Respir J. 2010;35(3):540–8. doi: 10.1183/09031936.00088209. [DOI] [PubMed] [Google Scholar]
- 61.Garcia-Rio F, Miravitlles M, Soriano JB, et al. EPI-SCAN Steering Committee Systemic inflammation in chronic obstructive pulmonary disease: a population-based study. Respir Res. 2010;11:63. doi: 10.1186/1465-9921-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sapey E, Ahmad A, Bayley D, et al. Imbalances between interleukin-1 and tumor necrosis factor agonists and antagonists in stable COPD. J Clin Immunol. 2009;29(4):508–16. doi: 10.1007/s10875-009-9286-8. [DOI] [PubMed] [Google Scholar]
- 63.Théoleyre S, Wittrant Y, Tat SK, Fortun Y, Redini F, Heymann D. The molecular triad OPG/RANK/RANKL: involvement in the orchestration of pathophysiological bone remodeling. Cytokine Growth Factor Rev. 2004;15:457–75. doi: 10.1016/j.cytogfr.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 64.Krishnan V, Bryant HU, Macdougald OA. Regulation of bone mass by Wnt signaling. J Clin Invest. 2006;116:1202–9. doi: 10.1172/JCI28551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rodda SJ, McMahon AP. Distinct roles for Hedgehog and canonical Wnt signaling enitors. Development. 2006;133:3231–44. doi: 10.1242/dev.02480. [DOI] [PubMed] [Google Scholar]
- 66.Almeida M, Han L, Bellido T, Manolagas SC, Kousteni S. Wnt proteins prevent apoptosis of both uncommitted osteoblast progenitors and differentiated osteoblasts by beta-catenin-dependent and -independent signaling cascades involving Src/ERK and phosphatidylinositol 3-kinase/AKT. J Biol Chem. 2005;280:41342–51. doi: 10.1074/jbc.M502168200. [DOI] [PubMed] [Google Scholar]
- 67.Glass DA, II, Bialek P, Ahn JD, et al. Canonical Wnt signaling in differentiated osteoblasts controls osteoclast differentiation. Dev Cell. 2005;8:751–64. doi: 10.1016/j.devcel.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 68.Patel MS, Karsenty G. Regulation of bone formation and vision by LRP5.N. N Engl J Med. 2002;346:1572–4. doi: 10.1056/NEJM200205163462011. [DOI] [PubMed] [Google Scholar]
- 69.Kneidinger N, Yildirim AÖ, Callegari J, et al. Activation of the WNT/beta-catenin pathway attenuates experimental emphysema. Am J Respir Crit Care Med. 2011;183(6):723–33. doi: 10.1164/rccm.200910-1560OC. [DOI] [PubMed] [Google Scholar]
- 70.Verma RP, Hansch C. Matrix metalloproteinases (MMPs): chemical-biological functions and (Q) SARs. Bioorg Med Chem. 2007;15(6):2223–68. doi: 10.1016/j.bmc.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 71.Brew K, Dinakarpandian D, Nagase H. Tissue inhibitors of metalloproteinases: evolution, structure and function. Biochim Biophys Acta. 2000;1477:267–83. doi: 10.1016/s0167-4838(99)00279-4. [DOI] [PubMed] [Google Scholar]
- 72.Hill PA, Murphy G, Docherty AJ, et al. The effects of selective inhibitors of matrix metalloproteinases (MMPs) on bone resorption and the identification of MMPs and TIMP-1 in isolated osteoclasts. J Cell Sci. 1994;107(pt 11):3055–64. doi: 10.1242/jcs.107.11.3055. [DOI] [PubMed] [Google Scholar]
- 73.Bolton CE, Stone MD, Edwards PH, Duckers JM, Evans WD, Shale DJ. Circulating matrix metalloproteinase-9 and osteoporosis in patients with chronic obstructive pulmonary disease. Chron Respir Dis. 2009;6(2):81–7. doi: 10.1177/1479972309103131. [DOI] [PubMed] [Google Scholar]
- 74.Zhang PF, Pan L, Luo ZY, Zhao HJ, Cai SX. Interrelationship of circulating matrix metalloproteinase-9, TNF-α and OPG/RANK/RANKL systems in COPD patients with osteoporosis. COPD. 2013;10(6):650–6. doi: 10.3109/15412555.2013.813928. [DOI] [PubMed] [Google Scholar]
- 75.Vicchio D, Yergey A, O’Brien K, Allen L, Ray R, Holick M. Quantification and kinetics of 25-hydroxyvitamin D3 by isotope dilution liquid chromatography/thermospray mass spectrometry. Biol Mass Spectrom. 1993;22(1):53–8. doi: 10.1002/bms.1200220107. [DOI] [PubMed] [Google Scholar]
- 76.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 77.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Endocrine Society Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 78.Førli L, Halse J, Haug E, et al. Vitamin D deficiency, bone mineral density and weight in patients with advanced pulmonary disease. J Intern Med. 2004;256:56–62. doi: 10.1111/j.1365-2796.2004.01337.x. [DOI] [PubMed] [Google Scholar]
- 79.Romme EA, Rutten EP, Smeenk FW, Spruit MA, Menheere PP, Wouters EF. Vitamin D status is associated with bone mineral density and functional exercise capacity in patients with chronic obstructive pulmonary disease. Ann Med. 2013;45:91–6. doi: 10.3109/07853890.2012.671536. [DOI] [PubMed] [Google Scholar]
