Abstract
Policy Points:
Racial/ethnic differences in the overuse of care (specifically, unneeded care that does not improve patients’ outcomes) have received little scholarly attention.
Our systematic review of the literature (59 studies) found that the overuse of care is not invariably associated with race/ethnicity, but when it was, a substantial proportion of studies found greater overuse of care among white patients.
The absence of established subject terms in PubMed for the overuse of care or inappropriate care impedes the ability of researchers or policymakers to synthesize prior scientific or policy efforts.
Context
The literature on disparities in health care has examined the contrast between white patients receiving needed care, compared with racial/ethnic minority patients not receiving needed care. Racial/ethnic differences in the overuse of care, that is, unneeded care that does not improve patients’ outcomes, have received less attention. We systematically reviewed the literature regarding race/ethnicity and the overuse of care.
Methods
We searched the Medline database for US studies that included at least 2 racial/ethnic groups and that examined the association between race/ethnicity and the overuse of procedures, diagnostic (care) or therapeutic care. In a recent review, we identified studies of overuse by race/ethnicity, and we also examined reference lists of retrieved articles. We then abstracted and evaluated this information, including the population studied, data source, sample size and assembly, type of care, guideline or appropriateness standard, controls for clinical confounding and financing of care, and findings.
Findings
We identified 59 unique studies, of which 11 had a low risk of methodological bias. Studies with multiple outcomes were counted more than once; collectively they assessed 74 different outcomes. Thirty-two studies, 6 with low risks of bias (LRoB), provided evidence that whites received more inappropriate or nonrecommended care than racial/ethnic minorities did. Nine studies (2 LRoB) found evidence of more overuse of care by minorities than by whites. Thirty-three studies (6 LRoB) found no relationship between race/ethnicity and overuse.
Conclusions
Although the overuse of care is not invariably associated with race/ethnicity, when it was, a substantial proportion of studies found greater overuse of care among white patients. Clinicians and researchers should try to understand how and why race/ethnicity might be associated with overuse and to intervene to reduce it.
Keywords: guideline adherence, inappropriate utilization, inappropriate test
“Americans should be able to count on receiving care that meets their needs and is based on the best scientific knowledge,” according to the Institute of Medicine's Crossing the Quality Chasm.1 Yet the evidence clearly shows that racial and ethnic minority patients often do not receive necessary and appropriate health care.2,3 This “underuse” of care among racial and ethnic minorities (depicted in the southeast quadrant of Figure 1)—especially in contrast to white patients’ receipt of appropriate and necessary care (northeast quadrant)—is commonly referred to as “disparities” in care.
Figure 1.
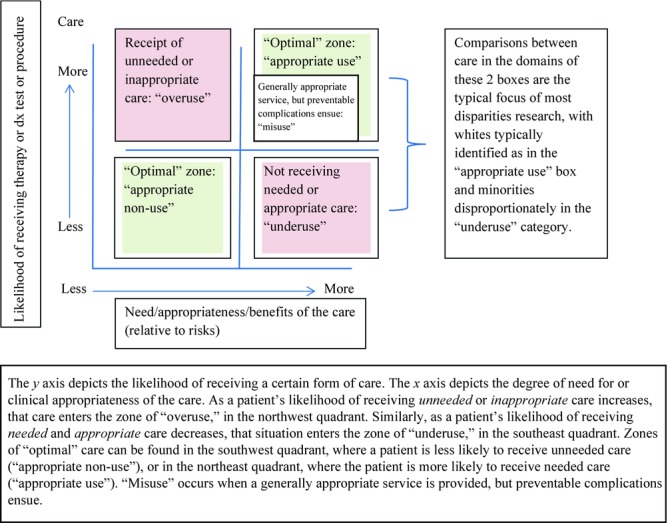
An Individual Patient's Appropriateness for and Likelihood of Receiving a Certain Form of Care
At the same time, it is increasingly clear that a sizable proportion of health care in the United States is “unnecessary”—that is, patients are receiving care that they do not need, which does not improve their health outcomes, and which may expose them to harm and risks,4 a situation referred to as the “overuse” of care (northwest quadrant of Figure 1). While much has been written about the geographic, health-systems, clinician, and payer factors associated with the overuse of care,5–8 less is known about the extent to which patients’ nonclinical characteristics, including sociodemographic factors like race/ethnicity, are associated with overuse.9
There are several indications that patient race/ethnicity might be related to overuse of care. Because patients’ attitudes, beliefs, and trust in medicine vary by race/ethnicity, these could differentially affect their risk for overuse. For example, white patients have greater “medical technology innovativeness,” more positive attitudes toward and receptivity to new drugs, devices, or procedures,10 which might contribute to their greater acceptance of and eagerness to obtain such therapies. In contrast, black patients have more pessimistic expectations of surgical outcomes, even for procedures like joint replacement with well-established efficacy, than do whites.11 While financial barriers are known impediments to the receipt of care,12–14 the converse may be true in that well-insured and affluent patients may be at increased risk for overuse.15 To the extent that whites, on average, are more optimistic about the health care system's ability to diagnose and cure them, and also have more financial resources to pay for care, this ironically may result in racial disparities in care in which white patients are at greater risk for overdiagnosis and overtreatment.
Clearly, patients are not the only potential drivers of overuse, given the many system- and clinician-level factors beyond their control. For example, receiving care in a region with practice patterns of more frequent visits, a greater use of hospital care and intensive care units, a greater supply of specialists and hospital beds,16,17 and greater physician investment in diagnostic testing centers or hospitals18 predisposes patients to receive more care than they would in areas with different characteristics. Conversely, the concentration of minority patients at institutions or with providers with fewer resources and cutting-edge technologies,19,20 besides impeding access to needed care, could also reduce the likelihood of their overusing newer diagnostic and therapeutic care with little marginal value over older therapies. These suppositions motivated us to conduct a systematic review of the medical literature to evaluate what is known about the relationship between patients’ race/ethnicity and their overuse of care.
Methods
We identified research on the overuse of medical or surgical diagnostic or therapeutic procedures or medications by race/ethnicity in the United States, related to established standards for overuse as codified in published clinical guidelines based on evidence linking appropriate care to better outcomes for individual patients. Guidelines and other initiatives to “choose wisely” (as in the ABIM [American Board of Internal Medicine] Foundation's Choosing Wisely campaign)21 are predicated on the assumption that an inappropriate use of clinical testing and therapies is at best wasteful of limited resources and at worst harmful to patients.
