Abstract
Background:
The aim of this study is to compare the safety and efficacy of conventional laparotomy with those of robotic and laparoscopic approaches to hepatectomy.
Database:
Independent reviewers conducted a systematic review of publications in PubMed and Embase, with searches limited to comparative articles of laparoscopic hepatectomy with either conventional or robotic liver approaches. Outcomes included total operative time, estimated blood loss, length of hospitalization, resection margins, postoperative complications, perioperative mortality rates, and cost measures. Outcome comparisons were calculated using random-effects models to pool estimates of mean net differences or of the relative risk between group outcomes. Forty-nine articles, representing 3702 patients, comprise this analysis: 1901 (51.35%) underwent a laparoscopic approach, 1741 (47.03%) underwent an open approach, and 60 (1.62%) underwent a robotic approach. There was no difference in total operative times, surgical margins, or perioperative mortality rates among groups. Across all outcome measures, laparoscopic and robotic approaches showed no difference. As compared with the minimally invasive groups, patients undergoing laparotomy had a greater estimated blood loss (pooled mean net change, 152.0 mL; 95% confidence interval, 103.3–200.8 mL), a longer length of hospital stay (pooled mean difference, 2.22 days; 95% confidence interval, 1.78–2.66 days), and a higher total complication rate (odds ratio, 0.5; 95% confidence interval, 0.42–0.57).
Conclusion:
Minimally invasive approaches to liver resection are as safe as conventional laparotomy, affording less estimated blood loss, shorter lengths of hospitalization, lower perioperative complication rates, and equitable oncologic integrity and postoperative mortality rates. There was no proven advantage of robotic approaches compared with laparoscopic approaches.
Keywords: Hepatectomy, Laparoscopy, Robotics, Meta-analysis, Minimally invasive surgery
INTRODUCTION
Historically, because of visibility issues and the complicated relationship between the liver and its vasculature, hepatectomy has presented a challenge to the surgeon. Laparoscopy for liver resection was first documented in the early 1990s, proving to be as safe as conventional open hepatectomy while retaining oncologic integrity.1–7 However, laparoscopy has limitations in transection, mobilization, and the ability to control bleeding. To overcome some of these shortcomings, robot-assisted approaches have been devised and implemented that broaden visualization from 2 dimensions to 3 dimensions and increase range of motion to 360° via the EndoWrist (Intuitive Surgical Inc., Sunnyvale, California). Although minimally invasive approaches to surgery are known to decrease postoperative pain scores and length of hospitalization (LOH), with the rising costs of health care, controversy continues to surround discussions of these approaches.
The focus of this study is to evaluate the role of minimally invasive techniques in liver surgery as compared with a conventional open approach. We compared data related to operative time, perioperative complications, LOH, surgical margins, mortality rates, and cost analysis to assess differing approaches. This is the first systematic review to include analysis of the robotic approach, reflecting trends in modern surgery.
MATERIALS AND METHODS
Identification of Trials and Data Extraction
Two independent reviewers conducted a systematic search of PubMed and Embase on articles published until August 2013. The following medical subject headings were used to locate articles: liver robotic, hepatic robotic, hepatic laparoscopic, hepatectomy laparoscopic, and hepatectomy open. The inclusion criteria for articles were as follows: (1) articles comparing conventional open liver resection with either a laparoscopic or robotic approach; (2) controlled clinical trials, multicenter studies, or randomized controlled trials; (3) studies that reported outcomes of intraoperative and postoperative outcomes, including total operative time, estimated blood loss (EBL), LOH, surgical margins, postoperative complications, and postoperative mortality rates; and (4) studies that reported a measure of variance (standard error, standard deviation, or confidence interval [CI]). The references of articles included in the analysis were manually searched for additional articles for inclusion. Excluded from analysis were articles on resection of colorectal cancer with synchronous liver metastasectomy and articles not published in English. In instances in which research groups reported findings using shared patient populations, the earliest publication by that research group was included for analysis. The results from the 2 independent reviews were compared for accuracy, with disagreement resolved by consensus. To achieve completeness and to assemble the most representative patient database, series with limited sample sizes were included so that their experience would find meaning in aggregate.
Statistical Analysis
The primary outcomes of interest in this study were total operative time, EBL, LOH, surgical margins, perioperative complications, and postoperative mortality rates. A cost analysis was included as a secondary outcome of interest. For continuous outcomes, mean net changes were calculated as primary outcomes, whereas for categorical outcomes, odds ratios (ORs) were calculated to examine the treatment effect. DerSimonian and Laird random-effects models were used to pool mean net changes or ORs across the studies.8 The presence of heterogeneity was assessed with the Cochran Q test, and the extent of heterogeneity was quantified with the I2 index. To assess publication bias, funnel plots were constructed for each outcome. The Begg rank correlation test was used to examine the asymmetry of the funnel plot, and the Egger weighted linear regression test was used to examine the association between the mean effect estimate and its variance. In addition, sensitivity analyses were conducted by excluding each study in turn to evaluate its relative influence on the pooled estimates. All analyses were conducted using Stata software, version 10 (StataCorp, College Station, Texas).