- 80.Janssens W, Bouillon R, Claes B, et al. Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene. Thorax. 2010;65(3):215–20. doi: 10.1136/thx.2009.120659. [DOI] [PubMed] [Google Scholar]
- 81.Persson LJ, Aanerud M, Hiemstra PS, Hardie JA, Bakke PS, Eagan TM. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS One. 2012;7:e38934. doi: 10.1371/journal.pone.0038934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brot C, Jurgensen RN, Sùrensen HO. The influence of smoking on vitamin D status and calcium metabolism. Eur J Clin Nutr. 1999;53:920–6. doi: 10.1038/sj.ejcn.1600870. [DOI] [PubMed] [Google Scholar]
- 83.Eastell R, Yergey AL, Vieira NE, Cedel SL, Kumar R, Riggs BL. Interrelationship among vitamin D metabolism, true calcium absorption, parathyroid function, and age in women: evidence of an age-related intestinal resistance to 1,25-dihydroxyvitamin D action. J Bone Miner Res. 1991;6:125–32. doi: 10.1002/jbmr.5650060205. [DOI] [PubMed] [Google Scholar]
- 84.Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001;22(4):477–501. doi: 10.1210/edrv.22.4.0437. [DOI] [PubMed] [Google Scholar]
- 85.Baldock PA, Thomas GP, Hodge JM, et al. Vitamin D action and regulation of bone remodeling: suppression of osteoclastogenesis by the mature osteoblast. J Bone Miner Res. 2006;21(10):1618–26. doi: 10.1359/jbmr.060714. [DOI] [PubMed] [Google Scholar]
- 86.Van Schoor NM, Visser M, Pluijm SM, Kuchuk N, Smit JH, Lips P. Vitamin D deficiency as a risk factor for osteoporotic fractures. Bone. 2008;42(2):260–6. doi: 10.1016/j.bone.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 87.Calverley PM, Anderson JA, Celli B, et al. TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356:775–89. doi: 10.1056/NEJMoa063070. [DOI] [PubMed] [Google Scholar]
- 88.Kanis JA, Johansson H, Oden A, et al. A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res. 2004;19(6):893–9. doi: 10.1359/JBMR.040134. [DOI] [PubMed] [Google Scholar]
- 89.Van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int. 2002;13(10):777–87. doi: 10.1007/s001980200108. [DOI] [PubMed] [Google Scholar]
- 90.Loke YK, Cavallazzi R, Singh S. Risk of fractures with inhaled corticosteroids in COPD: systematic review and meta-analysis of randomized controlled trials and observational studies. Thorax. 2011;66(8):699–708. doi: 10.1136/thx.2011.160028. [DOI] [PubMed] [Google Scholar]
- 91.Lee TA, Weiss KB. Fracture risk associated with inhaled corticosteroid use in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004;169(7):855–9. doi: 10.1164/rccm.200307-926OC. [DOI] [PubMed] [Google Scholar]
- 92.Mathioudakis AG, Amanetopoulou SG, Gialmanidis IP, et al. Impact of long-term treatment with low-dose inhaled corticosteroids on the bone mineral density of chronic obstructive pulmonary disease patients: aggravating or beneficial? Respirology. 2013;18(1):147–53. doi: 10.1111/j.1440-1843.2012.02265.x. [DOI] [PubMed] [Google Scholar]
- 93.Man SF, Sin DD. Thinning bone and inhaled corticosteroid in COPD: what to do until there is definitive proof? Chest. 2009;136(6):1448–9. doi: 10.1378/chest.09-1787. [DOI] [PubMed] [Google Scholar]
- 94.Van Staa TP, Laan RF, Barton IP, Cohen S, Reid DM, Cooper C. Bone density threshold and other predictors of vertebral fracture in patients receiving oral glucocorticoid therapy. Arthritis Rheum. 2003;48:3224–9. doi: 10.1002/art.11283. [DOI] [PubMed] [Google Scholar]
- 95.Weinstein SR. Glucocorticoid-induced bone disease. N Engl J Med. 2011;365:62–70. doi: 10.1056/NEJMcp1012926. [DOI] [PubMed] [Google Scholar]
- 96.Seeman E, Delmas PD. Bone quality–the material and structural basis of bone strength and fragility. N Engl J Med. 2006;354:2250–61. doi: 10.1056/NEJMra053077. [DOI] [PubMed] [Google Scholar]
- 97.Maricic M. Update on glucocorticoid-induced osteoporosis. Rheum Dis Clin North Am. 2011;37:415–31. doi: 10.1016/j.rdc.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 98.de Gregório LH, Lacativa PG, Melazzi AC, Russo LA. Glucocorticoid-induced osteoporosis. Arq Bras Endocrinol Metabol. 2006;50(4):793–801. doi: 10.1590/s0004-27302006000400024. [DOI] [PubMed] [Google Scholar]
