Abstract
Injuries continue to be the leading cause of death for the first four decades of life. These injuries result from a confluence of behavioral, physical, structural, environmental, and social factors. Taken together, these illustrate the importance of taking a broad and multileveled approach to injury prevention. Using examples from fall, fire, scald, and poisoning-related injuries, this article illustrates the utility of an approach that incorporates a social–environmental perspective in identifying and selecting interventions to improve the health and safety of individuals. Injury prevention efforts to prevent home injuries benefit from multilevel modifications of behavior, public policy, laws and enforcement, the environment, consumer products and engineering standards, as demonstrated with Frieden’s Health Impact Pyramid. A greater understanding, however, is needed to explain the associations between tiers. While interventions that include modifications of the social environment are being field-tested, much more work needs to be done in measuring social–environmental change and in evaluating these programs to disentangle what works best.
Keywords: falls, fire, Health Impact Pyramid, injury prevention, poisonings
The Burden of Injuries
Injuries continue to be the leading cause of death for the first four decades of life. Following motor vehicles, the home is the second most common location for fatal injuries in the United States (Runyan, Casteel, et al., 2005). The burden and costs of injuries at home are substantial. There are approximately 30,000 unintentional injury–related deaths at home each year (Mack, Rudd, Mickalide, & Ballesteros, 2013), and there are an average of 21 million medical visits made each year because of home injuries (Runyan, Perkis, et al., 2005). Leading causes of unintentional home injury deaths include falls, poisonings, and fire/burns. Together, these comprise 86% of all unintentional home injury deaths (Mack, Rudd, et al., 2013).
Home injuries result from a confluence of behavioral, physical, structural, environmental, and social factors, illustrating the importance of taking a broad multilevel approach to injury prevention that recognizes reciprocity between the person and the environment, as well as interdependence between points of intervention (Green & Kreuter, 2010). The objective of this manuscript is to illustrate the efficacy of this approach by focusing on several major causes of injuries in the home environment.
Conceptual Framework
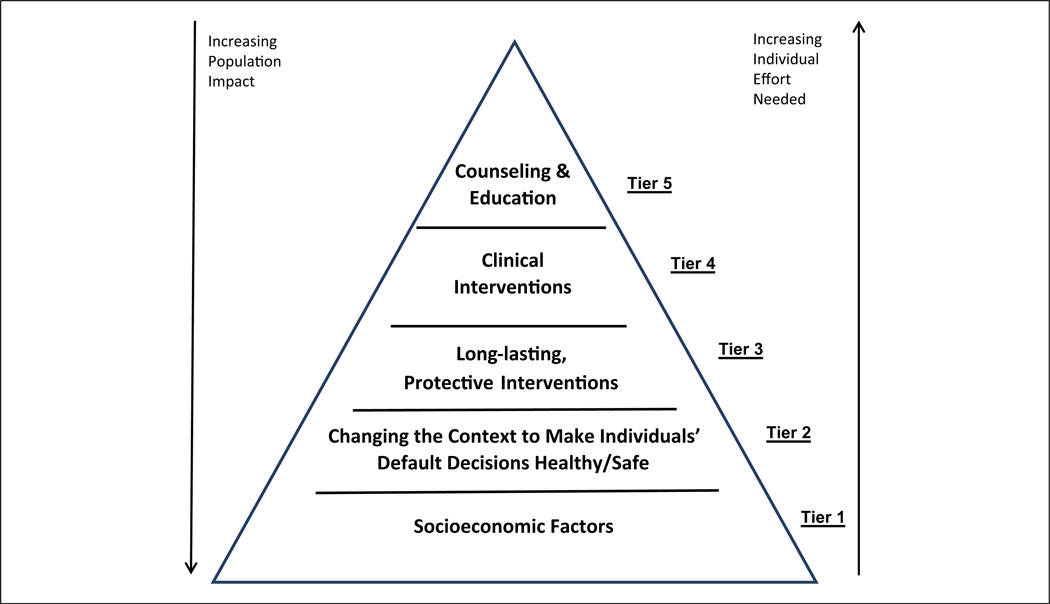
Recently, Frieden (2010) introduced a useful way to conceptualize and understand the potential public health impact of interventions. Briefly, he proposed a five-tiered Health Impact Pyramid (HIP), with interventions having the greatest population impact along the bottom tier and those with more limited broad public health impact at the top (Figure 1). Public health action and interventions represented by the bottom tier of the HIP require less individual effort. Programs at the higher tiers achieve limited public health impact largely because of their dependence on long-term individual behavior change and challenges of scalability. In other words, it is a challenge to introduce and scale up a program to larger and larger segments of the population that may require a tailored and culturally adapted modification to the intervention. And there may be substantial costs for that method. Frieden notes that making the “default” choice healthy and safe is essential while understanding that there is a natural tension between protection and personal freedom. The core tenets of the HIP apply to all public health problems— including injury prevention in the home.
Figure 1.
Health Impact Pyramid.
Note. Adapted from Frieden (2010).
