Abstract
Purpose: To investigate associations between fear of falling (FOF) and recurrent falls among women and men, and gender differences in FOF with respect to International Classification of Functioning (ICF). Methods: Community-dwelling people (n = 230, 75–93 years, 72% women) were included and followed 1 year regarding falls. Data collection included self-reported demographics, questionnaires, and physical performance-based tests. FOF was assessed with the question “Are you afraid of falling?”. Results were discussed with a gender relational approach. Results: At baseline 55% women (n = 92) and 22% men (n = 14) reported FOF. During the follow-up 21% women (n = 35) and 30% men (n = 19) experienced recurrent falls. There was an association between gender and FOF (p = 0.001), but not between FOF and recurrent falls (p = 0.79), or between gender and recurrent falls (p = 0.32). FOF was related to Personal factors and Activity and Participation. The relationship between FOF and Personal factors was in opposite directions for women and men. Conclusions: Results did not support the prevailing paradigm that FOF increases rate of recurrent falls in community-dwelling people, and indicated that the answer to “Are you afraid of falling?” might be highly influenced by gendered patterns.
Implications for Rehabilitation
The question “Are you afraid of falling?” has no predictive value when screening for the risk of falling in independent community-dwelling women or men over 75 years of age.
Gendered patterns might influence the answer to the question “Are you afraid of falling?” Healthcare personnel are recommended to be aware of this when asking older women and men about fear of falling.
Keywords: Falls, fear, gender, ICF, older people
Introduction
Falls among older people represent a major cause of injury-related hospitalization and mortality [1,2]. More than one third of community-dwelling adults older than 65 years suffer from falls each year [1–3], and the rate of falls rises steadily with age [4–6]. In most studies, it has been shown that older women are at higher risk for falls and recurrent falls than are older men [2,6–8]. Consequences of a fall can be devastating for the individual and impose significant costs on society. Falls prevention in older populations has therefore become an important area of research and practice [1].
Apart from physical injuries, many seniors suffer from psychological consequences such as a concern of repeated falls, which is conceptualized as a fear of falling (FOF) [9,10]. This concern could also appear in older people who have not previously fallen [11,12]. FOF is considered an independent risk factor for future falls [2], especially recurrent falls, in older people living at home [13]. Factors associated with FOF are: inability to rise from a chair, lower household income, use of a walking aid, poor self-reported health and balance problems, and lower educational level [14]. If excessive, FOF might lead to sedentary behaviour, social isolation, physical decline, and depression [15]. However, a concern about falling might also act as a protective factor when it leads to developing positive fall prevention coping skills, such as cautious gait on icy surfaces [8,9,16]. The reported prevalence of FOF among community-dwelling older people ranges between 12% and 65% [11]. A number of reports have stated that FOF is consistently more common in women [12,17,18]. In fact, this belief is so well established that some authors have excluded men from their research on FOF [15,19,20]. This could lead to the impression that female sex predisposes a person for developing FOF, and the exclusion of men in studies supports the belief that men are not concerned about falling. In this study, we have taken a gender perspective to further our understanding of gender differences when it comes to FOF.
According to gender relational theory, being a man or a woman is a dynamic construction shaped in interaction with other people [21]. The perceptions of manhood and womanhood, labelled masculinities and femininities, are constantly shaped and reshaped according to social expectations and, therefore, can change over a person's lifetime. Masculinities and femininities also shape health behaviours and experiences of health conditions [22,23]. For example, a dominant masculine ideal is that of the physically strong and independent man [24]. Men with this masculinity pattern are more likely to engage in competitive and risk-taking behaviour and less likely to seek help for physical ailments [22,25]. However, one needs to acknowledge that there are large variations among men just as there are variations among women. Gendered patterns are influenced by biological conditions, such as genes and hormones, as well as social classifications, such as ethnicity, class and age [21,22].
Advancing age adds a dimension to life that brings loss of function and resources and shapes health behaviours in interaction with gender relations [22]. Ageing normally leads to role transitions and shifts in social positions in different arenas such as leisure time, partnerships, or housekeeping [26]. Socio-economic factors also influence social positions in old age. For women, a shift in social position might be caused by a small pension when entering retirement because they are more likely to have worked in lower paid jobs than men. This might give them fewer opportunities to engage in leisure time activities [22,27]. In addition, women's retirement is often characterized by a continuation of domestic labour [28]. Despite this, older women in most cultures have been shown to increase their interest in health-promoting behaviours such as exercising and healthy eating [29].
Integrating a gender relational theory into health research of old age might deepen the understanding about gender differences, as well as similarities, and guide development of more effective interventions [21,25,30].
The biopsychosocial model of the International Classification of Functioning, Disability, and Health (ICF) [31] provides a useful framework for understanding the multi-factorial nature of falls and FOF [32,33]. This model offers a way to describe health and health-related conditions in which a person's functioning and disability are conceived as a dynamic interaction between different health conditions. The model reflects positive and negative aspects within the following components [31,34]: Body functions and structures – the anatomical and physiological parts of the body; Activity – the execution of tasks or actions; Participation – involvement in life situations; Personal factors – an individual's particular life background; and Environmental factors – the physical and social environment [31].
The purpose of the current study was to investigate the associations between FOF and recurrent falls among community-dwelling women and men aged 75 years and older and to investigate gender differences in FOF with respect to the components of the ICF. Results were interpreted with a gender relational approach.
Methods
Participants and recruitment
Cross-sectional and longitudinal data were collected as part of a project between 2004 and 2006 in a city in northern Sweden [35]. Briefly, participants were solicited through advertisements in the local press, senior citizen organizations, and primary care clinics. In total, 230 adults aged 75–93 years met the inclusion criteria of age ≥75 years, community-dwelling, ability to walk at least 10 m without support, and a score of ≥24 on the Mini-Mental State Examination. The study was approved by the Regional Ethical Review Board in Umeå (Dnr 2010/04-071 M).
Measurements and variables
Baseline assessments included self-reported demographics, health complaints, medication use, questionnaires, and physical tests. Bone mass density was assessed by dual-energy X-ray absorptiometry (DXA) [36] (Table 1).
Table 1.