- 99.Henneicke H, Gasparini SJ, Brennan-Speranza TC, Zhou H, Seibel MJ. Glucocorticoids and bone: local effects and systemic implications. Trends Endocrinol Metab. 2014;25(4):197–211. doi: 10.1016/j.tem.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 100.Canalis E, Bilezikian JP, Angeli A, Giustina A. Perspectives on glucocorticoid induced osteoporosis. Bone. 2004;34:593–8. doi: 10.1016/j.bone.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 101.Ohnaka K, Taniguchi H, Kawate H, Nawata H, Takayanagi R. Glucocorticoid enhances the expression of dickkopf-1 in human osteoblasts: novel mechanism of glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun. 2004;318(1):259–64. doi: 10.1016/j.bbrc.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 102.Wang Y, Wan C, Deng L, et al. The hypoxia-inducible factor alpha pathway couples angiogenesis to osteogenesis during skeletal development. J Clin Invest. 2007;117:1616–26. doi: 10.1172/JCI31581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pufe T, Scholz-Ahrens KE, Franke AT, et al. The role of vascular endothelial growth factor in glucocorticoid-induced bone loss: evaluation in a minipig model. Bone. 2003;33:869–76. doi: 10.1016/j.bone.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 104.Alesci S, De Martino MU, Illias I. Glucocorticoid-induced osteoporosis: from basic mechanisms to clinical aspects. Neuroimmunomodulation. 2005;12:1–19. doi: 10.1159/000082360. [DOI] [PubMed] [Google Scholar]
- 105.Dovio A, Perazzolo L, Saba L, et al. High-dose glucocorticoids increase serum levels of soluble Il-6 receptor alpha and its ratio to soluble gp130: an additional mechanism for early increased bone resorption. Eur J Endocrinol. 2006;154:745–51. doi: 10.1530/eje.1.02147. [DOI] [PubMed] [Google Scholar]
- 106.Takuma A, Kaneda T, Sato T, Ninomiya S, Kumegawa M, Hakeda Y. Dexamethasone enhances osteoclasts formation synergistically with transforming growth factor-beta by stimulating the priming of osteoclast progenitors for differentiation into osteoclasts. J Biol Chem. 2003;278:44667–74. doi: 10.1074/jbc.M300213200. [DOI] [PubMed] [Google Scholar]
- 107.Jia D, O’Brien CA, Stewart SA, Manolagas SC, Weinstein RS. Glucocorticoids act directly on osteoclasts to increase their life span and reduce bone density. Endocrinology. 2006;147:5592–9. doi: 10.1210/en.2006-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Markus JS, Mark SC, Hong Z. Glucocorticoid-induced osteoporosis: mechanisms, management, and future perspectives. Lancet Diabetes Endocrinol. 2013;1:59–70. doi: 10.1016/S2213-8587(13)70045-7. [DOI] [PubMed] [Google Scholar]
- 109.Weinstein RS. Glucocorticoid-induced osteoporosis and osteonecrosis. Endocrinol Metab Clin North Am. 2012;41(3):595–611. doi: 10.1016/j.ecl.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.LoCascio V, Ballanti P, Milani S, et al. A histomorphometric long-term longitudinal study of trabecular bone loss in glucocorticoid- treated patients: prednisone versus deflazacort. Calcif Tissue Int. 1998;62:199–204. doi: 10.1007/s002239900417. [DOI] [PubMed] [Google Scholar]
- 111.Humphrey EL, Williams JH, Davie MW, Marshall MJ. Effects of dissociated glucocorticoids on OPG and RANKL in osteoblastic cells. Bone. 2006;38(5):652–61. doi: 10.1016/j.bone.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 112.Ong T, Sahota O, Tan W, Marshall LA. United Kingdom perspective on the relationship between body mass index (BMI) and bone health: a cross sectional analysis of data from the Nottingham Fracture Liaison Service. Bone. 2014;59:207–10. doi: 10.1016/j.bone.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 113.Barrera G, Bunout D, Gattás V, de la Maza MP, Leiva L, Hirsch S. A high body mass index protects against femoral neck osteoporosis in healthy elderly subjects. Nutrition. 2004;20(9):769–71. doi: 10.1016/j.nut.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 114.De Laet C, Kanis JA, Odén A, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16:1330–8. doi: 10.1007/s00198-005-1863-y. [DOI] [PubMed] [Google Scholar]
- 115.Morin S, Tsang JF, Leslie WD. Weight and body mass index predict bone mineral density and fractures in women aged 40 to 59 years. Osteoporos Int. 2009;20(3):363–70. doi: 10.1007/s00198-008-0688-x. [DOI] [PubMed] [Google Scholar]
- 116.Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med. 2007;176(8):753–60. doi: 10.1164/rccm.200612-1749OC. [DOI] [PubMed] [Google Scholar]
- 117.Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160:1856–61. doi: 10.1164/ajrccm.160.6.9902115. [DOI] [PubMed] [Google Scholar]
