Abstract
Background
The results of conservative treatment of knee osteoarthritis (OA) are generally evaluated in epidemiological studies with clinical outcome measures as primary outcomes. Biomechanical evaluation of orthoses shows that there are potentially beneficial biomechanical changes to joint loading; however, evaluation in relation to clinical outcome measures in longitudinal studies is needed.
Questions/purposes
We asked (1) is there an immediate effect on gait in patients using a laterally wedged insole or valgus knee brace; (2) is there a late (6 weeks) effect; and (3) is there a difference between subgroups within each group with respect to patient compliance, body mass index, and OA status?
Methods
This was a secondary analysis of data from a previous randomized controlled trial of patients with early medial knee OA. A total of 91 patients were enrolled in that trial, and 73 (80%) completed it after 6 months. Of the enrolled patients, 80 (88%) met prespecified inclusion criteria for analysis in the present study. The patients were randomized to an insole or brace. Gait was analyzed with and without wearing the orthosis (insole or brace) at baseline and after 6 weeks. Measurements were taken of the knee adduction moment, ground reaction force, moment arm, walking speed, and toe-out angle. Data were analyzed with regression analyses based on an intention-to-treat principle.
Results
A mean reduction of 4% (± 10) (95% confidence interval [CI], −0.147 to −0.03, p = 0.003) of the peak knee adduction moment and 4% (± 13) (95% CI, −0.009 to −0.001, p = 0.01) of the moment arm at baseline was observed in the insole group when walking with an insole was compared with walking without an insole. A mean reduction of 1% (± 10) (95% CI, −0.002 to −0.001, p = 0.001) of the peak knee adduction moment and no reduction of the moment arm were measured after 6 weeks. No reduction of knee adduction moment, moment arm, or ground reaction force was seen in the brace group at baseline and after 6 weeks. Subgroup analysis showed no differences in biomechanical effect for obesity, stage of OA, and whether patients showed a clinical response to the treatment.
Conclusions
Laterally wedged insoles unload the medial compartment only at baseline in patients with varus alignment and by an amount that might not be clinically important. No biomechanical alteration was seen after 6 weeks of wearing the insole. Valgus brace therapy did not result in any biomechanical alteration. Taken together, this study does not show a clinically relevant biomechanical effect of insole and brace therapy in patients with varus medial knee OA.
Level of Evidence
Level I, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
The conservative treatment of patients with varus medial knee osteoarthritis (OA) is aimed at altering the biomechanics of the knee to reduce the medial load, reduce symptoms, and slow progression of medial knee OA in cases of malalignment [4, 18, 24]. In knee OA of the medial compartment, symptom reduction and functional improvement have been reported in patients fitted with a valgus unloader knee brace [11] or a laterally wedged insole [2, 14, 25]. Recently, a placebo-controlled trial found a valgus knee brace to be more effective than a neutral brace [11]. Other studies concluded that a laterally wedged insole may be no more effective than the neutral equivalent [2, 20] and that a neutral insole can reduce the load of the medial compartment [9, 14]. However, a Cochrane review rated the evidence as “low quality” that both the valgus knee brace and laterally wedged insole have benefits in the treatment of symptomatic medial knee OA [7]. These clinical effects are attributed to the mechanical unloading of the diseased compartment. However, the exact working mechanism is not fully understood and remains a subject of discussion.
Recently, we published the results of our randomized clinical trial (RCT) (ISRCTN92527149) investigating the clinical effects and static correction of malalignment in the frontal plane of a laterally wedged insole compared with a valgus brace [26]. Correction of malalignment was evaluated with a standardized standing whole-leg radiograph. Although both groups (valgus brace and wedged insole) had improved patient-reported outcomes, no significant change in alignment was seen on this static evaluation [26], so whether a brace or insole corrects malalignment in the frontal plane remains controversial [8, 15, 21, 23, 26].
Another possible explanation for the observed clinical improvement could be a dynamic alteration. If a laterally wedged insole or valgus brace unloads the medial compartment of the knee, and thus has a dynamic effect during walking, this could explain the clinical improvements seen in earlier studies. For this reason, we also performed a gait analysis in this RCT [26] in which patients with varus medial knee OA wearing a laterally wedged insole or valgus knee brace were included.
The aim of the present study is to present the results of our gait analysis of patients with medial knee OA treated with a laterally wedged insole or valgus knee brace. We asked (1) is there an immediate effect on gait in patients using a laterally wedged insole or valgus knee brace; (2) is there a late (6 weeks) effect; and (3) is there a difference between subgroups within each group with respect to patient compliance, body mass index (BMI), and OA status?
Materials and Methods
We used gait analysis data obtained from an RCT (ISRCTN92527149) [26] in which patients with medial knee OA were treated with a laterally wedged insole or valgus brace. Patients with symptomatic medial knee OA who visited the outpatient clinic between January 2006 and September 2007 were eligible for inclusion.