Description of the variables included in the statistical analyses.
| ICF | Variable | Standardized assessment or question and further information |
|---|---|---|
| Personal factors | Age | Self-reported, confirmed by national register, 75–93 years |
| Educational level | Three levels: 1 = ≤6 years, 2 = 7–9 years, 3 = ≥10 years | |
| Experienced falls | Self-reported fall events in the past year: 0 = no falls, 1 = 1 fall, 2 = ≥2 falls | |
| Experienced fractures | Self-reported fractures in the past 5 years: 0 = no fractures, 1 = 1 fracture, 2 = ≥2 fractures | |
| Perceived confidence of one's balance | Activities-specific Balance Confidence (ABC) scale [37]: 0–100 %: higher score indicates more self-reported balance confidence in 16 daily activities of greater or lesser challenge during position changes or walking | |
| Eating habits | Mini Nutritional Assessment [60]: 0–30 points: higher score indicates better self-reported nutritional status | |
| Emotional distress/ depressive symptoms | Geriatric Depression Scale 15 items [61]: (0–15 points): scores ≥5 points indicate depression might be present | |
| Other health conditions/comorbidities | Twenty self-reported comorbidities that might cause fall events: arthritis, stroke, Parkinson's disease, diabetes mellitus, lung diseases, heart diseases, cancer, hypertension, inflammatory bowel syndromes, thyroid disease, anaemia, B-vitamin deficiency, kidney diseases, epilepsy, depression, eye diseases, osteoarthritis in knees or feet, normal pressure hydrocephalus, polyneuropathy, leg ulcers | |
| Environmental factors | Residence | Self-reported: 1 = cottage/bungalow, 2 = apartment, 3 = senior living/sheltered housing |
| Living circumstances | Self-reported: 0 = living with another person(s), 1 = living alone | |
| Walking device | Self-reported: 0 = no device, 1 = use device indoors or outdoors | |
| Medication | Prescription drugs considered to be fall risk factors (calcium preparations, potassium sparing diuretics, oxicams, anilides, anxiolytics and hypnotics [benzodiazepine derivatives], and thiazides): 0 = no drugs, 1 = one risk drug, 2 = ≥2 risk drugs | |
| Clothing | Foot wear at home: 0 = shoes, 1 = slippers, 2 = bare feet or socks | |
| Attitude of others | Response to question: “Do you think somebody else is afraid that you might fall?”: 0 = no, 1 = I don't know, 2 = yes | |
| Body function and structure | Bone mineral density | Dual-energy X-ray absorptiometry at hip and spine [36]: 0 = normal bone density, 1 = osteopenia, 2 = osteoporosis |
| Dual-task cost in step width, counting backwards | A change in step width of 3.6 mm or more while counting backwards predicts falls [35]: 0 = ≤3.6 mm, 1 = >3.6 mm | |
| Dual-task cost in step width, carrying an object | A change in step width of 3.7 mm or less while carrying an object predicts falls [35]: 0 = ≥3.7 mm, 1 = <3.7 mm | |
| Trail Making Test B | Interval scale (time in seconds): higher score indicates slower performance [62] | |
| Attentional functions | Response to questions: “Do you need to think about being careful when walking:… indoors?… outdoors in the summer when on even ground?… on uneven ground?… during the winter on snowy ground?”: 0 = never/rarely, 1 = sometimes, 2 = often/always | |
| Cognitive state | Mini Mental State Examination [63], 0–30 points, higher score indicates better cognitive function | |
| Dizziness | For any reason: 0 = yes, 1 = no | |
| Sensation of falling | Response to questions “Do you feel unsteady when walking indoors?” and “… outdoors?”: 0 = never/rarely, 1 = sometimes, 2 = often/always | |
| Sensory functions: Visual acuity [64] | 1 = excellent, 2 = good, 3 = fair, 4 = poor | |
| Visual contrast [64] | 1 = excellent, 2 = good, 3 = fair, 4 = poor | |
| Hearing, subjective | Self-reported: 0 = normal, 1 = impaired | |
| Hearing, objective | As perceived by trained assessor using normal speaking tone: 0 = normal, 1 = impaired | |
| Touch | Monofilament 5.07 on sole of feet and lateral malleolus: 0 = normal, 1 = impaired | |
| Proprioception | Protractor placed between lower limbs, impaired if degrees differed between the positions of left and right big toes with eyes closed and feet up, mean of 5 trials: 1 = good, <2 degrees, 2 = between 2–4 degrees, 3 = impaired, >4 degrees | |
| Vibration | 128 Hz tuning fork at lateral malleolus and tibial tuberosity: 0 = normal, 1 = impaired | |
| Activity and Participation | Activities of Daily Living | Barthel Index [65], ordinal scale (0–20 points), higher score indicates higher level of independence |
| Basic mobility | Timed Up and Go [66], interval scale (time in seconds): higher score indicates slower performance in standing up, walking 3 m, walking back and sitting down | |
| Activity avoidance | Survey of Activities and Fear of Falling in the Older [38], ordinal scale (17–51 points): higher score indicates greater avoidant behaviour | |
| Maintaining upright position | Standing balance [67], ordinal scale (0–4 points): 0 = standing < 10 s with feet together, 1 = standing ≥10 s with feet together, 2 = standing in semi-tandem-position ≥10 s, 3 = standing in tandem-position 3–9.99 s, 4 = standing in tandem-position ≥10 s | |
| Changing position | 5 x Sit-to-Stand [68], interval scale (time in seconds): higher score equals a slower performance in standing up and sitting down | |
| Walking | Gait speed over 2.4 m [67], normal speed, interval scale (time in seconds): higher score indicates slower performance in walking straight forward | |
| Physical activity level (habitual) | Self-reported [69], ordinal scale: 1 = hardly any activity, 2 = sitting down most of the time, 3 = light physical activity, 4 = strenuous physical activity approximately 1–2 h every week, 5 = strenuous physical activity at least 3 h every week | |
| Non-definable | Self-rated health | Response to the question: “In general, would you say your health is excellent, very good, good, fair or poor?”, ordinal scale: 1 = excellent, 2 = very good, 3 = good, 4 = fair, 5 = poor |
Health complaints could be specific diseases such as heart failure or diabetes or subjective complaints such as dizziness. FOF was assessed by the single-item question “Are you afraid of falling?” with a three-category response scale (rarely/never, sometimes, or often/always). In addition, the participants completed the Activities-specific Balance Confidence scale (ABC) [37], the Survey of Activities and Fear of Falling in the Elderly (SAFFE) [38], and a global self-rated health questionnaire. For the last item the options were very poor, poor, fair, good and very good. Several physical performance-based tests were performed as well as assessments of sensory functions. The participants were also asked if they had fallen in the past year. In total, 44 variables were categorized into the components of the ICF in accordance with suggested linking rules [34,39] (Figure 1). A decision was made to combine the two components Activity and Participation into one factor (Activity and Participation) because they are associated with each other and some of the measurements could be linked to both. This approach has also been supported by the WHO when categories seem to overlap [31].
