Abstract
Patients with Morquio syndrome possess a number of characteristics which may complicate an anaesthetic procedure. The most important is that a deposition of mucopolysaccharides in the soft tissues of the oro-pharynx distorts the airway, making the airway management difficult, while the atlanto-axial instability puts these patients at risk of subluxation and quadriparesis.
As the endotracheal intubation in Morquio syndrome patients may be difficult or even impossible, we recommend the technique of awake fiberoptic intubation to be considered.
Our approach to awake fiberoptic intubation in an adult patient is described in this case report.
KEY WORDS: Morquio syndrome, mucopolysaccharidosis, neck instability, general anesthesia, fiberoptic intubation
INTRODUCTION
The mucopolysaccharidoses (MPS) are a family of lysosomal storage diseases that result in abnormal accumulation of glycosaminoglycans throughout the body. There is a broad spectrum in severety of expression of the musculoskeletal and neurological manifestations of these diseases, ranging from an early and obvious presentation, with rapid degeneration and death, to a nearly asymptomatic phenotype and normal life expectancy [1]. The Morquio–Brailsford syndrome, known as mucopolysaccharidosis type IV (MPS IV), is listed as a “rare disease” by the Office of Rare Diseases of National Institutes of Health, with a prevalence of 1/200 000-250 000 people. This deficiency leads to accumulation of keratin sulfate and chondroitin-6-sulfate in connective tissue, skeletal system und teeth [2]. Infiltration of the tissues may lead to anaesthetic problems. This includes distortion of upper airway anatomy with a large tongue and dental abnormalities which makes the endotracheal intubation difficult or impossible [3, 4]. Spinal abnormalities are common. Atlantoaxial instability with resultant myelopathy and spastic quadriparesis has been described in both, MPS IV and MPS VI. Cervical fixation at the occiput–to-C2 level is frequently needed in these patients and in fact profilactic occipito-cevical fusion has been strongly advocated for patients with Morquio syndrome independent of neurological symptoms [1, 5]. Cardiac abnormalities may be present. Aortic regurgitation is the most commonly observed valvular abnormality in patients with Morquio syndrome. However, few reports have been published describing cardiac surgery in patients with mucopolisaccharidosis, including Morquio syndrome, because valve disease becomes usually symptomatic only late in the course of these diseases [5]. MPS IV induced thoracic cage deformity, kyphoscoliosis, may reduce the long volumes and cause ventilation-perfusion mismatch [6]. Unlike other forms of mucopolysaccharoidoses, MPS IV patients have and retain normal intelligence throughout life [1]. As the patients with mucopolysaccharoidosis are being referred to hospital for surgery more frequently compared to average population, it is important to gain basic knowledge of the disease in spite of the low incidence of the syndrome [7]. An (art adapted) photo of a typical Morquio syndrome patient is attached as Figure 1.
FIGURE 1.

An art adapted photo of a typical Morquio syndrome patient by Peter Romberg
CASE REPORT