In Frieden’s HIP, efforts to address socioeconomic factors are at the base. The exact mechanism by which socioeconomic factors exert an effect on health are not always apparent, but poverty, low educational attainment, and relative deprivation can increase the exposure to environmental hazards. By the same token, socioeconomic factors also influence exposure to specific injury hazards, in the form of unsafe housing, neighborhood crime, inadequate access to preventive health care, increased crowding, and unaffordable safety devices.
The next tier up from the base includes public health interventions that change the environmental context for health and safety. These are generally policies to ensure safe products and environments, ensuring that the healthiest choice is the easiest choice to make. Interventions at this tier are hard to defeat. The third tier involves one-time protective interventions that can have long-term benefits. The fourth tier of the HIP involves direct clinical care that identifies potential risk and can modify care to reduce the risk of injury. At the top of the HIP are counseling and education practices.
Ideally, public health action for injury prevention engages all five tiers of the HIP to maximize synergy and the likelihood of long-term success. Some urge caution as not to lose sight of the interdependence of the levels (Green & Kreuter, 2010). Others argue that it is optimal to engage the levels simultaneously (Northridge & Freeman, 2011).
Intervention Strategies
There are some compelling examples illustrating the potential of addressing multiple tiers of the HIP for injury prevention. In this section, we review knowledge about selected programs and policies as a means of preventing home injuries. We focus on falls, fires and burns, scalds, and poisonings as these are some of the leading causes of injury-related morbidity and mortality in the home.
Fall Injury Prevention
Falls are a leading cause of home injuries (Mack, Rudd, et al., 2013; Runyan, Perkis, et al., 2005). Among children, young age (≤0–6 years), male gender, and low socioeconomic status have been shown to be risk factors for fall injuries among children (Mao, McKenzie, Xiang, & Smith, 2009). Important fall-related hazards for children in the home include baby walkers, stairs, windows above ground level, bathrooms, and certain furniture (Mack, Gilchrist, & Ballesteros, 2008; McDonald, Girasek, & Gielen, 2012). Beds have been identified as the leading product involved in injuries in infants, and as the leading product in the percentage of nonfatal home injury costs for children under 5 years of age (Mack, Gilchrist, & Ballesteros, 2007; Zaloshnja, Miller, Lawrence, & Romano, 2005). Outside play equipment, including play sets and trampolines, can also be dangerous for children. Residential hazards associated with falls among children include a lack of safety devices such as properly installed and used safety gates or window guards and structural defects (e.g., uneven floors; insufficient surfacing under play equipment).
Although few child fall prevention interventions have been rigorously evaluated, individual studies have suggested positive results. Voluntary regulations to extend the width of walkers (so as to not fit through doorways) and to modify the base to prevent tip-overs (Tier 2 “hard to defeat” interventions) were effective (Rodgers & Leland, 2008). Installing stair-gates has also been shown to be an effective home-based intervention (Kendrick et al., 2008). Other interventions that may help to prevent childhood fall injuries include window guards and window locks for windows above ground level (Tier 3) and balcony railings less than 4 inches apart (Tier 2). The evidence that window guards reduce childhood morbidity and mortality from falls comes primarily from dramatic results following a community-wide program to provide window guards in high-risk apartments, where falls declined 50% in the 2 years after the program’s inception (Barlow, Niemirska, Gandhi, & Leblanc, 1983; Spiegel & Lindaman, 1977). Building codes that require safe stair and balcony design and other home modifications are likely to be effective for fall prevention since they remove the need for home dwellers to modify their home for safety or to continually act to be safe—they make the default decision safety (Tier 2 of the HIP).
Among older adults, the leading cause of home unintentional injury death is falls. Individual behaviors and physical ability levels are important factors contributing to falls in older adults (Lord, Menz, & Sherrington, 2006; Stevens, Noonan, & Rubenstein, 2009), but falls in the home can also be prevented by recognizing and modifying home hazards and using key safety features. Structural residential hazards associated with falls among older adults include lack of handrails on stairs, lack of grab bars and nonslip surfaces in the bathroom, tripping or slipping hazards (e.g., throw rugs, waxed flooring), outdoor steps, inadequate lighting, and the presence of electrical or telephone cords in the walkway (Carter, Campbell, Sanson-Fisher, Redman, & Gillespie, 1997; Rosen, Mack, & Noonan, 2013). Homes can be designed and constructed to protect elderly occupants from fall-related injuries. The evidence that structural modifications, such as installation of handrails, grab bars, and improved lighting are promising interventions for reducing risk of falls among older adults comes from two systematic reviews (Gillespie et al., 2012; Turner et al., 2011). Fall prevention strategies that have been most effective have engaged multifaceted community-based approaches that consider the multiple causative factors in falls (individual and physical features—Tiers 2–5 of the HIP; Stevens, 2010).