Figure 1.
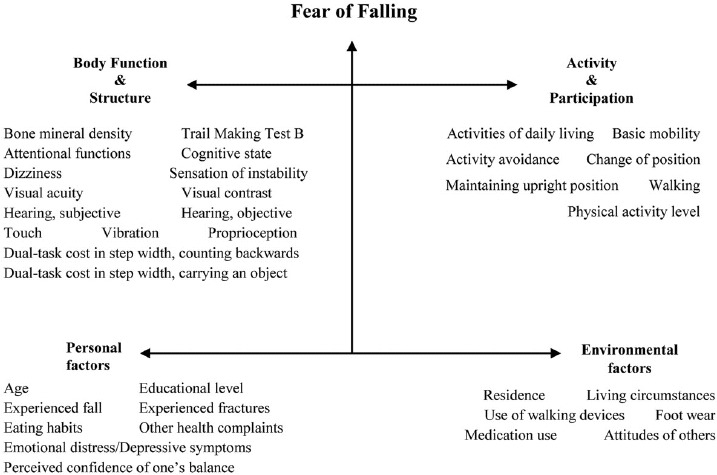
All fall risk factors organized in the model of International Classification of Functioning, Disability and Health (n = 44).
Gender is usually categorized within Personal factors, but we used gender as a grouping variable and, therefore, did not categorize gender. Global self-rated health has not been categorized in the ICF and was not included as an indicator of any latent variables. It was instead modelled as having a direct effect on FOF. All assessments were performed in a standardized manner by a skilled study physiotherapist at a research centre assisted by other physiotherapists, physiotherapy students in their final semester, a biomedical scientist, and a study nurse.
Falls were recorded by the participants with monthly calendars and reported every month for the 12 months following the baseline assessment. If the calendar was not returned on time, the participant was contacted by telephone. A fall was defined as “inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional changes in position to rest on furniture, walls or other objects” [8]. This study focuses on recurrent falls, defined as at least two falls within a 12-month period [40].
Statistical analyses
Data were analysed using SPSS including Analysis of Moment Structures (AMOS) version 19.0 for Windows (IBM SPSS Inc., Chicago, IL). A p value of 0.05 was considered to be statistically significant. People who fell once during follow-up were grouped with people who had not fallen. Thus, zero or one falls were compared to recurrent (≥ 2) falls.
Exploratory group-wise comparisons were performed using the Mann–Whitney U-test for continuous variables and the χ2 test for categorical variables. Relationships between FOF, recurrent falls, and gender were examined using a log-linear analysis of associations where FOF was dichotomized as yes (always/often/sometimes) or no (rarely/never).
A structural equation model (SEM) was used to investigate the relationships between FOF and the components of ICF in women and men. The first stage of SEM is to establish an acceptable measurement model, and then directional paths are added to form the structural model.
The measurement model, ICF
Confirmatory factor analysis (CFA) was used to assess the measurement model (ICF) by relating the observed measures to the factors, in this case the components of ICF [41]. All observed measures were adapted so that 0 equalled worst possible. To be able to uniquely estimate other parameters in the model, one factor loading for each latent variable was set to 1. These were selected based on prior considerations regarding the latent variable. In Personal factors, we selected the ABC indicator (perceived confidence of one's balance) to be set to 1; in Environmental factors we selected living circumstances; in Body function and structure we selected dizziness; and in Activity and Participation we selected the SAFFE (activity avoidance).
To evaluate model fit, goodness-of-fit was assessed with the ratio between χ2 and degree of freedom (CMIN/df) and with the root mean squared error of approximation (RMSEA). CMIN/df ratios in the range of 2 to 1 or 3 to 1 have been suggested to indicate an acceptable fit between the model and the sample data [42]. The RMSEA measures the difference between a specified model and the collected data. It has been suggested that RMSEA ≤0.05 indicates a good fit to the data, RMSEA ≤ 0.08 indicates an acceptable fit, and RMSEA ≥0.10 should not be accepted [43].
Structural equation model
After the measurement model was established, the relationships between the components of ICF (the factors) and FOF were investigated with the SEM, to provide estimates of the associations between the factors and FOF with regression weights. This method is widely used and permits the use of factors and allows relationships to be modelled simultaneously among multiple variables [41,44]. A multi-group approach with gender as the grouping variable was used to investigate which factors were related to FOF for women and men and the direction (positive or negative) of the relationships using the same structural model.
Results
Details of participant characteristics are presented in Table 2.
Table 2.
Baseline demographic and performance-based tests.