RESULTS
Search Results
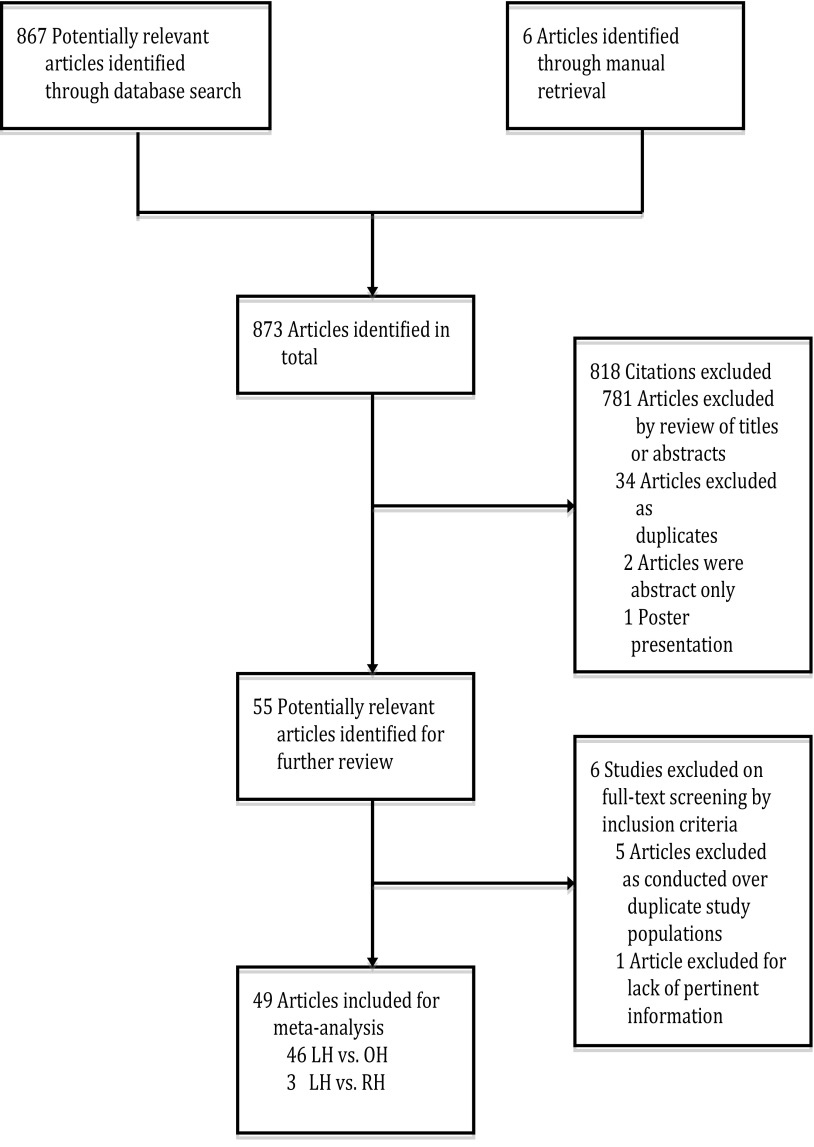
Eight hundred seventy-three abstracts were identified, 867 of which were obtained via searches of 2 databases, with an additional 6 retrieved through manual searches of references. The final set of articles undergoing analysis was attained using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Figure 1).9 Of the 873 abstracts identified, 55 underwent full-text review and 49 articles are included in this meta-analysis, with 3 comparing laparoscopic liver resection with robotic hepatectomy10–12 and 46 comparing laparoscopic liver resection with a conventional open approach (Table 1).13–58
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart showing literature search and study selection.9 LH = laparoscopic hepatectomy; OH = open hepatectomy; RH = robotic hepatectomy.
Table 1.
Studies Selected for Meta-Analysis
| Authors | Year | Country | Journal | Comparison | n |
|---|---|---|---|---|---|
| Packiam et al10 | 2012 | USA | J Gastrointest Surg | LHa vs RHa | 29 |
| Berber et al11 | 2010 | USA | HPB | LH vs RH | 32 |
| Troisi et al12 | 2013 | Belgium | Int J Med Robot | LH vs RH | 263 |
| Inoue et al13 | 2013 | Japan | Am Surg | LH vs OHa | 47 |
| Slakey et al14 | 2013 | USA | JSLS | LH vs OH | 62 |
| Kim et al15 | 2011 | South Korea | J Korean Surg Soc | LH vs OH | 55 |
| Abu Hilal et al16 | 2008 | UK | Eur J Surg Oncol | LH vs OH | 44 |
| Endo et al17 | 2009 | USA | Surg Laparosc Endosc Percutan Tech | LH vs OH | 21 |
| Cai et al18 | 2009 | Germany | Surg Endosc | LH vs OH | 38 |
| Ito et al19 | 2009 | USA | J Gastrointest Surg | LH vs OH | 130 |
| Morino et al20 | 2003 | USA | Surg Endosc | LH vs OH | 60 |
| Belli et al21 | 2007 | Italy | Surg Endosc | LH vs OH | 46 |
| Aldrighetti et al22 | 2008 | USA | J Gastrointest Surg | LH vs OH | 40 |
| Topal et al23 | 2008 | USA | Surg Endosc | LH vs OH | 152 |
| Kandil et al24 | 2012 | USA | Surgery | LH vs OH | 36 |
| Cannon et al25 | 2012 | USA | Surgery | LH vs OH | 175 |
| Polat26 | 2012 | Turkey | Surg Laparosc Endosc Percutan Tech | LH vs OH | 19 |
| Johnson et al27 | 2012 | USA | J Am Coll Surg | LH vs OH | 212 |
| Bhojani et al28 | 2012 | Canada | J Am Coll Surg | LH vs OH | 171 |
| Tranchart et al29 | 2010 | France | Surg Endosc | LH vs OH | 84 |
| Tang et al30 | 2005 | Hong Kong | Surg Endosc | LH vs OH | 17 |
| Lesurtel et al31 | 2003 | France | J Am Coll Surg | LH vs OH | 38 |
| Cheung et al32 | 2013 | Hong Kong | Ann Surg | LH vs OH | 60 |
| Kobayashi et al33 | 2013 | Japan | Surg Endosc | LH vs OH | 83 |
| Slim et al34 | 2012 | Italy | Langenbecks Arch Surg | LH vs OH | 92 |
| Hu et al35 | 2012 | China | Surg Laparosc Endosc Percutan Tech | LH vs OH | 26 |
| Hu et al36 | 2011 | China | World J Gastroenterol | LH vs OH | 60 |
| Gustafson et al37 | 2012 | USA | Surg Endosc | LH vs OH | 76 |