In addition to overuse and underuse, the Institute of Medicine (IOM) defined a third category of poor quality care, “misuse,” as situations in which a generally appropriate test or treatment is selected but leads to preventable complications, such as when a clinically appropriate antibiotic is prescribed for a patient's medical condition, but the patient has a known allergy to the antibiotic prescribed and develops an allergic reaction as a result.22 In the IOM's framework, issues of misuse are most often categorized as safety concerns, whereas issues of overuse and underuse are considered according to whether practice is consistent with the evidence.23 Because our focus is on the latter 2 categories, we excluded studies of misuse, following the strategy used in an earlier, related review by Korenstein and colleagues.6 We used the following acceptable standards for appropriate use:
Clinical recommendations based on a literature review and a multidisciplinary panel process like that by RAND.24
Published guidelines from a national or regional organization.
A universally accepted, well-referenced standard of care (eg, not using antibiotics to treat viral upper respiratory infections). Accordingly, we defined “overuse” as services that offer little or no benefit to individual patients, based on their specific clinical situation and in reference to the published guidelines for care.
Data Sources and Searches
In the absence of a Medical Subject Heading (“MESH” term) for overuse, we used an iterative, nonlinear search strategy to identify studies, using the Medline database (Box 1).
Box 1 Search Strategies.
Initial PubMed search strategy, conducted March 18, 2013 (n = 486):
(racial OR race OR ethnicity) (overuse OR “over use” OR inappropriate OR unnecessary OR overtreatment OR overtreat OR “over treatment” OR “over treat”) “United States”
Replication and extension of Korenstein and colleagues’ PubMed search strategy,6 conducted on June 3, 2013 (n = 1,196):
((((((((((“Guidelines as Topic” [Mesh] OR “Practice Guidelines as Topic” [Mesh] OR “Physician's Practice Patterns” [Mesh] OR “Drug Utilization Review” [Mesh] OR “Utilization Review” [Mesh] OR “Clinical Audit” [Mesh] OR “Guideline Adherence” [Mesh] OR “Health Services Misuse” [Mesh] OR “Delphi Technique” [Mesh] OR “Small-Area Analysis” [Mesh])) OR ((“Diagnostic Techniques and Procedures” [Mesh] OR “Prescriptions” [Mesh] OR “Surgical Procedures, Operative” [Mesh] OR “Methods” [Mesh]) AND “utilization” [Subheading])) OR (Overuse OR Appropriateness OR Inappropriateness OR “Inappropriate Medication” OR “Inappropriate Utilization” OR “Inappropriate Test” OR “Unnecessary Test”)))) AND ((((“Continental Population Groups” [Mesh]) OR “Ethnic Groups” [Mesh])) OR (Black OR African OR Hispanic OR Latino OR Latina OR Asian OR Caucasoid OR White OR race OR racial OR ethnicity))) AND (“has abstract”[Filter]) AND “humans”[Filter]) AND (“2009” [Date, Publication]: “3000” [Date, Publication]))) AND United States [Mesh]
Study Selection
We consulted a reference librarian for help in developing a search to identify studies of interest, which resulted in an initial search strategy including terms related to both overuse of care and race/ethnicity (see Box 1). This search of Medline for all years until March 2013 yielded 486 articles (Figure 2).
Figure 2.
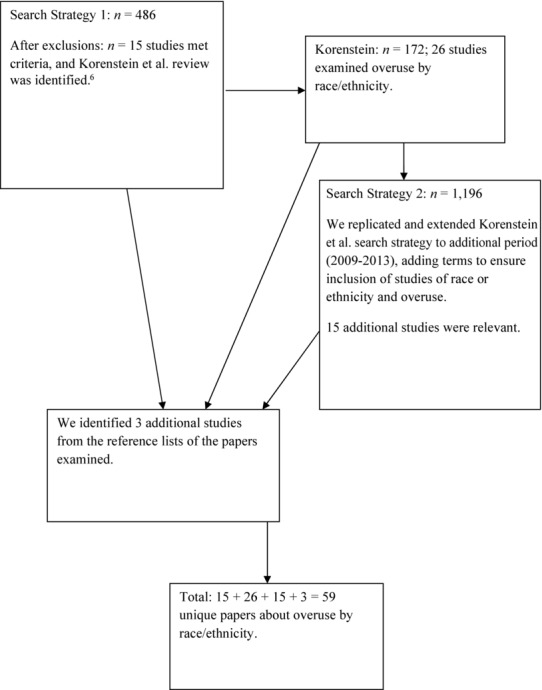
Flow Diagram
From these, we excluded research that (1) did not account for the clinical appropriateness of care, (2) focused on the misuse of care or unspecific forms of care (eg, hospital admissions), (3) examined patient adherence to recommended therapies (reasoning that patient self-reporting was less robust than other data on care received), (4) were qualitative studies, and (5) were thought pieces. We also excluded studies for which information on the use of care was obtained by the patient or provider self-report, those from unrepresentative settings (eg, a single site where n <50), and those focused on only one race/ethnic group (because we wanted to review the results of racial differences in overuse). After these exclusions, 15 studies remained.
During our initial search, we discovered a recent review of the literature, including 26 studies that examined race/ethnicity.6 Because that review ended at 2009, we replicated and extended the authors’ Medline search up to June 2013, adding terms to ensure the inclusion of studies on race or ethnicity and overuse (for specific syntax see Box 1). This search yielded 1,196 titles, of which 15 additional studies were relevant. We found 3 more studies from the reference lists of the papers examined, for a total of 59 unique papers on overuse by race/ethnicity.
Data Extraction and Quality Assessment
One of us (Nancy Kressin) reviewed titles generated from the Medline searches to identify abstracts warranting review. Then the other (Peter Groeneveld) evaluated a randomly selected set of 51 titles to determine the interrater reliability for the title selection process (κ = 0.856, very good). We then evaluated whether we agreed on whether the papers were appropriate to include, based on a review of the abstracts or the full text of a subset of 27 articles (κ = 1.00, excellent).
From each paper we extracted the medical condition or patient group studied, data sources, sampling method, sample size, treatment and/or diagnostic test studied, specific guidelines for overuse and/or appropriateness assessment (eg, RAND),24 and the specific race/ethnicity findings regarding overuse. We also ascertained whether either income or insurance status was accounted for in the statistical analyses, since these were important potentially confounding factors and their absence from the analyses increased the risk of bias. When no odds ratios were presented, we included any other available information, noting which data analyses were of poorer quality, such as when the authors did not conduct multivariate analyses or reported few details about their results. Since several studies examined multiple overuse outcomes, sometimes with differing results, we included results from some studies in multiple categories.
