Abstract
Objective
To determine the risk of difficulties with social communication and restricted/repetitive behaviors as well as the rate of autism in children institutionalized in early infancy and to assess the impact of a foster care intervention on ameliorating this risk.
Method
Children abandoned at birth and raised in institutions in Bucharest, Romania were randomly assigned to a care-as-usual group (institutional care, CAUG), or placed in family-centered foster care (FCG) as part of the Bucharest Early Intervention Project (BEIP). At approximately 10 years of age, the Social Communication Questionnaire (SCQ) was administered to caregivers of children in both groups, as well as to parents of a typically developing community sample (Never Institutionalized group, NIG) residing in Bucharest, Romania. Children scoring ≥ 12 on the SCQ underwent clinical evaluation for autism spectrum disorder (ASD).
Results
Caregivers of children with a history of institutionalization reported that these children had significantly more deviant behavior than never institutionalized children on all subdomains of the SCQ (all p<0.001). Children in the FCG had significantly lower scores on the SCQ than children in the CAUG (p<.001), particularly in the reciprocal social interaction domain, indicating that the intervention reduced problems in social communication. Three of 60 CAUG children, 2 of 57 FCG children, and none of the NIG children received a formal ASD diagnosis.
Conclusion
Early institutional rearing was associated with an increased risk of social communication difficulties and ASD. A family-centered foster care intervention improved social communication skills.
Keywords: institutional care, foster care, development, social communication, autism
Introduction
Children raised in institutions are at increased risk for a variety of adverse outcomes,1 including risk for “quasi-autistic” patterns of behavior.2, 3 In the English and Romanian Adoptees Study, quasi-autism was found in 11.1% of previously institutionalized children at 11–12 years of age.4 A similar disorder described as post-institutional autistic syndrome (PIAS) was found in 16% of previously institutionalized children adopted from Romania to the Netherlands at an average of 8 years of age.5 While children with these disorders have features overlapping with autism spectrum disorder (ASD) including social communication difficulties and repetitive behaviors,6, 7 the authors of those studies used the terms “quasi-autism” or PIAS to highlight several features seen in previously institutionalized children that differ from those often seen in “ordinary” ASD. These features include a general trend for decreasing severity of ASD features over time and an equal male:female ratio (compared to the 4:1 male:female ratio seen on average in other studies of ASD).8
Other studies, while not looking specifically at ASD, suggest that post-institutionalized children demonstrate behaviors often seen in ASD, including abnormalities in social approach, difficulties adjusting behavior to suit social context, and difficulties with peer relationships.4, 9–16 Children with a history of institutionalization also have an increased likelihood of demonstrating repetitive movements such as stereotypies.17
The Bucharest Early Intervention Project (BEIP), a randomized controlled trial of foster care versus institutional rearing, provides the opportunity to examine social communication abilities, restricted/repetitive behaviors, and presence of a diagnosis of ASD in institutionalized Romanian children randomly assigned to a continued institutional care-as-usual group (CAUG) or to a foster care intervention group (FCG). Similar to the studies by Rutter et al2, 4 and Hoksbergen et al,5 children in this study were placed in institutions early in life, most at birth. Because ASD cannot be reliably diagnosed in the newborn period or even in the first year of life even in countries where there is considerable awareness of the disorder,18, 19 it is unlikely that ASD was a reason for abandonment; instead, political pronatalist policies in the context of frequently insufficient financial and social support for child rearing led many children to be abandoned for social reasons.20, 21 Within institutions, medical determination of whether a child was “typically developing” or “handicapped” generally did not occur until the age of 3 years.22
Because of the random assignment to CAUG or FCG, the BEIP offers the unique opportunity to assess the extent to which foster care placement improved behaviors associated with autism, including social communication and restricted/repetitive behaviors. While prior studies in the BEIP have specifically examined attachment,15, 23, 24 teacher-rated social skills,16 and stereotypies,17 these findings are not always specific to ASD. No study has previously addressed the broad range of difficulties with social communication and restricted/repetitive behaviors specifically seen in ASD, nor the specific diagnosis of ASD, in a randomized sample.
The objectives of the current study are to: (1) describe the distribution of social communication difficulties and restricted/repetitive behaviors in children with a history of early institutional care, (2) evaluate the efficacy of a foster care intervention compared with continued institutional care in improving social communication and restricted/repetitive behaviors, and (3) investigate the prevalence of ASD in children with a history of early institutional care.
Method
Complete historical background, design, and ethical considerations of the BEIP have been previously described in detail.25–27 During the initial stages of the project, 187 children living in institutions in Bucharest, Romania, were initially evaluated by physical exam; those with obvious genetic syndromes, fetal alcohol syndrome, or microcephaly were excluded from the study. The remaining 136 children constituted the ever institutionalized group (EIG). Half of these children were randomly assigned to continued care-as-usual in the institution (CAUG), and the other half were randomized to a foster care group (FCG). Age at foster care placement in the FCG ranged from 7 to 33 months (Mean 22.6). Foster care was designed to replicate the home experience and caregiving quality that a never-institutionalized child received.27 A never-institutionalized community comparison group (NIG) was matched to the other groups by child age and gender.25
Institutional review boards at Boston Children’s Hospital, the University of Maryland, and Tulane University as well as the Institute for Maternal and Child Health and the local Commissions for Child Protection in Romania approved the study protocols. Informed consent was obtained from children’s legal guardians: biological parents, the local commissions for child protection, sector mayors, or adoptive parents. BEIP had a policy of noninterference, which meant that after randomization, child protection authorities could make decisions to alter placement; the most common result of this policy was that children in the CAUG were moved to family-centered care later in the study.28 All initial analyses in the current paper follow an intent-to-treat model, with children considered within their original assigned group. We performed follow-up analyses based on each child’s living situation, number of transitions between placements, and percent of life spent in an institution at the time of SCQ administration.