| Nguyen et al38 | 2011 | USA | Arch Surg | LH vs OH | 86 |
| Tu et al39 | 2011 | China | World J Gastroenterol | LH vs OH | 31 |
| Vanounou et al40 | 2010 | Canada | Ann Surg Oncol | LH vs OH | 73 |
| Castaing et al41 | 2009 | France | Ann Surg | LH vs OH | 120 |
| Carswell et al42 | 2009 | UK | BMC Surg | LH vs OH | 20 |
| Dagher et al43 | 2009 | France | Am J Surg | LH vs OH | 72 |
| Rowe et al44 | 2009 | Canada | Surg Endosc | LH vs OH | 30 |
| Sarpel et al45 | 2009 | USA | Ann Surg Oncol | LH vs OH | 76 |
| Tsinberg et al46 | 2009 | USA | Surg Endosc | LH vs OH | 74 |
| Cai et al47 | 2008 | China | Surg Endosc | LH vs OH | 62 |
| Lee et al48 | 2007 | Hong Kong | Hong Kong Med J | LH vs OH | 50 |
| Mala et al49 | 2002 | Norway | Surg Endosc | LH vs OH | 27 |
| Rau et al50 | 1998 | Germany | Hepatogastroenterology | LH vs OH | 34 |
| Shimada et al51 | 2001 | Japan | Surg Endosc | LH vs OH | 55 |
| Farges et al52 | 2002 | France | J Hepatobiliary Pancreat Surg | LH vs OH | 42 |
| Laurent et al53 | 2003 | France | Arch Surg | LH vs OH | 27 |
| Kaneko et al54 | 2005 | Japan | Am J Surg | LH vs OH | 58 |
| Polignano et al55 | 2008 | UK | Surg Endosc | LH vs OH | 50 |
| Lai et al56 | 2009 | China | Arch Surg | LH vs OH | 58 |
| Truant et al57 | 2011 | France | Surg Endosc | LH vs OH | 89 |
| Koffron et al58 | 2007 | USA | Ann Surg | LH vs OH | 400 |
LH = laparoscopic hepatectomy; OH = open hepatectomy; RH = robotic hepatectomy.
Description of Included Trials and Demographic Data
The 49 articles analyzed represent a total of 3702 patients, with sample sizes ranging from 17 to 400 patients. The distribution of the patients was as follows: 60 in the robotic group, 1901 in the laparoscopic group, and 1741 in the open group. Baseline patient demographic data, including sex, age, and body mass index, were well matched among groups (Table 2) Distribution of resection type by the 40 articles mentioning this characteristic is listed in Table 3.11–17,19–25,27–32,34,35,37–39,41–44,46–48,51–58
Table 2.
Demographic Characteristics
| Characteristic | Total (%) | LHa | OHa | RHa |
|---|---|---|---|---|
| Sex | ||||
| Male | 1535 (48.7) | 712 | 786 | 37 |
| Female | 1329 (42.1) | 705 | 601 | 23 |
| Age, y | 58.95 | 58.79 | 58.87 | 62.73 |
| BMIa | 26.67 | 26.46 | 26.31 | 31.00 |
| Lesions | ||||
| Mean number | 3.26 | 4.35 | 2.72 | 1.49 |
| Mean size, cm | 5.11 | 4.86 | 4.06 | 27.50 |
| Surgical indication | ||||
| CRCa metastases | 836 | 396 | 412 | 28 |
| Adenoma | 117 | 110 | 7 | 0 |
| FNHa | 127 | 109 | 18 | 0 |
| Hemangioma | 114 | 85 | 23 | 6 |
| HCCa | 951 | 436 | 509 | 6 |
| Hydatid cyst | 108 | 86 | 18 | 4 |
| Living donor | 52 | 32 | 20 | 0 |
| Cholangiocarcinoma | 15 | 8 | 6 | 1 |
BMI = body mass index; CRC = colorectal cancer; FNH = focal nodular hyperplasia; HCC = hepatocellular carcinoma; LH = laparoscopic hepatectomy; OH = open hepatectomy; RH = robotic hepatectomy.