Data Synthesis and Analysis
Most of the included studies were retrospective secondary analyses of available observational data for patients meeting certain diagnostic criteria. While some approaches to assessing the quality of research studies downgrade the evidence from observational studies,25 such assessments are more relevant to the evaluation of the efficacy of an intervention than to observational data on patterns of care provided. We nevertheless tried to exclude poor-quality studies a priori through the rigorous selection process just described.
For studies meeting these criteria and without a recognized evidence-grading system for the types of studies we included, we adapted an established system for assessing risks of bias in studies of prognostic factors.26 We determined that the most relevant study features that might influence bias among our studies were (1) whether the study sample was representative of the population of patients at risk, (2) the source or validity of the race data, and (3) the methods for accounting for potential confounding clinical factors. We also considered (4) whether the models included insurance status or income, since they would likely affect access to care, and (5) the adequacy of the statistical analysis and reporting of results.
First, we gave the highest grade, “A,” to samples derived from nationally representative populations such as Medicare, Veterans Affairs (VA), National Ambulatory Medical Care Survey / National Hospital Ambulatory Medical Care Survey, and other national samples. Regional (eg, large but less representative than national data) subsets of national samples were assigned a “B” grade, and single-site or small regional samples were assigned a “C” (see online Appendix Table 1 for sampling grades). Next, we evaluated the source or validity of the race variables in these studies; however, most articles did not describe how they assessed these, likely because the vast majority drew from national data, for which the reliability of the race field has been documented elsewhere (eg, Medicare, VA, SEER).27–29 For studies not using such databases, we noted the method of race ascertainment when it was available.
We then evaluated the methods by which the studies accounted for potential confounding clinical factors. Even though we already had limited our review to studies using existing guidelines to determine appropriateness, the studies varied in the data used to assess such appropriateness. Thus, we developed a basic rating system for the quality of the assessments of clinical confounding (see online Appendix Table 1 for ratings). Studies using detailed clinical data to assess guideline adherence were given the highest, “A,” rating. Studies using some limited clinical data beyond diagnostic, drug, or procedure codes (eg, cancer stage, prior treatments received) received a “B” rating, and those using only diagnostic, drug, or procedure codes received a “C” rating.
Because Hayden and colleagues advised against creating a “gestalt” scale score to summarize the overall quality of each paper,26 we did not do so; however, we did note risks of bias and considered these in our evaluation of the evidence, summarizing them by category of study results. We identified those studies with the highest-quality evidence, for example, those that had low risks of bias (LRoB) and, if they had either an “A” or a “B” grade for sample representativeness and clinical confounding, that also accounted for either insurance status (by either adjusting for this or studying an insured population) or income and had adequate statistical analysis and reporting.
Results
We identified 59 unique publications examining race/ethnicity and the overuse of specific forms of care; these studies collectively assessed 74 different outcomes. All the included studies compared at least 2 racial/ethnic groups, with whites being one of the groups in every study. When the study findings were not uniform (eg, differing evidence of overuse among multiple outcomes within the same study, n = 12), we nevertheless included the paper in our analysis and categorized it in more than one of the publication groups described later.
Thirty-two studies (32/74 = 43%) found either an overuse of care among white patients compared with racial/ethnic minorities or an association between nonwhite race or Hispanic ethnicity and higher rates of appropriate non-use than among whites (see online Appendix Table 1). Six of these studies presented evidence with low risks of bias (LRoB), which is noted in the following descriptions.
Five of the studies finding more overuse among whites focused on cardiovascular (CV) care, including more frequency among whites of implantable cardioverter-defibrillator placement30 and cardiac resynchronization therapy31 compared with blacks and Hispanics, and more use of coronary artery bypass graft surgery32 and percutaneous coronary intervention procedures (both LRoB)33,34 compared with blacks.
Nine studies looked at cancer care. White men with low-risk, localized prostate cancer were more likely than blacks to receive interventional treatment with surgery or radiation instead of the preferred strategy of active surveillance (LRoB).35 Among men with low-risk prostate cancer, blacks were less likely than whites to receive unnecessary bone scans (LRoB).36 Black elderly men with limited life expectancies were less likely to receive prostatic serum antigen testing than were whites.37 White colon cancer patients were more likely to receive more than the recommended follow-up surveillance than blacks were (LRoB).38 White women with ductal carcinoma in situ who shared or made their own decisions regarding mastectomy had a higher probability of receiving the less recommended procedure of mastectomy, although sharing in or making their own decisions did not lead African American women to a greater probability of mastectomy.39 White breast cancer patients rated unsuitable for accelerated partial breast irradiation were more likely to receive it than were either black or Hispanic women.40 White patients with advanced cancer were more likely to undergo mammography than were blacks, Asians, or Hispanics.41 Black patients had lower odds than white patients did of receiving a potentially inappropriate screening colonoscopy.42 White patients with Barrett's esophagus were more likely than blacks or Hispanics to receive surveillance endoscopy more frequently than recommended.43
Ten studies examined the overuse of antibiotics for infectious disease. Six studies found that white primary care patients were more likely to inappropriately receive antibiotics for viral upper respiratory infection (URI) symptoms than were blacks or nonwhites44–49 (and than Hispanics were in the latter 6 studies). Physicians were less likely to prescribe any antibiotics for nonwhite than for white children with a sore throat,50 than for whites for other viral diagnoses,51 than for blacks or for blacks and Hispanics with asthma,52 and than for nonwhites with otitis media.53
Eight studies were in other clinical domains. Blacks and Hispanics were less likely than whites to receive high-risk medications such as opioids and/or psychotropic medications.54 The odds of white nursing home patients receiving benzodiazepines or other potentially inappropriate medications were higher than for nonwhites or blacks.55,56 White children with minor blunt head trauma were more likely than blacks or Hispanics to receive inappropriate cranial computed tomography scans in the emergency department (ED).57 White children and adults with asthma were more likely to receive nonrecommended long-acting beta-agonist monotherapy than were blacks.58 A disproportionate number of renal patients classified as inappropriate for transplantation but still receiving transplants were white, compared with black (LRoB).59 Minorities with low back pain were less likely than whites to receive inappropriate imaging.60 Hispanic and multiracial patients were less likely than whites to receive inappropriate surveillance endoscopy.61