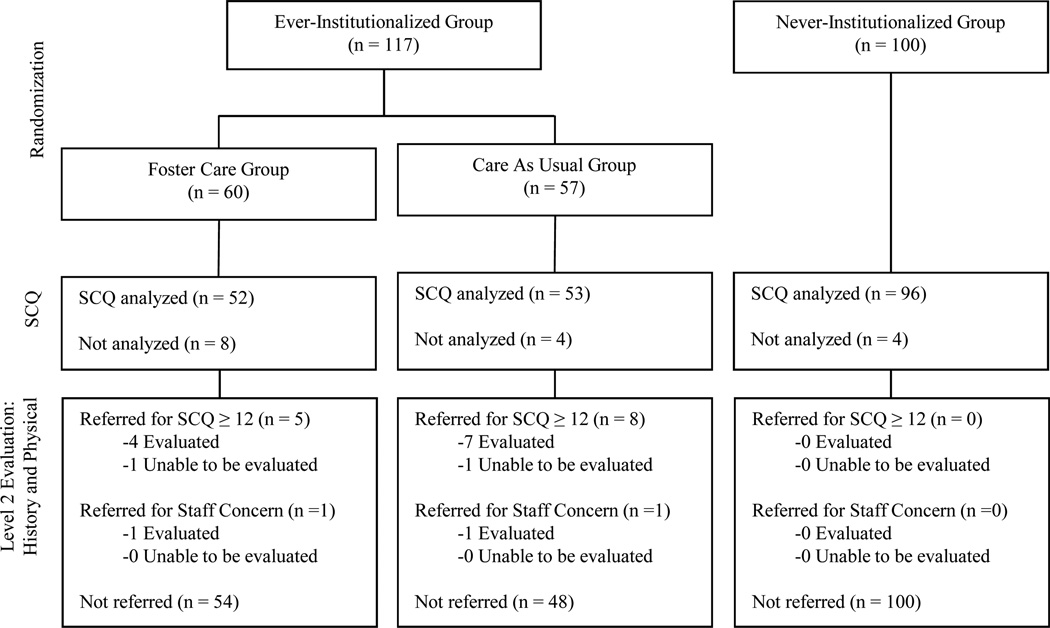
The Social Communication Questionnaire (SCQ; Western Psychological Services, 2003) is a validated parent-report screening measure that assesses for symptomatology associated with ASD.29 When each child was approximately 10 years of age (mean 10 years, range 8–11 years), the caregiver who knew the child best (biological parent, foster parent, adoptive parent or institutional caregiver) filled out the lifetime SCQ, which had been translated into Romanian and back-translated. With the SCQ, higher scores indicate more concerning behaviors, and a cutoff score of ≥15 is generally recommended as an indication of possible ASD. The manual also recommends using a slightly lower threshold in populations with other risk features. In this study, any child with an SCQ score ≥ 12 underwent a second level of evaluation. Additionally, BEIP psychologists who were familiar with the children in the study referred two children for whom they had clinical concern about possible ASD. The number of children from each group evaluated by the SCQ, referred due to clinical concern, and clinically evaluated for ASD is presented in Figure 1.
Figure 1.
Research and control participants evaluated at 8 years of age. Note: Children are shown undergoing Social Communication Questionnaire (SCQ) and subsequent autism spectrum disorder (ASD) evaluation, by group. Only children still participating in the study at age 8 are included here; reasons that some children discontinued participation are described elsewhere.33
Because the last half of the SCQ involves questions about the child’s behavior at 4–5 years of age, the SCQ was incomplete and thus not analyzed if the caregiver filling out the questionnaire did not have information about the child’s behavior at this age (FCG n = 5; CAUG n = 2). For one NIG participant, a parent refused to complete the questionnaire. For the remainder of children for whom the SCQ was not analyzed (FCG n = 3; CAUG n = 2; NIG n = 3) the SCQ was not completed because this questionnaire was added to the study protocol after the participant had completed his or her study visit. SCQ scores were also validated in our sample by assessing their correlation with scores on the Social Skills Rating System (SSRS),30 which measures social skills and problem behaviors through parent and teacher questionnaires, and academic competence through a teacher questionnaire.
The second level of evaluation involved an extensive history, physical examination, and structured observations of the child by a Romanian-speaking physician trained in the United States in ASD diagnosis. Diagnostic decisions were made using DSM-IV criteria,6 as the Autism Diagnostic Observation Schedule (ADOS) had not been validated in the Romanian language. DSM-5 criteria7 had not yet been published at the time of the examinations, but re-analysis of our data using DSM-5 criteria after their publication revealed no change in the number of research participants diagnosed with ASD.