The criteria for inclusion were pain and tenderness over the medial joint space in combination with radiographic osteoarthritic signs according to the Kellgren-Lawrence system of Grade I or higher and varus malalignment [13]. The criteria for exclusion were age younger than 35 years, symptoms not related to medial compartment OA, or an insufficient command of the Dutch language. This study was conducted according to the Declaration of Helsinki. Moreover, the protocol was approved by the local ethics committee and all patients gave their written informed consent.
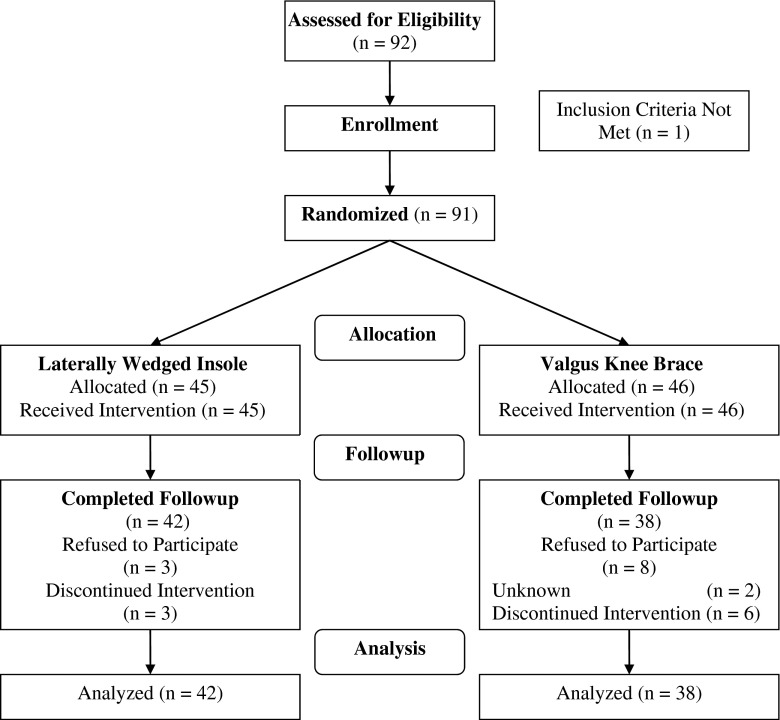
All patients were enrolled by one investigator (TMvR). A total of 91 patients were enrolled in the study [26], and 73 (80%) completed it. One patient with medial knee pain and clinical varus malalignment was excluded because no varus alignment was assessed by whole-leg radiograph, resulting in a total sample of 91 patients. These 91 patients were randomized to a laterally wedged insole (45 patients) or a valgus brace (46 patients). Patients were randomized according to a computer-generated procedure (block randomization with variable sizes of blocks); the randomization codes were held by an independent observer (SMAB-Z) to ensure masked blocking (Fig. 1). Three patients in the insole group and eight patients in the brace group refused to participate in the gait analysis after 6 weeks, which resulted in a study population of 80 patients (88%). Of these 80 patients, three in the insole group and six in the brace group changed their initial treatment during followup to other nonoperative or surgical treatments. The primary reason was no effect of treatment (three of three patients in the insole group and three of six patients in the brace group), but other reasons included bad fit of the brace, reduction of symptoms, and increased crepitus at the knee. Two patients were lost to followup for unknown reasons (Fig. 1).
Fig. 1.
Flowchart shows the study course.
The outcome assessor was not blinded to allocation. The grade of OA was scored according to Kellgren and Lawrence [13], measured on a standing short posteroanterior radiograph. Nineteen patients (42%) in the insole group and 12 patients (26%) in the bracing group had a Kellgren and Lawrence score ≥ III (Table 1).
Table 1.