The literature was not uniform, as we also found 9 instances (9/74 = 12%) of higher rates of diagnostic testing or treatment overuse among racial/ethnic minorities, and 2 of these studies had low risks of bias. Blacks, Asians, Native Americans, and whites had higher rates of inappropriate surveillance endoscopy than did Hispanics and multiracial patients.61 Non-Hispanics were less likely than Hispanics to receive nonrecommended tests during preventive health exams.62 Black men with intermediate-risk prostate cancer were more likely than whites to undergo nonrecommended radiographic imaging (LRoB).63 Overuse of carotid endarterectomy was higher among blacks and Hispanics than whites (LRoB).64 Black ED patients with acute ischemic stroke whose hypertension did not meet the criteria for blood pressure lowering were treated more often than whites.65 Inappropriate prescribing was more common overall among older black Americans than whites,54 as well as among all black and Hispanic versus white adults,56,66 and Hispanics were more likely than whites to receive psychotropics. African Americans and Hispanics were more likely than whites to receive skeletal muscle relaxants.54 African Americans seeing nurse practitioners (but not physicians) were more likely to receive antibiotics for viral URIs than were whites.47,67
We also found 33 (33/74 = 45%) instances in which possible racial/ethnic differences in overuse were examined but none were found; 6 studies in this group had low risks of bias. Inappropriate carotid endarterectomy did not differ by race/ethnicity (whites versus nonwhites)68 (LRoB; this study also evaluated the overuse of coronary angiography and upper gastrointestinal endoscopy and found no race/ethnicity differences in those either). Nor were there race/ethnicity differences in inappropriate diagnostic testing for coronary artery disease (whites versus blacks, Hispanics, and Asians; both with LRoB),69,70 overuse of transthoracic echocardiography (whites versus blacks, Hispanics, and Asians),71 or inappropriate coronary artery bypass grafting (whites versus blacks) (LRoB).33 In cancer screening and diagnosis, no race/ethnicity differences were found in the use of fecal occult blood testing (white, black, Asian/Pacific Islander, American Indian).72 Inappropriate surveillance colonoscopy among colorectal patients did not differ by race/ethnicity (white, black, Hispanic),73,74 nor did screening colonoscopy for Hispanic versus white patients.42 No race/ethnicity differences were found in the utilization of upper endoscopy for surveillance of gastric ulcers, or inappropriate use of bone scans or radiographic imaging for prostate cancer patients (white, black, Hispanic) (both LRoB).36,63 Seventeen studies found no race/ethnicity differences in the overuse of antibiotics, whether for pediatric asthma (white versus black and Hispanic)75 or among patients seeking care for colds, URIs, or bronchitis (primarily white versus black, with some studies also including Hispanics).44,47,49–51,76–85 Two additional studies found no race/ethnicity differences in patterns of antimicrobial use for URIs (white, black, Asian, Hispanic)86 or prescribing antipsychotics for older residents of long-term care facilities (white versus nonwhite).55 Older adults’ use of proton pump inhibitors did not differ by race/ethnicity (white, black, Hispanic),87 nor did their use of radiographs for low back pain (white versus nonwhite).88
We examined whether the studies in any of the 3 study categories systematically varied in quality. The quality of data was better among studies finding racial differences, with less poor-quality data among studies finding more overuse among whites (0.03% Grade C data), and 0% among those finding more overuse among minorities, compared with studies finding no race differences (15%; Table 1). Poor quality of confounding assessment was more common, however, in those studies finding more overuse among whites (59% Grade C) than in studies finding no racial differences (55%), or in studies finding more overuse by minorities (55%). There were few differences across study categories in the lack of assessments of insurance status or income (ranging from18% to 22%). Finally, poor-quality data analyses were most evident in the studies finding more overuse among minorities (44%) but were less evident in studies finding no race differences (18%) and studies finding higher rates of overuse by whites (16%).
Table 1.
Aspects of Studies by Study Category
| Study Categories | |||
|---|---|---|---|
| More Overuse | More Overuse | No Race | |
| Among | Among | Differences | |
| Whites (%) | Minorities (%) | in Overuse (%) | |
| Aspect of study | |||
| “C”-grade data qualitya | 0.03 | 0 | 15 |
| “C”-grade confoundingb | 59 | 55 | 55 |
| No assessment of insurance status or income | 22 | 22 | 18 |
| Poor-quality data analysis | 16 | 44 | 18 |
“C”-grade data quality defined as single-site or small regional samples, versus national (“A” grade) or large regional samples (“B” grade).
“C”-grade confounding defined as studies using only diagnostic, drug, or procedure codes, versus studies using detailed clinical data to assess guideline adherence (“A” rating) or studies using some limited clinical data beyond diagnostic, drug, or procedure codes (eg, cancer stage, prior treatments received, “B” rating).
In summary, in the highest-quality studies with the lowest risks of bias, we found evidence of overuse among whites, compared with racial/ethnic minorities, in 6 studies: CV care of whites versus blacks (2), cancer care of whites versus blacks (3), and renal care of whites versus blacks (1). Two studies with low risks of bias documented higher rates of overuse by racial/ethnic minorities: cancer care of whites versus blacks, Hispanics, and Asians (1) and CV care of whites versus Hispanics and blacks (1). Six studies with low risks of bias found no racial/ethnic differences in overuse: cancer care of whites versus nonwhites (2) and CV care of whites versus nonwhites/blacks, (4).
Discussion
In our systematic review, we examined studies of racial/ethnic variations in the overuse of health care. We identified 59 unique studies on this topic, which collectively reported 74 outcomes. A substantial proportion (43%) of the published evidence suggests a greater propensity for white patients to receive excessive testing and treatment, compared with minority patients; however, a similar proportion (45%) examined but did not find any racial/ethnic differences in overuse, while few studies found evidence of more overuse among racial/ethnic minorities compared with whites (12%). These proportions remained similar when limiting the denominator to the studies with the lowest risks of bias. Although the findings of these studies were not uniform in the direction or presence of the race/ethnicity effect on overuse, they do provide evidence that overuse varies by race/ethnicity and that when it does, whites more often experience overuse than do racial/ethnic minority patients. These findings suggest an ironic corollary to earlier findings in the disparities literature, that whites sometimes receive more unnecessary care than do minorities.