Demographics of the groups, and placement status at the time of this study visit, are described elsewhere.1
IQ was measured using the Wechsler Intelligence Scale for Children (WISC-IV; Wechsler, 2003); results of IQ testing at 8 years of age in the BEIP have been described previously.31 Among children who had an SCQ completed, 9 children did not have a WISC completed (CAUG, n = 4; FCG, n = 3; NIG, n = 2). None of the children who received an ASD diagnosis had WISC scores available, as the children’s level of functioning precluded administration of the WISC.
Head circumference percentiles were based on reference data from 0–18 years of age.32
All data were analyzed using IBM SPSS Statistics, version 21. Two-tailed t-tests were used to compare SCQ scores between groups. Linear regression was used to evaluate the relationship between SCQ scores and potential confounders. Analysis of variance (ANOVA) with post hoc Bonferroni correction was used to compare SCQ scores by current living situation at the time of the study. Pearson correlations were used to examine the relationship between SCQ and SSRS scores, and between SCQ and WISC scores.
Living Situation at Time of Study Visit: The initial results described below follow an intent-to-treat model, with all children included in their originally assigned group; hence, the findings may be considered a conservative estimate of the effects of the intervention on SCQ scores. However, in the years since the study began, many children in the CAUG had moved to government foster care, and some children in the FCG had moved to non-BEIP family-centered living situations. At the time of data collection, 14 children remained institutionalized; SCQ data was available for 11 of these children. For the analysis by current living situation, children currently living in BEIP foster care (FCG, n = 33) were compared to children currently living in government foster care (CAUG, n = 16; FCG, n = 4), children reintegrated with their biological families (CAUG, n=19; FCG, n = 12), and children currently living in an institution (CAUG, n = 11). Similar analyses have been conducted previously when examining other developmental outcomes in the BEIP.31, 33
Results
SCQ Scores
All data reported here includes only participants for whom an SCQ was completed.
Children with a History of Institutionalization: Caregivers of children in the EIG reported higher scores (more problems) on the SCQ overall, and on each subdomain of the SCQ, than caregivers of children in the NIG (Table 1). Within the EIG, simple linear regression demonstrated that SCQ scores did not significantly correlate with the total number of placement transitions (R2= .000, B = -.054, Standard Error = .371, β = -.014). However, scores did correlate with the total percentage of a child’s life spent in an institution, even when controlling for demographics and birth history (R2 = .141, B = .110, Standard Error = .029, β = .381). Children who had spent a longer period of their lives in an institution at age 8 had higher SCQ scores.
Table 1.
Social Communication Questionnaire (SCQ) Scores and Subscores by Group
| Ever Institutionalized |
Never Institutionalized |
Ever Institutionalized Group | ||
|---|---|---|---|---|
| Care-As-Usual | Foster Care | |||
| Total SCQ Score | 3.50 (7.38)*** | 0.02 (0.14) | 4.96 (9.21)# | 2.08 (4.66) |
| Domain | ||||
| Reciprocal Social Interaction | 1.42 (3.33)*** | 0.01 (0.10) | 2.12 (4.19)§ | 0.75 (2.02) |
| Communication | 0.91 (1.88)*** | 0.00 (0.00) | 1.17 (2.25) | 0.68 (1.44) |
| Restricted, Repetitive, and Stereotyped Patterns of Behavior | 0.51 (1.38)*** | 0.00 (0.00) | 0.58 (1.57) | 0.43 (1.18) |
Note: CAUG = care-as-usual group; EIG = ever-institutionalized group; FCG = foster care group; NIG = never-institutionalized group.
Note: All scores are expressed as mean (SD).
p ≤ .001 EIG vs. NIG, two-tailed independent-samples t test
p ≤ .001 CAUG vs. FCG, two-tailed independent-samples t test
p ≤ .01 CAUG vs. FCG, two-tailed independent-samples t test
Foster Care Intervention: Independent sample t-tests revealed CAUG children’s performance on the SCQ was worse than performance of children in the FCG. In particular, scores in the reciprocal social interaction domain were worse in the CAUG than in the FCG. Scores in the communication domain, and the restricted/repetitive behaviors domain, were not significantly different between CAUG and FCG (Table 1). Within the FCG, SCQ scores did not significantly correlate with age at placement (R2 = .001, B = .016, Standard Error = .091, β = .024).
After controlling for demographics and birth history by regression, group status (CAUG, FCG, or NIG) was still a significant predictor of SCQ score (see Table S1, available online).
SCQ scores significantly correlated with SSRS scores for social skills and problem behaviors, as assessed by parents and teachers. SCQ scores were not significantly correlated with SSRS scores for academic competence (see Table S2, available online).
Analysis by current living situation: Group means for percent of lifetime spent in the institution were as follows: CAUG 53.8% (SD 26.8%); FCG 19.8% (SD 7.8%). ANOVA revealed a significant between-group difference in SCQ score (F(3,91) = 4.96, p = .003). Post hoc Bonferroni analysis yielded significant differences (p < .05) in SCQ score between children living in institutions at the time of the study and those living in family-based care, but no significant differences in SCQ score between children in the various types of family-based care (biological family, government foster care, or BEIP foster care; Table 2).
Table 2.