Baseline characteristics of the study population and for the two intervention groups
| Baseline characteristics | Study population (n = 80) | Insole group (n = 42) | Brace group (n = 38) | Dropout (n = 11) |
|---|---|---|---|---|
| Women, number (%) | 41 (51) | 28 (67) | 13 (34) | 4 (36) |
| Age (years) | 54 (7) | 54 (7) | 54 (7) | 56 (7) |
| BMI (kg/m2) | 30 (5) | 30 (5) | 31 (5) | 30 (4) |
| VAS (0–10) | 6 (3) | 6 (3) | 6 (2) | 6 (4) |
| WOMAC (0–100) | 47 (18) | 47 (19) | 47 (16) | 40 (20) |
| Walking distance, number (%) | ||||
| Unimpaired | 36 (45) | 16 (38) | 20 (53) | 6 (55) |
| > 1 km | 29 (36) | 17 (40) | 12 (31) | 4 (36) |
| 500 m to 1 km | 10 (13) | 5 (12) | 5 (13) | 1 (9) |
| < 500 m | 5 (6) | 4 (10) | 1 (3) | 0 (0) |
| Analgesic use, number (%) | ||||
| None | 36 (45) | 18 (43) | 18 (47) | 8 (73) |
| When needed | 19 (24) | 10 (24) | 9 (24) | 1 (9) |
| Daily | 25 (31) | 14 (33) | 11 (29) | 2 (18) |
| Osteoarthritis medial K&L grade, number (%) | ||||
| 1 | 35 (41) | 15 (36) | 20 (53) | 4 (36) |
| 2 | 14 (18) | 8 (19) | 6 (16) | 2 (18) |
| 3 | 30 (38) | 18 (43) | 12 (32) | 5 (46) |
| 4 | 1 (1) | 1 (2) | 0 (0) | 0 (0) |
| Osteoarthritis lateral K&L grade, number (%) | ||||
| 0 | 57 (71) | 29 (69) | 28 (74) | 9 (82) |
| 1 | 19 (24) | 10 (24) | 9 (24) | 2 (18) |
| 2 | 2 (3) | 1 (2) | 1 (2) | 0 (0) |
| HKA angle (°)* | 7 (4) | 7 (4) | 7 (4) | 10 (4)† |
| Peak KAM (Nm) | 51 (18) | 55 (18) | NA | |
| Mean KAM (Nm) | 31 (14) | 33 (12) | NA | |
| Angular impulse (Nm/sec) | 23 (10) | 26 (10) | NA | |
All values are presented as mean (± SD) unless indicated otherwise; *positive angle represents varus alignment, negative angle represents valgus alignment; †significant difference between study population and lost to followup; BMI = body mass index; VAS = visual analog scale; K&L = Kellgren & Lawrence; HKA = hip-knee-ankle angle; KAM = knee adduction moment; NA = not available.
Mechanical alignment was assessed using the hip-knee-ankle angle (on a standing whole-leg radiograph). We used lateral fluoroscopic control by superimposing the dorsal aspect of the femoral condyles to ensure a perfect AP full-length exposure. The hip-knee-ankle angle is the angle measured between the following two lines: the mechanical axis of the femur (from the center of the femoral head to the central point between the tibial spines) and the mechanical axis of the tibia (from the center of the tibial spines to the center of the ankle). Earlier, we reported high intraobserver correlation coefficient (ICC = 0.98; 95% confidence interval [CI], 0.94–0.99) and interobserver (ICC = 0.97; 95% CI, 0.94–0.99) agreements for measurement of the hip-knee-ankle angle using this technique [6]. Before followup, among the insole and brace groups, three and eight patients refused to participate in the followup gait assessment, respectively. The patients who did not participate in the gait analysis at 6 weeks had a higher hip-knee-ankle angle compared with participants (p < 0.05).
Treatment Groups
All patients had been treated initially according to the guidelines of the Dutch College of General Practitioners, including patient education, physical therapy, and prescription of analgesic use. Patients were assigned either to the intervention group, receiving a shoe-inserted leather sole with a lateral-wedge cork elevation of 10 mm (6° wedge) along the entire length of the foot (Fig. 2), or to the control group receiving a knee brace (Fig. 3). The shoe-inserted sole was custom-made and fit by a specialized orthopaedic shoe technician. The valgus knee brace was commercially available for the right/left leg in four sizes (MOS Genu®; Bauerfeind AG, Kempen, Germany) and consisted of a thigh shell and a calf shell connected by coated aluminum hinges on the medial and lateral sides (Fig. 3). A specialized orthopaedic technician applied the brace. The degree of valgization depended on the degree of malalignment and the acceptance of the patient. Patients were instructed to wear the insole or brace as much as tolerated, and they were asked to register the number of hours per week they wore the orthosis.
Fig. 2.

An image of a left foot shows a leather sole and a laterally wedged cork elevation of 10 mm (6° wedge).
Fig. 3.

Anterior and lateral views of the right knee show a MOS Genu® knee brace with affixed markers.
Gait Analysis
When either the insole or valgus brace was first provided, we collected the baseline data directly. We analyzed the patients’ gait at baseline and after 6 weeks with and without the orthosis. Kinematic data (100 Hz) were collected unilaterally using three infrared cameras (Qualisys Proreflex, Gothenburg, Sweden). Passive retroreflective markers were placed at the following anatomic sites for the purpose of calibration: greater trochanter, medial and lateral femoral epicondyle, head of the fibula, tibial tuberosity, and medial and lateral malleoli. Markers located at the base of the first and at the tuberosity of the fifth metatarsal bone and at the lateral tuberosity of the calcaneus were glued to the shoe (Fig. 3). Patients were asked to wear the same comfortable shoes during the measurements and control pictures were taken to check the marker placement.
In addition, eight markers were put on two rigid frames that were attached by tape and Velcro straps to the middle part of the upper and lower leg. After a static calibration measure, all markers were removed except those on the frames and on the shoe. Kinetic data (200 Hz) were collected using an AMTI OR 6–7 force plate (AMTI, Watertown, MA, USA).