We found no clear patterns regarding race and overuse by clinical area, type of treatment, category of findings, or the study's risk of bias, although the quality of data was markedly poorer in those studies finding no race differences, and poorer-quality data analyses were most often evident in studies finding more overuse among minorities relative to whites. Also, the relative paucity of studies examining overuse by patients’ race/ethnicity was surprising, given the large literature on overuse and disparities in care. Among 172 overuse studies published between 1978 and 2009, only 26 (15%) even included the patients’ race or ethnicity in their analyses.6 Although we cannot identify all the potential drivers of the literature, we speculate that the earlier studies of overuse focused on the first phase of detecting and describing it, before the needed next phase of understanding the factors associated with such patterns, similar to the progression in the disparities literature from early studies documenting disparities to more recent work exploring the causes.90 While a 2001 review of the literature on racial disparities in invasive cardiac procedure use found 61 studies,3 the rapid expansion of the field since then, without a similarly large expansion of studies on race/ethnicity and overuse, suggests that disparities researchers may have focused on detecting evidence of underuse among minorities and may have precluded a simultaneous examination of overuse among whites or appropriate non-use among minorities. Challenges in quantifying overuse in the absence of established clinical guidelines may also be a reason for this. The limited availability of objectively developed clinical guidelines regarding appropriate care based on a patient's individual clinical situation and the absence of tools to incorporate his or her preferences for care91 are major barriers to defining, studying, and addressing overuse.
We found no evidence for clinician- or system-based causal etiology in the overuse studies included in this review, although neither was the focus of any of the studies. The literature on racial/ethnic disparities in care provides clues to additional factors that might be associated with overuse. Aspects of the health care system—its financing, accessibility, and quality—are associated with disparities in care,1 and racial/ethnic minority patients are more likely to access poorer-quality care.19,20,92 Because physicians and health care institutions caring for large numbers of minority patients have fewer resources20 and older, less cutting-edge care and technologies (but that might occasionally have a stronger evidence base or be less risky compared with newer technologies), minorities might be less vulnerable to overuse of certain diagnostic tests and treatments, even if they are simultaneously disadvantaged in their access to a large number of appropriate tests and treatments.
We did find much suggestive evidence for the negative effects of white patients’ attitudes toward and beliefs regarding overuse. White parents’ more frequent requests for inappropriate imaging for children with blunt head trauma,57 and higher rates of mastectomy among white women who could appropriately have had breast-conserving surgery and who played a greater role in their treatment decision making39 support the salience of white patients’ beliefs in the context of the overuse of care. We previously emphasized the need for disparities studies to collect information about patients’ attitudes and preferences,3 yet most of the subsequent studies (including our own) have examined how patients’ aversion to testing or treatment might impede their receipt of needed care rather than how patients’ excessive enthusiasm for testing or treatment might contribute to their receiving inappropriate care. Insofar as white patients’ attitudes and beliefs may predispose them to overuse, it is important to understand these dynamics in order to discourage them in the future. Clinicians should be aware of these attitudes when helping patients make informed decisions, in order to help them avoid unnecessary or potentially harmful care.
Attempts to reduce disparities have often focused on building patient attitudes that reinforce the value of care, such as trust in the system, clinicians, and the therapies that their physicians recommend. For example, an earlier effort sought to increase African Americans’ knowledge of and confidence in therapies for high blood pressure, as this population had clear patterns of inappropriate underuse.93 But sometimes a healthy skepticism regarding care may be well placed and beneficial in avoiding overuse. Indeed, current efforts by a partnership of the ABIM Foundation, physicians’ specialty groups, and Consumer Reports to help stem overuse (ChoosingWisely.org)21 suggest that patients should question their doctors about therapies or tests identified (by physicians) as being overused, and request explanations for why they are really needed, the potential downsides, other treatment/diagnostic options, and the cost of such care.94 While this is a laudable goal, it may be difficult for some patients to challenge the systemic factors associated with overuse,95 and additional efforts may be needed to support them.
It is important to consider the limitations of our findings. Although whites sometimes had a significantly higher rate of overuse, this does not mean that persons of other racial/ethnic groups did not also experience overuse, and a similar number of studies found no racial/ethnic differences in overuse. Furthermore, the absence of established subject terms in PubMed for the overuse of care or inappropriate care is a serious concern and impedes the ability of researchers or policymakers to synthesize earlier findings. Accordingly, our search strategy may have missed relevant studies, although we replicated an earlier search strategy and received extensive advice from a medical librarian in order to minimize these effects. Nonetheless, better informatics tools to accurately query the published science regarding this issue are urgently needed. We also were unable to rule out variations in health systems as an etiologic factor, because the studies we examined did not include that information. Finally, many of the studies we identified had risks of bias, mainly owing to the lack of detailed clinical data with which to assess appropriateness of care (an especially strong issue in studies of infectious disease care). This serious deficit in both the available data and the literature inhibited us from understanding the extent of overuse overall, as well as by race/ethnicity.
Even though minorities’ lower rates of inappropriate care, compared with those of whites, may be beneficial in some instances, unequal health care systems or biased practices should not be excused from scrutiny just because the outcomes are occasionally better for minorities. In addition, the overuse among whites may consume scarce resources and thus contribute to the underuse among minorities, further exacerbating disparities in care. Thus, problems with the fairness of both systems and practitioners must be identified and corrected, and minority patients’ distrust of physicians and health systems and their more pessimistic expectations of the outcomes of treatment must be addressed. It is vital that any corrections do not lead to more inappropriate care among minority patients but instead encourage appropriate care. Future disparities interventions should thus be carefully designed to minimize such unintended consequences.
Most of the literature on racial/ethnic differences in quality of care has examined the underuse of appropriate care, finding a lower receipt of such care in minorities. Accordingly, research and actions to address these disparities often focus on impediments to the receipt of care rather than on the broader influences on the use of health services. Our results extend the examination of disparities in quality of care to the overuse of care. Moreover, as did the underuse literature, we found evidence of a lower receipt of inappropriate care by minorities. This suggests that racial/ethnic differences in the quality of health care may pertain less to the appropriateness of the clinical action (as suggested by the underuse literature) and more to race-related influences on the underreceipt of health care services throughout the clinical appropriateness spectrum. Besides the need to understand the impediments to the receipt of appropriate care, our results highlight the need to apply a broader quality framework to examine all health care decision making.
Other researchers have argued in favor of an increased focus on overuse research,96 as well as the development of quality measures that look specifically at overuse.97 We agree that these may be valuable, but we also suggest that the focus of both the disparities and the overuse literatures be expanded to cover the overuse of care by race and ethnicity and that future research consider the possible effects of the systems, clinicians, and patients, in order to find all the drivers of the overuse of care. Efforts to optimize care for all patients are needed to reduce racial disparities in both underuse and overuse.
Acknowledgments
We thank Meng-Yun Lin, for her assistance in preparing the online table for this manuscript, and A'Llyn Ettien, head of Technical Services at the Boston University Alumni Medical Library, for her assistance in refining the search strategy for the review. We also appreciate the comments by David Coleman, Donna Washington, Said Ibrahim, and Paul Shekelle on earlier drafts of this manuscript.