A 31 year old man, with Morquio syndrome presented at our Orthopaedic Department with the pain on the hips, limiting his walking ability to maximally 10 minutes. Bilateral coxarthrosis with deformity of the joints was diagnosed. A unilateral, total hip replacement had to be performed on the right side first and after the period of revalidation, on the left, as well. His length was 170 cm and weight 79 kg. The patient had a large head which seemed to be positioned on his thorax because of extremely short neck. Inspection of the mouth showed a large tongue with a Mallampati score III. Past history revealed cervical stabilization by the posterior spondylodesis C0-C2. Recent radiological investigation of cervical spine detected abnormal shape and insufficient height of vertebral corpora and some degenerative changes (Figure 2. and 3.) Radiological examination of lumbar spine showed typical scoliosis and torsion, with low height and wide corpora. Cardiology report was normal and the lung function test revealed slight diffusion problems. He used no other drugs except pain medication (paracetamol and diclofenac). During preoperative evaluation it became clear that unsuccessful spinal anaesthesia for a recent minor procedure precluded use of this technique again. The remaining option was awake (sedated) fiberoptic intubation (AFI). Every step of AFI was explained to the patient and emphasized the importance of his cooperation. Enough time was planned for the preparations. The patient was given an infusion and connected to standard monitoring. To relieve the anxiety and to achieve some amnesia, 2 mg of midazolam was given intravenously. As it may prove very difficult (or impossible) to accomplish an oral AFI intubation, due to a narrow space between the large tongue and the pharynx wall and the sharp angle that has to be made by the scope towards the glottic opening, we prepared the nasal route as well. A vasoconstrictor, 0,5% xilometazoline nose drops were given first, followed by 2% lidocaine gel (2 cm) in each nostril. The tongue and the pharynx were prepared by spraying 4-6 ml of 2% lidocaine. After a few minutes it was possible to place de tong depressor deep enough to anesthetize the back of the tong and pharynx wall by spraying another 4-6 ml of 2% lidocaine spray, asking the patient to take a deep breath simultaneously. We avoid higher concentration of local anesthetic because it causes more irritation of the mucosa. After a few more minutes we checked the sensitivity of nasal and pharyngeal surface by touching it. Patient felt no discomfort and an Ovassapian intubating oro-pharyngeal airway was inserted easily. Nasal oxygen prongs were placed with the flow of 3 liter /min. Intravenous sedation was started by propofol continuous infusion 2mg/kg and remifentanyl 0,05 μg/kg/min. Antisialogog, atropine 0,5 mg was administered intravenously. The patient continued to breath spontaneously, felt comfortable and remained cooperative. The fiberscope was prepared so that an epidural catheter (with three standard side-openings at the end) was threaded via the working channel to be used for spraying the vocal cords. The fiberscope was passed via the intubating airway and the vocal cords appeared in view after some chin-lift maneuver. We used spray-as-you-go technique to anesthetize the vocal cords with 2 ml of 2% lidocaine. That provoked some coughing. After waiting for about 30 seconds, the fiberscope was passed through the glottis until the carina and the endotracheal tube railroaded to trachea. The tube position was confirmed by auscultation and capnography and general anesthesia induced. The operation was uneventful and awake extubation followed.
FIGURE 2.
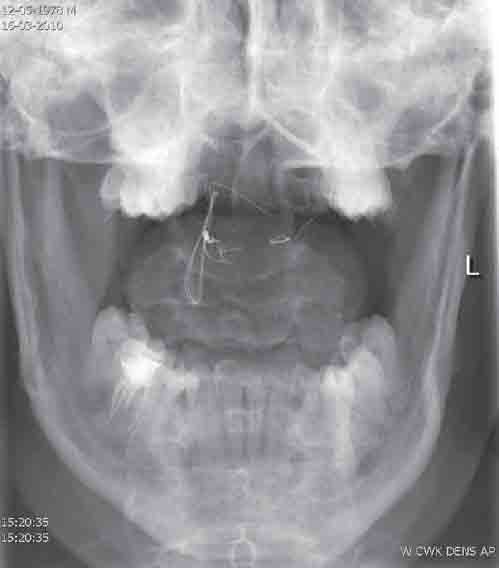
RTG photo of dens, preoperative.
FIGURE 3.

RTG photo of cervical spine, preoperative.