Social Communication Questionnaire (SCQ) Score by Placement at 8 Years of Age
| Placement at 8 years | n | SCQ Score |
|---|---|---|
| Institution | 11 | 11.7 (14.6) |
| BEIP foster care | 33 | 2.5 (5.5)** |
| Reintegrated with biological family | 31 | 2.9 (6.6)** |
| Government foster care | 20 | 3.0 (4.5)* |
Note: All SCQ scores are expressed as mean (SD). BEIP = Bucharest Early Intervention Project.
p ≤ .05,
p ≤ .01, as compared to Institutional placement
Correlation with IQ: Pearson correlations revealed that SCQ score was significantly associated with full scale IQ score, and each IQ subtest, in the FCG group. SCQ score was not significantly associated with full scale IQ score, or any IQ subtest, in the CAUG or NIG groups (see Table S3, available online).
Autism Diagnosis
3 of 57 CAUG children, 2 of 60 FCG children, and 0 of 100 NIG children met DSM-IV (and DSM-5) criteria for ASD.
Patient 1 (FCG) received an SCQ score of 24. He was born at 39 weeks weighing 3450g. He spent 2.5 months with his biological family before being placed in an institution, and was placed in BEIP foster care at 30 months of age. He remained with the same foster family since initial placement, although his foster father passed away when he was 8 years old. He was toilet trained and learned to dress himself at 9 years of age; he still had difficulty tying his shoes at the time of examination. Medications, prescribed by his local neurologist, included risperidone, gingko biloba, and hydrolyzed pig brain peptide. Physical examination was notable for three relatively large hyperpigmented areas on the skin; one 3cm, one 7cm, and one 11x20cm. Head circumference was 5–10th percentile. When asked to draw a picture, he drew a detailed train but had difficulty correctly approximating the edges of the lines to meet up correctly. He demonstrated some intermittent toe walking.
Social Communication: By history, he did not say any words when he started in foster care. His foster family had difficulty understanding him until he was about 5 years of age. He required reminders to make eye contact, particularly with other children his age. He often interrupted others when they were speaking and tended to refocus conversations to subjects that interested him. He tended to play in parallel with peers. Upon examination, he initially avoided eye contact, and later in the exam made inappropriately prolonged eye contact. While he was able to name many children in his class and list facts about them (describing, for example, that one girl is 15 years old, one boy often fights with other children, and one girl helps him make bracelets), he was unable to describe the difference between a friend and a classmate. When asked whether he feels happy or sad when he is alone, he answered that he feels happy. However, when asked what it feels like to be sad, he said, “alone.” When asked what makes him sad, he responded inappropriately, “To get happier.” When asked to make up a story about a picture of a farm, he named all the objects and animals on the farm; when asked specific questions (e.g., “Who do you think is in that house?”), he gave short and relatively unimaginative answers (e.g., “A family”).
Restricted and Repetitive Behaviors: By history, he became agitated if the routine changed at home. He displayed some motor stereotypies, including rocking, jumping, and making a tremoring motion with his elbows bent and his cheeks and lips moving when he was frustrated. When upset, he chewed his nails until they bled, talked continuously, and hit himself. On examination, he tended to echo the ends of his own sentences in a quieter voice. He provided information about specific interests without contextual prompts to do so, for example telling the examiner the numbers and routes of several buses on the local bus route.
Patient 2 (FCG) did not have an SCQ completed because the SCQ was added to the study protocol after his study visit, but he was referred due to staff concern. He was born at 38 weeks weighing 2900g. He was institutionalized at 2 months of age and randomized to foster care, which is where he was living at the time of his regular study visit. He had undergone a total of four care transitions, and had spent 27% of his life in an institution. However, due to behavioral concerns, his foster family felt unsafe caring for him, and by the time of his second level evaluation for autism, he had been moved back to a placement center. His head circumference was 10–25th percentile. Medications included risperidone, carbamazepine, and topiramate. He did not generally play with toys; he looked at them briefly and put them down. His gait was slightly wide-based but stable.
Social Communication: By history, he had not established relationships with peers. When the examiner pretended to fall and hurt her foot during the exam, he did not notice; when she pretended to cry, he looked briefly towards her, smiled slightly as if amused, and then turned back to look at some blocks. When the examiner smiled in front of him, he copied her facial expression one out of four times, but the expression looked like showing his teeth rather than an emotional smile. His caregiver described that he did show objects of interest to share enjoyment, and could point to indicate wants. He did turn to his name. His only words were “da” (yes) and “nu” (no), and he was able to appropriately use these words when asked if he wanted something, though tended to respond only when he was able to see the object in question. When told to “Say pa!” (say goodbye), he said “Da!” (yes). He appeared to enjoy playing with bubbles and clapped when others in the room clapped; however, he did not point to the bubbles, make eye contact with the examiner or check to see if she was watching the bubbles, or make any effort to request more bubbles.
Restricted and Repetitive Behaviors: When given a car, he turned it upside down and spun the wheels. By history, he displayed no focused interests, but agitation (running and hitting himself) with changes in routine. He frequently rocked between his front and back foot while standing, and when agitated or excited, he raised both arms above his head with the wrists flexed.
Patient 3 (CAUG) received an SCQ score of 33. She was born at 38 weeks weighing 2700g. She was institutionalized immediately at birth and has remained institutionalized her entire life. Her history was limited during the visit, as her caregiver from the institution was unable to stay for the visit. Head circumference was 75th percentile. She remained in diapers. She squatted in order to play, and did not sit in a chair or on the floor at all during the examination. She had a tendency to walk on her tiptoes.