Each patient completed five walking trials of 20 m with an average speed of 1 m/s with and without orthoses. Walking speed was self-determined. Patients wore their own shoes and were instructed to use the same footwear during followup. Postprocessing calculation of the kinematic and kinetic data was conducted using custom-made Matlab algorithms (MathWorks, Natick, MA, USA) blinded for the type of orthosis. The positions of anatomic landmarks were derived from the positions of the markers on the frames. Anatomic landmarks for the upper leg were the greater trochanter and femoral epicondyles. Anatomic landmarks for the lower leg were the tibial tuberosity and malleoli. From these landmarks, right-handed segment coordinate systems were defined. Joint kinematics were calculated using an X-Y-Z Euler rotation sequence equivalent to the joint coordinate system. Joint kinetics were calculated using three-dimensional inverse dynamics, and the external joint moment data were normalized to body mass (Nm/kg).
The biomechanical kinematic parameters of interest were the knee adduction moment, knee angular adduction impulse [22], ROM of the knee, toe-out angle of the foot, and walking speed. Knee adduction moment (Nm/kg) is widely regarded as a surrogate measure of the difference between medial and lateral knee loading [22].
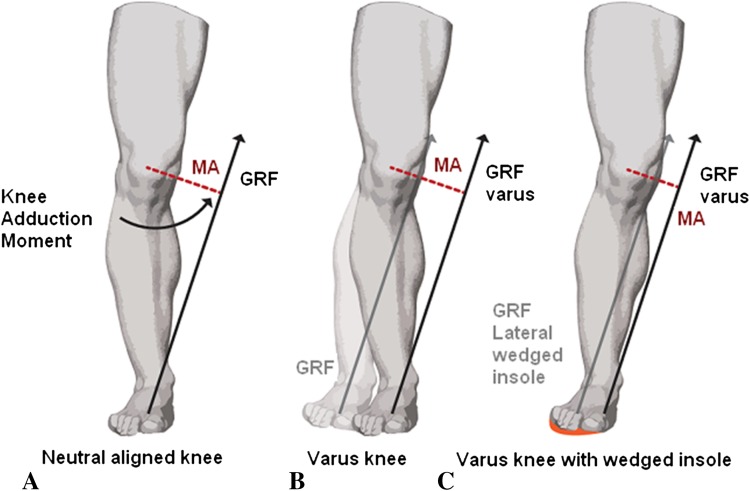
Throughout the entire stance phase of walking, the external adduction moment acts around the knee. The magnitude of knee adduction moment is influenced by the magnitude of the ground reaction force, the moment arm, and the mass and acceleration of lower limb segments (Fig. 4) [12, 22]. Peak knee adduction moment represents the maximum load differential between the medial and lateral compartment during one gait cycle. Mean knee adduction moment represents the mean load during the entire stance phase. The angular adduction impulse represents the total load on the medial compartment during one gait cycle. Walking with the foot externally rotated or a toe-out gait can reduce knee adduction moment in patients with medial knee OA [22]. We determined the toe-out angle from the line of progression drawn through the midpoint between the malleoli and the midpoint between the markers on the forefoot.
Fig. 4A–C.
Knee adduction moment during walking for a neutral aligned knee, a varus knee, and a varus knee with wedged insole is shown. The magnitude and direction of the ground reaction force are shown by the length and direction of the straight black or gray arrows. The length of the moment arm of the ground reaction force acting about the knee is indicated by a dotted line. (A) The neutral-aligned knee: knee adduction moment increases if the ground reaction force increases or the length of the moment arm increases. (B) For a varus knee deformity (superimposed over a neutrally aligned knee [light-shaded leg]), the moment arm (dotted line) is increased. (C) For the varus knee with a wedged insole, our hypothesis is that both the laterally wedged insole and the valgus knee brace shift the center of pressure, causing the ground reaction force to pass closer to the center of the knee. This effect decreases moment arm and reduces knee adduction moment compared with the situation without a lateral wedge. MA = moment arm; GRF = ground reaction force. (Adapted by permission from Macmillan Publishers Ltd: Nature Reviews Rheumatology. 2011;7:113–122. Copyright 2011.)
Sample Size
The sample size calculation in the initial RCT [26] was based on visual analog scale (VAS) pain score, which was the primary outcome of our RCT. Brouwer et al. [5] included patients according to similar criteria and reported a baseline mean VAS pain score of 6.0 (± 2.2). We hypothesized that a 1-point difference in VAS between the two groups would represent a clinically relevant difference, being 15% of the baseline score. To detect such a difference with two-sided testing (α = 0.05 and a power of 80%), we needed 40 patients in each group. With the assumption of a 15% rate of loss to followup, we included 91 patients. We did not recalculate statistical power or sample size for the present secondary analysis of knee biomechanics.