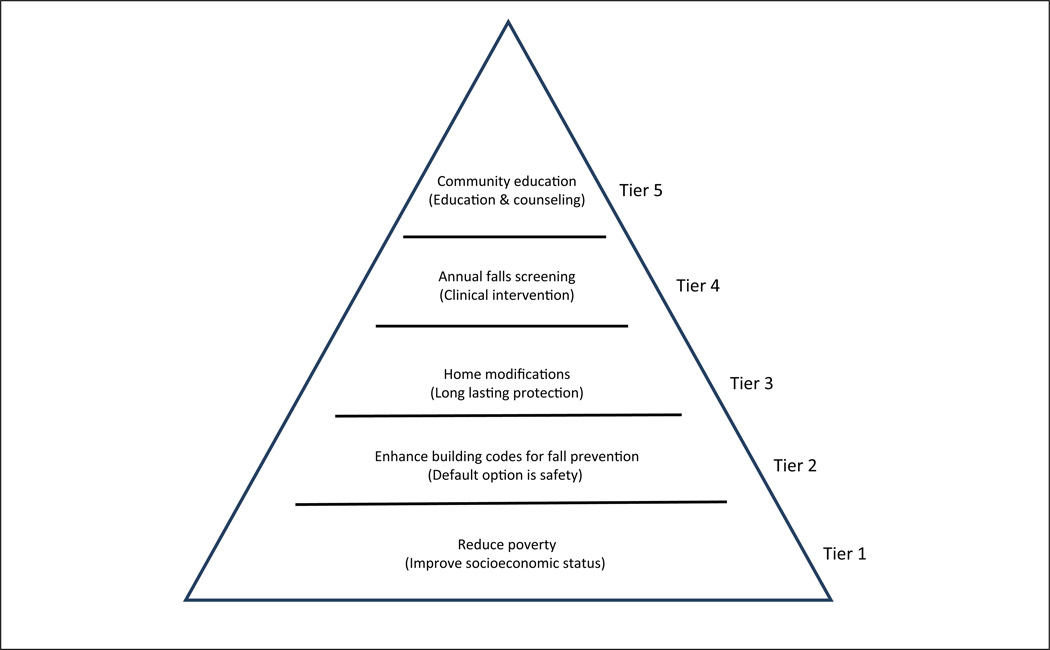
Older adult fall prevention activities could feasibly cover all tiers of the HIP and are illustrated in Figure 2. For example, at the base (Tier 1) reducing poverty can contribute to better living standards (including living in safer housing that incorporates up-to-date safety specifications). Enhancing building codes for safer stair design, including requiring hand rails on both sides of the stairs, is an example of Tier 2 level change that is somewhat difficult to defeat (hand rails would be difficult to remove). Some fall prevention programs work with older persons to remove home fall hazards, such as throw rugs. The removal of the rug is an example of a home modification that could have long-lasting protective impact (Tier 3), although an individual or new tenant could purchase a new throw rug. Effective screening, polypharmacy review, and the use of electronic medical records are examples of a Tier 4 strategy for older adult fall prevention (clinical intervention). These interventions, however, are limited by access to screenings, adherence to medical advice, and widespread implementation. While individually effective, the population-level impact of screening, poly-pharmacy review, and electronic health record use would be limited. Finally, community programs that provide educational sessions to older persons (Tier 5, counseling and education) may spur the individual to take action, but consistent and repeated messaging would be needed to have large population impact. Current fall prevention programs often engage multiple levels of the HIP at the same time (e.g., Stepping On fall prevention program (http://www.cdc.gov/HomeandRecreationalSafety/Falls/compendium/3.1_steppingon.html). Stepping On is a community-based program that combines education with action such as enhancing balance and strength, providing medication review, conducting vision screening, and assessing and remediating home hazards.
Figure 2.
Health Impact Pyramid for older adult fall prevention.
Note. Adapted from Frieden (2010).
Fire and Burn Injury Prevention
A primary risk factor for death and injury in residential fires is an absent or nonworking smoke alarm (Ballesteros & Kresnow, 2007; Istre, McCoy, Osborn, Barnard, & Bolton, 2001). Those at high risk of death due to fire or heightened difficulty in benefiting from smoke alarms include children 4 years and younger, older adults, those living in poverty, people with hearing, vision, or other physical or mental limitations or disabilities, and smokers (Istre et al., 2001). Households with income below the poverty level, with lower levels of education attainment, and those with older or no children were less likely to have a smoke alarm (Warda, Tenenbein, & Moffatt, 1999a). Additional groups at high risk for dying in a house fire include African Americans and people who live in substandard homes where emergency egress is often compromised (U.S. Fire Administration, 2006). Studies show that even though 90% of homes in the United States have smoke alarms, about one quarter are not functional (Ballesteros & Kresnow, 2007; Hannon & Shai, 2003).
Homes that are built according to strict building codes that address fire-safe material and construction, electrical specifications, and residential sprinklers protect residents regardless of basic socioeconomic factors (Insurance Institute for Business & Home Safety, 2011). Requiring all structures to conform to a minimum fire-safety code makes safety the default choice—Tier 2 of the HIP. That is not to say that codes eliminate socioeconomic differences in housing relative to fire risk, but rather, they can act to mitigate levels of risk (Gielen et al., 2012; U.S. Surgeon General, 2009). To be effective, building codes need to be enforced and updated, and older housing stock would need to be brought up to current code standards. Broad programs to make safe homes available to low-income families (bottom tier of HIP) have been successful in reducing injuries (Phelan et al., 2011).