Social Communication: She said no words, and responded only to very simple commands (e.g., “Come here.”) She vocalized only twice during the exam, whispering “Aaah” once spontaneously, and once when her caregiver reminded her to “say goodbye.” She made no eye contact, even when the examiner’s face was directly in front of her. She did not point, or look in the direction of a point. She used no gestures; according to her SCQ, she also had not used gestures at 4–5 years of age. On exam, she had no response when the examiner pretended to fall and cry. She did not make any efforts to show or share objects of interest with others. She demonstrated no functional or imaginative play.
Restricted and Repetitive Behaviors: She had some preferred objects, such as a pink spoon that she liked to carry in her pocket. When the examiner tried to blow bubbles, she took the bubble wand and broke it into small pieces, then carried it with her for the remainder of the visit. She spent a large part of the visit taking objects out of a bin and taking them apart when possible. During the examination, she spent some time looking closely at a white wall (possibly observing the heating unit on the wall), and at the video camera.
Patient 4 (CAUG) received an SCQ score of 33. She was born at 34 weeks weighing 2000g to an adolescent mother who had run away from home and returned pregnant; the mother died several years later. The research participant was institutionalized immediately at birth, and after a total of four transitions (having spent 34% of her life institutionalized), she was reintegrated with her biological family and came to the visit with her maternal grandmother. Her head circumference was 75th percentile. She was not yet toilet trained, but she could indicate when she needed to use the bathroom. She ate only purees until 8 years of age. She hit herself and kicked when she was upset. She generally slept well, although if anyone awoke her overnight, she would not go back to sleep.
Social Communication: By history, she said about 10 words, and followed simple one-step commands. She always played alone. She did not appear to notice when her grandmother was sad. On examination, her eye contact was only present when the examiner placed herself directly in front of her gaze. She used the examiner’s hand as a tool to remove a remote control car when it became caught on an object. She copied the examiner’s smile on most occasions, but did not appear surprised or change her expression when the examiner abruptly returned to a straight face. She turned to her name, but did not follow the examiner’s gaze or point without speech. She frequently appeared to be watching the examiner’s earrings rather than her face. She played with a doll and gave the doll to the examiner to hold while she pretended to feed the doll; however, she was quite rough in her handling of the doll, pressing the bottle in the direction of the doll’s mouth with considerable force.
Restricted and Repetitive Behaviors: By history, she became upset when the family changed the route they took to school. She played with toys by taking them apart into their individual pieces, although she also had a particular interest in dolls and pacifiers. She had frequent immediate echolalia, repeating most of the single words that were said to her in Romanian or English. She rocked occasionally, perseverated on wanting to play with bubbles, and tried to bolt from the room when the bubbles were removed.
Patient 5 (CAUG) received an SCQ score of 32. He was born at 38 weeks weighing 3900g. He was institutionalized immediately at birth, and after a total of five transitions (having spent 91% of his life institutionalized), he was again living in an institution at the time of examination. Head circumference was <5th percentile, and his ears were large. Medications included risperidone, zuclopentixol, trihexyphenidyl, carbamazepine, and nitrazepam. He was not toilet trained.
Social Communication: By history, he did not like to be around other children. He did not make eye contact, point, or turn to his name. He did not show his caregivers objects of interest, share enjoyment, or appear to notice when someone around him appeared happy or sad. On examination, he said no words and followed no commands.
Restricted and Repetitive Behaviors: He arrived to the visit wrapped in a hospital gown with his arms wrapped next to his body; his caregivers described that he liked the pressure from this. He had repetitive clicking of his tongue. He frequently stood on his toes and rocked back and forth. When agitated, he would occasionally hit himself, or hit or kick those around him.
Discussion
These results confirm and expand upon previous findings of increased risk for social communication difficulties, restricted/repetitive behaviors, and ASD in children with a history of institutionalization.2, 3, 5, 34, 35 History of institutionalization was associated with higher SCQ scores across all domains. Foster care placement was associated with improved SCQ scores, particularly in the reciprocal social interaction domain. Although foster care has previously been associated with a specific reduction in stereotypies,17 in this study foster care did not reduce the broader range of restricted/repetitive behaviors associated with ASD. These results indicate that placement in families leads to improved social communication skills amongst children exposed to early psychosocial deprivation.
We identified five children who met DSM criteria for ASD from amongst the 117 ever-institutionalized children examined in our study. Although such small numbers must be considered with caution, that is approximately a 3-fold increase from what would be expected in a typical community sample;36 in fact, none of the children from the never-institutionalized population in this study received an ASD diagnosis. Thus, a history of institutionalization appears to be related to an increased incidence of ASD, as seen in previous studies.2, 3, 5
This study has several limitations. While randomization of children to the CAUG or FCG allowed us to show specifically that the caregiving environment after initial institutionalization impacts SCQ scores, the process of abandonment itself was not random. Therefore, this study cannot address the degree to which differences between ASD rates (and SCQ scores) between ever-institutionalized and never-institutionalized children are from institutionalization itself versus genetic and prenatal factors that increase both the risk of abandonment and the risk of ASD. Additionally, the study’s non-interference policy led many children who were initially randomized to the CAUG to later be placed in government-sponsored foster care that did not exist when the study began, or to be reunited with their biological families; this would most likely underestimate the impact of foster care placement of SCQ score because the living situation for children in the CAUG became more similar to that of children in the FCG over time. Because SCQ scores are based on parent report, the possibility of observer bias exists (a problem with all parent report measures). Finally, the rates of ASD in the ever-institutionalized group, while large enough to suggest that institutionalization history is associated with increased ASD risk, are not large enough to allow determination of whether placement after initial institutionalization (CAUG versus FCG) significantly affects ASD rates.