Table 3.
Resection Type
| Resection Type | LHa | OHa | RHa |
|---|---|---|---|
| Monosegmentectomy | 304 | 250 | 7 |
| Subsegmentectomy/wedge | 270 | 249 | 15 |
| Bisegmentectomy | 173 | 141 | 8 |
| Left lateral sectionectomy | 323 | 231 | 2 |
| Right trisegmentectomy | 7 | 6 | 0 |
| Mixed segments | 26 | 0 | 8 |
| Right hepatectomy | 173 | 169 | 0 |
| Left hepatectomy | 113 | 72 | 0 |
| R extended hepatectomy | 12 | 22 | 0 |
| Major hepatectomy | 110 | 119 | 0 |
| Nonanatomical/atypical | 105 | 88 | 0 |
| P-S segment | 110 | 37 | 22 |
LH = laparoscopic hepatectomy; OH = open hepatectomy; RH = robotic hepatectomy.
Perioperative Outcomes
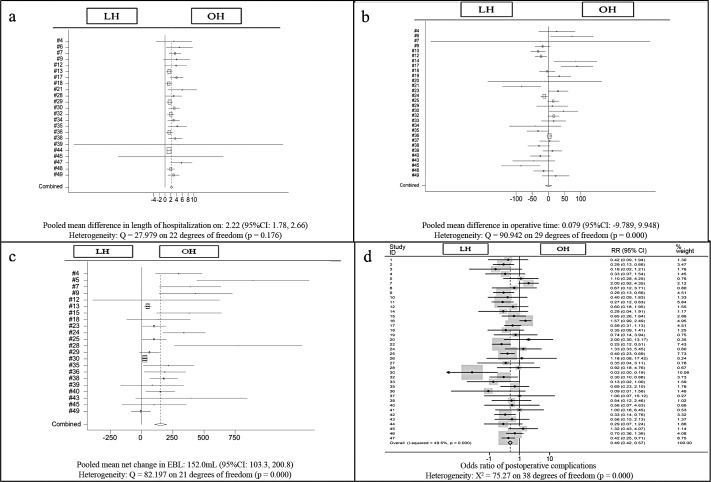
Forty-six publications reported total operative length, with similar results among groups10–13,15–24,26–36,38–58 (Figure 2a). The mean total operative time was 203.6 minutes, 203.9 minutes, and 234.8 minutes for the laparoscopic, open, and robotic groups, respectively.
Figure 2.
Forest plots and pooled analyses of mean difference in length of hospitalization (a), operative time (b), estimated blood loss (c), and odds ratio of postoperative complications (d). The mean difference is reported for each study (black boxes). LH = laparoscopic hepatectomy; OH = open hepatectomy.
Regarding EBL, 44 studies reported this variable.10–14,16–25,27–39,43,44,46–58 There was no difference between minimally invasive approaches, and there was a statistically significant increase in blood loss in laparotomy cases as compared with laparoscopy cases, with a pooled net mean change of 152.0 mL (95% CI, 103.3–200.8 mL) (Figure 2b).
The total number of conversions in the laparoscopic group was 106, which represents a 5.68% conversion rate to open surgery. In the robotic group, 9 cases required conversion to open surgery, representing a 15% conversion rate.
Twenty-nine studies included results of pathologic resection margin status in their analyses.13–16,19–21,23–25,28,29,31–33,38,41–43,45–49,51,53,56,57 Laparoscopy showed a significantly higher rate of negative surgical margins (pooled OR 1.06) as compared with laparotomy (pooled OR 1.01).
Postoperative Considerations
Forty-four studies reported LOH.10,12,13,15–32,34–40,42–44,46–58 As compared with patients undergoing the laparoscopic approach, those undergoing a conventional open approach had a significantly longer LOH (pooled mean difference, 2.22 days; 95% CI, 1.78–2.66 days) (Figure 2c).
Postoperative morbidity, including wound infection, biliary leakage, pleural effusion, bleeding, fluid collection, incisional hernia formation, renal failure, and ascites or cirrhotic decompensation, was reported by 47 articles.10–32,34–41,43–58 For total postoperative complications, minimally invasive approaches showed similar results with a rate significantly lower than that of the open group (OR, 0.49; 95% CI, 0.42–0.57) (Figure 2d). Specifically, minimally invasive approaches had lower rates of wound infections (OR, 0.39; 95% CI, 0.22–0.68), incisional hernias (OR, 0.20; 95% CI, 0.06–0.67), and ascites and cirrhotic decompensation events (OR, 0.50; 95% CI, 0.29–0.87) than the open group.
Forty studies reported data on postoperative mortality rates.10–20,22–37,39–43,45–49,53,54,56,57 There were no statistically significant differences between laparotomy and minimally invasive approaches for rates of both in-hospital mortality (OR, 1.01; 95% CI, 0.67–1.54) and postoperative mortality within 30 days of discharge (OR, 0.88; 95% CI, 0.41–1.88).