DISCUSSION
The Morquio –Brailsford syndrome is a progressive disorder of connective tissue. It is known as mucopolysac-charidosis type IV. The various enzymatic defects lead to accumulation of keratin sulfate and chondroitin-6-sulfate in connective tissue, skeletal system und teeth, brain, heart, liver, spleen and tracheobronchial tree, leading to characteristic physical appearance and resulting in end-organ disfunction [2]. The basic diagnostic test is the detection of excessive amount of these substances in urine. The airway issues by patients with Morquio syndrome are frequently complicated by cervical spine instability and the risk of subluxation (cord trans-section in a child reported in literature) [2]. Radiological investigation should be performed before the operation and the problems discussed with the radiologist and neurosurgeon, in case of elective surgery. In case of an emergency, the approach to the airway and the cervical spine should follow the guidelines used for patients with suspected cervical spine injury (rigid collar). The neck fixation increases the difficulty of the airway management. In addition to the airway issues, preoperative pulmonary testing should be performed in these patients. Respiratory function can be compromised by chronic respiratory disease, recurrent pulmonary infections, obstructive sleep apnea and kyphoscoliosis leading to restrictive lung. Cardiac infiltration may lead to myocardial dysfunction, coronary artery lesions and valvular dysfunction. The most important problems concerning the airway management are based on intracellular accumulation of mucopolysaccharides resulting in macroglossia, limited mouth opening due to involvement of temporo-mandibular joints, short neck and subglotic narrowing. These elements may lead to “cannot intubate -cannot ventilate situation” [2]. Oral fiberoptic technique might be difficult due to large, heavy, anteriorly placed, “hanging epiglotis” (sometimes resting on the tong base) making the passage of the fibrescope towards the glotic opening impossible. Nasal fiberoptic technique is strait forward, but might be difficult related to mucopolisaccharoide infiltration in the nasopharynx, with the increased risk of bleeding. Careful preoperative airway examination should be done to predict and evaluate the possible problems. When the airway risk is present, loco-regional technique should be applied if possible. However, the use of spinal anesthesia can be difficult due to progressive scoliosis. Also the optimal dose of local anesthetic is difficult to predict due to (heavy) growth retardation in some of these patients. Regardless of the technique chosen, all necessary equipment to deal with difficult airway should be readily available in case of complications or failure. There is also a controversy about the appropriate means of induction. Some anaesthesiologists prefer the use of intravenous and others of inhalational agents (especially in children), but most of the authors suggest to avoid the use of muscle-relaxants. The relaxation of the supraglottic tissue may preclude effective bag-mask ventilation [3]. Endo-tracheal intubation using fiberoptic technique, being minimally invasive and allowing neutral head position is strongly recommended in these patients [4]. Attention to maximize the respiratory function postoperative is essential to avoid the obstruction and postoperative respiratory failure.
CONCLUSION
In conclusion, we recommend the technique of awake, fiberoptic intubation to be considered in adult patients with Morquio syndrome. Oral fibreoptic approach, as less traumatic, should be the first choice, keeping in mind that nasal route might be needed, and should be prepared as well. We strongly recommend not to use muscle relaxants, as they may impair the efficacy of a bag-mask ventilation, leading to can-not -intubate can-not-ventilate situation.
DECLARATION OF INTERESTS
There are no competing interests amongst the authors and there is not going to be any forthcoming presentation.
REFERENCES
- [1].White KK, Steinman S, Mubarak SJ. Cervical stenosis and spastic quadriparesis in Morquio disease (MPS IV). A case report with twenty-six-year follow-up. J Bone Joint Surg Am. 2009;91(2):438–442. doi: 10.2106/JBJS.H.00148. [DOI] [PubMed] [Google Scholar]
- [2].Gösele S, Dithmar S, Holz FG, Völcker HE. Late diagnosis of Morquio syndrome. Clinical histopathological findings in a rare mucopolysaccharidosis. Klin Monbl Augenheilkd. 2000;217(2):114–117. doi: 10.1055/s-2000-10394. [DOI] [PubMed] [Google Scholar]
- [3].Tobias JD. Anesthetic care for the child with Morquio syndrome: general versus regional anesthesia. J Clin Anesth. 1999;11(3):242–246. doi: 10.1016/s0952-8180(99)00007-0. [DOI] [PubMed] [Google Scholar]
- [4].McLaughlin AM, Farooq M, Donnelly MB, Foley K. Anaesthetic considerations of adults with Morquio's syndrome - a case report. BMC Anesthesiol. 2010 Feb 26;10:2. doi: 10.1186/1471-2253-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Pagel PS, Almassi GH. Perioperative implications of Morquio syndrome in a 31-year-old woman undergoing aortic valve replacement. J Cardiothorac Vasc Anesth. 2009;23(6):855–857. doi: 10.1053/j.jvca.2008.12.009. [DOI] [PubMed] [Google Scholar]
- [6].Morgan KA, Rehman MA, Schwartz RE. Morquio's syndrome and its anaesthetic considerations. Paediatr Anaesth. 2002;12(7):641–644. doi: 10.1046/j.1460-9592.2002.00838.x. [DOI] [PubMed] [Google Scholar]
- [7].Bartz HJ, Wiesner L, Wappler F. Anaesthetic management of patients with mucopolysaccharidosis IV presenting for major orthopaedic surgery. Acta Anaesthesiol Scand. 1999;43(6):679–683. doi: 10.1034/j.1399-6576.1999.430614.x. [DOI] [PubMed] [Google Scholar]