Smoke alarms are a strong tool in the arsenal of fire safety (Ahrens, 2014). Codes or regulations that require smoke alarms (see http://www.ncsl.org/research/environment-and-natural-resources/smoke-and-carbon-monoxide-alarms-codes.aspx) can affect population health for a small investment. This benefit can occur outside of state and local regulations, for example, smoke alarms are required in all units owned by the U.S. Department of Housing and Urban Development (HUD) and all HUD-associated rental units. Smoke alarms fall into Tier 3 of the HIP because these protective interventions typically require some level of interaction with the resident. This may include installation and periodically testing the alarm to make sure it is operational and responding when the alarm sounds. And, unfortunately traditional smoke alarms did not require great effort to avoid the benefit. It was common to remove the battery to avoid nuisance alarms. Newer alarms are manufactured with long-lasting batteries sealed inside and the entire unit is replaced when the battery runs out, making it harder to defeat the protection. Alternatively, smoke alarms can be hardwired into the home’s electrical system, making it even more effective as a long-lasting protection.
Residential sprinklers are also a promising strategy to prevent deaths and injuries due to fires (Hall, Ahrens, & Evarts, 2012; U.S. Fire Administration, 2008) and are gaining greater acceptance as a feature of new home construction, although families may be reluctant to retrofit their homes because of perceptions of high cost (National Fire Protection Association, 2009). Furthermore, these systems are also relatively difficult to defeat and fit then within Tier 2 (for state requirements see http://www.firesprinklerinitiative.org/legislation/sprinkler-requirements-by-state.aspx).
It is critical, however, to pair improved access to fire safety products such as smoke alarms with fire safety education (HIP Tier 5) as education plays several key roles (Gielen, Sleet, & DiClemente, 2006). First, residents must know when they need a smoke alarm, where to purchase it, how to install it, and what to do when an alarm sounds. Only 23% of homes in the United States have a fire escape plan and practice it, yet all residents need to be prepared to exit a home when a smoke alarm sounds (Ballesteros & Kresnow, 2007). The fire escape plan should include at least two different ways of escape for each household resident and egress routes should not be blocked. A safe place should be designated outside of the home to meet after escaping the fire. Second, education is helpful in increasing the number of families with a functional smoke alarm (Kendrick et al., 2009). Both styles of smoke alarms (battery or hardwired) need to be checked regularly, and public service announcement reminders are often timed to coincide with when clocks are reset to daylight or standard times.
Public health interventions currently employed to reduce fire-related injuries and deaths fall largely within Tiers 5, 3, and 2 of the HIP. Pairing Tier 5 with interventions in Tiers 3 and/or 2 is an example of the interdependence between tiers so often necessary to achieve maximum impact (Warda, Tenenbein, & Moffatt, 1999b).
Scald Injury Prevention
Scalds and thermal and electrical burns are another outcome of home injuries. Between 1997 and 2002, 78,000 infants and toddlers were treated annually in ambulatory care settings for injuries due to contact with a hot object or substance (Hammig & Ogletree, 2006). Exposure in an adult for 2 seconds to water at a temperature of 150°F can result in a third-degree burn, and for children it can happen even more quickly (Diller, 2006).
Scald injuries can be prevented. Five years after a 1983 Washington State law required new water heaters to be pre-set at 120°F at the factory, 77% of homes tested had safe tap water temperatures accompanied by a reduction in the frequency, morbidity, and mortality of tap water burn injuries in children (Erdmann, Feldman, Rivara, Heimbach, & Wall, 1991). This is a clear example of a change in Tier 2 of the HIP, making the default action safer leading to improved outcomes. Individuals do not, however, have to expend significant effort to change the default. Therefore, home safety education (Tier 5) should also be employed to increase the proportion of families that have a safe hot tap water temperature (Babul, Olsen, Janssen, McIntee, & Raina, 2007; Kendrick et al., 2009). Some successful strategies to teach to decrease scalds include setting the temperature in water heaters to 120°F or lower; installing hot water temperature limiters at the faucet; using roll up cords for electric coffee pots; and using pots, pans, and kettles designed to be less likely to tip and spill hot liquids (Staunton, Frumkin, & Dannenberg, 2007). These strategies incorporate a mix of Tier 3 strategies (long-lasting protective interventions) and Tier 2 (changing the context to make safety hard to defeat) of Frieden’s HIP. However, Tier 5 strategies (education and counseling) can be important adjuncts to improve consumer (proper) use and to encourage policy makers and manufacturers’ behavior.
Poisoning Prevention
The majority of poisoning deaths in the United States are unintentional and rates have been rising steadily since 1992. The American Association of Poison Control Centers reports that there were more than 2.2 million poisoning exposures in 2012 (Mowry, Spyker, Cantilena, Bailey, & Ford, 2013). Males have higher rates of poisoning death than females across all age groups, although the rate for females has been rising rapidly (Mack, Jones, & Paulozzi, 2013). Much of the change in poisoning-related deaths among adults, however, comes as a result of changes in prescription drug use and prescribing. And although many poisoning exposures occur in the home regardless of age, we focus this section on poisonings among children as the decline in their poisonings demonstrates how the HIP works to achieve success.