Statistical Analysis
To evaluate the presence of a possible selective dropout during followup, we compared the baseline characteristics of the 80 patients seen at 6 weeks and the 11 patients lost to followup by using the Kruskal-Wallis test. We analyzed the immediate effect at baseline and the late effects after 6 weeks of wearing the orthoses. To evaluate the difference in improvement between both intervention groups at 6 weeks followup, linear regression analyses were performed with adjustment for the baseline values of the outcome measures. Knee adduction moment, ground reaction force, and moment arm were considered dependent variables. Allocated intervention, toe-out angle, walking speed, hip-knee-ankle angle, and BMI were considered independent variables.
Additionally, we performed explorative subgroup analyses in which we investigated the relationships between compliance, obesity, and radiographic severity of OA and our outcome measures. We divided patients into two groups based on brace use: those who used the brace more than 42 hours per week (7 days times 6 hours, or 75% of the working day) and those who did not.
The SPSS program, Version 20 (SPSS Inc, Chicago, IL, USA) was used for statistical analysis, and a p value of 0.05 was considered to be statistically significant.
Results
Immediate Effect: Difference Between Wearing and Not Wearing the Orthosis
At baseline, both interventions showed an immediate effect of wearing the orthosis. Peak knee adduction moment decreased by 4% (± 10) in the insole group and increased by 5% (± 16) in the brace group (p = 0.003). Mean knee adduction moment decreased by 1% (± 0) in the insole group and did not change in the brace group by 0% (± 0) (p = 0.001). The angular impulse decreased with 1% (± 17) in the insole group and increased with 8% (± 25) in the brace group (p = 0.196). The moment arm decreased by 4% (± 13) in the insole group and increased by 6% (± 18) in the brace group (p = 0.01). The ground reaction force was not reduced in either group (Table 2).
Table 2.
Immediate effect, reported as percentage change in knee adduction moment measures, ground reaction force, and moment arm at baseline, when wearing the orthosis (wedged insole or brace) compared with no orthosis
| Outcome | Insole group (n = 38) | Brace group (n = 42) | Betaǂ | 95% confidence interval | p value† |
|---|---|---|---|---|---|
| Knee adduction moment | |||||
| Peak (%) | −4 (10)* | 5 (16)* | −0.089 | −0.147 to −0.03 | 0.003 |
| Mean (%) | −1 (0)* | 0 (0)* | −0.001 | −0.002 to −0.001 | 0.001 |
| Angular impulse (%) | −1 (17)* | 8 (25)* | −1.578 | −3.989 to 0.833 | 0.196 |
| Ground reaction force (%) | 0 (10) | 1 (7) | −8.604 | −41.371 to 24.162 | 0.602 |
| Moment arm (%) | −4 (13) | 6 (18) | −0.005 | −0.009 to −0.001 | 0.01 |
All values are presented as mean (± SD) unless indicated otherwise; p values of significantly reduced outcomes are presented in bold; *positive value represents increased knee adduction moment, negative value represents decreased knee adduction moment; †corrected for toe-out angle and walking speed; ǂbeta represents the regression coefficient of the linear regression analysis.
Late Effect (6 Weeks): Difference Between Wearing and Not Wearing the Orthosis
After 6 weeks of wearing the orthosis, no difference in change of peak knee adduction moment, ground reaction force, or moment arm was found between the insole and brace groups. The change of peak knee adduction moment in the insole group (−1% [± 10]) did not differ with the change in the brace group (1 [± 12], p = 0.328). The change in ground reaction force did also not differ in the insole-group (0% [± 6]) compared with the brace group (2% [± 16], p = 0.969). The change of moment arm in the insole group was 0% (± 14) and in the brace group was 1% (± 11) (p = 0.188). The mean knee adduction moment decreased 4% (± 18) in the insole group and increased 4% (± 10) in the brace group (p = 0.035). The angular impulse decreased 2% (± 16) in the insole group and increased 6% (± 22) in the brace group (p = 0.036) (Table 3).
Table 3.
Late effects reported as patient-reported outcomes and percentage changes in knee adduction moment measures, ground reaction force, and moment arm, between walking with and without an orthosis (wedged insole or brace) after 6 weeks of wearing the orthosis
| Outcome | Insole group (n = 38)* | Brace group (n = 42)* | Beta|| | 95% confidence interval | p value |
|---|---|---|---|---|---|
| Compliance, number (%)* | 29 (76) | 19 (45) | – | – | 0.213 |
| Improved walking distance, number (%)§ | 11 (29) | 7 (17) | – | – | 0.375 |
| Knee adduction moment | |||||
| Peak (%)† | −1 (10) | 1 (12) | −0.024 | −0.073 to 0.025 | 0.328ǂ |
| Mean (%)† | −4 (18) | 4 (10) | −0.073 | −0.141 to −0.005 | 0.035 ǂ |
| Mean (%)† | −2 (16) | 6 (22) | −2.448 | −4.730 to −0.165 | 0.036 ǂ |
| Ground reaction force (%) | 0 (6) | 2 (16) | −0.001 | −0.059 to 0.057 | 0.969ǂ |
| Moment arm (%) | 0 (14) | 1 (11) | −0.019 | −0.046 to 0.009 | 0.188ǂ |
* All values are presented as mean (± SD) unless indicated otherwise; p values of significantly reduced outcomes are presented in bold; *compliant, if the orthosis was worn > 42 hours/week; †positive value represents an increased knee adduction moment, negative value represents a decreased knee adduction moment; ǂcorrected for toe-out angle and walking speed; §38% in the insole and 53% in the brace group had an unimpaired walking distance at baseline; ||beta represents the regression coefficient of the linear regression analysis.