| Women (n = 166) | Men (n = 64) | p Value | |
|---|---|---|---|
| Indicators of personal factors | |||
| Age (years), mean (SD) | 79.6 (3.6) | 79.3 (4.0) | 0.559 |
| Education ≤6 years, n (%) | 55 (33) | 19 (30) | 0.647 |
| History of falls past year, n (%) | 87 (52) | 39 (61) | 0.244 |
| History of fracture past five years, n (%) | 85 (51) | 10 (16) | <0.001 |
| Activities-specific Balance Confidence scale 0–100%, mean (SD) | 73 (1.9) | 82 (1.8) | <0.001 |
| Mini Nutritional Assessment, mean (SD) | 26 (2.4) | 27 (2.1) | 0.005 |
| Geriatric Depression Scale 15 items, 0–15 points, mean (SD) | 2 (2.1) | 1 (1.5) | 0.061 |
| Number of health complaints, mean (SD) | 2 (1.3) | 2 (1.2) | 0.079 |
| Indicators of environmental factors | |||
| Living in a house, n (%) | 46 (28) | 41 (64) | <0.001 |
| Living alone, n (%) | 110 (66) | 13 (20) | <0.001 |
| Uses walking device, n (%) | 67 (40) | 14 (21.9) | 0.009 |
| Uses ≥1 prescription druga, n (%) | 86 (52) | 19 (30) | 0.003 |
| Barefoot or socks indoors, n (%) | 21 (13) | 19 (30) | 0.002 |
| Others express concern about fall risk, n (%) | 100 (60) | 41 (64) | 0.432 |
| Indicators of body function & body structure | |||
| Osteoporosis or osteopenia, n (%) | 126 (82) | 38 (61) | 0.001 |
| Dual-task cost step width while counting backwards ≥3.6 mm, n (%) | 109 (80) | 40 (71) | 0.188 |
| Dual-task cost step width while carrying an object ≤3.7 mm, n (%) | 35 (21) | 11 (17) | 0.508 |
| Trail Making Test B (seconds), mean (SD) | 161 (55.4) | 161 (52.4) | 0.979 |
| Impaired visual acuity, n (%) | 14 (9) | 4 (6) | 0.565 |
| Impaired visual contrast, n (%) | 45 (29) | 14 (23) | 0.276 |
| Impaired hearing, in own opinion, n (%) | 11 (8) | 7 (13) | 0.340 |
| Impaired hearing, in observers opinion, n (%) | 161 (98) | 61 (95) | 0.372 |
| Impaired touch on soles of feet, n (%) | 42 (25) | 13 (20) | 0.427 |
| Impaired proprioception, n (%) | 58 (35) | 20 (31) | 0.596 |
| Impaired vibration malleolus, n (%) | 87 (55) | 44 (71) | 0.027 |
| Mini Mental State Examination, 0–30 points, mean (SD) | 28 (1.9) | 28 (1.7) | 0.637 |
| Chronic dizziness, n (%) | 30 (18) | 8 (13) | 0.308 |
| Often/always thinks about fall risk when… – walking indoors, n (%) | 55 (33) | 19 (30) | 0.615 |
| – walking outdoors on even ground, n (%) | 48 (29) | 8 (13) | 0.009 |
| – walking outdoors on uneven ground, n (%) | 131 (79) | 39 (61) | 0.005 |
| – walking outdoors on icy ground, n (%) | 158 (95) | 48 (75) | <0.001 |
| Often/always have a sensation of instability when… – walking indoors, n (%) | 62 (37) | 21 (33) | 0.521 |
| – walking outdoors, n (%) | 80 (48) | 26 (41) | 0.302 |
| Indicators of activity and participation | |||
| Activity of Daily Living, Barthel Index 0–20 points, mean (SD) | 20 (1) | 20 (0) | 0.029 |
| Timed Up-and-Go (seconds), mean (SD) | 10.5 (2.9) | 10.1 (2.4) | 0.354 |
| Survey of Activities and Fear of Falling in the Elderly, 17–51 points, mean (SD) | 23 (4.9) | 21 (4.3) | 0.003 |
| Impaired standing balance (<10 s feet together), n (%) | 1 (1) | 1 (2) | 0.482 |
| 5 × Sit-to-Stand (seconds), mean (SD) | 11.9 (4.0) | 11.1 (2.8) | 0.190 |
| Gait speed over 2.4 m (seconds), mean (SD) | 3.6 (1.0) | 3.7 (1.0) | 0.113 |
| Activity level summer, 0–5 points, mean (SD) | 3.8 (0.7) | 3.9 (0.9) | 0.354 |
| Activity level winter, 0–5 points, mean (SD) | 3.6 (0.7) | 3.7 (0.9) | 0.185 |
| Latent Factor: Global self-rated healthb 1–5 points, mean (SD) | 3.0 (0.8) | 2.6 (0.7) | 0.004 |
Calcium preparations, potassium sparing diuretics, oxicams, anilides, anxiolytics and hypnotics (benzodiazepine derivatives), thiazides.
1 = very poor, 2 = poor, 3 = fair, 4 = good, 5 = very good. Observed variables (indicators) are classified according to the International Classification of Functioning and Disability.
At baseline the mean age was 79.5 (SD 3.7) years with a range of 75–93 years. Among the 230 participants, 166 (72%) were women; 110 women (66%) and 13 men (20%) lived alone (p < 0.001); and 85 women (51%) and 10 men (16%) had experienced at least one fracture in the previous 5 years (p < 0.001). Of all participants, 126 of the women (82%) and 38 of the men (61%) were diagnosed with osteopenia or osteoporosis. FOF was reported by 92 of the women (55%) and by 14 of the men (22%). The distribution of responses to the question “Are you afraid of falling?” is shown in Table 3.
Table 3.
Distribution of the responses to the question “Are you afraid of falling?”.
| Responses | Women n = 166 | Men n = 64 |
|---|---|---|
| No/Yes | 74/92 | 50/14 |
| Rarely/Never | 74 (45) | 50 (78) |
| Sometimes | 54 (32) | 7 (11) |
| Often/Always | 38 (23) | 7 (11) |
Presented as numbers and proportions, n (%). “No” corresponded to Rarely/Never, and “Yes” corresponded to Sometimes and Often/Always.
After the follow-up year, 110 participants (48%) reported at least one fall event. Of them, 54 (23% of all) reported two or more fall events, in total 267 falls, including 19 men (30% of the men) and 35 women (21%). Furthermore, of the recurrent fallers, 27 (50%) reported FOF and 27 (50%) did not. Two participants reported extremely high numbers of falls; one woman fell 58 times and one man fell 49 times. The fall rate among participants was 0.1 falls per person-year excluding the two outliers.
Gender, fear of falling, and recurrent falls
The analysis confirmed a strong association between gender and FOF (women with FOF: 55% (n = 92); men with FOF: 22% (n = 14); p < 0.001). However, there was no association between FOF and recurrent falls (recurrent fallers with FOF: 50% (n = 27); recurrent fallers with no FOF: 50% (n = 27); p = 0.79) or between gender and recurrent falls (women with recurrent falls: 21% (n = 35); men with recurrent falls: 30% (n = 19); p = 0.32). The χ2 goodness-of-fit p value was 0.62, indicating that the log linear model fit the data well.