According to the 30th annual report of the American Association of Poison Control Centers National Poison Data System (NPDS; Mowry et al., 2013), most common exposures for children under age 5 years were ingestion of household products, such as cosmetics and personal care products, analgesics, household cleaning substances, foreign bodies/toys/miscellaneous, and topical preparations. Data from the Centers for Disease Control and Prevention (2012) show that there were only 42 fatal unintentional poisonings reported for children aged 0 to 4 years in 2012.
Studies show clear declines in poisonings after the passing of the Poison Prevention Packaging Act (PPPA) in 1970 (Clarke & Walton, 1979; Walton, 1982), which required a number of household substances to be packaged in child-resistant packaging. One study, however, revealed that a substantial number of the post-PPPA poisonings (as high as 40%) were due to either improperly secured safety caps or products that were not required to be packaged in a child-resistant container (Rodgers, 1996). While the safety caps allowed for the default of safety, safe behaviors are still needed to keep the caps on the bottles and not transfer the contents of the bottles to other containers (Tier 3 HIP).
Besides safety caps, other packaging of medication has shown to be important. This includes the use of unit-dose packaging where one pill or unit of medication resides in a see-through plastic blister (McDonald et al., 2012). To access the product, one has to force through the paper or foil backing. Poisonings can be averted by increasing the strength of the backing so that a child could not push through (Tier 2 HIP) but also by the sheer fact there is only one pill or unit of medication available, making it unable to defeat (McDonald et al., 2012). Using annual reports from the American Association of Poison Control Centers, Tenenbein (2005) showed that there was a decrease in the incidence of non-intentional ingestion of iron by young children and a decrease in the mortality of poisoning by iron after unit-dose packaging was first introduced. This research helped validate unit-dose packaging as an effective strategy for the prevention of iron poisoning and iron poisoning deaths in young children.
In addition to lower levels of Frieden’s HIP playing important roles in poisoning prevention for children, higher levels have contributions as well. Tier 3 of the HIP includes parents and other caregivers storing medications and other poisonous substances away from children, preferably locked in inaccessible cabinets or drawers. Doing this however, does not negate the importance of parental supervision. Schillie, Shehab, Thomas, and Budnitz (2009) used the National Electronic Injury Surveillance System (NEISS) to estimate the number of medication overdoses of children leading to emergency department visits. The results showed that four-fifths (or 82.2%) of the overdoses of children ≤18 years of age were from unsupervised ingestions and nearly all (97%) of the medication overdose cases of children aged 1 to 5 years were due to unsupervised ingestions. The authors contend that since young children have such curiosity and engage in hand-to-mouth behavior, engineering strategies such as unit-dose packaging and use of adaptors on bottles of liquid medication that serve as a needleless syringe and provide less content, are important. Tier 4 is demonstrated by the availability of clinical support from Poison Control Centers (universal phone number 1-800-222-1222), pediatricians, and other health care professionals; however, clinical intervention is prompted by telephone-related counseling and education (Tier 5), demonstrating the interdependency needed for impact. Educating children and parents about poisoning and poison prevention through community programs and interventions also demonstrates Tier 5 of the HIP, but may be limited by efficacy, reach, and scalability. Although implementing higher tiers of the HIP alone may not lead to clear declines in poisonings, their use in combination with lower levels will strengthen the overall impact. For example, while child-resistant caps on medicine may be a Tier 3 strategy (long-lasting protective intervention), supervisors of children will still need be vigilant to insure that lids on medicines are replaced after opening. Again, this illustrates the importance of Tier 5 strategies to educate and counsel parents and providers.
Conclusions
Injuries are not accidents: they are predictable and like many diseases, preventable. Injuries are related to many factors that span individual, interpersonal, organizational, community, and societal determinants. Effectively managing context by implementing the most appropriate mix of strategies is a critical factor for success (Hanson, Finch, Allegrante, & Sleet, 2012). While the HIP can illustrate the relative influence of five categories of interventions, their interdependence and synergistic effect cannot be overlooked (Green & Kreuter, 2010). Injury prevention, like other health problems, is most effectively addressed using a multilevel perspective (McLeroy, Bibeau, Steckler, & Glanz, 1988).
The costs and consequences of home injuries are significant, both on families and society. Injury prevention efforts to prevent home injuries will benefit from changes in behavior, public policy, laws and enforcement, environmental change, as well as improvements in consumer products and engineering standards. While injury statistics guide our practice and research to prevent home injuries, a more powerful force are the people behind the statistics whose lives can be spared and whose disabilities can be prevented. Reducing poverty, changing the social and environmental context (making the safe choices easy choices or the default ones), implementing one-time interventions that last, delivering clinical interventions, and providing essential counseling and education to facilitate individual behavior change are keys to effective home injury prevention.