Subgroup Analysis: Differences Between Wearing and Not Wearing the Orthosis
Within each of the brace and insole groups, no difference in knee adduction moment, angular impulse, ground reaction force, or moment arm between patients who did and did not use the brace at least 42 hours per week was found. Moreover, between obese and nonobese patients, and patients with doubtful (Kellgren and Lawrence ≤ II) versus definite or moderate radiographic OA (Kellgren and Lawrence ≥ III), no differences were seen in knee adduction moment, angular impulse, ground reaction force, or moment arm (Table 4).
Table 4.
Difference between with and without an orthosis (wedged insole or brace) for compliant and noncompliant patients after 6 weeks of wearing the orthosis
| Outcome | Insoles | Brace | ||
|---|---|---|---|---|
| Compliant (n = 29)* | Noncompliant (n = 13)* | Compliant (n = 19)* | Noncompliant (n = 19)* | |
| Improved walking distance, number (%)ǂ | 8 (28) | 3 (23) | 1 (5) | 6 (32) |
| Knee adduction moment§ | ||||
| Peak, % (SD)† | −2 (7) | 0 (17) | −1 (11) | 4 (13) |
| Mean, % (SD)† | −9 (38) | −3 (8) | 3 (10) | 5 (9) |
| Angular impulse, % (SD)† | −3 (15) | 3 (21) | 7 (20) | 4 (26) |
| Ground reaction force, % (SD)† | 0 (6) | −2 (7) | 2 (6) | 1 (7) |
| Moment arm, % (SD)† | −1 (13) | 4 (17) | 1 (13) | 1 (7) |
All values are presented as mean (± SD) unless indicated otherwise; *compliant, if the orthosis was worn > 42 hours/week; †negative value represents a reduction; ǂ41% of compliant and 31% of noncompliant patients had an unimpaired walking distance at baseline in the insole group; in the brace group, the values were 58% of compliant and 47% of noncompliant patients; §corrected for body mass index, hip-knee-ankle angle, baseline values, toe-out angle, walking speed, and compliance.
Discussion
Many patients with varus medial knee OA report improved clinical outcomes after treatment with a laterally wedged insole or valgus knee brace [7, 26]. These clinical effects are attributed to the mechanical unloading of the diseased compartment. However, the exact working mechanism is not fully understood and remains a subject of discussion. The aim of this study was to evaluate the biomechanical alterations in patients with medial knee OA randomized for laterally wedged insole or valgus knee brace treatment in a longitudinal study.
Some limitations of our study need to be addressed. First, the study was conducted in a tertiary referral university medical center, which could affect the generalizability of its results. However, the eligibility criteria were not highly selective and we therefore believe that the included patients are representative of patients with medial knee OA. Second, we did not analyze the contralateral leg and did not measure the lateral trunk lean; however, our patients were instructed to walk maintaining the trunk in a tall, upright position. Footwear was not standardized to quantify the joint moments. Patients were instructed to wear their same comfortable, flexible shoes during followups, and we therefore assumed that shoes did not affect the results of our study. Third, we included patients with a radiographic grade of OA ranging from I to IV on the Kellgren and Lawrence scale. Half of the patients had radiographic evidence of moderate knee OA. A study by Shimada and colleagues [25] reported that insoles have the greatest effect on knee adduction moment in early to mild OA (Kellgren and Lawrence Grade I–II). Our subgroup analysis showed no difference in effect sizes between the mild and moderate OA groups. However, our subgroup analysis might be underpowered and, therefore, the results may be an underestimation of the actual effect size.
In addition, patients who were compliant were defined a priori as patients using the insole or brace more than 42 hours per week (7 days times 6 hours, which represents 75% of the working day). The optimal time to wear an insole or brace during the day has not been determined, and compliance remains arbitrary. Therefore, this arbitrarily chosen threshold could affect the conclusions of our subgroup analysis. Lastly, the degree of valgus moment provided by the braces depended on the degree of malalignment and the acceptance of the patient. Patients were instructed to wear the brace as long as tolerated. Both malalignment and acceptance vary between patients and, therefore, so will the degree of correction. No other reasonable option was available. As a result, less tolerant patients could benefit less from the therapy.