Cost Analysis
Eight studies included cost analyses and discussion on this outcome.10,28,38,40,44,46,55,58 Of these, one was excluded because it was out of scope.58 Four studies reported cost differences between minimally invasive approaches and conventional approaches, with three comparing laparotomy with laparoscopy and one comparing a robotic approach with an open approach.10,28,46,55 These studies showed a nonsignificant trend of higher total operative costs of $334.10 (95% CI, –$753.50–$1421.60) for minimally invasive approaches. Four studies reported total hospital cost differences, with all comparing laparotomy with laparoscopy.28,40,46,55 These researchers found a trend of higher total hospital costs in patients undergoing the conventional open approach of $3223 (95% CI, –$474–$692). Of note, one additional article normalized cost values for both total operative costs and total hospital costs and was subsequently not included in the statistical analysis.38
DISCUSSION
This meta-analysis of 3702 patients over a 14-year period yielded 49 pertinent studies showing minimally invasive approaches for hepatectomy to be as safe and efficacious as conventional laparotomy, with similar total operative times. Minimally invasive approaches afford shorter LOH, decreased EBL, and decreased postoperative morbidity. Specifically, these approaches resulted in fewer incisional hernias, wound infections, and ascites or cirrhotic decompensation events and retained oncologic integrity. All approaches to liver resection resulted in similar mortality rates. In terms of cost, minimally invasive approaches required nearly the same amount of money in the operating room as the conventional approach but saved money over the entire LOH.
Favorable operative outcomes, such as decreased EBL and lower rates of postoperative morbidity, lend credence to increased implementation of minimally invasive approaches. Bile leaks and massive hemorrhages are two important perioperative considerations in hepatic surgery owing to the unique anatomic structure of the liver, with minimally invasive approaches showing decreased intraoperative blood loss and equitable postoperative bile leak rates. The observed lower EBL is likely multifactorial, owing to both hepatic vein tamponade from pneumoperitoneum and improved dissection via field magnification. Furthermore, higher EBL and consequent blood transfusions are associated with increased postoperative morbidity, helping explain the lower rates of postoperative morbidity observed in this study.59
Long-term mortality rates were reported for 22 of the included study samples.11,15,17,19,24,25,29,32,33,35,36,38,41,45,47,48,51,53,54,56,57 When immediate postoperative deaths were excluded, nonsignificant differences were found between laparoscopic hepatectomy and open hepatectomy for overall survival and for disease-free survival by all research groups except one. Kandil et al24 found no difference in overall survival (P = .818) but found a significant difference in disease-free survival, with 100% 3-year survival in laparoscopic hepatectomy patients versus 71.4% survival in open hepatectomy patients (P = .03). Of note, the operative indication for this research group was neuroendocrine metastasis, whereas the indications for the remaining groups were primarily hepatocellular carcinoma or colorectal cancer metastases (Table 2). Perhaps a survival advantage exists in this population of patients; however, further studies are needed to establish the potential validity of this relationship.
A focus of debate regarding implementation of minimally invasive surgery centers on cost. In comparing total operative costs and total hospital costs among groups, studies found that although operative costs were higher for laparoscopic groups, their hospitalization costs were lower because of shorter LOH, which is intimately tied to postoperative morbidity, as well as decreased intensive care unit admission rates.38,40,60 Only 1 article assessed comparative costs between robotic and conventional open approaches, finding increased operating room costs with the robotic approach.10 However, without discussion of total hospital costs, no conclusions can be drawn from that study regarding the potential financial tradeoff gained by implementing robotic intervention. Further studies including the economic impact of minimally invasive surgery are needed to advance this discussion.
Minimally invasive approaches to surgery afford the surgeon increased visibility and the patient decreased LOH, improved cosmesis, and decreased postoperative pain. Colorectal metastases are a leading indication for hepatectomy, for which a majority of patients need repeat hepatectomy. Minimally invasive approaches not only better facilitate reoperations in this patient population but also allow for simultaneous operations in colorectal cancer patients with synchronous hepatic metastases.61–64
Although this study is comprehensive and is the most current evaluation of approaches to liver resection, there are several limitations and shortcomings to our study. First, the included studies are nonrandomized, retrospective studies, making them of moderate quality with increased selection bias. Also contributing to selection bias was patient selection by the surgeon, wherein healthier patients more fit for surgery were more likely to undergo minimally invasive options, leading to more favorable postoperative outcomes. Furthermore, patients selected for laparoscopic surgery may have had more easily resectable tumors, possibly contributing to their relative increase in negative margins. Intimately linked to minimally invasive surgical outcomes is both the surgeon's experience with the procedure and the volume of cases to which each care center is accustomed, neither of which was included in these studies, thereby prohibiting subanalysis. These studies exhibited moderate heterogeneity, with varying surgical techniques and differing outcome measures. Specifically, significant heterogeneity in reporting of resection outcomes, positive and negative versus R0–R1, prevents subanalysis of this outcome.
Although 873 citations were initially identified, an overwhelming majority of these were out of scope, focusing on tangential topics relating to liver donations, radiofrequency ablation, and tumor staging. Moreover, although these articles may have marginally touched on some of our primary outcomes, they neglected to contain data pertinent to this study. Furthermore, patient overlap by research groups led to the exclusion of 5 articles from analysis, totaling 488 patient experiences that are not represented.