While interventions that include modifications of these factors are being field-tested, much more work needs to be done in measuring change and in evaluating programs that target the lower HIP tiers. In this context, understanding the important role for theories and theory-led interventions will be critical (Hayden, 2014), in addition to the prudent use of education and behavior change strategies that can support or promote structural and environmental change (Gielen, Sleet, & Parker, 2014). We can study the influence of such issues as cultural norms, socialization, social capital, concentration of poverty, and economic inequalities, on injury and its prevention, independent of the individual risk and protective factors involved; however, as Lieberman, Golden, and Earp (2013) point out, we must also be cognizant of the potential that structural and environmental change in the lower tiers of HIP may ignore or de-empower individuals and communities because “… efforts to tweak physical, social, economic, or political conditions in order to produce behavior change, without the active engagement of the individual affected, reflect a decision to prioritize certain choices over others” (Lieberman et al., 2013, p. 522).
We do not always need to wait for a complete understanding of what causes a condition to advance prevention. There are often natural experiments that arise out of a community’s desire to address social issues for reasons other than injury prevention that provide the opportunity to understand a multitude of interrelated factors and their relation to injury. For example, can poverty reduction or job-training programs also prevent child injury? Do efforts to provide social support to parents reduce unintentional childhood injury and maltreatment? How can efforts in the top tiers of HIP support or enhance efforts in the lower tiers? Studying the effect of programs and policies such as these can also inform our understanding of the pathways connecting the social environment and injury. Modifications that change the socio environmental conditions and those that make healthy and safe choices the default option (notably the lower two tiers of the HIP) hold the most promise to stimulate large populations changes in injuries. But as Green and Kreuter (2010) point out in their response to Frieden’s HIP, selecting among the various tiers of the pyramid “… might create an ‘either/or’ rather than an ‘and’ mentality about intervention strategies, losing sight of their interdependence” (p. 1824). Research and programmatic development across levels in the HIP, and investigating the interdependence between the levels, can lead to new discoveries, paradigms, and theories that will hold great potential for advancing the goal to reduce morbidity and mortality from home injuries even further.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
This article is part of a Health Education & Behavior supplement, “The Evidence for Policy and Environmental Approaches to Promoting Health,” which was supported by a grant to the Society for Public Health Education (SOPHE) from the Robert Wood Johnson Foundation.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplement Issue Note
The entire supplemental issue is open access at http://heb.sagepub.com/content/42/1_suppl.toc.
References
- Ahrens M. Smoke alarms in U.S. Home fires. 2014 Retrieved from http://www.nfpa.org/~/media/Files/Research/NFPA%20reports/Fire%20Protection%20Systems/ossmokealarms.pdf. [Google Scholar]
- Babul S, Olsen L, Janssen P, McIntee P, Raina P. A randomized trial to assess the effectiveness of an infant home safety programme. International Journal of Injury Control and Safety Promotion. 2007;14:109–117. doi: 10.1080/17457300701272474. [DOI] [PubMed] [Google Scholar]
- Ballesteros MF, Kresnow MJ. Prevalence of residential smoke alarms and fire escape plans in the U.S.: Results from the Second Injury Control and Risk Survey (ICARIS-2) Public Health Reports. 2007;122:224–231. doi: 10.1177/003335490712200212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow B, Niemirska M, Gandhi RP, Leblanc W. Ten years of experience with falls from a height in children. Journal of Pediatric Surgery. 1983;18:509–511. doi: 10.1016/s0022-3468(83)80210-3. [DOI] [PubMed] [Google Scholar]
- Carter SE, Campbell EM, Sanson-Fisher RW, Redman S, Gillespie WJ. Environmental hazards in the homes of older people. Age & Ageing. 1997;26:195–202. doi: 10.1093/ageing/26.3.195. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Injury prevention and control: Data & Statistics. 2012 (Web-based Injury Statistics Query and Reporting System [WISQARS]). Retrieved from http://www.cdc.gov/injury/wisqars.
- Clarke A, Walton WW. Effect of safety packaging on aspirin ingestion by children. Pediatrics. 1979;63:687–693. [PubMed] [Google Scholar]
- Diller KR. Adapting adult scald safety standards to children. Journal of Burn Care & Research. 2006;27:314–322. doi: 10.1097/01.BCR.0000216473.50837.12. [DOI] [PubMed] [Google Scholar]
- Erdmann TC, Feldman KW, Rivara FP, Heimbach DM, Wall HA. Tap water burn prevention: The effect of legislation. Pediatrics. 1991;88:572–577. [PubMed] [Google Scholar]