Prior studies have suggested that children with a history of institutionalization have a syndrome of quasi-autism that differs from classical ASD diagnosed in children without a history of institutionalization.2, 3, 5, 34 Our sample of children diagnosed with ASD is too small to make definitive statements about quasi-autism in this group, although it is worth noting that 2/5 children with ASD in our sample are female, and 0/5 children who met criteria for ASD had macrocephaly (although the true association between ASD and macrocephaly has been called into question recently).37 Of note, prior studies have also shown decreasing symptomatology over time in quasi-autism, but because SCQ data were collected at a single point in time, our study is not able to evaluate change over time. However, the fact remains that some children described herein met criteria for ASD as defined by DSM criteria, raising questions about whether children with a history of institutionalization are at increased risk for true ASD and not simply an ASD-like syndrome.
On the other hand, one reason for using the terms “quasi-autism” or PIAS to describe patterns of behavior seen in children with a history of institutionalization is to avoid any misinterpretation or erroneous extension of these findings to suggest that ASD occurs purely as a result of early psychosocial deprivation. In “quasi-autism,” severe environmental deprivation seems contributory to the phenotype (perhaps exacerbating underlying risk factors such as genetic predisposition, prenatal environment, and postnatal exposures), whereas in the vast majority of ASD cases, children are raised in caring families, and psychosocial deprivation does not play a significant role. The phenotypic similarities between these disorders may occur due to deprivation of differing types; in institutionalized children, the deprivation is environmentally induced, whereas in classic ASD, the disorder itself induces deprivation by causing children to have greater difficulty perceiving and understanding social cues from a typical environment.
It is interesting to note that SCQ scores increased as total percentage of a child’s life spent in an institution increased and were also elevated in children who were living in institutions at age 8. There are a number of potential causes for these findings. One is that cumulative time spent in an institution exacerbates social communication difficulties due to the lack of social stimulation and contingent responsivity found in typical families. A second possibility is that among children in the CAUG, those with greater social communication difficulties were less likely to be placed in family settings and so remained in the institution.
Among children randomized to foster care, SCQ score correlated with IQ score; this correlation was not present in the CAUG or NIG. One potential explanation for this finding is that those children who obtain maximal cognitive benefits from foster care are the same children who obtain maximal social benefits; in other words, IQ and SCQ scores may be linked on the pathway to recovery although not closely linked otherwise.29 Further research is necessary to better understand what may make some children better able to glean these benefits than others.
The results of this study suggest that early psychosocial deprivation is associated with greater social communication difficulties and an increased incidence of meeting criteria for ASD. High-quality foster care improves social communication in this population; this adds to the growing list of developmental domains that are altered in children with a history of institutionalization and can be improved by foster care, including attachment,15, 23, 24 stereotypies,17 language,38–40 cognition,31, 41 depression, anxiety,42, 43 and growth.44 However, high-quality foster care alone does not sufficiently eliminate the risk of quasi-autism in this population, and further studies evaluating the effects of specific interventions for this syndrome would be of benefit.
Supplementary Material
Clinical Guidance.
Children with a history of institutionalization are at increased risk for social communication difficulties, restricted/repetitive behaviors, and autism spectrum disorder.
Family-centered placement (rather than continued institutionalization) improves scores on the SCQ, particularly in the reciprocal social interaction domain.
Acknowledgments
The Sinneave Foundation, the John D. and Catherine T. MacArthur Foundation, the Binder Family Foundation, and the National Institute of Mental Health (MH091363) provided funding for this project (C.A.N.).
Disclosure: Dr. Levin has received grant funding from the Autism Science Foundation, the American Brain Foundation, the Nancy Lurie Marks Family Foundation, the Office of Graduate Medical Education and the Program for Patient Safety and Quality at Boston Children’s Hospital, and the Children’s Hospital Neurology Foundation at Boston Children’s Hospital. Dr. Fox has received grant funding from the National Institute of Mental Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the Binational Science Foundation. He has received royalties from Guilford Press, Oxford University Press, Wiley Press, and Harvard University Press. He has received honoraria for lectures to professional audiences. Dr. Zeanah has received grant support from the National Institute of Mental Health, the Irving Harris Foundation, and the Substance Abuse and Mental Health Services Administration. He has received royalties from Guilford Press and Harvard University Press. He has received honoraria for lectures to professional audiences. Dr. Nelson has received grant funding from the National Institute on Deafness and Other Communication Disorders, the US Department of Defense, the Simons Foundation, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the Rockefeller Center for Latin American Studies, an anonymous foundation donor, ANGEL, Merck, Grand Challenges/Canada, the Translational Research Program, and the Gates Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
April R. Levin, Laboratories of Cognitive Neuroscience at Boston Children's Hospital/Harvard Medical School, Boston.
Nathan A. Fox, University of Maryland, College Park.
Charles H. Zeanah, Jr., Tulane University School of Medicine, New Orleans.
Charles A. Nelson, Laboratories of Cognitive Neuroscience at Boston Children’s Hospital/Harvard Medical School, and the Harvard Center on the Developing Child, Cambridge, MA.