The only statistically significant difference noted between minimally invasive approaches was a roughly 10% lower conversion rate to open surgery in the laparoscopic group as compared with the robotic group. With only 3 comparative studies including a robotic group, the ability to accurately ascertain any relationship to the robotic group is limited by its underpowering and the subsequent inability to perform subgroup analysis. Further comparative studies that include robotic approaches are needed. At present, the limited volume is likely because of the financial investment and operative training required to implement robots into common surgical practice.
CONCLUSION
To our knowledge, this review represents the largest, most current analysis of outcomes related to minimally invasive approaches to hepatectomy, with minimally invasive approaches showing improved postoperative morbidity, retained oncologic integrity, and potentially decreased economic burden to the health care system. Furthermore, future research comparing the robotic approach with the laparoscopic approach, as well as assessing the cost associated with each approach, is warranted.
Contributor Information
Nicole R. Jackson, Department of Surgery, Tulane University School of Medicine, New Orleans, LA, USA.; Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA.
Adam Hauch, Department of Surgery, Tulane University School of Medicine, New Orleans, LA, USA..
Tian Hu, Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA..
Joseph F. Buell, Department of Surgery, Tulane University School of Medicine, New Orleans, LA, USA..
Douglas P. Slakey, Department of Surgery, Tulane University School of Medicine, New Orleans, LA, USA..
Emad Kandil, Department of Surgery, Tulane University School of Medicine, New Orleans, LA, USA..
References:
- 1. Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78(5 Pt 2):956–958. [PubMed] [Google Scholar]
- 2. Gagner MRM, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc. 1992;6:97–98. [Google Scholar]
- 3. Wayand W, Woisetschlager R. Laparoscopic resection of liver metastasis. Chirurg. 1993;64(3):195–197. [PubMed] [Google Scholar]
- 4. Bryant R, Laurent A, Tayar C, Cherqui D. Laparoscopic liver resection—understanding its role in current practice: the Henri Mondor Hospital experience. Ann Surg. 2009;250(1):103–111. [DOI] [PubMed] [Google Scholar]
- 5. Buell JF, Thomas MT, Rudich S, et al. Experience with more than 500 minimally invasive hepatic procedures. Ann Surg. 2008;248(3):475–486. [DOI] [PubMed] [Google Scholar]
- 6. Pilgrim CH, To H, Usatoff V, Evans PM. Laparoscopic hepatectomy is a safe procedure for cancer patients. HPB (Oxford). 2009;11(3):247–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Simillis C, Constantinides VA, Tekkis PP, et al. Laparoscopic versus open hepatic resections for benign and malignant neoplasms—a meta-analysis. Surgery. 2007;141(2):203–211. [DOI] [PubMed] [Google Scholar]
- 8. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 9. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. [DOI] [PubMed] [Google Scholar]
- 10. Packiam V, Bartlett DL, Tohme S, et al. Minimally invasive liver resection: robotic versus laparoscopic left lateral sectionectomy. J Gastrointest Surg. 2012;16(12):2233–2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J. Robotic versus laparoscopic resection of liver tumours. HPB (Oxford). 2010;12(8):583–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Troisi RI, Patriti A, Montalti R, Casciola L. Robot assistance in liver surgery: a real advantage over a fully laparoscopic approach? Results of a comparative bi-institutional analysis. Int J Med Robot. 2013;9(2):160–166. [DOI] [PubMed] [Google Scholar]
- 13. Inoue Y, Hayashi M, Tanaka R, Komeda K, Hirokawa F, Uchiyama K. Short-term results of laparoscopic versus open liver resection for liver metastasis from colorectal cancer: a comparative study. Am Surg. 2013;79(5):495–501. [PubMed] [Google Scholar]
- 14. Slakey DP, Simms E, Drew B, Yazdi F, Roberts B. Complications of liver resection: laparoscopic versus open procedures. JSLS. 2013;17(1):46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim HH, Park EK, Seoung JS, et al. Liver resection for hepatocellular carcinoma: case-matched analysis of laparoscopic versus open resection. J Korean Surg Soc. 2011;80(6):412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abu Hilal M, McPhail MJW, Zeidan B, et al. Laparoscopic versus open left lateral hepatic sectionectomy: a comparative study. Eur J Surg Oncol. 2008;34(12):1285–1288. [DOI] [PubMed] [Google Scholar]
- 17. Endo Y, Ohta M, Sasaki A, et al. A comparative study of the long-term outcomes after laparoscopy-assisted and open left lateral hepatectomy for hepatocellular carcinoma. Surg Laparosc Endosc Percutan Tech. 2009;19(5):e171–e174. [DOI] [PubMed] [Google Scholar]