This study showed an immediate reduction in the mean peak knee adduction moment of 4% (± 10) as a result of a reduction in mean moment arm of 4% (± 13) in the insole group. No reduction of knee adduction moment was seen in the brace group. An immediate reduction of 4% in peak knee adduction moment in the insole group is similar to that reported in other studies. A recent review of the literature reported reductions ranging from 4% to 12% for the laterally wedged insole with an inclination of 5° [22]. It was not possible to compare our results of the valgus brace with the literature. Only a few small studies, which investigated different types of braces, are available and the effect sizes vary [7]. Reductions of the medial load found in our and other studies are small and, although statistically significant, it is doubtful whether these small differences are clinically meaningful. Multiple authors have suggested that even small increases or decreases in knee adduction moment could have substantial effects on the progression of OA [3, 26]. However, to the best of our knowledge, no study with a followup longer than 12 months has been performed so far. For this reason, in our opinion, it is still unknown whether these small reductions in peak or mean medial load actually have disease-modifying effects on the progression of OA. A long-term followup study is necessary to establish such an effect.
After 6 weeks of wearing insoles, no reduction of peak knee adduction moment and no reduction of moment arm were seen. No reduction of knee adduction moment, ground reaction force, or moment arm was seen in the brace group at baseline and after 6 weeks. So, laterally wedged insoles were shown to reduce the knee adduction moment at baseline; however, the effect could no longer be found after 6 weeks. Nonetheless, the clinical improvements, as measured by VAS knee pain and WOMAC scores, were still present at 6 weeks [26]. This temporary biomechanical effect has not been described previously. Most previous studies analyzed gait only once, at baseline [8, 10, 16].
Our subgroup analysis did not indicate a different biomechanical effect related to obesity, stage of OA, or and whether patients showed a clinical response to the insole or knee brace treatment at baseline or after 6 weeks. Our subgroup analysis might be underpowered; however, big between-group differences would not be expected. Theoretically, insoles could reduce the ground reaction force by a so-called “cushioning effect.” Although we used soft wedged insoles along the entire length of the foot, we did not observe a reduction of ground reaction force in our study. A frequently used treatment modality for reducing ground reaction force is weight loss. Persons who are overweight with varus alignment will benefit greater owing to the interaction between alignment and body mass on dynamic knee joint loading with the association between alignment and load highest in patients with the highest mass [17, 19]. One study reported that a reduction in body weight of 1 kg (10 N) was associated with a 1% reduction (0.496 Nm) in knee adduction moment [17]. In comparison with our results, in which we observed a reduction of 4% of peak knee adduction moment in the insole group, weight reduction should be highly effective.
To reduce knee adduction moment in patients with medial knee OA, either moment arm or ground reaction force should be reduced. Insoles and braces are supposed options for reducing moment arm, to decrease the medial compartment load. Laterally wedged insoles reduce knee adduction moment temporarily, but the reduction of moment arm, and thus the valgus effect, is doubtful. Two small studies that compared the knee adduction moment data of neutral versus laterally wedged insoles show conflicting effects of the lateral wedge, but the differences were small in both studies [1, 2].
We conclude that only laterally wedged insoles result in a reduced mechanical load of the medial compartment, albeit temporarily. After 6 weeks of wearing, no reduced mechanical load was seen. The valgus knee brace did not result in a reduced mechanical load of the medial compartment at baseline and after 6 weeks. Thus, in this study we found no biomechanical argument to support the use of laterally wedged insoles or a valgus knee brace.
Acknowledgments
We thank all participants for completing the measurements. We also thank M. van der Ent MSc, for his help with designing Fig. 4.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Erasmus University Medical Centre, Rotterdam, The Netherlands.
References
- 1.Abdallah AA, Radwan AY. Biomechanical changes accompanying unilateral and bilateral use of laterally wedged insoles with medial arch supports in patients with medial knee osteoarthritis. Clin Biomech (Bristol, Avon). 2011;26:783–789. [DOI] [PubMed]
- 2.Bennell KL, Bowles KA, Payne C, Cicuttini F, Williamson E, Forbes A, Hanna F, Davies-Tuck M, Harris A, Hinman RS. Lateral wedge insoles for medial knee osteoarthritis: 12 month randomised controlled trial. BMJ. 2011;342:d2912. doi: 10.1136/bmj.d2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bennell KL, Bowles KA, Wang Y, Cicuttini F, Davies-Tuck M, Hinman RS. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis. 2011;70:1770–1774. doi: 10.1136/ard.2010.147082. [DOI] [PubMed] [Google Scholar]