References
- 1.Nelson CA, Fox NA, Zeanah CH. Romania’s Abandoned Children. Cambridge, MA: Harvard University Press; 2014. [Google Scholar]
- 2.Rutter M, Andersen-Wood L, Beckett C, et al. Quasi-autistic Patterns Following Severe Early Global Privation. J Child Psychol Psychiatry. 1999;40(4):537–549. [PubMed] [Google Scholar]
- 3.Rutter M, Kreppner J, Croft C, et al. Early adolescent outcomes of institutionally deprived and non-deprived adoptees. III. Quasi-autism. J Child Psychol Psychiatry. 2007;48(12):1200–1207. doi: 10.1111/j.1469-7610.2007.01792.x. [DOI] [PubMed] [Google Scholar]
- 4.Rutter M, Colvert E, Kreppner J, et al. Early adolescent outcomes for institutionally-deprived and non-deprived adoptees. I: disinhibited attachment. J Child Psychol Psychiatry. 2007;48(1):17–30. doi: 10.1111/j.1469-7610.2006.01688.x. [DOI] [PubMed] [Google Scholar]
- 5.Hoksbergen R, ter Laak J, Rijk K, van Dijkum C, Stoutjesdijk F. Post-Institutional Autistic Syndrome in Romanian adoptees. J Autism Dev Disord. 2005;35(5):615–623. doi: 10.1007/s10803-005-0005-x. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Publishing, Inc; 2000. [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Edition. Arlington, VA: American Psychiatric Publishing, Inc; 2013. [Google Scholar]
- 8.Fombonne E. Epidemiological surveys of autism and other pervasive developmental disorders: an update. J Autism Dev Disord. 2003;33(4):365–382. doi: 10.1023/a:1025054610557. [DOI] [PubMed] [Google Scholar]
- 9.Hodges J, Tizard B. Social and family relationships of ex-institutional adolescents. J Child Psychol Psychiatry. 1989;30(1):77–97. doi: 10.1111/j.1469-7610.1989.tb00770.x. [DOI] [PubMed] [Google Scholar]
- 10.Chisholm K. A three year follow-up of attachment and indiscriminate friendliness in children adopted from Romanian orphanages. Child Dev. 1998;69(4):1092–1106. [PubMed] [Google Scholar]
- 11.MacLean K. The impact of institutionalization on child development. Dev Psychopathol. 2003;15(4):853–884. doi: 10.1017/s0954579403000415. [DOI] [PubMed] [Google Scholar]
- 12.Roy P, Rutter M, Pickles A. Institutional care: associations between overactivity and lack of selectivity in social relationships. J Child Psychol Psychiatry. 2004;45(4):866–873. doi: 10.1111/j.1469-7610.2004.00278.x. [DOI] [PubMed] [Google Scholar]
- 13.Gunnar MR, van Dulmen MHM. Behavior problems in postinstitutionalized internationally adopted children. Dev Psychopathol. 2007;19(1):129–148. doi: 10.1017/S0954579407070071. [DOI] [PubMed] [Google Scholar]
- 14.Erol N, Simsek Z, Münir K. Mental health of adolescents reared in institutional care in Turkey: challenges and hope in the twenty-first century. Eur Child Adolesc Psychiatry. 2010;19(2):113–124. doi: 10.1007/s00787-009-0047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smyke AT, Zeanah CH, Gleason MM, et al. A randomized controlled trial comparing foster care and institutional care for children with signs of reactive attachment disorder. Am J Psychiatry. 2012;169(5):508–514. doi: 10.1176/appi.ajp.2011.11050748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almas AN, Degnan KA, Radulescu A, Nelson CA, Zeanah CH, Fox NA. Effects of early intervention and the moderating effects of brain activity on institutionalized children’s social skills at age 8. Proc Natl Acad Sci U S A. 2012;109(Suppl):17228–17231. doi: 10.1073/pnas.1121256109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bos KJ, Zeanah CH, Smyke AT, Fox NA, Nelson CA. Stereotypies in children with a history of early institutional care. Arch Pediatr Adolesc Med. 2010;164(5):406–411. doi: 10.1001/archpediatrics.2010.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shattuck PT, Durkin M, Maenner M, et al. Timing of identification among children with an autism spectrum disorder: findings from a population-based surveillance study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):474–483. doi: 10.1097/CHI.0b013e31819b3848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zwaigenbaum L. Advances in the early detection of autism. Curr Opin Neurol. 2010;23(2):97–102. doi: 10.1097/WCO.0b013e3283372430. [DOI] [PubMed] [Google Scholar]
- 20.Kligman G. The Politics of Reproduction in Ceausescu’s Romania: a Case Study in Political Culture. East Eur Polit Soc. 1992;6(3):364–418. [PubMed] [Google Scholar]
- 21.Greenwell F. The impact of child welfare reform on child abandoment and deinstitutionalization, Romania 1990–2000. Ann Demogr Hist (Paris) 2006;1:133–157. [Google Scholar]
- 22.Johnson DE, Miller LC, Iverson S, et al. The Health of Children Adopted From Romania. J Am Med Assoc. 2014;268(24):3446–3451. [PubMed] [Google Scholar]
- 23.Smyke AT, Zeanah CH, Fox NA, Nelson CA, Guthrie D. Placement in foster care enhances quality of attachment among young institutionalized children. Child Dev. 2010;81(1):212–223. doi: 10.1111/j.1467-8624.2009.01390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeanah CH, Smyke AT, Koga SF, Carlson E. Attachment in institutionalized and community children in Romania. Child Dev. 2005;76(5):1015–1028. doi: 10.1111/j.1467-8624.2005.00894.x. [DOI] [PubMed] [Google Scholar]