The measurement model, ICF
The CFA showed that the model fit of the ICF components was acceptable (CMIN/df = 2.7 and RMSEA = 0.086), except for the contextual factor Environmental factors. This factor did not have any significant factor loadings and, therefore, did not constitute a factor.
A higher score for the factor Personal factors was associated with longer education, better nutritional status, less experience of falls and fractures, and fewer depressive symptoms or other health complaints. Not all variables loaded significantly on this factor, and some differed between women and men. For instance, the variable age loaded significantly on this factor for men but not for women.
Almost all observed variables loaded significantly on the factor Body functions and structure for both women and men. A higher score was associated with, for example, a smaller change in step-width in walking while counting backwards; a higher speed on Trail Making Test B; and no hearing impairment. There were some sex differences. For example, the observed variable proprioception, for example, loaded significantly on the factor for men but not for women.
All variables loaded significantly on the factor Activity and participation for both women and men. A higher score on the factor indicated higher levels of independence in activities of daily living, less activity avoidance, performing well on performance-based tests, and a higher level of physical activity.
The structural equation model
Figure 2 shows the regression weights between the components of ICF (the factors) and FOF. The factor Body functions and structures and the “self-rated health” indicator did not have significant relationships to FOF. There was evidence for significant (p < 0.001) structural pathways for women and men both between the factor Activity and Participation and FOF and between the factor Personal factors and FOF.
Figure 2.
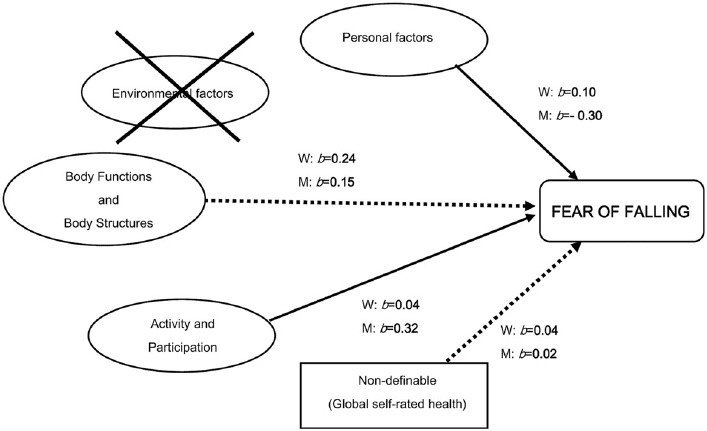
Structural equation model exploring the paths of the ICF model to Fear of Falling. The latent variables (factors) are represented by the circles. Values adjacent to arrows are regression weights, labelled as b. M = men, W = women. Solid paths are statistically significant (p < 0.001). These results provide support for the role of the ICF components Personal factors and Activity and Participation in relation to the Fear of Falling. No interrelationships between factors were tested.
The positive regression weights between Activity and Participation and FOF in both women and men indicated that a higher score on the factor meant less FOF. The relationship between Personal factors and FOF differed significantly (p < 0.001) between women and men. For women, the positive regression weight to FOF indicated that a higher (better) score on the factor yielded lower FOF. In contrast, men with a lower (worse) score on the factor reported lower FOF.
Discussion
Our study provides no evidence that FOF is an indication of increased risk of future recurrent falls, in contrast to the findings of other studies [2,7,13]. This lack of association was found in both women and men. The proportion of recurrent fallers was higher compared to many previous reports [13,45,46]. However, similar results to ours have been found by others [40,47], and even higher proportions (35%) have been reported within the same age group [48]. Our sample of volunteers was, in general, healthy and physically active and many of the participants reported spending a fair amount of time outdoors walking or bicycling, which may explain the high proportion of recurrent fallers.
Our study showed that even though a greater proportion of women reported FOF at baseline, there was no difference in the recurrence of falls between women and men during the follow-up year. This finding contradicts other studies where women have an increased risk for recurrent falls [6,7,13], but studies on recurrent falls are heterogeneous and some studies support our findings where no sex difference was found [45,46]. One explanation for the non-existing sex difference in our sample may be that many women were diagnosed with osteopenia or osteoporosis at baseline as part of the assessment. This information in itself may have influenced the women to be more careful during the following year. The same information was also given to some men, but they may have responded differently to this information, because of the idea that osteoporosis is a disease mainly affecting women. It is likely that some men do not want to acknowledge having a “woman's disease”, because of the threat to the masculine ideal.
The higher proportion of FOF in women compared to men is in agreement with other studies [12,17,18], but a certain degree of concern has been shown to protect from falls by increasing risk awareness and the adoption of safety-oriented behaviours [49]. This is confirmed by the lack of significant difference between men and women. It should, however, be noted that one in three women answered “sometimes” when asked about FOF. This could, in fact, reflect a moderate and adequate concern in relation to the actual risk of falling [10]. It is perhaps more intriguing why only 11% of the men answered “sometimes”.
In an attempt to investigate differences or similarities between women and men in a more comprehensive manner, the SEM was used with the ICF as the measurement model. Body functions and structures was not significantly related to FOF. This is surprising, because impairments in sensory functions may affect balance and gait, especially during dual-task conditions, and thus lead to FOF [14]. Even though Environmental factors (e.g. use of walking aids and psychoactive medications) have been shown to relate to a FOF, especially in women [17], this component did not constitute a factor. Two components emerged as significant in relation to FOF in both women and men: Personal factors and Activity and Participation.
Personal factors
This contextual factor includes aspects that influence individual personal characteristics, such as age, education, and previous experiences, and life-style choices.
Women and men are stereotyped across cultures. Women are considered to be more sensitive to emotions and open to feelings and to have lower self-esteem than men. In contrast, men are considered less fearful, less vulnerable, and more assertive than women. These differences have been shown to be greater in developed countries and less relevant in collectivist cultures. This indicates that they are social constructions rather than biological and, thus, are possible to change [50]. Assertiveness is strongly linked with status and largely comes from education and work roles. Historically, women's assertiveness changes over time, but men's assertiveness does not [23]. From this perspective, it could be suggested that women more easily admit to FOF than men do, because the masculinity ideal is for men to be physically strong, to be tough, and to demonstrate fearlessness and for women to be emotional and open about feelings [25]. Men have also been shown to be more likely to perceive that they have a low fall risk compared to women [51], and to express less concern for many other risks as well [52]. This fundamental attitude might influence the men's answer to the question “Are you afraid of falling?”. It has even been suggested that older men do not want to be seen in public with walkers, because it threatens their sense of independency and strength [22]. This reasoning might be true to some extent, but probably not all women or all men try to live up to these stereotyped presumptions.