- 18. Cai X-J, Wang Y-F, Liang Y-L, Yu H, Liang X. Laparoscopic left hemihepatectomy: a safety and feasibility study of 19 cases. Surg Endosc. 2009;23(11):2556–2562. [DOI] [PubMed] [Google Scholar]
- 19. Ito K, Ito H, Are C, et al. Laparoscopic versus open liver resection: a matched-pair case control study. J Gastrointest Surg. 2009;13(12):2276–2283. [DOI] [PubMed] [Google Scholar]
- 20. Morino M, Morra I, Rosso E, Miglietta C, Garrone C. Laparoscopic versus open hepatic resection: a comparative study. Surg Endosc. 2003;17(12):1914–1918. [DOI] [PubMed] [Google Scholar]
- 21. Belli G, Fantini C, D'Agostino A, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc. 2007;21(11):2004–2011. [DOI] [PubMed] [Google Scholar]
- 22. Aldrighetti L, Pulitanò C, Catena M, et al. A prospective evaluation of laparoscopic versus open left lateral hepatic sectionectomy. J Gastrointest Surg. 2008;12(3):457–462. [DOI] [PubMed] [Google Scholar]
- 23. Topal B, Fieuws S, Aerts R, Vandeweyer H, Penninckx F. Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc. 2008;22(10):2208–2213. [DOI] [PubMed] [Google Scholar]
- 24. Kandil E, Noureldine SI, Koffron A, Yao L, Saggi B, Buell JF. Outcomes of laparoscopic and open resection for neuroendocrine liver metastases. Surgery. 2012;152(6):1225–1231. [DOI] [PubMed] [Google Scholar]
- 25. Cannon RM, Scoggins CR, Callender GG, McMasters KM, Martin RCG. Laparoscopic versus open resection of hepatic colorectal metastases. Surgery. 2012;152(4):567–573. [DOI] [PubMed] [Google Scholar]
- 26. Polat FR. Hydatid cyst: open or laparoscopic approach? A retrospective analysis. Surg Laparosc Endosc Percutan Tech. 2012;22(3):264–266. [DOI] [PubMed] [Google Scholar]
- 27. Johnson LB, Graham JA, Weiner DA, Smirniotopoulos J. How does laparoscopic-assisted hepatic resection compare with the conventional open surgical approach? J Am Coll Surg. 2012;214(4):717–723. [DOI] [PubMed] [Google Scholar]
- 28. Bhojani FD, Fox A, Pitzul K, et al. Clinical and economic comparison of laparoscopic to open liver resections using a 2-to-1 matched pair analysis: an institutional experience. J Am Coll Surg. 2012;214(2):184–195. [DOI] [PubMed] [Google Scholar]
- 29. Tranchart H, Di Giuro G, Lainas P, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010;24(5):1170–1176. [DOI] [PubMed] [Google Scholar]
- 30. Tang CN, Tai CK, Ha JPY, Siu WT, Tsui KK, Li MKW. Laparoscopy versus open left lateral segmentectomy for recurrent pyogenic cholangitis. Surg Endosc. 2005;19(9):1232–1236. [DOI] [PubMed] [Google Scholar]
- 31. Lesurtel M, Cherqui D, Laurent A, Tayar C, Fagniez PL. Laparoscopic versus open left lateral hepatic lobectomy: a case-control study. J Am Coll Surg. 2003;196(2):236–242. [DOI] [PubMed] [Google Scholar]
- 32. Cheung TT, Poon RTP, Yuen WK, et al. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg. 2013;257(3):506–511. [DOI] [PubMed] [Google Scholar]
- 33. Kobayashi S, Nagano H, Marubashi S, et al. Hepatectomy based on the tumor hemodynamics for hepatocellular carcinoma: a comparison among the hybrid and pure laparoscopic procedures and open surgery. Surg Endosc. 2013;27(2):610–617. [DOI] [PubMed] [Google Scholar]
- 34. Slim A, Garancini M, Di Sandro S, et al. Laparoscopic versus open liver surgery: a single center analysis of post-operative in-hospital and post-discharge results. Langenbecks Arch Surg. 2012;397(8):1305–1311. [DOI] [PubMed] [Google Scholar]
- 35. Hu M-G, Ou-Yang C-G, Zhao G-D, Xu D-B, Liu R. Outcomes of open versus laparoscopic procedure for synchronous radical resection of liver metastatic colorectal cancer: a comparative study. Surg Laparosc Endosc Percutan Tech. 2012;22(4):364–369. [DOI] [PubMed] [Google Scholar]
- 36. Hu B-S, Chen K, Tan H-M, Ding X-M, Tan J-W. Comparison of laparoscopic versus open liver lobectomy (segmentectomy) for hepatocellular carcinoma. World J Gastroenterol. 2011;17(42):4725–4728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gustafson JD, Fox JP, Ouellette JR, et al. Open versus laparoscopic liver resection: looking beyond the immediate postoperative period. Surg Endosc. 2012;26(2):468–472. [DOI] [PubMed] [Google Scholar]
- 38. Nguyen KT, Marsh JW, Tsung A, Steel JJL, Gamblin TC, Geller DA. Comparative benefits of laparoscopic versus open hepatic resection: a critical appraisal. Arch Surg. 2011;146(3):348–356. [DOI] [PubMed] [Google Scholar]
- 39. Tu J-F, Huang X-F, Hu R-Y, You H-Y, Zheng X-F, Jiang F-Z. Comparison of laparoscopic and open surgery for pyogenic liver abscess with biliary pathology. World J Gastroenterol. 2011;17(38):4339–4343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vanounou T, Steel JL, Nguyen KT, et al. Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol. 2010;17(4):998–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B. Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg. 2009;250(5):849–855. [DOI] [PubMed] [Google Scholar]