- 25.Zeanah CH, Nelson CA, Fox NA, et al. Designing research to study the effects of institutionalization on brain and behavioral development: the Bucharest Early Intervention Project. Dev Psychopathol. 2003;15(4):885–907. doi: 10.1017/s0954579403000452. [DOI] [PubMed] [Google Scholar]
- 26.Zeanah CH, Fox NA, Nelson CA. The Bucharest Early Intervention Project: case study in the ethics of mental health research. J Nerv Ment Dis. 2012;200(3):243–247. doi: 10.1097/NMD.0b013e318247d275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smyke AT, Zeanah CH, Fox NA, Nelson CA. A new model of foster care for young children: The Bucharest Early Intervention Project. Child Adolesc Psychiatr Clin N Am. 2009;18(3):721–734. doi: 10.1016/j.chc.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Zeanah CH, Nelson CA. Ethical Considerations in International Research Collaboration: The Bucharest Early Intervention Project. Infant Ment Health J. 2006;27(6):559–576. doi: 10.1002/imhj.20107. [DOI] [PubMed] [Google Scholar]
- 29.Rutter M, Bailey A, Lord C. The Social Communication Questionnaire Manual. Torrance, CA: Western Psychological Services; 2003. p. 8. [Google Scholar]
- 30.Gresham FM, Elliott SN. Social Skills Rating System. Circle Pines, MN: American Guidance Service; 1990. [Google Scholar]
- 31.Fox NA, Almas AN, Degnan KA, Nelson CA, Zeanah CH. The effects of severe psychosocial deprivation and foster care intervention on cognitive development at 8 years of age: findings from the Bucharest Early Intervention Project. J Child Psychol Psychiatry. 2011;52(9):919–928. doi: 10.1111/j.1469-7610.2010.02355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roche AF, Mukherjee D, Guo S, Moore WM. Head Circumference Reference Data: Birth to 18 Years. Pediatrics. 1987;79(5):706–712. [PubMed] [Google Scholar]
- 33.Levin AR, Zeanah CH, Fox NA, Nelson CA. Motor outcomes in children exposed to early psychosocial deprivation. J Pediatr. 2014;164(1):123.e1–129.e1. doi: 10.1016/j.jpeds.2013.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Federici RS. Help for the Hopeless Child: A Guide for Families (With Special Discussion for Assessing and Treating the Post-Institutionalized Child) Alexandria, VA: Federici, Ronald S. and Associates; 1998. [Google Scholar]
- 35.Landgren M, Andersson Grönlund M, Elfstrand P-O, Simonsson J-E, Svensson L, Strömland K. Health before and after adoption from Eastern Europe. Acta Paediatr. 2006;95(6):720–725. doi: 10.1080/08035250500455871. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. Prevalence of Autism Spectrum Disorder among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2010. Atlanta: CDC; 2014. pp. 1–21. [PubMed] [Google Scholar]
- 37.Barnard-Brak L, Sulak T, Hatz JKI. Macrocephaly in children with autism spectrum disorders. Pediatr Neurol. 2011;44(2):97–100. doi: 10.1016/j.pediatrneurol.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 38.Windsor J, Benigno JP, Wing CA, et al. Effect of foster care on young children’s language learning. Child Dev. 2011;82(4):1040–1046. doi: 10.1111/j.1467-8624.2011.01604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Windsor J, Glaze LE, Koga SF. Language acquisition with limited input: Romanian institution and foster care. J Speech Lang Hear Res. 2007;50(5):1365–1381. doi: 10.1044/1092-4388(2007/095). [DOI] [PubMed] [Google Scholar]
- 40.Windsor J, Moraru A, Nelson CA, Fox NA, Zeanah CH. Effect of foster care on language learning at eight years: Findings from the Bucharest Early Intervention Project. J Child Lang. 2013;40(3):605–627. doi: 10.1017/S0305000912000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelson CA, Zeanah CH, Fox NA, Marshall PJ, Smyke AT, Guthrie D. Cognitive recovery in socially deprived young children: the Bucharest Early Intervention Project. Science (80- ) 2007;318(5858):1937–1940. doi: 10.1126/science.1143921. [DOI] [PubMed] [Google Scholar]
- 42.Zeanah CH, Egger HL, Smyke AT, et al. Institutional rearing and psychiatric disorders in Romanian preschool children. Am J Psychiatry. 2009;166(7):777–785. doi: 10.1176/appi.ajp.2009.08091438. [DOI] [PubMed] [Google Scholar]
- 43.Bos K, Zeanah CH, Fox NA, Drury SS, McLaughlin KA, Nelson CA. Psychiatric outcomes in young children with a history of institutionalization. Harv Rev Psychiatry. 2011;19(1):15–24. doi: 10.3109/10673229.2011.549773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnson DE, Guthrie D, Smyke AT, et al. Growth and associations between auxology, caregiving environment, and cognition in socially deprived Romanian children randomized to foster vs ongoing institutional care. Arch Pediatr Adolesc Med. 2010;164(6):507–516. doi: 10.1001/archpediatrics.2010.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.