- 4.Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RM, Reijman M, Pols HA, Bierma-Zeinstra SM. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56:1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 5.Brouwer RW, Bierma-Zeinstra SM, van Raaij TM, Verhaar JA. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate. A one-year randomised, controlled study. J Bone Joint Surg Br. 2006;88:1454–1459. doi: 10.1302/0301-620X.88B11.17743. [DOI] [PubMed] [Google Scholar]
- 6.Brouwer RW, Jakma TS, Bierma-Zeinstra SM, Ginai AZ, Verhaar JA. The whole leg radiograph: standing versus supine for determining axial alignment. Acta Orthop Scand. 2003;74:565–568. doi: 10.1080/00016470310017965. [DOI] [PubMed] [Google Scholar]
- 7.Brouwer RW, Jakma TS, Verhagen AP, Verhaar JA, Bierma-Zeinstra SM. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev. 2005;1:CD004020. [DOI] [PubMed]
- 8.Draganich L, Reider B, Rimington T, Piotrowski G, Mallik K, Nasson S. The effectiveness of self-adjustable custom and off-the-shelf bracing in the treatment of varus gonarthrosis. J Bone Joint Surg Am. 2006;88:2645–2652. doi: 10.2106/JBJS.D.02787. [DOI] [PubMed] [Google Scholar]
- 9.Fantini Pagani CH Hinrichs M, Bruggemann GP. Kinetic and kinematic changes with the use of valgus knee brace and lateral wedge insoles in patients with medial knee osteoarthritis. J Orthop Res. 2012;30:1125–1132. doi: 10.1002/jor.22032. [DOI] [PubMed] [Google Scholar]
- 10.Hinman RS, Bowles KA, Metcalf BB, Wrigley TV, Bennell KL. Lateral wedge insoles for medial knee osteoarthritis: effects on lower limb frontal plane biomechanics. Clin Biomech. 2012;27:27–33. doi: 10.1016/j.clinbiomech.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Hunter D, Gross KD, McCree P, Li L, Hirko K, Harvey WF. Realignment treatment for medial tibiofemoral osteoarthritis: randomised trial. Ann Rheum Dis. 2012;71:1658–1665. doi: 10.1136/annrheumdis-2011-200728. [DOI] [PubMed] [Google Scholar]
- 12.Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res. 2002;20:101–107. doi: 10.1016/S0736-0266(01)00081-X. [DOI] [PubMed] [Google Scholar]
- 13.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerrigan DC, Lelas JL, Goggins J, Merriman GJ, Kaplan RJ, Felson DT. Effectiveness of a lateral-wedge insole on knee varus torque in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2002;83:889–893. doi: 10.1053/apmr.2002.33225. [DOI] [PubMed] [Google Scholar]
- 15.Krohn K. Footwear alterations and bracing as treatments for knee osteoarthritis. Curr Opin Rheumatol. 2005;17:653–656. doi: 10.1097/01.bor.0000175460.75675.d3. [DOI] [PubMed] [Google Scholar]
- 16.Maly MR, Culham EG, Costigan PA. Static and dynamic biomechanics of foot orthoses in people with medial compartment knee osteoarthritis. Clin Biomech. 2002;17:603–610. doi: 10.1016/S0268-0033(02)00073-6. [DOI] [PubMed] [Google Scholar]
- 17.Messier SP, Gutekunst DJ, Davis C, DeVita P. Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2005;52:2026–2032. doi: 10.1002/art.21139. [DOI] [PubMed] [Google Scholar]
- 18.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moyer RF, Birmingham TB, Chesworth BM, Kean CO, Giffin JR. Alignment, body mass and their interaction on dynamic knee joint load in patients with knee osteoarthritis. Osteoarthritis Cartilage. 2010;18:888–893. doi: 10.1016/j.joca.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 20.Parkes MJ, Maricar N, Lunt M, LaValley MP, Jones R, Segal NA, Takahashi-Narita K, Felson DT. Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: a meta-analysis. JAMA. 2013;310:722–730. doi: 10.1001/jama.2013.243229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramsey DK, Briem K, Axe MJ, Snyder-Mackler L. A mechanical theory for the effectiveness of bracing for medial compartment osteoarthritis of the knee. J Bone Joint Surg Am. 2007;89:2398–2407. doi: 10.2106/JBJS.F.01136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reeves ND, Bowling FL. Conservative biomechanical strategies for knee osteoarthritis. Nat Rev Rheumatol. 2011;7:113–122. doi: 10.1038/nrrheum.2010.212. [DOI] [PubMed] [Google Scholar]
- 23.Richards JD, Sanchez-Ballester J, Jones RK, Darke N, Livingstone BN. A comparison of knee braces during walking for the treatment of osteoarthritis of the medial compartment of the knee. J Bone Joint Surg Br. 2005;87:937–939. doi: 10.1302/0301-620X.87B7.16005. [DOI] [PubMed] [Google Scholar]
- 24.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 25.Shimada S, Kobayashi S, Wada M, Uchida K, Sasaki S, Kawahara H, Yayama T, Kitade I, Kamei K, Kubota M, Baba H. Effects of disease severity on response to lateral wedged shoe insole for medial compartment knee osteoarthritis. Arch Phys Med Rehabil. 2006;87:1436–1441. doi: 10.1016/j.apmr.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 26.van Raaij TM, Reijman M, Brouwer RW, Bierma-Zeinstra SM, Verhaar JA. Medial knee osteoarthritis treated by insoles or braces: a randomized trial. Clin Orthop Relat Res. 2010;468:1926–1932. doi: 10.1007/s11999-010-1274-z. [DOI] [PMC free article] [PubMed] [Google Scholar]