- 42. Carswell KA, Sagias FG, Murgatroyd B, Rela M, Heaton N, Patel AG. Laparoscopic versus open left lateral segmentectomy. BMC Surg. 2009;9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dagher I, Di Giuro G, Dubrez J, Lainas P, Smadja C, Franco D. Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg. 2009;198(2):173–177. [DOI] [PubMed] [Google Scholar]
- 44. Rowe AJ, Meneghetti AT, Schumacher PA, et al. Perioperative analysis of laparoscopic versus open liver resection. Surg Endosc. 2009;23(6):1198–1203. [DOI] [PubMed] [Google Scholar]
- 45. Sarpel U, Hefti MM, Wisnievsky JP, Roayaie S, Schwartz ME, Labow DM. Outcome for patients treated with laparoscopic versus open resection of hepatocellular carcinoma: case-matched analysis. Ann Surg Oncol. 2009;16(6):1572–1577. [DOI] [PubMed] [Google Scholar]
- 46. Tsinberg M, Tellioglu G, Simpfendorfer CH, et al. Comparison of laparoscopic versus open liver tumor resection: a case-controlled study. Surg Endosc. 2009;23(4):847–853. [DOI] [PubMed] [Google Scholar]
- 47. Cai XJ, Yang J, Yu H, et al. Clinical study of laparoscopic versus open hepatectomy for malignant liver tumors. Surg Endosc. 2008;22(11):2350–2356. [DOI] [PubMed] [Google Scholar]
- 48. Lee KF, Cheung YS, Chong CN, et al. Laparoscopic versus open hepatectomy for liver tumours: a case control study. Hong Kong Med J. 2007;13(6):442–448. [PubMed] [Google Scholar]
- 49. Mala T, Edwin B, Gladhaug I, et al. A comparative study of the short-term outcome following open and laparoscopic liver resection of colorectal metastases. Surg Endosc. 2002;16(7):1059–1063. [DOI] [PubMed] [Google Scholar]
- 50. Rau HG, Buttler E, Meyer G, Schardey HM, Schildberg FW. Laparoscopic liver resection compared with conventional partial hepatectomy—a prospective analysis. Hepatogastroenterology. 1998;45(24):2333–2338. [PubMed] [Google Scholar]
- 51. Shimada M, Hashizume M, Maehara S, et al. Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc. 2001;15(6):541–544. [DOI] [PubMed] [Google Scholar]
- 52. Farges O, Jagot P, Kirstetter P, Marty J, Belghiti J. Prospective assessment of the safety and benefit of laparoscopic liver resections. J Hepatobiliary Pancreat Surg. 2002;9(2):242–248. [DOI] [PubMed] [Google Scholar]
- 53. Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez P-L. Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg. 2003;138(7):763–769. [DOI] [PubMed] [Google Scholar]
- 54. Kaneko H, Takagi S, Otsuka Y, et al. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg. 2005;189(2):190–194. [DOI] [PubMed] [Google Scholar]
- 55. Polignano FM, Quyn AJ, de Figueiredo RSM, Henderson NA, Kulli C, Tait IS. Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc. 2008;22(12):2564–2570. [DOI] [PubMed] [Google Scholar]
- 56. Lai ECH, Tang CN, Ha JPY, Li MKW. Laparoscopic Liver resection for hepatocellular carcinoma: ten-year experience in a single center. Arch Surg. 2009;144(2):143–148. [DOI] [PubMed] [Google Scholar]
- 57. Truant S, Bouras AF, Hebbar M, et al. Laparoscopic resection versus open liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: a case-matched study. Surg Endosc. 2011;25(11):3668–3677. [DOI] [PubMed] [Google Scholar]
- 58. Koffron AJ, Auffenberg G, Kung R, Abecassis M. Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg. 2007;246(3):385–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wu WC, Smith TS, Henderson WG, et al. Operative blood loss, blood transfusion, and 30-day mortality in older patients after major noncardiac surgery. Ann Surg. 2010;252(1):11–17. [DOI] [PubMed] [Google Scholar]
- 60. Cannon RM, Scoggins CR, Callender GG, Quillo A, McMasters KM, Martin RC., II Financial comparison of laparoscopic versus open hepatic resection using deviation-based cost modeling. Ann Surg Oncol. 2013;20(9):2887–2892. [DOI] [PubMed] [Google Scholar]
- 61. Leung KL, Lee JF, Yiu RY, Ng SS, Li JC. Simultaneous laparoscopic resection of rectal cancer and liver metastasis. J Laparoendosc Adv Surg Tech A. 2006;16(5):486–488. [DOI] [PubMed] [Google Scholar]
- 62. Lupinacci RM, Machado MA, Lupinacci RA, Herman P. Simultaneous left colectomy and standard hepatectomy reformed by laparoscopy. Rev Col Bras Cir. 2011;38(2):139–141. [DOI] [PubMed] [Google Scholar]
- 63. Geiger TM, Tebb ZD, Sato E, Miedema BW, Awad ZT. Laparoscopic resection of colon cancer and synchronous liver metastasis. J Laparoendosc Adv Surg Tech A. 2006;16(1):51–53. [DOI] [PubMed] [Google Scholar]
- 64. Polignano FM, Quyn AJ, Sanjay P, Henderson NA, Tait IS. Totally laparoscopic strategies for the management of colorectal cancer with synchronous liver metastasis. Surg Endosc. 2012;26(9):2571–2578. [DOI] [PubMed] [Google Scholar]