- 118.Vestbo J, Prescott E, Almdal T, et al. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart study. Am J Respir Crit Care Med. 2006;173(1):79–83. doi: 10.1164/rccm.200506-969OC. [DOI] [PubMed] [Google Scholar]
- 119.Agarwal K, Sharma L, Menon B, Gaur NS. Comparison of nutritional status in chronic obstructive pulmonary disease and asthma. Indian J Allergy Asthma Immunology. 2013;27(2):115–20. [Google Scholar]
- 120.Schols AM, Broekhuizen R, Weling-Scheepers CA, Wouters EF. Body composition and mortality in chronic obstructive pulmonary disease. Am J Clin Nutr. 2005;82:53–9. doi: 10.1093/ajcn.82.1.53. [DOI] [PubMed] [Google Scholar]
- 121.Vermeeren MA, Creutzberg EC, Schols AM, et al. COSMIC Study Group Prevalence of nutritional depletion in a large out-patient population of patients with COPD. Respir Med. 2006;100(8):1349–55. doi: 10.1016/j.rmed.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 122.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. European Working Group on Sarcopenia in Older People Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chung JH, Hwang HJ, Han CH, Son BS, Kim DH, Park MS. Association between Sarcopenia and metabolic syndrome in chronic obstructive pulmonary disease: The Korea National Health and Nutrition Examination Survey (KNHANES) from 2008 to 2011. COPD. 2015;12(1):82–9. doi: 10.3109/15412555.2014.908835. [DOI] [PubMed] [Google Scholar]
- 124.Coin A, Sergi G, Marin S, et al. Predictors of low bone mineral density in elderly males with chronic obstructive pulmonary disease: the role of body mass index. Aging Male. 2010;13(2):142–7. doi: 10.3109/13685531003657784. [DOI] [PubMed] [Google Scholar]
- 125.Bolton CE, Ionescu AA, Shiels KM, et al. Associated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004;170:1286–93. doi: 10.1164/rccm.200406-754OC. [DOI] [PubMed] [Google Scholar]
- 126.Jørgensen NR, Schwarz P. Osteoporosis in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2008;14(2):122–7. doi: 10.1097/MCP.0b013e3282f4efb6. [DOI] [PubMed] [Google Scholar]
- 127.Rondinone CM. Adipocyte-derived hormones, cytokines, and mediators. Endocrine. 2006;29(1):81–90. doi: 10.1385/endo:29:1:81. [DOI] [PubMed] [Google Scholar]
- 128.Cornish J, Callon KE, Bava U, et al. Leptin directly regulates bone cell function in vitro and reduces bone fragility in vivo. J Endocrinol. 2002;175:405–15. doi: 10.1677/joe.0.1750405. [DOI] [PubMed] [Google Scholar]
- 129.Thomas T, Gori F, Khosla S, Jensen MD, Burguera B, Riggs BL. Leptin acts on human marrow stromal cells to enhance differentiation to osteoblasts and to inhibit differentiation to adipocytes. Endocrinology. 1999;140:1630–8. doi: 10.1210/endo.140.4.6637. [DOI] [PubMed] [Google Scholar]
- 130.Holloway WR, Collier FM, Aitken CJ, et al. Leptin inhibits osteoclast generation. J Bone Miner Res. 2002;17:200–9. doi: 10.1359/jbmr.2002.17.2.200. [DOI] [PubMed] [Google Scholar]
- 131.Vondracek SF, Voelkel NF, McDermott MT, Valdez C. The relationship between adipokines, body composition, and bone density in men with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2009;4:267–77. doi: 10.2147/copd.s2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ducy P, Amling M, Takeda S, et al. Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell. 2000;100:197–207. doi: 10.1016/s0092-8674(00)81558-5. [DOI] [PubMed] [Google Scholar]
- 133.Elefteriou F, Ahn JD, Takeda S, et al. Leptin regulation of bone resorption by the sympathetic nervous system and CART. Nature. 2005;434:514–20. doi: 10.1038/nature03398. [DOI] [PubMed] [Google Scholar]
- 134.Reid IR. Relationships between fat and bone. Osteoporos Int. 2008;19:595–606. doi: 10.1007/s00198-007-0492-z. [DOI] [PubMed] [Google Scholar]
- 135.Pobeha P, Ukropec J, Skyba P, et al. Relationship between osteoporosis and adipose tissue leptin and osteoprotegerin in patients with chronic obstructive pulmonary disease. Bone. 2011;48(5):1008–14. doi: 10.1016/j.bone.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 136.Yohannes AM, Ershler WB. Anemia in COPD: a systematic review of the prevalence, quality of life, and mortality. Respir Care. 2011;56(5):644–52. doi: 10.4187/respcare.01002. [DOI] [PubMed] [Google Scholar]
- 137.Cesari M, Pahor M, Lauretani F, et al. Bone density and hemoglobin levels in older persons: results from the InCHIANTI study. Osteoporos Int. 2005;16:691–9. doi: 10.1007/s00198-004-1739-6. [DOI] [PubMed] [Google Scholar]