Funding/Support
Nancy Kressin was supported by a Senior Research Career Scientist award from the Veterans Affairs Health Services Research and Development Service (RCS-02-066-1). This research also was supported by a grant: NIH/NHLBI (1U01HL105342-01, N. Kressin, PI). The sponsors had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, and approval of the manuscript.
The opinions expressed in this article do not necessarily represent the official views of the Department of Veterans Affairs, Boston University, the University of Pennsylvania, or the National Institutes of Health.
Conflict of Interest Disclosures
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No disclosures were reported.
Supporting Information
Disclaimer: Supplementary materials have been peer-reviewed but not copyedited.
Appendix Table 1. Studies Assessing Racial/Ethnic Differences in Overuse of Care
References
- Institute of Medicine, Committee on Quality of Health Care in America. Crossing the Quality Chasm. Washington, DC: Institute of Medicine; 2001. [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine/National Academies Press; 2003. [PubMed] [Google Scholar]
- Kressin NR, Petersen LA.Racial differences in the use of invasive cardiovascular procedures: review of the literature and prescription for future research. Ann Intern Med. 2001;135:352–366. [DOI] [PubMed] [Google Scholar]
- Welch HG, Schwartz LM, Woloshin S.Overdiagnosed: Making People Sick in the Pursuit of Health. Boston, MA: Beacon Press; 2011. [Google Scholar]
- Welch HG, Black WC.Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–613. [DOI] [PubMed] [Google Scholar]
- Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S.Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012;172(2):171–178. [DOI] [PubMed] [Google Scholar]
- Keyhani S, Falk R, Bishop T, Howell E, Korenstein D.The relationship between geographic variations and overuse of healthcare services: a systematic review. Med Care. 2012;50(3):257–261. [DOI] [PubMed] [Google Scholar]
- Keyhani S, Falk R, Howell EA, Bishop T, Korenstein D.Overuse and systems of care: a systematic review. Med Care. 2013;50(6):503–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson R, Docteur E.Doing Better by Doing Less: Approaches to Tackle Overuse of Services. Princeton, NJ: Robert Wood Johnson Foundation; 2013. [Google Scholar]
- Groeneveld PW, Sonnad SS, Lee AK, Asch DA, Shea JE.Racial differences in attitudes toward innovative medical technology. J Gen Intern Med. 2006;21(6):559–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeneveld PW, Kwoh CK, Mor MK, et al. Racial differences in expectations of joint replacement surgery outcomes. Arthritis Rheum. 2008;59(5):730–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newacheck PW, Stoddard JJ, Hughes DC, Pearl M.Health insurance and access to primary care for children. N Engl J Med. 1998;338(8):513–519. [DOI] [PubMed] [Google Scholar]
- Kirby JB, Kaneda T.Unhealthy and uninsured: exploring racial differences in health and health insurance coverage using a life table approach. Demography. 2010;47(4):1035–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider AH, Scott VK, Rehman KA, et al. Racial disparities in surgical care and outcomes in the United States: a comprehensive review of patient, provider, and systemic factors. J Am Coll Surg. 2013;216(3):482–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brawley OW, Goldberg P.How We Do Harm: A Doctor Breaks Rank about Being Sick in America. New York, NY: St. Martin's Press; 2012. [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL.The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287. [DOI] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL.The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298. [DOI] [PubMed] [Google Scholar]
- Mitchell JM.The prevalence of physician self–referral arrangements after Stark II: evidence from advanced diagnostic imaging. Health Aff. 2007;26(3): w415–w424. [DOI] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Epstein AM.Low–quality, high–cost hospitals, mainly in south, care for sharply higher shares of elderly black, Hispanic, and Medicaid patients. Health Aff. 2011;30(10):1904–1911. [DOI] [PubMed] [Google Scholar]
- Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL.Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–584. [DOI] [PubMed] [Google Scholar]
- Cassel CK, Guest JA.Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–1802. [DOI] [PubMed] [Google Scholar]
- Chassin MR, Galvin RW.The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000–1005. [DOI] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS, eds.; Institute of Medicine Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- Brook RH, Chassin MR, Fink A, Kosecoff J.A method for the detailed assessment of the appropriateness of medical technologies. Intern J Technol Assess Health Care. 1986;2(1):53–63. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C.Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. [DOI] [PubMed] [Google Scholar]
- Zaslavsky AM, Ayanian JZ, Zaborski LB.The validity of race and ethnicity in enrollment data for Medicare beneficiaries. Health Serv Res. 2012;47(3, pt. 2):1300–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroupe KT, Tarlov E, Zhang Q, Haywood T, Owens A, Hynes DM.Use of Medicare and DOD data for improving VA race data quality. J Rehabil Res Dev. 2010;47(8):781–795. [DOI] [PubMed] [Google Scholar]
- Patel DA, Knowles A, Schwartz AG, Schwartz K.Evaluation of African–American and white racial classification in a surveillance, epidemiology, and end results cancer registry. Ethnicity Dis. 2005;15(4):713–719. [PubMed] [Google Scholar]
- Cook NL, Orav EJ, Liang CL, Guadagnoli E, Hicks LS.Racial and gender disparities in implantable cardioverter–defibrillator placement: are they due to overuse or underuse? Med Care Res Rev. 2011;68(2):226–246. [DOI] [PubMed] [Google Scholar]
- Farmer SA, Kirkpatrick JN, Heidenreich PA, Curtis JP, Wang Y, Groeneveld PW.Ethnic and racial disparities in cardiac resynchronization therapy. Heart Rhythm. 2009;6:325–331. [DOI] [PubMed] [Google Scholar]
- Maynard C, Fisher LD, Passamani ER, Pullum T.Blacks in the Coronary Artery Surgery Study (CASS): race and clinical decision making. Am J Public Health. 1986;76(12):1446–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider EC, Leape LL, Weissman JS, Piana RN, Gatsonis C, Epstein AM.Racial differences in cardiac revascularization rates: does “overuse” explain higher rates among white patients? Ann Intern Med. 2001;135:328–337. [DOI] [PubMed] [Google Scholar]