- Frieden TR. A framework for public health action: The health impact pyramid. American Journal of Public Health. 2010;100:590–595. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen A, Shields W, McDonald E, Frattaroli S, Bishai D, Ma X. Home safety and low-income urban housing quality. Pediatrics. 2012;130:1053–1059. doi: 10.1542/peds.2012-1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen A, Sleet DA, Parker E. Unintentional injury and behavior change. In: Kahan S, Gielen CA, Fagan PJ, Green LW, editors. Health behavior change in populations. Baltimore, MD: Johns Hopkins University Press; 2014. pp. 294–315. [Google Scholar]
- Gielen A, Sleet D, DiClemente R. Injury and violence prevention: Behavioral science theories, methods, and applications. 1st ed. San Francisco, CA: Jossey-Bass; 2006. [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green LW, Kreuter MW. Evidence hierarchies versus synergistic interventions. American Journal of Public Health. 2010;100:1824–1825. doi: 10.2105/AJPH.2010.197798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JR, Jr, Ahrens M, Evarts B. Sprinkler impact on fire injury. Quincy, MA: National Fire Protection Association; 2012. Fire Protection Research Foundation Rep.). Retrieved from http://www.nfpa.org/research/fire-protection-research-foundation/reports-and-proceedings/suppression/home-fire-sprinklers/sprinkler-impact-on-fire-injury. [Google Scholar]
- Hammig BJ, Ogletree RJ. Burn injuries among infants and toddlers in the United States, 1997–2002. American Journal of Health Behavior. 2006;30:259–267. doi: 10.5555/ajhb.2006.30.3.259. [DOI] [PubMed] [Google Scholar]
- Hannon L, Shai D. The truly disadvantaged and the structural covariates of fire death rates. Social Science Journal. 2003;40:129–136. [Google Scholar]
- Hanson DW, Finch CF, Allegrante JP, Sleet D. Closing the gap between injury prevention research and community safety promotion practice: Revisiting the public health model. Public Health Reports. 2012;127:147–155. doi: 10.1177/003335491212700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden J. Introduction to health behavior theory. 2nd ed. Burlington, MA: Jones & Bartlett Learning; 2014. [Google Scholar]
- Insurance Institute for Business & Home Safety. Rating the states Atlantic and Gulf Coast states. An assessment of residential building code and enforcement systems for life safety and property protection in hurricane-prone regions. 2011 Retrieved from http://www.disastersafety.org/wp-content/uploads/ibhs-rating-the-states.pdf. [Google Scholar]
- Istre GR, McCoy MA, Osborn L, Barnard JJ, Bolton A. Deaths and injuries from house fires. New England Journal of Medicine. 2001;344:1911–1916. doi: 10.1056/NEJM200106213442506. [DOI] [PubMed] [Google Scholar]
- Kendrick D, Smith S, Sutton AJ, Mulvaney C, Watson M, Coupland C, Mason-Jones A. The effect of education and home safety equipment on childhood thermal injury prevention: Meta-analysis and meta-regression. Injury Prevention. 2009;15:197–204. doi: 10.1136/ip.2008.020677. [DOI] [PubMed] [Google Scholar]
- Kendrick D, Watson MC, Mulvaney CA, Smith SJ, Sutton AJ, Coupland CA, Mason-Jones AJ. Preventing childhood falls at home: meta-analysis and meta-regression. American Journal of Preventive Medicine. 2008;35:370–379. doi: 10.1016/j.amepre.2008.06.038. [DOI] [PubMed] [Google Scholar]
- Lieberman L, Golden SD, Earp JA. Structural approaches to health promotion: What do we need to know about policy and environmental change? Health Education & Behavior. 2013;40:520–525. doi: 10.1177/1090198113503342. [DOI] [PubMed] [Google Scholar]
- Lord SR, Menz HB, Sherrington C. Home environment risk factors for falls in older people and the efficacy of home modifications. Age and Ageing. 2006;35(Suppl. 2):ii55–ii59. doi: 10.1093/ageing/afl088. [DOI] [PubMed] [Google Scholar]
- Mack KA, Gilchrist J, Ballesteros MF. Bunk bed–related injuries sustained by young children treated in emergency departments in the United States, 2001–2004, National Electronic Injury Surveillance System: All injury program. Injury Prevention. 2007;13:137–140. doi: 10.1136/ip.2006.013193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack KA, Gilchrist J, Ballesteros MF. Injuries among infants treated in emergency departments in the United States, 2001–2004. Pediatrics. 2008;121:930–937. doi: 10.1542/peds.2007-1731. [DOI] [PubMed] [Google Scholar]
- Mack KA, Jones C, Paulozzi LJ. Vital signs: Overdoses of prescription opioid pain relievers and other drugs among women—United States, 1999–2010. MMWR Morbidity and Mortality Weekly Report. 2013;62(26):537–542. [PMC free article] [PubMed] [Google Scholar]
- Mack KA, Rudd RA, Mickalide AD, Ballesteros MF. Fatal unintentional injuries in the home in the U.S., 2000–2008. American Journal of Preventive Medicine. 2013;44:239–246. doi: 10.1016/j.amepre.2012.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao SJ, McKenzie LB, Xiang H, Smith GA. Injuries associated with bathtubs and showers among children in the United States. Pediatrics. 2009;124:541–547. doi: 10.1542/peds.2008-2489. [DOI] [PubMed] [Google Scholar]
- McDonald E, Girasek D, Gielen A. Home injuries. In: Liller K, editor. Injury prevention for children and adolescents: Research, practice, and advocacy. Washington, DC: American Public Health Association; 2012. [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Mowry JB, Spyker DA, Cantilena LR, Jr, Bailey JE, Ford M. 2012 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th annual report. Clinical Toxicology. 2013;51:949–1229. doi: 10.3109/15563650.2013.863906. [DOI] [PubMed] [Google Scholar]