- 138.Korkmaz U, Korkmaz N, Yazici S, et al. Anemia as a risk factor for low bone mineral density in postmenopausal Turkish women. Eur J Intern Med. 2012;23(2):154–8. doi: 10.1016/j.ejim.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 139.Chen Z, Thomson CA, Aickin M, et al. Short list of women’s health initiative investigators. The relationship between incidence of fractures and anemia in older multiethnic women. J Am Geriatr Soc. 2010;58(12):2337–44. doi: 10.1111/j.1532-5415.2010.03183.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rutten EP, Franssen FM, Spruit MA, Wouters EF. Anemia is associated with bone mineral density in chronic obstructive pulmonary disease. COPD. 2013;10(3):286–92. doi: 10.3109/15412555.2012.744390. [DOI] [PubMed] [Google Scholar]
- 141.Fujimoto H, Fujimoto K, Ueda A, Ohata M. Hypoxemia is a risk factor for bone mass loss. J Bone Miner Metab. 1999;17(3):211–6. doi: 10.1007/s007740050087. [DOI] [PubMed] [Google Scholar]
- 142.Gustavsson A, Olsson T, Nordstrom P. Rapid loss of bone mineral density of the femoral neck after cessation of ice hockey training: a six-year longitudinal study in males. J Bone Miner Res. 2003;18(11):1964–9. doi: 10.1359/jbmr.2003.18.11.1964. [DOI] [PubMed] [Google Scholar]
- 143.de Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BC. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int. 2009;20(12):2111–25. doi: 10.1007/s00198-009-0938-6. [DOI] [PubMed] [Google Scholar]
- 144.Dougherty G. Quantitative CT in the measurement of bone quantity and bone quality for assessing osteoporosis. Med Eng Phys. 1996;18:557–68. doi: 10.1016/1350-4533(96)00011-2. [DOI] [PubMed] [Google Scholar]
- 145.Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database of Systematic Reviews. 2011;(7) doi: 10.1002/14651858.CD000333.pub2. Art. No.: CD000333. [DOI] [PubMed] [Google Scholar]
- 146.Polidoulis I, Beyene J, Cheung AM. The effect of exercise on pQCT parameters of bone structure and strength in postmenopausal women–a systematic review and meta-analysis of randomized controlled trials. Osteoporos Int. 2012 Jan;23(1):39–51. doi: 10.1007/s00198-011-1734-7. [DOI] [PubMed] [Google Scholar]
- 147.Lau RY, Guo X. A review on current osteoporosis research: with special focus on disuse bone loss. J Osteoporos. 2011;2011:293808. doi: 10.4061/2011/293808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lin C, Jiang X, Dai Z, et al. Sclerostin mediates bone response to mechanical unloading through antagonizing Wnt/β-catenin signaling. J Bone Miner Res. 2009;24(10):1651–61. doi: 10.1359/jbmr.090411. [DOI] [PubMed] [Google Scholar]
- 149.Vorrink SN, Kort HS, Troosters T, Lammers JW. Level of daily physical activity in individuals with COPD compared with healthy controls. Respir Res. 2011;12:33. doi: 10.1186/1465-9921-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Robinson JA, Chatterjee-Kishore M, Yaworsky PJ, et al. Wnt/beta-catenin signaling is a normal physiological response to mechanical loading in bone. J Biol Chem. 2006;281(42):31720–8. doi: 10.1074/jbc.M602308200. [DOI] [PubMed] [Google Scholar]
- 151.Mineo TC, Ambrogi V, Mineo D, Fabbri A, Fabbrini E, Massoud R. Bone mineral density improvement after lung volume reduction surgery for severe emphysema. Chest. 2005;127(6):1960–6. doi: 10.1378/chest.127.6.1960. [DOI] [PubMed] [Google Scholar]
- 152.Kiyokawa H, Muro S, Oguma T, et al. Impact of COPD exacerbations on osteoporosis assessed by chest CT scan. COPD. 2012;9(3):235–42. doi: 10.3109/15412555.2011.650243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Stanojkovic I, Kotur-Stevuljevic J, Spasic S, et al. Relationship between bone resorption, oxidative stress and inflammation in severe COPD exacerbation. Clin Biochem. 2013;46(16–17):1678–82. doi: 10.1016/j.clinbiochem.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 154.Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59(7):574–80. doi: 10.1136/thx.2003.019588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ward KD, Klesges RC. A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif Tissue Int. 2001;68(5):259–70. doi: 10.1007/bf02390832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Yoon V, Maalouf NM, Sakhaee K. The effects of smoking on bone metabolism. Osteoporos Int. 2012;23:2081–92. doi: 10.1007/s00198-012-1940-y. [DOI] [PubMed] [Google Scholar]