In our sample, the different directions in regression weights between Personal factors and FOF suggest different gendered patterns in response to the observed measures. We discuss one example more in depth. One of the significant variables was the experience of fractures during the previous 5 years. For women, more fractures meant a higher level of FOF, and this is a well-known relationship [12]. For men, the opposite was found: more fractures corresponded to lower level of FOF. In our sample, every other woman had experienced fractures. Eight of 10 women met the criteria for osteopenia or osteoporosis at baseline, a known risk factor for fractures [53].
Possible explanations for this higher prevalence in women have been extensively explored from a biological perspective, and the general conclusion is that “bones are shaped by culture” (i.e. the way we live in interaction with each other, rather than sex itself, plays a significant role in shaping the body) [54]. For instance, it has been shown that boys in Western countries are encouraged more than girls to take part in heavy sports and other activities that strengthen bone mass [55]. Girls are instead encouraged to play quiet games, and the lack of using the body at a younger age might influence the bone mineral density later in life. With advancing age, men and women appear to lose bone at the same rate once the peak bone mass is reached, but men already have an advantage [54]. Furthermore, young women often receive precautionary advice about being careful in various situations from concerned parents, friends, and media.
Young people, women as well as men, absorb cultural messages and their personalities are moulded by them until it becomes natural to think of women as more vulnerable than men [23]. This belief is probably reinforced by the common knowledge that older women have “brittle bones” – a persistent age and gendered stereotype – even though it has been recognized that more than half of older women who sustain fractures have a normal DXA scan. In fact, in some countries a DXA scan is not considered necessary in women aged 75 years or older because osteoporosis “may be assumed” in this group of people [56]. When taking these aspects into account, it might seem reasonable that women more easily become concerned about repeated fractures and, therefore, answer sometimes, often or always more often than the men when asked about FOF.
Some men did have experiences with fractures, but the opposite pattern on Personal factors might be explained by the following. Most men in our sample had spouses to rely on and felt no real concern about falling because women traditionally adopt the role as care-takers [22].
Activity and participation
This factor (component) includes performing activities and interacting with society and had the same direction for both women and men in relation to FOF. The results of our study support recent reports that FOF is strongly associated with a reduction in gait speed, decreased muscular strength, and impaired balance [14,57,58]. It has been stated that older women, in general, are weaker in their lower extremities than men are [59], which might explain the higher prevalence of FOF in women in some studies. In our study, the women performed similar as men on all performance-based tests. Regarding activity restriction due to the FOF, women scored, in general, lower on the SAFFE than men. Women were similarly active than men, and the fact that they did not experience more recurrent falls than the men supports the belief that a certain degree of FOF is beneficial and protects from falls.
Our study has limitations. First, we used gender as a binary variable, based on biology (i.e. sex). Stratifying findings by sex and label them as gender differences is common within public health research. This allowed us to compare men and women to simplify statistical calculations and to relate the findings to gender relational theory, which is rare [22,25,30]. However, due to the low number of included men, the results are more difficult to interpret. Second, we used a sample of convenience with volunteers who were, in general, healthy and physically active. This makes it hard to generalize the results to other groups of older people. It should also be acknowledged that there are probably cultural differences between countries, both in life style and the reporting of FOF. Third, all analyses were based on a small number of men, and very few of them considered themselves to have FOF. This fact alone supports our belief that men more easily deny fears, but results are more difficult to interpret. Fourth, the method for classifying variables followed the suggested linking-rules, but other constellations of observed variables might have produced different results. However, the ICF gave us the opportunity to analyse FOF within the whole life situation, using a variety of physical tests and questionnaires related to the risk of falling and FOF. This is an important strength. Finally, the data collection was performed during 2006, but we find no reason to believe that the results from our analysis should differ today. The interest about FOF has increased steadily in recent years and this study has the potential to add important aspects to a very complex phenomenon.
In conclusion, our results did not support the prevailing paradigm that FOF leads to an increased rate of recurrent falls in older independent community-dwelling people, and this lack of association was seen in both women and men. The question “Are you afraid of falling?” with the three response options dichotomized as “yes” or “no”, has no predictive value when screening for fall risk factors in this particular group of people, and is probably insufficient when assessing FOF. The answer sometimes should probably not be labelled as “yes”. We have shown that it is more likely that women answer sometimes due to gendered patterns, and inappropriately fall under the category “yes” when instead sometimes probably reflects a sound concern. The model fit with the ICF as the model was acceptable for all variables, except for Environmental factors. We found associations between FOF and Personal factors and Activity and Participation in both women and men. Different patterns in Personal factors indicated that the answer to the question “Are you afraid of falling?” might be influenced to some extent by societally shaped gendered patterns. The association to Activity and Participation confirmed that FOF is related to actual physical performance.
Acknowledgements
We would like to thank all the participants and colleagues that helped with baseline assessments.
Author contributions
All authors participated in conceiving and designing the study, interpreting data, and drafting the manuscript. E.N. and L.L.O. acquired the participants and the data. P.P., A.L., and L.L.O. performed the statistical analyses. E.N., C.A., A.L., and L.L.O. critically revised the manuscript. All authors read and approved the final manuscript.
Declaration of interest
The authors report no conflict of interest. Financial support was granted by the Swedish Research Council (521-2003-5538 and additional grant 5221-2011-3250).