- Epstein AM, Weissman JS, Schneider EC, Gatsonis C, Leape LL, Piana RN.Race and gender disparities in rates of cardiac revascularization: do they reflect appropriate use of procedures or problems in quality of care? Med Care. 2003;41(11):1240–1255. [DOI] [PubMed] [Google Scholar]
- Mishra MV, Shen X, Den RB, et al. Patterns of care for elderly men diagnosed with favorable–risk prostate cancer from 2004 to 2008: a population–based analysis. Am J Clin Oncol. 2013;36(6):606–611. [DOI] [PubMed] [Google Scholar]
- Palvolgyi R, Daskivich TJ, Chamie K, Kwan L, Litwin MS.Bone scan overuse in staging of prostate cancer: an analysis of a Veterans Affairs cohort. Urology. 2011;77:1330–1337. [DOI] [PubMed] [Google Scholar]
- Walter LC, Bertenthal D, Lindquist K, Konety BR.PSA screening among elderly men with limited life expectancies. JAMA. 2006;296:2336–2342. [DOI] [PubMed] [Google Scholar]
- Cooper GS, Kou TD, Reynolds HL., Jr. Receipt of guideline–recommended follow–up in older colorectal cancer survivors: a population–based analysis. Cancer. 2008;113:2029–2037. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Lantz PM, Janz NK, et al. Patient involvement in surgery treatment decisions for breast cancer. J Clin Oncol. 2005;23(24):5526–5533. [DOI] [PubMed] [Google Scholar]
- Hattangadi JA, Taback N, Neville BA, Harris JR, Punglia RS.Accelerated partial breast irradiation using brachytherapy for breast cancer: patterns in utilization and guideline concordance. J Natl Cancer Inst. 2012;104(1):29–41. [DOI] [PubMed] [Google Scholar]
- Sima CS, Panageas KS, Schrag D.Cancer screening among patients with advanced cancer. JAMA. 2010;304(14):1584–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffield KM, Han Y, Kuo YF, Riall TS, Goodwin JS.Potentially inappropriate screening colonoscopy in Medicare patients: variation by physician and geographic region. JAMA Intern Med. 2013:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El–Serag HB, Duan Z, Hinojosa–Lindsey M, et al. Practice patterns of surveillance endoscopy in a Veterans Affairs database of 29,504 patients with Barrett's esophagus. Gastrointest Endosc. 2012;76(4):743–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantrell R, Young AF, Martin BC.Antibiotic prescribing in ambulatory care settings for adults with colds, upper respiratory tract infections, and bronchitis. Clin Ther. 2002;24:170–182. [DOI] [PubMed] [Google Scholar]
- Linder JA, Singer DE, Stafford RS.Association between antibiotic prescribing and visit duration in adults with upper respiratory tract infections. Clin Ther. 2003;25:2419–2430. [DOI] [PubMed] [Google Scholar]
- Vanderweil SG, Pelletier AJ, Hamedani AG, Gonzales R, Metlay JP, Camargo CA., Jr. Declining antibiotic prescriptions for upper respiratory infections, 1993–2004. Acad Emerg Med. 2007;14(4):366–369. [DOI] [PubMed] [Google Scholar]
- Ma J, Stafford RS.Quality of US outpatient care: temporal changes and racial/ethnic disparities. Arch Intern Med. 2005;165:1354–1361. [DOI] [PubMed] [Google Scholar]
- Steinman MA, Landefeld CS, Gonzales R.Predictors of broad–spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA. 2003;289:719–725. [DOI] [PubMed] [Google Scholar]
- Rutschmann OT, Domino ME.Antibiotics for upper respiratory tract infections in ambulatory practice in the United States, 1997–1999: does physician specialty matter? J Am Board Fam Pract. 2004;17:196–200. [DOI] [PubMed] [Google Scholar]
- Linder JA, Bates DW, Lee GM, Finkelstein JA.Antibiotic treatment of children with sore throat. JAMA. 2005;294:2315–2322. [DOI] [PubMed] [Google Scholar]
- Thorpe JM, Smith SR, Trygstad TK.Trends in emergency department antibiotic prescribing for acute respiratory tract infections. Ann Pharmacother. 2004;38:928–935. [DOI] [PubMed] [Google Scholar]
- Vanderweil SG, Tsai CL, Pelletier AJ, et al. Inappropriate use of antibiotics for acute asthma in United States emergency departments. Acad Emerg Med. 2008;15(8):736–743. [DOI] [PubMed] [Google Scholar]
- Coco AS, Horst MA, Gambler AS.Trends in broad–spectrum antibiotic prescribing for children with acute otitis media in the United States, 1998–2004. BMC Pediatr. 2009;9:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugh MJ, Hanlon JT, Wang CP, et al. Trends in use of high–risk medications for older veterans: 2004 to 2006. J Am Geriatr Soc. 2011;59(10):1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson DG, Decker SL, Dwyer LL, et al. Antipsychotic and benzodiazepine use among nursing home residents: findings from the 2004 National Nursing Home Survey. Am J Geriatr Psychiatry. 2010;18(12):1078–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang B, Bachmann KA, He X, Chen R, McAllister JS, Wang T.Inappropriate prescriptions for the aging population of the United States: an analysis of the National Ambulatory Medical Care Survey, 1997. Pharmacoepidemiol Drug Safety. 2002;11(2):34. [DOI] [PubMed] [Google Scholar]
- Natale JE, Joseph JG, Rogers AJ, et al. Cranial computed tomography use among children with minor blunt head trauma: association with race/ethnicity. Arch Pediatr Adolesc Med. 2012;166(8):732–737. [DOI] [PubMed] [Google Scholar]
- Wasilevich EA, Clark SJ, Cohn LM, Dombkowski KJ.Long–acting β–agonist monotherapy among children and adults with asthma. Am J Manag Care. 2011;17(4):e91–e95. [PubMed] [Google Scholar]
- Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation—clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343(21):1537–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham HH, Landon BE, Reschovsky JD, Wu B, Schrag D.Rapidity and modality of imaging for acute low back pain in elderly patients. Arch Intern Med. 2009;169(10):972–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini SD, Eisen G, Mattek N, Schoenfeld P.Utilization of upper endoscopy for surveillance of gastric ulcers in the United States. Am J Gastroenterol. 2008;103:1920–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merenstein D, Daumit GL, Powe NR.Use and costs of nonrecommended tests during routine preventive health exams. Am J Prev Med. 2006;30:521–527. [DOI] [PubMed] [Google Scholar]
- Prasad SM, Gu X, Lipsitz SR, Nguyen PL, Hu JC.Inappropriate utilization of radiographic imaging in men with newly diagnosed prostate cancer in the United States. Cancer. 2012;118(5):1260–1267. [DOI] [PubMed] [Google Scholar]