- 157.Dimai HP, Domej W, Leb G, Lau KH. Bone loss in patients with untreated chronic obstructive pulmonary disease is mediated by an increase in bone resorption associated with hypercapnia. J Bone Miner Res. 2001;16(11):2132–41. doi: 10.1359/jbmr.2001.16.11.2132. [DOI] [PubMed] [Google Scholar]
- 158.Mittal CK. Oxygen-radical/nitric oxide mediates calcium-dependent hormone action on cyclic GMP system: a novel concept in signal transduction mechanisms. Mol Cell Biochem. 1995;14:9–150. 257–62. doi: 10.1007/BF01076585. [DOI] [PubMed] [Google Scholar]
- 159.Laitala T, Vaananen HK. Inhibition of bone resorption in vitro by antisense RNA and DNA molecules targeted against carbonic anhydrase II or two subunits of vacuolar H1-ATPase. J Clin Invest. 1994;93:2311–8. doi: 10.1172/JCI117235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Arnett TR. Acidosis, hypoxia and bone. Arch Biochem Biophys. 2010;503:103–9. doi: 10.1016/j.abb.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 161.Park JH, Park BH, Kim HK, Park TS, Baek HS. Hypoxia decreases Runx2/Cbfa1 expression in human osteoblast-like cells. Mol Cell Endocrinol. 2002;192(1–2):197–203. doi: 10.1016/s0303-7207(02)00036-9. [DOI] [PubMed] [Google Scholar]
- 162.Compston JE. Sex steroids and bone. Physiol Rev. 2001;81:419–47. doi: 10.1152/physrev.2001.81.1.419. [DOI] [PubMed] [Google Scholar]
- 163.Balasubramanian V, Naing S. Hypogonadism in chronic obstructive pulmonary disease: incidence and effects. Curr Opin Pulm Med. 2012;18(2):112–7. doi: 10.1097/MCP.0b013e32834feb37. [DOI] [PubMed] [Google Scholar]
- 164.Irwig MS. Male hypogonadism and skeletal health. Curr Opin Endocrinol Diabetes Obes. 2013;20:517–22. doi: 10.1097/01.med.0000436185.36717.76. [DOI] [PubMed] [Google Scholar]
- 165.Cummings SR, Bates D, Black DM. Clinical use of bone densitometry: scientific review. JAMA. 2002;288:1889–97. doi: 10.1001/jama.288.15.1889. [DOI] [PubMed] [Google Scholar]
- 166.Lorente Ramos RM, Azpeitia Armán J, Arévalo Galeano N, Muñoz Hernández A, García Gómez JM, Gredilla Molinero J. Dual energy X-ray absorptimetry: fundamentals, methodology, and clinical applications. Radiologia. 2012;54(5):410–23. doi: 10.1016/j.rx.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 167.Ionescu AA, Schoon E. Osteoporosis in chronic obstructive pulmonary disease. Eur Respir J. 2003;22(suppl 46):64s–75s. doi: 10.1183/09031936.03.00004609. [DOI] [PubMed] [Google Scholar]
- 168.Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO study group. Osteoporos Int. 1994;4:368–81. doi: 10.1007/BF01622200. [DOI] [PubMed] [Google Scholar]
- 169.Baim S, Leonard MB, Bianchi ML, et al. Official positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD pediatric position development conference. J Clin Densitom. 2008;11:6–21. doi: 10.1016/j.jocd.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 170.Leib ES, Binkley N, Bilezikian JP, Kendler DL, Lewiecki EM, Petak SM. Position development conference of the international society for clinical densitometry. Vancouver, BC, July 15–17, 2005. J Rheumatol. 2006;33:2319–21. [PubMed] [Google Scholar]
- 171.Baim S, Binkley N, Bilezikian JP, et al. Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference. J Clin Densitom. 2008 Jan-Mar;11(1):75–91. doi: 10.1016/j.jocd.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 172.Maghraoui AE, Roux C. DXA scanning in clinical practice. Q J Med. 2008;101:605–17. doi: 10.1093/qjmed/hcn022. [DOI] [PubMed] [Google Scholar]
- 173.Damilakis J, Adams JE, Guglielmi G, Link TM. Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur Radiol. 2010;20:2707–14. doi: 10.1007/s00330-010-1845-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Link TM. Osteoporosis imaging: state of the art and advanced imaging. Radiology. 2012;263(1):3–17. doi: 10.1148/radiol.12110462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kanis JA, Oden A, Johansson H, Borgström F, Ström O, McCloskey E. FRAX and its applications to clinical practice. Bone. 2009;44(5):734–43. doi: 10.1016/j.bone.2009.01.373. [DOI] [PubMed] [Google Scholar]
- 176.Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137–48. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 177.Ogura-Tomomatsu H, Asano K, Tomomatsu K, et al. Predictors of osteoporosis and vertebral fractures in patients presenting with moderate-to-severe chronic obstructive lung disease. COPD. 2012;9:332–7. doi: 10.3109/15412555.2012.667850. [DOI] [PubMed] [Google Scholar]