References
- 1.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Library. 2012;4:CD007146. doi: 10.1002/14651858.CD007146.pub3. doi: 10.1002/14651858.CD007146.pub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deandrea S, Lucenteforte E, Bravi F, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–68. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Kumar C. The patient who falls: “it's always a trade-off”. JAMA. 2010;303:258–66. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35:37–41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 5.Peel NM. Epidemiology of falls in older age. Can J Aging. 2011;30:1–13. doi: 10.1017/S071498081000070X. [DOI] [PubMed] [Google Scholar]
- 6.Stenhagen M, Nordell E, Elmståhl S. Falls in elderly people: a multifactorial analysis of risk markers using data from the Swedish general population study ‘Good Ageing in Skåne’. Aging Clin Exp Res. 2013;25:59–67. doi: 10.1007/s40520-013-0015-z. [DOI] [PubMed] [Google Scholar]
- 7.Rossat A, Fantino B, Nitenberg C, et al. Risk factors for falling in community-dwelling older adults: which of them are associated with the recurrence of falls? J Nutr Health Aging. 2010;14:787–91. doi: 10.1007/s12603-010-0089-7. [DOI] [PubMed] [Google Scholar]
- 8.WHO global report on falls prevention in older age. Available from: www.who.int/ageing/projects/falls_prevention_older_age/en/ [last accessed 6 Oct 2012]
- 9.Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health. 2011;23:3–23. doi: 10.1177/0898264310378039. [DOI] [PubMed] [Google Scholar]
- 10.Delbaere K, Close JC, Brodaty H, et al. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. Br Med J. 2010;341:c4165. doi: 10.1136/bmj.c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheffer AC, Schuurmans MJ, van Dijk N, et al. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- 12.Friedman SM, Munoz B, West SK, et al. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–35. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 13.Luukinen H, Koski K, Kivela SL, Laippala P. Social status, life changes, housing conditions, health, functional abilities and life-style as risk factors for recurrent falls among the home-dwelling elderly. Public Health. 1996;110:115–18. doi: 10.1016/s0033-3506(96)80057-6. [DOI] [PubMed] [Google Scholar]
- 14.Kumar A, Carpenter H, Morris R, et al. Which factors are associated with fear of falling in community-dwelling older people? Age Ageing. 2013. 6 Oct [Epub ahead of print]. [last accessed 20 Nov 2013] [DOI] [PubMed]
- 15.Austin N, Devine A, Dick I, et al. Fear of falling in older women: a longitudinal study of incidence, persistence, and predictors. J Am Geriatr Soc. 2007;55:1598–603. doi: 10.1111/j.1532-5415.2007.01317.x. [DOI] [PubMed] [Google Scholar]
- 16.Hadjistavropoulos T, Carleton RN, Delbaere K, et al. The relationship of fear of falling and balance confidence with balance and dual tasking performance. Psychol Aging. 2012;27:1–13. doi: 10.1037/a0024054. [DOI] [PubMed] [Google Scholar]
- 17.Zijlstra GA, van Haastregt JC, van Eijk JT, et al. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing. 2007;36:304–9. doi: 10.1093/ageing/afm021. [DOI] [PubMed] [Google Scholar]
- 18.Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84:565–70. doi: 10.2105/ajph.84.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murphy SL, Dubin JA, Gill TM. The development of fear of falling among community-living older women: predisposing factors and subsequent fall events. J Gerontol A Biol Sci Med Sci. 2003;58:943–7. doi: 10.1093/gerona/58.10.m943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mann R, Birks Y, Hall J, Torgerson D, Watt I. Exploring the relationship between fear of falling and neuroticism: a cross-sectional study in community-dwelling women over 70. Age Ageing. 2006;35:143–7. doi: 10.1093/ageing/afj013. [DOI] [PubMed] [Google Scholar]
- 21.Connell R. Gender, health and theory: conceptualizing the issue, in local and world perspective. Soc Sci Med. 2012;74:1675–83. doi: 10.1016/j.socscimed.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Calasanti T. Gender relations and applied research on aging. Gerontologist. 2010;50:720–34. doi: 10.1093/geront/gnq085. [DOI] [PubMed] [Google Scholar]
- 23.Twenge JM. Changes in women's assertiveness in response to status and roles: a cross-temporal meta-analysis, 1931–1993. J Pers Soc Psychol. 2001;81:133–45. [PubMed] [Google Scholar]
- 24.Connell R, Messerschmidt J. Hegemonic masculinity – rethinking the concept. Gender Soc. 2005;19:829–59. [Google Scholar]
- 25.Courtenay WH. Constructions of masculinity and their influence on men's well-being: a theory of gender and health. Soc Sci Med. 2000;50:1385–401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 26.Calasanti T, Slevin KF, King N. Ageism and feminism: from “et cetera” to center. Feminist Format. 2006;18:13–30. [Google Scholar]
- 27.Foster L, Walker A. Gender and active ageing in Europe. Eur J Age. 2013;10:3–10. doi: 10.1007/s10433-013-0261-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calasanti T. Feminist gerontology and old men. J Gerontol B Psychol Sci Soc Sci. 2004;59:305–14. doi: 10.1093/geronb/59.6.s305. [DOI] [PubMed] [Google Scholar]
- 29.Hurd Clarke L, Korotchenko A. Aging and the body: a review. Can J Aging. 2011;30:495–510. doi: 10.1017/S0714980811000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ohman A. Global public health and gender theory: the need for integration. Scand J Public Health. 2008;36:449–51. doi: 10.1177/1403494808094242. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization . ICF. International classification of functioning, disability and health. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 32.Beninato M, Portney LG, Sullivan PE. Using the International Classification of Functioning, Disability and Health as a framework to examine the association between falls and clinical assessment tools in people with stroke. Phys Ther. 2009;89:816–25. doi: 10.2522/ptj.20080160. [DOI] [PubMed] [Google Scholar]
- 33.Vieira ER, Berean C, Paches D, et al. Risks and suggestions to prevent falls in geriatric rehabilitation: a participatory approach. BMJ Qual Saf. 2011;20:440–8. doi: 10.1136/bmjqs.2010.042382. [DOI] [PubMed] [Google Scholar]