- National Fire Protection Association. Comparative analysis of housing cost and supply impacts of sprinkler ordinances at the community level. Quincy, MA: Author; 2009. Retrieved from http://www.firesprinklerinitiative.org/~/media/Fire%20Sprinkler%20Initiative/Files/Reports/FSI_Comparison_Analysis_Final_Report.pdf. [Google Scholar]
- Northridge ME, Freeman L. Urban planning and health equity. Journal of Urban Health. 2011;88:582–597. doi: 10.1007/s11524-011-9558-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan KJ, Khoury J, Xu Y, Liddy S, Hornung R, Lanphear BP. A randomized controlled trial of home injury hazard reduction: The HOME injury study. Archives of Pediatrics & Adolescent Medicine. 2011;165:339–345. doi: 10.1001/archpediatrics.2011.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers GB. The safety effects of child-resistant packaging for oral prescription drugs. Two decades of experience. JAMA Journal of the American Medical Association. 1996;275:1661–1665. [PubMed] [Google Scholar]
- Rodgers GB, Leland EW. A retrospective benefit-cost analysis of the 1997 stair-fall requirements for baby walkers. Accident Analysis & Prevention. 2008;40:61–68. doi: 10.1016/j.aap.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Rosen T, Mack KA, Noonan RK. Slipping and tripping: fall injuries in adults associated with rugs and carpets. Journal of Injury & Violence Research. 2013;5:61–69. doi: 10.5249/jivr.v5i1.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runyan CW, Casteel C, Perkis D, Black C, Marshall SW, Johnson RM, Viswanathan S. Unintentional injuries in the home in the United States Part I: Mortality. American Journal of Preventive Medicine. 2005;28:73–79. doi: 10.1016/j.amepre.2004.09.010. [DOI] [PubMed] [Google Scholar]
- Runyan CW, Perkis D, Marshall SW, Johnson RM, Coyne-Beasley T, Waller AE, Baccaglini L. Unintentional injuries in the home in the United States Part II: Morbidity. American Journal of Preventive Medicine. 2005;28:80–87. doi: 10.1016/j.amepre.2004.09.017. [DOI] [PubMed] [Google Scholar]
- Schillie SF, Shehab N, Thomas KE, Budnitz DS. Medication overdoses leading to emergency department visits among children. American Journal of Preventive Medicine. 2009;37:181–187. doi: 10.1016/j.amepre.2009.05.018. [DOI] [PubMed] [Google Scholar]
- Spiegel CN, Lindaman FC. Children can’t fly: A program to prevent childhood morbidity and mortality from window falls. American Journal of Public Health. 1977;67:1143–1147. doi: 10.2105/ajph.67.12.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staunton C, Frumkin H, Dannenberg A. Changing the built environment to prevent injury. In: Doll LS, Bonzo SE, Mercy JA, Sleet DA, editors. Handbook of injury and violence prevention. New York, NY: Springer; 2007. pp. 257–276. [Google Scholar]
- Stevens J. Atlanta, GA: Centers for Disease Conntrol and Prevention; 2010. A CDC compendium of effective fall interventions: What works for community-dwelling older adults. Retrieved from http://www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html. [Google Scholar]
- Stevens J, Noonan R, Rubenstein L. Older adult fall prevention: Perceptions, beliefs, and behaviors. American Journal of Lifestyle Medicine. 2009;4:16–20. [Google Scholar]
- Tenenbein M. Unit-dose packaging of iron supplements and reduction of iron poisoning in young children. Archives of Pediatrics & Adolescent Medicine. 2005;159:557–560. doi: 10.1001/archpedi.159.6.557. [DOI] [PubMed] [Google Scholar]
- Turner S, Arthur G, Lyons RA, Weightman AL, Mann MK, Jones SJ, Lannon S. Modification of the home environment for the reduction of injuries. Cochrane Database of Systematic Reviews. 2011;2:CD003600. doi: 10.1002/14651858.CD003600.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Fire Administration. Fire and the older adult. Washington, DC: Government Printing Office; 2006. (FA-300). [Google Scholar]
- U.S. Fire Administration. Home fire protection residential fire sprinkler systems save lives. 2008 (FA-43/February). Retrieved from http://www.usfa.fema.gov/downloads/pdf/publications/fa_43.pdf.
- U.S. Surgeon General. The Surgeon General’s call to action to promote healthy homes. Rockville, MD: Office of the Surgeon General (U.S.); 2009. [PubMed] [Google Scholar]
- Walton WW. An evaluation of the Poison Prevention Packaging Act. Pediatrics. 1982;69:363–370. [PubMed] [Google Scholar]
- Warda L, Tenenbein M, Moffatt ME. House fire injury prevention update. Part I. A review of risk factors for fatal and non-fatal house fire injury. Injury Prevention. 1999a;5:145–150. doi: 10.1136/ip.5.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warda L, Tenenbein M, Moffatt ME. House fire injury prevention update. Part II. A review of the effectiveness of preventive interventions. Injury Prevention. 1999b;5:217–225. doi: 10.1136/ip.5.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaloshnja E, Miller TR, Lawrence BA, Romano E. The costs of unintentional home injuries. American Journal of Preventive Medicine. 2005;28:88–94. doi: 10.1016/j.amepre.2004.09.016. [DOI] [PubMed] [Google Scholar]