- 178.Adams JE. Quantitative computed tomography. Eur J Radiol. 2009;71(3):415–24. doi: 10.1016/j.ejrad.2009.04.074. [DOI] [PubMed] [Google Scholar]
- 179.MacNeil JA, Boyd SK. Improved reproducibility of high resolution peripheral quantitative computed tomography for measurement of bone quality. Med Eng Phys. 2008;30:792–9. doi: 10.1016/j.medengphy.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 180.Donnelly E. Methods for assessing bone quality: a review. Clin Orthop Relat Res. 2011;469:2128–38. doi: 10.1007/s11999-010-1702-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Pistoia W, van Rietbergen B, Lochmuller EM, Lill CA, Eckstein F, Ruegsegger P. Estimation of distal radius failure load with microfinite element analysis models based on three-dimensional peripheral quantitative computed tomography images. Bone. 2002;30(6):842–8. doi: 10.1016/s8756-3282(02)00736-6. [DOI] [PubMed] [Google Scholar]
- 182.Krug R, Burghardt AJ, Majumdar S, Link TM. High-resolution imaging techniques for the assessment of osteoporosis. Radiol Clin North Am. 2010;48(3):601–21. doi: 10.1016/j.rcl.2010.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Adams JE. Advances in bone imaging for osteoporosis. Nat Rev Endocrinol. 2013;9:28–42. doi: 10.1038/nrendo.2012.217. [DOI] [PubMed] [Google Scholar]
- 184.Romme EA, Murchison JT, Phang KF, et al. Bone attenuation on routine chest CT correlates with bone mineral density on DXA in patients with COPD. J Bone Miner Res. 2012;27(11):2338–43. doi: 10.1002/jbmr.1678. [DOI] [PubMed] [Google Scholar]
- 185.Bon J, Fuhrman CR, Weissfeld JL, et al. Radiographic emphysema predicts low bone mineral density in a tobacco-exposed cohort. Am J Respir Crit Care Med. 2011;183(7):885–90. doi: 10.1164/rccm.201004-0666OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Bon JM, Leader JK, Weissfeld JL, et al. The influence of radiographic phenotype and smoking status on peripheral blood biomarker patterns in chronic obstructive pulmonary disease. PLoS One. 2009;4:e6865. doi: 10.1371/journal.pone.0006865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ohara T, Hirai T, Muro S, et al. Relationship between pulmonary emphysema and osteoporosis assessed by CT in patients with COPD. Chest. 2008;134(6):1244–9. doi: 10.1378/chest.07-3054. [DOI] [PubMed] [Google Scholar]
- 188.Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011;7:CD000333. doi: 10.1002/14651858.CD000333.pub2. [DOI] [PubMed] [Google Scholar]
- 189.Leuppi JD, Schuetz P, Bingisser R, et al. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA. 2013;309(21):2223–31. doi: 10.1001/jama.2013.5023. [DOI] [PubMed] [Google Scholar]
- 190.Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet. 2007;370:657–66. doi: 10.1016/S0140-6736(07)61342-7. [DOI] [PubMed] [Google Scholar]
- 191.Bischoff-Ferrari HA. Vitamin D and Fracture Prevention. Endocrinol Metab Clin North Am. 2010;39:347–53. doi: 10.1016/j.ecl.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 192.Boland R. Role of vitamin D in skeletal muscle function. Endocr Rev. 1986;7:434–47. doi: 10.1210/edrv-7-4-434. [DOI] [PubMed] [Google Scholar]
- 193.Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143:1129–36. doi: 10.1093/oxfordjournals.aje.a008690. [DOI] [PubMed] [Google Scholar]
- 194.Bischoff-Ferrari HA, Willett WC, Orav EJ, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;367(1):40–9. doi: 10.1056/NEJMoa1109617. [DOI] [PubMed] [Google Scholar]
- 195.Avenell A, Gillespie WJ, Gillespie LD, O’Connell DL. Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev. 2009;15(2):CD000227. doi: 10.1002/14651858.CD000227.pub3. [DOI] [PubMed] [Google Scholar]
- 196.Reginster JY. Antifracture efficacy of currently available therapies for postmenopausal osteoporosis. Drugs. 2011;71(1):65–78. doi: 10.2165/11587570-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 197.Lewiecki EM. Safety of long-term bisphosphonate therapy for the management of osteoporosis. Drugs. 2011;71(6):791–814. doi: 10.2165/11585470-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 198.Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc. 2008;83(9):1032–45. doi: 10.4065/83.9.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Amin D, Cornell SA, Gustafson SK, et al. Bisphosphonates used for the treatment of bone disorders inhibit squalene synthase and cholesterol biosynthesis. J Lipid Res. 1992;33(11):1657–63. [PubMed] [Google Scholar]