- 34.Scherer MJ, DiCowden MA. Organizing future research and intervention efforts on the impact and effects of gender differences on disability and rehabilitation: the usefulness of the International Classification of functioning, Disability and Health (ICF) Disabil Rehabil. 2008;30:161–5. doi: 10.1080/09638280701532292. [DOI] [PubMed] [Google Scholar]
- 35.Nordin E, Moe-Nilssen R, Ramnemark A, Lundin-Olsson L. Changes in step-width during dual-task walking predicts falls. Gait Posture. 2010;32:92–7. doi: 10.1016/j.gaitpost.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 36.Geusens P, Dinant G. Integrating a gender dimension into osteoporosis and fracture risk research. Gend Med. 2007;4:147–61. doi: 10.1016/s1550-8579(07)80055-6. [DOI] [PubMed] [Google Scholar]
- 37.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 38.Lachman ME, Howland J, Tennstedt S, et al. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE) J Gerontol B Psychol Sci Soc Sci. 1998;53:43–50. doi: 10.1093/geronb/53b.1.p43. [DOI] [PubMed] [Google Scholar]
- 39.Cieza A, Geyh S, Chatterji S, et al. ICF linking rules: an update based on lessons learned. J Rehabil Med. 2005;37:212–18. doi: 10.1080/16501970510040263. [DOI] [PubMed] [Google Scholar]
- 40.Beauchet O, Dubost V, Revel Delhom C, et al. How to manage recurrent falls in clinical practice: guidelines of the French Society of Geriatrics and Gerontology. J Nutr Health Aging. 2011;15:79–84. doi: 10.1007/s12603-011-0016-6. [DOI] [PubMed] [Google Scholar]
- 41.Brown T. Confirmatory factor analysis for applied research. New York: Guilford Press; 2006. [Google Scholar]
- 42.Carmines E, McIver J. Analyzing models with unobserved variables: analysis of covariance structures. Thousand Oaks (CA): Sage; 1981. [Google Scholar]
- 43.Browne M, Cudeck R. Alternative ways of assessing model fit. Newbury Park (CA): Sage; 1993. [Google Scholar]
- 44.Valentine JD, Simpson J, Worsfold C, Fisher K. A structural equation modelling approach to the complex path from postural stability to morale in elderly people with fear of falling. Disabil Rehabil. 2011;33:352–9. doi: 10.3109/09638288.2010.491575. [DOI] [PubMed] [Google Scholar]
- 45.O'Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 46.Wu TY, Chie WC, Yang RS, et al. Risk factors for single and recurrent falls: a prospective study of falls in community dwelling seniors without cognitive impairment. Prev Med. 2013;57:511–17. doi: 10.1016/j.ypmed.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 47.Kelsey JL, Procter-Gray E, Berry SD, et al. Reevaluating the implications of recurrent falls in older adults: location changes the inference. J Am Geriatr Soc. 2012;60:517–24. doi: 10.1111/j.1532-5415.2011.03834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Swanenburg J, de Bruin ED, Uebelhart D, Mulder T. Falls prediction in elderly people: a 1-year prospective study. Gait Posture. 2010;31:317–21. doi: 10.1016/j.gaitpost.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 49.Kwan MM, Tsang WW, Lin SI, et al. Increased concern is protective for falls in chinese older people: the chopstix fall risk study. J Gerontol A Biol Sci Med Sci. 2013;68:946–53. doi: 10.1093/gerona/gls338. [DOI] [PubMed] [Google Scholar]
- 50.Costa PT, Terracciano A, McCrae RR. Gender differences in personality traits across cultures: robust and surprising findings. J Pers Soc Psychol. 2001;81:322–31. doi: 10.1037/0022-3514.81.2.322. [DOI] [PubMed] [Google Scholar]
- 51.Hughes K, van Beurden E, Eakin EG, et al. Older persons' perception of risk of falling: implications for fall-prevention campaigns. Am J Public Health. 2008;98:351–7. doi: 10.2105/AJPH.2007.115055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gustafson PE. Gender differences in risk perception: theoretical and methodological perspectives. Risk Anal. 1998;18:805–11. doi: 10.1023/b:rian.0000005926.03250.c0. [DOI] [PubMed] [Google Scholar]
- 53.Bergström U, Björnstig U, Stenlund H, et al. Fracture mechanisms and fracture pattern in men and women aged 50 years and older: a study of a 12-year population-based injury register, Umeå, Sweden. Osteoporos Int. 2008;19:1267–73. doi: 10.1007/s00198-007-0549-z. [DOI] [PubMed] [Google Scholar]
- 54.Fausto-Sterling A. The bare bones of sex: part 1 – sex and gender. J Women Culture Soc. 2005;30:1491–527. [Google Scholar]
- 55.Young I. On female experiences: ‘throwing like a girl’ and other essays. New York: Oxford University Press; 2005. [Google Scholar]
- 56.Aspray TJ. New horizons in fracture risk assessment. Age Ageing. 2013;42:548–54. doi: 10.1093/ageing/aft095. [DOI] [PubMed] [Google Scholar]
- 57.Reelick MF, van Iersel MB, Kessels RP, Rikkert MG. The influence of fear of falling on gait and balance in older people. Age Ageing. 2009;38:435–40. doi: 10.1093/ageing/afp066. [DOI] [PubMed] [Google Scholar]
- 58.Rochat S, Bula CJ, Martin E, et al. What is the relationship between fear of falling and gait in well-functioning older persons aged 65 to 70 years? Archv Phys Med Rehabil. 2010;91:879–84. doi: 10.1016/j.apmr.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 59.Bohannon RW, Magasi SR, Bubela DJ, et al. Grip and knee extension muscle strength reflect a common construct among adults. Muscle Nerve. 2012;46:555–8. doi: 10.1002/mus.23350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vellas B, Guigoz Y, Garry PJ, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15:116–22. doi: 10.1016/s0899-9007(98)00171-3. [DOI] [PubMed] [Google Scholar]
- 61.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–72. [Google Scholar]
- 62.Corrigan JD, Hinkeldey NS. Relationships between parts A and B of the Trail Making Test. J Clin Psychol. 1987;43:402–9. doi: 10.1002/1097-4679(198707)43:4<402::aid-jclp2270430411>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 63.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 64.Lord SR. Visual risk factors for falls in older people. Age Ageing. 2006;35:ii42–5. doi: 10.1093/ageing/afl085. [DOI] [PubMed] [Google Scholar]
- 65.Mahoney FI, Barthel DW. Functional evaluation: The Barthel Index. Md State Med J. 1965;14:61–5. [PubMed] [Google Scholar]
- 66.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 67.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 68.Bohannon RW. Reference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from elders. Percept Mot Skills. 2006;103:215–22. doi: 10.2466/pms.103.1.215-222. [DOI] [PubMed] [Google Scholar]
- 69.Frandin K, Grimby G. Assessment of physical activity, fitness and performance in 76-years-olds. Scand J Med Sci Sports. 1994;4:41–6. [Google Scholar]