- Halm EA, Tuhrim S, Wang JJ, et al. Racial and ethnic disparities in outcomes and appropriateness of carotid endarterectomy: impact of patient and provider factors. Stroke. 2009;40(7):2493–2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grise EM, Adeoye O, Lindsell C, et al. Emergency department adherence to American Heart Association guidelines for blood pressure management in acute ischemic stroke. Stroke. 2012;43(2):557–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linder JA, Chan JC, Bates DW.Evaluation and treatment of pharyngitis in primary care practice: the difference between guidelines is largely academic. Arch Intern Med. 2006;166(13):1374–1379. [DOI] [PubMed] [Google Scholar]
- Ladd E.The use of antibiotics for viral upper respiratory tract infections: an analysis of nurse practitioner and physician prescribing practices in ambulatory care, 1997–2001. Am Acad Nurse Pract. 2005;17:416–424. [DOI] [PubMed] [Google Scholar]
- Brook RH, Park RE, Chassin MR, Solomon DH, Keesey J, Kosecoff J.Predicting the appropriate use of carotid endarterectomy, upper gastrointestinal endoscopy, and coronary angiography. N Engl J Med. 1990;323:1173–1177. [DOI] [PubMed] [Google Scholar]
- Carlisle DM, Leape LL, Bickel S, et al. Underuse and overuse of diagnostic testing for coronary artery disease in patients presenting with new–onset chest pain. Am J Med. 1999;106:391–398. [DOI] [PubMed] [Google Scholar]
- Ko DT, Ross JS, Wang Y, Krumholz HM.Determinants of cardiac catheterization use in older Medicare patients with acute myocardial infarction. Circulation. 2010;3(1):54–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick JN, Ky B, Rahmouni HW, et al. Application of appropriateness criteria in outpatient transthoracic echocardiography. J Am Soc Echocardiogr. 2009;22:53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partin MR, Powell AA, Bangerter A, et al. Levels and variation in overuse of fecal occult blood testing in the Veterans Administration. J Gen Intern Med. 2012;27(12):1618–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A, Kuo YF, Goodwin JS.Many patients who undergo surgery for colorectal cancer receive surveillance colonoscopies earlier than recommended by guidelines. Clin Gastroenterol Hepatol. 2013;11(1):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin JS, Singh A, Reddy N, Riall TS, Kuo YF.Overuse of screening colonoscopy in the Medicare population. Arch Intern Med. 2011;171(15):1335–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul IM, Maselli JH, Hersh AL, Boushey HA, Nielson DW, Cabana MD.Antibiotic prescribing during pediatric ambulatory care visits for asthma. Pediatrics. 2011;127(6):1014–1021. [DOI] [PubMed] [Google Scholar]
- Gonzales R, Camargo CA, Jr, MacKenzie T, et al. Antibiotic treatment of acute respiratory infections in acute care settings. Am Emerg Med. 2006;13:288–294. [DOI] [PubMed] [Google Scholar]
- Mangione–Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH.The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics. 1999;103:711–718. [DOI] [PubMed] [Google Scholar]
- Nyquist AC, Gonzales R, Steiner JF, Sande MA.Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998;279:875–877. [DOI] [PubMed] [Google Scholar]
- Hall KK, Philbrick J, Nadkarni M.Evaluation and treatment of acute bronchitis at an academic teaching clinic. Am J Med Sci. 2003;325:7–9. [DOI] [PubMed] [Google Scholar]
- Hare ME, Gaur AH, Somes GW, Arnold SR, Shorr RI.Does it really take longer not to prescribe antibiotics for viral respiratory tract infections in children? Ambul Pediatr. 2006;6:152–156. [DOI] [PubMed] [Google Scholar]
- Harris RH, MacKenzie TD, Leeman–Castillo B, et al. Optimizing antibiotic prescribing for acute respiratory tract infections in an urban urgent care clinic. J Gen Intern Med. 2003;18:326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans CT, Smith B, Parada JP, Kurichi JE, Weaver FM.Trends in antibiotic prescribing for acute respiratory infection in veterans with spinal cord injury and disorder. J Antimicrob Chemother. 2005;55:1045–1049. [DOI] [PubMed] [Google Scholar]
- Hong SY, Taur Y, Jordan MR, Wanke C.Antimicrobial prescribing in the USA for adult acute pharyngitis in relation to treatment guidelines. J Eval Clin Pract. 2011;17(6):1176–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone S, Gonzales R, Maselli J, Lowenstein SR.Antibiotic prescribing for patients with colds, upper respiratory tract infections, and bronchitis: a national study of hospital–based emergency departments. Ann Emerg Med. 2000;36(4):320–327. [DOI] [PubMed] [Google Scholar]
- Gonzales R, Steiner JF, Sande MA.Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278(11):901–904. [PubMed] [Google Scholar]
- Vergidis P, Hamer DH, Meydani SN, Dallal GE, Barlam TF.Patterns of antimicrobial use for respiratory tract infections in older residents of long–term care facilities. J Am Geriatr Soc. 2011;59(6):1093–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CJ, Korc B, Ross JS.Appropriate proton pump inhibitor use among older adults: a retrospective chart review. Am J Geriatr Pharmacother. 2008;6:249–254. [DOI] [PubMed] [Google Scholar]
- Isaacs DM, Marinac J, Sun C.Radiograph use in low back pain: a United States emergency department database analysis. J Emerg Med. 2004;26:37–45. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Switzer G, Hyman K, Crowley–Matoka M, Fine MJ.Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96(12):2113–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr EA, Hayward RA.Patient–centered performance management: enhancing value for patients and health care systems. JAMA. 2013;310(2):137–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ly DP, Lopez L, Isaac T, Jha AK.How do black–serving hospitals perform on patient safety indicators? Implications for national public reporting and pay–for–performance. Med Care. 2010;48(12):1133–1137. [DOI] [PubMed] [Google Scholar]
- Ogedegbe GO, Boutin–Foster C, Wells MT, et al. A randomized controlled trial of positive–affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med. 2012;172(4):322–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- When to say “Whoa!” to your doctor: common tests and treatments you probably don't need. Consumer Reports 2012;77(6):12–13. [PubMed] [Google Scholar]
- Kressin NR, Atz JM.Mind the outcomes. JAMA. 2013;309(1):40–41. [DOI] [PubMed] [Google Scholar]
- Keyhani S, Siu AL.The underuse of overuse research. Health Serv Res. 2008;43(6):1923–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathias JS, Baker DW.Developing quality measures to address overuse. JAMA. 2013;309(18):1897–1898. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Table 1. Studies Assessing Racial/Ethnic Differences in Overuse of Care