- 200.Pazianas M, van der Geest S, Miller P. Bisphosphonates and bone quality. Bonekey Rep. 2014;3:529. doi: 10.1038/bonekey.2014.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lozano-Calderon SA, Colman MW, Raskin KA, Hornicek FJ, Gebhardt M. Use of bisphosphonates in orthopedic surgery: pearls and pitfalls. Orthop Clin North Am. 2014;45(3):403–16. doi: 10.1016/j.ocl.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 202.Bilezikian JP. Efficacy of bisphosphonates in reducing fracture risk in postmenopausal osteoporosis. Am J Med. 2009;122(2 suppl):S14–21. doi: 10.1016/j.amjmed.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 203.Smith BJ, Laslett LL, Pile KD, et al. Randomized controlled trial of alendronate in airways disease and low bone mineral density. Chron Respir Dis. 2004;1(3):131–7. doi: 10.1191/1479972304cd025oa. [DOI] [PubMed] [Google Scholar]
- 204.Jansen JP, Bergman GJ, Huels J, Olson M. The efficacy of bisphosphonates in the prevention of vertebral, hip, and nonvertebral-nonhip fractures in osteoporosis: a network meta-analysis. Semin Arthritis Rheum. 2011;40(4):275–84. e1–2. doi: 10.1016/j.semarthrit.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 205.Bone HG, Hosking D, Devogelaer JP, et al. Alendronate Phase III Osteoporosis Treatment Study Group Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med. 2004;350:1189–99. doi: 10.1056/NEJMoa030897. [DOI] [PubMed] [Google Scholar]
- 206.Watts NB, Diab DL. Long-term use of bisphosphonates in osteoporosis. J Clin Endocrinol Metab. 2010;95:1562. doi: 10.1210/jc.2009-1947. [DOI] [PubMed] [Google Scholar]
- 207.Blick SK, Dhillon S, Keam SJ. Teriparatide: a review of its use in osteoporosis. Drugs. 2008;68(18):2709–37. doi: 10.2165/0003495-200868180-00012. [DOI] [PubMed] [Google Scholar]
- 208.Whitfield JF, Morley P, Willick GE. Parathyroid hormone, its fragments and their analogs for the treatment of osteoporosis. Treat Endocrinol. 2002;1(3):175–90. doi: 10.2165/00024677-200201030-00005. [DOI] [PubMed] [Google Scholar]
- 209.Saag KG, Zanchetta JR, Devogelaer JP, et al. Effects of teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: thirty-six-month results of a randomized, double-blind, controlled trial. Arthritis Rheum. 2009;60:3346–55. doi: 10.1002/art.24879. [DOI] [PubMed] [Google Scholar]
- 210.Saag KG, Shane E, Boonen S, et al. Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med. 2007;357:2028–39. doi: 10.1056/NEJMoa071408. [DOI] [PubMed] [Google Scholar]
- 211.Moen MD, Keam SJ. Denosumab: a review of its use in the treatment of postmenopausal osteoporosis. Drugs Aging. 2011;28(1):63–82. doi: 10.2165/11203300-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 212.Scott LJ. Denosumab: a review of its use in postmenopausal women with osteoporosis. Drugs Aging. 2014;31:555–76. doi: 10.1007/s40266-014-0191-3. [DOI] [PubMed] [Google Scholar]
- 213.Tsai JN, Uihlein AV, Lee H, et al. Teriparatide and denosumab, alone or combined, in women with postmenopausal osteoporosis: the DATA study randomised trial. Lancet. 2013;382(9886):50–6. doi: 10.1016/S0140-6736(13)60856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Tsai JN, Uihlein AV, Burnett-Bowie SM, et al. Comparative Effects of Teriparatide, Denosumab, and Combination Therapy on Peripheral Compartmental Bone Density, Microarchitecture, and Estimated Strength: the DATA-HRpQCT Study. J Bone Miner Res. 2015;30(1):39–45. doi: 10.1002/jbmr.2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Lehouck A, van Remoortel H, Troosters T, Decramer M, Janssens W. COPD and bone metabolism: a clinical update. Rev Mal Respir. 2010;27(10):1231–42. doi: 10.1016/j.rmr.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 216.Mazokopakis EE, Starakis IK. Recommendations for diagnosis and management of osteoporosis in COPD men. ISRN Rheumatol. 2011;2011:901416. doi: 10.5402/2011/901416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Grossman J, Gordon R, Ranganath VK, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2010;60(11):1515–26. doi: 10.1002/acr.20295. [DOI] [PubMed] [Google Scholar]
- 218.Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19(4):385–97. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Langhammer A, Forsmo S, Syversen U. Long-term therapy in COPD: any evidence of adverse effect on bone? Int J Chron Obstruct Pulmon Dis. 2009;4:365–80. doi: 10.2147/copd.s4797. [DOI] [PMC free article] [PubMed] [Google Scholar]